Abstract
Background:
Hepatic function is closely associated with prognosis in patients with hepatocellular cancer (HCC). In this study, a meta-analysis of the published studies was performed to assess the prognostic value of ALBI grade in HCC patients.
Methods:
Databases, including PubMed, EMbase, Web of Science, and Cochrane Library were retrieved up to August 2018. The primary outcome was OS and secondary outcome was DFS, the prognostic impact of which was assessed by using hazard ratio (HRs) with corresponding 95% confidence intervals (CIs). The enrolled studies were analyzed by using STATA version 12.0 software.
Results:
A total of 22,911 patients with HCC in 32 studies were included. Our results demonstrated that high pretreatment ALBI is associated with poor OS (HR = 1.719, 95%CI: 1.666–1.771, P = .000, univariate results; HR = 1.602, 95%CI: 1.470–1.735, P = .000, multivariate results) and poor DFS (HR = 1.411, 95%CI: 1.262–1.561, P = .000, univariate results; HR = 1.264, 95%CI: 1.042–1.485, P = .000, multivariate results). Meanwhile, when the analysis was stratified into subgroups, such as treatment methods, sample size, geographic area, and ALBI grade, the significant correlation in ALBI and poor long-term survival was not altered.
Conclusion:
High pretreatment ALBI is closely associated with poor prognosis in HCC, and High ALBI should be treated as an ideal predictor during hepatocellular therapy.
Keywords: albumin to bilirubin ratio, hepatic function, hepatocellular cancer, prognostic factor
1. Introduction
Hepatocellular cancer is the fifth most common aggressive malignancies in the world, which leads to the second cancer-related mortality.[1] The prognosis of hepatocellular patients was assessed according to several factors, such as hepatic function, tumor burden, hepatitis virus type, and performance status. The liver function was mostly defined by Child-Pugh's class, while Barcelona Clinic Liver Cancer staging system was used to provide guidelines for HCC treatment frequently.[2] Due to the high recurrence and mortality rate, various molecular markers have been reported to show prognostic importance in patients with HCC.[3] Among them, the ALBI (calculate as log10 bilirubin∗0.66 + albumin∗0.085) was first proved to be not only a marker to assess hepatic function but also a prognostic factor to predict long-term survival in HCC patients in 2015.[4] Different from Child-Pugh's class, ALBI grade only contains two parameters, including albumin and bilirubin. Recently, several studies have confirmed that the ALBI grade successfully predicted the OS and DFS in HCC patients after curative hepatectomy, radiotherapy, transarterial chemoembolization, and sorafenib.[5–8]
However, there is still no consensus on the clinical value of ALBI grade. Because of that, the Child-Pugh's class is the only tool to assess the hepatic function. Therefore, we performed this meta-analysis to evaluate the prognostic role of ALBI grade in patients with HCC.
2. Methods
2.1. Literature search strategy
A systematic literature search was performed in PubMed, EMbase, Web of Science, and Cochrane library (up to August 1st, 2018). In each database, the following terms were combined as key words: (hepatocellular or liver) and (tumor or cancer or carcinoma or adenocarcinoma or malignant) and (“albumin to bilirubin ratio” or “albumin/bilirubin” or “albumin to bilirubin” or “ALBI” or ”albumin and bilirubin”),as well as (“overall survival” or ”disease-free survival” or recurrence or mortality, prognosis or prognostic or predict).
2.2. Inclusion criteria
The inclusion criteria were as follows: (1) patients with hepatocellular carcinoma; (2) prognostic value of ALBI was evaluated on overall survival (OS), disease-free survival (DFS), progression-free survival (PFS), mortality or recurrence rate; (3) the survival outcomes were measured by hazard ratio (HRs) with 95% confidence interval (CIs), Kaplan–Meier curve, or data for calculating HR with its corresponding 95%CI; (4) studies were full text and published in English. The studies would be excluded if they met the following criteria: (1) case reports, reviews, letters, and comments; (2) studies could not provide sufficient data to calculate the HR with 95%CI; (3) researches were not performed on human beings; (4) non-English publications.
2.3. Data extraction
All the studies were carefully reviewed, and data were extracted from each study, including study ID (first author's name and publication year), country, sample size, cancer stage, treatment method, survival outcome, analysis model, data source, and follow-up period by two independent researchers. The inconsistencies between reviewers were resolved by a third investigator through discussion. If studies could only provide Kaplan–Meier curve, the HRs for OS and DFS were extracted from them by using Engauge Digitizer version 4.1 (http://digitizer.sourceforge.net/). In this study, we extracted prognostic data as much as possible both from univariate and multivariate analyses.
2.4. Statistical analysis
In this study, we used STATA version 12.0 (Stata Corporation, Collage Station, TX, USA) to perform meta-analysis. HRs with corresponding 95%CI were used to assess the prognostic value of ALBI on OS and DFS in patients with HCC. The heterogeneity between studies was tested by Cochran's Q and Higgins I2 statistics. If there was no heterogeneity (<50%, P > .1), fixed-effect model would be used. Otherwise, the random-effect model was applied. The high ALBI was closely associated with poor survival outcome when HR > 1. Publication bias was measured by Begg's test and Egger's test with graph. Normally, the result was defined as statistically significant if P < .05. The ALBI score was calculated as log10 bilirubin∗0.66 + albumin∗0.085, and stratified as follows: grade 1: <−2.60; grade 2: −2.60 to −1.39; and grade 3: >−1.39.
