Abstract
An international survey led by the International Society of Nephrology in 2016 assessed the current capacity of kidney care worldwide. To better understand how governance and leadership guide kidney care, items pertinent to government priority, advocacy, and guidelines, among others, were examined. Of the 116 responding countries, 36% (n = 42) reported CKD as a government health care priority, which was associated with having an advocacy group (χ2 = 11.57; P = 0.001). Nearly one-half (42%; 49 of 116) of countries reported an advocacy group for CKD, compared with only 19% (21 of 112) for AKI. Over one-half (59%; 68 of 116) of countries had a noncommunicable disease strategy. Similarly, 44% (48 of 109), 55% (57 of 104), and 47% (47 of 101) of countries had a strategy for nondialysis CKD, chronic dialysis, and kidney transplantation, respectively. Nearly one-half (49%; 57 of 116) reported a strategy for AKI. Most countries (79%; 92 of 116) had access to CKD guidelines and just over one-half (53%; 61 of 116) reported guidelines for AKI. Awareness and adoption of guidelines were low among nonnephrologist physicians. Identified barriers to kidney care were factors related to patients, such as knowledge and attitude (91%; 100 of 110), physicians (84%; 92 of 110), and geography (74%; 81 of 110). Specific to renal replacement therapy, patients and geography were similarly identified as a barrier in 78% (90 of 116) and 71% (82 of 116) of countries, respectively, with the addition of nephrologists (72%; 83 of 116) and the health care system (73%; 85 of 116). These findings inform how kidney care is currently governed globally. Ensuring that guidelines are feasible and distributed appropriately is important to enhancing their adoption, particularly in primary care. Furthermore, increasing advocacy and government priority, especially for AKI, may increase awareness and strategies to better guide kidney care.
Keywords: acute kidney injury, advocacy, chronic kidney disease, global, governance, survey
Leadership and governance are essential for overseeing and guiding an effective health care system.1 Leadership directs the strategic vision and facilitates progress through appropriate resource management,2 and governance encourages consistency and accountability.3 Together, leadership and governance create awareness, develop strategies, set priorities, and generate consistent, sustainable, and accountable action. In kidney care, effective and sustainable leadership and governance are pertinent for the development of high-quality programs, as well as for raising awareness and developing action plans for universal access to care, a globally recognized priority of any health care system.4 Acute kidney injury (AKI) and chronic kidney disease (CKD) are conditions with considerable public health implications due to associations with adverse health outcomes and high health care costs.5, 6 It is well established that AKI is a major driver for CKD and is associated with noncommunicable diseases (NCDs), yet it receives little attention compared with other conditions.7 Similarly, awareness of CKD is low despite CKD being common and expensive as well as increasing the risk of adverse events in people with other NCDs.7 As such, effective leadership and governance, as components of health care systems, are essential across countries to ensure these conditions receive adequate national and international priority. The extent and impact of the various leadership and governance structures (policies, guidelines, and frameworks) for AKI and CKD across countries remains unclear.
As part of the Global Kidney Health Atlas (GKHA) project, a multinational survey conducted through the International Society of Nephrology (ISN),8, 9 we set out to understand the distribution of leadership and governance structures for kidney care worldwide. Furthermore, we sought to describe the modes of operation, specifically focusing on priority actions, advocacy efforts, strategies, guidelines, awareness, and barriers.
Results
In total, 125 of 130 countries (96%) that received an invitation participated in the survey. Of these, 93% (n = 116) responded to the questions relevant to leadership and governance. Complete details on the response rate and population coverage of the survey have been published elsewhere.8, 9
Priority of and advocacy for kidney care
CKD was recognized as a health care priority (defined as outlining principles, defining practices, or both10) by government in 36% (n = 42) of countries overall, and in 53% (9 of 17), 52% (16 of /31), 20% (6 of 30), and 29% (11 of 38) of low-, lower middle-, upper middle-, and high-income countries, respectively (Table 1). Overall, 42% (49 of 116) reported the existence of an advocacy group at higher levels of government to raise the profile of CKD and its prevention. This was more common in low- (53%; 9 of 17) and lower middle- (48%; 15 of 31) income countries compared with upper middle- (37%; 11 of 30) and high- (37%; 14 of 38) income countries (Table 1). Overall, 46% (49 of 116) had neither CKD identified as a government health care priority nor an advocacy group for CKD. Identifying CKD as a government health care priority was significantly associated with having an advocacy group for CKD (χ2 = 11.57; P = 0.001). Advocacy for AKI was less than one-half that for CKD (Table 1).
Table 1.
Recognition of CKD as a health care priority by government and presence of advocacy groups across countries
| Region | CKD |
AKI |
|||
|---|---|---|---|---|---|
| Number of responding countries | Health care priority | Availability of an advocacy group | Number of responding countries | Availability of an advocacy group | |
| Overall | 116 | 42 (36) | 49 (42) | 112 | 21 (19) |
| ISN region | |||||
| Africa | 30 | 14 (47) | 16 (53) | 28 | 9 (32) |
| Eastern and Central Europe | 16 | 2 (13) | 3 (19) | 16 | 1 (6) |
| LAC | 16 | 5 (31) | 7 (44) | 15 | 3 (20) |
| Middle East | 13 | 6 (46) | 6 (46) | 13 | 1 (8) |
| NIS and Russia | 6 | 3 (50) | 3 (50) | 6 | 2 (33) |
| North America | 2 | 0 (0) | 2 (100) | 1 | 0 (0) |
| North and East Asia | 6 | 2 (33) | 0 (0) | 6 | 0 (0) |
| OSEA | 13 | 4 (31) | 8 (62) | 13 | 3 (23) |
| South Asia | 5 | 3 (60) | 1 (20) | 5 | 1 (20) |
| Western Europe | 9 | 3 (33) | 3 (33) | 9 | 1 (11) |
| World Bank Income Group | |||||
| Low income | 17 | 9 (53) | 9 (53) | 16 | 4 (25) |
| Lower middle income | 31 | 16 (52) | 15 (48) | 30 | 10 (33) |
| Upper middle income | 30 | 6 (20) | 11 (37) | 29 | 5 (17) |
| High income | 38 | 11 (29) | 14 (37) | 37 | 2 (5) |
AKI, acute kidney injury; CKD, chronic kidney disease; ISN, International Society of Nephrology; LAC, Latin America and the Caribbean; NIS, Newly Independent States (of the former Soviet Union); OSEA, Oceania and Southeast Asia. Values are n or n (%).
