Abstract
The health workforce is the cornerstone of any health care system. An adequately trained and sufficiently staffed workforce is essential to reach universal health coverage. In particular, a nephrology workforce is critical to meet the growing worldwide burden of kidney disease. Despite some attempts, the global nephrology workforce and training capacity remains widely unknown. This multinational cross-sectional survey was part of the Global Kidney Health Atlas project, a new initiative administered by the International Society of Nephrology (ISN). The objective of this study was to address the existing global nephrology workforce and training capacity. The questionnaire was administered online, and all data were analyzed and presented by ISN regions and World Bank country classification. Overall, 125 United Nations member states responded to the entire survey, with 121 countries responding to survey questions pertaining to the nephrology workforce. The global nephrologist density was 8.83 per million population (PMP); high-income countries reported a nephrologist density of 28.52 PMP compared with 0.31 PMP in low-income countries. Similarly, the global nephrologist trainee density was 1.87 PMP; high-income countries reported a 30 times greater nephrology trainee density than low-income countries (6.03 PMP vs. 0.18 PMP). Countries reported a shortage in all care providers in nephrology. A nephrology training program existed in 79% of countries, ranging from 97% in high-income countries to 41% in low-income countries. In countries with a training program, the majority (86%) of programs were 2 to 4 years, and the most common training structure (56%) was following general internal medicine. We found significant variation in the global density of nephrologists and nephrology trainees and shortages in all care providers in nephrology; the gap was more prominent in low-income countries, particularly in African and South Asian ISN regions. These findings point to significant gaps in the current nephrology workforce and opportunities for countries and regions to develop and maintain a sustainable workforce.
Keywords: acute kidney injury, chronic kidney disease, education and training, health manpower, nephrology, workforce
Health workforce, in general, is the cornerstone of a country’s health care system.1 Countries cannot reach universal health coverage2 and sustainable development goals3 without an investment in human resources. To achieve that, countries need adequate numbers of qualified workforce members delivering and managing their health care system. A nephrology workforce in particular is critical to meet the growing worldwide burden of kidney disease4, 5, 6 and its risk factors, such as diabetes,7 obesity,8 and an aging population,9 and the increasing demand of renal replacement therapy (RRT) and kidney care in both high-income and low-income countries.10 Indeed, nephrologist caseload was found to be associated with mortality of dialysis patients.11 Various studies have already examined the state of the nephrology workforce, highlighting the gaps and deficiencies in workforce availability and quality.12, 13, 14, 15, 16, 17, 18 In 1 review of the global nephrology workforce, Sharif et al.12 identified multiple factors responsible for the global shortage in the nephrology workforce and suggested a detailed and comprehensive nephrology workforce planning that is backed by government policy and legislation to ensure effective delivery and sustainability of kidney disease care. Another study that examined kidney care structures across 17 European countries identified limited workforce capacity, among many others, as a common barrier to the care of people with non–dialysis-dependent chronic kidney disease (CKD).13
The objective of this cross-sectional survey that was part of the Global Kidney Health Atlas (GKHA) project, a new initiative to assess kidney care in all world regions administered under the umbrella of the International Society of Nephrology (ISN), was to comprehensively examine the existing nephrology workforce in the form of the number of nephrologists and nephrology trainees; nephrology training capacity in terms of availability, duration, and structure; and the perceived shortages in health care providers pertaining to nephrology across all 10 ISN regions19 and 2014 World Bank country classification20 as low-, lower-middle–, upper-middle–, and high-income nations, based on the World Health Organization (WHO) building blocks.21
Results
Response rate
Responses were received from a total of 125 of 130 UN member states (96% response rate) across 10 ISN regions, and 121 countries answered survey questions pertaining to nephrology workforce. Further details on the response rate and population coverage of the survey have been described elsewhere.22
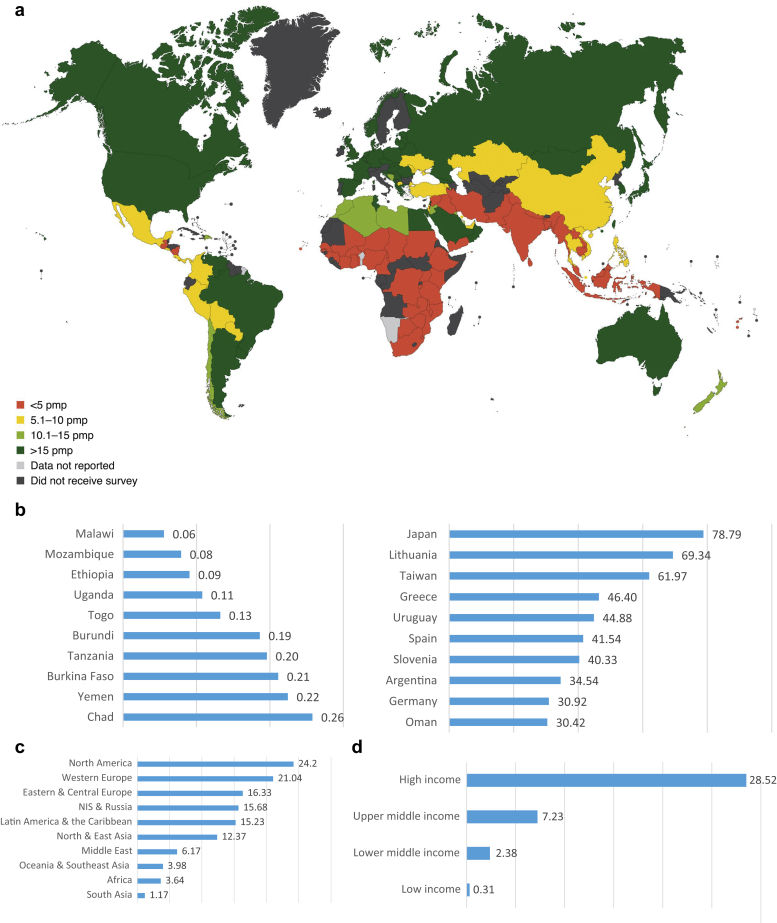
Global density of nephrologists
Overall, the density of nephrologists reported was 8.83 per million population (PMP) (Table 1, Figure 1a). There was considerable variation in density of nephrologists among World Bank income groups and ISN region countries. High-income countries had the highest nephrologist density (28.52 PMP), followed by upper-middle–income (7.23 PMP), lower-middle–income (2.38 PMP), and-low income (0.31 PMP) countries (Table 1). Of the 10 countries with the lowest nephrologist density, 9 belonged to the Africa ISN region, and sub-Saharan Africa specifically. Yemen, in the Middle East ISN region, was the exception (Figure 1b). In contrast, the countries with the highest nephrologist density were from different ISN regions. Japan (North and East Asia region) reported the highest density, followed by Lithuania (Eastern and Central Europe region), Taiwan (North and East Asia region), Greece (Western Europe region), Uruguay (Latin America region), Spain (Western Europe region), Slovenia (Eastern and Central Europe region), Argentina (Latin America region), Germany (Western Europe region) and Oman (Middle East region) (Figure 1b).
