Abstract
Background
We explored the distinct trajectories of functional decline among older adults in Japan, and evaluated whether the frequency of outings, an important indicator of social activity, predicts the identified trajectories.
Methods
We analyzed data on 2,364 adults aged 65 years or older from the Japan Aichi Gerontological Evaluation Study. Participants were initially independent and later developed functional disability during a 31-month follow-up period. We used the level of long-term care needs certified in the public health insurance system as a proxy of functional ability and linked the fully tracked data of changes in the care levels to the baseline data. A low frequency of outings was defined as leaving one’s home less than once per week at baseline. We applied a growth mixture model to identify trajectories in functional decline by sex and then examined the association between the frequency of outings and the identified trajectories using multinomial logistic regression analysis.
Results
Three distinct trajectories were identified: “slowly declining” (64.3% of men and 79.7% of women), “persistently disabled” (4.5% and 3.7%, respectively), and “rapidly declining” (31.3% and 16.6%, respectively). Men with fewer outings had 2.14 times greater odds (95% confidence interval, 1.03–4.41) of being persistently disabled. The association between outing frequency and functional decline trajectory was less clear statistically among women.
Conclusions
While the majority of older adults showed a slow functional decline, some showed persistent moderate disability. Providing more opportunities to go out or assistance in that regard may be important for preventing persistent disability, and such needs might be greater among men.
Key words: functional decline, trajectory, homebound persons, older people, Japan
INTRODUCTION
Population aging has been observed and is accelerating worldwide. The World Health Organization has proposed global strategies to maintain the functional ability and intrinsic capacity of older adults by removing barriers to participation and compensating for capacity losses.1 Japan is the global leader in the rapidity of population aging: in 2015, the proportion of older people aged 65 or more was 26.7%, and by 2060, this proportion is expected to reach upwards of 40%.2 The Japanese government implemented a public long-term care insurance (LTCI) system in 2000 and has since faced the challenges of both sustaining the system financially and improving its performance in maintaining and improving the functional ability of those insured.
To overcome these challenges, it is necessary to determine how older people’s functional ability changes and what environments are most conducive to declines. Han et al identified five distinct trajectories of functional ability among community-dwelling older adults: independent, consistently low or high disability, and a gradual change towards low or high disability.3 In Japan, Liang et al classified three trajectories of functional impairment over 10 years: minimal function decrement, early onset and accelerated in the 80s, and late onset in the 70s–80s.4 However, comparatively few studies have identified these trajectories using an objective indicator of older adults’ functional ability.
Potential predictors of the trajectories in older adults’ functional ability are biological, socioeconomic, and psychosocial in nature.3–5 Among these factors, the psychosocial risk factors (eg, social relationships) are especially important to consider when planning interventions in community settings. A previous systematic review suggested that having few social contacts is a critical risk factor of functional disability in older adults.6 However, we still have relatively little understanding of the association between social connections and trajectories in functional disability in older adults.7
To improve our understanding of this association, we focused on the frequency of outings as a proxy indicator of the level of social activity and connectedness. Research has shown that fewer outings predicts the incidence of functional disability, cognitive decline, and premature mortality among older adults.8 In Japan, there is a condition called “tojikomori” where individuals do not go out frequently, despite not having functional problems in the physical, mental, or cognitive domains.9 Tojikomori is considered preventable because it is related to individuals’ social relationships and environment.10 In this study, we explored the distinct trajectories of functional decline—measured using an objective evaluation scheme—and whether going out less often in the absence of functional problems predicts these identified trajectories.
METHODS
Study subjects
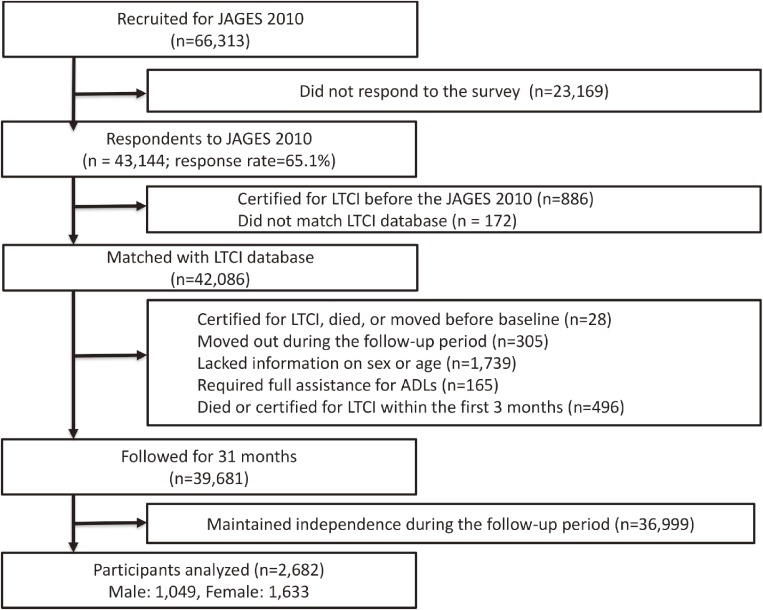
We used data from the Japan Gerontological Evaluation Study (JAGES), which is an on-going longitudinal study targeting community-dwelling and functionally independent older adults aged ≥65 years (see the flow chart of participation in Figure 1). Functional independency was defined as not being certified for Japan’s LTCI system. The JAGES survey conducted in 2010 served as the baseline for our longitudinal observations, with which we combined individual LTCI data provided from 12 municipalities in six prefectures. Within these 12 municipalities, 26,690 older adults were randomly selected across six municipalities, and a census was taken in the other six municipalities (yielding a further 39,623 older adults). Of the 66,313 adults surveyed, 43,144 returned the questionnaire (response rate 65.1%); of these, the data of 42,086 were matched with the LTCI database. We excluded those who had been certified for LTCI or had died or moved before the survey date (n = 28), who moved out from their current residence during the follow-up period (n = 305), who lacked information on sex or age (n = 1,739), who required full assistance for activities of daily living (ADLs) (n = 165), or who died or were certified as needing long-term care within the first 3 months from baseline (n = 496). Finally, we excluded those who maintained their independence during the follow-up period (n = 36,999). This was because the proportion was too large (87.9% of those who had data matched with the LTCI database over 31 months) to ensure accurate classification of the trajectories of individuals requiring long-term care. Thus, a total of 2,682 participants were analyzed. The JAGES protocol was reviewed and approved by the ethics committee on research of human subjects at Nihon Fukushi University (No. 10-05), and the use of the JAGES data for this study was approved by the Ethics Committee of the Faculty of Medicine, University of Tokyo (No. 10555).
