Abstract
An adequate stable fixation implant should be used for medial opening-wedge high tibial osteotomy (MOWHTO) to promote rapid bone healing without complications. To date, the highest fixation stability has been observed for angular stable locking plates. However, there is still little medical literature regarding breakage of these plates. The purpose of the present study was to report the results of plate breakage around D-hole with the use of both types of locking plate fixation for MOWHTO.
Medical records of 12 patients who experienced plate breakage after MOWHTO with either a TomoFix or OhtoFix plate between August 2013 and August 2016 were retrospectively reviewed.
A total of 12 patients (7 males and 5 females) who experienced plate breakage at the screw hole just above the osteotomy were evaluated (age, 63 ± 8 years; body mass index (BMI), 28 ± 2 kg/m2; opening gap height, 12 ± 2 mm). There were 9 patients (75%) with plate breakage and loss of correction necessitating revision surgery, and 11 patients (92%) had lateral cortical hinge fractures postoperatively. Of the 9 patients with loss of correction necessitating revision surgery, 4 had a TomoFix plate and 5 had an OhtoFix plate. The only statistically significant association with broken plates lost reduction was the presence of lateral cortical hinge fractures (P = .003), but there was no significant association with age, gender, BMI, diabetes, smoking, plate type, opening gap height, and material used to fill the wedge. In addition, mean knee society score in the 12 patients was significantly higher postoperatively than preoperatively (P < .001).
Since the amount of plate breakage was just over 1% and with only 12 in total, no true conclusion can be made with certainty. However, in the face of no lateral hinge or cortical disruption, there is a 99% success rate with the plate described. If the lateral hinge is disrupted, a restriction of activity or weight bearing may be needed.
Keywords: complications, high tibial osteotomy, locking plate, open wedge
1. Introduction
High tibial osteotomy (HTO) is a well-established procedure used to treat medial compartment knee osteoarthritis (OA). An adequate stable fixation implant is necessary for medial opening-wedge HTO (MOWHTO) to promote rapid bone healing without complications because the medial opening creates an extremely unstable condition in the proximal tibia.[1] Although several fixatives have been used for MOWHTO, including a combination of short or long, locked or unlocked, and with or without a metal block, the highest fixation stability has been observed for angular stable locking plates.[2] Previous studies described several concerns regarding TomoFix plates (Synthes, Oberdorf, Switzerland), such as local irritation and no purchase of D-hole which means the most distal screw hole of proximal screw holes due to the relatively large plate profile.