Abstract
Objectives. To investigate racial/ethnic and gender inequities in the compensation and benefits of US health care workers and assess the potential impact of a $15-per-hour minimum wage on their economic well-being.
Methods. Using the 2017 Annual Social and Economic Supplement to the Current Population Survey, we compared earnings, insurance coverage, public benefits usage, and occupational distribution of male and female health care workers of different races/ethnicities. We modeled the impact of raising the minimum wage to $15 per hour with different scenarios for labor demand.
Results. Of female health care workers, 34.9% of earned less than $15 per hour. Nearly half of Black and Latina female health care workers earned less than $15 per hour, and more than 10% lacked health insurance. A total of 1.7 million female health care workers and their children lived in poverty. Raising the minimum wage to $15 per hour would reduce poverty rates among female health care workers by 27.1% to 50.3%.
Conclusions. Many US female health care workers, particularly women of color, suffer economic privation and lack health insurance. Achieving economic, gender, and racial/ethnic justice will require significant changes to the compensation structure of health care.
Women constitute the vast majority of health care workers in the United States. Although most US physicians are male, women occupy more than 85% of positions as nurses and as nursing, home health, and personal care aides.1 Nearly 20% of women in the US workforce are employed in health care, and this share is likely to grow in coming years given projected growth in women-dominated health care fields.2 The US Bureau of Labor Statistics anticipates that health care employment will increase nearly twice as fast as the population, and 5 of the 10 occupations projected to have the greatest employment growth through 2026 are in health care, with “home health care services”—an occupation whose workforce is 88% female—leading the projections.3,4
The wages and benefits of health care workers thus have significant implications for women’s economic well-being and, consequently, their health. This is of particular importance given that many health care jobs in which women represent the majority of workers are low paying—and even within the same jobs, women tend to be paid less than their male counterparts.5 There is also significant evidence that workers of color across all industries receive lower compensation than do their White colleagues, with women of color particularly disadvantaged.6 Within health care, Black women were the only group of women who experienced a decline in median wages between 2005 and 2015, from $16.06 to $15.71 per hour.7
Existing literature has briefly described the experiences of specific demographic groups and health care professions, as well as the health insurance coverage of health care workers before the passage of the Affordable Care Act.7–17 However, a systematic analysis of the gender and racial/ethnic distribution of wages among workers across the health care industry—and the prevalence of poverty, uninsurance, and poor health among low-wage female workers of different races—has not been conducted. Moreover, the possible effects of labor market policies on socioeconomic and health outcomes among female health care workers are not known.
This study addresses this critical gap in the literature with nationally representative US data from 2017. We first examined wage distributions for male and female workers in the US health care system, as well as racial/ethnic subgroups of female workers, quantifying the share of workers of each demographic group currently earning less than $15 per hour. We then examined rates of poverty, insurance coverage, public benefit utilization, and poor self-reported health among female and male health care workers, and among women of different races/ethnicities. Finally, we assessed potential consequences of raising the minimum wage to $15 per hour, a popular policy proposal recently adopted by 6 major US cities and by several large private hospital systems and health insurance firms.18–20
METHODS
We used data from the 2017 Annual Social and Economic (ASEC) Supplement to the Current Population Survey (CPS), a population-based survey conducted by the US Census Bureau and the Bureau of Labor Statistics.21 The ASEC collects nationally representative data on the noninstitutionalized US civilian population, including detailed information on income and noncash benefits (e.g., food subsidies and health insurance). Health care workers within the ASEC were identified via industry of employment codes (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org). Industry (rather than occupation) codes were used to identify health care workers to ensure that relevant “nonmedical” workers, such as hospital food service workers, were included in our analysis.
We computed hourly wages for all workers by summing all wage, salary, and “non-farm business” income and dividing by the hours worked per year (the product of weeks worked and usual hours worked per week). We constructed measures of household poverty, health insurance coverage, public housing assistance, and self-reported health. We used weights provided by the Census Bureau to yield nationally representative estimates. Additional details are provided in Appendix A.
We computed descriptive statistics for men and women and for women of different self-reported races/ethnicities in the health care and general workforce, comparing hourly wages and household incomes. For each demographic group, we also assessed the proportion earning less than $15 per hour, the proportion of workers and their children living below the federal poverty line and below 200% of poverty (using health care workers’ self-reported number of dependent children living in their households), receipt of public housing assistance, health insurance coverage, and the proportion rating their overall health as “poor” or “fair” (as opposed to “good,” “very good,” or “excellent”). We also examined differences in the occupation distribution for each of the demographic groups. Specifically, we examined the proportion employed in each of the 5 largest health care occupations represented in the data (determined on the basis of the ranking of the weighted number of workers within the health care industry with CPS occupation codes). We did not conduct analyses of differences in economic outcomes within occupations because of sample size limitations.
