Abstract
Introduction:
The aim of this study was to determine the predictors of 30-day postoperative complications for surgical treatment of lumbar spinal stenosis with degenerative spondylolisthesis (LSSDS) in patients undergoing decompression and fusion or decompression alone.
Methods:
A retrospective review of 253 unique patients undergoing surgical intervention for LSSDS in the American College of Surgeons National Surgical Quality Improvement Program database was conducted.
Results:
The overall 30-day postoperative complication rate for the population was 16.6% (95% confidence interval [CI], 12.0% to 21.0%). Transfusions (8.9%), readmissions (5.9%), and unplanned returns to the OR (3.6%) were the most frequently observed complications across the population. ASA score and surgical time were found to be significant predictors of 30-day complications (ASA score: OR = 1.971; 95% CI, 1.077 to 3.609; P = 0.028; surgical time: OR = 1.006; 95% CI, 1.003 to 1.010; P < 0.001). Holding all other variables constant, multilevel cases, the inclusion of a fusion procedure, and body mass index were not found to be significant predictors of 30-day complications (P = 0.917, P = 0.464, and P = 0.572, respectively).
Discussion and Conclusions:
ASA score and OR time are leading indicators of complications, specifically for the LSSDS patient population. These are two easily attainable data points that are available for all surgical cases and could be used a clinical red flag for potential complications.
Lumbar spinal stenosis with degenerative spondylolisthesis (LSSDS) is a relatively common adult degenerative spinal condition. LSSDS can result in a variety of symptoms, including axial back pain, radicular leg pain, and neurogenic claudicatory pain.1 It has been established that patients undergoing surgical treatment for LSSDS showed substantially greater improvement in pain and function over a period of 2 years than those treated nonsurgically.1,2 In addition, favorable 30-day outcomes for surgical treatment of LSSDS have been demonstrated across multiple studies.3 Despite these findings, debate over the optimal surgical intervention remains. A seminal 1995 article by Herkowitz and Sidhu4 concluded that the addition of fusion to decompression is the near-consensus optimal surgical treatment for LSSDS. To this point, various studies demonstrated that patients undergoing decompression with concurrent arthrodesis had better relief of pain in the back and lower limbs,5,6 less chance of vertebral slip progression,6 less chance of recurrent stenosis,7 and better overall clinical outcomes.5,6,7,8 Given this body of evidence, the use of decompression with concomitant fusion has proliferated in the treatment of LSSDS, resulting in a reduction in the rate of decompression alone from 12% in 1999 to 4% in 2011.8 Despite these trends, a series of recent findings suggest that decompression alone may remain a viable alternative in the surgical treatment of LSSDS. In the Spinal Laminectomy versus Instrumented Pedicle Screw trial, grade I DS patients with stable spondylolisthesis undergoing decompression and fusion had a greater increase in Short Form Health Survey physical component scores after 2, 3, and 4 years, but no significant improvement in the Oswestry Disability Index score after 2 years compared with the decompression alone group.9 The primary aim of this study was to determine the predictors of 30-day postoperative complications for surgical treatment of LSSDS in patients undergoing decompression and fusion or decompression alone.
Methods
A retrospective review of 253 unique patients undergoing surgical intervention for LSSDS in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database was conducted. Patients were included if they had a primary International Classification of Diseases version 10 (ICD-10) diagnosis code of M43.16—spondylolisthesis, lumbar region, or a primary ICD-9 diagnosis code 738.4—acquired spondylolisthesis. Patients were then divided into two groups of surgical approaches based on Current Procedural Terminology (CPT) codes: fusion (ie, any procedure including a CPT code of 22585, 22586, 22612, 22630, 22633, 22800, 22840, 22558, 22586, 22612, 22614, 22630, 22632, 22633, 22634, 22808, 22840, 22841, 22842, 22849, 22850, 22851, and 22852) and decompression alone (ie, any procedure including a CPT code of 63017, 63030, 63042, 63047, 63267, 64708, 63035, 63047, and 63048 without an accompanying fusion code). Surgeries were also classified as either single level or multilevel, with multilevel cases denoted by the inclusion of additional segment codes (ie, 22585, 22614, 22632, 22842, or 63017).