[3,4] A new implant with an improved design, OhtoFix (Ohtomedical, Goyang, Korea), was developed to address some of these challenges for Asian patients. Biomechanical studies on both plates in a single load to failure test have shown that the ultimate failure load for the TomoFix plate and the OhtoFix plate was close to the axial compressive force of an adult tibiofemoral joint during level walking.[5,6] However, it remains unclear whether the biomechanical superiority of both plates over the axial compressive load applied in adult knees leads to greater knee stability in the clinical setting. To date, there is still little medical literature regarding breakage of both plates. The present study was designed to report the results of plate breakage around D-hole with the use of both types of locking plate fixation for MOWHTO in a series of patients. The major predictor for plate breakage was hypothesized to be associated with the presence of lateral cortical hinge fractures in these patients.
2. Materials and methods
2.1. Materials
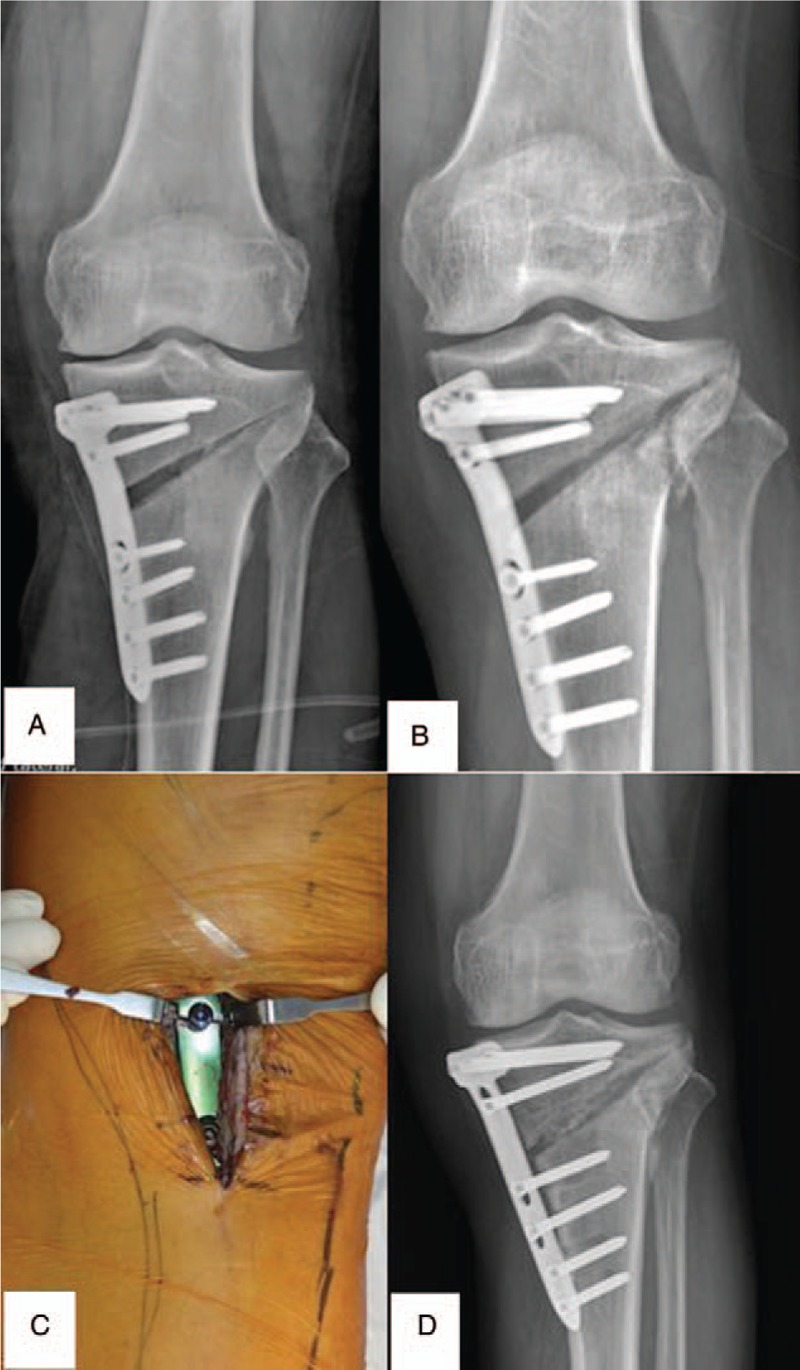
In this retrospective analysis of a multicenter case series involving 3 high-volume surgical centers, medical records for 971 patients with various deformity and OA of the medial knee joint compartment who received MOWHTO with either TomoFix or OhtoFix plates between August 2013 and August 2016 were reviewed to identify the occurrence of 12 patients who experienced plate breakage. Patients considered ineligible for MOWHTO with fixation by 1 of the 2 plates included those with diagnosis of symptomatic OA of the patellofemoral joint and lateral compartment, rheumatoid arthritis, and high-grade ligamentous laxity. However, we included all patients who received MOWHTO using 2 long rigid plates without age restriction because the indication of MOWHTO should not be merely patient age, but also the status of OA in other compartments and on additional ligamentous instability. Data was transcribed into study-specific paper case report forms. Copies of case report forms were transferred to our institution for processing and data entry. Demographic characteristics including age, gender, body mass index (BMI), diabetes, smoking, plate type, lateral cortical hinge fractures, opening gap height, and material used to fill the wedge are summarized in Table 1. Because this was a retrospective study using only medical records and radiographic data for anonymous patients who had already undergone treatment, it was not possible to obtain informed consent at the time of the study. Thus, the need for informed consent was waived. This study was approved by the institutional review board.
Table 1.
Baseline characteristics included in this study.
2.2. Surgical protocols and clinical settings
Three surgeons, 1 from each institution, were involved in the surgeries. All 3 had more than 8 years of clinical experience as specialists in MOWHTO surgery. The surgical techniques and protocols are described below.
