Abstract
Background:
Bipolar affective disorder (BPAD) is an episodic psychiatric disorder that is associated with considerable morbidity. Psychiatrists have found it difficult to treat the disorder owing to the variety of presentation and variety of challenges in clinical decision-making. To guide the clinicians, the concept of predominant polarity (PP) in BPAD has become important. This review was conducted to understand the definition, epidemiology, relationship with sociodemographic and clinical parameters, and implications of PP in BPAD.
Methodology:
The review was conducted after selecting 17 original research studies from PubMed using appropriate search terms.
Results:
There is no consensus definition of PP. Epidemiological data showed varied results, although most common PP demonstrated in most studies was depressive polarity. The relation between sociodemographic and clinical parameters also lacked uniformity, although certain patterns could be identified in their relationships. The implications of PP in diagnostics, treatment, and classificatory system are discussed.
Conclusion:
PP in BPAD conveys clinically important information that aids a clinician in decision-making. Further studies are required so that we can understand the neurobiological underpinning of the concept.
Key words: Bipolar disorder, depression, DSM 5, mania, predominant polarity
INTRODUCTION
Bipolar affective disorder (BPAD) is one of the widely prevalent mental disorders, with a lifetime prevalence of 2.4%.[1] BPAD usually follows an episodic course with the occurrence of recurrent (at least one) manic, hypomanic, or mixed episode in conjunction with depressive episodes, with varying degrees of interepisodic remission. A significant amount of the lifetime of patients with BPAD is spent in suffering from affective symptoms,[2] with a higher chance of time being spent in depressive episodes. The disorder is also highly associated with suicidality and medical comorbidities. However, data from various Asian centers, including India, tend to differ on this front. Studies[3,4] from this region have shown that patients with BPAD tend to have a course predominantly characterized by manic episodes. Such patients with predominant manic episodes, though they tend to have a higher chance of syndromal recovery, also have a higher chance of relapse.[5] Thus, it can be said that the course and outcome of BPAD show significant interpatient variation, as a result of which the clinical decision-making in BPAD remains complicated.
For a long time, researchers have been trying to find proxy clinical markers that could reliably predict the future course of BPAD. One such marker was the polarity of the first episode. A retrospective study done on 150 patients with BPAD from India, using the retrospective life chart method, found out that in around 85% of the cases, mania was the first episode and also the most frequent episode.[4] The finding was further supported by another study[6] which also showed that patients presenting with first-episode mania tended to have more manic episodes subsequently. But soon it became apparent that there is a need for better predictive entities. Various studies thus adopted a longitudinal observation of the course of the illness. The initial studies done on patients with BPAD-I and BPAD-II showed an overwhelming depressive presentation.[7,8] But the studies from the tropical regions showed a stark difference and there the manic presentation was more prevalent.[4] The developments in psychopharmacology complemented these findings. Newer classification divided drugs as Class A (stabilizers from above), Class B (stabilizer from below), and Class C (stabilizer from euthymia).[9] Experts speculated that the trick to effective management of BPAD lies in the fact that if we can obtain clinical information that will enable us to reliably predict the course of the disorder, that will allow us to tailor our prophylactic treatment approaches.[10]
The concept of predominant polarity (PP) of BPAD is important in this context. The concept was first described by Angst[11] while describing the course of 95 patients with BPAD followed up for more than 16 years. He classified the patients into three classes: “preponderantly manic,” “preponderantly depressed,” and “nuclear.” However, even before that attempt, Leonhard, in his sample of 117 patients with BPAD, had shown that 17.9% had a predominantly manic presentation, 25.6% had a predominant depressive presentation, and 56.4% had an equivocal presentation. Subsequently, the entity of PP in BPAD has generated sufficient interest in the researchers. This review was hence conducted to collect the available evidence regarding PP in BPAD.
METHODOLOGY
A search was conducted on PubMed to address the following research questions:
What has been the accepted definition of PP in BPAD in the literature?
What is the epidemiology of PP in BPAD?
What is the relation of PP with sociodemographic and clinical parameters of patients with BPAD?
What are the implications of determination of PP in BPAD?
A search was conducted on US National Library of Medicine's PubMed/MEDLINE using the following search terms: “Bipolar affective disorder,” “Bipolar disorder,” “mood disorder,” “predominant polarity,” “mania,” “hypomania,” “depression.” Appropriate medical subject heading terms (MeSH) were accessed and used. The terms “Bipolar Disorder” [Mesh] AND “predominant polarity” were added to the search builder and articles were accessed. No restriction was placed regarding the time of publication. A secondary search was conducted among the references of the studies, and appropriate studies were accessed.
Study selection
For the purpose of this article, only original articles were included. The abstracts of the studies were initially screened, and full texts of the selected studies were accessed. Only articles whose full text could be accessed and were in English language were included in this review. Overall, 17 article were selected for this review [Figure 1].
