Abstract
Objectives
This study was aimed to establish the most effective premature ovarian failure (POF) mouse model using Cyclophosphamide (CTX), busulfan (Bu), and cisplatin considering treatment duration of anticancer drugs and natural recovery time.
Methods
POF was induced by intraperitoneally injecting CTX (120 mg/kg)/Bu (12 mg/kg) for 1 to 4 weeks or cisplatin (2 mg/kg) for 3 to 14 days to C57BL/6 female mice aged 6 to 8 weeks. Controls were injected with equal volume of saline for the same periods. Body weight was measured every week, and ovarian and uterine weights were measured after the last injection of anticancer drug. To assess ovarian function, POF-induced mice were superovulated with pregnant mare serum gonadotropin and human chorionic gonadotropin, and then mated with male. After 18 hours, zygotes were retrieved and cultured for 4 days. Finally, the mice were left untreated for a period of times after the final injection of anticancer drug, and the time for natural recovery of ovarian function was evaluated.
Results
After 2 weeks of CTX/Bu injection, ovarian and uterine weights, and ovarian function were decreased sharply. Cisplatin treatment for 10 days resulted in a significant decrease in ovarian and uterine weight, and ovarian function. When POF was induced for at least 2 weeks for CTX/Bu and for at least 10 days for cisplatin, ovarian function did not recover naturally for 2 weeks and 1 week, respectively.
Conclusions
These results suggest that CTX/Bu should be treated for at least 2 weeks and cisplatin for at least 10 days to establish the most effective primary ovarian insufficiency mouse model.
Keywords: Busulfan, Cisplatin, Cyclophosphamide, Mice, Primary ovarian insufficiency
Introduction
Premature ovarian failure (POF) is classically defined as 4 to 6 months of amenorrhea in women under the age of 40 years, who have elevated serum follicle stimulating hormone (FSH) levels (hypergonadotropic hypogonadism, usually over 40 IU/L) and low estradiol level (less than 50 pg/mL).1,2 Recently, POF also referred to as primary ovarian insufficiency (POI). This condition can be transient or progressive, and usually results in eventual premature menopause.3 POI can be taken to encompass occult, biochemical and overt states, whereas POF is best considered as only the final stage of POI.4,5 POF is characterized by loss of follicles, ovarian function, and estrogen production, and finally resulting in infertility.6,7 Its incidence is estimated to be as high as 1 in 100 by the age of 40, and 1 in 1,000 by the age of 30. Potential etiologies for POI are genetic, autoimmune, metabolic, infectious, and iatrogenic (ovarian surgery, radiotherapy, or chemotherapy) factors.3,8
Importantly, early ovarian failure is a cause of refractory infertility and management for POI should reflect a comprehensive approach. To date, many treatment methods have been applied and they include hormone replacement therapy,9 in vitro fertilization methods,10 and cell therapy using stem cells.11,12,13,14 However, effective treatments and drugs for POF treatment are very limited. Therefore, new strategies for improving treatment are absolutely required.15,16
In this respect, many studies have used POF animal models to identify molecular mechanisms of POF and to develop the therapeutic agents.17,18 Currently, POF animal models are being made using various anticancer drugs. Cyclophosphamide (CTX), busulfan (Bu), and cisplatin are representative anticancer drugs. However, the POF induction effect of these anticancer drugs varies widely depending on the treatment period and concentration. Especially, when POF is induced by an anticancer drug and then the anticancer drug is stopped, POF can be recovered naturally as time goes by. Most studies overlook this point. Therefore, this study is aimed to suggest the most effective POF mouse model using CTX, Bu, and cisplatin considering treatment duration of anticancer drugs and natural recovery time.
Materials and Methods
1. Experimental animals
All experimental mice were purchased from Hanasangsa (Busan, Korea) and housed in a temperature- and humidity-controlled animal facility under a 12-hours light-dark cycles with food and water available ad libitum. All experiments were performed in accordance with ‘the Guide for the Care and Use of Laboratory Animals’ of Pusan National University Hospital Institutional Animal Care and Use committee.