The incision was placed longitudinally on the medial aspect of the proximal tibia. Subperiosteal dissection was performed and followed by partial stripping of the pes anserinus and the superficial medial collateral ligament to create a space for the osteotomy plate. Two guide wires were positioned parallel to the tibial slope at different points below the medial joint line towards the upper part of the fibular head (safe zone)[7] in an oblique manner under fluoroscopic control. When satisfactorily positioned, the osteotomy was performed using an oscillating saw, a 3-coupled osteotome, and a thin osteotome to a distance of up to 1 cm from the lateral cortex, maintaining the lateral cortical hinge. The osteotomy was gradually widened until the weight-bearing line (WBL) passed through the lateral aspect of the lateral tibial spine using the cable method. The WBL was defined as a line drawn from the center of the femoral head to the center of the superior articular surface of the talus. To maintain posterior tibial slope, the anterior gap of the osteotomy was created at approximately two-thirds of the posterior opening gap at the posteromedial corner of the proximal tibia. The osteotomy was stabilized using both plates with 4 screws placed proximally and 4 screws placed distally without a wedge block while the correction was retained with a laminar bone spreader. If the level of osteotomy is directed toward proximal to the fibular head, we performed the necessary steps to compress the lateral cortical hinge. After osteotomy stability was confirmed, a porous β-tricalcium phosphate bone substitute was inserted into the gaps (>12 mm) to minimize postoperative loss of correction. The same postoperative rehabilitation regimen was used in 12 patients and consisted of partial weight bearing until 4 to 6 weeks after surgery. After 4 to 6 weeks and radiographic control, full weight bearing was achieved.[8]
2.3. Radiographic evaluation
Postoperative radiographs and 3-dimensional computed tomography (3D CT) scanning were analyzed for the presence of lateral cortical hinge fractures. Postoperative multislice CT scanning (Brilliance 64, Phillips, Cleveland, OH) was conducted using 5 mm coronal, 5 mm sagittal, and 3 mm axial slices of the knee, proximal femur, and distal tibia 1 week after surgery. Two experienced orthopedic surgeons using a picture archiving and communication system (PI View STAR version 5025; Infinitt, Seoul, Korea) evaluated the presence of lateral cortical hinge fractures in all 12 patients twice, with a 2-week interval between measurements.
2.4. Statistical analyses
Statistical analyses were performed using SPSS statistical software version 20 (IBM Corp., Armonk, NY). Chi-square, Fisher exact test and odds ratio (OR) with 95% confidence intervals (CI) were used in univariate analysis to assess individual effects of plate breakage. Multiple logistic regression analysis was performed using the backward stepwise method with criterion for entry set at P-value < .05 and criterion for removal set at P-value > .10. All variables with a P-value < .05 on univariate analysis were used to identify the independent factors related to plate breakage, controlling for age and gender. The reliability of measuring the presence of lateral cortex fractures was determined by calculating the intraclass correlation coefficient (ICC) and the standard error of measurement, with ICC values >0.75, 0.4 to 0.75, and <0.4 representing good, fair, and poor reliability/accuracy, respectively. At an alpha level of 0.05 and a power of 0.8, we conducted a post hoc power analysis to detect a mean difference of 5 points for knee society score (KSS) from before to after surgery. This study included 12 patients, with adequate power, to detect significant differences in KSS (0.806) from before to after surgery.
3. Results
From the initial 971 patients, 12 patients met the inclusion/ exclusion criteria and were used in the study. The proportion of knees with plate breakage showed similar findings for the 3 institutions (5/370 vs 4/348 vs 3/253).
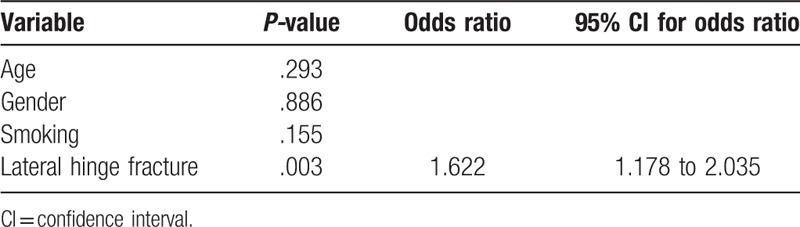
The intra- and inter-observer reliabilities of the presence of lateral cortical hinge fractures ranged from 0.755 to 0.848 and from 0.749 to 0.841, respectively. Mean KSS in the 12 patients was significantly higher postoperatively than preoperatively (92 ± 4 vs 55 ± 7, P < .001). A total of 12 patients (7 males and 5 females) who experienced plate breakage at the screw hole just above the osteotomy were evaluated (age, 63 ± 8 years; BMI, 28 ± 2 kg/m2; opening gap height, 12 ± 2 mm). Nine patients (75%) experienced plate breakage with loss of correction necessitating revision surgery, and 11 patients (92%) experienced lateral cortical hinge fractures postoperatively. Of the 9 patients with loss of correction necessitating revision surgery, 4 had a TomoFix plate (Fig. 1A–D) and 5 had an OhtoFix plate (Fig. 2A–D). Univariate analyses were used to assess the individual effects of plate breakage. Age (P = .063), gender (P = .735), BMI (P = .479), diabetes (P = .735), plate type (P = .263), opening gap height (P = .588), and material used to fill the wedge (P = .735) did not have statistically significant associations. However, statistically significant differences were observed for smoking (P = .046) and the presence of lateral cortical hinge fractures (P = .007) (Table 2). Multiple logistic regression analyses were performed to identify independent factors related to plate breakage. All variables with P < .05 on univariate analysis indicated that the presence of lateral cortical hinge fractures was the major predictor of plate breakage (OR = 1.622; 95% CI, 1.178–2.035; P = .003) (Table 3).