Strategies for kidney care
Fifty-nine percent (68 of 116) of countries overall had a national NCD strategy, and 18% (21 of 116) reported having a strategy under development (Table 2). A higher proportion of high-income countries (26%; 10 of 38), compared with low-income countries (12%; 2 of 17), reported no NCD strategy.
Table 2.
Existence of national strategies for NCD and CKD across 116 countries
| Region | NCD strategya |
CKD strategyb |
||||
|---|---|---|---|---|---|---|
| Yes | Under development | No | Nondialysis | Dialysis | Transplant | |
| Overall | 68 (59) | 21 (18) | 27 (23) | 48 (44) | 57 (55) | 47 (47) |
| ISN region | ||||||
| Africa | 18 (60) | 9 (30) | 3 (10) | 8 (31) | 8 (35) | 7 (30) |
| Eastern and Central Europe | 7 (44) | 1 (6) | 8 (50) | 6 (38) | 9 (60) | 8 (57) |
| LAC | 9 (56) | 5 (31) | 2 (13) | 10 (63) | 8 (50) | 10 (63) |
| Middle East | 6 (46) | 4 (31) | 3 (23) | 5 (38) | 8 (73) | 5 (50) |
| NIS and Russia | 3 (50) | 0 (0) | 3 (50) | 2 (33) | 4 (67) | 3 (50) |
| North America | 2 (100) | 0 (0) | 0 (0) | 1 (50) | 1 (50) | 0 (0) |
| North and East Asia | 6 (100) | 0 (0) | 0 (0) | 4 (67) | 4 (67) | 1 (17) |
| OSEA | 11 (85) | 0 (0) | 2 (15) | 7 (58) | 7 (58) | 5 (45) |
| South Asia | 2 (40) | 1 (20) | 2 (40) | 1 (33) | 3 (75) | 3 (75) |
| Western Europe | 4 (44) | 1 (11) | 4 (44) | 4 (44) | 5 (56) | 5 (56) |
| World Bank Income Group | ||||||
| Low income | 10 (59) | 5 (29) | 2 (12) | 6 (38) | 3 (23) | 4 (31) |
| Lower middle income | 16 (52) | 5 (16) | 10 (32) | 9 (35) | 14 (58) | 9 (39) |
| Upper middle income | 17 (57) | 8 (27) | 5 (17) | 15 (52) | 20 (67) | 17 (57) |
| High income | 25 (66) | 3 (8) | 10 (26) | 18 (47) | 20 (54) | 17 (49) |
CKD, chronic kidney disease; ISN, International Society of Nephrology; LAC, Latin America and the Caribbean; NCD, noncommunicable disease; NIS, Newly Independent States (of the former Soviet Union); OSEA, Oceania and Southeast Asia. Values are n (%).
Number of countries that answered this question (denominator) is 116.
Existence of a strategy, whether as an independent strategy or incorporated into a NCD strategy. Number of countries that answered this question (denominator) is 109 (nondialysis CKD), 104 (chronic dialysis), and 101 (kidney transplantation).
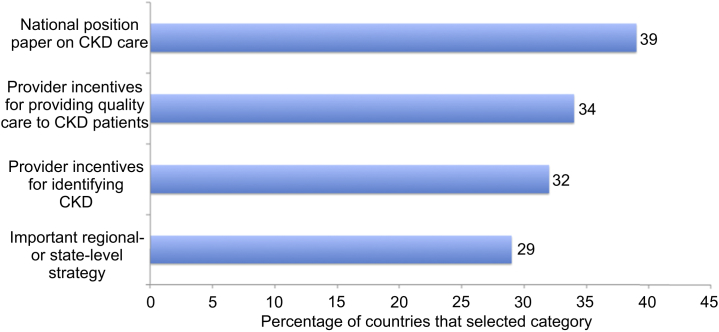
In total, 44% (48 of 109) of countries reported a national strategy for improving the care of nondialysis CKD patients, 55% (57 of 104) for chronic dialysis patients, and 47% (47 of 100) for kidney transplantation patients (Table 2). Conversely, 40% (46 of 116) of countries reported no national strategy for CKD care (irrespective of nondialysis CKD, chronic dialysis, or transplant). In these countries, other initiatives that identified CKD as a health care priority included having strategies at a regional or state level, a national position paper on CKD (a document providing an overview of information and recommendations for kidney care, but not mandated by legislation), and incentives for identifying CKD and providing quality care to CKD patients (Figure 1).
Figure 1.
Reported distribution of initiatives for promoting chronic kidney disease (CKD) as a health care priority among countries with no national strategy for CKD (n = 38). Of the 46 countries with no CKD strategy, 38 responded to this question. Percentages do not sum to 100% as countries were able to select more than 1 option.
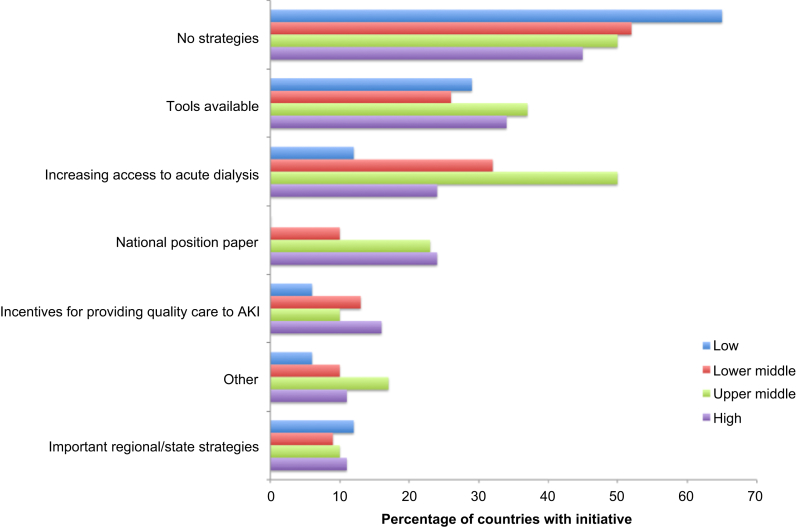
Forty-nine percent of countries (57 of 116) reported at least 1 strategy for improving the identification of AKI (Figure 2). The most common strategies were having tools available (32%; 37 of 116) and increasing access to acute dialysis facilities (31%; n = 36). Sixteen percent of countries (19 of 116) reported a national position paper on AKI identification and care (Figure 2). Position papers were more common in high- (24%; 9 of 38) and upper middle- (23%; 7 of 30) income countries compared with lower middle-income countries (10%; 3 of 31). No low-income (0%) countries reported a national position paper on AKI identification and care (Figure 2).