We then estimated the potential impacts on wages, poverty rates, and income of raising the minimum wage to $15 per hour, a policy that is prominent in public debate and has been adopted by 6 US cities and independently by some private health care organizations.18–20 We considered 2 alternative scenarios for this simulation. First, we examined the case in which the demand for low-wage health care labor is inelastic—that is, employers would not reduce the size of their workforce or the hours employees worked in response to the minimum wage change. The majority of empirical studies on minimum wage increases, including those focused on the health care industry, have suggested that disemployment from implementation of minimum wage policies is minimal.22,23 Indeed, health care employment may be particularly resistant to disemployment effects of raising the minimum wage, as an aging population has increased demand for health care services, and most low-wage health care jobs are not easily automated or exported.24
We then evaluated a scenario with a high elasticity of demand for low-wage health care labor. This analysis was based on a recent study that found that raising the minimum wage in Seattle, Washington, to $13 per hour resulted in a 9.4% loss of hours by low-wage workers (defined as those earning less than $19 per hour).25 This study was used as the basis for our second analysis for 2 reasons. First, it represents 1 of the few empirical studies of US minimum wages in the range of $15 per hour. Second, this study is an outlier relative to the literature in terms of the disemployment effects it identifies; thus, our second analysis represents a conservative estimate of the positive effects of a $15-per-hour minimum wage.23 We viewed our analysis as descriptive, as we did not assume any positive spillover effects of the minimum wage increase on workers earning more than $15 per hour or any negative effects on receipt of public benefits. In addition, the analysis did not consider any potential loss of fringe benefits with implementation of minimum wage policies, though the evidence in the economics literature on whether such losses occur is mixed.26
We conducted all analyses with SAS 9.4 statistical software (SAS Institute, Cary, NC). We used the χ2 test to derive confidence intervals (CIs) and P values and balanced repeated replication with replicate weights provided by the CPS, which account for the survey’s complex sample design.
RESULTS
Our sample included 185 914 adult survey respondents (weighted population = 320.4 million) of whom 10 477 respondents (weighted population = 18.6 million) were health care workers and 8089 (weighted population = 14.2 million) were female health care workers. Among female health care workers in the sample, 1249 were Black (weighted population = 2 368 338), 1109 were Latina (weighted population = 1 732 923), 84 were Native American (weighted population = 97 698), 557 were Asian (weighted population = 919 042), 4972 were White (weighted population = 8 875 959), and 118 were other races (weighted population = 196 327).
Of all employed women, 18.2% (95% CI = 17.6%, 18.8%) were employed in health care (as compared with 5.1% [95% CI = 4.9%, 5.2%] of employed men) and the share of health care workforce who were women was far higher than the share in all other industries (76.4% [95% CI 74.4%, 78.4%] vs 43.3% [95% CI = 40.6%, 46.0%]; P < .001). Black women were particularly overrepresented, with 23.8% (95% CI = 22.7%, 24.8%) of all employed Black women working in health care.
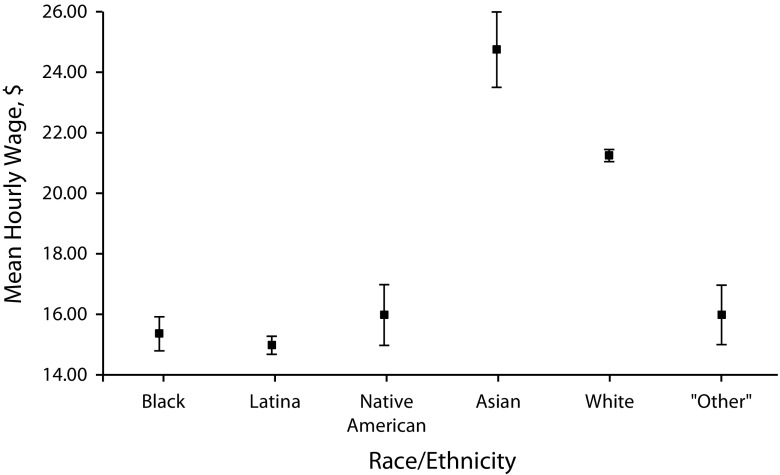
The median hourly wage for female health care workers ($19.23; 95% CI = $19.02, $19.44) was higher than for women in other industries ($16.34; 95% CI = $16.20, $16.49; P < .001), but was 24.9% less than that of male health care workers ($25.46; 95% CI = $24.80, $26.12; P < .001). Among female health care workers, median hourly wages varied dramatically by race/ethnicity (Figure 1). Latina women had the lowest median hourly wages ($15.00; 95% CI = $14.62, $15.30), followed by Black women ($15.38; 95% CI = $14.84, $15.89). Native American and “other” female health care workers both had median hourly wages of $16.00 (95% CIs = $14.99, $17.00 and $14.95, $16.98, respectively). By contrast, White women had a median hourly wage of $21.24 (95% CI = $21.00, $21.44) and Asian women had a median hourly wage of $24.73 (95% CI = $23.37, $25.97).
FIGURE 1—
Median Hourly Wages of Female Health Care Workers, by Self-Identified Race/Ethnicity: Annual Social and Economic Supplement to the Current Population Survey, United States, 2017
Note. All values were calculated by using Current Population Survey sampling weights, and confidence intervals were derived by using balanced repeated replication with replicate weights provided by the Current Population Survey.
