Abstract
Objective:
Negative affect (NA) reactivity to daily stressors may confer health risks over and above stressor exposure, especially in chronically-angry adults. This randomized controlled trial tests the hypothesis that a 12-week cognitive behavior therapy (CBT) anger reduction treatment would decrease NA reactivity to daily stressors assessed via ambulatory diary for those in the treatment but not wait list group.
Method:
158 healthy adults aged 20–45 years, 53.20% female, scoring high on Spielberger trait anger, were randomly assigned to CBT treatment or wait list control, and completed 24 hours of pre-randomization and post-intervention ecological momentary assessment (EMA) of NA intensity and stress events every 20 ± 5 minutes. A longitudinal model using a generalized estimating equation examined whether stressor exposure and NA reactions to momentary stressors changed from pre- to post-treatment in the CBT group.
Results:
There was a significant 3-way interaction (t28 = 2.29, p = .03) between stressor, treatment group, and EMA day indicating NA reactivity decreased for the treatment group 1.60 points more than for wait list (a 379.38% greater change in NA reactivity). NA during stressors was 1.18 points lower (a 28.42% decrease) for the treatment group at EMA day 2 (p = 0.04) while wait list NA during stressors non-significantly increased.
Conclusions:
CBT to decrease chronic anger is associated with lower NA reactivity to daily stressors in this sample and could be a promising treatment to mitigate the health impact of stress in this clinical population.
Keywords: trait anger, stress reactivity, ecological momentary assessment, cognitive behavior therapy, negative affect
Stress is a complex reaction to an internal or external agent experienced as a threat to one’s well-being that causes the individual to recruit cognitive, affective, and physiological systems for the restoration of homeostasis and safety (Lazarus, 1993). Although stress responses can be adaptive, the association between stress exposure and markers of physical health risk, such as inflammation, is well established for both acute stress studied in laboratory settings (Kamarck et al., 1997; Marsland, Walsh, Lockwood, & John-Henderson, 2017) and chronic daily stress that persists over time (Richardson et al., 2012; Rosengren et al., 2004; Steptoe & Kivimaki, 2013; Sumner et al., 2016).
Recent longitudinal evidence suggests that the health-compromising effects of stress may derive not only from exposure to stress but also from affective reactivity to that exposure, that is, the magnitude of an individual’s emotional response to a stressful event (Bolger & Zuckerman, 1995; Charles, Piazza, Mogle, Sliwinski, & Almeida, 2013; Mroczek et al., 2013). In a longitudinal study of 435 participants from the National Study of Daily Experiences (Almeida, 2017) who completed a series of daily diary interviews between 1995 and 1996, greater affective reactivity to daily stressors, but not frequency of exposure to daily stressors, was associated with an increased risk of reporting a chronic physical health condition 10 years later (Piazza, Charles, Sliwinski, Mogle, & Almeida, 2013). Cross-sectional analysis of data from 872 participants in that same study revealed that people who reported greater reductions in positive affect on days when stressors were reported had elevated levels of inflammation indexed by Interleukin-6 even after controlling for relevant covariates and stressor frequency (Sin, Graham-Engeland, Ong, and Almeida 2015). These data suggest that affective responses to daily stress, over and above exposure to the stress, may have effects on health.
Daily stress events can be associated with changes in multiple types of negative affect (NA; including but not limited to anxiety, sadness, and anger) depending on the nature of the external threat (Schilling & Diehl, 2014). Internal consistency between different types of momentary NA has emerged (Merz et al., 2013; Crawford, 2004) in studies using scales such as the Positive and Negative Affect Schedule (PANAS; (Watson, 1988). For this reason, Schilling and Diehl (2014) have called NA the “domain of choice” for measuring the impact of daily stressors (p.73) in both momentary and trait NA studies (Bleil, Gianaros, Jennings, Flory, & Manuck, 2008). However while associations between stress and NA have been explored in various nonclinical (Montpetit, Bergeman, Deboeck, Tiberio, & Boker, 2010; Schilling & Diehl, 2014) and clinical samples (Peeters, Nicolson, Berkhof, Delespaul, & deVries, 2003), NA reactivity to stress in the chronic anger population has not received similar attention.
As Bolger (1990) proposed, individual differences in personality can influence patterns of stressor exposure, affective reactions to stress, and coping choices, adding nuance to the understanding of why the experience of stress is a greater risk for some than for others. For example, several studies have found that the association between stress and negative affect (NA) is moderated by levels of trait neuroticism (Bolger & Schilling, 1991; Bolger & Zuckerman, 1995; Mroczek & Almeida, 2004) and individual differences in coping and resilience resources (Montpetit et al., 2010). Trait anger and hostility have been associated with adverse cardiac health outcomes in previously healthy populations (Everson-Rose et al., 2014; Williams, Nieto, Sanford, & Tyroler, 2001) and poorer outcomes for patients with coronary heart disease (e.g. (Chida & Steptoe, 2009; Kucharska-Newton et al., 2014). Stress exposure and reactivity patterns therefore become a compelling focus for clinical intervention in the high trait anger population.
Chronic anger is characterized by anticipatory monitoring of perceived slights, attacks, or unjust actions on the part of others (Barazzone & Davey, 2009; Gardner & Moore, 2008; Owen, 2011). Coupled with this habitual interpersonal vigilance, some studies have shown increased intensity and duration of anger responses to daily provocations for those higher in trait anger (Tafrate, Kassinove, & Dundin, 2002) and hostility (Enkelmann et al., 2005; Smith, Glazer, Ruiz, & Gallo, 2004; Vella, Kamarck, Flory, & Manuck, 2012). Following Bolger and Zuckerman’s model of a differential exposure-reactivity model, we propose that high trait anger and hostility increase both the likelihood of daily stressor exposure, and the magnitude of emotional reactivity to that exposure (Bolger & Zuckerman, 1995), compromising an individual’s ability to effectively regulate his or her NA response to daily stress. This formulation suggests that a cognitive behavioral therapy (CBT) intervention to shift cognitive frameworks and impart skills for reducing reactivity may mitigate the health risks associated with high trait anger.