Figure 2.
National policies and strategies for identifying acute kidney injury (AKI), by World Bank income group across 116 countries. Percentages do not sum to 100% as countries were able to select more than 1 option.
National or regional organizations, either physician- or patient-oriented, that provide financial resources for kidney care were much higher for CKD (53% of countries; 62 of 116) than AKI (23%; 27 of 116). The presence of CKD organizations was lower in low-income countries (29%; 5 of 17) compared with high-income countries (66%; 25 of 38), and likewise for AKI organizations (6%; 1 of 17 and 29%; 11 of 38, respectively).
Awareness and adoption of guidelines for kidney care
Overall, access to management and referral guidelines was less common for AKI (53%; 61 of 116) than CKD (79%; 92 of 116) (Table 3). A lack of guidelines was more common among low-income countries than high-income countries, for both AKI and CKD. National guidelines for AKI and CKD were available in 7% (8 of 116) and 27% (31 of 116) of countries, respectively (Table 3). Access to international guidelines was slightly less for AKI (45%; 52 of 116) and CKD (52%; 60 of 116). AKI guidelines covered identification of AKI in inpatient (95%; 57 of 60) and outpatient (67%; 40 of 60) settings, access to dialysis treatment (93%; 56 of 60), timing and urgency for nephrology referral (80%; 48 of 60), and protocols for mitigating risk of AKI in specific situations (70%; 42 of 60). CKD guidelines covered complication management (86%; 79 of 92), identification of CKD progression (88%; 81 of 92), timing and urgency of nephrology referral (87%; 80 of 92), risk factor management (84%; 77 of 92), and multidisciplinary care approaches (71%; 65 of 92).
Table 3.
Availability of and access to management and referral guidelines for kidney care across 116 countries
| Region | AKI management and referral guidelines |
CKD management and referral guidelines |
||||||
|---|---|---|---|---|---|---|---|---|
| National | Regional | International | None | National | Regional | International | None | |
| Overall | 8 (7) | 1 (1) | 52 (45) | 55 (47) | 31 (27) | 1 (1) | 60 (52) | 24 (21) |
| ISN region | ||||||||
| Africa | 2 (7) | 0 (0) | 8 (27) | 20 (67) | 4 (13) | 0 (0) | 13 (43) | 13 (43) |
| Eastern and Central Europe | 0 (0) | 0 (0) | 15 (94) | 1 (6) | 2 (13) | 0 (0) | 13 (81) | 1 (6) |
| LAC | 1 (6) | 0 (0) | 7 (44) | 8 (50) | 9 (56) | 0 (0) | 7 (44) | 0 (0) |
| Middle East | 0 (0) | 0 (0) | 5 (38) | 8 (62) | 1 (8) | 1 (8) | 8 (62) | 3 (23) |
| NIS and Russia | 2 (33) | 0 (0) | 3 (50) | 1 (17) | 1 (17) | 0 (0) | 5 (83) | 0 (0) |
| North America | 0 (0) | 0 (0) | 2 (100) | 0 (0) | 1 (50) | 0 (0) | 1 (50) | 0 (0) |
| North and East Asia | 0 (0) | 0 (0) | 2 (33) | 4 (67) | 3 (50) | 0 (0) | 3 (50) | 0 (0) |
| OSEA | 2 (15) | 1 (8) | 3 (23) | 7 (54) | 6 (46) | 0 (0) | 2 (15) | 5 (38) |
| South Asia | 0 (0) | 0 (0) | 1 (20) | 4 (80) | 0 (0) | 0 (0) | 3 (60) | 2 (40) |
| Western Europe | 1 (11) | 0 (0) | 6 (67) | 2 (22) | 4 (44) | 0 (0) | 5 (56) | 0 (0) |
| World Bank Income Group | ||||||||
| Low income | 0 (0) | 0 (0) | 3 (18) | 14 (82) | 1 (6) | 0 (0) | 6 (35) | 10 (59) |
| Lower middle income | 5 (16) | 0 (0) | 11 (35) | 15 (48) | 7 (23) | 0 (0) | 16 (52) | 8 (26) |
| Upper middle income | 1 (3) | 1 (3) | 14 (47) | 14 (47) | 9 (30) | 0 (0) | 16 (53) | 5 (17) |
| High income | 2 (5) | 0 (0) | 24 (63) | 12 (32) | 14 (37) | 1 (3) | 22 (58) | 1 (3) |
AKI, acute kidney injury; CKD, chronic kidney disease; ISN, International Society of Nephrology; LAC, Latin America and the Caribbean; NIS, Newly Independent States (of the former Soviet Union); OSEA, Oceania and Southeast Asia. Values are n (%).
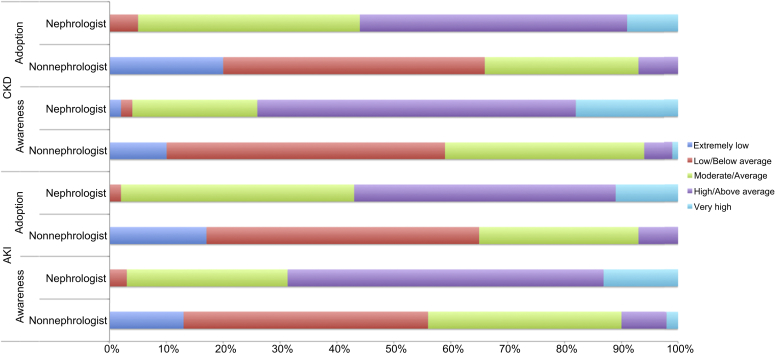
In countries that did have guidelines for AKI or CKD or both, awareness and adoption of the guidelines were lower among nonnephrologist physicians than among nephrologists (Figure 3). Very few countries reported an extremely low or low awareness or adoption of AKI guidelines among nephrologists (3%; 2 of 60 and 2%; 1 of 60, respectively), whereas among nonnephrologist physicians, the rate of countries reporting an extremely low or low awareness or adoption was 56% (34 of 61) and 65% (39 of 60), respectively. Similarly, an extremely low or low awareness or adoption of CKD guidelines was uncommon among nephrologists (4%; 4 of 91 and 5%; 5 of 92, respectively), and was more than one-half (59%; 54 of 92 and 66%; 60 of 91) among nonnephrologist physicians. When income level was considered, awareness of AKI guidelines among nonnephrologist physicians was lower in low-income countries than in high-income countries as 100% (3 of 3) of low- and 50% (13 of 26) of high-income countries reported an extremely low or low awareness. Adoption of AKI guidelines among nonnephrologist physicians was also lower in low-income countries (100%; 3 of 3) than in high-income countries (58%; 15 of 26). Likewise, low-income countries reported an extremely low or low awareness (86%; 6 of 7) and adoption (86%; 6 of 7) of CKD guidelines among nonnephrologist physicians, which was comparatively lower in high-income countries (46%; 17 of 37 and 54%, 20 of 37, respectively). Among nephrologists, the awareness and adoption of guidelines were similar across income groups for both AKI and CKD.
