Abstract
Objectives
Excessive and inappropriate use of antibiotics increases antimicrobial resistance. The aim of this study was to determine the magnitude and determinants of antibiotic dispensing without prescription in Spain by the simulated patient technique.
Methods
A cross-sectional study was conducted with all the pharmacies in a region of north-west Spain (n = 977), between December 2016 and January 2017. Four actors visited the pharmacies simulating a respiratory infection. Four incremental levels of pressure were used to obtain an antibiotic. The education and sex of the person who was dispensing and the area where the pharmacy was located were recorded. The effect of these independent variables on the dispensing of an antibiotic without prescription (1 = yes, 0 = no) was modelled by logistic regression.
Results
An antibiotic was obtained in 18.83% (95% CI = 16.5%–21.41%) of the visits. The area influenced the dispensing of antibiotics without a medical prescription, with a greater likelihood of dispensing in rural (OR = 1.79; 95% CI = 1.20–2.68) or semi-rural (OR = 1.66; 95% CI = 1.13–2.44) areas than in urban areas. No association was found with the sex or the training of the person who dispensed the antibiotic. In the pharmacies in urban areas, a lower level of pressure was needed to obtain the antibiotic.
Conclusions
This study shows that one-fifth of the pharmacies still dispense antibiotics without prescription, especially under patient pressure. A rural setting has been identified as a risk factor for dispensing without prescription, so it must be taken into account for future interventions.
Introduction
Resistance to antibiotics is a major challenge facing public health,1 due to the morbidity, mortality and costs it generates.2 It is not only a local problem, but also a global one because travellers contribute to the spread of antimicrobial drug resistance.3 Currently, no one doubts that it is linked to the excessive and inappropriate use of antibiotics. The majority of consumption is outside hospitals and, except for North America and some European countries, part of this is due to self-medication.4 Controlling access to non-prescribed antibiotics is a key element in decreasing it, and pharmacies play a fundamental role in this.
Spain is one of the countries with the highest consumption of antibiotics in the EU and consumption does not cease to grow.5 It is estimated that 30% of the dispensed antibiotics are not charged to the public reimbursement system,6 but how much is due to other non-reimbursed resources (e.g. private medicine) and how much to the dispensing of antibiotics without a medical prescription (DAwMP), an unlawful practice,7 is unknown. Estimating this is a challenge: the use of interviews or surveys can produce results biased by the Hawthorne effect. A robust method could be the simulated patient (SP) method,8 where an individual visits a pharmacy simulating specific symptoms and requiring an antibiotic. DAwMP near to the real ones are obtained and it allows the quality of pharmaceutical care to be assessed.
Using the SP technique, this study aimed to quantify the magnitude of DAwMP in the north-west of Spain and to determine the associated factors.
Methods
Design and population
A cross-sectional study was conducted in two provinces (A Coruña and Pontevedra) of north-western Spain. The sampling was comprehensive, including all the pharmacies in the studied geographical area (n = 977).
Study setting
In Spain, the National Health System covers practically all the population and medical care is free. Patients contribute to drug costs depending on the treatment and their income.9 Drugs can only be dispensed in pharmacies, and some kinds, such as antibiotics, require a medical prescription.
Data collection
The SP technique was used.10 Four amateur actors (two women and two men with apparent ages between 30 and 45 years) visited the pharmacies between December 2016 and January 2017; ∼10 pharmacies were visited per day by each SP. They were trained by an expert SP,11 so that the representation would be uniform.
The same symptoms as in previous studies were represented:11,12 sore throat, difficulty swallowing and feeling feverish, in addition to congestion and cough. Four gradually incremental levels of pressure were used to obtain an antibiotic without prescription: (i) request for medication to relieve the symptoms; (ii) request for a stronger medication than that offered; (iii) request for an antibiotic; and (iv) specific request for amoxicillin.
In a data collection notebook (case report form) we recorded the result of the demand process, reason why DAwMP did not occur, pharmaceutical care (referral to a doctor, questions about allergies and pregnancy), sex and training (pharmacist or assistant) of dispenser and area where the pharmacy was located [rural (<10000 inhabitants), semi-rural (between 10000 and 50000 inhabitants) and urban (>50000 inhabitants)].
Ethics
The Galician Ethics Committee approved the study (code number 2015/597). No personal data of professionals were recorded. We generated an automatic code for each pharmacy, which made it impossible for the researchers to match each record to the corresponding pharmacy and its outcome in the demand process.
Outcomes and analysis
The effects of independent variables on DAwMP (1 = yes, 0 = no) were modelled by simple logistic regression (crude analysis) and by multiple logistic regression (adjusted analysis). The variables with a P value <0.20 in the bivariate analysis were considered potentially confounding. They were confirmed as confounders if they produced a >10% change in the coefficient when they were deleted from the multivariate model. The results were expressed as ORs and 95% CIs.