Figure 1.
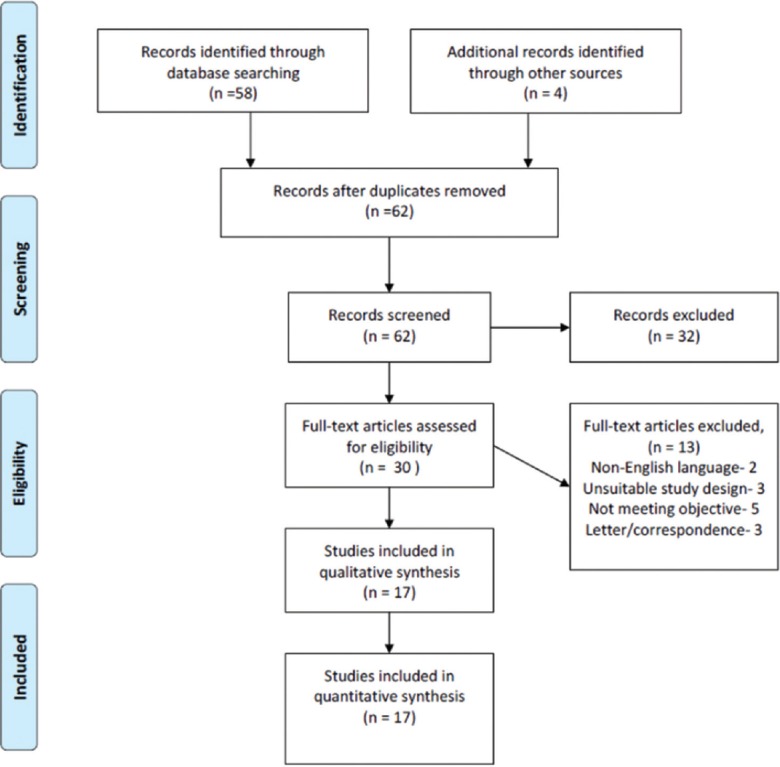
Results of literature search
RESULTS
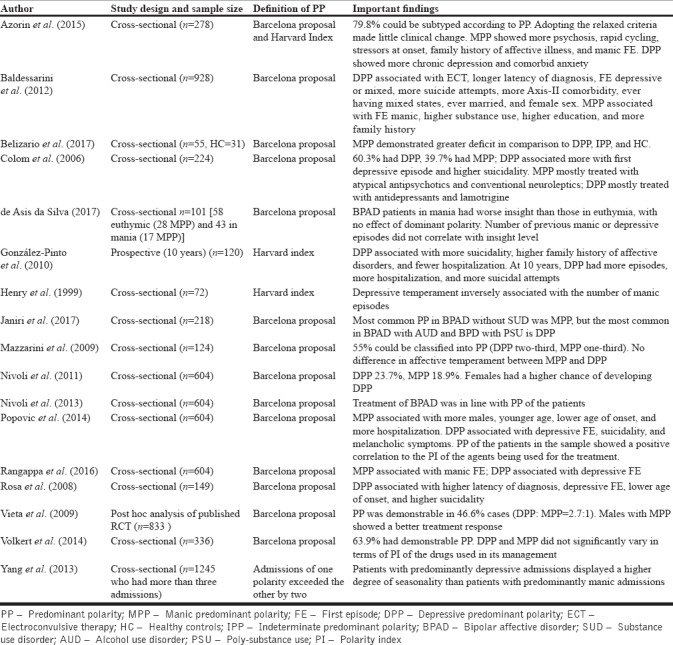
Table 1 describes the studies that have been included in this review. The evidence from the included studies has been hereby arranged so as to address the initial research questions:
Table 1.
Summary of the studies included in the review
Definition
One of the major points of contention among the studies included the definition used to classify patients according to PP. The most frequently used criteria were those proposed by Colom et al.,[12] where if two-thirds of the episode is of a particular polarity, the PP of that patient is the corresponding PP. This is also considered as the strict criteria or the Barcelona proposal. On the basis of these criteria, the patients can be classified as manic PP (two-thirds of the episode are manic/hypomanic), depressive PP (two-thirds of the episodes are depressive), or indeterminate PP (neither of the polarity has a two-thirds majority). To clarify, if a patient has had three manic/hypomanic episodes and one depressive episode in the lifetime, then the PP of the patient is manic PP. The other criteria that have also been used, considered the relaxed criteria, are when any one of the polarities of the episodes gain a 51% majority, the PP of the patient is the corresponding polarity.[13] This criterion is also called the Harvard index. Evidently, Harvard index has less diagnostic stability when compared with the Barcelona proposal. But the Barcelona proposal is considered by many as too restrictive, where around 38%–44% of the patients could not be assigned a PP.[14] The two sets of criteria were compared in one study[15] which showed that the relaxed criteria allowed more patients to be allotted in either manic PP or depressive PP, but that did not significantly change the predictive information gained.
