Abstract
Introduction:
Outpatient surgery has a great opportunity to demonstrate the role of using mobile video conference (VC) postoperatively. Our patients use technology to help decision making in finding physicians. The authors aim to assess patient's perception on the use of mobile apps for VC with the surgeon and/or staff.
Methods:
Consenting patients completed a questionnaire of 10 questions preoperatively and postoperatively to assess the difference in opinion.
Results:
Overall, 120 patients completed the questionnaire preoperatively with 58% female population, 71% younger than 65 years, and 67% having a GED/higher education. Fifty-two patients had surgery with 54% female population, and 60% were younger than 65 years. All patients had mobile apps for VC with 55% using WhatsApp, 40% using Facetime, and 5% other. In person, being with a trained educator at the office was the preferred method for learning about surgical procedures. Overall, four patients contacted the surgeon directly preoperatively. After surgery, 8 of 52 patients (15%) used VC to the surgeon directly, and 37 patients used the VC with the team.
Conclusion:
With advances in new technology, the use of mobile video conferencing adds a new forum for communication with patients. In the outpatient surgical setting, this forum would improve patient-physician relations.
Patient-to-physician interaction has improved with the advances made in communication and access to information via the Internet and electronic devices. The plethora of avenues of communication has led to the increase in health-seeking behaviors of patients. These avenues include being able to research current symptoms, make appointments online, review several physicians in a specialized field nearest to their location, and most recently, being able to speak with a physician via video conference (VC) to determine differentials and the best mode of therapy.
The role of technology in medicine is mainly used by patients in decision making for finding and assessing physicians. Millennials have challenged several industries in recent years, and medicine is on the verge of change with these new challenges. Physicians need to embrace technology not only in daily practice of EMR usage but also in the follow-up of patients.
Telemedicine has been defined in 2004 by the Society of American Gastrointestinal and Endoscopic Surgeons.1 Teleconference is a real-time and live interactive program in which one set of participants are at one or more locations and the other set of participants are at another location. The teleconference allows for interaction, including audio and/or video, and possibly other modalities, between at least two sites.1 A study by Augestad and Lindsetmo2 has demonstrated the use of video conferencing for surgeons and its benefits, especially, in rural areas. Newer technology has allowed mobile video conferencing with an encryption specifically to the application or mobile phone.3 This increases the level of security while allowing for the ease of communication.
Outpatient health care and follow-up has a great opportunity in demonstrating the role using VC in the follow-up of patients postoperatively before and in between clinic visits. This allows direct visual and audio communication, giving assurance to both physicians and patients. The authors postulate that the use of mobile video conferencing not only will improve the patient-surgeon relationship but also is a tool to assist in the diagnosis of any postoperative complications, especially in the outpatient setting. As such, we assessed patients' attitudes toward, and the potential use of, mobile video conferencing as a means of communication between surgeon and patients.