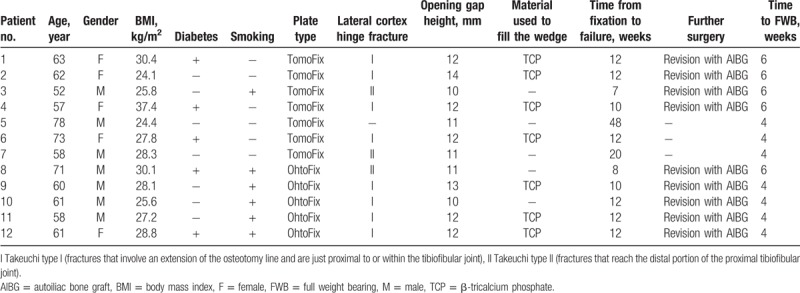
Figure 1.
A–D. 52-year-old man (Case 3; Table 1) (A) TomoFix plate breakage around the D-hole on anteroposterior radiograph 7 weeks postoperatively. (B) A postoperative 3D computed tomography scan showing the existence of a lateral cortical hinge fracture (type II). (C) Intraoperative views showing the TomoFix plate breakage around the D-hole. (D) Revision surgery successfully carried out with TomoFix plate and autoiliac bone graft 10 weeks after the primary intervention.
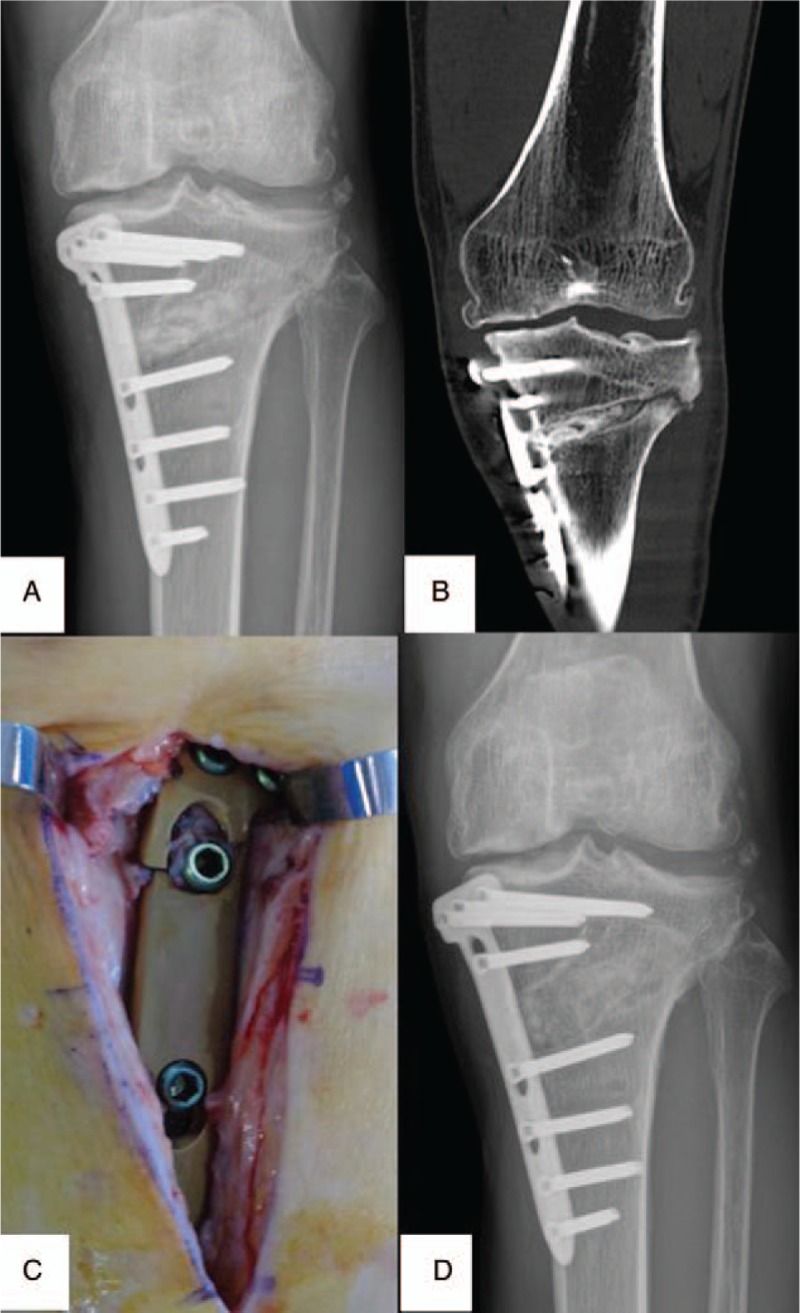
Figure 2.