The median household income of men working in health care was 25.0% higher than that of women working in health care ($100 022 [95% CI = $97 089, $102 955] vs $80 000 [95% CI = $78 692, $81 307]; P < .001). The gender disparity in the health care industry was larger than in other industries, where male employees’ median income exceeded that of female employees by 7.5% ($78 503 [95% CI = $78 014, $78 992] vs $72 999 [95% CI = $72 429, $73 568]; P < .001). We found substantive racial/ethnic differences in household income for female health care workers. Native American women had the lowest median household income ($54 026; 95% CI = $48 206, $59 669), followed closely by Black women ($55 010; 95% CI = $53 209, $56 805), “other” women ($59 747; 95% CI = $50 741, $68 526), and Latina women ($60 000; 95% CI = $57 171, $62 273). White female health care workers had a median household income of $88 684 (95% CI = $87 384, $89 897) and Asian women $117 006 (95% CI = $112 382, $121 621).
Table 1 compares the socioeconomic characteristics of female and male health care workers. Women were significantly more likely than were men to earn less than $15 per hour (34.9% vs 23.4%; P < .001), and to live in poverty (5.0% vs 2.4%; P < .001); indeed, 87% of all health care workers in poverty were women. In addition, 7.7% (weighted population = 1 003 621; 95% CI = 6.8%, 8.7%) of female health care workers’ children lived in poverty. In total, 1.7 million female health care workers and their children lived in poverty.
TABLE 1—
Characteristics of Health Care Workers by Gender: Annual Social and Economic Supplement to the Current Population Survey, United States, 2017
| Women |
Men |
|||
| No. | % of Workers or Their Children (95% CI) | No. | % of Workers or Their Children (95% CI) | |
| Weighted no. | 14 190 336 | 100 | 4 388 700 | 100 |
| Wage < $15/h | 4 954 876 | 34.9 (34.1, 35.8) | 1 026 912 | 23.4 (21.3, 25.5) |
| Workers with household incomes < 100% of federal poverty line | 702 429 | 5.0 (4.4, 5.5) | 104 865 | 2.4 (1.9, 2.8) |
| Children with household incomes < 100% of federal poverty line | 1 003 621 | 7.7 (6.8, 8.7) | 81 158 | 2.4 (2.3, 2.5) |
| Workers with household incomes < 200% of federal poverty line | 2 542 515 | 17.3 (16.2, 18.4) | 428 427 | 9.8 (8.9, 10.6) |
| Children with household incomes < 200% of federal poverty line | 3 401 992 | 26.2 (24.3, 28.2) | 331 601 | 9.8 (9.2, 10.3) |
| Receive food stamps | 1 062 821 | 7.5 (6.7, 8.2) | 173 529 | 4.0 (3.4, 4.5) |
| Live in public housing or receive rent subsidy | 374 049 | 2.6 (2.1, 3.2) | 69 015 | 1.6 (1.3, 1.9) |
| Uninsured | 1 012 298 | 7.1 (6.5, 7.8) | 341 871 | 7.8 (6.8, 8.9) |
| Medicaid | 1 415 365 | 10.0 (9.2, 10.8) | 286 198 | 6.5 (5.9, 7.2) |
| Report poor or fair self-rated health | 829 769 | 5.8 (5.2, 6.5) | 203 893 | 4.6 (4.2, 5.1) |
| Occupation | ||||
| Registered nurses (median wage $31.25/h) | 2 510 080 | 17.7 (17.1, 18.3) | 271 521 | 6.2 (5.5, 6.8) |
| Nursing, psychiatric, and home health aides (median wage $12.64/h) | 1 565 915 | 11.0 (10.6, 11.5) | 243 765 | 5.5 (4.8, 6.3) |
| Physicians and surgeons (median wage $67.00/h) | 343 210 | 2.4 (2.2, 2.7) | 537 642 | 12.3 (11.1, 13.4) |
| Personal and home care aides (median wage $11.35/h) | 645 089 | 4.5 (4.3, 4.8) | 114 438 | 2.6 (2.2, 3.0) |
| Medical and health services managers (median wage $31.73/h) | 446 093 | 3.1 (2.9, 3.4) | 183 547 | 4.2 (3.6, 4.7) |
Note. CI = confidence interval. All values are weighted populations (%). The 95% CIs were calculated by using balanced repeated replication with replicate weights provided by the Current Population Survey. Occupations chosen are the top 5 (in weighted number of workers) in the entire sample of health care workers.
Of female health care workers, 7.5% (weighted population = 1 062 821; 95% CI = 6.7%, 8.2%) relied on food stamps and 2.6% (weighted population = 374 049; 95% CI = 2.1%, 3.2%) received housing support. Of all female health care workers, 10.0% (weighted population = 1 415 365; 95% CI = 9.2%, 10.8%) received health insurance through Medicaid and 7.1% lacked health insurance altogether (weighted n = 1 012 298; 95% CI = 6.5%, 7.8%). Furthermore, 5.8% of female health care workers (weighted population = 829 769; 95% CI = 5.2%, 6.5%) reported being in poor or fair health. Among the 5 largest health care occupations, women were more than twice as likely as men to work as nurses (median wage $31.24 per hour) or nursing, psychiatric, and home health aides (median wage $12.64 per hour), and were significantly more likely to work as personal and home care aides (median wage $11.35 per hour). Men were more than 5 times as likely as women to work as physicians or surgeons (median wage $67.00 per hour) and were also more likely than women to work as medical and health services managers (median wage $31.73 per hour).