Figure 1. Flow chart of participants in this study.
Assessment of functional ability
We used the certified long-term care levels of the national LTCI as an index of functional ability. According to this system, individuals are classified into one of seven care levels based on the severity of their physical and cognitive disability via a home-visit interview and physician examination. A lower care level implied worse functional ability. Moreover, the seven care levels are framed by independence (level 8) and death (level 0), such that functional ability falls on a continuum between these two states. For instance, level 3 (youkaigo 3) refers to “complete support needed in toileting, bathing, dressing, and all other basic ADLs.” The details of each care level are provided elsewhere.11
The validity period of each care level is, in principle, 6 months for the initial certification and 12 months for each subsequent certification. However, older adults can apply for a re-evaluation of their care level whenever they wish. We obtained information on the date of certification and the care levels until 31 months after baseline or death from the LTCI database. Then, we aggregated the information on care levels for every 3 months to create equidistant intervals of observation for the trajectory analysis.
Low frequency of outings
We defined a low frequency of outings as leaving one’s home less than once per week.12,13 The frequency of leaving home was measured at the time of baseline survey using a single question: “How often do you usually go outside the house?”. Possible answers were “almost every day,” “2 to 3 times per week,” “about once per week,” “1 to 2 times per month,” “several times in a year,” and “never”. Although this single-question measure has not been formally validated, it has been widely used in previous studies,8,14 as well as in the process of certification by the government for long-term nursing care.15
Covariates
The potential confounding factors were socio-demographic characteristics (ie, age, marital status, education years, equivalent household income, household composition, and urbanization [population density]), health status (self-reported body mass index [BMI], current medical history [at least one of the following diseases: stroke, cancer, bone or heart diseases], self-rated health, and depressive symptoms according to a score of 6 or more on the short version of the Geriatric Depression Scale [GDS-15]),16,17 and physiological variables (intellectual activity and instrumental ADLs assessed using the Tokyo Metropolitan Institute of Gerontology Index of Competence).18
Modeling and analysis
First, we used a growth mixture model (GMM) to identify the trajectories in functional ability by sex. GMM is considered more appropriate than is a conventional latent growth curve model for the investigation of individual trajectories when those trajectories are heterogeneous. This is because it assumes that the population consists of distinct sub-groups of trajectories.19 A multivariate skewness/kurtosis test (SK test) revealed that the distribution of long-term care levels was not normal, so we applied a non-normal GMM, which can fit non-normal data considerably better than can normal mixture models.20
The time in months from baseline until the date of certification of long-term care levels was used as the time scale; this ranged from 4 to 31 months (ie, 10 time points). We constructed the trajectory models according to the number of trajectory classes (2 to 4) and trajectory shape (linear, quadratic, or cubic) and chose the best-fitting model according to the lowest Bayesian information criterion (BIC), adjusted Lo-Mendell-Rubin likelihood ratio test (Adj. LMR-LRT), and study objective (identification of comparable trajectories of functional ability). Then, we evaluated the average posterior probabilities of each class (a value of above 0.70 indicated good discrimination). Age was included as a covariate in the GMM. The GMM analysis was conducted using Mplus 7 (Muthén & Muthén, Los Angeles, CA, USA).
We then used multinomial logistic regression analysis, stratified by sex, to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) for exhibiting a pattern of deterioration (ie, the base outcome was “slowly declining”). In model 1, we adjusted for the socio-demographic characteristics, and in model 2, we added health status and the physiological variables to model 1. We then performed a sensitivity analysis, which involved performing the logistic regression analysis again but excluding participants aged 85 years or older, for whom less frequent outings and deterioration in functional ability are considered natural phenomena associated with aging. We also excluded participants who died in the first 6 months from baseline because rapid deterioration of function and death within 6 months is likely the result of disease. Finally, we controlled for long-term care level at the first certification. Because the baseline care levels differed substantially between “slow decline toward low disability” and “persistently moderate decline,” we wanted to check if the association between outing frequency and trajectories in functional disability remained even after controlling for the initial long-term care levels. Two-sided alphas of 0.05 were considered statistically significant. The regression analyses were conducted using STATA 14.1 (Stata Corp, College Stations, TX, USA).
RESULTS
The baseline characteristics of the 2,682 participants (1,049 men and 1,633 women) are shown in Table 1. Men and women had average ages of 79.0 and 80.2 years, respectively. Furthermore, 16.6% of men and 19.4% of women had a low frequency of outings. During the 31-month follow-up period, 17.6% of men and 14.1% of women were certified as completely dependent for many ADLs (ie, had care level 3 or lower [youkaigo 3 to 5]), and 27.3% of men and 10.5% of women died.
