Abstract
Facial contouring is a complex procedure performed to alter tissue contents and restore facial appearance. However, it is difficult to measure the amount of the tissue volume that is needed. This study demonstrated the use of preoperative computer simulation (PCS) and 3-dimensional (3D) printing in contouring procedure to maximize outcomes.
Three-dimensional surface imaging (3DSI) or computed tomography imaging (CTI) data were reconstructed into a 3D model by Mimics software. PCS was performed by simulating the changes in bone and soft tissue. The stimulating volume change was calculated by Boolean operations. Finally, the virtual model was exported into 3D printer to produce physical templates to guide surgical plan. PCS and actual postoperative results were compared using objective rating scales and by cephalometrical measurements.
With the direct guidance of PCS and 3D templates, contouring procedure was performed accurately. Satisfactory facial contouring was achieved with less operative time. As the plastic surgery panel rated, 45.8% of the 3DSI results and 41.7% of the CTI results were identical with the actual outcome, and 0% of them was poor. There were no significant differences in patient satisfaction between the PCS of 3DSI and CTI.
Preoperative computer simulation is an accurate method for designing contour adjustment plans, and can be an efficient and reliable predictor of outcomes with customized templates.
Keywords: 3-dimensional printing, contouring adjustment, preoperative computer simulation
1. Introduction
Facial appearance plays an important role in an individual's quality of life. Both bones and facial soft tissues are involved in patients with craniomaxillofacial deformities. Over time, individuals become sensitive to changes in their facial appearance.[1] Plastic surgery for facial correction requires meticulous and accurate presurgical, surgical, and postsurgical planning, because even very subtle alterations in facial proportions can strongly affect appearance.[2] However, it is technically difficult to measure and determine the extent and depth of potential surgical changes. Because of a lack of objective measurements, surgeons have had to estimate the magnitude of change by personal experience.[3] This may contribute to discrepancies between clinical outcomes and patient expectations. Therefore, careful planning of surgery and methods to reliably predict facial changes are very important in maximizing surgical outcomes that conform to patient expectations.
The digital imaging technology is widely used to assist disease diagnosis and guide treatment.[4–7] Recently, preoperative computer simulation (PCS) and 3-dimensional (3D) models have been applied to the surgical adjustment of craniomaxillofacial defects.[8] Maxillofacial soft tissue prediction systems have been reported relevant and suitable for fast and accurate prediction of postoperative facial outcomes in daily clinical practice.[9] In addition, the application of reduction templates produced by 3D printers during contouring procedures has been found to improve the efficiency and accuracy of surgery and to maximize outcomes.[10] To obtain an ideal expected effect conforming to patient expectations, and also to improve surgical accuracy and efficiency, we integrated PCS and 3D printing for contouring correction during plastic surgery (Fig. 1).
Figure 1.
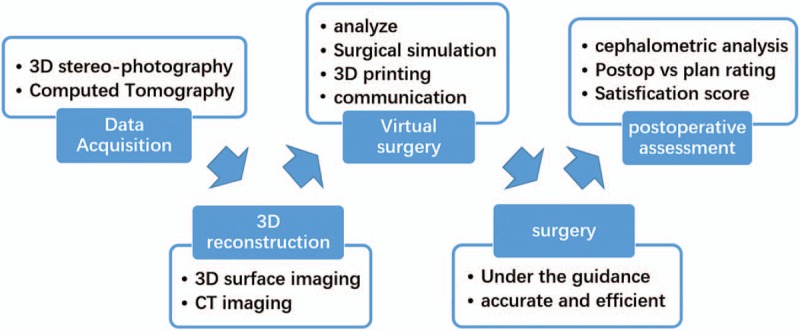
Study flowchart.
2. Materials and methods
2.1. Patients
This study enrolled 36 patients with facial defects or imperfections who underwent contouring procedures aided by customized templates based on PCS between July, 2015 and September, 2016. These patients (24 females and 12 males) had a mean age of 22.9 years (range 18–29 years). This research was approved by the Ethical Review Board in Nanfang Hospital, Guangzhou, China.