Table 1.
Density of nephrologists and nephrology trainees and shortage in nephrology care providers in 121 countries
| Region/group | Total number PMPa |
Shortage in workforce components (n [%]b) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nephrologists | Nephrology trainees | Nephrologists | Dietitians | Renal pathologists | Laboratory technicians | Social workers | Pharmacists | Vascular access coordinators | Nurse practitioners | Counselors/psychologists | Transplant coordinators | Dialysis nurses | Dialysis technicians | Primary care physicians | |
| Overall | 8.83 | 1.87 | 89 (74) | 94 (78) | 104 (86) | 42 (35) | 75 (62) | 36 (30) | 98 (81) | 73 (60) | 81 (67) | 84 (69) | 83 (69) | 72 (60) | 41 (34) |
| ISN region | |||||||||||||||
| Africa | 3.64 | 1.77 | 28 (85) | 30 (91) | 33 (100) | 14 (42) | 17 (52) | 12 (36) | 29 (88) | 19 (58) | 27 (82) | 28 (85) | 25 (76) | 25 (76) | 13 (39) |
| Eastern & Central Europe | 16.33 | 3.41 | 10 (59) | 13 (76) | 11 (65) | 2 (12) | 12 (71) | 1 (6) | 14 (82) | 8 (47) | 11 (65) | 8 (47) | 10 (59) | 6 (35) | 4 (24) |
| Latin America & the Caribbean | 15.23 | 1.89 | 14 (88) | 9 (56) | 16 (100) | 6 (38) | 7 (44) | 4 (25) | 15 (94) | 12 (75) | 7 (44) | 11 (69) | 13 (81) | 10 (63) | 6 (38) |
| Middle East | 6.17 | 1.22 | 11 (85) | 10 (77) | 11 (85) | 3 (23) | 9 (69) | 6 (46) | 9 (69) | 8 (62) | 8 (62) | 10 (77) | 10 (77) | 6 (46) | 3 (23) |
| NIS & Russia | 15.68 | 1.64 | 4 (67) | 6 (100) | 4 (67) | 2 (33) | 4 (67) | 0 (0) | 4 (67) | 3 (50) | 5 (83) | 4 (67) | 1 (17) | 2 (33) | 1 (17) |
| North America | 24.20 | 1.33 | 1 (50) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (50) | 0 (0) | 1 (50) | 0 (0) | 0 (0) | 1 (50) | 1 (50) | 1 (50) |
| North & East Asia | 12.37 | 3.62 | 4 (67) | 5 (83) | 5 (83) | 1 (17) | 6 (100) | 1 (17) | 6 (100) | 5 (83) | 4 (67) | 4 (67) | 3 (50) | 4 (67) | 3 (50) |
| Oceania & Southeast Asia | 3.98 | 0.71 | 11 (85) | 12 (92) | 13 (100) | 8 (62) | 11 (85) | 5 (38) | 12 (92) | 12 (92) | 11 (85) | 12 (92) | 11 (85) | 11 (85) | 5 (38) |
| South Asia | 1.17 | 0.41 | 4 (80) | 4 (80) | 4 (80) | 4 (80) | 4 (80) | 4 (80) | 4 (80) | 3 (60) | 4 (80) | 5 (100) | 4 (80) | 4 (80) | 2 (40) |
| Western Europe | 21.04 | 3.88 | 2 (20) | 5 (50) | 7 (70) | 2 (20) | 5 (50) | 2 (20) | 5 (50) | 2 (20) | 4 (40) | 2 (20) | 5 (50) | 3 (30) | 3 (30) |
| World Bank income group | |||||||||||||||
| Low income | 0.31 | 0.18 | 15 (94) | 16 (100) | 16 (100) | 9 (56) | 10 (63) | 9 (56) | 15 (94) | 8 (50) | 13 (81) | 14 (88) | 13 (81) | 14 (88) | 6 (38) |
| Lower-middle income | 2.38 | 0.78 | 28 (80) | 29 (83) | 33 (94) | 14 (40) | 20 (57) | 9 (26) | 28 (80) | 24 (69) | 26 (74) | 32 (91) | 24 (69) | 23 (66) | 11 (31) |
| Upper-middle income | 7.23 | 1.19 | 26 (84) | 23 (74) | 27 (87) | 10 (32) | 20 (65) | 8 (26) | 27 (87) | 19 (61) | 19 (61) | 21 (68) | 22 (71) | 19 (61) | 9 (29) |
| High income | 28.52 | 6.03 | 20 (51) | 26 (67) | 28 (72) | 9 (23) | 25 (64) | 10 (26) | 28 (72) | 22 (56) | 23 (59) | 17 (44) | 24 (62) | 16 (41) | 15 (38) |
ISN, International Society of Nephrology; NIS, newly independent states; PMP, per million population.
PMP density of nephrologists and nephrology trainees calculated by taking the median of absolute number of nephrologists and/or nephrology trainees provided by each country respondents, divided by country’s population in millions.
Percentages calculated as the number of responding countries divided by the total number of responding countries, overall and by region.
Figure 1.
(a) Global distribution of density of nephrologists per million population (PMP) from 121 countries. (b) Countries with the lowest and highest density of nephrologists PMP from 121 countries. (c) Density of nephrologists PMP from 121 countries grouped by International Society of Nephrology region. (d) Density of nephrologists PMP from 121 countries grouped by World Bank income group. Adapted with permission from Bello AK, Levin A, Tonelli M, et al. Assessment of global kidney health care status. JAMA. 2017;317:1864–1881.22 Copyright © American Medical Association.
Overall, countries in the Africa ISN region reported a low density (3.64 PMP) of nephrologists (Table 1). The lowest numbers were reported from sub-Saharan countries, namely Malawi (0.06 PMP), Mozambique (0.08 PMP), and Ethiopia (0.09 PMP). On the other hand, the highest numbers were reported from North African countries, namely Egypt (21.65 PMP), Tunisia (16.31 PMP), Libya (12.48 PMP), and Algeria (11.38 PMP) (Supplementary Figure S1).
Eastern and Central European countries reported a high density (16.33 PMP) of nephrologists (Table 1). However, there was wide variation in nephrologist density among the countries in the region. Turkey (6.30 PMP), Moldova (9.02 PMP), and Macedonia (9.54 PMP) reported the lowest densities of nephrologists, while Lithuania (69.34 PMP) and Slovenia (40.33 PMP) reported the highest, a difference of 63.04 between each end of the spectrum (Supplementary Figure S1).