A–D. Plain radiographs of Case 8 (Table 1) showing (A) the immediate postoperative film and (B) OhtoFix plate breakage around the D-hole and the existence of a lateral cortical hinge fracture (type II) on anteroposterior radiograph 12 weeks postoperatively. (C) Intraoperative views showing the OhtoFix plate breakage around the D-hole. (D) Revision surgery successfully carried out with TomoFix plate and autoiliac bone graft 13 weeks after the primary intervention.
Table 2.
Univariate comparison between no revision group and revision group.
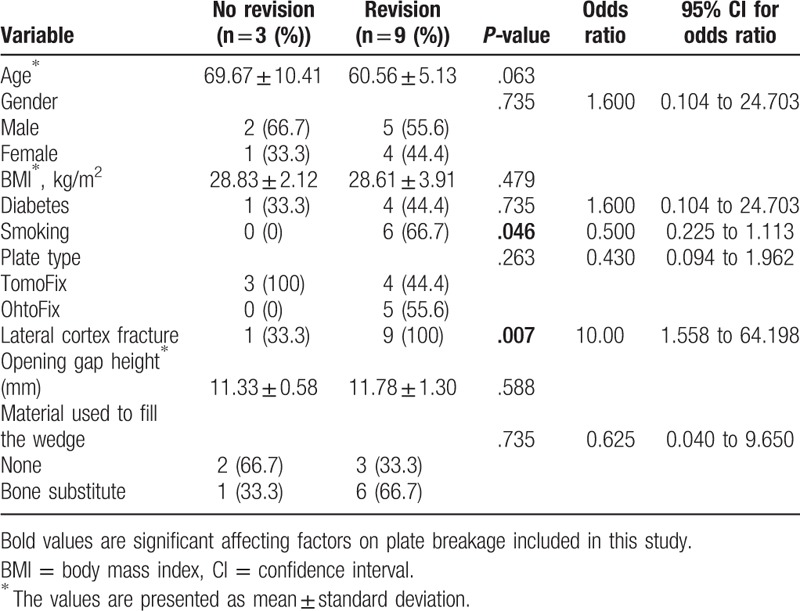
Table 3.
Independent factors related to breakage of the plate.
4. Discussion
This retrospective case series of 12 patients demonstrated plate breakage at the screw hole just above the osteotomy after MOWHTO with either TomoFix or OhtoFix plates, 9 by plate breakage with loss of correction requiring revision surgery and 3 by plate breakage. Furthermore, the major predictor of plate breakage in these patients was associated with the presence of lateral cortical hinge fractures, confirming our hypotheses.
Achieving stable fixation in MOWHTO is important to avoid adverse events including nonunion and even plate breakage, especially for early full weight bearing in young and active patients.[9] Unfortunately, not all patients who underwent placement of angular stable locking plates experienced good fixation stability, even though these plates were shown to offer superior stability under both compression and torsion compared to nonlocking plates.[10] Two sets of factors may be related to complications such as nonunion and plate breakage after MOWHTO. One set is inevitable or difficult to protect and is not associated with the surgical technique, whereas the other can be reduced by an effective surgical procedure. The former factors have been associated with patients, suggesting that smoking and diabetes are considered a relative contraindication for MOWHTO and negatively influence the results of MOWHTO. One study that evaluated rates of adverse events in MOWHTO classified adverse events into different grades of severity by comparing patient-reported outcomes in 323 patients. That study showed that active smokers had a higher rate of nonunion (4.8%) than ex-smokers (4.3%) and non-smokers (2.4%) while diabetic patients had a higher rate of nonunion (16.6%) compared with non-diabetic patients (2.6%).[11] Although the age of the patient has to be taken into consideration for MOWHTO, previous studies have not identified increased risk of failure events due to reductions in the former type of fixators or lateral closing-wedge HTO independent of the patient age.[12,13] Furthermore, the indication of MOWHTO should not be merely patient age, but also the status of OA in other compartments and on additional ligamentous instability. It is possible that surgical technique is the most likely culprit and that lateral cortical hinge fracture is a surrogate. For example, we performed our osteotomy proximal to the fibular head, as illustrated in Figure 2, and therefore the lateral cortical hinge is not stabilized by the ligaments of the proximal tibiofibular joint, which is important when there is a lateral cortical hinge fracture. In other words, an adequate surgical procedure, such as lateral cortex preservation may be more likely to improve fixation stability.[14] Previous studies have reported that the risk of lateral cortical hinge fractures in MOWHTO is as high as 90% when the correcting angle is higher than 8° because of the limited plasticity of cortical bone.[15] This situation may contribute to increased micromotion at the osteotomy site, subsequently leading to loss of correction, nonunion, and plate breakage if unrecognized or unaddressed, although the appearance of osseous consolidation would differ according to fracture type.[16,17] The present study simultaneously analyzed the clinical predictors for plate breakage. The variables examined were age, gender, BMI, diabetes, smoking, plate type, lateral cortical hinge fractures, opening gap height, and material used to fill the wedge. Multiple logistic regression analyses and concomitant controlling of relationships among independent predictors were used. Lateral cortical hinge fractures were significantly correlated with plate breakage.