Table 1. Characteristics of study participants by trajectory patterns and sex at baseline.
| Characteristics of study participants | ||||||||||||
| Men (n = 1,049) | Women (n = 1,633) | |||||||||||
| Slowly declining (n = 674) | Persistently disabled (n = 47) | Rapidly declining (n = 328) | Slowly declining (n = 1,301) | Persistently disabled (n = 61) | Rapidly declining (n = 271) | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Age | ||||||||||||
| 65–74 | 154 | 22.8 | 8 | 17.0 | 92 | 28.0 | 213 | 16.4 | 11 | 18.0 | 60 | 22.1 |
| 75–84 | 389 | 57.7 | 31 | 66.0 | 156 | 47.6 | 760 | 58.4 | 34 | 55.7 | 150 | 55.4 |
| 85– | 131 | 19.4 | 8 | 17.0 | 80 | 24.4 | 328 | 25.2 | 16 | 26.2 | 61 | 22.5 |
| Marital status | ||||||||||||
| Married | 490 | 72.7 | 40 | 85.1 | 236 | 72.0 | 469 | 36.0 | 28 | 45.9 | 101 | 37.3 |
| Single | 120 | 17.8 | 5 | 10.6 | 60 | 18.3 | 693 | 53.3 | 27 | 44.3 | 145 | 53.5 |
| Missing | 64 | 9.5 | 2 | 4.3 | 32 | 9.8 | 139 | 10.7 | 6 | 9.8 | 25 | 9.2 |
| Education (years) | ||||||||||||
| ≤9 | 346 | 51.3 | 33 | 70.2 | 177 | 54.0 | 718 | 55.2 | 38 | 62.3 | 165 | 60.9 |
| ≥10 | 267 | 39.6 | 10 | 21.3 | 114 | 34.8 | 417 | 32.1 | 14 | 23.0 | 73 | 26.9 |
| Missing/others | 61 | 9.1 | 4 | 8.5 | 37 | 11.3 | 166 | 12.8 | 9 | 14.8 | 33 | 12.2 |
| Equivalized income | ||||||||||||
| 1.99 million yen or less | 292 | 43.3 | 26 | 55.3 | 145 | 44.2 | 480 | 36.9 | 24 | 39.3 | 103 | 38.0 |
| 2 million yen or more | 213 | 31.6 | 16 | 34.0 | 98 | 29.9 | 315 | 24.2 | 14 | 23.0 | 70 | 25.8 |
| Missing | 169 | 25.1 | 5 | 10.6 | 85 | 25.9 | 506 | 38.9 | 23 | 37.7 | 98 | 36.2 |
| Household composition | ||||||||||||
| With spouse/children/others | 560 | 83.1 | 44 | 93.6 | 276 | 84.1 | 946 | 72.7 | 44 | 72.1 | 211 | 77.9 |
| Live alone | 64 | 9.5 | 2 | 4.3 | 22 | 6.7 | 254 | 19.5 | 10 | 16.4 | 42 | 15.5 |
| Missing | 50 | 7.4 | 1 | 2.1 | 30 | 9.1 | 101 | 7.8 | 7 | 11.5 | 18 | 6.6 |
| Urbanization | ||||||||||||
| Urban (>1,500 population/km2) | 88 | 13.1 | 7 | 14.9 | 42 | 12.8 | 156 | 12.0 | 4 | 6.6 | 33 | 12.2 |
| Semi-urban (1,000–1,500 population/km2) | 258 | 38.3 | 12 | 25.5 | 113 | 34.5 | 448 | 34.4 | 20 | 32.8 | 78 | 28.8 |
| Rural (<1,000 population/km2) | 328 | 48.7 | 28 | 59.6 | 173 | 52.7 | 697 | 53.6 | 37 | 60.7 | 160 | 59.0 |
| Body mass index | ||||||||||||
| <18.5 | 75 | 11.1 | 11 | 23.4 | 46 | 14.0 | 129 | 9.9 | 6 | 9.8 | 35 | 12.9 |
| 18.5–24.9 | 402 | 59.6 | 24 | 51.1 | 182 | 55.5 | 672 | 51.7 | 28 | 45.9 | 144 | 53.1 |
| ≥25 | 115 | 17.1 | 8 | 17.0 | 51 | 15.5 | 279 | 21.4 | 12 | 19.7 | 47 | 17.3 |
| Missing | 82 | 12.2 | 4 | 8.5 | 49 | 14.9 | 221 | 17.0 | 15 | 24.6 | 45 | 16.6 |
| Current medical history | ||||||||||||
| No | 409 | 60.7 | 19 | 40.4 | 170 | 51.8 | 644 | 49.5 | 31 | 50.8 | 138 | 50.9 |
| Yes | 265 | 39.3 | 28 | 59.6 | 158 | 48.2 | 657 | 50.5 | 30 | 49.2 | 133 | 49.1 |
| Self-rated health | ||||||||||||
| Very good/Good | 364 | 54.0 | 15 | 31.9 | 176 | 53.7 | 736 | 56.6 | 28 | 45.9 | 137 | 50.6 |
| Poor/very poor | 283 | 42.0 | 31 | 66.0 | 144 | 43.9 | 511 | 39.3 | 32 | 52.5 | 122 | 45.0 |
| Missing | 27 | 4.0 | 1 | 2.1 | 8 | 2.4 | 54 | 4.2 | 1 | 1.6 | 12 | 4.4 |
| Depressive symptoms (GDS-15) | ||||||||||||
| No depressive symptoms (GDS-15 <6) | 315 | 46.7 | 14 | 29.8 | 152 | 46.3 | 580 | 44.6 | 25 | 41.0 | 116 | 42.8 |
| Depressive symptoms (GDS-15 ≥6) | 212 | 31.5 | 25 | 53.2 | 101 | 30.8 | 339 | 26.1 | 16 | 26.2 | 71 | 26.2 |
| Missing | 147 | 21.8 | 8 | 17.0 | 75 | 22.9 | 382 | 29.4 | 20 | 32.8 | 84 | 31.0 |
| Intellectual activity | ||||||||||||
| 4 points (full marks) | 339 | 50.3 | 19 | 40.4 | 146 | 44.5 | 564 | 43.4 | 20 | 32.8 | 105 | 38.7 |
| 3 points and under | 258 | 38.3 | 24 | 51.1 | 147 | 44.8 | 570 | 43.8 | 30 | 49.2 | 129 | 47.6 |
| Missing | 77 | 11.4 | 4 | 8.5 | 35 | 10.7 | 167 | 12.8 | 11 | 18.0 | 37 | 13.7 |
| Instrumental activities of daily living | ||||||||||||
| 5 points (full marks) | 321 | 47.6 | 16 | 34.0 | 140 | 42.7 | 652 | 50.1 | 19 | 31.1 | 114 | 42.1 |
| 4 points and under | 286 | 42.4 | 28 | 59.6 | 155 | 47.3 | 479 | 36.8 | 33 | 54.1 | 122 | 45.0 |
| Missing | 67 | 9.9 | 3 | 6.4 | 33 | 10.1 | 170 | 13.1 | 9 | 14.8 | 35 | 12.9 |
| Frequency of outings | ||||||||||||
| Higher | 518 | 76.9 | 30 | 63.8 | 243 | 74.1 | 949 | 72.9 | 37 | 60.7 | 185 | 68.3 |
| Low | 99 | 14.7 | 15 | 31.9 | 60 | 18.3 | 240 | 18.4 | 16 | 26.2 | 61 | 22.5 |
| Missing | 57 | 8.5 | 2 | 4.3 | 25 | 7.6 | 112 | 8.6 | 8 | 13.1 | 25 | 9.2 |
GDS-15, short version of the Geriatric Depression Scale.