The primary outcome measure was any complication in the 30 days after surgery. Across the population, the following 30-day complications were observed and included in the analysis: surgical site infection, pneumonia, reintubation, pulmonary embolism, urinary tract infection, blood transfusion, deep vein thrombosis, unplanned return to the OR, and readmission. All statistical analysis was performed using SPSS version 22 (IBM). Chi-square analysis was conducted to compare complication rates between the dichotomous groups and was used as a basis for targeting variables for inclusion in the regression model. Binomial logistic regression was used to examine the relationship between independent variables and the primary outcome variable and evaluate the predictive power of independent variables.
Results
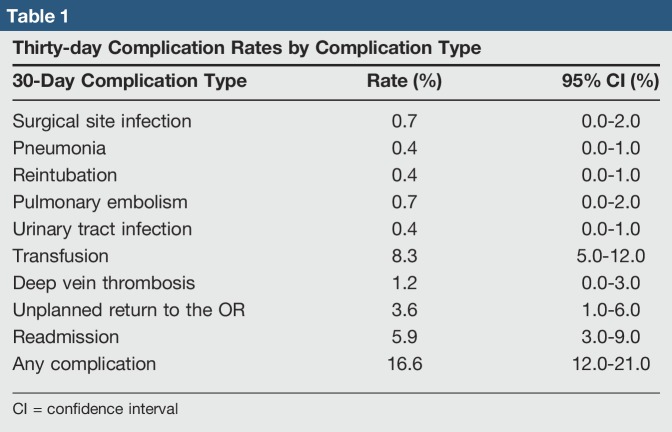
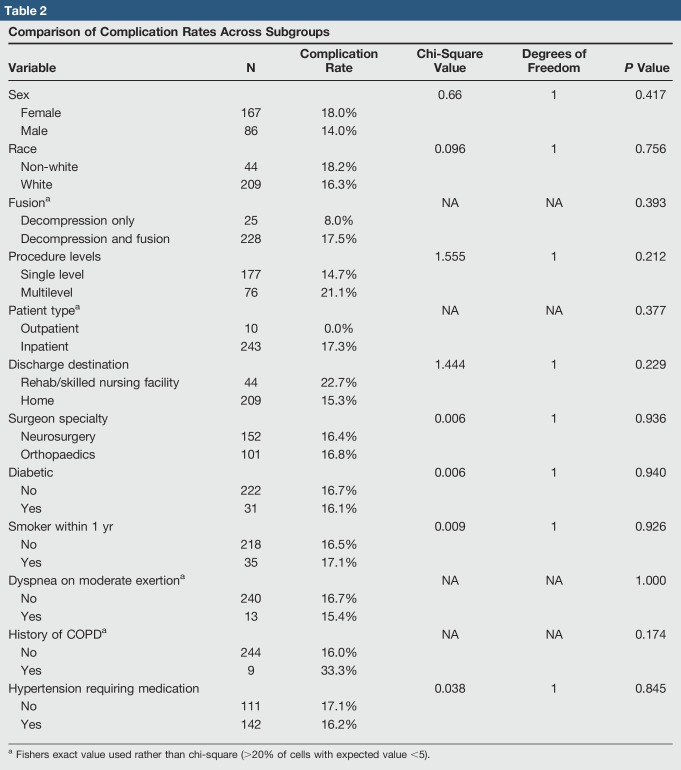
The study population examined was 66% female, 83% white, and had a mean age of 61.9 ± 12.7 years and mean body mass index (BMI) of 31.2 ± 6.3 kg/m2. The overall 30-day postoperative complication rate for the population was 16.6% (95% confidence interval [CI], 12.0% to 21.0%). Transfusions (8.9%), readmissions (5.9%), and unplanned returns to the OR (3.6%) were the most frequently observed complications across the population. The rates of each observed complication are presented in Table 1. Using chi-square analysis, complication rates between various dichotomous subgroups were compared and are presented in Table 2. Notably, no statistically significant between-group differences were observed across any of the subgroups, although clinically relevant trends were observed. Although not statistically significant, complication rates were higher when a fusion was performed in conjunction with decompression (decompression only = 8.0% versus decompression and fusion = 17.5%; P = 0.393), in multilevel procedures (single level = 14.7% versus multilevel = 21.1%; P = 0.212), and when patients were discharged to a rehab facility (discharge to a rehab facility = 22.7% versus discharge to home = 15.3%; P = 0.229).