Another source of debate has been the status of the mixed episodes. Many studies had considered the mixed episodes in the calculation in the denominator, but the mixed episodes were assigned to neither polarity for the sake of calculation according to the previously mentioned criteria.[16] A few other studies[15] had included mixed episodes under the purview of “mania-like episodes” and had calculated accordingly. The Diagnostic and Statistical Manual 5th edition (DSM 5)[17] has removed the diagnostic entity of bipolar I disorder, mixed episode, which required simultaneously meeting criteria for mania and depression and has added a specifier instead “with mixed features.” Thus, further discussion in this regard can be considered redundant.
Epidemiology
The epidemiological studies on PP in BPAD have been largely inconclusive, failing to provide us with any trend. A multicentric study conducted across five centers, namely, Barcelona, Catalonia (Spain); Belmont, Massachusetts (USA); Buenos Aires, (Argentina); Cagliari, Sardinia (Italy); and Bundang, Gyeonggi (Korea), including 928 patients with BPAD-I, found that 199 (21.4%) had manic PP, 290 (31.25%) had depressive PP, and 439 (47.3%) had indeterminate PP.[15] An Indian study that included 285 patients with BPAD-I[18] showed that the prevalence of manic PP in the sample was 79.3%, whereas the prevalence of depressive PP was only 13.7%. Another study[16] conducted in Germany in a sample of 336 patients with BPAD-I and BPAD-II showed that 169 (50.3%) had depressive PP and 46 (13.7%) had manic PP, whereas the rest had indeterminate PP. Another study from Barcelona, Spain,[12] conducted on 224 patients with BPAD, showed that 135 (60.3%) had depressive PP and 89 (39.7%) had manic PP.
Factors associated with predominant polarity
The studies have been able to provide evidence that certain sociodemographic and clinical parameters are associated with PP which are summarized in Table 2.
Table 2.
Relationship of predominant polarity of bipolar disorder with sociodemographic and clinical parameters
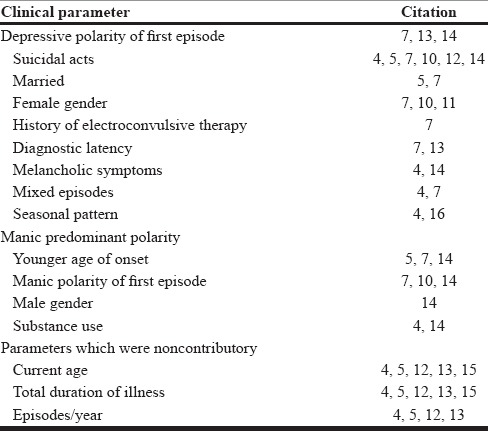
The general trend shown by the studies was that patients with a predominant depressive polarity usually had a higher chance of being female,[15,18,19] though certain other studies[12,13,20,21] could not replicate this finding. These patients usually had a depressive episode as their first episode[15,21,22] and a longer latent period before the disorder is diagnosed. The course of illness in these patients is usually characterized by melancholic symptoms,[12,22] mixed episodes,[12,15] and a seasonal pattern.[12] These patients were likely to have a history of suicidal acts[12,13,15,18,20,22] and receiving electroconvulsive therapy.[15]
The patients with a manic PP tended to have an earlier age of onset[13,15,22] and male gender.[22] However, many other studies failed to show male gender preponderance in manic PP.[12,15,23] These patients also usually had a manic episode as their first episode[15,18,22] and a higher prevalence of substance use.[12,22]
The relationship between seasonal pattern and predominant polarity
It has already been mentioned in the previous section that patients with depressive PP tended to show a seasonal pattern when compared with patients with manic PP.[12,24] One of the studies which explained this result had followed up an inpatient cohort of 9619 patients with BPAD.[24] The study also showed that other than PP, the polarity of the first episode can also predict the development of seasonal pattern in these patients. A mixed polarity followed by a depressive polarity of the first episode was associated more with the seasonal pattern when compared with a manic index episode.