Negative affective reactivity to stressors lends itself to an ecological momentary assessment (EMA) approach to the investigation of the stressor–affect relationship (Kamarck et al., 2005; Tennen, Affleck, & Armeli, 2005). While there is a strong evidence base for CBT as an effective treatment for decreasing chronic anger (Lee & DiGiuseppe, 2018), the inclusion of EMA monitoring in a randomized controlled trial of CBT for questionnaire-assessed trait anger addresses a need for greater ecological validity identified by a recent review of the literature (Fernandez, Malvaso, Day, & Guharajan, 2018). In particular, the use of EMA allows a comparison of NA at moments with and without reported stressors in order to quantify reactivity in daily life before and after the CBT intervention. In this paper, we examine the association between stressor exposure and NA intensity on a moment-to-moment basis in a treatment study of adults high in trait anger and hostility that significantly reduced trait anger scores for those in the CBT but not wait list condition (Sloan et al., 2010). We also examine whether a CBT treatment protocol to reduce hostility alters the association between ambulatory measures of NA and current stressful events during one day of EMA monitoring. Specifically, we hypothesize that (1) NA will be higher during current relative to non-stress moments for both groups at both EMA days, and that after 12 weeks of CBT treatment, those in the treatment group will have (2) lower NA at EMA day 2 during current stress moments compared to the wait list group, and (3) lower NA reactivity during current stressor moments compared to non-stressor moments, while the wait list group will not have lower NA reactivity.
Method
Study Design
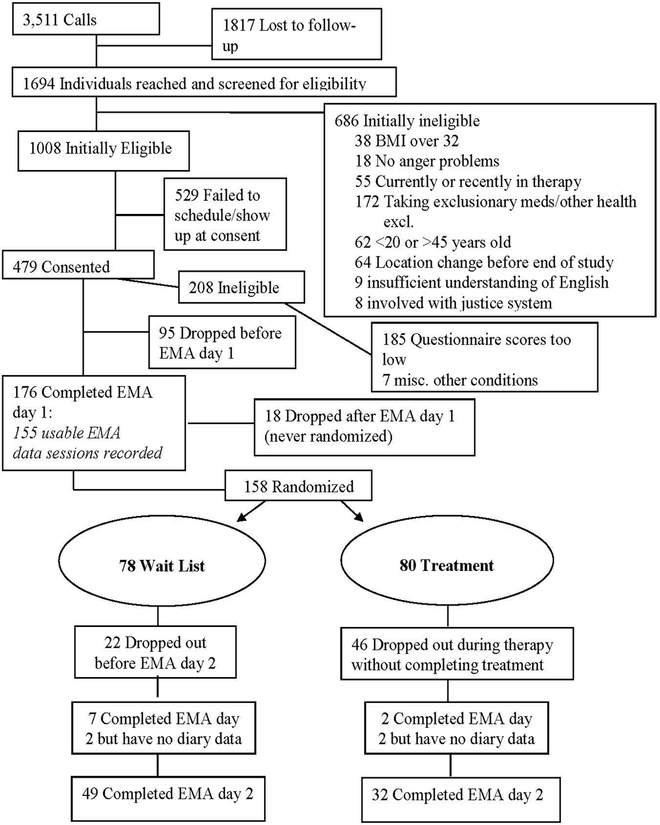
The parent study was a randomized controlled trial to test the hypothesis that a 12-week CBT anger and hostility reduction treatment would increase cardiac autonomic regulation in participants who were high in trait anger and hostility as measured by two standard assessments (Sloan et al., 2010). Participants completed a 24 hours of ambulatory monitoring assessing affect intensity and stressor exposure during waking hours at study entry and again after the intervention and these EMA data form the basis for the present study. (See Figure 1 for a CONSORT diagram). This research was approved by the New York State Psychiatric Institute Institutional Review Board.
Figure 1:
CONSORT participant flow diagram
Participants
Participants were recruited from the New York City area via print, Internet, and radio advertisements to receive a “free anger-management treatment program” as part of their participation in a research study. Data collection lasted from November 2000 to February 2005. Initially eligible participants were between the ages of 20 and 45 years of age, with a BMI ≤ 32, and had no significant medical problems. Participants were required to score ≥26 on the 50-point Cook-Medley Hostility Scale (Cook & Medley, 1954), and ≥25 on the 30-point trait anger scale of the Spielberger State-Trait Anger Expression Inventory (STAXI) questionnaire (Spielberger, 1988), assessed at an initial appointment after participants provided informed consent.
Study clinicians then interviewed each initially eligible participant individually before randomization to assess the suitability of CBT treatment for their presenting anger problems. During this interview, the clinician assessed treatment goals and psychiatric history to rule out serious clinical issues including current major depressive disorder, anxiety disorder, past or current suicidal ideation or self-injurious behavior, personality disorders, and substance use disorders. The clinician also reviewed the study protocol with the participant, including the possibility of randomization to the wait list condition. Participants who were deemed to need immediate treatment or for whom the CBT protocol was considered inappropriate were referred for treatment elsewhere. Eligible participants reported long-standing anger issues that caused them significant distress in domestic, interpersonal, occupational, and/or public domains of daily life, without any past or current physical aggression or court referral to anger management treatment (as intrinsic motivation for treatment would be uncertain). Additionally they were not receiving any other psychological treatment or taking psychoactive medications. A typical participant’s anger usually manifested as uncontrolled outbursts, or as a more contained internal experience with fewer outbursts.
Experimental Protocol
Prior to randomization and again after the 12-week treatment period, participants completed 24 hours of electrocardiogram (ECG) monitoring to capture 24-hour heart rate variability (HRV), which was the primary outcome of the study. This monitoring period length is standard of care in clinical cardiology and the frequency of prompts is similar to other studies of momentary affect (Ebner-Priemer & Trull, 2009), which evidence suggests is sufficient to capture individual differences in NA states while still providing estimates that are robust against the mood effects of a particular day (Edmondson, 2013). Eligible participants reported to the laboratory at 8AM on a weekday for baseline testing. A Marquette 8500 ECG recorder was attached to Two ECG leads were attached to channels CM2 and CM5 of the Marquette 8500 ECG recorder (Marquette Electronics Inc., Milwaukee, Wisconsin), after which participants completed a laboratory mental stress task protocol described elsewhere (Sloan et al., 2010). After the laboratory study and until the following morning, participants resumed their regular daily activities while continuing with ECG recording and carrying a pre-programmed Palm IIIe personal digital assistant (PDA; Palm, Inc., Sunnyvale, CA). The PDA was programmed to beep every 20 ± 5 minutes between 8:15am and 11:00pm, and participants began responding to prompts after the conclusion of their laboratory session until initiation of sleep. Each prompt presented a brief series of questions about stress and NA and responses were entered into the PDA.