A recent biomechanical study showed that high locking plate stiffness prevented sufficient micromotion to stimulate new bone formation in the osteotomy adjacent to the plate.[18] However, the current clinical results suggest that these laboratory observations do not translate to observations of persistent instability at the osteotomy site. A cadaver study showed that relatively high stiffness linked to locking plates may not offer the motion needed to obtain adequate callus formation for physiologic healing, which can lead to nonunion and plate breakage.[19] These results were consistent with those of a previous study showing that 64 consecutive patients with distal femur fractures stabilized with locking plates had inconsistent and asymmetric callus formation, which may be attributable to the high stiffness of the locking plates.[20] Nevertheless, controlled micromotion may not necessarily enhance homogenous distribution of callus formation because the medial opening creates an extremely unstable condition at the osteotomy site when the lateral cortical hinge is disrupted.[1] The discrepancy between the present study and previous studies may be attributable in part to axial and torsional stiffness reductions by 58% and 68%, respectively, when the lateral hinge is disrupted in MOWHTO.[15] Therefore, the biomechanical advantages of lower stiffness in locking plates may only be present under these compressive loading test conditions. This was supported by the results of a biomechanical study in which the wedge micromotions of 1-leg plate systems were significantly greater than those of 2-leg plate systems, with bone-screw loosening and construct instability.[21]
Decreased support in the lateral hinge area is a precursor for the loss of correction that may lead to plate breakage after MOWHTO. Various efforts have been made to obtain secure fixation stability with lateral cortical hinge fractures, including proper plate fitting to the bony surface and proper screw insertion from the central area of the medial side to the hinge area of the lateral side in the proximal fragment. However, these ideal situations are not common in clinical settings because several anatomical changes may occur depending on patients and the degree of correction.[5,22] The current results suggest that, clinically, care should be made to avoid a cortical hinge fracture of the MOWHTO because this can lead to increase in plate breakage and reinforcement of the predicted stress concentration area in 2 plates may have advantages during MOWHTO. This includes increasing plate thickness and width around the D-hole (Fig. 3A and B), similar to findings of the second-generation Puddu plate, which was 0.5 mm thicker. In addition, maximum stresses appeared at the screw hole just above the osteotomy in the inner side of the TomoFix plate with bone grafts.[23]