2.2. Preoperative computer simulation
2.2.1. Method A: 3D surface imaging
Patients desiring improvements in a flatter nose or shorter chin underwent stereo-photography by 3D surface imaging (3DSI) before and after surgery. Data were processed by VETRA M3 3D capture software (Allergan, New York, NY) to reconstruct a 3D model. Subsequently, a 3D model was printed as the customized template to aid in actual surgery.
2.2.2. Method B: computed tomography imaging
Patients desiring improvements in zygoma or mandibular reduction, underwent spiral computed tomography (CT) scans at 1.0 mm slice thickness before and after surgery. The CT data were exported to Mimics software (Materialise, Brussels, Belgium), and axial images were used to construct a 3D model. In PCS, a soft tissue simulation was run based on simulated skeletal movements using a finite element modeling (FEM) soft tissue simulation algorithm. A 3D-printed customized template based on bone tissue simulation was used to direct the surgical process.
2.3. Outcome assessments
Surgical outcomes were assessed by 3 independent professional plastic surgeons. The difference between preoperative simulations and actual postoperative results was assessed by consensus of the 3 panelists on a scale of 1 to 4, where 1 = identical, 2 = similar, 3 = approximate, and 4 = poor. Patient satisfaction was assessed by a survey conducted at the 6-month follow-up visit, during which an independent surgeon questioned patients regarding overall satisfaction with outcomes. Patients rated their satisfaction on a scale of 1 (dissatisfaction) to 4 (satisfaction).[11]
2.4. Cephalometric analysis
Differences between preoperative simulations and actual postoperative results were assessed using anatomical landmarks in the 3D model, using cephalometric radiography, as previously described.[12,13] This tool has been used for rapid measurements of selected anatomical parts of the face.[14,15] Both the 3DSI and computed tomography imaging (CTI) data were transferred to a corresponding standard reference frame, which included 8 soft tissue landmarks (the nasion, nasal tip, pogonion, and menton in the 3DSI, and the 2 zygomatic arches and the 2 angles of the mandible in CTI) and 4 bony tissue landmarks (the 2 zygomatic arches and the 2 angles of the mandible) (Fig. 2 and Fig. 3).[16] The displacements of landmarks in the horizontal, vertical, and Euclidean directions between the PCS and the actual postoperative results were calculated to determine whether the actual postoperative results conformed to the simulations.[17]
Figure 2.
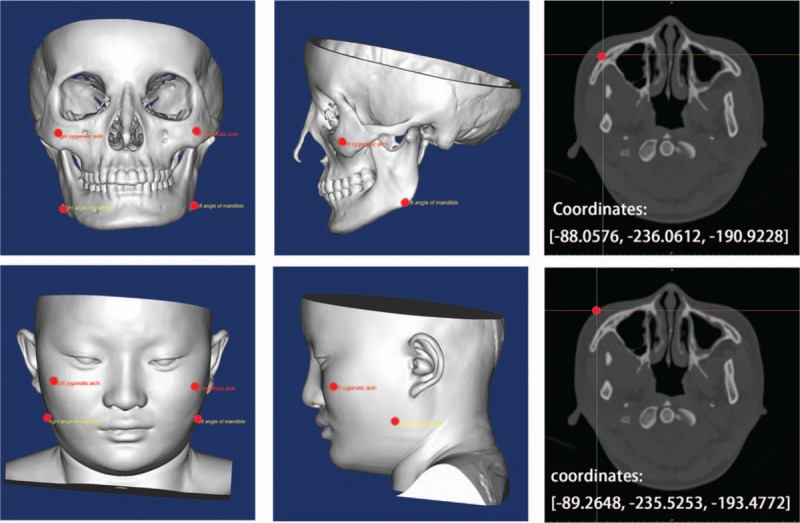
Anatomical landmarks of bone tissue in the 3-dimensional (3D) model. The anatomical landmarks in bone tissue (upper panel). The anatomical landmarks in soft tissue. The landmarks include the zygomatic arches and the angles of the mandible (lower panel).
Figure 3.