This is a systematic review and meta-analysis, which does not need to be approved by the institutional review board or Ethics committee.
3. Results
3.1. Study search
A total of 299 articles were identified after searching four databases (PubMed, EMbase, Web of Science and Cochrane library) and their reference lists. Eight-seven articles remained after duplicates were removed. Then, 45 articles were removed after reading the title and abstract. After reading the full-text articles, those which could not provide HRs with 95%CI (n = 6) and irrelevant topic (n = 4) were extracted. Finally, 32 articles were included in this meta-analysis (Fig. 1).
Figure 1.
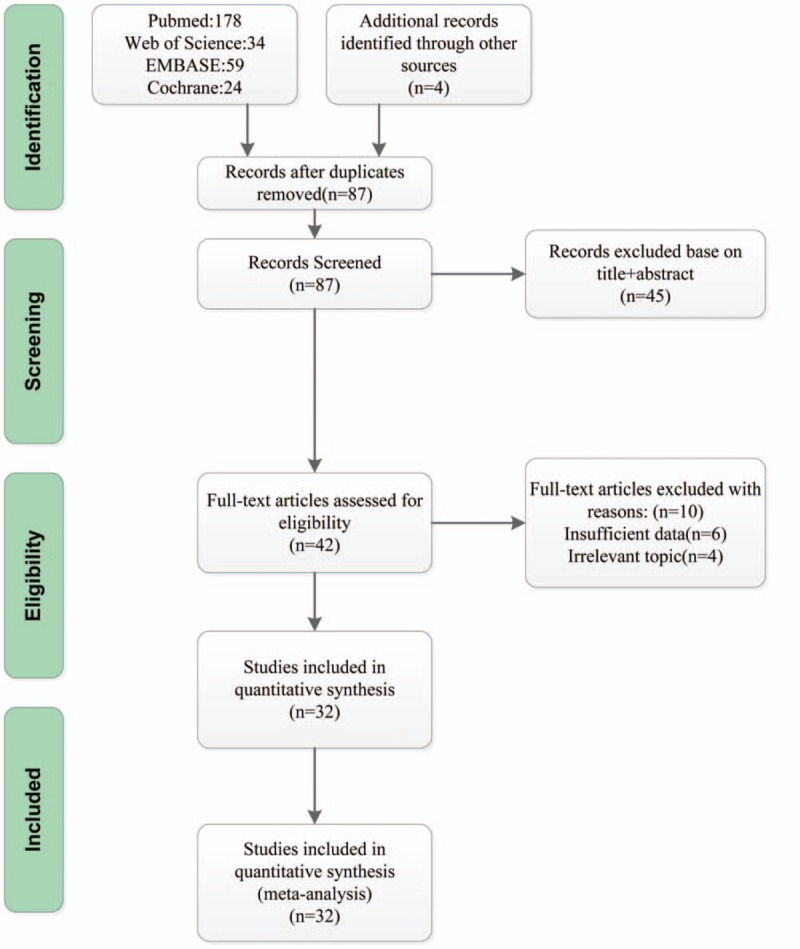
Flow diagram for study selection.
3.2. Cohort characteristics
32 studies were finally included in our analysis.[4–35] The sample size varied from 40 to 3030. With respect to the study region, 15 studies were performed in China, 5 in United Kingdom, 4 in Japan, 3 in Korea, 2 in Canada, 1 in Germany, 1 in Egypt and 1 in United States. The publication date ranged from 2015 to 2018. Twenty-three studies provided overall survival (OS), 2 provided disease-free survival (DFS) and 7 provided both OS and DFS. Other information including cancer stage, treatment method, and follow-up period were presented in Table 1 .