Upon the completion of 24 hours of monitoring, participants returned the ECG recorder and PDA by mail, and after receipt of equipment by the research team, were randomized to either a wait list control group or active CBT anger reduction treatment. After completion of 12 weekly sessions of treatment or wait list, participants returned for EMA day 2 testing and completed another 24-hour ECG monitoring with PDA diary data collection. After this second session, wait list participants began treatment. EMA day 3 laboratory testing and 24-hour ECG monitoring was conducted as a 6-month posttreatment follow-up for the treatment group and immediately after completing treatment for the wait list group. Participants received monetary compensation for each EMA day they completed. Here, we report the results of the PDA diary data collection at EMA day 1 and day 2. Data collection staff members were blind to randomization group.
Measurement of Stressors and Negative Affect
At each EMA prompt, participants reported exposure to stressors since last prompt, ratings of current NA, and responses to other questions about activity, location, physical position, and social interaction. The questions about stressful events began with a frequency count of stressors since last beep (“Since last beep, how many stressful events?”), whether a stress event was “current,” (“The MOST stressful event since the last beep: How long ago was it?”) and whether the most stressful event was interpersonal or not. Regarding measurements of NA, participants were asked to estimate how “irritated or annoyed,” “nervous or anxious,” and “sad or disappointed” they felt “right now” on a 7-point Likert scale (with 0 = “not at all” and 6= “very”) and NA at each prompt time was operationalized as a sum of responses to those 3 diary items (for an NA sum range of 0–18). Other affect items also assessed but not included in the current hypotheses were “happy”, “relaxed”, “tired or drained”, and “alert or energetic,” as the present analysis focused only on items with negative valence that have shown strong positive correlations with each other in the stress reactivity literature (Crawford & Henry, 2004). Similarly to “irritable” in the PANAS (Watson, Clark, & Tellegen, 1988), the milder language of “irritated or annoyed” was chosen to represent momentary anger in the diary in order to facilitate participants’ attending to angry feelings across a continuum from mild to extreme rather than only the more intense or obvious expressions of anger. There was high internal consistency for NA between these three diary items at EMA day 1 (Cronbach α=.77) and EMA day 2 (Cronbach α=.83). Following the approach of Sliwinski, Almeida, Smyth, and Stawski (2009), we operationalized NA reactivity to stressors as the numeric rating of composite NA during episodes when a stressor was reported compared to the level of NA when no stressor was reported.
Cognitive Behavior Therapy Treatment
The purpose of the CBT intervention was to reduce the amount of time patients spent experiencing anger on a daily basis. Participants met with one of three clinicians (E. Gorenstein, C. Monk, or F.Tager) individually for 45–60 minutes, once a week, for 12 consecutive weeks. The manualized treatment developed by Drs. Ethan Gorenstein and Felice Tager follows an exposure-based counter conditioning model in which participants are coached to apply cognitive, physical, and behavioral skills to decrease angry reactions to anger-provoking events (Gorenstein, Tager, Shapiro, Monk, & Sloan, 2007). An anger event was defined as having three components: (a) the triggering event, (b) the person’s internal reaction (including cognitive appraisal of the event and physiological arousal), and (c) a behavioral or verbal response. Treatment components included: (1) psychoeducation on the conceptual model of persistent anger, (2) self-monitoring of significant angry feelings, (3) cognitive restructuring of thoughts reported in self-monitoring logs, (4) behavior therapy (including social and communication skills training, and problem-solving training), (5) relaxation combined with visualized exposure to anger-provoking situations in session, and (6) in vivo exposure (i.e. contrived exposure to anger-provoking situations in daily life combined with application of cognitive-behavioral skills). The session-by-session treatment was delivered as a complete sequence of these six components, while allowing clinicians to use their judgment in placing emphasis on certain components over others depending on the individual needs of each participant. Participants assigned to the control group were placed on a 12-week waiting list for treatment, after which they received the same CBT-treatment as the intervention group.
Statistical Analysis
Differences between treatment groups (CBT and wait list) in demographic characteristics at baseline and differences in dropout were assessed using t-tests for continuous variables and chi-square tests for categorical variables.
A longitudinal model utilizing a generalized estimating equation was used to examine whether stressor exposure and affective reactions to momentary stressors changed from pre- to post-treatment in the CBT group. The longitudinal model was run on all randomized participants included the effects of treatment group (CBT compared to wait list), ambulatory NA and stressor assessment (EMA day 2 compared to EMA day 1), stressor (current stressor compared to no stressor), all of their 2-way interactions (group*EMA day, group*stressor, EMA day*stressor) and their 3-way interaction (group*EMA day*stressor). The longitudinal model controlled for age, sex, ethnicity, and baseline trait anger. Pre-specified contrasts that can be explored only when the 3-way interaction is significant were included to estimate effects of stressor and treatment in relation to the hypotheses of interest. Cohen’s d effect sizes were computed using F-test statistics for pre-specified contrasts, where 0.2 is a small effect, 0.5 is a moderate effect, and 0.8 is a large effect (Cohen, 1988; Thalheimer & Cook, 2002).
Analyses were done in SAS® version 9.4 using PROC GLIMMIX. All statistical tests were 2-sided with significance level of 5%. To run longitudinal models in SAS, complete data is not required, and even the model that analyzes incomplete data provides unbiased results under the assumption that unobserved values are missing-at-random (Little, 2002). Our analysis of dropout across groups and within the CBT group showed no significant association with demographic characteristics, trait anger, trait hostility, stressor frequency or NA at baseline. Thus, missing data could be assumed to be missing-at-random and their analysis is expected to lead to unbiased estimates.
Results
Demographic information appears in Table 1. One hundred fifty eight participants were randomized to either the CBT (n=80) or wait list (n=78) groups. At baseline, the groups did not differ on age, sex, ethnicity, trait anger, or trait hostility (all p-values are > 0.05). The primary analysis found randomization to the treatment group to be associated with a significant reduction in trait anger scores relative to baseline (−1.071± 0.286, p < .001; (Sloan et al., 2010).
Table 1.