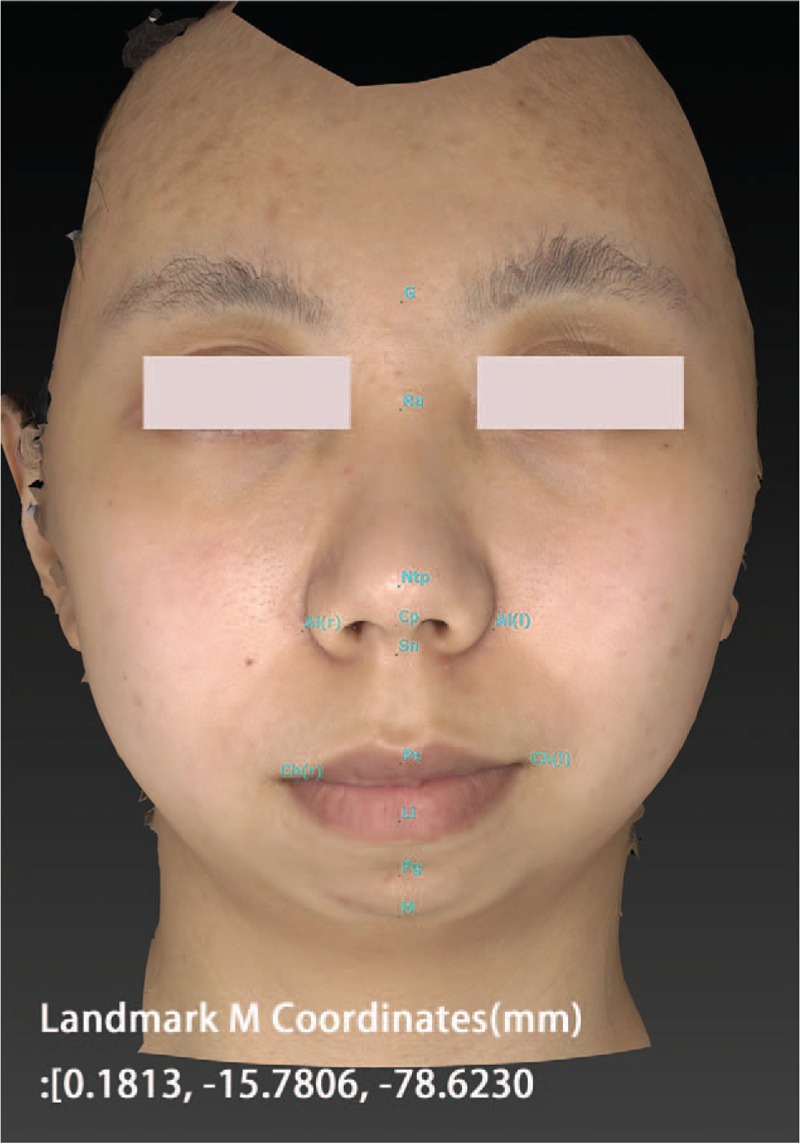
Anatomical landmarks in the 3-dimensional (3D) surface model. The green dots show the anatomical landmark in the side facial contour, including the root of the nose, the nasal tip, and the pogonion. The landmark M represents the menton.
2.5. Statistical analysis
All statistical analyses were performed using the Statistical Package for the Social Sciences, version 19.0 (SPSS, IBM Company, Chicago, IL). Differences in patient satisfaction were compared between the PCS of the 3DSI and CTI groups by Fisher exact tests and t tests. Statistical significance was defined as P < .05.
2.6. Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
3. Results
The 36 patients included 32 women and 4 men of mean age 27.9 years (range 18–39 years). Twenty-four patients underwent rhinoplasty or mentoplasty to improve their lateral facial contours. The other 12 patients underwent zygomatic or mandibular reduction to adjust their front facial contours. The mean follow-up period was 7.2 months (range 4–18 months).
The panel of 3 professional plastic surgeons rated PCS images of 3DSI versus outcomes as identical for 11 patients (45.8%), similar for 10 (41.7%), approximate for 3 (12.5%), and poor for none (0%). The same panel rated PCS images of CTI versus outcomes as identical for 5 patients (41.7%), similar for 4 (33.3%), approximate for 3 (16.6%), and poor for none (0%) (Table 1).
Table 1.
Accuracy ratings and patient satisfaction scores for PCS of the 3DSI and CTI groups.

On a scale of 1 to 4, the mean (±SD) patient satisfaction score was 3.17 ± 0.72 for the PCS of 3DSI and 3.13 ± 0.95 for the PCS of CTI. There was no significant difference between the 2 groups (P > .05) (Table 1).