Methods
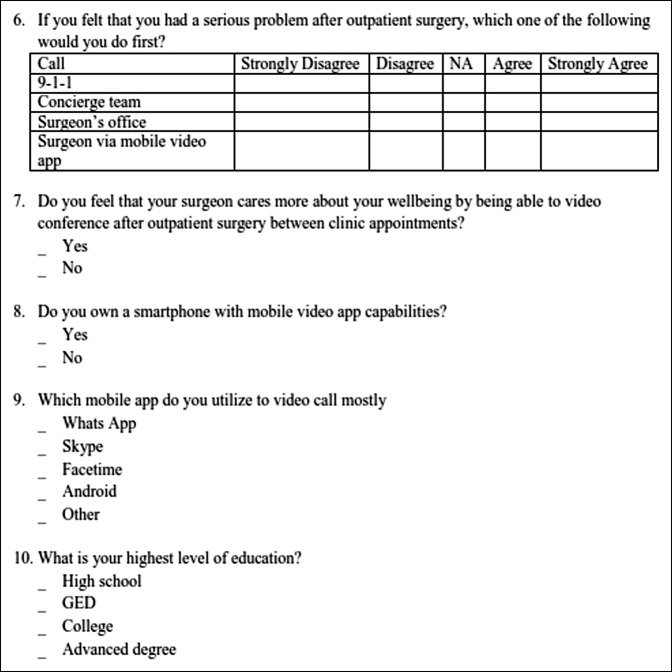
Patients who presented to an orthopedic institute were presented with a questionnaire. The surveys were given to each patient by the clerical staff as part of the registration package along with other general health registration and survey questionnaires. No instructions were given to the patient or clerk regarding the study forms, and completion was voluntary and anonymous with no identification on the forms. Age younger than 18 years was the only exclusion criteria. Patients were also informed of the communication options to contact the office via a telephone number, an independent surgical concierge team directly with a mobile phone number, or with mobile VC app. All patients were also given access to the surgeon's mobile number4 and a team member from the independent concierge service Surgical Education Responsibilities Value and Empathy to use mobile VC app. The survey questions were developed with insights from the literature regarding communication methods between patients and physicians4,5,6,7,8,9,10,11,12,13,14,15,16,17,18 and to address numerous issues (Figure 1). To determine patient attitudes regarding surgery and the use of mobile VC app, we asked the surveyed participants using a five-point Likert scale: preferred mode of education before consenting for surgery (question 1) and preferred method about learning about surgery (question 2). Potential topics of promoting the use of mobile VC app were elicited with questions 3 and 4. To assess communication routes after surgery, we surveyed patients’ responses to a minor problem (question 5) and a serious problem (question 6). Question 7 investigated whether respondents thought that their treating surgeon cared more about their personal well-being if he or she offered the opportunity to video call after outpatient surgery. Question 8 sought to determine how many patients owned a smartphone with mobile VC app capabilities. Question 9 sought to determine which app was being used for VC. Question 10 investigated the potential effects of education level on the answers to the above questions. Consenting patients for surgery had access to both in-person and VC educational sessions for preoperative counseling and instructional material. Materials included a demonstration using bone models, videos, patient testimonials, and literature as online and printed materials. Access to team postoperatively via phone calls, mobile video conferencing, and visits from concierge service was discussed with each patient at the time of scheduling and also at patient education class with the concierge (Surgical Education Responsibilities Value and Empathy) team.
Figure 1.
Questionnaire for the use of mobile app in video conference patients.
We followed 120 patients who consented to be part of this study and completed the survey over the period from June 2016 to December 2016. Patients who proceeded to surgery were given educational classes and informed of outcomes and complications. Patients were followed in the immediate postoperative period and were given a 10-question survey to prospectively assess patient attitudes regarding surgery and the use of mobile VC app postoperatively. Documentation of patients in the study who called after the initial visit and after surgery was recorded, and the reason for the call documented.
Results
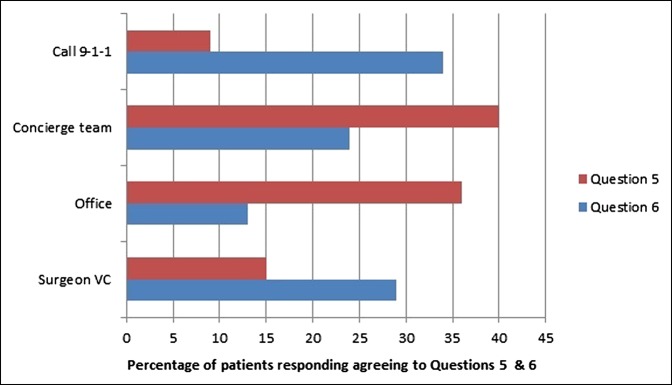
A total of 120 patients completed questionnaire preoperatively from a sample of 150 patients with 58% female population and 71% younger than 65 years. A total of 52 patients had surgery from the completed survey group with 54% female population and 60% younger than 65 years. All patients had a mobile app for video conferencing with 55% using WhatsApp, 40% using Facetime, and 5% using Skype and/or other. In person, being with a trained educator at the office was the preferred mode and method of learning about surgical procedures (questions 1 and 2). However, 92% of patients agreed or strongly agreed considering the use of mobile VC in communicating with the surgeon, mostly for the surgical procedure and postoperative surgical day (questions 3 and 4). For questions 5 and 6, patients would call surgeons office or concierge team for minor problems. For major problems, they would call 9-1-1 or surgeon via mobile VC app Figure 2. Eighty-three percent of patients thought that having mobile video app access suggested that their surgeon was more caring preoperatively compared with 89% postoperatively. Overall, four patients contacted surgeon directly calling mobile phone but no one used VC preoperatively. After surgery, 8 of 52 patients (15%) used VC to the surgeon directly, and 37 patients contacted the concierge team using VC before the first postoperative visit. The other seven patients did not call or VC office, concierge team, or surgeon.
