Abstract
Objectives. To identify opioids associated with a spike in opioid-related mortality in Wayne County, Michigan, from July 2016 through February 2017.
Methods. We reviewed records from the Wayne County Medical Examiner’s Office of 645 people who died because of accidental nonmedically prescribed opioid overdoses from July 2015 through July 2017. We analyzed basic demographics, locations of death, and all opioid toxicology results. Decedents who died in hospitals were excluded.
Results. Of the 645 people who died because of nonmedically prescribed opioid overdoses, 65% were male and 63% were White, with an average age of 43 years. Carfentanil was detected in 129 (20%) cases. During the 8-month mortality spike, carfentanil was detected in 114 of 419 cases (average = 27.2%; range = 6.4%–45.2%). Substances most frequently detected with carfentanil included morphine (57%), 6-monoacetylmorphine (38%), fentanyl (43%), norfentanyl (33%), tetrahydrocannabinol (34%), and cocaine (29%).
Conclusions. The Wayne County spike in mortality temporally corresponded with the detection of carfentanil and a proportional increase in opioid overdose deaths with detectable carfentanil.
Public Health Implications. The abrupt decrease in carfentanil-detected mortality coincided with an announcement indicating an impending ban on fentanyl analogs from China, which suggests that source control is an effective countermeasure.
Over the past 25 years, the United States has experienced sporadic epidemics of accidental overdose and death caused by fentanyl and fentanyl analogs added to heroin.1–5 Shortly after the ultrapotent fentanyl analog carfentanil was first identified in Michigan in July 2016,6 Wayne County experienced a spike in opioid-related deaths that began in July 2016 and ended February 2017. Carfentanil is an extremely powerful μ opioid agonist used as a veterinary tranquilizing agent. It is reportedly 100 times more potent than fentanyl and 10 000 times more potent than morphine.7 Carfentanil and other fentanyl analogs have been increasingly found in heroin in both the United States and Europe.8
In response to the identification of carfentanil, the Michigan Department of Health and Human Services issued a Health Alert Network notification in October 2016 to hospitals, local health departments, emergency first responders, and medical control agencies to use extreme caution when handling unknown substances and chemicals and to be alert for patients with suspected opioid overdose who do not have the anticipated response to naloxone. This includes lack of respiratory status improvement with normal doses of naloxone or patients who require larger than expected naloxone doses to reverse respiratory toxicity.
Wayne State University researchers partnered with the Wayne County Medical Examiner’s Office to evaluate the substances associated with this spike in opioid-related deaths. Researchers collected information on all 645 accidental nonmedically prescribed opioid overdose deaths that occurred from July 2015 through July 2017.
METHODS
The research team identified deaths from the Wayne County Medical Examiner’s Office database that occurred from July 2015 through July 2017 in which (1) the immediate cause of death was “drug intoxication” or “toxicity” and included a nonmedically prescribed opioid (i.e., heroin and its metabolites [diacetylmorphine, 6-monoacetylmorphine or 6-MAM, and morphine], fentanyl, 3-methyl fentanyl, acetyl fentanyl, acryl fentanyl, butyryl fentanyl, furanyl fentanyl, 4-ANPP, carfentanil, U-47700) and (2) the manner of death was accidental. We selected July 2015 to establish 1 year of baseline rates of opioid overdose deaths in Wayne County prior to detection of carfentanil.
Board-certified medical examiners assessed cause and manner of death in all cases after performing complete postmortem examinations to exclude other causes of death. Cases that did not have complete toxicology reports were not included for analysis. Demographics (i.e., age, sex, and race), date of death, location of death, and toxicology reports with all positive findings were obtained for cases that met inclusion criteria. Toxicology reports included quantitative data from both blood and urine. NMS laboratories (Willow Grove, PA) performed the toxicology analyses and screens for more than 250 substances and substance metabolites with comprehensive liquid chromatography and time-of-flight mass spectrometry. New substances are added to the screen as standards become available. We used the χ2 and Student t tests for statistical analysis.