Of note, while hospitals employed the largest number of low-wage (< $15 per hour) health care workers (Table A, available as a supplement to the online version of this article at http://www.ajph.org), such workers represented a far larger share of the total workforce in home health care (56.8%), nursing homes (51.8%), and other residential care facilities (55.1%) than in hospitals (21.2%).
Table 2 presents the socioeconomic data for female health care workers of different self-identified racial/ethnic groups. Nearly 50% of Black, Latina, and “other” female health care workers earned less than $15 per hour, versus 26.3% (95% CI = 24.3%, 28.4%) of Asian women and 28.8% (95% CI = 27.8%, 29.9%) of White women. Black, Latina, and “other” women and their children were also significantly more likely to live in poverty than White and Asian women; strikingly, 1 in 6 children of Black female health care workers lived in poverty. Black, Latina, Native American, and “other” women were more likely than their White and Asian female peers to rely on food stamps, public housing support, or Medicaid, and more than 10% of Black and Latina female health care workers themselves lacked health insurance. Perhaps related, more than 7% of Black and Latina female health care workers reported poor or fair health.
TABLE 2—
Characteristics of Female Health Care Workers by Self-Reported Race/Ethnicity: Annual Social and Economic Supplement to the Current Population Survey, United States, 2017
| Black |
Latina |
Native American |
Asian |
White |
Other |
|||||||
| No. | % of Workers or Their Children (95% CI) | No. | % of Workers or Their Children (95% CI) | No. | % of Workers or Their Children (95% CI) | No. | % of Workers or Their Children (95% CI) | No. | % of Workers or Their Children (95% CI) | No. | % of Workers or Their Children (95% CI) | |
| Weighted no. | 2 368 388 | 1 732 923 | 97 698 | 919 042 | 8 875 959 | 196 327 | ||||||
| Wage < $15/h | 1 159 233 | 48.9 (47.3, 50.5) | 865 405 | 49.9 (48.0, 51.9) | 38 594 | 39.5 (32.4, 46.6) | 241 900 | 26.3 (24.3, 28.4) | 2 560 361 | 28.8 (27.8, 29.9) | 89 384 | 45.5 (39.9, 51.1) |
| Workers with household incomes < 100% of federal poverty line | 250 514 | 10.6 (9.5, 11.7) | 153 128 | 8.8 (7.9, 9.8) | 4 072 | 4.2 (1.5, 6.8) | 25 514 | 2.8 (2.0, 3.6) | 245 057 | 2.8 (2.5, 3.0) | 24 145 | 12.3 (8.7, 15.9) |
| Children of health care workers with household incomes < 100% of federal poverty line | 405 811 | 16.7 (15.0, 18.5) | 217 599 | 11.9 (10.5, 13.3) | 8 596 | 8.6 (3.3, 13.9) | 28 022 | 2.9 (2.1, 3.8) | 312 143 | 4.2 (3.7, 4.6) | 31 450 | 15.0 (9.7, 20.3) |
| Workers with household incomes < 200% of federal poverty line | 732 205 | 31.0 (29.4, 32.4) | 514 248 | 29.7 (28.1, 31.3) | 32 469 | 33.2 (25.6, 40.9) | 99 028 | 10.8 (9.3, 12.3) | 1 014 401 | 11.4 (10.9, 12.0) | 60 164 | 30.6 (25.8, 35.5) |
| Children of health care workers with household incomes < 200% of federal poverty line | 1 059 694 | 43.7 (41.3, 46.1) | 731 334 | 40.1 (37.4, 42.5) | 34 905 | 34.9 (25.2, 44.5) | 102 027 | 10.7 (9.2, 12.3) | 1 263 275 | 16.9 (15.8, 17.8) | 90 332 | 43.0 (33.3, 52.8) |
| Receive food stamps | 354 818 | 15.0 (13.8, 16.2) | 204 704 | 11.8 (10.6, 13.0) | 15 560 | 15.9 (10.1, 21.7) | 31 013 | 3.4 (2.5, 4.3) | 428 187 | 4.8 (4.4, 5.2) | 28 539 | 14.5 (10.8, 18.3) |
| Live in public housing or receive rent subsidy | 176 446 | 7.5 (6.5, 8.4) | 85 163 | 4.9 (4.1, 5.7) | 9 839 | 10.1 (5.4, 14.7) | 14 307 | 1.6 (0.9, 2.2) | 73 275 | 0.8 (0.7, 1.0) | 15 019 | 7.6 (4.2, 11.1) |
| Uninsured | 249 897 | 10.6 (9.5, 11.6) | 176 296 | 10.2 (9.3, 11.1) | 5 937 | 6.1 (3.2, 8.9) | 42 709 | 4.6 (3.4, 5.9) | 527 636 | 5.9 (5.5, 6.3) | 9 823 | 5.0 (2.7, 7.3) |
| Medicaid | 357 312 | 15.1 (14.0, 16.2) | 278 120 | 16.0 (14.8, 17.3) | 20 249 | 20.7 (14.3, 27.2) | 79 744 | 8.7 (7.3, 10.1) | 639 629 | 7.2 (6.8, 7.6) | 40 311 | 20.5 (16.0, 25.1) |
| Report poor or fair self-rated health | 174 375 | 7.4 (6.6, 8.2) | 136 675 | 7.9 (7.0, 8.8) | 5 578 | 5.7 (3.1, 8.3) | 36 295 | 3.9 (3.2, 4.7) | 463 738 | 5.2 (4.8, 5.6) | 13 108 | 6.7 (4.1, 9.3) |
| Occupation | ||||||||||||
| Registered nurses (median wage $31.25/h) | 284 735 | 12.0 (10.9, 13.1) | 159 435 | 9.2 (8.2, 10.2) | 10 266 | 10.5 (7.6, 13.4) | 228 005 | 24.8 (22.5, 27.1) | 1 805 439 | 20.3 (19.6, 21.1) | 22 201 | 11.3 (7.6, 15.0) |