Figure 2.
Bar chart showing the percentage of patients responding agree/strongly agree to questions 5 and 6.
Discussion
Physician-patient interaction can be built on effective and ample communication, allowing for successful delivery of medical care. Patients are less likely to sue if physicians are accessible, give more explanation, and allow patients to have a greater understanding of their complaints and medical issues with access to information to goals of care and making patient believe like part of the decision-making process.4,5,8,9,13,14,17,18 Common methods of physician-patient communication include direct face-to-face communication during the office visit, through an office staff, or through returned telephone calls by the physician. As technology advances, video conferencing has been demonstrated as an option to follow-up patients.19,20,21,22 The advent of video conferencing on mobile phones adds a simple, encrypted, and effective method to follow patients. The potential for excessive use by patients may limit its attractiveness to physicians, but the potential to enhance the patient-physician relationship and to promptly respond to urgent issues are substantial.
This study aimed to determine patient opinion pre- and postoperatively to the use of mobile apps for patient education and postoperative follow-ups. Patients surveyed preferred to be educated in person by a trained educator. They would either call the office for minor issues and 9-1-1 or surgeon for major issues after the surgery. Looking at the calls received, before surgery, no patients tried to VC the surgeon, except four patients, who called his cell phone because of their inability to get through to office for a refill in medications and update for revision surgery. After surgery, patients showed restraint in calling the surgeon unless they thought that they had a serious problem or had difficulty contacting the scheduler or secretary. During this 6-month period, the surgeon received 8 of 52 (15%) VC calls, whereas 37 patients contacted concierge team using VC (Figure 3) before the first postoperative visit. The other seven patients did not call or VC before the first postoperative appointment.
Figure 3.
Screen shot demonstrating video conferencing with patient. A, With C-collar. B, After dressing removal.
The interesting findings of the survey were the fact that 83% of the surveyed patients thought that their treating surgeon cared more about their well-being if he or she is able to mobile VC, which increased in postoperative surveyed participants. More than 90% of patients agreed that they would mobile VC their surgeon if they had the option preoperatively.
This is in contrast to the postoperative data, in which 8 of 52 (15%) called surgeon postoperatively. Several studies5,9,13,14,18 assess patient satisfaction with ample communication with patients. Patients were more satisfied with their physician if he or she were considered to be caring and more accessible. Assessing malpractice and litigation, Adamson et al5 found that orthopaedic surgeons with a better rapport with their patients, who took more time to explain, and who were available had a fewer malpractice suits. Litigious patients’ feeling inversely correlated with their perception of a caring physician, as reported by Lester and Smith.13 Wofford et al18 demonstrated that 15% of formal patient complaints resulted from the perceived unavailability of the physician, which include the lack of follow-up care and unanswered phone calls to the physician's office.