Figure 3.
Reported awareness and adoption of acute kidney injury (AKI) and chronic kidney disease (CKD) guidelines among nonnephrologist physicians and nephrologists in countries with available AKI (n = 61) and CKD (n = 92) guidelines.
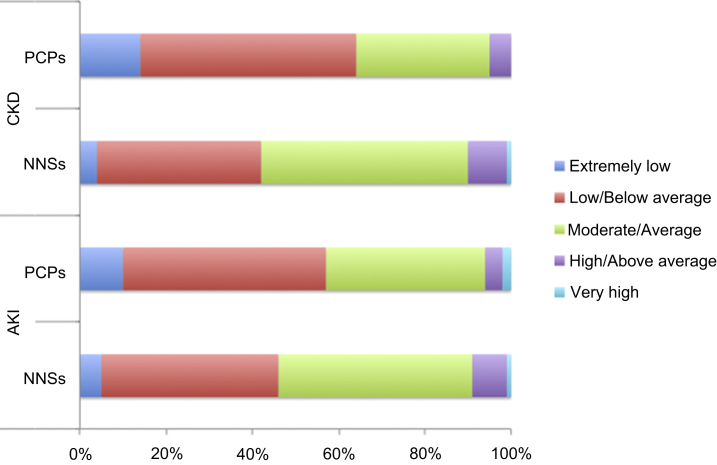
Awareness of AKI and CKD
Among nonnephrologist specialists, awareness of AKI was extremely low or low in 46% (53 of 116) of countries, and awareness of CKD was similarly extremely low or low in 42% of countries (49 of 116) (Figure 4). Considering income group, a rating of extremely low or low awareness of AKI among nonnephrologist specialists was reported in 53% (9 of 17) of low-income countries, compared with only 32% (12 of 38) of high-income countries. Likewise, a rating of extremely low or low awareness of CKD was reported in 53% (9 of 17) of low-income countries and in 24% (9 of 38) of high-income countries.
Figure 4.
Reported levels of awareness of acute kidney injury (AKI) and chronic kidney disease (CKD) among nonnephrologist specialists (NNSs) and primary care physicians (PCPs) across 116 countries.
Awareness of AKI and CKD among primary care physicians was similar (Figure 4). Overall, an extremely low or low level of awareness among primary care physicians was reported in 57% (66 of 116) of countries for AKI and in 64% (74 of 116) for CKD. Among primary care physicians, awareness of AKI was extremely low or low in 71% of low-income countries (12 of 17) and in 66% (25 of 38) of high-income countries. The proportion of low- and high-income countries that reported an extremely low or low awareness of CKD was higher in low-income countries (82%; 14 of 17) than in high-income countries (37%; 14 of 38).
Barriers to optimal kidney care
Respondents were asked to select factors they believed to be barriers (i.e., a factor that limits the delivery of optimal care) of kidney disease care and barriers of renal replacement therapy (RRT). Most countries (91%; 100 of 110) identified patient-related factors (knowledge, attitude) as a primary barrier of optimal kidney care, followed by physician-related factors (availability, access, knowledge, and attitude; 84%; 92 of 110) (Table 4). Geography, that is, distance from care or prolonged travel time, was a barrier to kidney care for 74% (81 of 110) of countries. Availability of nephrologists was a barrier in only 20% (22 of 110) of countries, as was the availability, access, or capability of the health care system. With respect to RRT, patient-related factors were the highest reported barrier (78%; 90/ of 115), however this was less of a barrier than that reported for kidney care in general (Table 4). Availability of nephrologists and the health care system were barriers for most countries (72%; 83 of 115 and 74%; 85 of 115, respectively), comparably much higher than reported for general kidney care. Physicians were less of a barrier for RRT (65%; 75 of 115) than for general kidney care, and geography was essentially an equal barrier for RRT (71%; 82 of 115) as for general kidney care (Table 4). The existence of barriers of optimal kidney disease care was generally higher in low-income countries than in high-income countries, most notably with respect to geography (94% vs. 38%, respectively). The presence of geography, nephrologist, the health care system, and physician-related barriers were all at least 40% higher in low-income countries than in high-income countries (Table 4).
Table 4.