To analyse whether the area influenced the level of pressure required to obtain the antibiotic, we performed a sub-analysis of those pharmacies classified as DAwMP. We created a binary variable, with a value of 1 if the antibiotic was obtained at the first or second level of pressure (the antibiotic was not openly requested) and 0 for those at the third or fourth level (the SP requested an antibiotic).
Results
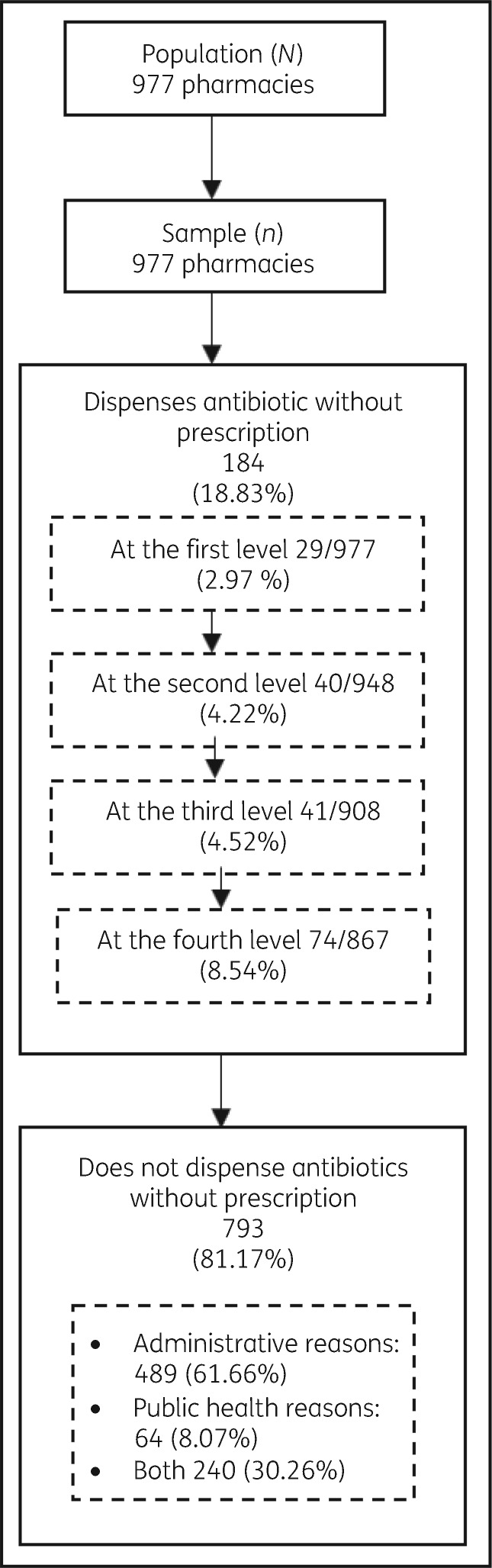
An antibiotic was obtained in 184 pharmacies (18.83%; 95% CI = 16.50%–21.41%), mostly between the third and fourth levels of pressure (Figure 1). Of the pharmacies that carried out DAwMP, 74.5% explained the frequency with which the antibiotic should be taken, 24.5% asked about allergies to medications, 35.9% recommended seeing a doctor, and 37.5% asked female SPs about the possibility of pregnancy.
Figure 1.
Flow of participants through the study.
The most frequently dispensed antibiotic was amoxicillin (n = 127, 69.0%), in 7% of cases in combination with clavulanic acid. Azithromycin (n = 42, 22.8%), co-trimoxazole (n = 7, 3.8%), moxifloxacin (n = 4, 2.2%), cefuroxime (n = 2, 1.1%), clarithromycin (n = 1, 0.5%) and clindamycin (n = 1, 0.5%) were obtained less frequently. The level of pressure at which each antibiotic was obtained can be found in Table S1 (available as Supplementary data at JAC Online). In most cases, an over-the-counter cold medicine was offered instead of an antibiotic.
Associated factors
It was found that the area influenced DAwMP (Table 1) and DAwMP was more likely in rural (OR = 1.79; 95% CI = 1.20–2.68) or semi-rural (OR = 1.66; 95% CI = 1.13–2.44) areas. There were no differences as a function of sex or the training of the person who dispensed medication. There were also no differences between the four SPs.
Table 1.