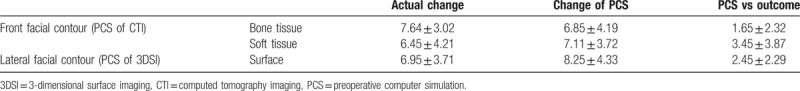
Cephalometric analysis showed that the actual contour change in bone tissue after zygomatic or mandibular reduction was 7.64 ± 3.02 mm. The difference between CTI result and actual bone tissue change is 1.65 ± 2.32 mm. The actual change in soft tissue contour was 6.45 ± 4.21 mm. The difference between CTI result and actual soft tissue change is 3.45 ± 3.87 mm. The contour of the nose and chin had an actual change of 6.95 ± 3.71 mm, and the difference between 3DSI result and actual soft tissue change is 2.45 ± 2.29 mm (Table 2).
Table 2.
Cephalometric analysis.
4. Case report
4.1. Case 1: nasal adjustment
4.1.1. Data acquisition and analysis
A 33-year-old patient with a flat nose was photographed using the 3D capture system. Her stereoscopic images were transferred to a 3D model (Fig. 4, left). Clinical and 3D analysis indicated a flat nasal dorsum, sharp nasofrontal angle, and wide and obtuse nasal tip. The goals of surgery were to raise the nasal dorsum and reshape the nasal tip to improve her appearance.
Figure 4.
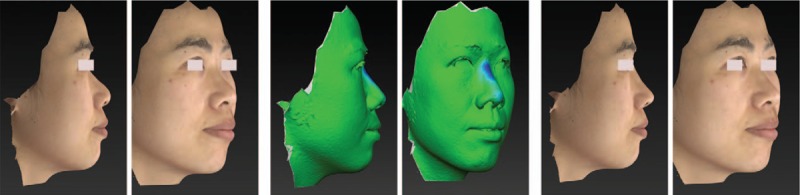
Nasal adjustment with PCS. Preoperative image (left), PCS model (middle), and image obtained 90 days after surgery (right). PCS = preoperative computer simulation.
4.1.2. PCS and the customized template
The change in nasal dorsum was simulated by Boolean operations between PCS and preoperative measurements to determine the size and shape of the customized template (Fig. 4, middle), and it was printed by rapid prototyping. During surgery, the surgeon sculpted the silicone implant according to the customized template.
4.1.3. Postoperative outcomes
Three months after surgery, improvements in the nasal dorsum, nasofrontal angle, and nasal tip were shown. These changes contributed to a better appearance, which met the patient's expectations (Fig. 4, right).
4.2. Case 2: mandibular adjustment
4.2.1. Data acquisition and analysis
A 22-year-old female patient with serious mandibular distraction was photographed using the 3D capture system, and her stereoscopic images were transferred to a 3D model (Fig. 5, left). Clinical and 3D analyses showed severe retrognathia. The goals of surgery were to insert implants to advance and lengthen the chin in the coronal and vertical directions.
Figure 5.
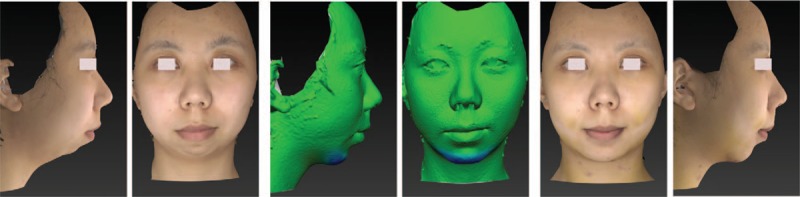
Mandibular adjustment with PCS. Preoperative image (left), PCS model (middle), and image obtained 90 days after surgery (right). PCS = preoperative computer simulation.
4.2.2. PCS and the customized template
Changes in the chin were stimulated preoperatively by Boolean operations to determine the size and shape of the customized template (Fig. 5, middle). Based on the PCS, a customized template was printed by rapid prototyping. During surgery, the surgeon sculpted the implant according to the customized template to obtain an expected size and shape.
4.2.3. Postoperative outcomes
Ninety days after surgery, an increase in mandibular length and an advance in mandibular position were observed (Fig. 5, right).