2. POF mouse model establishment
C57BL/6 female mice aged 6 to 8 weeks were treated with CTX/Bu or cisplatin for the induction of POF. In the CTX/Bu group, the mice were injected intraperitoneally with 120 mg/kg CTX (Sigma Aldrich, St. Louis, MO, USA) and 12 mg/kg Bu (Sigma Aldrich) for 1, 2, and 4 weeks. In the cisplatin group, the mice were administered 2 mg/kg cisplatin (Sigma Aldrich) for 3, 5, 10, and 14 days. Controls were injected with equal volume of saline for the same periods. CTX and cisplatin were prepared in saline, and Bu was dissolved in 100% dimethyl sulfoxide and then diluted in saline. The general condition and body weight of the mice were measured every week.
3. Weighting of ovary and uterus, and evaluation of ovarian function
After the last injection of each anticancer drug, some mice were sacrificed and dissected to determine the weight of the ovaries and uterus. On the other hand, in order to investigate changes in ovarian function, others were superovulated by intraperitoneal injection with 0.1 mL of 5 IU pregnant mare serum gonadotropin (PMSG; Sigma Aldrich) followed by injection of 5 IU of human chorionic gonadotropin (hCG; Sigma Aldrich) approximately 48 hours later. Then the superovulated mice were immediately paired with 6- to 8-week-old individual male.
Eighteen hours after hCG injection, female mice with a confirmed vaginal plug were killed by cervical dislocation, and cumulus-enclosed one-cell embryos (zygotes) were retrieved from the oviductal ampulae and denuded by incubation for 1 minute with 0.1% hyaluronidase (Sigma Aldrich) in PBS (Giboc BRL, Grand Island, NY, USA). Zygotes were pooled and washed 3 times in G-IVF-plus medium (Vitrolife, Göteborg, Sweden) with 10% serum substitute supplement (SSS; Irvine Scientific, Santa Ana, CA, USA). Healthy zygotes only were cultured in 20-µL drops of Gl-plus medium (Vitrolife) with 10% SSS for the first 2 days, and then G2-plus medium (Vitrolife) with 10% SSS for the latter 2 days under paraffin-oil at 37℃ in a 5% CO2 incubator, and the media were changed daily.
4. Confirmation of natural recovery of POF
To determine the duration of recovery of damaged ovarian function, mice were left untreated for a period of times after the final injection of CTX/Bu (n = 12) and Cisplatin 9 (n = 16). And then, the mice were superovualted and their ovarian functions were evaluated.
5. Statistical analysis
An SPSS program (Version 17.0; SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The number of zygotes retrieved and blastocyst formation rate were analyzed by one-way analysis of variance and λ2-test. Statistical analysis for comparison of body weight and ovarian and uterine weight was performed by Student t-test. A P value of < 0.05 was considered statistically significant.
Results
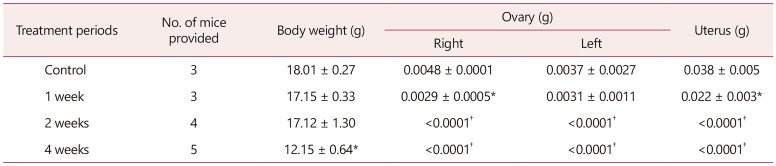
1. Changes in body weight, ovarian and uterine weight after CTX/Bu treatment
Whether the CTX/Bu treatment affects body weight, ovarian weight and uterine weight was examined according to the treatment period. As the treatment period increased, the weight of ovaries and uterus as well as body weight decreased significantly. In particular, after 2 weeks of treatment, the weight of ovaries and uterus decreased sharply (Table 1).
Table 1. Effects of cyclophosphamide/busulfan treatment on weights of body, ovaries, and uterus.
*P < 0.05, †P < 0.01 (versus control)
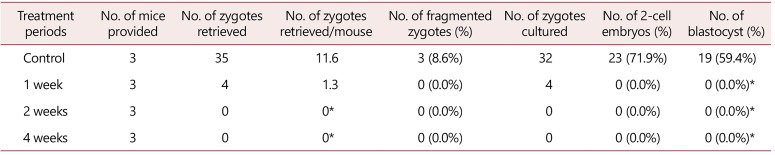
2. Changes in ovarian function after CTX/Bu treatment
To investigate whether CTX/Bu treatment affect ovarian function, the POF-induced mice were superovulated and mated with male. And then zygotes were retrieved and cultured for 4 days. The number and embryo development rate to blastocyst of zygotes were measured. Both the number of zygotes retrieved and embryo development rate were significantly decreased from 1 week of CTX/Bu treatment compared to the control. No zygotes were developed into blastocyst (Table 2). This result means that the CTX/Bu treatment reduced not only body weight and ovarian and uterine weight, but also ovarian function.