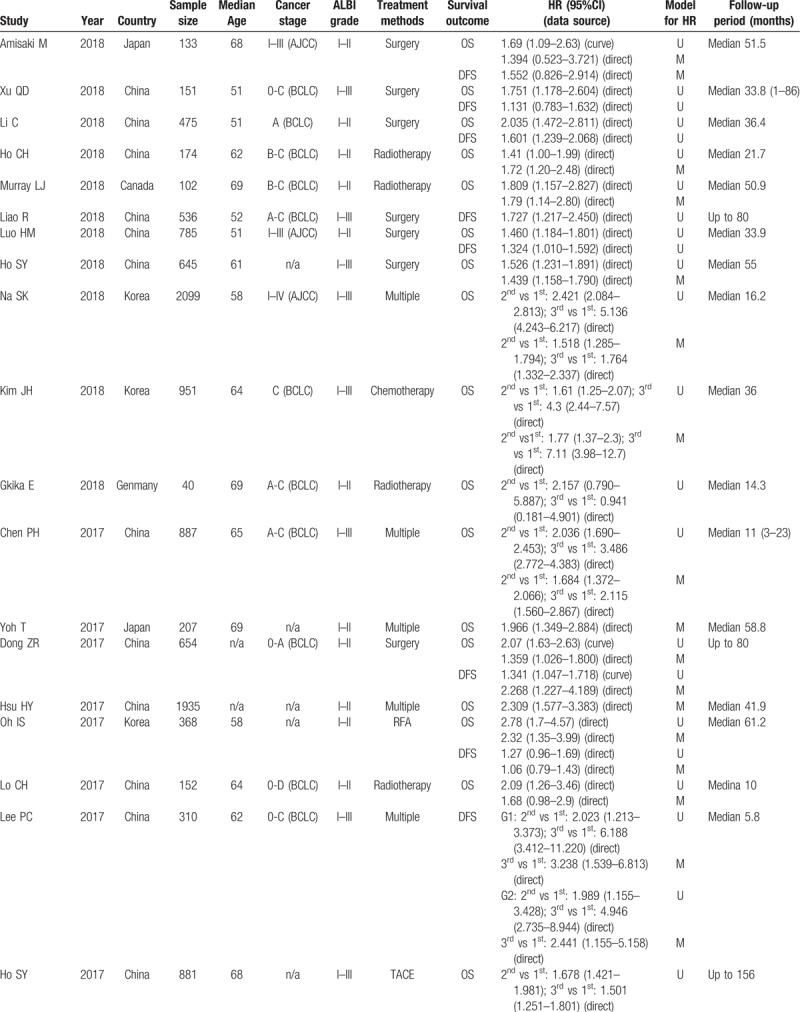
Table 1.
Characteristics of studies included in the analysis.
3.3. Meta-analysis on OS
The prognostic value of ALBI on OS was identified by both univariate and multivariate analyses. Because of the severe heterogeneity (I2 = 83.7%, P = .000), the random-effect model was used. We found that high ALBI grade was associated with poor OS (HR = 2.060, 95%CI: 1.909–2.211, P = .000). Besides, the multivariate analysis group showed similar result (HR = 1.577, 95%CI: 1.464–1.691, P = .000). The fixed-effect model was performed because of the low heterogeneity (I2 = 15.2%, P = .272). These results illustrated that HCC patients with high ALBI grade suffered from poor long-term survival (Fig. 2 A and B).
Figure 2.
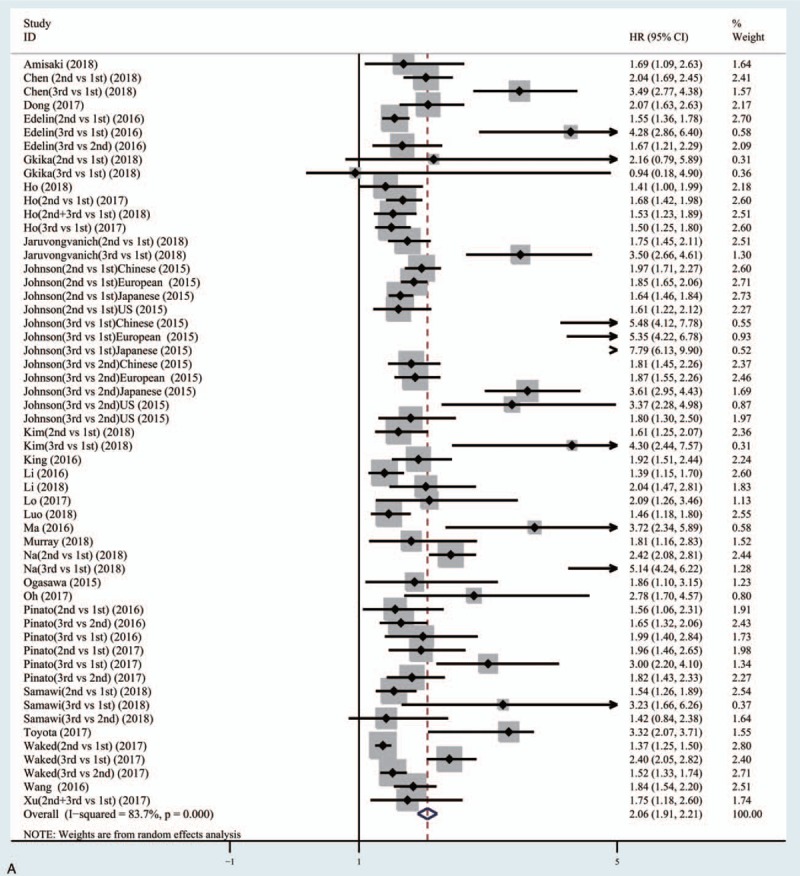
Meta-analysis forest plots for correlation of albumin-to-bilirubin ratio (ALBI) and overall survival (OS) based on univariate analysis results (A) and multivariate analysis results (B).