4.3. Case 3: craniomaxillofacial adjustment data acquisition and analysis
A 22-year-old woman with a square face underwent CT, with the data transferred to a 3D model. Clinical and 3D analyses both showed that the zygoma and mandibular angle were prominent. The goals were to achieve an oval face and smooth contour by reducing the prominence of the zygoma and mandibular angle (Fig. 6).
Figure 6.
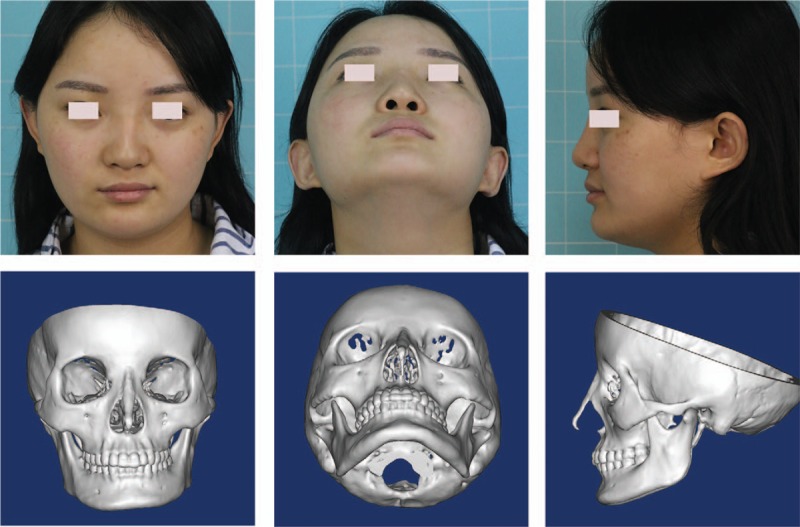
Craniomaxillofacial adjustment. The preoperative image (left) and 3D model based on CT data (right). 3D = 3-dimensional, CT = computed tomography.
4.3.1. PCS and the customized template
Soft tissue simulation was performed based on simulated skeletal movements using a FEM soft tissue simulation algorithm (Fig. 7). Based on the simulation, a customized template was designed and printed (Fig. 8). During surgery, as guided by the PCS and customized template, the surgeon cut and ground certain parts of the mandible to obtain the expected shape.
Figure 7.
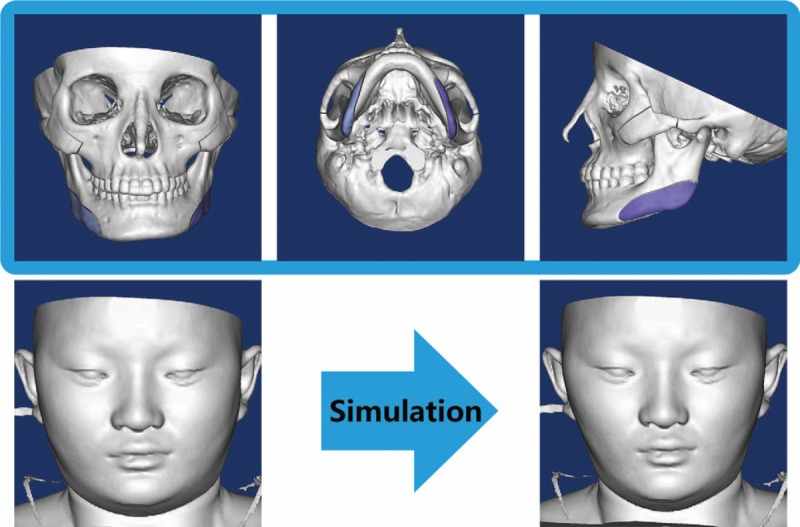
A PCS based on a 3D model of bone tissue. 3D = 3-dimensional, PCS = preoperative computer simulation.
Figure 8.