Self-reported barriers to optimal kidney disease care and RRT across countries
| Region | Optimal kidney disease care (n = 110) |
Optimal renal replacement therapy (n = 116) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Geographya | Physicianb | Patientc | Nephrologistsd | Health care systeme | Other | Geographya | Physicianb | Patientc | Nephrologistsd | Health care systeme | Other | |
| Overall | 81 (74) | 92 (84) | 100 (91) | 22 (20) | 22 (20) | 8 (7) | 82 (71) | 75 (65) | 90 (78) | 83 (72) | 85 (73) | 40 (34) |
| ISN region | ||||||||||||
| Africa | 28 (97) | 23 (79) | 26 (90) | 7 (24) | 7 (24) | 0 (0) | 25 (83) | 22 (73) | 21 (70) | 25 (83) | 29 (97) | 6 (20) |
| Eastern and Central Europe | 5 (38) | 11 (85) | 13 (100) | 0 (0) | 0 (0) | 0 (0) | 5 (31) | 4 (25) | 9 (56) | 7 (44) | 9 (56) | 5 (31) |
| LAC | 13 (81) | 13 (81) | 11 (69) | 13 (81) | 13 (81) | 6 (38) | 13 (81) | 9 (56) | 12 (75) | 13 (81) | 4 (25) | 3 (19) |
| Middle East | 6 (50) | 11 (92) | 12 (100) | 0 (0) | 0 (0) | 0 (0) | 6 (46) | 10 (77) | 11 (85) | 9 (69) | 12 (92) | 5 (38) |
| NIS and Russia | 5 (83) | 4 (67) | 5 (83) | 0 (0) | 0 (0) | 0 (0) | 5 (83) | 3 (50) | 6 (100) | 4 (67) | 3 (50) | 1 (17) |
| North America | 1 (50) | 2 (100) | 2 (100) | 0 (0) | 0 (0) | 0 (0) | 1 (50) | 1 (50) | 2 (100) | 2 (100) | 2 (100) | 1 (50) |
| North and East Asia | 2 (33) | 6 (100) | 6 (100) | 0 (0) | 0 (0) | 0 (0) | 4 (67) | 4 (67) | 6 (100) | 4 (67) | 4 (67) | 4 (67) |
| OSEA | 11 (85) | 13 (100) | 13 (100) | 1 (8) | 1 (8) | 1 (8) | 12 (92) | 13 (100) | 13 (100) | 12 (92) | 13 (100) | 8 (62) |
| South Asia | 5 (100) | 5 (100) | 5 (100) | 0 (0) | 0 (0) | 0 (0) | 5 (100) | 5 (100) | 5 (100) | 5 (100) | 5 (100) | 2 (40) |
| Western Europe | 5 (63) | 4 (50) | 7 (88) | 1 (13) | 1 (13) | 1 (13) | 6 (67) | 4 (44) | 5 (56) | 2 (22) | 4 (44) | 5 (56) |
| World Bank Income Group | ||||||||||||
| Low income | 16 (94) | 15 (88) | 16 (94) | 6 (35) | 6 (35) | 1 (6) | 15 (88) | 14 (82) | 14 (82) | 14 (82) | 17 (100) | 4 (24) |
| Lower middle income | 28 (93) | 26 (87) | 28 (93) | 5 (17) | 5 (17) | 2 (7) | 28 (90) | 22 (71) | 26 (84) | 29 (94) | 24 (77) | 11 (35) |
| Upper middle income | 24 (83) | 24 (83) | 24 (83) | 8 (28) | 6 (21) | 2 (7) | 23 (77) | 21 (70) | 24 (80) | 24 (80) | 21 (70) | 6 (20) |
| High income | 13 (38) | 27 (79) | 32 (94) | 3 (9) | 5 (15) | 3 (9) | 16 (42) | 18 (47) | 26 (68) | 16 (42) | 23 (61) | 19 (50) |
ISN, International Society of Nephrology; LAC, Latin America and the Caribbean; NIS, Newly Independent States (of the former Soviet Union); OSEA, Oceania and Southeast Asia, RRT, renal replacement therapy. Values are n (%).
Distance from care or prolonged travel time.
Availability, access, knowledge, attitude.
Knowledge, attitude.
Availability.
Availability, access, capability.
Discussion
Summary of results and implications
Advocacy and national policy
The GKHA survey showed low prioritization of CKD by government and minimal presence of advocacy groups. Low- and lower middle-income countries reported higher rates of prioritization and advocacy. This could be due to a higher burden of kidney disease in these regions,11 or a lower capacity for kidney care. Advocacy for AKI was even lower. The ISN launched the “0by25” initiative in 2013, aiming to eliminate all preventable deaths from AKI worldwide by 2025.12 However, its implementation in developing countries has been difficult. Reasons may include a lack of resources to diagnose and treat AKI, limited information on the epidemiology and causes of AKI, or low awareness of how AKI impacts patient outcomes.13 Furthermore, this initiative is not integrated into existing programs and instead, typically is presented in nephrology forums. This results in a poor dissemination of information regarding the program’s existence. However, the GKHA survey did not aim to identify reasons for, or areas of, prioritization, nor whether action was generated as a result of this prioritization. Further clarification regarding what efforts are planned and implemented is important to identify next steps and goals for governance and leadership.
National strategies for CKD and AKI were lacking in over half of countries, despite a high occurrence of national strategies for NCDs in general. While the prevalence of CKD is less than the 4 main NCDs defined by the World Health Organization (cardiovascular disease, cancer, respiratory diseases, and diabetes),14 CKD may lead to poorer health outcomes and is associated with an increased morbidity of NCDs and therefore deserves political attention.7 Of the countries that did report a CKD strategy, there were fewer strategies for nondialysis CKD than for transplantation and chronic dialysis CKD. Early implementation of CKD prevention programs has resulted in the greatest cost savings in countries that have adopted universal health care coverage,7 and therefore strategies on earlier stages of kidney disease may help reduce the burden of CKD and NCDs in general.
Similarly, national strategies for AKI prevention and management were low overall and nonexistent in low-income countries. Due to the burden of AKI and the potential of it leading to CKD,7 strategies to reduce AKI are important. Incorporating AKI and CKD in overarching NCD strategies, or creating strategies specifically for kidney disease, may reduce the overall morbidity due to these conditions.
Increasing advocacy may have an impact on policy. For example, the number of countries with a national salt reduction strategy doubled over a 5-year period, of which 60% involved advocacy organizations in their leadership and strategic approach.15 Specific to kidney disease, the impact of the Kidney Disease Outcomes Quality Initiative guidelines advocating for standardized terminology has greatly benefited research and practice.16 The GKHA survey showed a significant relationship between having CKD as an established government health care priority and the presence of an advocacy group for CKD. However, it is unknown whether advocacy drives priority or vice versa, or whether other confounding factors impact this association. Advocacy is a wide-ranging term and can refer to patient groups, organizations, and providers, and while all forms are important for government prioritization in various ways, evidence on the optimal channels for delivering messages, for example, media, is limited.17 The development of appropriate strategies is important for future goals; therefore understanding the best ways to advocate for kidney disease care is needed. Increasing communication between leaders in nephrology (nephrologists, researchers, and other experts) and governing bodies (national and regional administrators) will help create strategies that are evidence-based and guided through expertise.