Table 1.
Thirty-day Complication Rates by Complication Type
Table 2.
Comparison of Complication Rates Across Subgroups
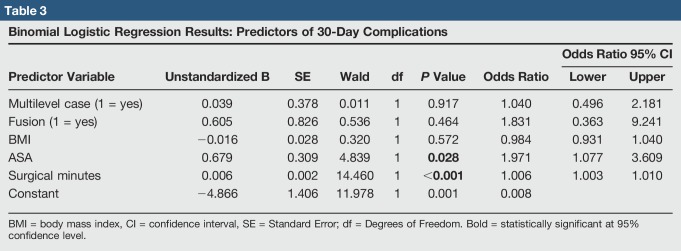
The results of the binomial logistic regression model are presented in Table 3. Using the five variables that were selected for inclusion in the regression, 13.2% of the variance in complication rates is explained by the model. The analysis reveals that the ASA score and surgical time were found to be significant predictors of 30-day complications. The results suggest that holding all other variables constant, a 1-unit increase in the ASA score increases the odds of the postoperative complication by approximately 97.1% (OR = 1.971; 95% CI, 1.077 to 3.609; P = 0.028). In addition, a 1-minute increase in the surgical time increases the odds of the postoperative complication by approximately 0.6% (OR = 1.006; 95% CI, 1.003 to 1.010; P < 0.001). Holding all other variables constant, multilevel cases, the inclusion of a fusion procedure, and BMI were not found to be significant predictors of 30-day complications (P = 0.917, P = 0.464, and P = 0.572, respectively).
Table 3.
Binomial Logistic Regression Results: Predictors of 30-Day Complications
Discussion and Conclusions
Our findings confirm the applicability of the ASA score and OR time as leading indicators of complications, specifically for the LSSDS patient population. Our findings are similar to those of other studies, which demonstrated the association of the ASA score and OR time with suboptimal outcomes such as prolonged length of stay and surgical site infections after spine surgery.10,11 These are two easily attainable data points that are available for all surgical cases and could be used as a clinical red flag for potential complications. However, the addition of a fusion to decompression, multilevel surgeries, and patient BMI were not found to be significant predictors of 30-day complications. It could be interpreted that these commonly cited risk factors may have less impact than presumed on 30-day postoperative complications for patients undergoing surgical treatment for LSSDS. Despite this possibility, we propose that these do remain significant drivers of clinical outcome, given the fact that chi-square analysis displayed meaningful, albeit not statistically significant differences in complication rates between the groups with the addition of fusion or multilevel surgery. A final noteworthy aspect of this study is the transfusion rate that was observed in the patient population. Within our cohort, 21 of the 42 (50%) reported complications were from blood transfusions, a rate of 8.3%. Compared with this rate, Weinstein et al1 reported postoperative transfusion rates of 16% in the randomized cohort and 24% in the observational cohorts of patients undergoing surgery for LSSDS in the SPORT trial, whereas Golinvaux et al reported a postoperative transfusion rate of 18.2% in an analysis of patients in the ACS-NSQIP database undergoing surgery for LSSDS in 2010 to 2011. Given the substantially lower transfusion rates demonstrated by our study, we propose that significant progress has been made in recent years to reduce postoperative transfusions through programs such as the Choosing Wisely campaign,12 surgical approach, the expanded use of advanced intraoperative hemostatic agents, and the use of synthetic antifibrinolytic drugs such as tranexamic acid.