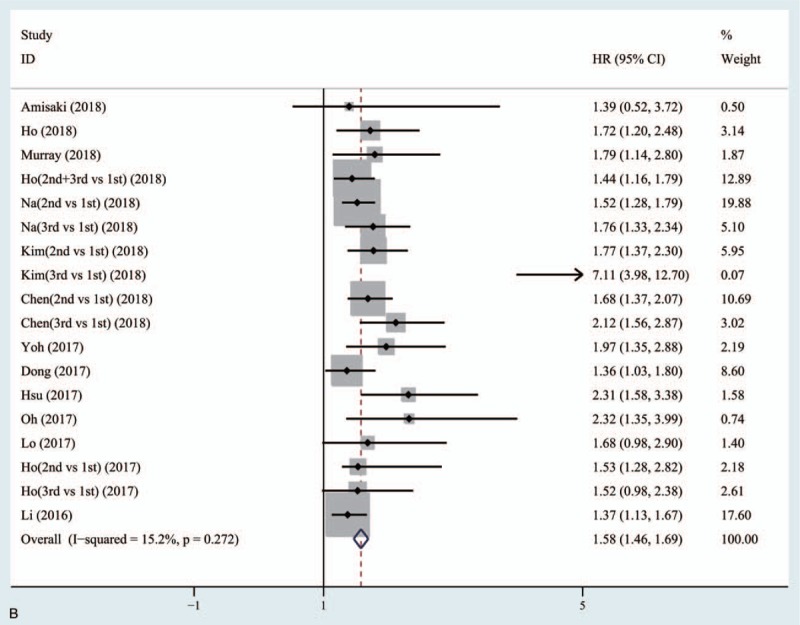
3.4. Meta-analysis on DFS
Nine studies with 4312 HCC patients were included for analysis of disease-free survival (DFS). Due to the low heterogeneity (univariate group: I2 = 49.5%, P = .031; multivariate group: I2 = 31.6%, P = .199), the fixed-effect model was used in both groups. The univariate group (HR = 1.411, 95%CI: 1.262–1.561, P = .000) and multivariate group (HR = 1.264, 95%CI: 1.042–1.485, P = .000) showed that HCC patients with high ALBI grade were closely associated with early tumor recurrence (Fig. 3A and B).
Figure 2 (Continued).
Meta-analysis forest plots for correlation of albumin-to-bilirubin ratio (ALBI) and overall survival (OS) based on univariate analysis results (A) and multivariate analysis results (B).
3.5. Subgroup meta-analysis according to potential confounding factors
We performed subgroup meta-analysis when severe heterogeneity was found in OS univariate analysis group. The OS univariate analysis group was stratified into four parameters, including treatment method, geographic area, sample size, and ALBI grade. The subsequent result (high ALBI grade is associated with poor OS) was not altered (Table 2).
Table 1 (Continued).
Characteristics of studies included in the analysis.
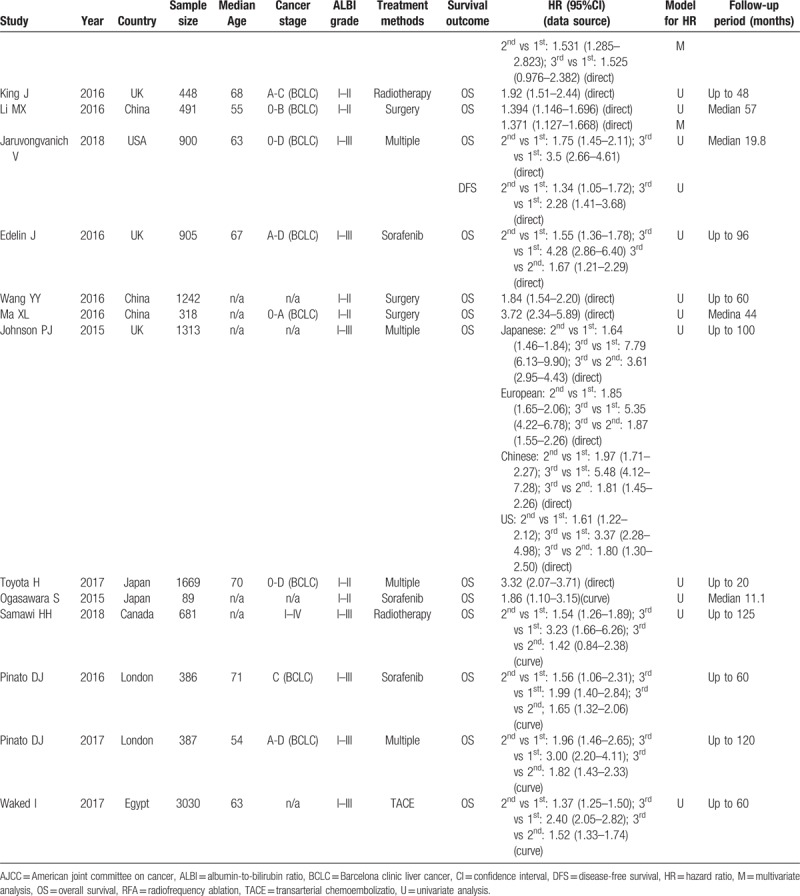
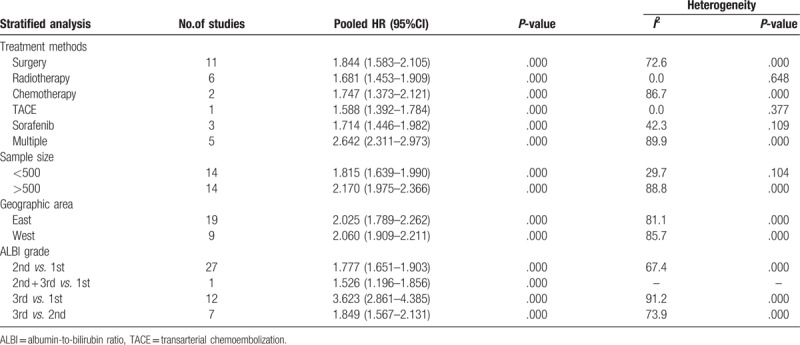
Table 2.