The relationship between temperament and predominant polarity
A few studies tried to examine the relationship between PP and affective temperament. In their study, Henry et al.[25] provided some rudimentary evidence that hyperthymic temperament was positively correlated with a higher number of manic episodes and depressive temperament was correlated with a higher number of depressive episodes. However, the study was not conducted using the concept of PP. Subsequently, Mazzarini et al.[20] compared the temperament between patients with BPAD [depressive PP (n = 22) vs manic PP (n = 47)] and unipolar depressive disorders (n = 19). They found that patients with depressive PP or manic PP did not have any significant differences in terms of temperament. One possible reason behind this could be the fact that the study did not have a large enough sample size to garner enough power. But patients with BPAD had significantly less depressive temperament and higher cyclothymic and hyperthymic temperament. Finally, Azorin et al.,[26] in their study conducted among 278 patients with BPAD (79.8% depressive PP and 20.2% manic PP), were able to show that patients with manic PP had higher cyclothymic and hyperthymic temperament.
The relationship between substance use and predominant polarity
Substance use disorders and PP have been shown to bear a complicated relationship. A few studies have been able to show that if substance use precedes the first affective episode in BPAD, the possibility of manic PP is higher.[12,22] However, these studies failed to show any relationship between current substance use and PP. In a long-term follow-up study[13] of up to 10 years, the authors demonstrated no significant differences in alcohol and other substance use at baseline. But in patients with manic PP, the frequency of alcohol and other substance abuse decreased significantly when compared with depressive PP. This result was further supported by another study[27] which compared the PP among BPAD patients without substance use (n = 86), BPAD patients with alcohol use (n = 69), and BPAD patients with polysubstance use (n = 63). The authors found that patients with BPAD without substance use tended to have a manic PP, whereas those with alcohol use or polysubstance use tended to have a depressive PP.
The relationship between insight, cognitive functions and predominant polarity
In a study[28] involving 55 euthymic patients with BPAD distinguished in terms of their PP (manic PP 17, depressive PP 22, indeterminate PP 16) and 31 healthy controls, the authors used a neuropsychological battery testing for attention, verbal fluency, planning, and memory. The study showed that patients with manic PP were significantly poor performers in alternating attention, verbal fluency, and delayed memory when compared with all other groups. Patients with depressive PP showed no deficit in any of the tests when compared with manic PP or indeterminate PP. The authors even speculated that the cognitive deficits in BPAD might be related to the polarity of the episodes rather than the number of episodes. Another study,[29] involving 101 patients with BPAD [58 euthymic (28 MPP) and 43 in mania (17 MPP)] showed that PP does not have any bearing on the level of insight.
Polarity index
The concept of PP has led to the advent of the concept of polarity index (PI). PI as a construct is a number that denotes the ability of a drug used in the management of BPAD to prevent episodes of either polarity. It is defined as the ratio of the number needed to treat (NNT) for prevention of a depressive episode to the NNT for prevention of a manic episode. A PI of more than 1 denotes a superior antimanic property, whereas a PI of less than 1 denotes a superior antidepressive property. Popovic et al.,[22] in a sample of 604 patients with BPAD, showed that patients who had manic PP were cumulatively treated with drugs with a higher PI when compared with patients with depressive PP. A similar attempt[16] on a sample of German patients (n = 336) found that the concept fitted poorly to their sample as there was no significant difference in the PI of the regime used in the management of patients with manic PP or depressive PP. The authors speculated that one of the major reasons behind the negative result could have been the fact that many of the drugs which were a part of the study could not be analyzed as there was no PI assigned to them (e.g., antidepressants). In spite of such results, PI remains a useful construct and should be a focus of further research.
The implications of predominant polarity
The expression of PP in a patient with BPAD conveys a substantial amount of information about the patient. Table 2 has already stated the important sociodemographic and clinical parameters that can be associated with certain PP. Colom et al.[12] were able to demonstrate that different PPs are associated with very different management goals in BPAD-I and BPAD-II. In BPAD-II, the most common PP is the depressive PP, and the most important target should be to prevent a depressive episode, whereas in BPAD-I, prevention of both manic and depressive episodes is important.
The elaboration of PP in BPAD can also imply a lot of information regarding the treatment choices made for the patients. A naturalistic study[30] has been able to demonstrate that the treatment strategies predominantly used in a cohort of patients with BPAD are in line with their PP. The authors conducted a principal component analysis of a sample of 604 patients with BPAD. The three main prescription patterns that arose were “antimanic stabilization package” for “predominantly manic-psychotic BPAD-I patients,” “antidepressive stabilization package” for patients with depressive PP, and “antibipolar II package” including antidepressant monotherapy for patients with BPAD II with depressive PP. The antimanic stabilization package consisted of mood stabilizers (lithium, valproate, and carbamazepine), three atypical antipsychotics (clozapine, risperidone, and olanzapine), and electroconvulsive therapy. The antidepressive stabilization package consisted of lamotrigine and atypical antipsychotics such as quetiapine. The antibipolar II package, on the other hand, comprised the use of antidepressants such as tricyclic antidepressants, monoamine oxidase inhibitors, serotonin selective reuptake inhibitors, and serotonin/noradrenaline reuptake inhibitors. In another sample of 788 patients with bipolar depression,[23] it was found that PP could be established in 367 patients, the majority of whom had depressive PP. Males in this sample with predominant depressive polarity showed a worse outcome to treatment when compared with males with manic PP. This pattern could not, however, be seen among the females in the sample.