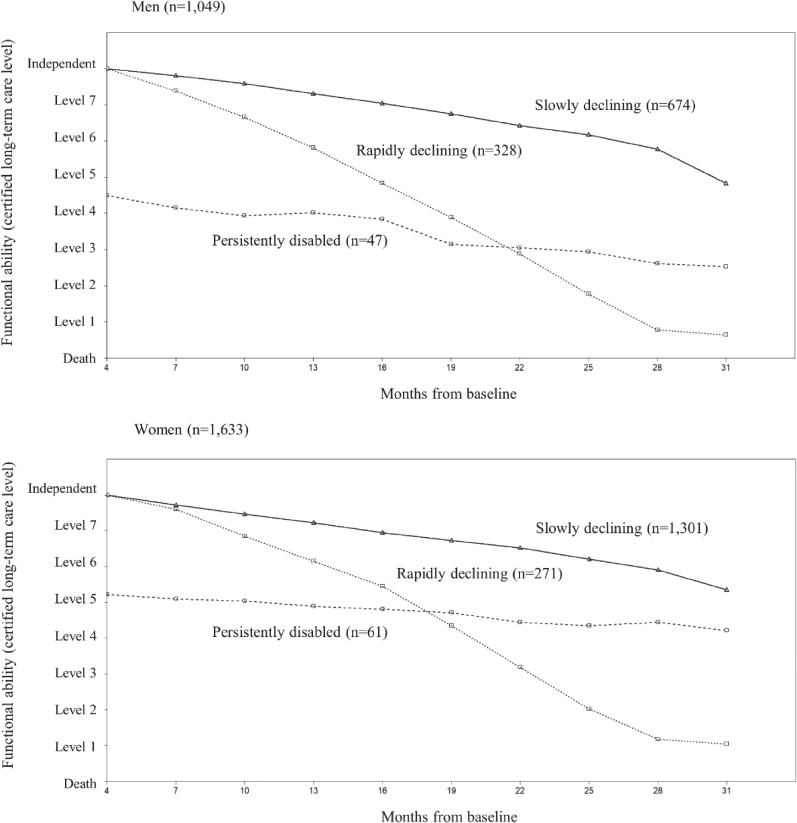
We chose a model containing three distinct trajectories of the quadratic type for both men and women. The GMM analysis showed that the BICs for the quadratic trajectories were better than those for the linear trajectories. Furthermore, while the BICs improved as the number of classes increased, we ultimately chose three classes based on the Adj. LMR-LRT (see eTable 1). Figure 2 illustrates the trajectories of certified long-term care levels for men and women, which were categorized as follows: “slowly declining” (674 men [64.3%] and 1,301 women [79.7%]); “persistently disabled” (47 men [4.5%] and 61 women [3.7%]); and “rapidly declining” (328 men [31.3%] and 271 women [16.6%]).
Figure 2. Sample trajectories in functional ability over time by sex. The Y axis shows functional ability (lower care levels indicate worse functional ability). The X axis shows the months from baseline (4 to 31 months). All participants were “independent” in terms of functional ability from 0 (baseline) to 3 months.
Table 2 shows the results of the multinomial logistic regression analysis by sex. After adjusting for the socio-demographic characteristics (model 1), we found a significant adjusted OR (AOR) for the “persistently disabled” trajectory for men who went outdoors less than once per week (compared with men who went outdoors once per week or more) (AOR 2.68; 95% CI, 1.14–6.28). The results for model 2 (which adjusted for the covariates of model 1 + health status and physiological variables) revealed an attenuated, but still statistically significant, AOR (2.14; 95% CI, 1.03–4.41). However, the AORs for the “rapidly declining” trajectory for both men and women and that for the “persistently disabled” trajectory for women were not statistically significant, although the direction of the associations was positive. We found similar results for the three sensitivity analyses (see eTable 2, eTable 3, and eTable 4).