Awareness of CKD and AKI among physicians
Nonnephrologist physicians play a key role in preventing and managing kidney disease. Due to the high prevalence of kidney disease worldwide and a comparable shortage of nephrologists, primary care physicians are often the health care professionals caring for patients with kidney disease.5 Furthermore, primary care physicians, and to a lesser degree nonnephrologist specialists (predominantly cardiologists and endocrinologists), play a key role in monitoring patients with early-stage kidney disease that may not yet require referral to a nephrologist. As such, awareness of CKD and AKI is imperative in nonnephrologist physicians. In the GKHA survey, awareness of CKD and AKI was reported as low or moderate in nonnephrologist specialists, and awareness was even less among primary care physicians. Linking of nephrologists with primary care physicians has been shown to improve the process for identifying CKD and increasing awareness of risk factors, among other benefits,18 and could help increase awareness of CKD among nonnephrologist physicians. Similarly, increasing awareness of AKI among nonnephrologist physicians is essential for preventing AKI.19 The GKHA survey showed a lower level of awareness of kidney disease among nonnephrologist physicians in low-income countries. While there are likely other matters of high priority in these regions, kidney disease remains a major problem for developing countries,20 and efforts to increase awareness in these regions is important.21
Awareness and adoption of guidelines
Presumably due to the low global attention to kidney disease, awareness of both CKD and AKI guidelines as reported in the GKHA survey was fairly low in nonnephrologist physicians, particularly in low- and lower middle-income countries. Even where awareness was reported, the adoption of guidelines among nonnephrologist physicians was low. Reduced adoption of kidney disease guidelines in low- and lower middle-income countries had been observed previously, prompting a meeting organized by the Kidney Disease: Improving Global Outcomes foundation to reflect on barriers of adoption.22 Research investigating barriers of adherence to kidney disease guidelines among renal health care professionals identified system-level and kidney-disease-specific barriers; for example, lack of health insurance, workforce shortages, inadequate knowledge or data, and a lack of policies.23 In the GKHA survey, awareness and adoption of guidelines was higher for nephrologists, irrespective of income level. Employing leadership to increase communication between nephrologists and nonnephrologist physicians may increase the awareness and circulation of guidelines and promote their adoption. However, reasons unrelated to awareness, as outlined by the Kidney Disease: Improving Global Outcomes, should be addressed through the creation of context-specific guidelines to ensure they are feasible based on local capacity. Other research identifying possible causes of the implementation gap between kidney disease guidelines and clinical practice in primary care24 could also be leveraged to generate strategies to disseminate guidelines appropriately to enhance their uptake in practice.
Barriers to optimal kidney care
Top barriers to kidney care identified in the GKHA survey were related to patient, physician, and geography factors. Previous research has suggested patient-related barriers in chronic disease management are related to patients’ finances,25, 26 attitudes or beliefs, knowledge, language, and comorbidities,26 among others. Other research, specific to kidney disease, identified a number of patient-reported barriers to care,27 including, for example, a lack of understanding about kidney disease, feeling unwell or low mood, limited knowledge on permissible foods, issues on maintaining dietary and fluid restrictions, lack of motivation, and other stressors in their life aside from kidney disease.27 Recognizing the barriers patients face enables appropriate resources to enhance their understanding or support better management of their health. Likewise, provider-related barriers can be addressed through capacity building (continuing medical education), reward for performance, and quality improvement (e.g., audit and feedback).28, 29 Factors such as providers’ beliefs, attitudes, and knowledge, and patient-provider interaction and communication have previously been suggested as barriers to care.26 Geography, likely reflecting rurality, is a common barrier to accessing many health care services, due to the need to travel long distances and limited availability of health care professionals,30 among other reasons. Telehealth and rural peer-support groups31 may be beneficial in reducing this barrier. Nephrologist density is low, particularly in low- and lower- middle-income groups.9 Increasing the supply of well-trained nephrologists may reduce provider-related barriers of kidney care.9 Understanding other provider shortages (e.g., dialysis nurses, psychologists) may also close the gaps of care related to provider limitations. Sharing of resources within the global nephrology community may also increase the quality and consistency of kidney care, particularly in areas where access to guidelines is low.
Similar to the barriers to kidney care, the top barriers of RRT were identified in the GKHA survey as related to patients, physicians (including nephrologists), and geography. Limitations of the health care system were also identified. This finding coincides with other research that described challenges to patients’ optimal RRT preparation as limited health system resources, provider skills, and patient attitudes and cultural differences.32 As patients requiring RRT may need closer care from a nephrologist, having a short supply of nephrologists would undoubtedly be a barrier to RRT. Exploring how kidney care delivery can be shared across multiple providers may enhance the use of multidisciplinary teams33 and thereby address nephrologist-related shortages that limit capacity of RRT.
Priorities and recommendations for action
Increase the prioritization of kidney disease
The GKHA survey reported only one-third of countries recognize CKD, which was more prevalent in low-income countries, as a health care priority by government. Investigating the factors influencing this priority (e.g., competing priorities or a lack of information) is important. Moreover, evaluating how priority translates into action is also important. Appropriate knowledge translation between the nephrology leadership and national and regional administrators may increase the recognition of the costs of CKD and its association with other more common NCDs, possibly leading to an increase in government prioritization of kidney disease.
Develop effective advocacy groups for kidney disease
Advocacy groups facilitate dialogue among patients, providers, and policymakers and are essential for appropriate knowledge translation. The GKHA survey revealed few advocacy groups for both CKD and AKI. Developing national groups may help prioritize kidney disease and engage and empower patients to better manage their health. Expanding the presence of international advocacy groups, such as the ISN, may help connect countries to encourage information sharing and support.
Leverage existing strategies and policies for kidney care
Incorporating aspects of kidney care into existing strategies and policies may help increase capacity. For example, expanding strategies for common NCDs to include elements of kidney care may be appropriate as there are often shared comorbidities or a bidirectional association. Increasing awareness of how kidney disease relates to these conditions may demonstrate the appropriateness of including kidney care in these common strategies.
Raise the awareness and adoption of guidelines for kidney care
Nearly one-half of countries reported no access to AKI guidelines, and CKD guidelines were inaccessible in 20% of countries. Awareness and adoption of guidelines was particularly low among primary care physicians. As these physicians play a critical role in the prevention of end-stage renal disease, increasing the adoption of guidelines in primary care is important. Ensuring guidelines are accessible, appropriate to local contexts, and feasible may help increase their dissemination and use.
This study consistently collected data from purposively selected respondents using a survey developed through a validated conceptual framework.3 Nearly 90% (116 of 130) of countries responded to questions pertaining to governance and leadership. Data were reviewed by regional and national stakeholders and confirmed with findings from a literature review of secondary data sources. However, this study has limitations. As with any survey, there is a potential for subjective responses due to the limitations of the respondents’ knowledge and further, for social desirability bias. Of particular note, only 2 of the 15 countries representing the ISN region of North America and the Caribbean responded to the survey (Canada and United States), which has great risk of selection bias. Furthermore, this study collected information on the existence of strategies and policies and did not inquire on the implementation or action as a result of these policies.