Pre-randomization participant demographics
| CBT (n=80) | Wait list (n=78) | ||
|---|---|---|---|
| Characteristic | Mean ± SD or n (%) | Mean ± SD or n (%) | p-value |
| Sex (female) | 42 (52.5%) | 42 (53.85%) | .87 |
| Age (years) | 30.64 ± 6.70 | 30.91 ± 6.77 | .80 |
| Ethnic Origin | .64 | ||
| Asian/Pacific Islander | 5 (6.25%) | 9 (11.54%) | |
| Black, Non-Hispanic | 14 (17.50%) | 16 (20.51%) | |
| Hispanic | 18 (22.50%) | 18 (23.08%) | |
| White, Non-Hispanic | 41 (51.25%) | 32 (41.03%) | |
| Native American, Other or Unknown | 2 (2.50%) | 3 (3.85%) | |
| Trait Anger | 30.80 (4.66) | 30.69 (3.85) | .87 |
| Trait Hostility | 32.71 (5.78) | 32.72 (5.37) | .99 |
Dropout Analysis
A total of 90 participants completed EMA day 2 (CBT n = 34, wait list n = 56), but due to nine cases of PDA equipment failure, 81 of those participants provided EMA data for both baseline and follow-up assessments (CBT n = 32, wait list n = 49; See Figure 1). Dropouts were defined as participants who exited the study before completion of treatment or 12 weeks of waiting without completing EMA day 2 and there were no participants who exited the study prematurely but still provided EMA day 2 data. No significant differences were found between those who dropped out and those who completed the protocol on sex, age, ethnicity, or baseline trait anger or hostility scores across both groups, though rates of dropout before follow-up testing were significantly higher for those randomized to the CBT group (60% vs. 37%; χ2 (1) = 8.23, p < .01). Additionally, across both groups, there were no significant differences in baseline momentary NA (b = −0.37, SE = 0.73, p = .62) or in the likelihood of reporting a stressful event (b = 0.082, SE = 0.34, p = .81) between those who completed the study compared to those who dropped out. Among the CBT group only, there were also no significant differences between dropouts and completers on any of these demographic factors or baseline trait anger or hostility scores.
EMA Hypotheses
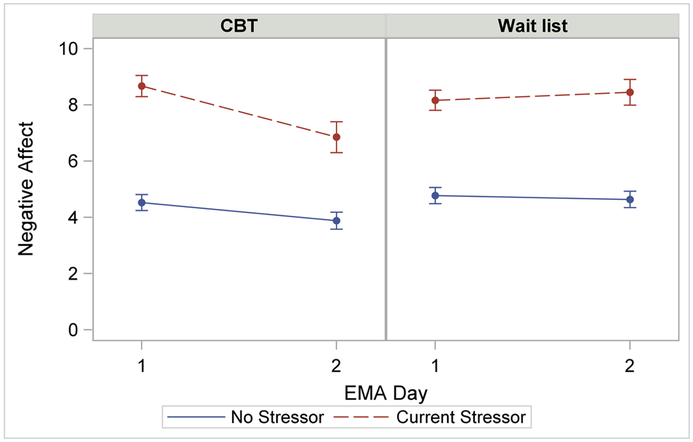
Participants completed a total of 7,186 diary entries across the two EMA monitoring days. The average number of diary prompts each participant completed was 30.20 (SD= 5.88) on EMA day 1 and 30.18 (SD= 5.20) on EMA day 2. Among those in the CBT group, 87.34% (69 of 79) of participants had at least one missing NA value at EMA day 1 with a median compliance rate of 86.36%, and 90.63% (29 of 32) had at least one missing NA value at EMA day 2 with a median compliance rate of 84.50%. Among those in the wait list group, 84.21% (64 of 76) had at least one missing NA value at EMA day 1 with a median compliance rate of 86.75%, and 84.31% (43 of 51) had at least one missing NA value at EMA day 2 with a median compliance rate of 84.85%. There were no group differences in the proportion of completers or the compliance rate between groups at either EMA day (p > .05). Descriptive statistics for NA ratings across groups, EMA days, and stressor vs. non-stressor moments appear in Table 2 and Figure 2. Participants were more likely to report current stressors at the first EMA day compared to the second (OR = 0.58, 95% CI = [0.4, 0.77], p < .001); this did not differ across treatment conditions (p = .60).
Table 2.
Mean negative affect (NA) during non-stressor and stressor moments for each group at each EMA day.
| CBT | Wait list | |||
|---|---|---|---|---|
| EMA day 1 Mean ± SE | EMA day 2 Mean ± SE | EMA day 1 Mean ± SE | EMA day 2 Mean ± SE | |
| Current stressor | 8.67 (0.38) | 6.85 (0.55) | 8.17 (0.36) | 8.45 (0.46) |
| No stressor | 4.53 (0.28) | 3.88 (0.30) | 4.78 (0.29) | 4.64 (0.29) |
Figure 2.
Negative affect (NA) model adjusted means by treatment group during moments with and without reported current stressors
Table 3 presents the results and computed effect sizes of the pre-specified contrasts for the EMA model. The significant 3-way interaction (t28 = 2.29, p = .030 , Cohen’s d = .37) between stressor, treatment group, and EMA day indicates a differential effect of stressor on NA from EMA day 1 to day 2 between the treatment and wait list groups. The effect size for this interaction was found to exceed Cohen’s (1988) convention for a small effect (d = .2).
Table 3.
Model estimated effects of pre-specified contrasts predicting negative affect (NA)
| Pre-specified simple effects estimates | Cohen’s d ES | |||||
|---|---|---|---|---|---|---|
| Contrasts | Estimate | SE | DF | t | p-value | |
| 3-way interaction (CBT X Stressor X EMA day): | 1.60 | 0.70 | 28 | 2.29 | .03 | 0.37 |
| CBT only: | ||||||
| Current vs no stressor, EMA day 2 vs EMA day 1 | −1.18 | 0.55 | 28 | −2.15 | .04 | 0.34 |
| EMA day 1, current vs no stressor | 4.15 | 0.27 | 28 | 15.65 | <.001 | 2.51 |
| EMA day 2, current vs no stressor | 2.97 | 0.48 | 28 | 6.18 | <.001 | 0.99 |
| Wait list only: | ||||||
| Current vs no stressor, EMA day 2 vs EMA day 1 | 0.42 | 0.44 | 28 | 0.97 | .34 | 0.16 |
| EMA day 1, current vs no stressor | 3.39 | 0.24 | 28 | 14.32 | <.001 | 2.29 |
| EMA day 2, current vs no stressor | 3.81 | 0.37 | 28 | 10.34 | <.001 | 1.66 |
| Additional contrasts | ||||||
| Current stressor at EMA day 2, treatment vs wait list | −1.56 | 0.71 | 28 | −2.23 | .034 | 0.36 |
Negative Affect During Stressor Moments
The first hypothesis proposed that that NA on a 0–6 point Likert scale would be higher during current stressor moments relative to non-stressor moments within each treatment group and at each EMA day. For CBT participants on the first EMA day, NA was significantly higher by 4.15 points (representing 91.67% higher NA) during current stressor moments compared to non-stressor moments, and at the second EMA day, NA was significantly higher by 2.97 points (representing 76.44% higher NA) during current stressor moments compared to non-stressor moments (both p < .001). For participants randomized into the wait list group on the first EMA day, NA was significantly higher by 3.39 points (representing 71.00% higher NA) during current stressor moments compared to non-stressor moments, and on the second EMA day NA was also significantly higher by 3.81 points (representing 82.23% higher NA) during current stressor moments compared to non-stressor moments (both p < .001).