RESULTS
Between July 2015 and July 2017, 645 people died because of accidental nonmedically prescribed opioid overdoses in Wayne County. Carfentanil was detected in 129 (20%) cases overall. All decedents studied were primarily male (65%) and White (63%), with an average age of 43 years. Table A (available as a supplement to the online version of this article at http://www.ajph.org) catalogs and compares demographics of decedents with and without detectable carfentanil as well as other opioids and substances of abuse detected on postmortem toxicology analysis. Decedents with carfentanil detected were more likely to be male (P = .047) and to have died in Detroit, Michigan (67% vs 50%; P = .001). The substances most frequently detected with carfentanil included the heroin (diacetylmorphine) metabolites morphine (57%) and 6-MAM (38%); fentanyl (43%) and its major metabolite norfentanyl (33%); tetrahydrocannabinol (34%); and cocaine (29%). In comparison, the substances most commonly detected in decedents without detectable carfentanil were fentanyl (52%) and its metabolite norfentanyl (38%); heroin metabolites morphine (45%) and 6-MAM (29%); and ethanol (32%). Decedents with detectable carfentanil were more likely to have detectable heroin metabolites morphine (57% vs 45%; P = .01) and 6-MAM (38% vs 29%; P = .02); furanyl fentanyl (26% vs 2%; P < .001); and U-47700 (12% vs 3%; P < .001). Decedents without detectable carfentanil were more likely to have detectable acetyl fentanyl (8% vs 1%; P = .002), hydrocodone (20% vs 9%; P = .003), oxymorphone (7% vs 2%; P = .016), oxycodone (8% vs 2%; P = .02), and methadone (9% vs 2%; P = .005).
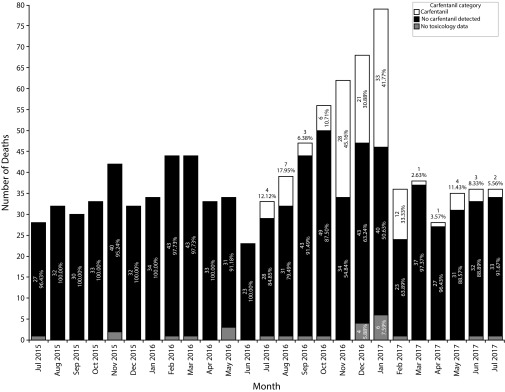
Figure 1 displays opioid overdose deaths per month from July 2015 to July 2017, with a noted increase in deaths beginning in July 2016 through February 2017. Carfentanil was detected in 114 of 419 cases during this 8-month period. During these months, 6.4% to 45.2% (average = 27.2%) of the decedents had carfentanil detected, compared with only 2.5% to 11.4% (average = 6.4%) after the spike (March–July 2017). Despite the precipitous decline in overall mortality noted in February 2017, 33% of decedents still had detectable carfentanil. Corresponding to the decreased proportion of deaths with detectable carfentanil, mortality rates returned to the baseline rates recorded before the presumed introduction of carfentanil (July 2015–June 2016). Carfentanil was the only opioid that was detected more frequently during the spike in opioid-related mortality.
FIGURE 1—
Wayne County, Michigan, Opioid Overdose Deaths per Month: July 2015–July 2017
DISCUSSION
Short-lived spikes or epidemics in overdoses and death caused by opioids have occurred intermittently in the United States.1–5 Since 2013, national opioid overdose death rates have shown a sustained acceleration linked to the increasing presence of fentanyl and its analogs. This study characterized an 8-month spike in mortality in Wayne County (July 2016–February 2017) that occurred shortly after the detection of carfentanil.
Carfentanil likely contributed to the local spike in mortality for many reasons. The accidental nonmedically prescribed opioid out-of-hospital death rate prior to the detection of carfentanil averaged 34 cases per month. During the spike, the average number of deaths per month jumped to 52.4, with carfentanil detected in 14.3 deaths per month. After February 2017, carfentanil was sporadically detected in decedents, which corresponded to an overall decline in opioid death rates. Carfentanil was the only opioid that was found more frequently during the spike. Fentanyl was the opioid most commonly found in decedents overall but did not track with the peaking of deaths. Other opioids, including acetyl fentanyl, acryl fentanyl, furanyl fentanyl, and U-47700, were not found nearly as often. Finally, the temporal association of the decline in carfentanil-associated deaths with China’s mid-February announcement to place carfentanil on the list of controlled substances on March 1, 2017, the presumed subsequent decrease in supply, and the abrupt decline in death rates add plausibility that carfentanil contributed to the spike in deaths.9
This study had several limitations. First, the Wayne County Medical Examiner evaluated only those individuals who died within Wayne County; Wayne County residents who died in other counties were not counted. Second, routine testing for carfentanil and other fentanyl analogs began in July 2016. Whether these analogs contributed to mortality before this date is unknown. Third, patients who were admitted to the hospital and died days after admission often did not have confirmatory toxicology reports and were not included in this analysis. This would have led to undercounting. Finally, our results are specific to Wayne County and may not be generalizable.