In the Western Europe ISN region, countries overall reported a very high density (21.04 PMP) of nephrologists (Table 1). All countries in the region reported higher densities than the global average (8.83 PMP). Israel (9.69 PMP) reported the lowest density of nephrologists, while Greece (46.40 PMP) reported the highest (Supplementary Figure S1).
In the Oceania and Southeast Asia (OSEA) ISN region, countries overall reported a low density (3.98 PMP) of nephrologists (Table 1). Within the region, Burma (0.37 PMP), Indonesia (0.43 PMP), and Laos (0.43 PMP) reported the lowest densities of nephrologists, while Australia (20.88 PMP), New Zealand (13.07 PMP), and Singapore (9.69 PMP) reported the highest (Supplementary Figure S1).
In the North and East Asia ISN region, countries overall reported a high density (12.37 PMP) of nephrologists (Table 1). Japan (78.79 PMP) reported the highest density of nephrologists in the region and globally, followed by Taiwan (61.97 PMP), South Korea (18.32 PMP), Hong Kong (16.31 PMP), and Mongolia (15.04 PMP). Although China reported the highest absolute number of nephrologists globally (mean: 8500), it had the lowest density within its region (5.12 PMP) (Supplementary Figure S1).
In the North America ISN region, both responding countries reported a density of nephrologists higher than the global average of 8.83 PMP: 17.81 PMP in Canada and 24.89 PMP in the USA (Supplementary Figure S1). Furthermore, the region reported the highest density (24.2 PMP) of nephrologists of all 10 ISN regions (Table 1).
In the Latin America and Caribbean ISN region, countries overall reported a high density (15.23 PMP) of nephrologists (Table 1). However, there was wide variation among countries in the region, ranging from Guatemala (3.02 PMP) and Nicaragua (3.72 PMP) with the lowest densities to Uruguay (44.88 PMP) and Argentina (34.54 PMP) with the highest (Supplementary Figure S1).
In the Middle East ISN region, countries overall reported a low density (6.17 PMP) of nephrologists (Table 1). Yemen (0.22 PMP), which had one of the lowest densities of nephrologists globally, Iraq (1.03 PMP), and West Bank and Gaza (2.15 PMP) reported the lowest densities of nephrologists in the region, while Oman (30.42 PMP), Lebanon (22.64 PMP), and Saudi Arabia (17.66 PMP) reported the highest (Supplementary Figure S1).
In the newly independent states (NIS) and Russia ISN region, countries overall reported a high density (15.68 PMP) of nephrologists (Table 1). Kazakhstan (5.51 PMP) and Armenia (8.18 PMP) reported the lowest densities of nephrologists in the region, while Georgia (23.32 PMP) and Belarus (20.86 PMP) reported the highest (Supplementary Figure S1).
In the South Asia ISN region, countries overall reported the lowest density (1.17 PMP) of nephrologists globally (Table 1). Within the region, Bangladesh (0.65 PMP) and Sri Lanka (0.91 PMP) reported the lowest densities of nephrologists, while Pakistan (2.51 PMP) and India (1.04 PMP) reported the highest (Supplementary Figure S1).
Global density of nephrology trainees
Similar to nephrologist density, there was significant variation in density of nephrology trainees among World Bank income groups and ISN regions (Table 1). Overall, the global density of nephrology trainees was 1.87 PMP. The prevalence of nephrology trainees in high-income countries was more than 30-fold that in low-income countries (6.03 vs. 0.18) (Table 1). The prevalence of nephrology trainees in lower-middle– and upper-middle–income level countries was 0.78 PMP and 1.19 PMP, respectively. Seven of the 10 countries with the lowest nephrology trainee densities were from the Africa ISN region, again sub-Saharan Africa specifically: Ethiopia, Uganda, Tanzania, Burundi, Ghana, Zambia, and Malawi. The other 3 countries were Indonesia and Cambodia (OSEA region) and Ukraine (NIS and Russia region). In contrast, the 10 countries with the highest nephrologist trainee densities were from different ISN regions, including 3 from the Africa ISN region, which contrasted sharply with the 7 African countries that were in the lowest density list. Japan (North and East Asia ISN region) reported the highest density followed by Kuwait (Middle East ISN region), Libya (Africa ISN region), Croatia (Eastern and Central Europe ISN region), Bahrain (Middle East ISN region), Serbia (Eastern and Central Europe ISN region), Norway (Western Europe ISN region), Greece (Western Europe ISN region), Algeria (Africa ISN region), and Egypt (Africa ISN region).
In the Africa ISN region, all sub-Saharan countries reported trainee densities lower than the global average (1.87 PMP). Ethiopia (0.02 PMP), Uganda (0.05 PMP), and Tanzania (0.06 PMP) reported the lowest densities. North African countries reported the highest densities of trainees, with Libya (18.72 PMP) first followed by Algeria (9.10 PMP), Egypt (8.93 PMP), and Tunisia (5.44 PMP).
In the Eastern and Central Europe ISN region, most of the countries reported trainee densities above the global average, with Slovakia (0.92 PMP) being the exception. The highest trainee density was reported by Croatia (13.44 PMP), followed by Serbia (9.75 PMP), Slovenia (7.56 PMP), and Lithuania (6.24 PMP).
In the Latin America and the Caribbean ISN region, Colombia (0.43 PMP) and Peru (0.49 PMP) reported the lowest trainee density, followed by Costa Rica (0.62 PMP) and Chile (0.91 PMP). The highest density was reported by Argentina (5.76 PMP), Uruguay (4.79 PMP), Dominican Republic (3.15 PMP), and Brazil (2.20 PMP).
In the Middle East ISN region, Kuwait (20.62 PMP), Bahrain (13.37 PMP), and Qatar (2.73 PMP) reported the highest trainee densities. Iran (0.26 PMP) and Iraq (0.32 PMP) reported the lowest densities.
In the NIS and Russia ISN region, Armenia (3.44 PMP), Belarus (2.19 PMP), and Russia (2.11 PMP) reported trainee densities higher than the global average. In contrast, Ukraine (0.23 PMP) and Kazakhstan (0.83 PMP) reported trainee densities below the global average.
In the North America ISN region, United States reported a nephrology trainee density (1.24 PMP) lower than the average global density. In contrast, Canada (2.14 PMP) reported a density higher than the global average.
In the North and East Asia ISN region, there was the greatest variation in trainee density within a region of all 10 ISN regions. Japan (35.46 PMP) reported one of the highest trainee densities globally, while Taiwan (5.56 PMP), Hong Kong (2.04 PMP), Mongolia (2.00 PMP), and South Korea (1.12 PMP) reported significantly lower densities. China (1.46 PMP) reported the second lowest density in the region, yet it reported the highest absolute number of nephrology trainees (n = 1667).