Stratified meta-analysis based on overall survival (OS) univariate analysis.
3.6. Publication bias
Publication bias was confirmed both in OS univariate analysis group (Egger's test P = .015, Begg's test P = .018) and multivariate analysis group (Egger's test P = 0.028, Begg's test P = .081). Because the numbers of articles were <10 in DFS group, the publication bias was not performed (Fig. 4A and B).
Figure 3.
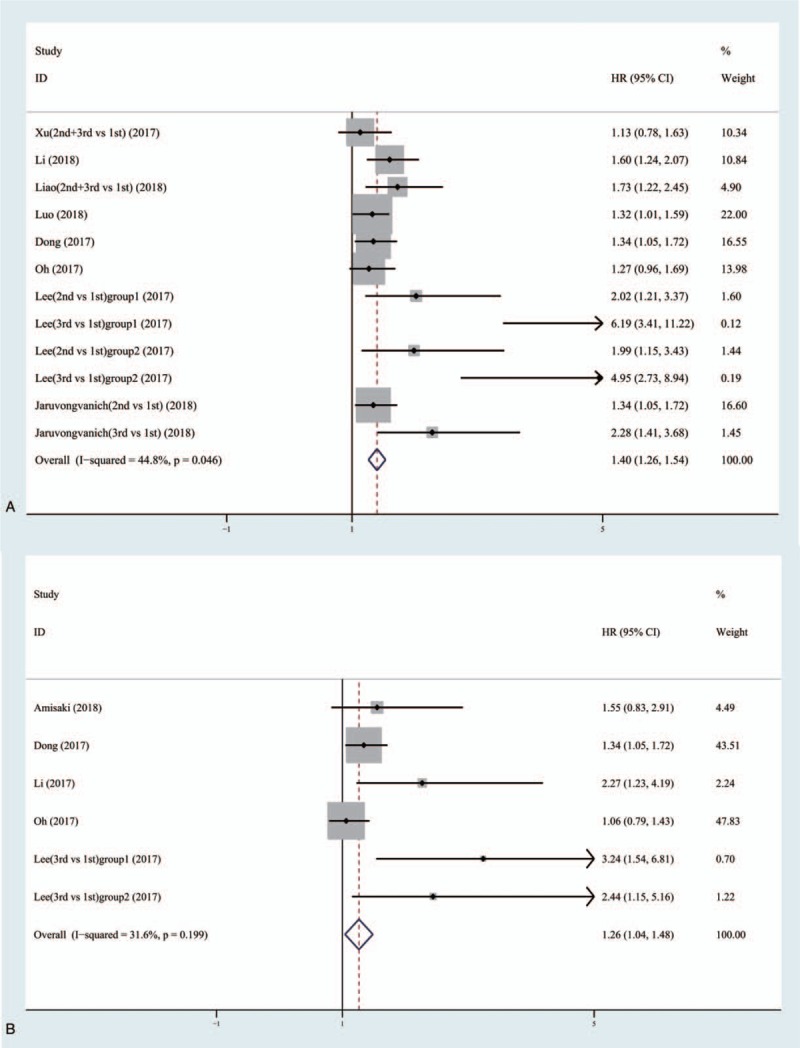
Meta-analysis forest plots for correlation of albumin-to-bilirubin ratio (ALBI) and disease-free survival (DFS) based on univariate analysis results (A) and multivariate analysis results (B).
Figure 4.