DISCUSSION
This review was able to find two sets of definitions for PP. Arguably, the Barcelona proposal has been the more widely used definition so far, but the relevance of the Harvard index remains when the research design does not endorse a diagnostic orphan or “indeterminate polarity.” However, the scope for further research to achieve a unifying definition remains. The diagnostic status of the mixed episodes also was a source of ambiguity, much of which has been made redundant following the publication of DSM 5[17] and the anticipated changes according to the beta version of International Classification of Disease 11th edition.[31]
No major trend arose from the epidemiological studies. But certain trends have been speculated in the literature, where authors have found a manic preponderance in tropical areas and a depressive preponderance from the temperate regions.[3] Studies that included patients with BPAD-I also showed a higher prevalence of manic PP.[15] However, that could not be replicated in patients with BPAD-II. Hence, we should potentially invest some efforts to find out any trends, if they exist, and the reason behind that.
The studies reviewed have been able to associate various clinical features with certain PPs. But many of the findings could not be replicated across research. One important reason could be that all the studies did not have the methodological rigor to negate the effect of confounding factors adequately. Another reason could be a recall bias against the non-PP of the clinical course. However, in spite of that, the associated parameters convey important information that could aid decision-making. It is important to recall at this stage that evidence suggests that there is a very close association of PP with the polarity of the first episode. Manic PP has been closely linked with substance use and male gender. Depressive PP is associated with female gender, suicidality, and higher diagnostic latency. Studies also demonstrated that patients with manic PP tended to have higher cognitive deficits when compared with those with a depressive PP. The existing literature also supports the fact that cognitive impairment in BPAD is not just state-dependent and that probably certain cognitive deficits also persist in remission.[32]
The concept of PP and PI also seems to complement each other. Patients with manic PP were usually treated with drugs with higher PI (denoting superior antimanic property) when compared with depressive PP and vice versa. This review points out that we should be guided by the PI of the drugs while choosing appropriate stabilizing medication. However, certain deficiencies need to be corrected. For example, the PI of certain drugs cannot be calculated. The PI of paliperidone cannot be calculated because the NNT for depressive episodes is negative. Again, due to the definition of PI, an agent which is very good in both antimanic and anti-depressive properties cannot be differentiated from an agent which is weak in both antimanic and antidepressive properties. More research is also required to further substantiate the evidence that the prophylactic serum levels of lithium may vary according to the PP of the patients.[33,34] The prophylactic serum level is less for prevention of a depressive episode when compared for a manic episode.
A lot of enthusiasm was there regarding the possibility of PP to be a specifier in the DSM 5 criteria,[35] which has subsided after its publication. Although it has not been accepted as a specifier, the facts that mixed episode has ceased to be an independent polarity and that there has to be a polarity attributed to any episode even with mixed features reiterate the importance of PP. The current belief is indeed that PP remains an important clinical variable in the management of BPAD.[36]
LIMITATIONS
The available literature has not been able to reach a single definition of consensus. As a result, it has been difficult to compare the results of the studies. Although some efforts have been made to find out the differential effects of this variety, further research is required to arrive at a consensus. In the same vein, we need to think about how we should interpret the substantial information that we have been able to accumulate about the so-called “indeterminate polarity.” Does it actually represent a distinct group of patients with BPAD? Or is it just a victim of a categorical conceptualization of a construct?
In spite of the concept not being very new, there has been a dearth of large-scale prospective data. It should also be noted that the studies that were conducted are from a few centers. As a result, there is ample scope and requirement of replicating the findings across other centers.