In conclusion, governance and leadership in kidney care is important to drive strategies and provide guidelines to overall enhance the quality of care. Linking nephrologists, researchers, and other experts in kidney care with national and regional administrators may encourage evidence-based policies built on expertise. Furthermore, advocacy plays an important role in governance and leadership through connecting patients, providers, and policymakers to increase awareness and communication. Better understanding barriers to optimal kidney care and developing evidence-based, feasible, and context-appropriate strategies may lead to an improved capacity for kidney care.
Materials and Methods
Full details of the GKHA project have been published elsewhere.8, 9 In brief, a multinational survey was developed by the ISN to assess readiness, capacity, and response to CKD and AKI based on the World Health Organization building blocks of a health system.3 Country representatives of ISN-affiliated countries were invited to participate in the survey, based on their expertise in nephrology and health care administration.
Leadership and governance is listed as 1 of these 6 building blocks, and 10 core indicators have been set for evaluating its presence and efficacy.3 These indicators focus primarily on national health strategies and policies, management, collaboration and partnership, standardized optimal practice through guidelines, and accountability. Effective leadership and governance is critical in health care, as it impacts the development, implementation, and sustainability of public health programs to optimize national health goals.34 As such, this work sought to understand the current level of leadership and governance worldwide with respect to kidney care.
Items in the GKHA survey related to leadership and governance were selected to describe the current global situation of kidney care with respect to advocacy and national policy, awareness and adoption of guidelines, and barriers to kidney care and RRT. Key terms were defined in the questionnaire distributed to survey respondents to ensure clarity.
-
•
Advocacy: parliamentary committee (government) or nongovernment organization.
-
•
Adoption of guidelines: application in clinical practice.
-
•
Policy: specific official decision or set of decisions designed to carry out a course of action endorsed by a government body, including a set of goals, priorities, and main directions for attaining these goals. The policy document may include a strategy to give effect to the policy.
-
•
Strategy: long-term plan designed to achieve a particular goal for AKI or CKD care.
-
•
Guidelines: recommended evidence-based course of action for prevention or management of AKI or CKD or both.
Data analyses were conducted using STATA 13 software (Stata Corporation, College Station, TX). The unit of analysis was responding country, and results were stratified by ISN region35 and 2014 World Bank country classification as low-, lower middle-, upper middle-, and high-income nations.36 Responses were summarized using descriptive statistics and reported as counts and percentages. To examine the relationship between country-reported CKD government priority and advocacy, a Pearson chi-squared test statistic was estimated with 1 degree of freedom.
Disclosure
Publication of this article was supported by the International Society of Nephrology. The International Society of Nephrology holds all copyrights on the data obtained through this study.
EBF declared seeing private patients on a part-time basis. MBG declared receiving lecture fees from Amgen, B Braun, Leo Pharma, Novartis, Novo-Nordisk, Promopharm, Roche, Sanofi, Servier, Sophadial, and Sothema. VJ declared receiving consulting fees from Baxter and Medtronic; and current grant support from the Department of Biotechnology, Government of India, Baxter, and GlaxoSmithKline. DWJ declared receiving consulting fees from AstraZeneca; lecture fees from Baxter Healthcare and Fresenius Medical Care; and support from Baxter Extramural and Clinical Evidence Council grants. KK-Z declared receiving past and will receive future consulting and lecture fees from Abbott, AbbVie, Alexion, Amgen, AstraZeneca, Aveo, Chugai, DaVita, Fresenius, Genentech, Haymarket Media, Hospira, Kabi, Keryx, Novartis, Pfizer, Relypsa, Resverlogix, Sandoz, Sanofi, Shire, Vifor, and UpToDate; will receive future consulting and lecture fees from ZS-Pharma; currently receives grant support from National Institutes of Health; and is serving as an expert witness engagement for GranuFlo. RK declared receiving lecture fees from Baxter Healthcare. JP declared receiving consulting fees from Fresenius Medical Care, Baxter Healthcare, Otsuka, and Boehringer Ingelheim; lecture fees from Baxter Healthcare; and currently receives grant support from Canadian Institutes of Health Research and Baxter Healthcare. All the other authors declared no competing interests.
Acknowledgments
We thank Dr. Valerie Luyckx for her contribution to the Global Kidney Health Atlas project and manuscript, Sandrine Damster, research project manager at the International Society of Nephrology (ISN), and Alberta Kidney Disease Network staff (Ghennete Houston, Sue Szigety, Sophanny Tiv) for their support with the organization and conduct of the survey and project management. We thank the ISN staff (Louise Fox and Luca Segantini) for their support. We thank the executive committee of the ISN, the ISN regional leadership, and the leaders of the ISN affiliate societies at regional and country levels for their support toward the success of this initiative.
