Abstract
Background:
Bipolar affective disorder (BAD) is a severe mental illness which results in serious lifelong struggles and challenges. The full impact of stressful life events (SLEs) on the course of BAD is poorly understood.
Materials and Methods:
A cross-sectional study was conducted on 128 consecutive patients with BAD currently admitted with a relapse. Our objectives were (1) to estimate the proportion, type, and timing of preonset SLEs in relapsed BAD patients and (2) to study the association between SLEs and selected clinical variables in this group. Semi-structured proforma, Young Mania Rating Scale, Hamilton Rating Scale for Depression, Presumptive Stressful Life Events Scale, and Brief Psychiatric Rating Scale were used. Statistical analysis was done using R software for Windows.
Results:
About 69.5% (89/128) of patients reported preonset SLEs – among which 50 (56.2%) had mania and 39 (43.8%) had depression. Conflict with in-laws and financial problems were the commonly reported SLEs. The mean duration between SLEs and the relapse was 19.73 ± 4.8 days. BPRS score was significantly high in subjects with preonset SLEs (P = 0.022). No significant association was detected between SLEs and the type of episode during relapse (P = 0.402).
Conclusion:
This study emphasizes the significance of SLEs in the relapse and longitudinal course of BAD. Understanding the association of SLEs and relapse in BAD will help in predicting further relapses and developing newer pharmacological and nonpharmacological measures targeting this aspect, thereby maximizing both symptom reduction and quality of life in patients with BAD.
Key words: Bipolar affective disorder, relapse, Southern India, stressful life events
INTRODUCTION
Bipolar affective disorder (BAD) is a complex, severe, disabling, recurrent, and multifactorial psychiatric illness that affects approximately 1% of the world's population.[1] Contrary to the classical teaching about its episodic course, in reality, several patients with BAD do not reach full interepisodic remission and continue to have residual subsyndromal symptomatology, leading to functional impairment and impaired quality of life.[1] Convincing evidence exists for the role of genetic risk factors on the onset and course of this disorder. As inferred from epigenetic studies, the genetic vulnerability is potentiated by early-life events, which then act as important determinants for the first clinical manifestations of the disease.[2]
In addition to the biological factors, psychosocial factors also influence the onset, type, timing, and outcome of affective episodes.[3] The term “life events” refers to any substantial changes in personal surroundings resulting in personal and social consequences. Life events might occur unexpectedly or in an anticipated manner.[4] Stressful life events (SLEs) are described as discrete quantifiable circumstances that can have a severe negative impact.[5]
Considerable literature seems to confirm an existing link between SLEs and BAD.[6,7,8,9,10] SLEs are more likely experienced by patients with BAD before the episodes than by nonpsychiatric controls and SLEs appear to be more prevalent before the relapse in patients with BAD in comparison to other time periods in their life.[6,7] Among all the SLEs, the role of loss – bereavement, interpersonal separations, loss of self-esteem, and other losses – is more emphasized in relation to relapse of mood disorders.[3] Some of the proposed mechanisms for the association between SLEs and BAD include early adversity sensitization, kindling/behavioral sensitization, hypothalamo-pituitary-adrenal (HPA) axis dysfunction, neurogenic hypothesis, and social rhythm disruption.[3,4,11,12,13,14]
SLEs have played key roles in inducing relapses and recurrences in BAD by causing unhealthy affective fluctuations.[15] SLEs have been found to be associated with the initiation of manic episodes (more than depressive episodes), earlier episodes (rather than later episodes), and early onset of illness in bipolar patients.[16] In relapsed BAD patients, the SLEs preceding manic relapse were mainly related to social life (e.g., afraid of defamation, loss of social prestige) and goal attainment, whereas those preceding depressive relapses were mostly related to personal life (e.g., the death of loved one).[3,17] Expressed emotions and chronic stress were polarity-specific predictors of depressive recurrence, although episodic stress was a predictor of both manic and depressive recurrence.[9] The time-frame for SLEs' precipitating relapse of BAD has been proposed to be 4 weeks for manic and 6 months for depressive relapses. The presence of a stressor predicted a longer time to functional recovery in life domains: up to 112 days in work/school in bipolar patients.[1] There are several studies, on the contrary, which did not find any significant relationship between SLEs and bipolar disorder.[18,19,20,21] Even though positive studies outnumber negative studies, it is difficult to establish a causal link between SLEs and BAD, not only because of the large methodological variability of these studies and their results but also because the SLEs may be the consequence, rather than the cause, of the illness.[9]
The Indian population, which is currently pacing through the rapid change phase of industrialization and urbanization, is subjected to the increased psychological stress of modern life, which, in turn, might contribute to the causation of mental illnesses, including mood disorders, among the vulnerable. There are only limited studies from India regarding the role of SLEs in bipolar disorder.[3,15,22,23,24]
The primary objective of this research is to estimate the proportion, type, and timing of preonset SLEs in relation to relapse in BAD. We also planned to study the association between SLEs and selected clinical variables among relapsed patients with BAD, which was kept as our secondary objective.