CONCLUSION
In the aftermath of the release of DSM 5, where the concept of PP was disregarded and not accepted as a course specifier, the enthusiasm seems to have died down. This is reflected by the fact that the number of studies subsequent to its release has been sparse. But there is no denying the fact that PP remains a useful construct in our clinical practice. One of the putative reasons behind this apparent disregard may be the fact that we are trying to move toward a psychiatric classification that is less dependent on phenomenology and more on neurobiology. Hence, our further efforts should be focused on developing neurobiological correlates of PP. Further studies should be conducted on genetics, neurobiology, and neuropsychology and to find biomarkers of PP in BPAD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Merikangas KR, Jin R, He J-P, Kessler RC, Lee S, Sampson NA, et al. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. [Last cited on 2018 Jun 09];Arch Gen Psychiatry [Internet] 2011 68:241–51. doi: 10.1001/archgenpsychiatry.2011.12. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21383262 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Judd LL, Schettler PJ, Akiskal HS, Maser J, Coryell W, Solomon D, et al. Long-term symptomatic status of bipolar I vs. bipolar II disorders. [Last cited on 2018 Apr 20];Int J Neuropsychopharmacol [Internet] 2003 6:S1461145703003341. doi: 10.1017/S1461145703003341. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12890306 . [DOI] [PubMed] [Google Scholar]
- 3.Subramanian K, Kattimani S. Geographical predisposition to a mania-predominant course of bipolar disorder in Asia. [Last cited on 2018 Jun 09];Asian J Psychiatr [Internet] 2017 30:73–4. doi: 10.1016/j.ajp.2017.08.005. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28837940 . [DOI] [PubMed] [Google Scholar]
- 4.Karthick S, Kattimani S, Rajkumar RP, Bharadwaj B, Sarkar S. Long term course of bipolar I disorder in India: Using retrospective life chart method. [Last cited on 2018 Jun 09];J Affect Disord [Internet] 2015 173:255–60. doi: 10.1016/j.jad.2014.10.056. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25462425 . [DOI] [PubMed] [Google Scholar]
- 5.Gignac A, McGirr A, Lam RW, Yatham LN. Recovery and recurrence following a first episode of mania. [Last cited on 2018 Jun 09];J Clin Psychiatry [Internet] 2015 76:1241–8. doi: 10.4088/JCP.14r09245. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25845021 . [DOI] [PubMed] [Google Scholar]
- 6.Gignac A, McGirr A, Lam RW, Yatham LN. Course and outcome following a first episode of mania: Four-year prospective data from the Systematic Treatment Optimization Program (STOP-EM) [Last cited on 2018 Jun 09];J Affect Disord [Internet] 2015 175:411–7. doi: 10.1016/j.jad.2015.01.032. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25678174 . [DOI] [PubMed] [Google Scholar]
- 7.Judd LL, Akiskal HS, Schettler PJ, Coryell W, Endicott J, Maser JD, et al. A prospective investigation of the natural history of the long-term weekly symptomatic status of bipolar II disorder. [Last cited on 2018 Jun 20];Arch Gen Psychiatry [Internet] 2003 60:261–9. doi: 10.1001/archpsyc.60.3.261. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12622659 . [DOI] [PubMed] [Google Scholar]
- 8.Judd LL, Akiskal HS, Schettler PJ, Endicott J, Maser J, Solomon DA, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. [Last cited on 2018 Jun 20];Arch Gen Psychiatry [Internet] 2002 59:530–7. doi: 10.1001/archpsyc.59.6.530. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12044195 . [DOI] [PubMed] [Google Scholar]
- 9.Ketter TA, Calabrese JR. Stabilization of mood from below versus above baseline in bipolar disorder: A new nomenclature. [Last cited on 2018 Jun 20];J Clin Psychiatry [Internet] 2002 63:146–51. doi: 10.4088/jcp.v63n0210. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11874216 . [DOI] [PubMed] [Google Scholar]
- 10.Carvalho AF, Quevedo J, McIntyre RS, Soeiro-de-Souza MG, Fountoulakis KN, Berk M, et al. Treatment implications of predominant polarity and the polarity index: A comprehensive review. [Last cited on 2018 Apr 19];Int J Neuropsychopharmacol [Internet] 2014 18 doi: 10.1093/ijnp/pyu079. Available from: https://academic.oup.com/ijnp/article-lookup/doi/10.1093/ijnp/pyu079 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Angst J. The course of affective disorders. II. Typology of bipolar manic-depressive illness. [Last cited on 2018 Apr 20];Arch Psychiatr Nervenkr [Internet] 1978 226:65–73. doi: 10.1007/BF00344125. Available from: http://www.ncbi.nlm.nih.gov/pubmed/708228 . [DOI] [PubMed] [Google Scholar]
- 12.Colom F, Vieta E, Daban C, Pacchiarotti I, Sánchez-Moreno J. Clinical and therapeutic implications of predominant polarity in bipolar disorder. [Last cited on 2018 Feb 10];J Affect Disord [Internet] 2006 93:13–7. doi: 10.1016/j.jad.2006.01.032. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16650901 . [DOI] [PubMed] [Google Scholar]
- 13.González-Pinto A, Alberich S, Barbeito S, Alonso M, Vieta E, Martínez-Arán A, et al. Different profile of substance abuse in relation to predominant polarity in bipolar disorder: The Vitoria long-term follow-up study. [Last cited on 2018 Apr 19];J Affect Disord [Internet] 2010 124:250–5. doi: 10.1016/j.jad.2009.11.005. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0165032709004984 . [DOI] [PubMed] [Google Scholar]
- 14.Colom F, Vieta E, Suppes T. Predominant polarity in bipolar disorders: Refining or redefining diagnosis? [Last cited on 2018 Apr 19];Acta Psychiatr Scand [Internet] 2015 132:324–6. doi: 10.1111/acps.12503. Available from: http://doi.wiley.com/10.1111/acps.12503 . [DOI] [PubMed] [Google Scholar]
- 15.Baldessarini RJ, Undurraga J, Vázquez GH, Tondo L, Salvatore P, Ha K, et al. Predominant recurrence polarity among 928 adult international bipolar I disorder patients. [Last cited on 2018 Apr 19];Acta Psychiatr Scand [Internet] 2012 125:293–302. doi: 10.1111/j.1600-0447.2011.01818.x. Available from: http://doi.wiley.com/10.1111/j.1600-0447.2011.01818.x . [DOI] [PubMed] [Google Scholar]
- 16.Volkert J, Zierhut KC, Schiele MA, Wenzel M, Kopf J, Kittel-Schneider S, et al. Predominant polarity in bipolar disorder and validation of the polarity index in a German sample. [Last cited on 2018 Apr 19];BMC Psychiatry [Internet] 2014 14:322. doi: 10.1186/s12888-014-0322-8. Available from: http://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-014-0322-8 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Home | APA DSM-5 [Internet] [Last cited on 2016 Jan 31]. Available from: http://www.dsm5.org/Pages/Default.aspx .