Table 2. Multinomial logistic regression analysis of the “persistently disabled” or “rapidly declining” trajectory compared to the “slowly declining” trajectory by sex.
| Men (n = 1,049) | Women (n = 1,633) | |||||||||||||||
| Persistently disabled (vs Slowly declining) | ||||||||||||||||
| Model 1a | Model 2b | Model 1a | Model 2b | |||||||||||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | |||||
| Frequency of outings | ||||||||||||||||
| Higher | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Low | 2.68 | 1.14 | 6.28 | 0.023* | 2.14 | 1.03 | 4.41 | 0.040* | 1.64 | 1.02 | 2.64 | 0.043* | 1.20 | 0.68 | 2.12 | 0.524 |
| Missing | 0.69 | 0.10 | 4.79 | 0.709 | 0.74 | 0.14 | 3.86 | 0.725 | 1.78 | 1.12 | 2.83 | 0.015 | 1.67 | 0.61 | 4.55 | 0.319 |
| Age | ||||||||||||||||
| 65–74 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| 75–84 | 1.57 | 0.69 | 3.57 | 0.278 | 1.50 | 0.61 | 3.67 | 0.379 | 0.85 | 0.41 | 1.75 | 0.652 | 0.79 | 0.35 | 1.77 | 0.572 |
| 85– | 1.09 | 0.27 | 4.47 | 0.900 | 1.13 | 0.25 | 5.08 | 0.876 | 0.96 | 0.61 | 1.52 | 0.861 | 0.78 | 0.45 | 1.34 | 0.361 |
| Education (years) | ||||||||||||||||
| ≤9 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| ≥10 | 0.35 | 0.14 | 0.89 | 0.027* | 0.37 | 0.14 | 0.96 | 0.041* | 0.63 | 0.38 | 1.05 | 0.078 | 0.67 | 0.39 | 1.15 | 0.150 |
| Missing/others | 1.92 | 0.67 | 5.50 | 0.225 | 1.89 | 0.68 | 5.21 | 0.221 | 1.00 | 0.43 | 2.33 | 0.991 | 0.82 | 0.38 | 1.74 | 0.599 |
| Household composition | ||||||||||||||||
| With spouse/children/others | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Live alone | 0.67 | 0.14 | 3.27 | 0.620 | 0.60 | 0.13 | 2.84 | 0.519 | 1.16 | 0.57 | 2.37 | 0.687 | 1.25 | 0.62 | 2.53 | 0.529 |
| Missing | 0.37 | 0.05 | 2.76 | 0.335 | 0.41 | 0.06 | 2.87 | 0.372 | 2.03 | 0.48 | 8.57 | 0.334 | 2.07 | 0.43 | 9.97 | 0.363 |
| Urbanization | ||||||||||||||||
| Urban (>1,500 population/km2) | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Semi-urban (1,000–1,500 population/km2) | 0.55 | 0.36 | 0.84 | 0.006* | 0.60 | 0.39 | 0.91 | 0.017* | 1.71 | 1.05 | 2.81 | 0.032* | 1.70 | 1.11 | 2.61 | 0.016* |
| Rural (<1,000 population/km2) | 0.93 | 0.56 | 1.54 | 0.786 | 0.99 | 0.56 | 1.75 | 0.968 | 1.98 | 1.81 | 2.16 | <0.001 | 2.02 | 1.77 | 2.32 | <0.001 |
| Body mass index | ||||||||||||||||
| <18.5 | 2.33 | 1.24 | 4.40 | 0.009* | 1.06 | 0.40 | 2.84 | 0.900 | ||||||||
| 18.5–24.9 | 1.00 | 1.00 | ||||||||||||||
| ≥25 | 1.26 | 0.41 | 3.87 | 0.685 | 1.08 | 0.56 | 2.10 | 0.822 | ||||||||
| Missing | 1.10 | 0.34 | 3.60 | 0.874 | 1.66 | 0.76 | 3.63 | 0.203 | ||||||||
| Current medical history | ||||||||||||||||
| No | 1.00 | 1.00 | ||||||||||||||
| Yes | 1.93 | 0.90 | 4.14 | 0.092 | 0.75 | 0.48 | 1.16 | 0.198 | ||||||||
| Instrumental activities of daily living | ||||||||||||||||
| 5 points (full marks) | 1.00 | 1.00 | ||||||||||||||
| 4 points and under | 1.15 | 0.75 | 1.76 | 0.523 | 2.27 | 1.42 | 3.64 | 0.001* | ||||||||
| Missing | 0.95 | 0.20 | 4.64 | 0.952 | 1.04 | 0.34 | 3.17 | 0.944 | ||||||||
| Rapidly declining (vs Slowly declining) | ||||||||||||||||
| Model 1a | Model 2b | Model 1a | Model 2b | |||||||||||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | OR | 95% CI | P-value | |||||
| Frequency of outings | ||||||||||||||||
| Higher | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Low | 1.16 | 0.88 | 1.53 | 0.291 | 1.11 | 0.82 | 1.50 | 0.498 | 1.29 | 0.96 | 1.73 | 0.086 | 1.12 | 0.87 | 1.44 | 0.388 |
| Missing | 0.88 | 0.48 | 1.61 | 0.675 | 0.91 | 0.53 | 1.55 | 0.723 | 1.21 | 0.68 | 2.18 | 0.519 | 1.10 | 0.50 | 2.42 | 0.805 |
| Age | ||||||||||||||||
| 65–74 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| 75–84 | 0.64 | 0.51 | 0.80 | <0.001* | 0.61 | 0.48 | 0.77 | <0.001* | 0.66 | 0.50 | 0.87 | 0.004* | 0.63 | 0.50 | 0.79 | <0.001* |
| 85– | 0.93 | 0.55 | 1.60 | 0.799 | 0.87 | 0.50 | 1.51 | 0.613 | 0.57 | 0.33 | 0.98 | 0.042* | 0.50 | 0.33 | 0.76 | 0.001* |
| Education (years) | ||||||||||||||||
| ≤9 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| ≥10 | 0.84 | 0.68 | 1.03 | 0.087 | 0.87 | 0.68 | 1.10 | 0.251 | 0.75 | 0.58 | 0.97 | 0.026* | 0.74 | 0.58 | 0.95 | 0.017* |
| Missing/others | 1.38 | 0.70 | 2.73 | 0.350 | 1.31 | 0.66 | 2.58 | 0.437 | 1.02 | 0.66 | 1.57 | 0.923 | 0.98 | 0.55 | 1.73 | 0.938 |
| Household composition | ||||||||||||||||
| With spouse/children/others | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Live alone | 0.59 | 0.35 | 1.00 | 0.051 | 0.58 | 0.32 | 1.06 | 0.075 | 0.71 | 0.53 | 0.94 | 0.018* | 0.74 | 0.55 | 0.99 | 0.042* |
| Missing | 1.22 | 0.85 | 1.73 | 0.279 | 1.24 | 0.83 | 1.85 | 0.296 | 0.86 | 0.51 | 1.46 | 0.585 | 0.82 | 0.44 | 1.53 | 0.531 |