This study emphasizes the need for exploring the SLEs in relapsed BAD patients. Understanding the association of SLEs with relapse in BAD will help in predicting further such relapses and developing newer pharmacological and nonpharmacological measures targeting this aspect, thereby maximizing both symptom reduction and quality of life in patients with BAD.
MATERIALS AND METHODS
This was a cross-sectional study in which 128 consecutive patients admitted in psychiatry ward of MOSC Medical College, Kolenchery, Kerala, India, between March 2016 and September 2017, with relapse of BAD, who met the inclusion criteria, constituted the study sample. The sample size calculated based on estimate of proportion with α =5%, p = 33%,[25] and d = 10% using the given formula was 85:
As the total number of consecutive patients who met the inclusion criteria during the stipulated study period was 128, we preferred the higher among the two sample sizes.
Operational definitions
These definitions were operationalized for this study by the authors, after reviewing certain previous studies.[26,27,28,29]
Relapse
Worsening or reoccurrence of manic, depressive, or mixed affective signs and symptoms after a period of eight weeks of a premorbid level of functioning.
Preonset period
One month period back from the day of onset of symptoms, that is, the day on which the informant started recognizing that the patient is obviously abnormal and needs intervention.
Inclusion criteria
All patients in the age group of 18–60 years belonging to either sex, who got admitted to the psychiatry ward with a relapse, and having a diagnosis of BAD – current episode manic/depressive/mixed (F31.1, F31.2, F31.3, F31.4, F31.5, F31.6) based on International Classification of Diseases – 10th Edition Diagnostic Criteria for Research (ICD-10 DCR) classification of Mental and Behavioral disorders, were recruited. Written informed consent was obtained from the patient and/or relative if the patient lacked the capacity to give valid consent. For such patients, when they regained that capacity, the consent was taken from them in addition to their relatives.
Exclusion criteria
Clinically diagnosed cases of delirium, organic mood (affective) disorder, mental retardation, end-stage medical illnesses (chronic kidney disease, chronic liver disease, congestive heart failure), and newly diagnosed cases of BAD were excluded. The newly diagnosed cases of BAD were excluded to retain the uniformity of the study group – which should contain definite BAD cases who were on standard regime for BAD as per the institution protocol when they relapsed, and the hospital records were cross-checked to determine whether the relapse met the operational criteria as per this study.
Assessment
The ICD-10 DCR was used to diagnose BAD in the subjects.[30] The following tools were used for assessment:
Presumptive Stressful Life Events Scale (PSLES)[31]
Hamilton Rating Scale for Depression (HAM-D)[32]
Young Mania Rating Scale (YMRS)[33]
Brief Psychiatric Rating Scale (BPRS).[34]
A semi-structured proforma was used to collect data regarding sociodemographic and clinical variables such as details of the current episode, the timing of SLEs, substance use, family history, medical comorbidities, PSLES, BPRS, HAM-D, and YMRS scores at intake and follow-up.
Procedure
The study protocol got approval from the Institutional Ethics Committee. The sociodemographic and clinical details were recorded using the semi-structured proforma. YMRS or HAM-D (depending on the polarity of the affective episode during relapse) and BPRS were administered at intake to assess the severity of relapse. These scales were reapplied at the time of clinical remission (i.e., when the patients ceased to exhibit any mood symptoms), either at the time of discharge or during subsequent out-patient department follow-ups, to check whether YMRS became <12 or HAM-D <7, to confirm the remission. PSLES was administered to quantify the preonset SLEs when the patients reached remission – both clinically and when YMRS became <12 or HAM-D <7. The proportion, type, and timing of the preonset SLEs were estimated. The relationship between preonset SLEs and variables such as the type of affective episode in relapse, the severity of current episode (YMRS, HAM-D, BPRS scores), and duration of inpatient stay during the relapse were analyzed.