Treatment Effect on Negative Affect During Stressor Moments
The second hypothesis proposed that NA during stressors would be lower on EMA day 2 for the treatment but not wait list group. Negative affect was significantly lower by 1.6 points (18.88% lower NA) for those undergoing CBT treatment compared to those randomized into the wait list group (p = .034).
Treatment Effect on Negative Affect Reactivity During Stressor Moments
The third hypothesis proposed that NA reactivity to stressors would decrease at EMA day 2 relative to EMA day 1 for the treatment group. During current stressor moments compared to non-stressor moments, CBT participants had significantly lower NA by 1.18 points (representing 28.42% lower NA) at EMA day 2 compared to EMA day 1 (p = .04). In contrast, during current stressor moments compared to non-stressor moments, wait list participants showed a non-significant change of 0.42 points (12.45%) at EMA day 2 compared to EMA day 1 (p = .34). The difference in changes in NA from EMA day 1 to EMA day 2 between participants randomized to the CBT or wait list group is estimated by the 3-way interaction and its significance: the CBT treatment group had a 1.60-point greater decrease in reactivity compared to the wait list group (p =.03).
Differential Dropout Sensitivity Analysis
To assess potential bias of the results due to differential dropout between treatment groups, we re-analyzed the data using a conservative approach assuming the worst-case scenario for missingness (replacing CBT group participants missing EMA day 2 values with waitlist participants with complete data). We computed what the overall findings would be if participants from the CBT group with missing EMA day 2 data behaved similarly to participants in the wait list group who received no treatment but completed EMA day 2 measurements, i.e. we simulated that they had no effect of treatment at all. To re-analyze the data under this worst-case scenario, we used a technique similar to bootstrapping in which we randomly selected 18 waitlist participants with replacement who completed all observations to substitue 18 randomly selected CBT participants that were missing EMA day 2 observations. Sampling with replacement means that if a wait-list participant was selected to substitute the first CBT participant that was missing EMA day 2, the same wait-list participant could be again randomly selected to substitute the next CBT participant that was missing EMA day 2. All wait-list participants are always available to substitute each CBT participant. This way, the independence of substituted subjects can be guaranteed. Adding these 18 waitlist participants to the CBT group balanced the dropout rates in both groups to approximately 37%. We then conducted the primary analysis on this new dataset and did so 500 times, each time randomly selecting 18 waitlist participants with complete data.
Of the 500 simulations, the median p-value for the 3-way interaction between stressor, treatment group, and EMA day was 0.12 with an interquartile range (IQR) between .045 and .304. For 26% of the simulations, the p-value was below the 5% level and for 44% of the simulations the p-value was below the 10% level. This means that even when heavily biasing ourselves against finding a significant 3-way interaction by replacing 18 CBT participants with 18 waitlist participants, we still see at least a trend level of significance almost half of the time. This analysis suggests that the significant stressor*treatment group*EMA day interaction is not the result of differential treatment group dropout.
Discussion
In this randomized controlled trial of a CBT intervention participants high in trait anger and trait hostility that significantly decreased trait anger, NA measured in daily life was significantly higher during moments when participants reported current stressors, relative to moments with no stressors. Additionally, 12 weeks of CBT treatment compared to the wait list condition was associated with significantly lower NA when current stressors were reported as well as significantly lower NA stress reactivity. Other EMA studies have found similar positive associations between daily stress and NA in non-clinical populations (Mroczek & Almeida, 2004; Sliwinski et al., 2009; Stawski, Sliwinski, Almeida, & Smyth, 2008). However, these field observations are unique because in addition to providing observations of NA reactivity to stressors in a clinical population at higher risk for negative health outcomes (Pimple et al., 2015; Smith & MacKenzie, 2006), the current analyses also evaluate the effects of a treatment to decrease the trait-like clinical presentation of one specific negative emotion, anger, on momentary NA stress reactivity.
To explore why a treatment to reduce chronic anger, but not to improve stress management per se, could nonetheless be associated with lower NA during stressors, it is useful to revisit cognitive models of each of the two constructs: stress reactivity and trait anger. The transactional stress appraisal model (Folkman, Lazarus, Dunkel-Schetter, DeLongis, & Gruen, 1986) theorizes stress reactivity as a two-step process in which an individual first makes a primary cognitive appraisal of the extent to which an internal or external agent threatens his or her wellbeing, followed by a secondary appraisal of available coping resources (Folkman et al., 1986). For individuals with high levels of chronic anger, primary appraisals are biased towards hostile interpretations of situational input such that difficult interactions with other people and daily hassles are immediately appraised as personally targeting the individual (Wilkowski and Robinson (2010). Examples of primary appraisals of daily challenges from participants in the current study included that others were: “deliberately trying to get on my nerves,” “out to get me,” and “ignoring me on purpose.”
The cognitive model of anger and reactive aggression further elucidates our understanding of what may happen during secondary appraisal for an individual high in trait anger (Wilkowski & Robinson, 2010). Once a provocation is encountered, the ruminative attention style characteristic of chronic anger prolongs cognitive contact with the incident through repetitive thoughts, often leading to an amplification of emotional intensity and greater duration of emotional response (Wilkowski & Robinson, 2007). From this heightened level of emotional activation, it becomes more difficult for an individual to recruit the effortful control that would allow him or her to interrupt rumination and suppress reactive aggression tendencies in favor of more effective behavior choices (Wilkowski & Robinson, 2007).
The targets of cognitive behavioral anger-reduction treatment are thus two-fold: cognitive reframing strategies to generate more balanced primary interpretations of anger provocations, and the learning and rehearsal of new coping strategies participants can use when anger is triggered. Participants’ responses when asked to “indicate an alternative, more balanced interpretation of the …event that triggered an emotional reaction” suggest possible mechanisms by which CBT treatment could have contributed to lower NA reactivity. For example, the stressor of almost being hit by a cyclist was reframed from “he was trying to hit me” to “he’s just not paying attention.” Similarly, the appraisal that “this person is ignoring my email” was reframed as “this person might be on vacation and may not have received my email;” a less personalized explanation that is more likely to lead to problem solving behavior, such as re-sending the email or making a follow-up phone call.