References
- 1.Uneke C.J., Ezeoha A.E., Ndukwe C.D. Enhancing leadership and governance competencies to strengthen health systems in Nigeria: assessment of organizational human resources development. Healthc Policy. 2012;7:73–84. [PMC free article] [PubMed] [Google Scholar]
- 2.Department for Health Policy, Development, and Services, Health Systems and Services, World Health Organization . World Health Organization; Working paper 10, WHO/HSS/healthsystems/2007.3.Geneva, Switzerland: 2007. Towards Better Leadership and Management in Health: Report on an International Consultation on Strengthening Leadership and Management in Low-Income Countries: 29 January–1 February 2007, Accra, Ghana. [Google Scholar]
- 3.World Health Organization . World Health Organization; Geneva, Switzerland: 2010. Monitoring the Building Blocks of the Health Systems: A Handbook of Indicators and Their Measurement Strategies. [Google Scholar]
- 4.The Lancet Universal health coverage—looking to the future. Lancet. 2016;388:2837. doi: 10.1016/S0140-6736(16)32510-7. [DOI] [PubMed] [Google Scholar]
- 5.Jha V., Garcia-Garcia G., Iseki K. Chronic kidney disease: global dimension and perspectives. Lancet. 2013;382:260–272. doi: 10.1016/S0140-6736(13)60687-X. [DOI] [PubMed] [Google Scholar]
- 6.Mehta R.L., Cerda J., Burdmann E.A. International Society of Nephrology's 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385:2616–2643. doi: 10.1016/S0140-6736(15)60126-X. [DOI] [PubMed] [Google Scholar]
- 7.Couser W.G., Remuzzi G., Mendis S. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80:1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 8.Bello A.K., Johnson D.W., Feehally J. Global Kidney Health Atlas (GKHA): design and methods. Kidney Int Suppl. 2017;7:145–153. doi: 10.1016/j.kisu.2017.08.001. https://doi.org/10.1016/j.kisu.2017.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bello A.K., Levin A., Tonelli M. Assessment of global kidney health care status. JAMA. 2017;317:1864–1881. doi: 10.1001/jama.2017.4046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sabik L.M., Lie R.K. Priority setting in health care: lessons from the experiences of eight countries. Int J Equity Health. 2008;7:4. doi: 10.1186/1475-9276-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jha V., Arici M., Collins A.J. Understanding kidney care needs and implementation strategies in low- and middle-income countries: conclusions from a “Kidney Disease: Improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int. 2016;90:1164–1174. doi: 10.1016/j.kint.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Stanifer J.W., Muiru A., Jafar T.H., Patel U.D. Chronic kidney disease in low- and middle-income countries. Nephrol Dial Transplant. 2016;31:868–874. doi: 10.1093/ndt/gfv466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ponce D., Balbi A. Acute kidney injury: risk factors and management challenges in developing countries. Int J Nephrol Renovasc Dis. 2016;9:193–200. doi: 10.2147/IJNRD.S104209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feehally J. The ISN 0by25 Global Snapshot Study. Ann Nutr Metab. 2016;68(suppl 2):29–31. doi: 10.1159/000446202. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. Noncommunicable Diseases: Fact Sheet 2015. Available at: http://www.who.int/mediacentre/factsheets/fs355/en/. Accessed February 13, 2017.
- 16.Trieu K., Neal B., Hawkes C. Salt reduction initiatives around the world—a systematic review of progress towards the global target. PLoS One. 2015;10:e0130247. doi: 10.1371/journal.pone.0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coresh J. A decade after the KDOQI CKD guidelines: impact on research. Am J Kidney Dis. 2012;60:701–704. doi: 10.1053/j.ajkd.2012.08.012. [DOI] [PubMed] [Google Scholar]
- 18.Bou-Karroum L., El-Jardali F., Hemadi N. Using media to impact health policy-making: an integrative systematic review. Implement Sci. 2017;12:52. doi: 10.1186/s13012-017-0581-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haley W.E., Beckrich A.L., Sayre J. Improving care coordination between nephrology and primary care: a quality improvement initiative using the renal physicians association toolkit. Am J Kidney Dis. 2015;65:67–79. doi: 10.1053/j.ajkd.2014.06.031. [DOI] [PubMed] [Google Scholar]
- 20.Li P.K., Burdmann E.A., Mehta R.L. Acute kidney injury: global health alert. Kidney Int. 2013;83:372–376. doi: 10.1038/ki.2012.427. [DOI] [PubMed] [Google Scholar]
- 21.Garcia-Garcia G., Jha V. Chronic kidney disease in disadvantaged populations. Ind J Nephrol. 2015;25:65–69. doi: 10.4103/0971-4065.150078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perico N., Remuzzi G. Need for chronic kidney disease prevention programs in disadvantaged populations. Clin Nephrol. 2015;83(suppl 1):42–48. doi: 10.5414/cnp83s042. [DOI] [PubMed] [Google Scholar]
- 23.van der Veer S.N., Tomson C.R., Jager K.J. Bridging the gap between what is known and what we do in renal medicine: improving implementability of the European Renal Best Practice guidelines. Nephrol Dial Transplant. 2014;29:951–957. doi: 10.1093/ndt/gft496. [DOI] [PubMed] [Google Scholar]
- 24.Tsang J.Y., Blakeman T., Hegarty J. Understanding the implementation of interventions to improve the management of chronic kidney disease in primary care: a rapid realist review. Implement Sci. 2016;11:47. doi: 10.1186/s13012-016-0413-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell D.J., Manns B.J., Weaver R.G. Financial barriers and adverse clinical outcomes among patients with cardiovascular-related chronic diseases: a cohort study. BMC Med. 2017;15:33. doi: 10.1186/s12916-017-0788-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nam S., Chesla C., Stotts N.A. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93:1–9. doi: 10.1016/j.diabres.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Lo C., Teede H., Fulcher G. Gaps and barriers in health-care provision for co-morbid diabetes and chronic kidney disease: a cross-sectional study. BMC Nephrol. 2017;18:80. doi: 10.1186/s12882-017-0493-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Eijkenaar F., Emmert M., Scheppach M. Effects of pay for performance in health care: a systematic review of systematic reviews. Health Policy. 2013;110:115–130. doi: 10.1016/j.healthpol.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 29.Shaw J., Wong I., Griffin B. Principles for health system capacity planning: insights for healthcare leaders. Healthc Q. 2017;19:17–22. doi: 10.12927/hcq.2017.25016. [DOI] [PubMed] [Google Scholar]
- 30.Brundisini F., Giacomini M., DeJean D. Chronic disease patients' experiences with accessing health care in rural and remote areas: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser. 2013;13:1–33. [PMC free article] [PubMed] [Google Scholar]
- 31.Lauckner H.M., Hutchinson S.L. Peer support for people with chronic conditions in rural areas: a scoping review. Rural Remote Health. 2016;16:3601. [PubMed] [Google Scholar]
- 32.Greer R.C., Ameling J.M., Cavanaugh K.L. Specialist and primary care physicians' views on barriers to adequate preparation of patients for renal replacement therapy: a qualitative study. BMC Nephrol. 2015;16:37. doi: 10.1186/s12882-015-0020-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Collister D., Russell R., Verdon J. Perspectives on optimizing care of patients in multidisciplinary chronic kidney disease clinics. Can J Kidney Health Dis. 2016;3:32. doi: 10.1186/s40697-016-0122-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kirigia J.M., Kirigia D.G. The essence of governance in health development. Int Arch Med. 2011;4:11. doi: 10.1186/1755-7682-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.International Society of Nephrology. Regions. Available at: https://www.theisn.org/about-isn/regions. Accessed August 22, 2017.
- 36.World Bank. World Bank country and lending groups—World Bank data help desk. Available at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519. Accessed August 22, 2017.