To our knowledge, this study is the first to use the ACS-NSQIP database to specifically analyze predictors of postoperative complications for patients undergoing surgery for LSSDS. A limitation of this study is its retrospective nature and its limited sample size based on 1 year of national data. Because of the limited sample size, subgroup analysis was underpowered to detect significant differences at the 95% confidence level. In addition, the predictive value of the overall model is limited as demonstrated by its explanation of approximately 13.2% of the variance in 30-day complications. This phenomenon highlights the heterogeneous nature of LSSDS that may not be adequately captured by the level of data captured in cross-specialty registries such as the ACS-NSQIP database. To validate the findings of this work, comparison studies using discipline-specific databases must be conducted to establish homogenous subgroups based on clinically relevant factors such as Meyerding grade, disk height, slip angle, and the presence of segmental instability. Future prospective studies should be conducted to evaluate these findings, and additional evaluation of predictors for clinical and patient-reported quality-of-life outcomes beyond the 30-day postoperative period should be conducted.
Footnotes
Neither of the following authors nor any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Turcotte and Dr. Patton.
References
- 1.Weinstein JN, Lurie JD, Tosteson TD, et al. : Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med 2007;356:2257-2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weinstein JN, Lurie JD, Tosteson TD, et al. : Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis: Four-year results in the spine patient outcomes research trial (SPORT) randomized and observational cohorts. J Bone Joint Surg 2009;91:1295-1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Golinvaux NS, Basques BA, Bohl DD, Yacob A, Grauer JN: Comparison of 368 patients undergoing surgery for lumbar degenerative spondylolisthesis from the SPORT trial with 955 from the NSQIP database. Spine 2015;40:342-348. [DOI] [PubMed] [Google Scholar]
- 4.Herkowitz HN, Sidhu KS: Lumbar spine fusion in the treatment of degenerative conditions: Current indications and recommendations. J Am Acad Orthop Surg 1995;3:123-135. [DOI] [PubMed] [Google Scholar]
- 5.Herkowitz HN, Kurz LT: Degenerative lumbar spondylolisthesis with spinal stenosis: A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 1991;73:802-808. [PubMed] [Google Scholar]
- 6.Bolesta MJ, Bohlman HH: Degenerative spondylolisthesis: The role of arthrodesis. Presented at the 56th Annual Meeting of the American Academy of Orthopaedic Surgeons, Las Vegas, February 14, 1989.
- 7.Postacchini F, Cinotti G: Bone regrowth after surgical decompression for lumbar spinal stenosis. J Bone Joint Surg Br 1992;74:862-869. [DOI] [PubMed] [Google Scholar]
- 8.Kepler CK, Vaccaro AR, Hilibrand AS, et al. : National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine 2014;39:1584-1589. [DOI] [PubMed] [Google Scholar]
- 9.Ghogawala Z, Dziura J, Butler WE, et al. : Laminectomy plus fusion versus Laminectomy alone for lumbar spondylolisthesis. N Engl J Med 2016;374:1424-1434. [DOI] [PubMed] [Google Scholar]
- 10.Sebastian A, Huddleston P, Kakar S, Habermann E, Wagie A, Nassr A: Risk factors for surgical site infection after posterior cervical spine surgery: An analysis of 5,441 patients from the ACS NSQIP 2005-2012. Spine J 2016;16:504-509. [DOI] [PubMed] [Google Scholar]
- 11.Basques BA, Fu MC, Buerba RA, Bohl DD, Golinvaux NS, Grauer JN: Using the ACS-NSQIP to identify factors affecting hospital length of stay after elective posterior lumbar fusion. Spine 2014;39:497-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Society of Hematology: Choosing Wisely Campaign: Ten Things Physicians and Patients Should Question. http://www.choosingwisely.org/societies/american-society-of-hematology/. [Google Scholar]
- 13.Shi H, Ou Y, Jiang D, Quan Z, Zhao Z, Zhu Y: Tranexamic acid reduces perioperative blood loss of posterior lumbar surgery for stenosis or spondylolisthesis: A randomized trial. Medicine (Baltimore) 2017;96:e5718. [DOI] [PMC free article] [PubMed] [Google Scholar]