Figure 3.
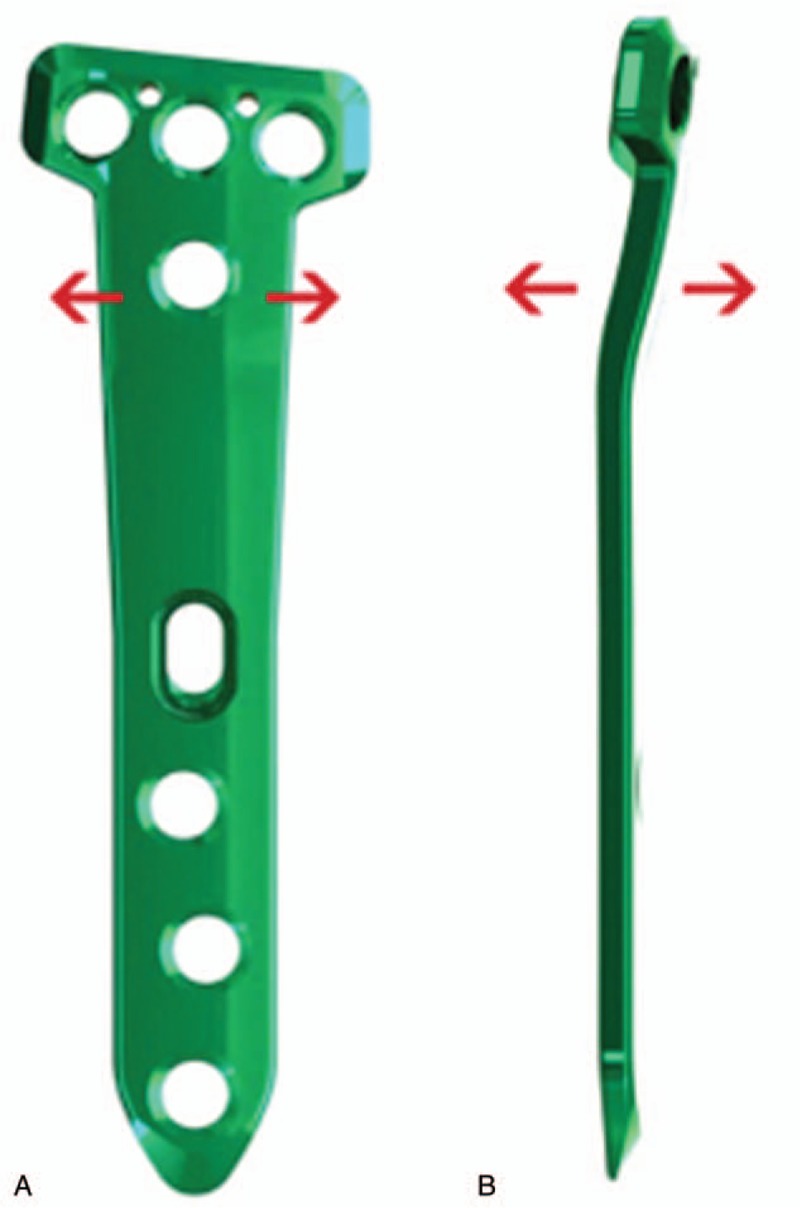
(A) and (B) OhtoFix plate modifications show increasing plate thickness and width around the D-hole.
We acknowledge the limitations of this study, as it is retrospective; however, relatively rare events such as breakage of angular stable locking plates after MOWHTO are difficult to study in prospective analyses and are often suitable for retrospective manner. Second, we also did not compare the locking plates examined in this study to other plate options, such as a combination of short or long, locked or unlocked, and with or without a metal block during MOWHTO. Therefore, future randomized trials are required to definitively assess the efficacy and safety of the 2 locking plate types. Third, we could not include information on the number of overall cases in which aspect failures differed from successful treatment owing to the limited data reported from the 3 different hospitals. Finally, multisurgeon and multicenter design may introduce heterogeneity or bias in determining which patients were deemed potentially lateral cortical hinge fractures. However, high-volume surgeons with substantial experience managing complications after MOWHTO cared for the majority of these patients, resulting in mitigating single surgeon or institution biases.
5. Conclusions
Since the amount of plate breakage was just over 1% and with only 12 in total, no true conclusion can be made with certainty. However, in the face of no lateral hinge or cortical disruption, there is a 99% success rate with the plate described. If the lateral hinge is disrupted, a restriction of activity or weight bearing may be needed to avoid the risk of plate breakage.
Author contributions
Conceptualization: Kyung-Wook Nha, Young-Soo Shin.
Investigation: Kyung-Wook Nha, Young-Soo Shin.
Resources: Kyung-Wook Nha, Woon-Hwa Jung, Young-Gon Koh, Young-Soo Shin.
Visualization: Kyung-Wook Nha, Young-Soo Shin.
Data curation: Woon-Hwa Jung, Young-Gon Koh, Young-Soo Shin.
Formal analysis: Young-Soo Shin.
Methodology: Young-Soo Shin.
Supervision: Young-Soo Shin.
Validation: Young-Soo Shin.
Writing – original draft: Young-Soo Shin.
Writing – review and editing: Young-Soo Shin.
Young-Soo Shin orcid: 0000-0003-1030-9979.
Footnotes
Abbreviations: BMI = body mass index, KSS = knee society score, MOWHTO = medial opening-wedge high tibial osteotomy.
Research of this study was performed at Veterans Health Service Medical Center.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article, nor have any funds been received in support of this study.
There are no conflicts of interest between any of the contributors to this manuscript.