Table 2. Effects of cyclophosphamide/busulfan treatment on ovarian function.
*P < 0.01 (versus control)
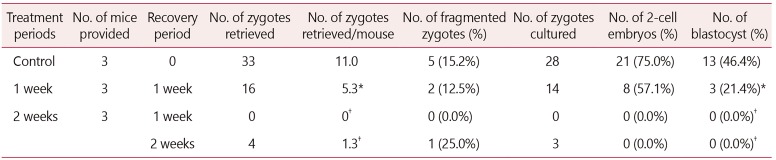
3. Natural recovery of ovarian failure after stopping CTX/Bu treatment
In order to investigate how long the ovarian function of POF-induced mice was recovered naturally after the last injection of CTX/Bu, the mice were left untreated for a period of times. And then ovarian function of the mice was evaluated as described earlier. When the mice were injected with CTX/Bu for one week and then were left untreated for one week, the average number of zygotes retrieved was 5.3, which was about half that of the control group (11.0), and the embryo development rate to blastocyst was also 21.4%, which was also half of that of the control group (46.4%). However, when CTX/Bu was injected for 2 weeks, ovarian function was not recovered at all after the recovery period of 2 weeks (Table 3). This result means that ovarian function is not naturally recovered for at least 2 weeks when POF is induced with CTX/Bu for 2 weeks.
Table 3. Natural recovery of ovarian failure after stopping cyclophosphamide/busulfan treatment.
*P < 0.05, †P < 0.01 (versus control)
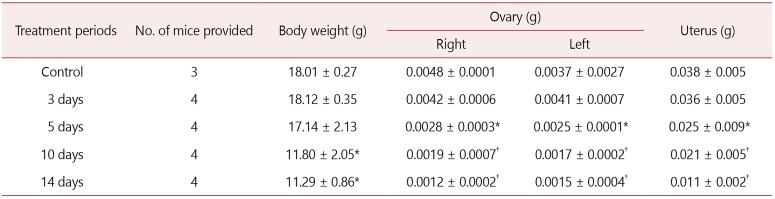
4. Changes in body weight, ovaries and uterine weight after cisplatin treatment
In other experiment, we examined the effect of cisplatin treatment for POF induction on body weight, ovarian and uterine weight according to the cisplatin treatment period. As the treatment period increased, the weight of ovaries and uterus as well as body weight decreased. In particular, from 10 days of cisplatin injection, the weight of ovaries and uterus decreased significantly (Table 4).
Table 4. Effects of cisplatin treatment on weights of body, ovaries, and uterus.
*P < 0.05, †P < 0.01 (versus control)
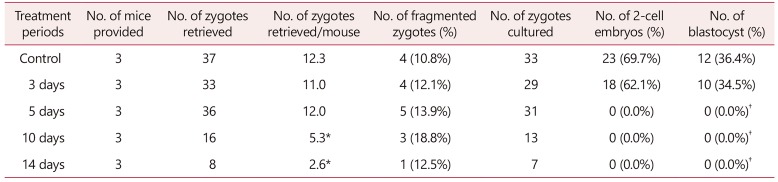
5. Changes in ovarian function after cisplatin treatment
To investigate whether cisplatin treatment practically decreases ovarian function, mice were superovulated and mated with male. And then, zygotes were retrieved from the superovulated mice and cultured for 4 days. Both the number of zygotes retrieved and embryo development to blastocyst gradually decreased with the treatment period compared to the control. The average number of zygotes retrieved and embryo development rate were 5.3 and 0% at 10 days of cisplatin treatment, and 2.6 and 0% at 14 days treatment, respectively, which were significantly decreased compared to the control (12.3 and 36.4%). No zygotes were developed into blastocyst from 5 days of cisplatin injection (Table 5). This result means that oocyte quality began to deteriorate from 5 days of cisplatin treatment, and ovarian function was sufficiently inhibited by treatment for 10 days or more.
Table 5. Effects of cisplatin treatment on ovarian function.