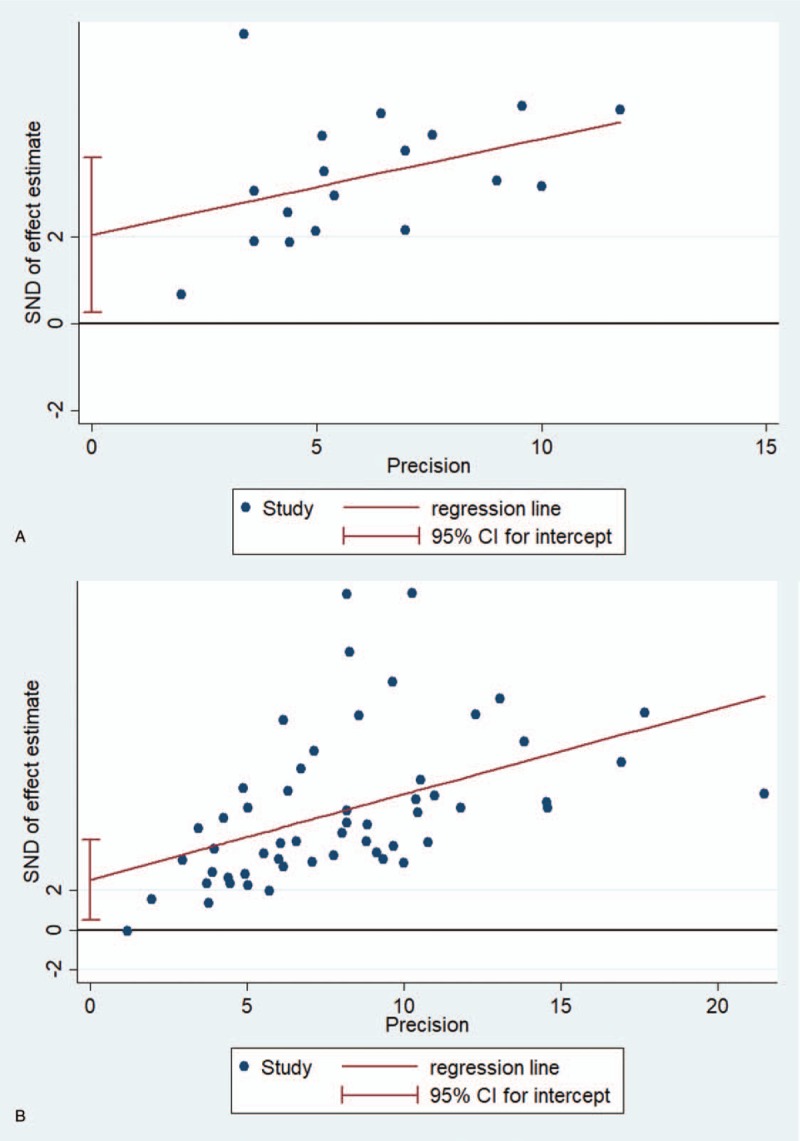
Egger's test for the evaluation of potential publication bias in overall survival (OS) univariate analysis (A) and multivariate analysis (B) groups.
4. Discussion
To the best of our knowledge, this is the first meta-analysis assessing the prognostic value of the ALBI grade in patients with HCC. In this research, 32 studies were conducted to investigate the relationship between ALBI grade and long-term survival in HCC patients. The result consistently indicated that the high ALBI grade was significantly associated with poor survival and early recurrence in patients with HCC.
Hepatic dysfunction was closely associated with high incidence of tumor recurrence and poor long-term survival of patients with HCC.[36] The liver failure rate was about 63.1% in patients with mortality. Those who had cancer progression without hepatic failure account for a minority. The result clearly indicated the importance of hepatic function for the long-term survival of HCC patients. Therefore, various types of tools using to assess hepatic function were proposed to manage treatment of HCC patients.
The Child-Pugh's class was first proposed by Child in 1964. Five parameters of patients, including general condition, ascites, serum bilirubin, serum albumin, and prothrombin time, were divided into three levels scoring 1, 2, and 3, respectively. The hepatic function was divided into three levels (A, B, and C) according to the sum score, which indicated different severity of liver damage. However, the general condition of patients was often difficult to measure, so Pugh proposed to replace the general condition with the presence or absence of hepatic encephalopathy. Finally, the Child-Pugh class, most frequently used in clinic, was formed.
The ALBI grade has been proved to be a simple, evidence-based tool to assess the hepatic function of patients. Compared to the Child-Pugh's class, the ALBI grade only involves two items including albumin and bilirubin (log10bilirubin∗0.66 + albumin∗0.085). As first mentioned by Johnson in 2015,[4] the ALBI grade has been evaluated for long-term survival and disease recurrence in HCC patients in recent years. There are many methods to treat hepatic cancer, including curative resection, chemotherapy, transarterial chemoembolization, and radiotherapy.[6,18,19,30] No matter how treatment methods changed, the ALBI grade system consistently showed significantly prognostic value for OS and DFS in patients with HCC. In the present studies, ALBI grade showed better predicted value and distribution in survival prognosis of patients with HCC than Child-Pugh's class.[22,31] Our research further confirmed that the ALBI was a good alternative grading system to assess the long-term survival and tumor recurrence in patients with HCC.
There are some limitations which should be declared here. First, the HRs with 95%CI were extracted from articles, because the original data were not available. Second, all of the studies conducted were retrospective. Most of them only provided HRs with 95%CI from univariate analysis and some only provide Kaplan–Meier curve. For that, we had to extract the survival data by using the Engauge Digitizer. Due to these, the heterogeneity in OS univariate group was severe. Third, the publication bias was found both in OS univariate and multivariate analyses groups. Only published articles were included in this meta-analysis, which might be partly responsible for that. Finally, the number of articles to assess the prognostic value of DFS was quite few, which may threaten the reliability of pooled results in that regard. Therefore, further investigations were required to confirm the prognostic value of ALBI grade in patients with HCC.