| Nursing, psychiatric, and home health aides (median wage $12.64/h) | 553 745 | 23.4 (21.8, 24.9) | 231 419 | 13.4 (12.1, 14.6) | 20 831 | 21.3 (15.4, 27.2) | 65 568 | 7.1 (5.8, 8.4) | 672 013 | 7.6 (7.1, 8.0) | 22 338 | 11.4 (7.2, 15.5) |
| Physicians and surgeons (median wage $67.00/h) | 50 644 | 2.1 (1.6, 2.7) | 13 050 | 0.8 (0.5, 1.0) | 0 | … | 51 729 | 5.6 (4.5, 6.8) | 224 036 | 2.5 (2.2, 2.8) | 3 751 | 1.9 (0.3, 3.5) |
| Personal and home care aides (median wage $11.35/h) | 178 130 | 7.5 (6.5, 8.5) | 134 528 | 7.8 (6.7, 8.8) | 14 059 | 14.4 (8.1, 20.6) | 63 167 | 6.9 (5.6, 8.1) | 251 256 | 2.8 (2.5, 3.1) | 3 949 | 2.0 (0.8, 3.2) |
| Medical and health services managers (median wage $31.73/h) | 46 109 | 1.9 (1.5, 2.4) | 27 866 | 1.6 (1.2, 2.0) | 2 571 | 2.6 (0.5, 4.8) | 28 286 | 3.1 (2.3, 3.9) | 330 603 | 3.7 (3.4, 4.0) | 10 659 | 5.4 (2.7, 8.1) |
Note. CI = confidence interval. All values are weighted populations (%). The 95% CIs were calculated by using balanced repeated replication with replicate weights provided by the Current Population Survey.
Within the 5 largest health care occupations, White and Asian women were overrepresented relative to women as a whole among registered nurses and among physicians and surgeons, and White women were also overrepresented among medical and health services managers. Black, Latina, Native American, and Asian women were all overrepresented among personal and home care aides, and Black, Latina, Native American, and “other” women were overrepresented among nursing, psychiatric, and home health aides. More than 30% of all Black women employed in health care were employed as nursing, psychiatric, and home health or personal and home care aides, both occupations with median wages less than $15 per hour.
The predicted effects on health care workers of increasing the minimum wage to $15 per hour are shown in Table 3. In the first scenario, which assumes a zero wage elasticity for labor demand, increasing the minimum wage to $15 per hour would increase the average annual income of workers currently earning less than $15 per hour by $7653 ($7682 for all women, and $8326 for Black, Latina, Native American, and “other” women), at a total system-wide cost of $45.8 billion (95% CI = $44.4, $47.2 billion), equivalent to 1.3% of total US health spending.26 Under these assumptions, raising the minimum wage would raise nearly 900 000 health care workers and their children out of poverty.
TABLE 3—
Projecting the Effects of a $15-per-Hour Minimum Wage on the Poverty Status and Incomes of Health Care Workers and Their Dependents: Annual Social and Economic Supplement to the Current Population Survey, United States, 2017
| Current Baseline |
$15/h Minimum Wage, Assuming No Disemployment Effects |
$15/h Minimum Wage, Assuming 9.4% Reduction in Hours for All Persons Earning < $19/h |
||||
| No. | % of Workers or Their Children (95% CI) | No. | % of Workers or Their Children (95% CI) | No. | % of Workers or Their Children (95% CI) | |
| All health care workers with household incomes < 100% of federal poverty line | 807 285 | 4.3 (4.1, 4.6) | 409 079 | 2.2 (2.0, 2.4) | 591 809 | 3.2 (3.0, 3.4) |
| Female health care workers with household incomes < 100% of poverty | 702 429 | 5.0 (4.7, 5.2) | 348 951 | 2.5 (2.2, 2.7) | 511 722 | 3.6 (3.3, 3.9) |
| Black, Latina, Native American, and “other” female health care workers with household incomes < 100% of federal poverty line | 490 681 | 8.8 (8.2, 9.5) | 239 890 | 4.3 (3.9, 4.8) | 332 620 | 6.0 (5.4, 6.5) |
| Children of all health care workers with household incomes < 100% of federal poverty line | 1 155 745 | 7.0 (6.5, 7.6) | 654 529 | 4.0 (3.6, 4.4) | 992 273 | 6.1 (5.5, 6.6) |
| Average annual income bonus for all health care workers currently earning < $15/h, $ | NA | 7 653 (7 523, 7 782) | 5 103 (4 982, 5 223) | |||
| Average annual income bonus for female health care workers currently earning < $15/h, $ | NA | 7 682 (7 542, 7 821) | 5 152 (5 019, 5 284) | |||
| Average annual income bonus for Black, Latina, Native American, and “other” female health care workers currently earning < $15/h, $ | NA | 8 326 (8 118, 8 533) | 5 769 (5 575, 5 963) | |||
Note. CI = confidence interval; NA = not applicable. All values are weighted populations (%) or values calculated based on weighted populations. The 95% CIs were calculated by using balanced repeated replication with replicate weights provided by the Current Population Survey.