*P < 0.05, †P < 0.01 (versus control)
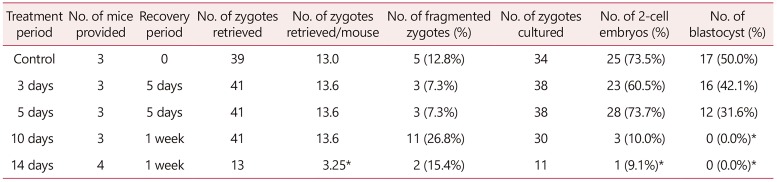
6. Natural recovery of POI after stopping cisplatin treatment
Finally, we examined how long the ovarian function of POF-induced mice was recovered naturally after the last injection of cisplatin. When the mice were injected with cisplatin for 10 days and then were left untreated for 1 week, the average number of zygotes retrieved was 13.6, which was nearly same as the control group (13.0), but the embryo development rate to blastocyst was 0%. When cisplatin was injected for 10 days and then left untreated for 1 week, the average number of zygotes retrieved and embryo development rate were 3.25 and 0%, which was significantly reduced compared to the control group (Table 6). Therefore, this result means that when inducing a POF model with cisplatin, it is most preferable to inject for 10 to 14 days.
Table 6. Natural recovery of ovarian failure after stopping cisplatin treatment.
*P < 0.01 (versus control)
Discussion
Ovarian aging is the main cause of age-related decline in fertility in women, and this is one of the most difficult causes to resolve in the treatment of infertility. For this reason, our research team was working on the development of a substance that could overcome or rescue ovarian aging and have tried to establish the mouse POF as a model for evaluating the efficacy of such substance. Among many anticancer drugs, CTX, Bu, and cisplatin have been widely used to induce POF models. However, the concentration and duration of treatment were very different for each researcher.
Jiang et al.19 reported that when CTX (120 mg/kg) and Bu (12 mg/kg) was injected daily to female mice at 2 months of age, there was no difference in body weight, the ovary size was slightly smaller, and the number of follicles was significantly reduced at 30 days in CTX/Bu-treated mice compared to the control group. In a study of Zhang et al.20 comparing the induction effects of POF by different anticancer drugs, they showed that when CTX and Bu were treated alone for 30 days, there was no difference in body weight, related serum hormonal level, and pathological changes in ovary and uterus. Previously, it has reported that CTX and Bu have relatively low toxicity compared to other anticancer drugs,21,22 but they induced the sufficient damage to the ovaries.19,23,24 So we performed a preliminary study to construct POF model by injecting daily CTX (120 mg/kg) and Bu (12 mg/kg) to 30 female mice aged 6 weeks for 4 weeks. However, unexpected results were observed: mice began to loss body weight from 1 week and about half of the mice started to die from around 2 weeks. We also have attempted to establish POF mouse model using cisplatin (2 mg/kg). Cisplatin was injected for 7 days. And then a substance for the recovery of ovarian function was treated to cisplatin-induced POF mice to investigate whether this substance recovery reduced ovarian function in POF mice. The POF mice recovered naturally within one week and we could not tell whether the improvement of ovarian function was due to our testing substance or natural recovery. Therefore, we have performed the present study to establish an effective POF mouse model using CTX, Bu, and cisplatin considering the complete inhibition and the natural recovery period of ovarian function depending on concentrations and durations of anticancer drugs.
In this respect, the present study clearly shows that it is most effective to use 14 days for CTX/Bu and 10 to 14 days for cisplatin to establish the POF model in mice. These treatment periods not only reliably induced ovarian failure by inhibiting ovarian function, but were not recovered naturally for at least 2 weeks, making it very useful for investigating the improvement effect of ovarian failure for the 2 weeks.
Whether ovarian failure is induced well is verified by several factors, which include body weight, locomotor activity, ovarian and uterine weight, folliculogenesis and follicle counting on ovarian histology, and serum estradiol and FSH concentration, etc. In the present study, body weight, ovarian and uterine weight, and ovarian function were examined to assess whether POF was induced. Ovarian function was defined by the number of zygotes retrieved after superovulation, and followed by mating and developmental competency.
One interesting finding is that changes in body weight can be a useful indicator of the induction of POF. In the present study, although anticancer drugs were administered for the same period, if the body weight did not decrease, ovarian function as well as ovarian and uterine size were normal. In contrast, if body weight was greatly reduced, ovarian and uterine size became very small and hard, and ovarian function was also severely inhibited. In addition, after the last injection of anticancer drugs, mice with rapidly increasing body weight were also recovering in size of the ovaries and uterus, and the ovarian function was also restored naturally. These results indicate that body weight change can be a primary effective indicator for POF induction.