In regard to secondary appraisal of coping choices, some behavioral examples of improved effortful control reported by participants included: “Went into another room to calm down”; “did some deep breathing”; “tried to put myself in her shoes”; “went on with my day”; and “spoke calmly instead of yelling.” The specific coping skills taught as part of the intervention (such as relaxation, communication skills, and problem solving) generally aid in the regulation of many states of NA in addition to anger (Gross, 2007) so it is possible that a skills-generalization effect across different kinds of NA may account for the current findings.
The current study had several limitations. While the strength of a randomized controlled trial design lies in its comparison condition, there are specific limitations introduced by the choice of a wait list control for the evaluation of psychotherapy interventions (Furukawa et al., 2014; Mohr et al., 2009). These limitations include possible inflation of intervention effect sizes if the intervention target worsens in the control group during the wait list period, and the possibility of increased dropout as well as lack of equivalence in reasons for dropout between the two conditions (Mohr et al., 2009). Participants assigned to wait list in this study were made aware that they would receive the treatment after 12 weeks, however it remains unknown what factors contributed to the high rate of attrition seen in both groups (and especially the intervention group). The present analyses have not uncovered any significant differences between baseline randomization group characteristics or those who completed the protocol compared to those who did not, and a conservative posthoc sensitivity analysis of differential dropout between the groups yielded a persistent effect of treatment on stressor reactivity. It remains possible that participants found the protocol too burdensome or experienced fluctuations in their motivation to change over the course of the intervention, though the intervention’s negative association with NA reactivity to stress is nonetheless clinically promising in this at-risk population. Taking these limitations into account, future studies of CBT for high trait anger should include an active, structured control activity (such as supportive psychotherapy) as well as consideration of the participant burden of completing both a 12-week course of CBT and two ambulatory monitoring appointments. Additionally, building task analysis questions (Greenberg, 2007) or measures of behavior into the EMA diary could shed additional light on how learning from therapy sessions may be translating into participants’ daily lives.
Generalizability of these results is limited to those with chronic anger who would self-select to enroll in outpatient treatment, indicating a certain level of readiness for change. Motivation to engage in treatment and effectiveness of the treatment techniques offered herein might differ for patients legally mandated to receive treatment, or individuals for whom physical aggression is an additional presenting concern. The current participants were all drawn from a single major metropolitan area, which may be skewed toward high daily experience of current stress moments. Assessing a more specific description of stressors (for example, the Daily Inventory of Stressful Events (Almeida, Wethington, & Kessler, 2002) could offer insight into whether associations of NA with stress vary depending on stressor type.
As Folkman emphasizes in the transactional model (Folkman et al., 1986), exposure to stress agents and availability of coping resources are subject to moment-to-moment fluctuations and highly informed by one’s environmental and interpersonal context, and lend themselves to momentary assessment methods. Though stress exposure cannot always be controlled, CBT, in its aim to help patients build available coping skills for stress challenge moments, may offer a unique clinical contribution to lowering NA reactivity and its associated risk.
Public Health Significance.
Chronic anger and negative reactions to stress can increase health risks. This study suggests that a commonly-used psychotherapy treatment to help decrease persistent feelings of anger is also associated with lower negative feelings (including irritation, anxiety, and sadness) when a person encounters a stressful event in their daily life.
Acknowledgments
This study was supported by Grant R01 HL63872 from the National Heart, Lung, and Blood Institute (R.P.S.), Grant K02 MH01491 from the National Institute of Mental Health (R.P.S.), and by the Nathaniel Wharton Fund.
References:
- Almeida DM, Wethington E, & Kessler RC (2002). The daily inventory of stressful events: an interview-based approach for measuring daily stressors. Assessment, 9(1), 41–55. doi: 10.1177/1073191102091006 [DOI] [PubMed] [Google Scholar]
- Almeida DM Midlife in the United States (MIDUS 1) National Study of Daily Experiences (NSDE), 1996-1997. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2017-11-17 10.3886/ICPSR03725.v5 [DOI] [Google Scholar]
- Barazzone N, & Davey GC (2009). Anger potentiates the reporting of threatening interpretations: An experimental study. Journal of anxiety disorders, 23(4), 489–495. doi: 10.1016/j.janxdis.2008.10.007 [DOI] [PubMed] [Google Scholar]
- Bleil ME, Gianaros PJ, Jennings JR, Flory JD, & Manuck SB (2008). Trait negative affect: toward an integrated model of understanding psychological risk for impairment in cardiac autonomic function. Psychosomatic medicine, 70(3), 328–337. doi: 10.1097/PSY.0b013e31816baefa [DOI] [PubMed] [Google Scholar]
- Bolger N (1990). Coping as a personality process: A prospective study. Journal of personality and social psychology, 59(3), 525–537. doi: 10.1037/0022-3514.59.3.525 [DOI] [PubMed] [Google Scholar]
- Bolger N, & Schilling EA (1991). Personality and the problems of everyday life: The role of neuroticism in exposure and reactivity to daily stressors. Journal of personality, 59(3), 355–386. doi: 10.1111/j.1467-6494.1991.tb00253.x [DOI] [PubMed] [Google Scholar]
- Bolger N, & Zuckerman A (1995). A framework for studying personality in the stress process. Journal of personality and social psychology, 69(5), 890–902. doi: 10.1037//0022-3514.69.5.890 [DOI] [PubMed] [Google Scholar]