Under the second set of assumptions—that a $15-per-hour minimum wage would cause workers earning less than $19 per hour to see a 9.4% reduction in their hours—the economic impacts were more modest; 215 476 workers and 163 472 children would be lifted above the poverty line. In this scenario, the average affected worker would see a wage bonus of $5103 ($5152 for all women and $5769 for Black, Latina, Native American, and “other” women). The total cost to the health care system under these assumptions would be $23.0 billion (95% CI = $21.8, $24.3 billion), 0.7% of total US health expenditures.
DISCUSSION
The health care system not only provides care to patients but also exerts a powerful influence on the economic well-being of its large workforce. In the United States, that workforce is starkly stratified by race/ethnicity and gender, with women predominating and women of color particularly concentrated in low-wage positions. In 2017, we found that 1.7 million female US health care workers and their children lived below the poverty line, more than 7% lacked health insurance coverage, and many relied on public assistance for health coverage, food security, and housing.
Although several recent studies have examined gender-based pay disparities for doctors and nurses, less attention has been given to the experiences of the far larger number of women in lower-wage positions that account for the majority of health care employment.27 The few studies of workers in specific low-wage health care occupations have not addressed gender disparities.11–17 A handful of older studies assessed insurance coverage of health care workers before the passage of the 2010 Affordable Care Act, but our findings suggest that uninsurance persists among health care workers.8–10
We examined $15-per-hour minimum-wage policies as a potential intervention that might improve the welfare of low-wage female health care workers given this policy’s recent popularity among policymakers, its implementation in 6 major US cities, and the fact that some health care organizations have independently raised minimum wages to these levels.18,19 Our findings suggest that the universal adoption of this policy would reduce the number of female health care workers living in poverty by as much as 50.3% if demand for labor was inelastic. Assuming that raising the minimum wage would cause a substantial loss of work hours, we found that a $15-per-hour minimum wage would reduce poverty among female health care workers by a smaller, but still substantive fraction, 27.1%.
The true effect size is likely closer to the estimates of our first (inelastic labor demand) scenario. The bulk of empirical evidence finds little disemployment effects from raising the minimum wage.22,23 Moreover, wage increases of the size we posit are unlikely to raise the price of services enough to cause a substantial reduction in the demand for health care.28 Although a rise in the minimum wage to $15 per hour could theoretically lead to a loss of fringe benefits such as health insurance, the literature does not conclusively demonstrate that such tradeoffs exist.26 In fact, low-skilled workers experience fewer unmet medical needs in states with higher minimum wages, likely because of their increased ability to afford out-of-pocket health care costs.29,30 In addition, the health care sector may be relatively protected from disemployment effects: the demand for health care labor is growing and few health care jobs can be automated or outsourced overseas (because of the face-to-face nature of health care work, particularly within low-wage occupations).26,28,31
Socioeconomic status is an important social determinant of health. Previous studies have identified a direct relationship between income and improvement in several health outcomes, including infant mortality and birth weight, smoking rates, adolescent pregnancy rates, life expectancy, obesity, subjective well-being, and self-reported health (see additional references, available as a supplement to the online version of the article at http://www.ajph.org). Multiple studies have also projected that raising the minimum wage would reduce population-level mortality.30,32 These findings suggest that raising the minimum wage would improve health and health care access among low-wage health care workers.
Beyond minimum wages, other public policies may also substantially improve the welfare of low-wage health care workers. For example, an extensive literature suggests that the Earned Income Tax Credit (EITC), a refundable federal tax credit for low- and moderate-income working individuals, is among the largest antipoverty programs in the United States, lifting 4.4 million US children out of poverty in 2015 and 2016.33 The effects of the EITC are concentrated among working single women with children who have household incomes between 75% and 150% of poverty, which corresponds closely to the vulnerable population of female health care workers identified in our analysis.34 Expansion of the EITC, a policy with broad support across political party lines, therefore merits further investigation as a strategy for improving the well-being of female health care workers.
Countervailing economic trends beyond those shaped by public policies may also influence the wages of workers in the health care industry. In particular, growing nationwide demand for health care labor—particularly for occupations currently represented in the bottom of the health care wage distribution—could serve as a force to increase wages.24 However, the benefits of this growing demand may be distributed inequitably across race and gender groups for a number of reasons, including discrimination in the labor market.