Statistical analysis
Chi-square test was done to study the association between SLEs and selected categorical variables. We compared the duration of inpatient stay and YMRS, HAM-D, and BPRS scores in the two groups – the groups with and without preonset SLEs – using Mann–Whitney U test, as the data violated normality assumption. P < 0.05 was considered statistically significant. Statistical analyses were performed using R software for Windows.
RESULTS
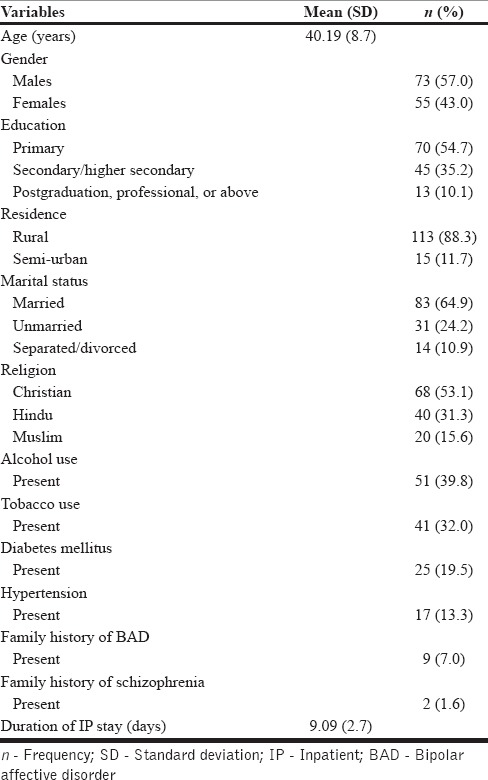
Sociodemographic and clinical characteristics of the study group are recorded in Table 1. About 69.5% (89/128) of the relapsed BAD patients had SLEs in the preonset period. About 72.6% (53/73) of the relapsed males reported preonset SLEs versus 65.5% (36/55) of the relapsed females – the difference was, however, not statistically significant (χ2 = 0.46, P = 0.49).
Table 1.
Sociodemographic and clinical characteristics of the study group
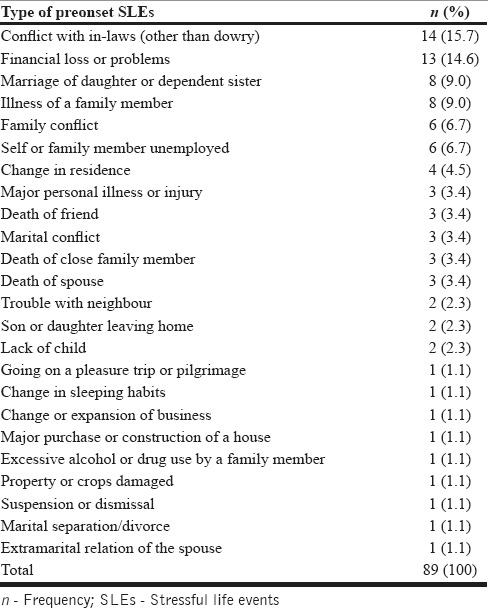
The most frequent SLEs reported were a conflict with in- laws (16%) and financial loss or problems (15%) [Table 2]. When males and females were considered separately, financial loss or problems, conflicts with in-laws (other than dowry), unemployment of self or a family member, and marriage of daughter or dependent sister were the most frequent SLEs among males, whereas females reported conflicts with in-laws (other than dowry), family conflict, and illness of family member as the commonly occurring SLEs. The mean duration between the SLEs and relapse was 19.73 ± 4.9 days.
Table 2.