Influence of independent variables on DAwMP
| Characteristic | DAwMP |
ORa | 95% CI | P | ||
|---|---|---|---|---|---|---|
| no, n (%) | yes, n (%) | |||||
| Sex | women | 634 (82.2) | 137 (17.8) | 1 | ||
| men | 159 (77.2) | 47 (22.8) | 1.37 | 0.94–1.99 | 0.101 | |
| Areab | urban | 360 (85.7) | 60 (14.3) | 1 | ||
| semi-rural | 242 (78.3) | 67 (21.7) | 1.66 | 1.13-2.44 | 0.010 | |
| rural | 191 (77.0) | 57 (23.0) | 1.79 | 1.20–2.68 | 0.005 | |
| Identification | pharmacist | 454 (81.7) | 102 (18.4) | 1 | ||
| assistant | 136 (84.5) | 25 (15.5) | 0.82 | 0.51–1.32 | 0.410 | |
| no identification | 203 (78.1) | 57 (21.9) | 1.25 | 0.87–1.80 | 0.230 | |
| SP number | 1 | 200 (80.3) | 49 (19.7) | 1 | ||
| 2 | 193 (83.2) | 39 (16.8) | 0.82 | 0.52–1.31 | 0.417 | |
| 3 | 189 (77.8) | 54 (22.2) | 1.17 | 0.75–1.80 | 0.488 | |
| 4 | 211 (83.4) | 42 (16.6) | 0.81 | 0.52–1.28 | 0.371 | |
Crude analysis. None of the independent variables has shown a confounding effect.
Area: rural (<10000 inhabitants), semi-rural (between 10000 and 50000 inhabitants) and urban (>50000 inhabitants).
The sub-analysis of the pharmacies that carried out DAwMP showed an increased risk of obtaining an antibiotic without an SP request in urban areas compared with rural areas (1/OR = 2.29; 95% CI = 1.08–4.83).
No DAwMP
Among the pharmacies that did not carry out DAwMP, 91.9% provided reasons related to administration; for instance, pharmacies are not allowed to sell antibiotics (Figure 1). In 30.26% of the cases, this was reinforced with reasons related to health (absence of a diagnosis, development of resistance or possible viral aetiology). Furthermore, 83.61% advised consulting a doctor.
Discussion
This large study with SPs shows that almost one-fifth of the pharmacies carried out DAwMP and that this depended on the area and the customer’s level of pressure. This indicates the need for interventions to reduce this practice and their prioritization in rural environments.
Our percentage of visits resulting in DAwMP (18.8%) is lower than that obtained by other studies carried out with the same methodology in another part of Spain, where 47.9% was obtained.11 It is also lower than those reported in other countries,4 which may indicate that the recent campaigns to reduce inappropriate use of antibiotics have been effective. We believe that the comparison of studies using SPs should be done cautiously. The symptomatology and levels of pressure used may differ. SPs even frequently request the antibiotic for a family member, which can affect DAwMP.
We also found that DAwMP was lower than that obtained in a survey in a nearby area (65%).7 This may be due to various aspects: the study included dispensing for other infections (urinary tract, dental infections) and a cumulative percentage was obtained, such that a pharmacist could be classified as carrying out DAwMP even if he or she only did so occasionally (for example, for a regular customer).
As in a medical consultation, the patient's pressure is decisive in obtaining an antibiotic.13 We also found higher DAwMP in rural areas. This may be because there are no nearby continuous medical care centres, which was also observed in a study in the same setting.7 However, antibiotics were obtained at lower levels of pressure in urban areas, perhaps because these areas are more commercial or the professionals bear a greater workload, which could lead to a poorer quality of dispensing.14
This study also allowed pharmaceutical care to be rated. Almost three-quarters of the pharmacies suggested consulting a doctor. In some cases, they referred the patient directly to the doctor without offering any product over the counter, because they considered the diagnosis doubtful. Increasing access of pharmacists to clinical guidelines on respiratory infections might be beneficial for the health system. Pharmacies would act like a screening test, decreasing the demand for consultation in primary care and/or emergency wards for common and self-limiting diseases. If educational interventions were carried out conjointly in pharmacies and the general population (to decrease erroneous knowledge on antibiotics),15 the inappropriate use of antibiotics could be reduced.
Strengths and limitations
As strengths, we stress that this is the SP study with the largest sample size that we know of,4,16 and that the sampling was exhaustive. The visits were carried out in a short period of time (minimizing the impact of interventions that may have taken place at the same time) and there were no differences in the number of antibiotics obtained by the four actors. In addition, by using SPs rather than surveys we avoided the social desirability bias17,18 (obtaining socially accepted answers) and this allowed appraisal of the effect of patient pressure.
As limitations, it should be noted that the number of antibiotics obtained without a medical prescription can vary for regular customers and according to the type of infection the SP claims to have.
Conclusions
Reducing self-medication with antibiotics is essential in the fight against drug resistance. This study shows that 19% of pharmacies still carry out DAwMP at the insistence of a client and it has identified the rural area as a risk factor. Interventions aimed at reducing dispensing of non-prescribed antibiotics should be carried out, prioritizing them in rural pharmacies.