- Charles ST, Piazza JR, Mogle J, Sliwinski MJ, & Almeida DM (2013). The wear and tear of daily stressors on mental health. Psychological science, 24(5), 733–741. doi: 10.1177/0956797612462222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chida Y, & Steptoe A (2009). The association of anger and hostility with future coronary heart disease: a meta-analytic review of prospective evidence. Journal of the American College of Cardiology, 53(11), 936–946. doi: 10.1016/j.jacc.2008.11.044 [DOI] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical Power Analysis for the Behavioral Sciences (2nd Edition ed.). Hillsdale: Lawrence Erlbaum. [Google Scholar]
- Cook WW, & Medley DM (1954). Proposed hostility and pharisiac-virtue scales for the MMPI. Journal of applied psychology, 38, 414–418. doi: 10.1037/h0060667 [DOI] [Google Scholar]
- Crawford JR, & Henry JD (2004). The positive and negative affect schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. The British journal of clinical psychology / the British Psychological Society, 43(Pt 3), 245–265. doi: 10.1348/0144665031752934 [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, & Trull TJ (2009). Ecological momentary assessment of mood disorders and mood dysregulation. Psychological assessment, 21(4), 463–475. doi: 10.1037/a0017075 [DOI] [PubMed] [Google Scholar]
- Edmondson D, Shaffer JA, Chaplin WF, Burg MM, Stone AA & Schwartz JE (2013). Trait anxiety and trait anger measured by ecological momentary assessment and their correspondence with traditional trait questionnaires. Journal of research in personality, 47, 843–852. doi: 10.1016/j.jrp.2013.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enkelmann HC, Bishop GD, Tong EM, Diong SM, Why YP, Khader M, & Ang J (2005). The relationship of hostility, negative affect and ethnicity to cardiovascular responses: an ambulatory study in Singapore. International journal of psychophysiology: official journal of the International Organization of Psychophysiology, 56(2), 185–197. doi: 10.1016/j.ijpsycho.2004.12.003 [DOI] [PubMed] [Google Scholar]
- Everson-Rose SA, Roetker NS, Lutsey PL, Kershaw KN, Longstreth WT, Sacco RL,… Alonso, A. (2014). Chronic Stress, Depressive Symptoms, Anger, Hostility, and Risk of Stroke and Transient Ischemic Attack in the Multi-Ethnic Study of Atherosclerosis. Stroke, 45(8), 2318–2323. doi: 10.1161/Strokeaha.114.004815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez E, Malvaso C, Day A, & Guharajan D (2018). 21st Century Cognitive Behavioural Therapy for Anger: A Systematic Review of Research Design, Methodology and Outcome. Behav Cogn Psychother, 1–20. doi: 10.1017/S1352465818000048 [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, & Gruen RJ (1986). Dynamics of a stressful encounter: cognitive appraisal, coping, and encounter outcomes. Journal of personality and social psychology, 50(5), 992–1003. doi: 10.1037/0022-3514.50.5.992 [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Noma H, Caldwell DM, Honyashiki M, Shinohara K, Imai H,… Noma HO (2014). Waiting list may be a nocebo condition in psychotherapy trials: A contribution from network meta-analysis. Acta Psychiatrica Scandinavica, 130(3), pp. 181–92. doi: 10.1111/acps.12275 [DOI] [PubMed] [Google Scholar]
- Gardner FL, & Moore ZE (2008). Understanding clinical anger and violence: The anger avoidance model. Behavior modification, 32(6), 897–912. doi: 10.1177/0145445508319282 [DOI] [PubMed] [Google Scholar]
- Gorenstein EE, Tager FA, Shapiro PA, Monk C, & Sloan RP (2007). Cognitive-behavior therapy for reduction of persistent anger. Cognitive and behavioral practice, 14(2), 168–184. doi: 10.1016/j.cbpra.2006.07.004 [DOI] [Google Scholar]
- Greenberg LS, (2007). A guide to conducting a task analysis of psychotherapeutic change. Psychotherapy Research, 17(1), 15–30. doi: 10.1080/10503300600720390 [DOI] [Google Scholar]
- Gross JJ, Thompson RA. (2007). Emotion Regulation: Conceptual Foundations (Gross JJ Ed.). New York: Guilford Press. [Google Scholar]
- Kamarck TW, Everson SA, Kaplan GA, Manuck SB, Jennings JR, Salonen R, & Salonen JT (1997). Exaggerated blood pressure responses during mental stress are associated with enhanced carotid atherosclerosis in middle-aged Finnish men: findings from the Kuopio Ischemic Heart Disease Study. Circulation, 96(11), 3842–3848. doi: 10.1161/01.CIR.96.11.3842 [DOI] [PubMed] [Google Scholar]
- Kamarck TW, Schwartz JE, Shiffman S, Muldoon MF, Sutton-Tyrrell K, & Janicki DL (2005). Psychosocial stress and cardiovascular risk: What is the role of daily experience? Journal of personality, 73(6), 1749–1774. doi: 10.1111/j.0022-3506.2005.00365.x [DOI] [PubMed] [Google Scholar]
- Kucharska-Newton AM, Williams JE, Chang PP, Stearns SC, Sueta CA, Blecker SB, & Mosley TH (2014). Anger Proneness, Gender, and the Risk of Heart Failure. Journal of Cardiac Failure, 20(12), 1020–1026. doi: 10.1016/j.cardfail.2014.09.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus RS (1993). From psychological stress to the emotions: a history of changing outlooks. Annual review of psychology, 44, 1–21. doi: 10.1146/annurev.ps.44.020193.000245 [DOI] [PubMed] [Google Scholar]
- Lee AH, & DiGiuseppe R (2018). Anger and aggression treatments: a review of meta-analyses. Curr Opin Psychol, 19, 65–74. doi: 10.1016/j.copsyc.2017.04.004 [DOI] [PubMed] [Google Scholar]
- Little RJA, & Rubin DB (2002). Statistical analysis with missing data (2nd ed.). New York, NY: John Wiley & Sons. [Google Scholar]
- Marsland AL, Walsh C, Lockwood K, & John-Henderson NA (2017). The effects of acute psychological stress on circulating and stimulated inflammatory markers: A systematic review and meta-analysis. Brain, behavior, and immunity, 64, 208–219. doi: 10.1016/j.bbi.2017.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merz EL, Malcarne VL, Roesch SC, Ko CM, Emerson M, Roma VG, & Sadler GR (2013). Psychometric properties of Positive and Negative Affect Schedule (PANAS) original and short forms in an African American community sample. Journal of affective disorders, 151(3), 942–949. doi: 10.1016/j.jad.2013.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Spring B, Freedland KE, Beckner V, Arean P, Hollon SD,… Kaplan R (2009). The selection and design of control conditions for randomized controlled trials of psychological interventions. Psychother Psychosom, 78(5), 275–284. doi: 10.1159/000228248 [DOI] [PubMed] [Google Scholar]