5. Conclusion
This meta-analysis consistently indicated that the high ALBI grade was significantly associated with poor long-term survival and early tumor recurrence in patients with HCC. ALBI grade can be used as a prognostic biomarker in HCC patients in clinical work. However, the large prospective studies should be performed to identify the predict value of the ALBI grade.
Author contributions
Conceptualization: Yixin Xu, Xuezhong Xu.
Validation: Yulin Tan, Yibo Wang.
Writing – original draft: Cheng Xi.
Writing – review & editing: Xuezhong Xu.
Footnotes
Abbreviations: ALBI = albumin-to-bilirubin ratio, CIs = confidence intervals, DFS = disease-free survival, HCC = hepatocellular cancer, HRs = hazard ratio, OS = overall survival.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87–108. [DOI] [PubMed] [Google Scholar]
- [2].Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis 1999;19:329–38. [DOI] [PubMed] [Google Scholar]
- [3].Minguez B, Lachenmayer A. Diagnostic and prognostic molecular markers in hepatocellular carcinoma. Dis Markers 2011;31:181–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Johnson PJ, Berhane S, Kagebayashi C, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol 2015;33:550–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Xu Q, Yan Y, Gu S, et al. A novel inflammation-based prognostic score: the fibrinogen/albumin ratio predicts prognoses of patients after curative resection for hepatocellular carcinoma. J Immunol Res 2018;2018:4925498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Gkika E, Bettinger D, Krafft L, et al. The role of albumin-bilirubin grade and inflammation-based index in patients with hepatocellular carcinoma treated with stereotactic body radiotherapy. Strahlenther Onkol 2018;194:403–13. [DOI] [PubMed] [Google Scholar]
- [7].Waked I, Berhane S, Toyoda H, et al. Transarterial chemo-embolisation of hepatocellular carcinoma: impact of liver function and vascular invasion. Br J Cancer 2017;116:448–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Samawi HH, Sim HW, Chan KK, et al. Prognosis of patients with hepatocellular carcinoma treated with sorafenib: a comparison of five models in a large Canadian database. Cancer Med 2018;DOI 10.1002/cam4.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Kim JH, Sinn DH, Lee JH, et al. Novel albumin-bilirubin grade-based risk prediction model for patients with hepatocellular carcinoma undergoing chemoembolization. Dig Dis Sci 2018;63:1062–71. [DOI] [PubMed] [Google Scholar]
- [10].Chen PH, Hsieh WY, Su CW, et al. Combination of albumin-bilirubin grade and platelets to predict a compensated patient with hepatocellular carcinoma who does not require endoscopic screening for esophageal varices. Gastrointest Endosc 2018;88:230–9. e232. [DOI] [PubMed] [Google Scholar]
- [11].Yoh T, Seo S, Ogiso S, et al. Proposal of a new preoperative prognostic model for solitary hepatocellular carcinoma incorporating (18)F-FDG-PET imaging with the ALBI grade. Ann Surg Oncol 2018;25:542–9. [DOI] [PubMed] [Google Scholar]
- [12].Dong ZR, Zou J, Sun D, et al. Preoperative albumin-bilirubin score for postoperative solitary hepatocellular carcinoma within the milan criteria and Child-Pugh A cirrhosis. J Cancer 2017;8:3862–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Amisaki M, Uchinaka E, Morimoto M, et al. Post-operative albumin-bilirubin grade predicts long-term outcomes among Child-Pugh grade A patients with hepatocellular carcinoma after curative resection. Hepatobiliary Pancreat Dis Int 2018;17:502–9. [DOI] [PubMed] [Google Scholar]
- [14].Hsu HY, Yu MC, Lee CW, et al. RAM score is an effective predictor for early mortality and recurrence after hepatectomy for hepatocellular carcinoma. BMC Cancer 2017;17:742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Oh IS, Sinn DH, Kang TW, et al. Liver Function Assessment Using Albumin-Bilirubin Grade for Patients with Very Early-Stage Hepatocellular Carcinoma Treated with Radiofrequency Ablation. Dig Dis Sci 2017;62:3235–42. [DOI] [PubMed] [Google Scholar]
- [16].Lo CH, Liu MY, Lee MS, et al. Comparison between Child-Turcotte-Pugh and Albumin-Bilirubin scores in assessing the prognosis of hepatocellular carcinoma after stereotactic ablative radiation therapy. Int J Radiat Oncol Biol Phys 2017;99:145–52. [DOI] [PubMed] [Google Scholar]
- [17].Lee PC, Chen YT, Chao Y, et al. Validation of the albumin-bilirubin grade-based integrated model as a predictor for sorafenib-failed hepatocellular carcinoma. Liver Int 2018;38:321–30. [DOI] [PubMed] [Google Scholar]