Supplementary Material
Acknowledgements
We would like to thank the four SPs for their work and Virginia Navascues for her assistance with the English text.
Funding
This study was supported by a Health Research Fund (Fondo de Investigación Sanitaria) grant (PI15/00844) from the Carlos III Health Institute (Instituto de Salud Carlos III). The funder had no role in the study design, data collection and analysis, or decision to publish.
Transparency declarations
None to declare.
Author contributions
M. Z.-C., A. F., M. C. G., M. P.-L., P. L.-V. and J. M. V.-L. designed the study; the fieldwork was coordinated by M. Z.-C., M. P.-L. and A. F.; M. Z.-C. undertook database management and statistical analysis; interpretation of the statistical analysis was performed by M. Z.-C., M. P.-L. and A. F.; and the text was drafted by M. Z.-C. and A. F.; and discussed in depth with M. P.-L., M. C. G., P. L.-V. and J. M. V.-L.
References
- 1. Laxminarayan R, Duse A, Wattal C. et al. Antibiotic resistance—the need for global solutions. Lancet Infect Dis 2013; 13: 1057–98. [DOI] [PubMed] [Google Scholar]
- 2. O’Neill J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. 2014. https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf.
- 3. Von Wintersdorff CJH, Penders J, Stobberingh EE. et al. High rates of antimicrobial drug resistance gene acquisition after international travel, The Netherlands. Emerg Infect Dis 2014; 20: 649–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Morgan DJ, Okeke IN, Laxminarayan R. et al. Non-prescription antimicrobial use worldwide: a systematic review. Lancet Infect Dis 2011; 11: 692–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. ECDC. Summary of the Latest Data on Antibiotic Consumption in the European Union.2017. https://ecdc.europa.eu/sites/portal/files/documents/Final_2017_EAAD_ESAC-Net_Summary-edited%20-%20FINALwith%20erratum.pdf.
- 6. Campos J, Ferech M, Lázaro E. et al. Surveillance of outpatient antibiotic consumption in Spain according to sales data and reimbursement data. J Antimicrob Chemother 2007; 60: 698–701. [DOI] [PubMed] [Google Scholar]
- 7. Zapata-Cachafeiro M, González-González C, Váquez-Lago JM. et al. Determinants of antibiotic dispensing without a medical prescription: a cross-sectional study in the north of Spain. J Antimicrob Chemother 2014; 69: 3156–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Watson M, Norris P, Granas A.. A systematic review of the use of simulated patients and pharmacy practice research. Int J Pharm Pract 2006; 14: 83–93. [DOI] [PubMed] [Google Scholar]
- 9. Legido-Quigley H, Urdaneta E, Gonzalez A. et al. Erosion of universal health coverage in Spain. Lancet 2013; 382: 1977.. [DOI] [PubMed] [Google Scholar]
- 10. Caamaño F, Ruano A, Figueiras A. et al. Data collection methods for analyzing the quality of the dispensing in pharmacies. Pharm World Sci 2002; 24: 217–23. [DOI] [PubMed] [Google Scholar]
- 11. Guinovart MC, Figueras A, Llop JC. et al. Obtaining antibiotics without prescription in Spain in 2014: even easier now than 6 years ago. J Antimicrob Chemother 2015; 70: 1270–1. [DOI] [PubMed] [Google Scholar]
- 12. Llor C, Cots JM.. The sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin Infect Dis 2009; 48: 1345–9. [DOI] [PubMed] [Google Scholar]
- 13. Lopez-Vazquez P, Vazquez-Lago JM, Figueiras A.. Misprescription of antibiotics in primary care: a critical systematic review of its determinants. J Eval Clin Pract 2012; 18: 473–84. [DOI] [PubMed] [Google Scholar]
- 14. Caamaño F, Tomé-Otero M, Takkouche B. et al. Influence of pharmacists’ opinions on their dispensing medicines without requirement of a doctor’s prescription. Gac Sanit Sespas 2005; 19: 9–14. [DOI] [PubMed] [Google Scholar]
- 15. TNS Opinion & Social. Special Eurobarometer 445: Antimicrobial Resistance. Brussels, Belgium, 2016. https://ec.europa.eu/health/amr/sites/amr/files/eb445_amr_generalreport_en.pdf. [Google Scholar]
- 16. Chang J, Ye D, Lv B. et al. Sale of antibiotics without a prescription at community pharmacies in urban China: a multicentre cross-sectional survey. J Antimicrob Chemother 2017; 72: 1235–42. [DOI] [PubMed] [Google Scholar]
- 17. Peabody JW, Luck J, Glassman P. et al. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA 2000; 283: 1715–22. [DOI] [PubMed] [Google Scholar]
- 18. Brenner PS, DeLamater J.. Lies, damned lies, and survey self-reports? Identity as a cause of measurement bias. Soc Psychol Q 2016; 79: 333–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.