- Montpetit MA, Bergeman CS, Deboeck PR, Tiberio SS, & Boker SM (2010). Resilience-as-process: negative affect, stress, and coupled dynamical systems. Psychology and aging, 25(3), 631–640. doi: 10.1037/a0019268 [DOI] [PubMed] [Google Scholar]
- Mroczek DK, & Almeida DM (2004). The Effect of Daily Stress, Personality, and Age on Daily Negative Affect. Journal of personality, 72(2), pp. 55-378. doi: 10.1111/j.0022-3506.2004.00265.x15016068 [DOI] [PubMed] [Google Scholar]
- Mroczek DK, Stawski RS, Turiano NA, Chan W, Almeida DM, Neupert SD, & Spiro A 3rd. (2013). Emotional reactivity and mortality: longitudinal findings from the VA Normative Aging Study. J Gerontol B Psychol Sci Soc Sci, 70(3), 398–406. doi: 10.1093/geronb/gbt107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen JM (2011). Transdiagnostic cognitive processes in high trait anger. Clinical psychology review, 31(2), 193–202. doi: 10.1016/j.cpr.2010.10.003 [DOI] [PubMed] [Google Scholar]
- Peeters F, Nicolson NA, Berkhof J, Delespaul P, & deVries M (2003). Effects of daily events on mood states in major depressive disorder. Journal of abnormal psychology, 112(2), 203–211. [DOI] [PubMed] [Google Scholar]
- Piazza JR, Charles ST, Sliwinski MJ, Mogle J, & Almeida DM (2013). Affective reactivity to daily stressors and long-term risk of reporting a chronic physical health condition. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine, 45(1), 110–120. doi: 10.1007/s12160-012-9423-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pimple P, Shah A, Rooks C, Bremner JD, Nye J, Ibeanu I,… Vaccarino, V. (2015). Association between anger and mental stress-induced myocardial ischemia. American heart journal, 169(1), 115-+. doi: 10.1016/j.ahj.2014.07.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, & Edmondson D (2012). Meta-analysis of perceived stress and its association with incident coronary heart disease. The American journal of cardiology, 110(12), 1711–1716. doi: 10.1016/j.amjcard.2012.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, …INTERHEART investigators (2004). Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet, 364(9438), 953–962. doi: 10.1016/S0140-6736(04)17019-0 [DOI] [PubMed] [Google Scholar]
- Schilling OK, & Diehl M (2014). Reactivity to stressor pile-up in adulthood: effects on daily negative and positive affect. Psychology and aging, 29(1), 72–83. doi: 10.1037/a0035500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sin NL, Graham-Engeland JE, Ong AD, & Almeida DM (2015). Affective reactivity to daily stressors is associated with elevated inflammation. Health psychology, 34(12), pp. 1154–65. doi: 10.1037/hea000024026030309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliwinski MJ, Almeida DM, Smyth J, & Stawski RS (2009). Intraindividual change and variability in daily stress processes: findings from two measurement-burst diary studies. Psychology and aging, 24(4), 828–840. doi: 10.1037/a0017925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan RP, Shapiro PA, Gorenstein EE, Tager FA, Monk CE, McKinley PS, … Bigger JT Jr. (2010). Cardiac autonomic control and treatment of hostility: A randomized controlled trial. Psychosomatic medicine, 72(1), 1–8. doi: 10.1097/PSY.0b013e3181c8a529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TW, Glazer K, Ruiz JM, & Gallo LC (2004). Hostility, anger, aggressiveness, and coronary heart disease: An interpersonal perspective on personality, emotion, and health. Journal of personality, 72(6), 1217–1270. doi: 10.1111/j.1467-6494.2004.00296.x [DOI] [PubMed] [Google Scholar]
- Smith TW, & MacKenzie J (2006). Personality and risk of physical illness. Annual review of clinical psychology, 2, 435–467. doi: 10.1146/annurev.clinpsy.2.022305.095257 [DOI] [PubMed] [Google Scholar]
- Spielberger CD (1988). State-trait anger expression inventory: Professional manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Stawski RS, Sliwinski MJ, Almeida DM, & Smyth JM (2008). Reported exposure and emotional reactivity to daily stressors: the roles of adult age and global perceived stress. Psychology and aging, 23(1), 52–61. doi: 10.1037/0882-7974.23.1.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, & Kivimaki M (2013). Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health, 34, 337–354. doi: 10.1146/annurev-publhealth-031912-114452 [DOI] [PubMed] [Google Scholar]
- Sumner JA, Khodneva Y, Muntner P, Redmond N, Lewis MW, Davidson KW, … Safford MM (2016). Effects of Concurrent Depressive Symptoms and Perceived Stress on Cardiovascular Risk in Low- and High-Income Participants: Findings From the Reasons for Geographical and Racial Differences in Stroke (REGARDS) Study. J Am Heart Assoc, 5(10). doi: 10.1161/JAHA.116.003930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tafrate RC, Kassinove H, & Dundin L (2002). Anger episodes in high- and low-trait-anger community adults. Journal of clinical psychology, 58(12), 1573–1590. doi: 10.1002/jclp.10076 [DOI] [PubMed] [Google Scholar]
- Tennen H, Affleck G, & Armeli S (2005). Personality and daily experience revisited. Journal of personality, 73(6), 1465–1483. doi: 10.1111/j.1467-6494.2005.00355.x [DOI] [PubMed] [Google Scholar]
- Thalheimer W, & Cook S (2002). How to calculate effect sizes from published research articles: A simplified methodology. www.work-learning.com/effect_sizes.htm
- Vella EJ, Kamarck TW, Flory JD, & Manuck S (2012). Hostile mood and social strain during daily life: A test of the transactional model. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine, 44, 341–352. doi: 10.1007/s12160-012-9400-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of personality and social psychology, 54(6), 1063–1070. [DOI] [PubMed] [Google Scholar]
- Wilkowski BM, & Robinson MD (2007). Keeping one’s cool: trait anger, hostile thoughts, and the recruitment of limited capacity control. Personality & social psychology bulletin, 33(9), 1201–1213. doi: 10.1177/0146167207301031 [DOI] [PubMed] [Google Scholar]
- Wilkowski BM, & Robinson MD (2010). The anatomy of anger: an integrative cognitive model of trait anger and reactive aggression. Journal of personality, 78(1), 9–38. doi: 10.1111/j.1467-6494.2009.00607.x [DOI] [PubMed] [Google Scholar]
- Williams JE, Nieto FJ, Sanford CP, & Tyroler HA (2001). Effects of an angry temperament on coronary heart disease risk: The Atherosclerosis Risk in Communities Study. American journal of epidemiology, 154(3), 230–235. doi: 10.1093/aje/154.3.230 [DOI] [PubMed] [Google Scholar]