Physician-patient communication is therefore of utmost importance in decreasing the perception of lack of care and communication. In a study at the University of Michigan health services, the authors demonstrated that within implementing full disclosure of medical errors, there was no increase in liability compensation and cost.23 Newman et al24 in a recent study demonstrated poor physician-patient communication and the difference in perception with overestimation of both the risks of myocardial infarction and the potential benefit of hospital admission between physicians and patients. The results showed that patients reported discussing the likelihood of their symptoms being the result of myocardial infarction in 65% of cases, whereas physicians reported this in 46%.24 A patient-integrated approach to perceived problem diagnosis, goals of management, and possible follow-up should be the aim of physicians, thereby decreasing medical errors and poor physician-patient interactions.24
This study notes the following limitations; specifically, the survey assessed for mobile video conferencing and was developed from issues discussed in the literature regarding physician-patient communication and based off a similar study because it relates to access to a physician via a mobile phone.4 The survey was anonymous, and patients were told that the physician would not know the results of the survey or that the results would not affect care in any way. Because of this measure, the likelihood that patients would feel pressure to respond in a certain manner would be reduced.
The results of the survey come from one surgeon's practice in one subspecialty that is not a representative of all populations, and therefore, its results may be different for rural areas, developing countries, pediatric or elderly populations, people with HIV, and burn victims, especially when caregivers become involved. A recent randomized controlled trial demonstrated that mobile app follow-up care neither affects complication rates nor patient-reported satisfaction scores, but it improves patient-reported convenience scores.25 As a change of policy for outpatient follow-up, we have established a team who will mobile VC patient on immediate postoperative period and follow-up call before first postoperative visit.
Conclusion
The advances in technology allow for improvement in health care with the use of telemedicine. Using mobile video conferencing adds a new forum that is an easily accessible form of communication with patients. In the outpatient surgical setting, this forum could improve physician-patient relations.
Acknowledgments
The authors would like to thank Saily Lopez and the Surgical Education Responsibilities Value and Empathy (S.E.R.V.E) team for their assistance with this project.
Footnotes
Dr. Chin or an immediate family member has stock or stock options held in SpineFrontier; has received research or institutional support from LES Society; and as received nonincome support (such as equipment or services), commercially derived honoraria, or other non–research-related funding (such as paid travel) from SpineFrontier; and serves as a board member, owner, officer, or committee member of LES Society. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Pencle, Ms. Benny, Ms. Quijada, and Dr. Seale.
References
- 1.Society of American Gastrointestinal Endoscopic Surgeons (SAGES). https://wwwsagesorg/publications/guidelines/guidelines-for-the-surgical-practice-of-telemedicine/. Accessed March 15, 2010.
- 2.Augestad KM, Lindsetmo RO: Overcoming distance: Video-conferencing as a clinical and educational tool among surgeons. World J Surg 2009;33:1356-1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.http://www.atris.io/o-and-p/new-whatsapp-end-to-end-encryption-free-hipaa-compliant-messaging/,in http://wwwatrisio/o-and-p/new-whatsapp-end-to-end-encryption-free-hipaa-compliant-messaging/. Accessed January 11, 2017.