| Urbanization | ||||||||||||||||
| Urban (>1,500 population/km2) | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||||||
| Semi-urban (1,000–1,500 population/km2) | 0.93 | 0.66 | 1.30 | 0.679 | 0.95 | 0.69 | 1.32 | 0.768 | 0.85 | 0.69 | 1.04 | 0.111 | 0.82 | 0.66 | 1.02 | 0.069 |
| Rural (<1,000 population/km2) | 1.13 | 0.79 | 1.60 | 0.504 | 1.17 | 0.84 | 1.63 | 0.343 | 1.10 | 0.90 | 1.35 | 0.361 | 1.10 | 0.90 | 1.35 | 0.348 |
| Body mass index | ||||||||||||||||
| <18.5 | 1.41 | 0.89 | 2.24 | 0.144 | 1.23 | 0.80 | 1.89 | 0.355 | ||||||||
| 18.5–24.9 | 1.00 | 1.00 | ||||||||||||||
| ≥25 | 0.96 | 0.70 | 1.33 | 0.818 | 0.75 | 0.59 | 0.94 | 0.013* | ||||||||
| Missing | 1.23 | 0.80 | 1.89 | 0.345 | 1.01 | 0.68 | 1.51 | 0.952 | ||||||||
| Current medical history | ||||||||||||||||
| No | 1.00 | 1.00 | ||||||||||||||
| Yes | 1.55 | 1.20 | 2.01 | 0.001* | 0.89 | 0.64 | 1.24 | 0.496 | ||||||||
| Instrumental activities of daily living | ||||||||||||||||
| 5 points (full marks) | 1.00 | 1.00 | ||||||||||||||
| 4 points and under | 1.09 | 0.70 | 1.71 | 0.694 | 1.44 | 0.95 | 2.19 | 0.086 | ||||||||
| Missing | 1.14 | 0.50 | 2.62 | 0.752 | 1.02 | 0.58 | 1.81 | 0.935 | ||||||||
CI, confidence interval; GDS-15, short version of the Geriatric Depression Scale; OR, odds ratio.
Only covariates that are significantly related to at least one of the trajectories are listed.
aAdjusted for age, marital status, education years, equivalent annual household income, household composition, and urbanization.
bAdjusted for the covariates in Model 1 + body mass index, current medical history, self-rated health, depression (GDS-15 ≥6), intellectual activities, and instrumental activities of daily living.
*P < 0.05.
DISCUSSION
Our models suggested three distinct trajectories of functional ability for both men and women. Moreover, men with a low frequency of outings at baseline had 2.14 times greater odds of belonging to the “persistently disabled” trajectory, rather than the “slowly declining” trajectory, compared to men with a higher frequency of outings after adjusting for potential confounders.
The identified trajectories were consistent with those identified in previous studies.3–5 However, we expanded on past evidence by examining the trajectories from the first occurrence of functional disability, along with how social activity predicts these trajectories. Yu et al found that leisure activities were related to a “functional maintenance” trajectory (which is a desirable pattern)7; however, they included people with functional disabilities at baseline. In this study, we limited participants to those who were independent at baseline to decrease the possibility of reverse causation.
Several plausible mechanisms might explain the link between frequency of outings and the trajectories of functional decline among older men. First, a low frequency of outings may lead to limited social relationships, which in turn could directly lead to the deterioration of functional ability. Outing frequency is directly related to the size of one’s social network,14 which promotes healthy behaviors by increasing opportunities to access health services and information.21,22 Furthermore, social relationships might help prevent rapid deterioration in functional ability via social support, which can indirectly affect health by improving mental health.22 In an intervention study examining how community salons affect older people, the risk of being certified for long-term care was halved. The suggested mechanism of this was that participating in these salons expanded participants’ social network, thus enabling them to obtain greater social support.23
Another possibility is that outing frequency reflects the level of physical activity, such as walking. The frequency of outings is significantly associated with physical activity level,24 and exercise (including walking) is effective for improving cognitive function.25,26 Thus, remaining in the house might lead to a decrease in the body’s functional or cognitive reserves, leading to a continual decline in physical or cognitive resilience until they require long-term care.
Alternatively, however, it may also be possible that people who belonged to the “persistently disabled” group already had a tendency to stay in their houses at the time of baseline because their functions were somewhat weak. Physical or cognitive functions might not be the same at the baseline for all study participants, even though none of them needed nursing care. Therefore, the study results need cautious interpretation and further research is required to confirm that the observed associations are causal.