Type and distribution of preonset stressful life events
Among those with preonset SLEs, 56.2% (50/89) had mania and 43.8% (39/89) had depression. Of all the BAD relapses, 66.7% (50/75) of the manic episodes had preonset SLEs when compared with 73.6% (39/53) of the depressive episodes. The association between SLEs and the type of affective episode during relapse was not statistically significant (χ2 = 0.413, P = 0.52). About 34.8% (31/89) of the relapsed patients with preonset SLEs had psychotic symptoms on mental status examination, whereas only 20.5% (8/39) of those without preonset SLEs had psychotic symptoms. However, the association was not statistically significant (χ2 = 1.99, P = 0.158).
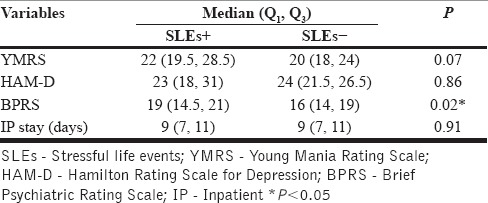
BPRS score was found to be significantly higher in bipolar patients with preonset SLEs (P = 0.022) [Table 3].
Table 3.
Comparison of clinical variables among relapsed bipolar affective disorder patients with and without preonset stressful life events
DISCUSSION
The study group consisted of middle-aged patients, with a mean age of 40.19 ± 8.7 years, comparable to similar previous studies.[15,35,36] Nearly 70% (89 of 128) of the patients experienced SLEs within 1 month prior to the relapse. This suggests a rather stable and high prevalence of SLEs during the preonset period of relapse, which was also reported in other studies.[10,23]
Among the 128 consecutive patients, 75 (58.6%) had mania, whereas 53 (41.4%) had depression. The proportion of relapsed subjects with preonset SLEs in our study was greater for patients with mania (56.2%) than depression (43.8%). Among the total sample of relapsed patients and those with relapse who had preonset SLEs, mania seemed to outnumber depression in contrast to the depression-predominant course patterns of BAD witnessed in Western literature.[25,37] The overrepresentation of mania in relapsed bipolar patients is replicated in similar reports, mostly from tropical regions, like India, Nigeria, and Hong Kong, which is hypothesized to be due to the effects of bright sunlight and a less variable day–night cycle on the zeitgeber.[24] We took remitted patients for analyzing SLEs as studies pointed out that the affective symptoms present during the relapse can influence and color the reporting of SLEs.[15]
In this study, conflict with in-laws (other than dowry), financial loss or problems, illness of family member, marriage of daughter or dependent sister, unemployment in self or family member, and family conflicts were the most frequently reported SLEs implicated in the relapse of BAD. This finding is concurrent with the existing global literature.[15,23,38,39] In a comparative study of family interactions of patients with schizophrenia or BAD, Miklowitz et al. reported that patients with BAD, especially those with relatives having high verbal interactional behaviors, often took a predominantly externalizing, refusing attitude in interactions and frequently opposed the opinions, criticisms, or suggestions expressed by relatives, often resulting in a conflictual interaction rather than domestic violence which occurs during manic episodes.[40] In addition, the emotional dynamics within the family and negative expressed emotions also contribute to family conflicts.[40] The differences in the kinds of SLEs leading to the relapse in BAD could be due to different methodology, region, season, cultural factors, or the use of different rating scales for quantifying SLEs and the different preonset time periods considered in various studies.
The mean time period between pre-onset SLEs and relapse was 19.73 ± 4.9 days in our study. The effect of those SLEs which occurred shortly before relapse indicates that such life events have an acute, rather than a delayed effect on the risk of relapse and/or that SLEs per se and not other etiological factors (e.g., comorbid personality disorder, substance use) can act as triggers for more affective relapses.[10]
Although we did not find any significant association between SLEs and the type of affective episode during relapse as well as the intensity of manic or depressive symptoms during relapse, psychotic symptoms were more commonly, but not significantly, present in the relapsed affective episodes of those who reportedly had preonset SLEs. This could be interpreted as one of the impacts of SLEs on the clinical course of BAD, as psychotic features indicate a more severe course of illness.[4] BPRS scores were found to be significantly higher in the group with preonset SLEs, but further interpretations are limited as we did not perform an item-wise comparison of BPRS scores in the two groups.