- 4.Chin KR, Adams SB, Jr, Khoury L, Zurakowski D: Patient behavior if given their surgeon's cellular telephone number. Clin Orthop Relat Res 2005;439:260-268. [DOI] [PubMed] [Google Scholar]
- 5.Adamson TE, Bunch WH, Baldwin DC, Oppenberg A: The virtuous orthopaedist has fewer malpractice suits. Clin Orthop Relat Res 2000;378:104-109. [DOI] [PubMed] [Google Scholar]
- 6.American Health Information Management A: Practice brief: Portable computer security: American health information management association. J AHIMA 2000;71:80A-80C. [PubMed] [Google Scholar]
- 7.Entman SS, Glass CA, Hickson GB, Githens PB, Whetten-Goldstein K, Sloan FA: The relationship between malpractice claims history and subsequent obstetric care. JAMA 1994;272:1588-1591. [PubMed] [Google Scholar]
- 8.Hickson GB, Clayton EW, Githens PB, Sloan FA: Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA 1992;267:1359-1363. [PubMed] [Google Scholar]
- 9.Huycke LI, Huycke MM: Characteristics of potential plaintiffs in malpractice litigation. Ann Intern Med 1994;120:792-798. [DOI] [PubMed] [Google Scholar]
- 10.Kane B, Sands DZ: Guidelines for the clinical use of electronic mail with patients: The AMIA internet working group, task force on guidelines for the use of clinic-patient electronic mail. J Am Med Inform Assoc 1998;5:104-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaplan SH, Greenfield S, Ware JE: Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989;27:S110-127. [DOI] [PubMed] [Google Scholar]
- 12.Katz SJ, Moyer CA, Cox DT, Stern DT: Effect of a triage-based E-mail system on clinic resource use and patient and physician satisfaction in primary care: A randomized controlled trial. J Gen Intern Med 2003;18:736-744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lester GW, Smith SG: Listening and talking to patients. A remedy for malpractice suits? West J Med 1993;158:268-272. [PMC free article] [PubMed] [Google Scholar]
- 14.Levinson W, Roter DL, Mullooly JP, Dull VT, Frankel RM: Physician-patient communication: The relationship with malpractice claims among primary care physicians and surgeons. JAMA 1997;277:553-559. [DOI] [PubMed] [Google Scholar]
- 15.Liederman EM, Morefield CS: Web messaging: A new tool for patient-physician communication. J Am Med Inform Assoc 2003;10:260-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patt MR, Houston TK, Jenckes MW, Sands DZ, Ford DE: Doctors who are using e-mail with their patients: A qualitative exploration. J Med Internet Res 2003;5:e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Suarez-Almozar ME: Patient-physician communication. Curr Opin Rheumatol 2004;16:91-95. [DOI] [PubMed] [Google Scholar]
- 18.Wofford MM, Wofford JL, Bothra J, Kendrick SB, Smith A, Lichstein PR: Patient complaints about physician behaviors: A qualitative study. Acad Med 2004;79:134-138. [DOI] [PubMed] [Google Scholar]
- 19.Hickey S, Gomez J, Meller B, et al. : Interactive home telehealth and burns: A pilot study. Burns 2017;43:1318-1321. [DOI] [PubMed] [Google Scholar]
- 20.Moore AB, Krupp JE, Dufour AB, et al. : Improving transitions to post-acute care for elderly patients using a novel video-conferencing program: ECHO- care transitions. Am J Med 2017;130:1199-1204. [DOI] [PubMed] [Google Scholar]
- 21.Cai LZ, Caceres M, Dangol MK, et al. : Accuracy of remote burn scar evaluation via live video-conferencing technology. Burns 2016; Dec 5 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 22.Bounthavong M, Pruitt LD, Smolenski DJ, Gahm GA, Bansal A, Hansen RN: Economic evaluation of home-based telebehavioural health care compared to in-person treatment delivery for depression. J Telemed Telecare 2018;24:84-92. [DOI] [PubMed] [Google Scholar]
- 23.Kachalia A, Kaufman SR, Boothman R, et al. : Liability claims and costs before and after implementation of a medical error disclosure program. Ann Intern Med 2010;153:213-221. [DOI] [PubMed] [Google Scholar]
- 24.Newman DH, Ackerman B, Kraushar ML, et al. : Quantifying patient-physician communication and perceptions of risk during admissions for possible acute coronary syndromes. Ann Emerg Med 2015;66:13-18.e11. [DOI] [PubMed] [Google Scholar]
- 25.Armstrong KA, Coyte PC, Brown M, Beber B, Semple JL: Effect of home monitoring via mobile app on the number of in-person visits following ambulatory surgery: A randomized clinical trial. JAMA Surg 2017;152:622-627. [DOI] [PMC free article] [PubMed] [Google Scholar]