- [18].Ho SY, Liu PH, Hsu CY, et al. Prognostic role of noninvasive liver reserve markers in patients with hepatocellular carcinoma undergoing transarterial chemoembolization. PLoS One 2017;12:e0180408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].King J, Palmer DH, Johnson P, et al. Sorafenib for the Treatment of Advanced Hepatocellular Cancer - a UK Audit. Clin Oncol (R Coll Radiol) 2017;29:256–62. [DOI] [PubMed] [Google Scholar]
- [20].Li MX, Zhao H, Bi XY, et al. Prognostic value of the albumin-bilirubin grade in patients with hepatocellular carcinoma: validation in a Chinese cohort. Hepatol Res 2017;47:731–41. [DOI] [PubMed] [Google Scholar]
- [21].Jaruvongvanich V, Sempokuya T, Wong L. Is there an optimal staging system or liver reserve model that can predict outcome in hepatocellular carcinoma? J Gastrointest Oncol 2018;9:750–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Wang YY, Zhong JH, Su ZY, et al. Albumin-bilirubin versus Child-Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br J Surg 2016;103:725–34. [DOI] [PubMed] [Google Scholar]
- [23].Ma XL, Zhou JY, Gao XH, et al. Application of the albumin-bilirubin grade for predicting prognosis after curative resection of patients with early-stage hepatocellular carcinoma. Clin Chim Acta 2016;462:15–22. [DOI] [PubMed] [Google Scholar]
- [24].Toyoda H, Kumada T, Tada T, et al. Differences in the impact of prognostic factors for hepatocellular carcinoma over time. Cancer Sci 2017;108:2438–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Li C, Zhang XY, Peng W, et al. Preoperative albumin-bilirubin grade plus platelet-to-lymphocyte ratio predict the outcomes of patients with BCLC stage A hepatocellular carcinoma after liver resection. Medicine (Baltimore) 2018;97:e11599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Pinato DJ, Sharma R, Citti C, et al. The albumin-bilirubin grade uncovers the prognostic relationship between hepatic reserve and immune dysfunction in HIV-associated hepatocellular carcinoma. Aliment Pharmacol Ther 2018;47:95–103. [DOI] [PubMed] [Google Scholar]
- [27].Murray LJ, Sykes J, Brierley J, et al. Baseline Albumin-Bilirubin (ALBI) score in western patients with hepatocellular carcinoma treated with stereotactic body radiation therapy (SBRT). Int J Radiat Oncol Biol Phys 2018;101:900–9. [DOI] [PubMed] [Google Scholar]
- [28].Liao R, Li DW, Du CY, et al. Combined preoperative ALBI and FIB-4 is associated with recurrence of hepatocellular carcinoma after curative hepatectomy. J Gastrointest Surg 2018;22:1679–87. [DOI] [PubMed] [Google Scholar]
- [29].Luo HM, Zhao SZ, Li C, et al. Preoperative platelet-albumin-bilirubin grades predict the prognosis of patients with hepatitis B virus-related hepatocellular carcinoma after liver resection: A retrospective study. Medicine (Baltimore) 2018;97:e0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Ho SY, Liu PH, Hsu CY, et al. Comparison of twelve liver functional reserve models for outcome prediction in patients with hepatocellular carcinoma undergoing surgical resection. Sci Rep 2018;8:4773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Na SK, Yim SY, Suh SJ, et al. ALBI versus Child-Pugh grading systems for liver function in patients with hepatocellular carcinoma. J Surg Oncol 2018;117:912–21. [DOI] [PubMed] [Google Scholar]
- [32].Edeline J, Blanc JF, Johnson P, et al. A multicentre comparison between Child Pugh and Albumin-Bilirubin scores in patients treated with sorafenib for Hepatocellular Carcinoma. Liver Int 2016;36:1821–8. [DOI] [PubMed] [Google Scholar]
- [33].Ogasawara S, Chiba T, Ooka Y, et al. Liver function assessment according to the Albumin-Bilirubin (ALBI) grade in sorafenib-treated patients with advanced hepatocellular carcinoma. Invest New Drugs 2015;33:1257–62. [DOI] [PubMed] [Google Scholar]
- [34].Pinato DJ, Yen C, Bettinger D, et al. The albumin-bilirubin grade improves hepatic reserve estimation post-sorafenib failure: implications for drug development. Aliment Pharmacol Ther 2017;45:714–22. [DOI] [PubMed] [Google Scholar]
- [35].Ho CHM, Chiang CL, Lee FAS, et al. Comparison of platelet-albumin-bilirubin (PALBI), albumin-bilirubin (ALBI), and child-pugh (CP) score for predicting of survival in advanced hcc patients receiving radiotherapy (RT). Oncotarget 2018;9:28818–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Toyoda H, Lai PB, O’Beirne J, et al. Long-term impact of liver function on curative therapy for hepatocellular carcinoma: application of the ALBI grade. Br J Cancer 2016;114:744–50. [DOI] [PMC free article] [PubMed] [Google Scholar]