In the induction of POF model, most studies have focused how anticancer drugs inhibit ovarian function and follicular development. However, in addition to this, it is also very important to identify the period during which the inhibited ovarian function is naturally recovered. If we are performing a study to develop a new substance to treat POF and the period of treatment of this substance is 2 weeks, it should be confirmed that induced ovarian failure does not naturally recover within a period of at least 2 weeks after the last administration of anticancer drugs. This is because it is possible to distinguish whether the recovery of ovarian failure is due to a drug or a natural recovery. However, reports on the natural recovery period of ovarian failure are very limited. Sun et al.11 reported that the POF mice did not recover to the normal level within 1 month when CTX (50 mg/kg) was intraperitoneally administered for 15 consecutive days. Liu et al.17 showed no change in ovarian weight after 14 days of CTX (70 mg/mg) injection. Wang et al.14 showed that in the POF mice induced by cisplatin (2 mg/kg) treatment for 7 consecutive days, ovarian weight and follicle counts were significantly decreased at 21 days, indicating that ovarian failure by cisplatin was not recovered naturally until 21 days. These results are somewhat different from results of our present study, which showed that ovarian failure was not restored naturally until 2 weeks after CTX/Bu injection for 2 weeks, and one week after cisplatin injection for more than 10 days. The difference in these results may be due to differences in the concentrations of anticancer drugs and the species of mice used in the experiment.
In conclusion, these results suggest that CTX (120 mg/kg)/Bu (12 mg/kg) should be treated for at least over 2 weeks and cisplatin (2 mg/kg) for at least over 10 days to establish the most effective POI mouse model, assuming no spontaneous recovery for at least 2 weeks unless these anticancer drugs cause rapid body weight loss and death of the mice. In the future, this study may contribute to the effective establishment of the POF mouse model for the development of therapeutic drugs and the study of mechanism of POF.
Acknowledgement
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2017R1A2B4010859).
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Welt CK. Primary ovarian insufficiency: a more accurate term for premature ovarian failure. Clin Endocrinol (Oxf) 2008;68:499–509. doi: 10.1111/j.1365-2265.2007.03073.x. [DOI] [PubMed] [Google Scholar]
- 2.Norling A, Hirschberg AL, Rodriguez-Wallberg KA, Iwarsson E, Wedell A, Barbaro M. Identification of a duplication within the GDF9 gene and novel candidate genes for primary ovarian insufficiency (POI) by a customized high-resolution array comparative genomic hybridization platform. Hum Reprod. 2014;29:1818–1827. doi: 10.1093/humrep/deu149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cox L, Liu JH. Primary ovarian insufficiency: an update. Int J Womens Health. 2014;6:235–243. doi: 10.2147/IJWH.S37636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nelson LM. Clinical practice. Primary ovarian insufficiency. N Engl J Med. 2009;360:606–614. doi: 10.1056/NEJMcp0808697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qin Y, Sun M, You L, Wei D, Sun J, Liang X, et al. ESR1, HK3 and BRSK1 gene variants are associated with both age at natural menopause and premature ovarian failure. Orphanet J Rare Dis. 2012;7:5. doi: 10.1186/1750-1172-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ameratunga D, Weston G, Osianlis T, Catt J, Vollenhoven B. In vitro fertilisation (IVF) with donor eggs in post-menopausal women: are there differences in pregnancy outcomes in women with premature ovarian failure (POF) compared with women with physiological age-related menopause? J Assist Reprod Genet. 2009;26:511–514. doi: 10.1007/s10815-009-9351-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sills ES, Brady AC, Omar AB, Walsh DJ, Salma U, Walsh AP. IVF for premature ovarian failure: first reported births using oocytes donated from a twin sister. Reprod Biol Endocrinol. 2010;8:31. doi: 10.1186/1477-7827-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hernández-Angeles C, Castelo-Branco C. Early menopause: A hazard to a woman's health. Indian J Med Res. 2016;143:420–427. doi: 10.4103/0971-5916.184283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cartwright B, Robinson J, Seed PT, Fogelman I, Rymer J. Hormone replacement therapy versus the combined oral contraceptive pill in premature ovarian failure: A randomized controlled trial of the effects on bone mineral density. J Clin Endocrinol Metab. 2016;101:3497–3505. doi: 10.1210/jc.2015-4063. [DOI] [PubMed] [Google Scholar]