In the South Asia ISN region, all countries reported trainee densities below the global average. India (0.24 PMP) and Nepal (0.25 PMP) reported the lowest while Pakistan (1.26 PMP) and Bangladesh (0.71 PMP) reported the highest densities.
In the Western Europe ISN region, all countries reported trainee densities above the global average, except Israel (1.62 PMP). Netherlands (2.51 PMP), Belgium (2.65 PMP), and France (5.26 PMP) reported the lowest trainee densities in the region, while Norway (9.60 PMP), Greece (9.28 PMP), and Spain (7.23 PMP) reported the highest.
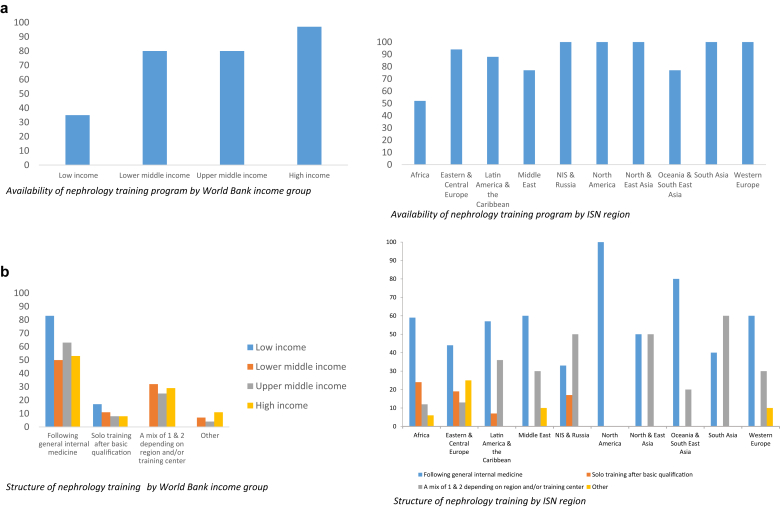
Availability of nephrology training programs
Overall, 79% of countries reported the availability of a nephrology training program. Nearly all (97%) of high-income countries and 80% of upper-middle– and lower-middle–income countries reported having a program. Less than one-half (41%) of low-income countries reported having a program (Figure 2a).
Figure 2.
(a) Availability of nephrology training programs in 121 countries. (b) Structure of nephrology training programs in 121 countries. (Continued)
Across the 10 ISN regions, all countries (100%) in 5 ISN regions—North America, North and East Asia, NIS and Russia, South Asia, and Western Europe—reported availability of training programs. In the other 5 ISN regions, the numbers of countries reporting training programs varied: Eastern and Central Europe, 94%; Latin America, 88%; Middle East, 77%; OSEA, 77%; and Africa, 52% (Figure 2a).
Structure and duration of nephrology training programs
The structure of nephrology training programs varied across countries. Overall, nephrology as a subspecialty following general internal medicine was the most reported training structure (56%). The next most reported structure was a mixed system of subspecialty and solo training for nephrology trainee depending on the region and/or training center (27%). Few countries reported solo training alone (9%) or other training arrangements (7%).
Overall, low-income countries reported training structures that were either subspecialty following general internal medicine (86%) or solo training (14%). Within the 3 other income groups, disribution across the training structure options showed minimum variation; there were similar percentage rates of countries in each income group reporting each of the 4 different training structure options (Figure 2b).
Nephrology as a subspecialty following general internal medicine was the most reported training structure across all ISN regions except NIS and Russia (33%), South Asia (40%), and North and East Asia (50%). Solo training was reported in only 4 ISN regions: Africa, 24%; Eastern and Central Europe, 19%; Latin America, 7%; and NIS and Russia, 17%. A mixed system was reported across all regions except North America, where all countries (100%) in the region reported nephrology training as a subspecialty. Other training arrangements were reported in 4 ISN regions: Africa, 6%; Eastern and Central Europe, 25%; Middle East, 10%; and Western Europe, 10% (Figure 2b).
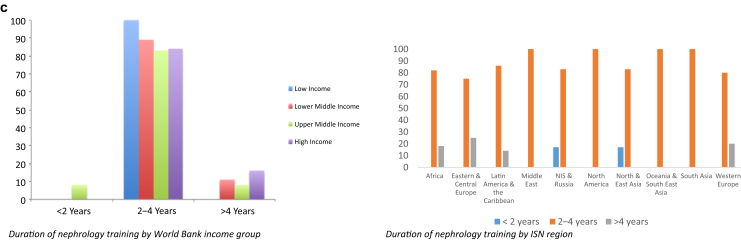
Of the countries (79%) that had a nephrology training program, 2% had a less than 2-year program, 86% had a program between 2 and 4 years, and 11% had a program of more than 4 years. Across income groups, the majority of programs were 2 to 4 years. All (n = 6) training programs offered in low-income countries were of this duration. Of the 11 countries that offered programs of more than 4 years, 55% were high-income, 18% were lower-middle–income, and 18% were upper-middle–income countries. Of these, 9% had a program of more than 4 years (Figure 2c).
Overall, most countries in the 10 ISN regions had training programs between 2 and 4 years. Programs of more than 4 years were reported in only 4 regions: Africa, 18%; Eastern and Central Europe, 25%; Latin America, 14%; and Western Europe, 20%. Programs of less than 2 years were reported in only 2 regions: NIS and Russia (17%) and North and East Asia (17%) (Figure 2c).
Shortages in health care providers in nephrology workforce
A shortage in nearly all health care provider categories essential to nephrology care was identified across all ISN regions and World Bank income groups (Table 1). Overall, the majority of countries reported a shortage in renal pathologists (86%) and vascular access coordinators (81%). Shortages were also reported by a majority of countries in the following provider categories: dietitians (78%), transplant coordinators (69%), dialysis nurses (69%), counselors and/or psychologists (67%), social workers (62%), nurse practitioners (NPs) (60%), and dialysis technicians (60%). Shortages of laboratory technicians, primary care physicians, and pharmacists were reported by less than 35% of countries. Notably, nearly three-quarters (74%) of countries reported a shortage of nephrologists (Table 1).
Low-income countries reported renal pathologists and dietitians as the provider categories with the highest shortages (100%). Lower-middle–income countries reported renal pathologists and transplant coordinators as the provider categories with the highest shortages, with 94% and 91%, respectively. Upper-middle–income countries reported renal pathologists (87%), vascular access coordinators (87%), and nephrologists (84%) as the categories with the highest shortages. In high-income countries, yet again renal pathologists (72%) and vascular access coordinators (72%) were the categories with the highest reported shortages. Overall, shortages of all health care providers, with the exception of primary care physicians (PCPs) and pharmacists, were evident across all income groups (Supplementary Figure S2A).