- 18.Rangappa SB, Munivenkatappa S, Narayanaswamy JC, Jain S, Reddy YCJ. Predominant mania course in Indian patients with bipolar I disorder. [Last cited on 2018 Apr 19];Asian J Psychiatr [Internet] 2016 22:22–7. doi: 10.1016/j.ajp.2016.04.006. Available from: http://linkinghub.elsevier.com/retrieve/pii/S1876201816301757 . [DOI] [PubMed] [Google Scholar]
- 19.Nivoli AMA, Pacchiarotti I, Rosa AR, Popovic D, Murru A, Valenti M, et al. Gender differences in a cohort study of 604 bipolar patients: The role of predominant polarity. [Last cited on 2018 Apr 23];J Affect Disord [Internet] 2011 133:443–9. doi: 10.1016/j.jad.2011.04.055. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21620480 . [DOI] [PubMed] [Google Scholar]
- 20.Mazzarini L, Pacchiarotti I, Colom F, Sani G, Kotzalidis GD, Rosa AR, et al. Predominant polarity and temperament in bipolar and unipolar affective disorders. [Last cited on 2018 Apr 19];J Affect Disord [Internet] 2009 119:28–33. doi: 10.1016/j.jad.2009.03.016. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0165032709001293 . [DOI] [PubMed] [Google Scholar]
- 21.Rosa AR, Andreazza AC, Kunz M, Gomes F, Santin A, Sanchez-Moreno J, et al. Predominant polarity in bipolar disorder: Diagnostic implications. [Last cited on 2018 Mar 09];J Affect Disord [Internet] 2008 107:45–51. doi: 10.1016/j.jad.2007.07.021. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17804081 . [DOI] [PubMed] [Google Scholar]
- 22.Popovic D, Torrent C, Goikolea JM, Cruz N, Sánchez-Moreno J, González-Pinto A, et al. Clinical implications of predominant polarity and the polarity index in bipolar disorder: A naturalistic study. [Last cited on 2018 Apr 19];Acta Psychiatr Scand [Internet] 2014 129:366–74. doi: 10.1111/acps.12179. Available from: http://doi.wiley.com/10.1111/acps.12179 . [DOI] [PubMed] [Google Scholar]
- 23.Vieta E, Berk M, Wang W, Colom F, Tohen M, Baldessarini RJ. Predominant previous polarity as an outcome predictor in a controlled treatment trial for depression in bipolar I disorder patients. [Last cited on 2018 Apr 23];J Affect Disord [Internet] Elsevier. 2009 119:22–7. doi: 10.1016/j.jad.2009.02.028. Available from: https://www.sciencedirect.com/science/article/pii/S0165032709000974 . [DOI] [PubMed] [Google Scholar]
- 24.Yang AC, Yang C-H, Hong C-J, Liou Y-J, Shia B-C, Peng C-K, et al. Effects of age, sex, index admission, and predominant polarity on the seasonality of acute admissions for bipolar disorder: A population-based study. [Last cited on 2018 Apr 19];Chronobiol Int [Internet] 2013 30:478–85. doi: 10.3109/07420528.2012.741172. Available from: http://www.tandfonline.com/doi/full/10.3109/07420528.2012.741172 . [DOI] [PubMed] [Google Scholar]
- 25.Henry C, Lacoste J, Bellivier F, Verdoux H, Bourgeois ML, Leboyer M. Temperament in bipolar illness: Impact on prognosis. [Last cited on 2018 Apr 24];J Affect Disord [Internet] Elsevier. 1999 56:103–8. doi: 10.1016/s0165-0327(98)00219-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10701467 . [DOI] [PubMed] [Google Scholar]
- 26.Azorin JM, Adida M, Belzeaux R. Predominant polarity in bipolar disorders: Further evidence for the role of affective temperaments. [Last cited on 2018 Apr 19];J Affect Disord [Internet] 2015 182:57–63. doi: 10.1016/j.jad.2015.04.037. Available from: http://linkinghub.elsevier.com/retrieve/pii/S016503271500261X . [DOI] [PubMed] [Google Scholar]