Limitations
Our study has a number of limitations. As with all surveys, there is concern that our data may have been biased by participants’ inaccurate self-report; however, the CPS is considered highly reliable, and has been used for decades to generate US government employment estimates (see additional references, available as a supplement to the online version of the article at http://www.ajph.org). We analyzed data from a single year and, hence, could not illuminate factors, such as secular changes in demand for health care services, that may influence wage levels over time.
Our analysis focused on nationwide wage, income, and benefit patterns across all health care settings, and grouped many occupations together. Further elucidation of the experience of workers in specific low-wage health care occupations, regions, or work settings (e.g., for-profit vs nonprofit, small vs large) might identify the parts of the health care industry in which low-wage work is most prevalent, as well as heterogeneous effects of tax or labor market policies.15,16 Although our analysis was not designed to identify the mechanisms that generate gender and racial inequities, such as differential access to education or discrimination on the part of employers, this represents a promising area for further research.
In the minimum-wage analyses, our second (conservative) scenario relied on data on employment effects of a $13-per-hour minimum wage in a single city, as $15-per-hour policies are new, and studies of their economic effects have not been conducted. Analyses of the effects of a $15-per-hour minimum wage on health care workers should be updated when empirical data on these higher minimum wages become available.
Public Health Implications
Income is an important determinant of health, and reducing socioeconomic inequity has been recognized as an important lever for improving population health. We found that the wage policies of US health care institutions consign many of their employees, predominantly women and particularly women of color, to poverty or near-poverty. Put differently, nearly 5% of all people living in poverty in the United States are health care workers or their children.35 Our results demonstrate that achieving economic, gender, and racial/ethnic justice in the United States requires changes to the compensation structure of health care employment, and suggest that health care institutions should look inward when designing and implementing efforts to address socioeconomic determinants of health.
ACKNOWLEDGMENTS
A. S. Venkataramani acknowledges a Mentored Patient-Oriented Research Career Development Award from the National Institutes of Health (K23MH106362).
CONFLICTS OF INTEREST
We declare no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
In consultation with the office of the institutional review board of the University of Pennsylvania, it was determined that this study did not require institutional review board review, as it utilized only publicly available de-identified data.
Footnotes
REFERENCES
- 1.Women’s Bureau, US Department of Labor. Most common occupations for women. 2015. Available at: https://www.dol.gov/wb/stats/most_common_occupations_for_women.htm#chart2. Accessed February 6, 2018.
- 2.Bureau of Labor Statistics. Employed persons by detailed industry, sex, race, and Hispanic or Latino ethnicity. 2018. Available at: https://www.bls.gov/cps/cpsaat18.htm. Accessed February 7, 2018.
- 3.Bureau of Labor Statistics. Employment by major industry sector. 2017. Available at: https://www.bls.gov/emp/ep_table_201.htm. Accessed February 1, 2018.
- 4.Bureau of Labor Statistics. Women in the labor force: a databook. 2017. Available at: https://www.bls.gov/opub/reports/womens-databook/2017/home.htm. Accessed January 20, 2018.
- 5.Greene J, El-Banna MM, Briggs LA, Park J. Gender differences in nurse practitioner salaries. J Am Assoc Nurse Pract. 2017;29(11):667–672. doi: 10.1002/2327-6924.12512. [DOI] [PubMed] [Google Scholar]
- 6.Women’s Bureau, US Department of Labor. Women’s earnings and the gender wage gap. 2017. Available at: https://www.dol.gov/wb/resources/Womens_Earnings_and_the_Wage_Gap_17.pdf. Accessed July 14, 2018.
- 7.Appelbaum E. Black women in healthcare face declining real wages. Center for Economic and Policy and Research. 2017. Available at: http://cepr.net/blogs/cepr-blog/black-women-in-healthcare-face-declining-real-wages. Accessed July 14, 2018.
- 8.Case BG, Himmelstein DH, Woolhandler S. No care for the caregivers: declining health insurance coverage for health care personnel and their children, 1988–1998. Am J Public Health. 2002;92(3):404–408. doi: 10.2105/ajph.92.3.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chou CF, Johnson PJ, Ward A, Blewett LA. Health care coverage and the health care industry. Am J Public Health. 2009;99(12):2282–2288. doi: 10.2105/AJPH.2008.152413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ebenstein W. Health insurance coverage of direct support workers in the developmental disabilities field. Ment Retard. 2006;44(2):128–134. doi: 10.1352/0047-6765(2006)44[128:HICODS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 11.Dill JS, Morgan JC, Marshall VW, Pruchno R. Contingency, employment intentions, and retention of vulnerable low-wage workers: an examination of nursing assistants in nursing homes. Gerontologist. 2013;53(2):222–234. doi: 10.1093/geront/gns085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stacey CL. Finding dignity in dirty work: the constraints and rewards of low-wage home care labour. Sociol Health Illn. 2005;27(6):831–854. doi: 10.1111/j.1467-9566.2005.00476.x. [DOI] [PubMed] [Google Scholar]
- 13.Butter IH, Carpenter ES, Kay BJ. Gender hierarchies in the health labor force. Int J Health Serv. 1987;17(1):133–149. doi: 10.2190/0UQ0-WV6P-2R6V-2QDQ. [DOI] [PubMed] [Google Scholar]
- 14.Ribas V, Dill JS, Cohen PN. Mobility for care workers: job changes and wages for nurse aides. Soc Sci Med. 2012;75(12):2183–2190. doi: 10.1016/j.socscimed.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 15.Smith K, Baughman R. Caring for America’s aging population: a profile of the direct-care workforce. Mon Labor Rev. 2007;130(20):20–26. [Google Scholar]
- 16.Montgomery RJ, Holley L, Deichert J, Kasloski K. A profile of home care workers from the 2000 census: how it changes what we know. Gerontologist. 2005;45(5):593–600. doi: 10.1093/geront/45.5.593. [DOI] [PubMed] [Google Scholar]
- 17.Dill J. Jobs or Careers? Mobility Among Low-Wage Workers in Healthcare Organizations [dissertation]. Chapel Hill, NC: The University of North Carolina at Chapel Hill; 2011.