In the Africa ISN region, shortages in all providers were reported by more than 36% of countries. The most frequently reported shortages were of renal pathologists (100%) and dietitians (91%). More than one-half of the countries reported shortages of vascular access coordinators (88%), transplant coordinators (85%), counselors and/or psychologists (82%), dialysis technicians (76%), dialysis nurses (76%), and social workers (52%). Less than one-half of the countries reported shortages of laboratory technicians (42%) and pharmacists (36%). More countries reported shortages of nephrologists (85%) than of NPs (58%) or PCPs (39%) (Supplementary Figure S2B).
In the Middle East ISN region, most countries (85%) reported shortages of nephrologists and renal pathologists. More than three-quarters (77%) of countries reported shortages of dialysis nurses, transplant coordinators, and dietitians. More than one-half (62%–69%) of countries reported a lack of counselors and/or psychologists, vascular access coordinators, and social workers. Less than one-half of the countries reported shortages of dialysis technicians (46%), pharmacists (46%), and laboratory technicians (23%). More countries reported shortages of NPs (62%) than of PCPs (23%) (Supplementary Figure S2B).
In the Latin American and Caribbean ISN region, all countries (100%) reported a shortage of renal pathologists, while only 25% of countries reported a shortage of pharmacists. More than one-half of countries reported shortages of vascular access coordinators (94%), dialysis nurses (81%), transplant coordinators (69%), and dialysis technicians (63%). Less than one-half of the countries reported shortages of dietitians (56%), social workers (44%), counselors and/or psychologists (44%), and laboratory technicians (38%). More countries reported shortages of nephrologists (88%) than of NPs (75%) or PCPs (38%) (Supplementary Figure S2B).
In the North and East Asia ISN region, all countries (100%) reported shortages of both vascular access coordinators and social workers. More than one-half of countries reported shortages of all providers with the exception of pharmacists (17%) and laboratory technicians (17%). More countries reported a shortage of nephrologists (67%) than of NPs (83%) or PCPs (50%) (Supplementary Figure S2B).
In the South Asia ISN region, all countries (100%) reported a shortage of transplant coordinators. Eighty percent of countries reported shortages of all other providers. More countries reported shortages of nephrologists (80%) than of NPs (60%) or PCPs (40%) (Supplementary Figure S2B).
In the OSEA ISN region, all countries (100%) reported a shortage of renal pathologists. More than 80% of countries reported shortages of transplant coordinators (92%), vascular access coordinators (92%), dietitians (92%), dialysis technicians (85%), dialysis nurses (85%), counselors and/or psychologists (85%), social workers (85%), and laboratory technicians (62%). More countries reported shortages of NPs (92%) than of nephrologists (85%) or PCPs (38%) (Supplementary Figure S2B).
In the Eastern and Central European ISN region, most countries reported shortages of vascular access coordinators (82%), dietitians (76%), social workers (71%), counselors and/or psychologists (65%), renal pathologists (65%), and dialysis nurses (59%). Less than one-half of the countries reported shortages of transplant coordinators (47%) or dialysis technicians (35%). Few countries reported shortages of pharmacists (6%) or laboratory technicians (12%). More countries reported shortages of nephrologists (59%) than of NPs (47%) or PCPs (24%) (Supplementary Figure S2B).
In the NIS and Russia ISN region, all countries (100%) reported a shortage of dietitians, whereas no country in the region reported a shortage of pharmacists. More than one-half of countries reported shortages of counselors and/or psychologists (83%), transplant coordinators (67%), vascular access coordinators (67%), social workers (67%), or renal pathologists (67%). Few countries reported shortages of dialysis technicians (33%), laboratory technicians (33%), or dialysis nurses (17%). More countries reported shortages of nephrologists (67%) than of NPs (50%) or PCPs (17%) (Supplementary Figure S2B).
In the North America ISN region, the United States reported a shortage in nephrologists, PCPs, NPs, dialysis technicians, dialysis nurses, and pharmacists. Canada reported no shortage in any of the listed workforce. Overall, the North American ISN region had the lowest reported shortage in nephrology care providers (Supplementary Figure S2B).
In the Western Europe ISN region, renal pathologists (70%) were the most frequently reported shortage. Fifty percent of the countries reported shortages of dialysis nurses, vascular access coordinators, social workers, and dietitians. Less than one-half of the countries reported shortages in counselors and/or psychologists (40%), dialysis technicians (30%), transplant coordinators (20%), pharmacists (20%), and laboratory technicians (20%). More countries reported shortages of PCPs (30%) than of nephrologists (20%) or NPs (20%) (Supplementary Figure S2B).
Discussion
Summary of results and implications
The survey results showed marked inequities in the existing nephrology workforce and training capacities between countries, within regions, and across ISN regions and 2014 World Bank income groups. There were significant differences in nephrologist and nephrology trainee densities between high- and low-income countries, an absence of nephrology training programs in a large percentage of low-income countries, and shortages of all nephrology care providers in all income groups. Most countries with nephrology training programs reported training durations between 2 to 4 years, with few countries reporting more than 4 or less than 2 training years. The majority of countries reported their nephrology training structure as subspecialty training following general internal medicine, while the rest reported either solo training after primary medical qualification or a mixed system depending on the region and/or training center.
Gaps, threats, and opportunities toward sustainable provision of nephrology workforce
This study has identified several important gaps in the existing global nephrology workforce and training capacity. A key gap in kidney care was the significant variation in nephrologist density across income groups and ISN regions. This gap was most prominent in low-income countries, which reported a nephrologist density of just 0.31 PMP but accounted for more than one-half of the world’s population. Africa, with more than 1.2 billion in population, and South Asia, home of one-fourth of the world’s population, had the lowest densities of nephrologists (3.64 PMP and 1.17 PMP, respectively). These highly populated regions face the same increases in demand for health services for noncommunicable diseases as the rest of the world, in addition to the burden of communicable disease.10 The shortage can be attributed to many factors, such as limited physician training capacity23 and immigration of skilled workers across and between regions.24 Some opportunities to address this challenge include increasing workforce retention by providing incentive and opportunities for professional development locally in low-income countries and adopting policies of fair recruitment in high-income countries.25 Another opportunity lies in building the scope of PCPs in kidney care management.26
There was also a gap in nephrology trainee density. Low-income countries reported a trainee density 30 times lower than that of high-income countries. When analyzed by ISN region, 7 of the 10 lowest densities were in sub-Saharan Africa, and all countries from South Asia reported trainee densities below the global average. In contrast, all countries from North America and Western Europe reported densities above the global average. Considerable disparity was also found within ISN regions; for example, in the North and East Asia ISN region, China reported a trainee density 30 times lower than that of Japan. Although this study’s results showed adequate current nephrology trainee densities in high-income countries, many studies have shown decreased interest in the field.14, 27 Some high-income countries rely on foreign-trained doctors to cover shortages in nephrology manpower. For example, a study from Oman showed that the majority of practicing nephrologists were expatriate physicians, with local doctors representing only 14% of the workforce.28 In the United States, a recent report showed that international medical graduates represented 47% of active nephrologists and 65% of nephrology trainees.29 A recent survey from Canada suggested that, although the current nephrologist workforce may have been adequate until now, the number of trainees may not adequately meet future demand.30
Scaling up the current nephrologist workforce may not be feasible, especially for low-income countries, because it requires investment of time and money to produce highly qualified nephrologists. However, countries who are short in supply of nephrologists and face large demands for kidney care may adopt alternative models of care in the short term. One suggested approach is involving nursing and allied health care professionals through task substitution and sharing to increase efficiency of care and decrease nephrologist workload while maintaining high standards and optimal patient important outcomes.31, 32 Countries may need 9 to 10 years to produce 1 physician, and many countries with critical shortages of nephrologists cannot afford the time lag, nor possibly the cost of training. An at least partial solution may be found in utilizing allied health care professionals, but it is important that they be held to high standards of accreditation and training in nephrology care to maintain the quality of patient care.