PUBLIC HEALTH IMPLICATIONS
The addition of novel opioids to the heroin supply marks the third wave of the opioid crisis.10 The United States has had sporadic outbreaks of opioids in the past. Because of the potency of these new opioids, drug distributors’ experience with titrating appropriate doses is limited, leading to spikes in unintentional overdoses that can overwhelm emergency medical services, hospitals, and medical examiners. Thus, timely identification is of utmost importance with public health outreach to clinicians and users, including distribution of point-of-care fentanyl testing. Finally, this episode underlines the potential critical importance of international policy: direct source control of the ultrapotent opioids may be particularly effective. Whether seizures of carfentanil by law enforcement contributed to the decline in mortality is unknown.
ACKNOWLEDGMENTS
We would like to acknowledge all staff at the Wayne County Medical Examiner Office, the Michigan Department of Health and Human Services, and NMS Laboratories.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
HUMAN PARTICIPANT PROTECTION
This study was exempt from approval by the Wayne State University institutional review board.
REFERENCES
- 1.Hibbs J, Perper J, Winek CL. An outbreak of designer drug–related deaths in Pennsylvania. JAMA. 1991;265(8):1011–1013. doi: 10.1001/jama.265.8.1011. [DOI] [PubMed] [Google Scholar]
- 2.Schumann H, Erickson T, Thompson TM, Zautcke JL, Denton JS. Fentanyl epidemic in Chicago, Illinois and surrounding Cook County. Clin Toxicol (Phila) 2008;46(6):501–506. doi: 10.1080/15563650701877374. [DOI] [PubMed] [Google Scholar]
- 3.Smialek JE, Levine B, Chin L, Wu SC, Jenkins AJ. A fentanyl epidemic in Maryland 1992. J Forensic Sci. 1994;39(1):159–164. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention (CDC) Nonpharmaceutical fentanyl-related deaths—multiple states, April 2005-March 2007. MMWR Morb Mortal Wkly Rep. 2008;57(29):793–796. [PubMed] [Google Scholar]
- 5.Algren DA, Monteilh CP, Punja M et al. Fentanyl-associated fatalities among illicit drug users in Wayne County, Michigan (July 2005-May 2006) J Med Toxicol. 2013;9(1):106–115. doi: 10.1007/s13181-012-0285-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Deadly opioid carfentanil confirmed in Michigan, 19 associated deaths identified in Wayne County [press release]. Lansing: State of Michigan, October 6, 2016. Available at: https://www.michigan.gov/som/0,4669,7-192-29942_73920_74076-395078--,00.html. Accessed March 19, 2018.
- 7.George AV, Lu JJ, Pisano MV, Metz J, Erickson TB. Carfentanil—an ultra potent opioid. Am J Emerg Med. 2010;28(4):530–532. doi: 10.1016/j.ajem.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 8. Drug Enforcement Administration Strategic Intelligence Section. National Heroin Threat Assessment Summary—Updated. DEA Intelligence Report. June 2016. Available at: https://www.dea.gov/sites/default/files/2018-07/hq062716_attach.pdf. Accessed March 19, 2018.
- 9.Kinetz E. China carfentanil ban a “game-changer” for opioid epidemic. February 16, 2017. Available at: https://www.usnews.com/news/world/articles/2017-02-15/china-makes-deadly-opioid-carfentanil-a-controlled-substance. Accessed March 19, 2018.
- 10.Dasgupta N, Beletsky L, Ciccarone D. Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health. 2018;108(2):182–186. doi: 10.2105/AJPH.2017.304187. [DOI] [PMC free article] [PubMed] [Google Scholar]