An association between frequency of outings and the “persistently disabled” trajectory was found in this study, but only in men. This gender difference is consistent with previous findings, which suggest that a low frequency of outings is a greater risk for the onset of functional decline in men than in women.27 One of the potential reasons for this may be that men and women tend to build their social relations in different places. When the study participants were still in the workforce, their social network mainly comprised work colleagues for men and individuals in the community for women (given that many of them were homemakers in Japan).28 As a result, women who are aged over 65 years old—even those who only go out less than once per week—might receive more social support from people in their communities.29 Furthermore, compared with men who remain in the house, women who do so might still have higher levels of physical activity because of their greater participation in housekeeping.30
A strength of this study was its use of a prospective cohort design with large panel data at 10 time points. Additionally, we used an objective indicator of functional ability as an outcome measurement, and controlled for various confounders, including socio-demographics and physiological variables. This study also has several limitations. First, the data on long-term care levels were obtained only for people who applied for the LTCI. Individuals who did not use public LTCI for any reason, such as being able to afford private nursing care, would be considered independent in our analysis. However, as a rule, all people living in Japan over 40 years old are insured by the LTCI; therefore, we assume that few people in need of LTCI do not apply for it. Second, reverse causation remains possible, as we did not adjust for some confounders relating to the preliminary stage of functional decline. To improve our inferences of causality, we restricted study participants to those who were independent at baseline, excluded persons who were certified for long-term care within 3 months after the baseline, and adjusted for the major diseases related to long-term care level and ADLs at baseline. Third, the magnitudes of the gap between each functional ability levels are not even across the levels evaluated using national LTCI system and mortality information. Moreover, death is conceptually different from functional ability. The potential solution may be to exclude cases of death. However, we believe that it is important to understand the patterns of declining functional ability among all older people who can be the targets of long-term care prevention measures in the community. Thus, we have conceptualized death as being at the end of the continuum of functional disability. Finally, the database contained no information on those who were certified as “non-applicable (independent)” after initially being certified as needing long-term care. This indicates that individuals whose long-term care level ultimately reached independence were considered to have maintained the care level that they previously had. However, in a 5-year period, such cases account for less than 1% of all certified persons requiring long-term care.31
In conclusion, we identified three distinct trajectories of functional abilities among community-dwelling older people during a 31-month observation period. Furthermore, a low frequency of outings was associated with a future pattern of maintaining moderate functional decline among older men, but not with a future rapid decline. The study results need to be cautiously interpreted due to the possible reverse causation that weaker functions at baseline caused fewer outings. If the observed association was causal, interventions to promote outings for older people, such as increasing opportunities to access community events and ease of access to restaurants and retail stores,32 might be effective in slowing the decline of functional ability among men with better initial care levels. It also would be necessary to consider the sex-specific factors related to a low frequency of outings.
ACKNOWLEDGEMENTS
This work was supported by JSPS (Japan Society for the Promotion of Science) KAKENHI Grants (JP15H01972, JP16K13443, JP17K15847, JP25253052), a Health Labor Sciences Research Grant (H28-Choju-Ippan-002, H28-Junkanki-Ippan-008), the Research and Development Grants for Longevity Science from the Japan Agency for Medical Research and Development (AMED), the Personal Health Record (PHR) Utilization Project from AMED, the Research Funding for Longevity Sciences from the National Center for Geriatrics and Gerontology (29-42), and the World Health Organization (WHO APW 2017/713981). The funding sources had no role in the design, execution, analysis, and interpretation of data, or in preparation of the manuscript.
Conflicts of interest: None declared.
Author contribution: NK developed the study design. JS participated in the study design, analyzed data, and drafted the manuscript. NK and MS contributed to the analysis and discussion. YT and NK cleaned the dataset for the present study. YT, MH, TT, and KK contributed to the discussion and reviewed the manuscript. KK is the principal investigator of the JAGES project, helped to develop the idea of the study, and reviewed and edited the manuscript. All authors approved the final version of the manuscript for publication.
APPENDIX A. SUPPLEMENTARY DATA
The following is the supplementary data related to this article:
eTable 1. Fit statistics for growth mixture model (GMM)
eTable 2. Multinomial logistic regression analysis among participants by sex after excluding those who died in the first 6 months from baseline
eTable 3. Multinomial logistic regression analysis among participants by sex, excluding those aged 85 years or more
eTable 4. Multinomial logistic regression analysis after adjusting for long-term care levels at the initial certification.
REFERENCES
- 1.World Health Organization. Multisectoral action for a life course approach to healthy ageing: draft global strategy and plan of action on ageing and health. 2016.
- 2.Cabinet Office, Government of Japan. Annual Report on the Aging Society: 2016. 2016. [Google Scholar]
- 3.Han L, Allore H, Murphy T, Gill T, Peduzzi P, Lin H. Dynamics of functional aging based on latent-class trajectories of activities of daily living. Ann Epidemiol. 2013;23:87–92. 10.1016/j.annepidem.2012.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liang J, Shaw BA, Krause NM, et al. Changes in functional status among older adults in Japan: successful and usual aging. Psychol Aging. 2003;18:684–695. 10.1037/0882-7974.18.4.684 [DOI] [PubMed] [Google Scholar]
- 5.Dodge HH, Du Y, Saxton JA, Ganguli M. Cognitive domains and trajectories of functional independence in nondemented elderly persons. J Gerontol A Biol Sci Med Sci. 2006;61:1330–1337. 10.1093/gerona/61.12.1330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stuck AE, Walthert JM, Nikolaus T, Büla CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–469. 10.1016/S0277-9536(98)00370-0 [DOI] [PubMed] [Google Scholar]
- 7.Yu HW, Chen DR, Chiang TL, Tu YK, Chen YM. Disability trajectories and associated disablement process factors among older adults in Taiwan. Arch Gerontol Geriatr. 2015;60:272–280. 10.1016/j.archger.2014.12.005 [DOI] [PubMed] [Google Scholar]
- 8.Fujita K, Fujiwara Y, Chaves PH, Motohashi Y, Shinkai S. Frequency of going outdoors as a good predictors for incident disability of physical function as well as disability recovery in community-dwelling older adults in rural Japan. J Epidemiol. 2006;16:261–270. 10.2188/jea.16.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hirai H, Kondo K. Review of the literature on the ‘Tojikomori’ elderly in Japan study trends, definition, and review of cohort studies. Nihon Koshu Eisei Zasshi. 2007;54:293–303 (in Japanese). [PubMed] [Google Scholar]
- 10.Shinkai S, Fujita K, Fujiwara Y, et al. Prevalence and characteristics of different types of homeboundness among community-living adults. Nihon Koshu Eisei Zasshi. 2005;52:443–455 (in Japanese). [PubMed] [Google Scholar]
- 11.Kondo N, Suzuki K, Minai J, Yamagata Z. Positive and Negative effects of finance-based social capital on incident functional disability and mortality: an 8-year prospective study of elderly Japanese. J Epidemiol. 2012;22:543–550. 10.2188/jea.JE20120025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koyama S, Aida J, Kondo K, et al. Does poor dental health predict becoming homebound among older Japanese? BMC Oral Health. 2016;16:51. 10.1186/s12903-016-0209-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yasumura S. Homebound elderly people in Japan-special reference to intervention study including life review method. Nippon Ronen Igakkai Zasshi. 2003;40:470–472 (in Japanese). 10.3143/geriatrics.40.470 [DOI] [PubMed] [Google Scholar]
- 14.Yokoyama H, Haga H, Yasumura S, et al. Study on characteristics of house-bound elderly with declined outing: from the difference in the level of ADL. Jpn J Gerontol. 2005;26:424–437 (in Japanese). [Google Scholar]
- 15.Ministry of Health and Labor. Instructions of the Nursing Care Prevention Manual. 2009.