Nephrology training programs were absent in many parts of the world. Almost one-half of the Africa ISN region reported a lack of nephrology training programs, and only 41% of low-income countries had such training. This gap is a major limiting factor for the abilities of countries to produce the future nephrologist workforce and to achieve self-reliance in providing kidney care to their populations. To scale up their nephrologist workforce, countries need to focus on producing local qualified professionals, ideally through partnerships with other countries and organizations with sufficient resources to help them establish training programs. For instance, as part of its building capacity and outreach initiative, the ISN has a fellowship program for trainees to travel to an advanced center to obtain skills and training and then return to their home country to practice.33 Since its inception, the program has sponsored more than 600 fellows.34
Another gap highlighted in this study was a shortage of all nephrology care providers across all ISN regions and World Bank income groups. The most frequently reported shortages were in renal pathologists and vascular access coordinators. Such shortages of health care providers exacerbate the adverse impacts of nephrologist shortages on kidney care that exist in many parts of the world. Health care policies in such countries should ideally cater to and support commensurate scaling up of all nephrology care providers (such as NPs, dialysis nurses, and physician assistants) rather than focusing narrowly on nephrologists and/or physicians.
Strengths and limitations of the study
This is the most comprehensive study of the global nephrology workforce and training capacity to date. The study had a high response rate and adequate representation of the world population (>93%). An established method was used to define and monitor current global nephrologist and nephrology trainee capacities. Specifically, health workforce density was used to estimate health workforce relative to the population size, as recommended by the WHO in its building blocks of health systems handbook.21 This indicator had the advantages of being simple to calculate and analyze, and being easy to understand and present to a broad audience. However, it did not take into account all dimensions critical for health workforce, such as quality, efficiency, accessibility and geographic distribution of health workforce, and annual output of health care graduates.21 This may have led to underestimation of the actual capacity of the nephrology workforce and warrants the need for further research. In the present survey, countries provided information on availability, duration, and structure of training. Other important factors in addressing training capacity are quality of training, volume, and location within the country, all of which were beyond the scope of this paper. Physicians who specialize in the management of kidney disorders (nephrologists) are the primary providers of kidney care in many parts of the world. However, depending on the region and health care setting, other caregivers such as PCPs may assume the role of nephrologists in providing kidney care. As there is no agreed standard for nephrologist density, the current study used calculated global densities of nephrologists and nephrology trainees to describe each country’s and region’s current nephrology workforce relative to the rest of the world.
Priorities and recommendations for action
-
1.
Scale up the current nephrology workforce through training qualified providers by implementing evidence-based, competence-based, and community-oriented curriculums.35, 36
-
2.
Develop robust methodology to collect data and monitor the current and future nephrology workforce.21
-
3.
Increase use of allied health professionals to increase efficiency and decrease the load on nephrologists through task substitution and/or sharing while maintaining high standards and optimal patient-important outcomes.31, 32, 37, 38, 39, 40
-
4.
Leverage cost-effective technology to increase access to specialist care while building the scope of PCPs and other allied health professionals in managing and improving outcomes of kidney patients.41, 42, 43, 44
-
5.
Augment research and scholarly activity in nephrology workforce development, management, and maintenance.45
Future work
The results of this study show a significant gap in the nephrology workforce. There is a need to move beyond the numbers and conduct more research to ascertain the other factors that influence workforce development and monitoring, such as distribution within countries and regions, demographics and age of the current workforce, and annual graduation rate of nephrologists, PCPs, NPs, and other nephrology health care providers. Moreover, there is a pressing need to research how to maximize the roles of PCPs and allied health professionals in sharing the management of kidney disease with nephrologists.
In conclusion, this study involved examining global nephrology workforce and training capacity, an essential component of any country’s health care system and especially important in nephrology to face the growing burden of kidney disease globally. With the finding of shortages of nephrologists and all health workforce related to nephrology, it can be concluded that in most parts of the world, people who need kidney care receive either suboptimal care or no kidney care at all. The lack of necessary workforce can have huge implications for individuals as well as for public health. Countries need to scale up their current nephrology workforce, develop robust methods to collect data on their human resources, and implement short- and long-term policies to produce and maintain a qualified and equitable nephrology workforce.
Methods
This cross-sectional survey was part of the GKHA project, an initiative administered under the umbrella of the ISN to assess kidney care in all world regions. The survey was conducted across all UN member states, with a particular focus on the 130 countries with ISN affiliate societies. All 10 ISN regional boards (Africa, Eastern and Central Europe, Latin America and the Caribbean, Middle East, North America, North and East Asia, OSEA, NIS and Russia, South Asia, and Western Europe) were sent an invitation letter to participate. Potential survey respondents were identified using a nonprobability, purposive sampling approach, and they involved key stakeholders identified by the country and regional nephrology leadership through the ISN, including at least 3 key representatives per country sourced from national nephrology society leadership; policy makers, including those involved directly with kidney care organization (renal policy makers) and those with a more general scope (nonrenal); and patients’ organizations, foundations, and other advocacy groups. The survey was delivered electronically (via SurveyMonkey).
The GKHA questionnaire was divided into 2 sections that addressed the core areas of countries and regional capacity for kidney care delivery. A detailed description of all survey sections has been reported elsewhere.22, 46
This study focused on the “Health Workforce for Nephrology” module of the GKHA survey. It consisted of 9 items subdivided into 2 components: existing manpower capacity and nephrology training capacity.