A few researchers have proposed moderators of life stress in BAD. Certain factors such as interpersonal dependency, introversion, and obsessionality have been found to increase the risk for relapse after a negative SLE, whereas interpersonal events, interpersonal dependency, and the interaction of these two factors have been found to predict higher symptom severity scores and faster relapse in BAD. In addition, female gender and cognitive vulnerability can predict depressive symptoms after negative SLEs, whereas cognitive vulnerability and pre-event hypomanic symptoms can act as predictors for manic symptoms after life events.[41]
Including clinically as well as rating scale score-wise remitted patients for analyzing SLEs, without allowing the affective or psychotic symptoms to influence the reporting of SLEs, is one of the strengths of our study. Our study had several limitations also. The sample constituted by inpatients from a tertiary care teaching hospital would not represent patients with BAD in the general population. The causality of the particular SLEs leading on to the current relapse could not be established because of the cross-sectional study design. Life events can very well be associated with either the causation of or a consequence of mood episodes, which will be difficult to distinguish. Treatment adequacy and adherence could be independent predictors of relapse in BAD, which were not quantified in our study. We studied only a limited number of variables associated with SLEs and relapse in BAD. We had restricted the SLEs to those included in PSLES strictly; hence, the effects of more remote stressful events, such as childhood trauma, which may affect an individual's sensitivity to stressors in adult life,[22] were not examined. Some of the data were gathered retrospectively and may, thus, be distorted by recall.
Of recent, there is a growing interest in defining and exploring the factors leading to relapse in BAD and in discovering newer interventions based on these parameters. Several important avenues for future research need to be mentioned, such as exploration of the influence of personality profile and cognitive factors[3] of the patients (e.g., attribution styles, perfectionism, problem-solving skill deficits, maladaptive schemata and coping styles), subtype of BAD, social support, subjective experience of SLEs, severity and critical timing of SLEs, and building consensus on the most reliable as well as valid phenotyping and assessment tools, to design more and more prospective community-based research plans with truly large sample sizes – all of which will ultimately result in reduction in the chances of relapse and recurrences, thereby enhancing the functional recovery and quality of life in patients with BAD.[4]
CONCLUSION
SLEs, predominantly family conflicts and finance-related problems, were present in a significant proportion of relapsed BAD patients.
Assessing life events can be of great help in future to plan strategic interventions to combine pharmacotherapy with psychotherapies based on psychoeducation and interpersonal, family, and cognitive–behavioral interventions which focus on addressing the SLEs, coping with them effectively, alleviating their negative impact in terms of symptom reduction, delay of recurrence, as well as modifying interpersonal functioning and even preventing negative life events by anticipating and mitigating the ways in which individuals' symptoms, characteristics, and circumstances may contribute to the occurrence of acute events.[1] BAD is a major health concern, both for the individual and for the society, and more information is still needed about the factors leading on to its relapses.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors wish to acknowledge with deep gratitude the guidance and help offered by Dr. Kalesh M Karun (PhD), Assistant Professor, Department of Bio-statistics, MOSC Medical College, Kolenchery, during statistical analysis of the data. Also, they express their heartfelt gratitude toward their colleagues and all those subjects and their family members who participated in this study for their kind co-operation and goodwill.