- 27.Janiri D, Di Nicola M, Martinotti G, Janiri L. Who's the leader, mania or depression? predominant polarity and alcohol/polysubstance use in bipolar disorders. [Last cited on 2018 Apr 19];Curr Neuropharmacol [Internet] 2017 15:409–16. doi: 10.2174/1570159X14666160607101400. Available from: http://www.eurekaselect.com/openurl/content.php?genre=article&issn=1570-159X&volume=15&issue=3&spage=409 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Belizario GO, Gigante AD, de Almeida Rocca CC, Lafer B. Cognitive impairments and predominant polarity in bipolar disorder: A cross-sectional study. [Last cited on 2018 Mar 09];Int J bipolar Disord [Internet] Springer. 2017 5:15. doi: 10.1186/s40345-017-0085-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28332122 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Assis da Silva R, Mograbi DC, Camelo EVM, Peixoto U, Santana CMT, Landeira-Fernandez J, et al. The influence of current mood state, number of previous affective episodes and predominant polarity on insight in bipolar disorder. [Last cited 2018 Jun 09];Int J Psychiatry Clin Pract [Internet] 2017 21:266–70. doi: 10.1080/13651501.2017.1324991. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28554235 . [DOI] [PubMed] [Google Scholar]
- 30.Nivoli AMA, Colom F, Pacchiarotti I, Murru A, Scott J, Valentí M, et al. Treatment strategies according to clinical features in a naturalistic cohort study of bipolar patients: A principal component analysis of lifetime pharmacological and biophysic treatment options. [Last cited on 2018 Apr 23];Eur Neuropsychopharmacol [Internet] 2013 23:263–75. doi: 10.1016/j.euroneuro.2012.07.015. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22939529 . [DOI] [PubMed] [Google Scholar]
- 31.Kurumaji A. [The trends of mood disorders in ICD-11: bipolar and depressive disorders] [Last cited on 2018 Jun 10];Seishin Shinkeigaku Zasshi [Internet] 2013 115:60–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23691796 . [PubMed] [Google Scholar]
- 32.Sagar R, Sahu A, Pattanayak RD, Chatterjee B. Assessment of cognitive functions in bipolar I disorder: A 1-year naturalistic follow-up study. [Last cited on 2018 Jun 10];Bipolar Disord [Internet] Wiley/Blackwell (10.1111) 2018 20:248–59. doi: 10.1111/bdi.12584. Available from: http://doi.wiley.com/10.1111/bdi.12584 . [DOI] [PubMed] [Google Scholar]
- 33.Severus WE, Kleindienst N, Evoniuk G, Bowden C, Möller HJ, Bohus M, et al. Is the polarity of relapse/recurrence in bipolar-I disorder patients related to serum lithium levels? Results from an empirical study. [Last cited on 2018 May 01];J Affect Disord [Internet] 2009 115:466–70. doi: 10.1016/j.jad.2008.10.009. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19019453 . [DOI] [PubMed] [Google Scholar]
- 34.Kleindienst N, Severus WE, Greil W. Are serum lithium levels related to the polarity of recurrence in bipolar disorders? Evidence from a multicenter trial. [Last cited on 2018 May 01];Int Clin Psychopharmacol [Internet] 2007 22:125–31. doi: 10.1097/01.yic.0000224788.21406.c8. Available from: https://insights.ovid.com/crossref?an=00004850-200705000-00001 . [DOI] [PubMed] [Google Scholar]
- 35.Henry C, Etain B. New ways to classify bipolar disorders: Going from categorical groups to symptom clusters or dimensions. [Last cited on 2018 Apr 19];Curr Psychiatry Rep [Internet] 2010 12:505–11. doi: 10.1007/s11920-010-0156-0. Available from: http://link.springer.com/10.1007/s11920-010-0156-0 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Colom F, Vieta E. The road to DSM-V. Bipolar disorder episode and course specifiers. [Last cited on 2018 Apr 19];Psychopathology [Internet] 2009 42:209–18. doi: 10.1159/000218518. Available from: https://www.karger.com/Article/FullText/218518 . [DOI] [PubMed] [Google Scholar]