- 10.Slopień R, Warenik-Szymankiewicz A. Premature ovarian failure: diagnosis and treatment. Clin Exp Obstet Gynecol. 2014;41:659–661. [PubMed] [Google Scholar]
- 11.Sun M, Wang S, Li Y, Yu L, Gu F, Wang C, et al. Adipose-derived stem cells improved mouse ovary function after chemotherapy-induced ovary failure. Stem Cell Res Ther. 2013;4:80. doi: 10.1186/scrt231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terraciano P, Garcez T, Ayres L, Durli I, Baggio M, Kuhl CP, et al. Cell therapy for chemically induced ovarian failure in mice. Stem Cells Int. 2014;2014:720753. doi: 10.1155/2014/720753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lai D, Wang F, Yao X, Zhang Q, Wu X, Xiang C. Human endometrial mesenchymal stem cells restore ovarian function through improving the renewal of germline stem cells in a mouse model of premature ovarian failure. J Transl Med. 2015;13:155. doi: 10.1186/s12967-015-0516-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Z, Wang Y, Yang T, Li J, Yang X. Study of the reparative effects of menstrual-derived stem cells on premature ovarian failure in mice. Stem Cell Res Ther. 2017;8:11. doi: 10.1186/s13287-016-0458-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rebar RW. Premature ovarian “failure” in the adolescent. Ann N Y Acad Sci. 2008;1135:138–145. doi: 10.1196/annals.1429.000. [DOI] [PubMed] [Google Scholar]
- 16.Qin Y, Jiao X, Simpson JL, Chen ZJ. Genetics of primary ovarian insufficiency: new developments and opportunities. Hum Reprod Update. 2015;21:787–808. doi: 10.1093/humupd/dmv036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu TE, Wang S, Zhang L, Guo L, Yu Z, Chen C, et al. Growth hormone treatment of premature ovarian failure in a mouse model via stimulation of the Notch-1 signaling pathway. Exp Ther Med. 2016;12:215–221. doi: 10.3892/etm.2016.3326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.He L, Ling L, Wei T, Wang Y, Xiong Z. Ginsenoside Rg1 improves fertility and reduces ovarian pathological damages in premature ovarian failure model of mice. Exp Biol Med (Maywood) 2017;242:683–691. doi: 10.1177/1535370217693323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jiang Y, Zhao J, Qi HJ, Li XL, Zhang SR, Song DW, et al. Accelerated ovarian aging in mice by treatment of busulfan and cyclophosphamide. J Zhejiang Univ Sci B. 2013;14:318–324. doi: 10.1631/jzus.B1200181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang T, Yan D, Yang Y, Ma A, Li L, Wang Z, et al. The comparison of animal models for premature ovarian failure established by several different source of inducers. Regul Toxicol Pharmacol. 2016;81:223–232. doi: 10.1016/j.yrtph.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Copelan EA, Biggs JC, Szer J, Thompson JM, Crilley P, Brodsky I, et al. Allogeneic bone marrow transplantation for acute myelogenous leukemia, acute lymphocytic leukemia, and multiple myeloma following preparation with busulfan and cyclophosphamide (BuCy2) Semin Oncol. 1993;20:33–38. [PubMed] [Google Scholar]
- 22.de Magalhaes-Silverman M, Lister J, Rybka W, Wilson J, Ball E. Busulfan and cyclophosphamide (BU/CY2) as preparative regimen for patients with lymphoma. Bone Marrow Transplant. 1997;19:777–781. doi: 10.1038/sj.bmt.1700733. [DOI] [PubMed] [Google Scholar]
- 23.Han YS, Lee AR, Song HK, Choi JI, Kim JH, Kim MR, et al. Ovarian volume in Korean women with polycystic ovary syndrome and its related factors. J Menopausal Med. 2017;23:25–31. doi: 10.6118/jmm.2017.23.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim HG, Song YJ, Na YJ, Yang J, Choi OH. A rare case of an autoamputated ovary with mature cystic teratoma. J Menopausal Med. 2017;23:74–76. doi: 10.6118/jmm.2017.23.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]