REFERENCES
- 1.Yan-Meier L, Eberhart NK, Hammen CL, Gitlin M, Sokolski K, Altshuler L, et al. Stressful life events predict delayed functional recovery following treatment for mania in bipolar disorder. Psychiatry Res. 2011;186:267–71. doi: 10.1016/j.psychres.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bergink V, Larsen JT, Hillegers MH, Dahl SK, Stevens H, Mortensen PB, et al. Childhood adverse life events and parental psychopathology as risk factors for bipolar disorder. Transl Psychiatry. 2016;6:e929. doi: 10.1038/tp.2016.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumari A, Jahan M. Distressful life events in affective disorder. J Indian Acad Appl Psychol. 2006;32:193–200. [Google Scholar]
- 4.Aldinger F, Schulze TG. Environmental factors, life events, and trauma in the course of bipolar disorder. Psychiatry Clin Neurosci. 2017;71:6–17. doi: 10.1111/pcn.12433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Low NC, Dugas E, O'Loughlin E, Rodriguez D, Contreras G, Chaiton M, et al. Common stressful life events and difficulties are associated with mental health symptoms and substance use in young adolescents. BMC Psychiatry. 2012;12:116. doi: 10.1186/1471-244X-12-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glassner B, Haldipur CV, Dessauersmith J. Role loss and working-class manic depression. J Nerv Ment Dis. 1979;167:530–41. doi: 10.1097/00005053-197909000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Kennedy S, Thompson R, Stancer HC, Roy A, Persad E. Life events precipitating mania. Br J Psychiatry. 1983;142:398–403. doi: 10.1192/bjp.142.4.398. [DOI] [PubMed] [Google Scholar]
- 8.Miklowitz DJ, Goldstein MJ, Nuechterlein KH, Snyder KS, Mintz J. Family factors and the course of bipolar affective disorder. Arch Gen Psychiatry. 1988;45:225–31. doi: 10.1001/archpsyc.1988.01800270033004. [DOI] [PubMed] [Google Scholar]
- 9.Bries A, Reynaert C, Zdanowicz N. Could bipolarity be influenced by stressful life events? A reflection based on a case report. Psychiatr Danub. 2014;26(Suppl 1):31–5. [PubMed] [Google Scholar]
- 10.Simhandl C, Radua J, König B, Amann BL. The prevalence and effect of life events in 222 bipolar I and II patients: A prospective, naturalistic 4 year follow-up study. J Affect Disord. 2015;170:166–71. doi: 10.1016/j.jad.2014.08.043. [DOI] [PubMed] [Google Scholar]
- 11.Lau BW, Lee JC, So K. Neurogenic hypothesis and psychiatric disorders. Chin Sci Bull. 2013;58:3188–98. [Google Scholar]
- 12.Dienes KA, Hammen C, Henry RM, Cohen AN, Daley SE. The stress sensitization hypothesis: Understanding the course of bipolar disorder. J Affect Disord. 2006;95:43–9. doi: 10.1016/j.jad.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Urosević S, Abramson LY, Harmon-Jones E, Alloy LB. Dysregulation of the behavioral approach system (BAS) in bipolar spectrum disorders: Review of theory and evidence. Clin Psychol Rev. 2008;28:1188–205. doi: 10.1016/j.cpr.2008.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malkoff-Schwartz S, Frank E, Anderson BP, Hlastala SA, Luther JF, Sherrill JT, et al. Social rhythm disruption and stressful life events in the onset of bipolar and unipolar episodes. Psychol Med. 2000;30:1005–16. doi: 10.1017/s0033291799002706. [DOI] [PubMed] [Google Scholar]
- 15.Subramanian K, Sarkar S, Kattimani S, Philip Rajkumar R, Penchilaiya V. Role of stressful life events and kindling in bipolar disorder: Converging evidence from a mania-predominant illness course. Psychiatry Res. 2017;258:434–7. doi: 10.1016/j.psychres.2017.08.073. [DOI] [PubMed] [Google Scholar]
- 16.Beyer JL, Kuchibhatla M, Cassidy F, Krishnan KR. Stressful life events in older bipolar patients. Int J Geriatr Psychiatry. 2008;23:1271–5. doi: 10.1002/gps.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson SL, Cueller AK, Ruggero C, Winett-Perlman C, Goodnick P, White R, et al. Life events as predictors of mania and depression in bipolar I disorder. J Abnorm Psychol. 2008;117:268–77. doi: 10.1037/0021-843X.117.2.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hall KS, Dunner DL, Zeller G, Fieve RR. Bipolar illness: A prospective study of life events. Compr Psychiatry. 1977;18:497–502. doi: 10.1016/0010-440x(77)90050-5. [DOI] [PubMed] [Google Scholar]