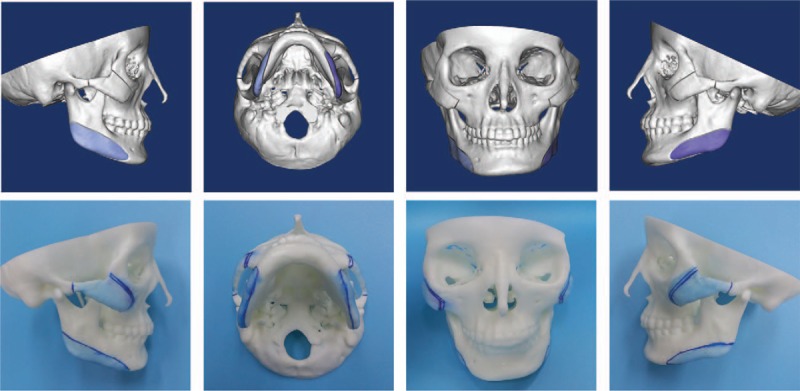
A 3D printed model used to direct the surgical process. 3D = 3-dimensional.
4.3.2. Postoperative outcomes
Compared with preoperative appearance (Fig. 9, upper), postoperative result showed that the prominent zygoma and mandible were reduced to obtain a smoother contour, with an oval-shaped face evident after surgery (Fig. 9, lower).
Figure 9.

Images obtained preoperatively (left) and 90 days after surgery (right).
5. Discussion
The success of plastic and reconstructive surgery depends not only on the surgical techniques, but also on the accuracy and effectiveness of the surgical plan. The method described in the current study may yield satisfactory surgical plans. Objective assessments by a panel of professional plastic surgeons, cephalometric analysis, and patient satisfaction all indicated that PCS has great potential to predict postoperative facial contour. Moreover, the use of 3D printed customized template can help guide the surgery toward a satisfying outcome. Patient satisfaction with the PCS obtained by 3DSI was similar to that obtained by the CTI system, suggesting that these 2 systems are both effective in surgical planning of facial contouring.
Traditional computer-aided maxillofacial planning systems are based on 2-dimensional (2D) lateral x-rays. These images, however, cannot thoroughly fully show surface details, are prone to landmark errors and overlap of structures, and do not allow complex 3D movements.[18] These limitations are effectively overcome by 3D imaging systems. Sectional images obtained from CTI were used in the construction of 3D models, with surgeons having no difficulties recognizing and assessing morphologic changes in bones and internal organs of most patients. Thus, the PCS of CT image-reconstructed 3D models was suitable for the planning of craniomaxillofacial surgery that mainly involved bone tissue adjustment. Surgery on soft tissue can be planned using 3DSI. Unlike CT, 3DSI uses triangulation, which overlays multiple images of the same object from different angles to form a 3D image.[19]
In this study, we performed plastic surgery procedures under the guidance of customized templates. Three-dimensional printing has proven extremely useful in the production of customized templates, such as jaw and nose prostheses. These customized templates ensure that the required components provide an exact fit and maximize an early return of function. These templates may also pave the way toward customized implants, reducing operation time and improving patient satisfaction. Moreover, 3D-printed customized template can provide surgeons with a thorough understanding of the surgical plan and the relevant anatomy. Although our studies demonstrated that PCS and 3D printing could provide surgeons with a more thorough understanding of the surgical plan and the anatomy of the surgical region, surgeon's skill in surgical planning and execution was still the primary determinant of surgical outcomes. Moreover, prolonged exposure of patients to radiation can be potentially harmful. Pregnant patients or children should avoid the radiation exposures.
6. Conclusions
Preoperative computer simulation is an accurate method for designing surgical plans for contour adjustment and may be an efficient and reliable predictor of favorable outcomes. Customized templates manufactured using the combination of PCS and 3D printing can provide surgeons with a more thorough understanding of the surgical plan and the anatomy of the surgical region. The customized template generally achieves satisfactory outcomes for patients, suggesting that surgeons should consider incorporating PCS into their preoperative consultations with patients who desire an aesthetic contour.
Author contributions
Conceptualization: Feng Lu, Rong Fu.
Formal analysis: Shih Yuan-Liang.
Investigation: Hui Zeng, Shih Yuan-Liang, Gan Xie.
Methodology: Gan Xie.
Software: Hui Zeng.
Writing – original draft: Hui Zeng.
Writing – review & editing: Hui Zeng, Rong Fu.
Footnotes
Abbreviations: 3D = 3-dimensional, 3DSI = 3-dimensional surface imaging, CTI = computed tomography imaging, PCS = preoperative computer simulation.