Survey respondents were asked about the absolute numbers of nephrologists and nephrology trainees in their country. Density was calculated by measuring the median of absolute numbers of nephrologists and/or nephrology trainees reported by at least 3 key representatives of each country and then converting it to PMP to estimate numbers relative to the population size. The density overall, and in each ISN region and World Bank income group, was calculated by the total number of nephrologists and/or nephrology trainees divided by the total number of population. Survey respondents were also asked about any perceived shortages in health care providers essential to the nephrology workforce. Given the list of staff categories, respondents were directed to indicate which ones had shortages; they also had an option to indicate no shortage of any of the staff listed.
Survey respondents were asked about the availability of a nephrology training program (for physicians) in their country, and details regarding the duration and structure of training. They were also asked to select the training pathway most relevant to their country from 4 options: (i) following general internal medicine; (ii) solo training after basic qualification as medical doctor; (iii) a mix of the first 2 options depending on region and/or training center; or, (iv) other, with the option to provide details in an open-ended response.
The term health workforce was defined as “all people engaged in actions whose primary intent is to enhance health.”21 It was a holistic definition that encompassed both health service delivery staff and administration staff. The survey focused on nephrology workforce—specifically nephrologists, dietitians, renal pathologists, laboratory technicians, social workers, pharmacists, vascular access coordinators, NPs, counselors and/or psychologists, transplant coordinators, dialysis nurses, dialysis technicians, and general practitioners and/or PCPs.
Disclosure
Publication of this article was supported by the International Society of Nephrology. The ISN holds all copyrights on the data obtained through this study.
EB-F declared seeing private patients on a part-time basis. MBG declared receiving lecture fees from AMGEN, B Braun, Leo Pharma, Novartis, Novo-Nordisk, Promopharm, Roche, Sanofi, Servier, Sophadial, and Sothema. BB declared receiving consulting fees from Otsuka and receives current grant support from Amgen. DCH declared receiving lecture fees from Roche Myanmar and Otsuka. VJ declared receiving consulting fees from Baxter and Medtronic and current grant support from the Department of Biotechnology, Government of India, Baxter, and GlaxoSmithKline. DWJ declared receiving consulting fees from AstraZeneca; lecture fees from Baxter Healthcare and Fresenius Medical Care; and support from Baxter Extramural and Clinical Evidence Council grants. KK-Z declared receiving past and future consulting and lecture fees from Abbott, AbbVie, Alexion, Amgen, AstraZeneca, Aveo, Chugai, DaVita, Fresenius, Genentech, Haymarket Media, Hospira, Kabi, Keryx, Novartis, Pfizer, Relypsa, Resverlogix, Sandoz, Sanofi, Shire, Vifor, and UpToDate; future consulting and lecture fees from ZS-Pharma; current grant support from National Institutes of Health; and expert witness engagement for GranuFlo. RK declared receiving lecture fees from Baxter Healthcare. JP declared receiving consulting fees from Fresenius Medical Care, Baxter Healthcare, Otsuka, Boehringer Ingelheim; lecture fees from Baxter Healthcare; and current grant support from Canadian Institutes of Health Research and Baxter Healthcare. All the other authors declared no competing interests.
Acknowledgments
We thank Drs. Marcello Tonelli and Valerie Luyckx for their contributions to the project and manuscript. We thank Sandrine Damster, research project manager at the International Society of Nephrology (ISN), and Alberta Kidney Disease Network (AKDN) staff (Ghennete Houston, Sue Szigety, and Sophanny Tiv) for their support with the organization and conduct of the survey and project management. We thank the ISN staff (Louise Fox and Luca Segantini) for their support. We thank the executive committee of the ISN, the ISN regional leadership, and the leaders of the ISN affiliate societies at regional and country levels for their support toward the success of this initiative.
Footnotes
Figure S1. Nephrologist density PMP from 121 countries grouped by ISN region.
Figure S2. (A) Shortages in nephrology care providers from 121 countries grouped by World Bank income group.
Figure S2. (B) Shortages in nephrology care providers from 121 countries grouped by ISN region.
Supplementary material is linked to the online version of the paper at www.kisupplements.org.
Supplementary Material
Nephrologist density PMP from 121 countries grouped by ISN region.
(A) Shortages in nephrology care providers from 121 countries grouped by World Bank income group.
(B) Shortages in nephrology care providers from 121 countries grouped by ISN region.
References
- 1.World Health Organization. The world health report 2006 – working together for health. Available at: http://www.who.int/whr/2006/en/.
- 2.Reich M.R., Harris J., Ikegami N. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387:811–816. doi: 10.1016/S0140-6736(15)60002-2. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Health workforce requirements for universal health coverage and the Sustainable Development Goals. Available at: http://www.who.int/hrh/resources/health-observer17/en/.
- 4.Hill N.R., Fatoba S.T., Oke J.L. Global prevalence of chronic kidney disease–a systematic review and meta-analysis. PLoS One. 2016;11 doi: 10.1371/journal.pone.0158765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Couser W.G., Remuzzi G., Mendis S., Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80:1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 6.The global issue of kidney disease. Lancet. 2013;382:101. doi: 10.1016/S0140-6736(13)61545-7. [No authors listed] [DOI] [PubMed] [Google Scholar]
- 7.Whiting D.R., Guariguata L., Weil C., Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y., Chen X., Song Y. Association between obesity and kidney disease: A systematic review and meta-analysis. Kidney Int. 2008;73:19–33. doi: 10.1038/sj.ki.5002586. [DOI] [PubMed] [Google Scholar]
- 9.Prakash S., O'Hare A.M. Interaction of aging and chronic kidney disease. Semin Nephrol. 2009;29:497–503. doi: 10.1016/j.semnephrol.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liyanage T., Ninomiya T., Jha V. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 11.Harley K.T., Streja E., Rhee C.M. Nephrologist caseload and hemodialysis patient survival in an urban cohort. J Am Soc Nephrol. 2013;24:1678–1687. doi: 10.1681/ASN.2013020123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharif M.U., Elsayed M.E., Stack A.G. The global nephrology workforce: emerging threats and potential solutions! Clin Kidney J. 2016;9:11–22. doi: 10.1093/ckj/sfv111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bello A.K., Levin A., Manns B.J. Effective CKD care in European countries: challenges and opportunities for health policy. Am J Kidney Dis. 2015;65:15–25. doi: 10.1053/j.ajkd.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 14.Parker M.G., Ibrahim T., Shaffer R. The future nephrology workforce: will there be one? Clin J Am Soc Nephrol. 2011;6:1501–1506. doi: 10.2215/CJN.01290211. [DOI] [PubMed] [Google Scholar]
- 15.Mehrotra R., Shaffer R.N., Molitoris B.A. Implications of a nephrology workforce shortage for dialysis patient care. Semin Dialysis. 2011;24:275–279. doi: 10.1111/j.1525-139X.2011.00933.x. [DOI] [PubMed] [Google Scholar]
- 16.Katz I.J., Gerntholtz T., Naicker S. Africa and nephrology: the forgotten continent. Nephron Clin Pract. 2011;117:C320–C326. doi: 10.1159/000321524. [DOI] [PubMed] [Google Scholar]
- 17.Manns B.J., Mendelssohn D.C., Taub K.J. The economics of end-stage renal disease care in Canada: incentives and impact on delivery of care. Int J Health Care Finance Econ. 2007;7:149–169. doi: 10.1007/s10754-007-9022-y. [DOI] [PubMed] [Google Scholar]
- 18.Field M. Addressing the global shortage of nephrologists. Nat Clin Pract Nephrol. 2008;4:583. doi: 10.1038/ncpneph0951. [DOI] [PubMed] [Google Scholar]
- 19.The International Society of Nephrology (ISN). ISN Regions. 2017. Available at: https://www.theisn.org/about-isn/regions. Accessed August 23, 2017.