- 18.Herman B. Aetna competitors unlikely to match $16 minimum wage move. Modern Health Care. January 14, 2015. Available at: http://www.modernhealthcare.com/article/20150114/NEWS/301149980. Accessed February 6, 2018.
- 19.McClusky PD. Which hospitals pay the highest starting wages? Boston Globe. January 7, 2016. Available at: https://www.bostonglobe.com/business/2016/01/07/which-hospitals-pay-highest-starting-wages/YXiJrsAPGSsxGvEAyaueeP/story.html. Accessed February 6, 2018.
- 20.The Economic Policy Institute. Minimum wage tracker. 2018. Available at: https://www.epi.org/minimum-wage-tracker/#/min_wage. Accessed May 10, 2018.
- 21.Flood S, King M, Ruggles S, Warren JR. Integrated Public Use Microdata Series, Current Population Survey: Version 5.0. Minneapolis, MN: University of Minnesota; 2017.
- 22.Wolfers J. What do we really know about the employment effects of the minimum wage? In: Strain MR, editor. The U.S. Labor Market: Questions and Challenges for Public Policy. Washington, DC: American Enterprise Institute; 2016. pp. 106–120. [Google Scholar]
- 23.Neumark D, Wascher W. Minimum wages and employment: a review of evidence from the new minimum wage research. Cambridge, MA: National Bureau of Economic Research; 2007.
- 24.Keehan SP, Stone DA, Poisal JA. National health expenditure projections 2016–25: price increases, aging push sector to 20 percent of economy. Health Aff (Millwood) 2017;36(3):553–563. doi: 10.1377/hlthaff.2016.1627. [DOI] [PubMed] [Google Scholar]
- 25.Jardim E, Long MC, Plotnick R, van Inwegen E, Vigdor J, Wething H. Minimum wage increases, wages, and low-wage employment: evidence from Seattle. Cambridge, MA: National Bureau of Economic Research; 2017.
- 26.Clemens J, Kahn LB, Meer J. The minimum wage, fringe benefits, and worker welfare. Cambridge, MA: National Bureau of Economic Research; 2018.
- 27.Muench U, Sindelar J, Busch SH, Buerhaus PI. Salary differences between male and female registered nurses in the United States. JAMA. 2015;313(12):1265–1267. doi: 10.1001/jama.2015.1487. [DOI] [PubMed] [Google Scholar]
- 28.Machin S, Rahman L, Manning A. Where the minimum wage bites hard: introduction of minimum wages to a low-wage sector. J Eur Econ Assoc. 2003;1(1):154–180. [Google Scholar]
- 29.McCarrier KP, Zimmerman FJ, Ralston JD, Martin DP. Associations between minimum wage policy and access to health care: evidence from the Behavioral Risk Factor Surveillance System, 1996–2007. Am J Public Health. 2011;101(2):359–367. doi: 10.2105/AJPH.2006.108928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tsao TY, Konty KJ, Van Wye G et al. Estimating potential reductions in premature mortality in New York City from raising the minimum wage to $15. Am J Public Health. 2016;106(6):1036–1041. doi: 10.2105/AJPH.2016.303188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Potter N. The effect of the Santa Fe living wage ordinance in Santa Fe, New Mexico. Albuquerque, NM: University of New Mexico Bureau of Business and Economic Research; 2006.
- 32.Cole BL, Shimkhada R, Morgenstern H, Kominksi G, Fielding JE, Wu S. Projected health impact of the Los Angeles City living wage ordinance. J Epidemiol Community Health. 2005;59(8):645–650. doi: 10.1136/jech.2004.028142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fox L. US Census Bureau Current Population Reports, P60-261, the supplemental poverty measure: 2016. 2017. Available at: https://www.census.gov/content/dam/Census/library/publications/2017/demo/p60-261.pdf. Accessed February 6, 2018.
- 34.Hoynes HW, Patel AJ. Effective policy for reducing inequality? The earned income tax credit and the distribution of income. Cambridge, MA: National Bureau of Economic Research; 2015.
- 35.Semega JL, Fontenot KR, Kollar MA. US Census Bureau, Current Population Reports, P60-259, income and poverty in the United States: 2016. 2017. Available at: https://census.gov/content/dam/Census/library/publications/2017/demo/P60-259.pdf. Accessed February 2, 2018.