- 19.Chung RK, Langeluddecke P, Tennant C. Threatening life events in the onset of schizophrenia, schizophreniform psychosis and hypomania. Br J Psychiatry. 1986;148:680–5. doi: 10.1192/bjp.148.6.680. [DOI] [PubMed] [Google Scholar]
- 20.Sclare P, Creed F. Life events and the onset of mania. Br J Psychiatry. 1990;156:508–14. doi: 10.1192/bjp.156.4.508. [DOI] [PubMed] [Google Scholar]
- 21.McPherson H, Herbison P, Romans S. Life events and relapse in established bipolar affective disorder. Br J Psychiatry. 1993;163:381–5. doi: 10.1192/bjp.163.3.381. [DOI] [PubMed] [Google Scholar]
- 22.Shaik S, Rajkumar RP, Menon V, Sarkar S. Gender, life events, and depression: An exploratory study. Indian J Psychol Med. 2017;39:330–5. doi: 10.4103/0253-7176.207339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yadav R, Kandre D. Stressful life events in bipolar mood disorder. Int J Res Med. 2016;5:109–14. [Google Scholar]
- 24.Subramanian K, Sarkar S, Kattimani S. Bipolar disorder in Asia: Illness course and contributing factors. Asian J Psychiatr. 2017;29:16–29. doi: 10.1016/j.ajp.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 25.Malkoff-Schwartz S, Frank E, Anderson B, Sherrill JT, Siegel L, Patterson D, et al. Stressful life events and social rhythm disruption in the onset of manic and depressive bipolar episodes: A preliminary investigation. Arch Gen Psychiatry. 1998;55:702–7. doi: 10.1001/archpsyc.55.8.702. [DOI] [PubMed] [Google Scholar]
- 26.Hirschfeld RM, Calabrese JR, Frye MA, Lavori PW, Sachs G, Thase ME, et al. Defining the clinical course of bipolar disorder: Response, remission, relapse, recurrence, and roughening. Psychopharmacol Bull. 2007;40:7–14. [PubMed] [Google Scholar]
- 27.Leff JP, Fischer M, Bertelsen A. A cross-national epidemiological study of mania. Br J Psychiatry. 1976;129:428–42. doi: 10.1192/bjp.129.5.428. [DOI] [PubMed] [Google Scholar]
- 28.Hunt N, Bruce-Jones W, Silverstone T. Life events and relapse in bipolar affective disorder. J Affect Disord. 1992;25:13–20. doi: 10.1016/0165-0327(92)90088-n. [DOI] [PubMed] [Google Scholar]
- 29.Ambelas A. Psychologically stressful events in the precipitation of manic episodes. Br J Psychiatry. 1979;135:15–21. doi: 10.1192/bjp.135.1.15. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva: World Health Organization; 1993. pp. 89–103. [Google Scholar]
- 31.Singh G, Kaur D, Kaur H. Presumptive stressful life events scale (psles) – A new stressful life events scale for use in India. Indian J Psychiatry. 1984;26:107–14. [PMC free article] [PubMed] [Google Scholar]
- 32.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 34.Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10:790–812. [Google Scholar]
- 35.Chatterjee S, Kulhara P. Symptomatology, symptom resolution and short term course in mania. Indian J Psychiatry. 1989;31:213–8. [PMC free article] [PubMed] [Google Scholar]
- 36.Kemner SM, van Haren NE, Bootsman F, Eijkemans MJ, Vonk R, van der Schot AC, et al. The influence of life events on first and recurrent admissions in bipolar disorder. Int J Bipolar Disord. 2015;3:6. doi: 10.1186/s40345-015-0022-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry. 2002;59:530–7. doi: 10.1001/archpsyc.59.6.530. [DOI] [PubMed] [Google Scholar]
- 38.El Kissi Y, Krir MW, Ben Nasr S, Hamadou R, El Hedda R, Bannour S, et al. Life events in bipolar patients: A comparative study with siblings and healthy controls. J Affect Disord. 2013;151:378–83. doi: 10.1016/j.jad.2013.05.098. [DOI] [PubMed] [Google Scholar]
- 39.Hosang GM, Korszun A, Jones L, Jones I, McGuffin P, Farmer AE, et al. Life-event specificity: Bipolar disorder compared with unipolar depression. Br J Psychiatry. 2012;201:458–65. doi: 10.1192/bjp.bp.112.111047. [DOI] [PubMed] [Google Scholar]
- 40.Miklowitz DJ, Goldstein MJ, Nuechterlein KH. Verbal interactions in the families of schizophrenic and bipolar affective patients. J Abnorm Psychol. 1995;104:268–76. doi: 10.1037//0021-843x.104.2.268. [DOI] [PubMed] [Google Scholar]
- 41.Johnson SL. Life events in bipolar disorder: Towards more specific models. Clin Psychol Rev. 2005;25:1008–27. doi: 10.1016/j.cpr.2005.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]