SY-L and ZH contribute equally and should be co-first authors.
FL and FR contribute equally and should be co-corresponding authors.
The authors report no conflicts of interest.
References
- [1].Pan B, Zhang G, Xia JJ. Prediction of soft tissue deformations after CMF surgery with incremental kernel ridge regression. Comput Biol Med 2016;75:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Lippincott Williams and Wilkins, Farkas LG. Anthropometry of the Head and Face. 2nd ed1994. [Google Scholar]
- [3].Murray DJ, Edwards G, Mainprize JG, et al. Advanced technology in the management of fibrous dysplasia. J Plast Reconstr Aesthet Surg 2008;8:906–16. [DOI] [PubMed] [Google Scholar]
- [4].Abdel Razek AA. Computed tomography and magnetic resonance imaging of maxillofacial lesions in renal osteodystrophy. J Craniofac Surg 2014;25:1354–7. [DOI] [PubMed] [Google Scholar]
- [5].Abdel Razek AA. Diagnostic role of magnetic resonance imaging in obstructive sleep apnea syndrome. J Comput Assist Tomogr 2015;39:565–71. [DOI] [PubMed] [Google Scholar]
- [6].Razek AA, Huang BY. Soft tissue tumors of the head and neck: imaging-based review of the WHO classification. Radiographics 2011;31:1923–54. [DOI] [PubMed] [Google Scholar]
- [7].Razek AAKA. MR imaging of neoplastic and non-neoplastic lesions of the brain and spine in neurofibromatosis type I. Neurol Sci 2018;39:821–7. [DOI] [PubMed] [Google Scholar]
- [8].Mollemans W1, Schutyser F, Nadjmi N. Predicting soft tissue deformations for a maxillofacial surgery planning system: from computational strategies to a complete clinical validation. Med Image Anal 2007;11:282–301. [DOI] [PubMed] [Google Scholar]
- [9].Mollemans W, Schutyser F, Van Cleynenbreugel J, et al. Tetrahedral mass spring model for fast soft tissue deformation. Lecture Notes Comput Sci 2003;IS4TM:145–54. [Google Scholar]
- [10].Wang R, Li G, Liu C. Three-dimensional printing of reduction template in the contouring of craniofacial fibrous dysplasia. J Craniofac Surg 2016. [DOI] [PubMed] [Google Scholar]
- [11].Marchetti C, Bianchi A, Muyldermans L. Validation of new soft tissue software in orthognathic surgery planning. Maxillofac Surg 2011;40:26–32. [DOI] [PubMed] [Google Scholar]
- [12].Broadbent BH. A new X-ray technique and its application in orthodontics. Angle Orthod 1931;1:45–60. [Google Scholar]
- [13].Athanasiou AE. Mosby-Wolfe, Orthodontic Cephalometry. London: 1995. [Google Scholar]
- [14].Geng J. Structured-light 3D surface imaging: a tutorial. Adv Opt Photonics 2011;3:128–60. [Google Scholar]
- [15].Arun KS, Huang TS, Blostein SD. Least-squares fitting of two 3-d point sets. IEEE Trans Pattern Anal Machine Intelligence 1987;9: [DOI] [PubMed] [Google Scholar]
- [16].Swennen GRJ, Schutyser F, Barth EL, et al. A new method of 3-D cephalometry part I: the anatomic cartesian 3-D reference system. J Craniofac Surg 2006;17:314e325. [DOI] [PubMed] [Google Scholar]
- [17].Chabanas M, Mare’caux C. Evaluating soft tissue simulation in maxillofacial surgery using preoperative and postoperative CT scans. In: Proceedings of CARS. 2004; 419–424. [Google Scholar]
- [18].Liebregts J, Xi T, Timmermans M. Accuracy of three-dimensional soft tissue simulation in bimaxillary osteotomies. J Craniomaxillofac Surg 2015;43:329–35. [DOI] [PubMed] [Google Scholar]
- [19].Yu MS, Jang YJ. Preoperative computer simulation for Asian rhinoplasty patients: analysis of accuracy and patient preference. Aesthet Surg J 2014;34:1162–71. [DOI] [PubMed] [Google Scholar]