- 16.Wada T, Ishine M, Sakagami T, et al. Depression in Japanese community-dwelling elderly—prevalence and association with ADL and QOL. Arch Gerontol Geriatr. 2004;39:15–23. 10.1016/j.archger.2003.12.003 [DOI] [PubMed] [Google Scholar]
- 17.Burke WJ, Roccaforte WH, Wengel SP. The short form of the Geriatric Depression Scale: a comparison with the 30-item form. J Geriatr Psychiatry Neurol. 1991;4:173–178. [DOI] [PubMed] [Google Scholar]
- 18.Koyano W, Shibata H, Nakazato K, Haga H, Suyama Y. Measurement of competence: reliability and validity of the TMIG Index of Competence. Arch Gerontol Geriatr. 1991;13:103–116. 10.1016/0167-4943(91)90053-S [DOI] [PubMed] [Google Scholar]
- 19.Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24:882–891. 10.1111/j.1530-0277.2000.tb02070.x [DOI] [PubMed] [Google Scholar]
- 20.Muthén B, Asparouhov T. Growth mixture modeling with non-normal distributions. Stat Med. 2015;34:1041–1058. 10.1002/sim.6388 [DOI] [PubMed] [Google Scholar]
- 21.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. 10.1016/S0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 22.Cohen S. Social relationships and health. Am Psychol. 2004;59:676–684. 10.1037/0003-066X.59.8.676 [DOI] [PubMed] [Google Scholar]
- 23.Hikichi H, Kondo N, Kondo K, Aida J, Takeda T, Kawachi I. Effect of a community intervention programme promoting social interactions on functional disability prevention for older adults: propensity score matching and instrumental variable analyses, JAGES Taketoyo study. J Epidemiol Community Health. 2015;69:905–910. 10.1136/jech-2014-205345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tanaka C, Yoshida H, Amano H, et al. Physical activity level and physical, mental and social factors in community-dwelling elderly people. Nihon Koshu Eisei Zasshi. 2006;53:671–680 (in Japanese). [PubMed] [Google Scholar]
- 25.van Uffelen JG, Chinapaw MJ, van Mechelen W, Hopman-Rock M. Walking or vitamin B for cognition in older adults with mild cognitive impairment? A randomised controlled trial. Br J Sports Med. 2008;42:344–351. 10.1136/bjsm.2007.044735 [DOI] [PubMed] [Google Scholar]
- 26.Heyn P, Abreu BC, Ottenbacher KJ. The effects of exercise training on elderly persons with cognitive impairment and dementia: a meta-analysis. Arch Phys Med Rehabil. 2004;85:1694–1704. 10.1016/j.apmr.2004.03.019 [DOI] [PubMed] [Google Scholar]
- 27.Hamazaki Y, Morikawa Y, Morimoto S, Nakagawa H. Difference in the impact of homebound status on functional decline between independent older men and women: a 2 year follow-up study. Jpn J Nurs Sci. 2016;13:265–275. 10.1111/jjns.12109 [DOI] [PubMed] [Google Scholar]
- 28.Nobe M. An examination of sex differences in the structure of social networks and in the availability of social support for the elderly. Jpn Sociol Rev. 1999;50:375–392 (in Japanese) 10.4057/jsr.50.375 [DOI] [Google Scholar]
- 29.Saito T, Kondo K, Murata C, Jeong S, Suzuki K, Kondo N; JAGES Group . Gender and regional differences in going-out, social, and leisure activities among older adults Findings from the JAGES Project. Nihon Koshu Eisei Zasshi. 2015;62:596–608 (in Japanese). [DOI] [PubMed] [Google Scholar]
- 30.Takahashi K, Yasumura S, Yabe J, Haga H. The actual condition of the roles in the community and at home and the investigation of relevant factors in the homebound elderly in the Tohoku district. J Health Welfare Stat. 2007;54:9–16 (in Japanese). [Google Scholar]
- 31.Kijima H. A study on levels of care changes for individuals requiring long-term care at home -With reference to the level of care service use and changes in the level of care needs-. Research reports of Suzuka University of Medical Science. 2007:39–52 (in Japanese).
- 32.Murayama H, Yoshie S, Sugawara I, Wakui T, Arami R. Contextual effect of neighborhood environment on homebound elderly in a Japanese community. Arch Gerontol Geriatr. 2012;54:67–71. 10.1016/j.archger.2011.03.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.