References
- [1].Shin YS, Kim KH, Sim HB, et al. Comparison between two angular stable locking plates for medial opening-wedge high tibial osteotomy: decisive wedge locking plate versus TomoFix™. J Orthop Sci 2016;21:791–7. [DOI] [PubMed] [Google Scholar]
- [2].Chae DJ, Shetty GM, Lee DB, et al. Tibial slope and patellar height after opening wedge high tibia osteotomy using autologous tricortical iliac bone graft. Knee 2008;15:128–33. [DOI] [PubMed] [Google Scholar]
- [3].Jung WH, Chun CW, Lee JH, et al. Comparative study of medial opening-wedge high tibial osteotomy using 2 different implants. Arthroscopy 2013;29:1063–71. [DOI] [PubMed] [Google Scholar]
- [4].Valkering KP, van den Bekerom MP, Kappelhoff FM, et al. Complications after tomofix medial opening wedge high tibial osteotomy. J Knee Surg 2009;22:218–25. [DOI] [PubMed] [Google Scholar]
- [5].Han SB, Bae JH, Lee SJ, et al. Biomechanical properties of a new anatomical locking metal block plate for opening wedge high tibial osteotomy: uniplane osteotomy. Knee Surg Relat Res 2014;26:155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Agneskirchner JD, Freiling D, Hurschler C, et al. Primary stability of four different implants for opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2006;14:291–300. [DOI] [PubMed] [Google Scholar]
- [7].Han SB, Lee DH, Shetty GM, et al. A “safe zone” in medial open-wedge high tibia osteotomy to prevent lateral cortex fracture. Knee Surg Sports Traumatol Arthrosc 2013;21:90–5. [DOI] [PubMed] [Google Scholar]
- [8].Brinkman JM, Lobenhoffer P, Agneskirchner JD, et al. Osteotomies around the knee: patient selection, stability of fixation and bone healing in high tibial osteotomies. J Bone Joint Surg Br 2008;90:1548–57. [DOI] [PubMed] [Google Scholar]
- [9].Noyes FR, Mayfield W, Barber-Westin SD, et al. Opening wedge high tibial osteotomy: an operative technique and rehabilitation program to decrease complications and promote early union and function. Am J Sports Med 2006;34:1262–73. [DOI] [PubMed] [Google Scholar]
- [10].Stoffel K, Stachowiak G, Kuster M. Open wedge high tibial osteotomy: biomechanical investigation of the modified Arthrex Osteotomy Plate (Puddu Plate) and the TomoFix Plate. Clin Biomech (Bristol, Avon) 2004;19:944–50. [DOI] [PubMed] [Google Scholar]
- [11].Martin R, Birmingham TB, Willits K, et al. Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med 2014;42:1118–26. [DOI] [PubMed] [Google Scholar]
- [12].Ryu SM, Park JW, Na HD, et al. High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis with kissing lesions in relatively young patients. Knee Surg Relat Res 2018;30:17–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Floerkemeier S, Staubli AE, Schroeter S, et al. Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 2013;21:170–80. [DOI] [PubMed] [Google Scholar]
- [14].Meidinger G, Imhoff AB, Paul J, et al. May smokers and overweight patients be treated with a medial open-wedge HTO? Risk factors for non-union. Knee Surg Sports Traumatol Arthrosc 2011;19:333–9. [DOI] [PubMed] [Google Scholar]
- [15].Rose T, Imhoff AB. Complications after transgenicular osteotomies. Oper Tech Orthop 2007;17:80–6. [Google Scholar]
- [16].Miller BS, Dorsey WO, Bryant CR, et al. The effect of lateral cortex disruption and repair on the stability of the medial opening wedge high tibial osteotomy. Am J Sports Med 2005;33:1552–7. [DOI] [PubMed] [Google Scholar]
- [17].van Heerwaarden R, Najfeld M, Brinkman M, et al. Wedge volume and osteotomy surface depend on surgical technique for distal femoral osteotomy. Knee Surg Sports Traumatol Arthrosc 2013;21:206–12. [DOI] [PubMed] [Google Scholar]
- [18].Roderer G, Gebhard F, Duerselen L, et al. Delayed bone healing following high tibial osteotomy related to increased implant stiffness in locked plating. Injury 2014;45:1648–52. [DOI] [PubMed] [Google Scholar]
- [19].Bottlang M, Doornink J, Lujan TJ, et al. Effects of construct stiffness on healing of fractures stabilized with locking plates. J Bone Joint Surg Am 2010;92suppl 2:12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Lujan TJ, Henderson CE, Madey SM, et al. Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation. J Orthop Trauma 2010;24:156–62. [DOI] [PubMed] [Google Scholar]
- [21].Kazimoğlu C, Akdoğan Y, Şener M, et al. Which is the best fixation method for lateral cortex disruption in the medial open wedge high tibial osteotomy? A biomechanical study. Knee 2008;15:305–8. [DOI] [PubMed] [Google Scholar]
- [22].Luo CA, Lin SC, Hwa SY, et al. Biomechanical effects of plate area and locking screw on medial open tibial osteotomy. Comput Methods Biomech Biomed Eng 2015;18:1263–71. [DOI] [PubMed] [Google Scholar]
- [23].Golovakhа ML, Orljanski W, Benedetto K-P, et al. Comparison of theoretical fixation stability of three devices employed in medial opening wedge high tibial osteotomy: a finite element analysis. BMC Musculoskelet Disord 2014;15:230–42. [DOI] [PMC free article] [PubMed] [Google Scholar]