- 20.The World Bank. World Bank Country and Lending Groups – World Bank Data Help Desk. Available at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed August 23, 2017.
- 21.World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Available at: http://www.who.int/healthinfo/systems/monitoring/en/.
- 22.Bello A.K., Levin A., Tonelli M. Assessment of global kidney health care status. JAMA. 2017;317:1864–1881. doi: 10.1001/jama.2017.4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mullan F., Frehywot S., Omaswa F. Medical schools in sub-Saharan Africa. Lancet. 2011;377:1113–1121. doi: 10.1016/S0140-6736(10)61961-7. [DOI] [PubMed] [Google Scholar]
- 24.Mullan F. The metrics of the physician brain drain. New Engl J Med. 2005;353:1810–1818. doi: 10.1056/NEJMsa050004. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. Health in 2015: from MDGs, millennium development goals to sdgs, sustainable development goals. Available at: http://apps.who.int/medicinedocs/documents/s22230en/s22230en.pdf.
- 26.Shahinian V.B., Saran R. The role of primary care in the management of the chronic kidney disease population. Adv Chronic Kidney Dis. 2010;17:246–253. doi: 10.1053/j.ackd.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Daniels M.N., Maynard S., Porter I. Career interest and perceptions of nephrology: a repeated cross-sectional survey of internal medicine residents. PLoS One. 2017;12 doi: 10.1371/journal.pone.0172167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alshishtawy M.M. Developing a strategic plan for medical specialties in oman. Oman Med J. 2008;23:10–14. [PMC free article] [PubMed] [Google Scholar]
- 29.Association of American Medical Colleges. 2016 physician specialty data report. Available at: https://www.aamc.org/data/workforce/reports/457712/2016-specialty-databook.html.
- 30.Ward D.R., Manns B., Gil S. Results of the 2014-2015 Canadian Society of Nephrology workforce survey. Can J Kidney Health Dis. 2016;3:25. doi: 10.1186/s40697-016-0117-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Laurant M., Reeves D., Hermens R. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev. 2005;2 doi: 10.1002/14651858.CD001271.pub2. [DOI] [PubMed] [Google Scholar]
- 32.Hongoro C., McPake B. How to bridge the gap in human resources for health. Lancet. 2004;364:1451–1456. doi: 10.1016/S0140-6736(04)17229-2. [DOI] [PubMed] [Google Scholar]
- 33.Feehally J., Brusselmans A., Finkelstein F.O. Improving global health: measuring the success of capacity building outreach programs: a view from the International Society of Nephrology. Kidney Int Suppl. 2016;6:42–51. doi: 10.1016/j.kisu.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harris D.C.H., Dupuis S., Couser W.G., Feehally J. Training nephrologists from developing countries: does it have a positive impact? Kidney Int Suppl. 2012;2:275–278. doi: 10.1038/kisup.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Okel J., Okpechi I.G., Qarni B. Nephrology training curriculum and implications for optimal kidney care in the developing world. Clin Nephrol. 2016;86:110–113. doi: 10.5414/CNP86S123. [DOI] [PubMed] [Google Scholar]
- 36.Parker M.G. Nephrology training in the 21st century: toward outcomes-based education. Am J Kidney Dis. 2010;56:132–142. doi: 10.1053/j.ajkd.2009.11.029. [DOI] [PubMed] [Google Scholar]
- 37.Anderson J.E., Torres J.R., Bitter D.C. Role of physician assistants in dialysis units and nephrology. Am J Kidney Dis. 1999;33:647–651. doi: 10.1016/s0272-6386(99)70214-3. [DOI] [PubMed] [Google Scholar]
- 38.Steinman T.I. Nephrology workforce shortfall: solutions are needed. Am J Kidney Dis. 1999;33:798–800. doi: 10.1016/s0272-6386(99)70238-6. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization. Task shifting to tackle health worker shortages - global recommendations and guidelines. Available at: http://www.who.int/healthsystems/task_shifting/en/.
- 40.Federspiel F., Mukhopadhyay S., Milsom P. Global surgical and anaesthetic task shifting: a systematic literature review and survey. Lancet. 2015;385:46. doi: 10.1016/S0140-6736(15)60841-8. [DOI] [PubMed] [Google Scholar]
- 41.Gordon E.J., Fink J.C., Fischer M.J. Telenephrology: a novel approach to improve coordinated and collaborative care for chronic kidney disease. Nephrol Dial Transpl. 2013;28:972–981. doi: 10.1093/ndt/gfs552. [DOI] [PubMed] [Google Scholar]
- 42.Haley W.E., Beckrich A.L., Sayre J. Improving care coordination between nephrology and primary care: a quality improvement initiative using the renal physicians association toolkit. Am J Kidney Dis. 2015;65:67–79. doi: 10.1053/j.ajkd.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 43.Drawz P.E., Archdeacon P., McDonald C.J. CKD as a model for improving chronic disease care through electronic health records. Clin J Am Soc Nephrol. 2015;10:1488–1499. doi: 10.2215/CJN.00940115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Osman M.A., Okel J., Okpechi I.G. Potential applications of telenephrology to enhance global kidney care. BMJ Global Health. 2017;2 doi: 10.1136/bmjgh-2017-000292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Floege J., Mak R.H., Molitoris B.A. Nephrology research–the past, present and future. Nat Rev Nephrol. 2015;11:677–687. doi: 10.1038/nrneph.2015.152. [DOI] [PubMed] [Google Scholar]
- 46.Bello AK, Johnson DW, Harris D, et al. Global kidney health atlas: design and methods. Kidney Int Suppl, in press. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Nephrologist density PMP from 121 countries grouped by ISN region.
(A) Shortages in nephrology care providers from 121 countries grouped by World Bank income group.
(B) Shortages in nephrology care providers from 121 countries grouped by ISN region.