Abstract
Background:
Mental disorders cause considerable morbidity and disability, and there is ample evidence that mental disorders are positively associated with household food insecurity.
Methods:
A cross-sectional survey was conducted for a period of 2 months at Bakultala slum of Bankura town involving 152 people of ≥18 and ≤60 years of age selected using simple random sampling technique to estimate the prevalence of mental disorders and to find out its correlates. Information pertaining to socio-demographics and household food security (HHFS) and “ potential psychiatric case” were collected through a house to house interview of the head of the household, using predesigned questionnaire, Bengali version of self-reporting questionnaire, and 6-item household food security scale (HFSS).
Results:
In total, 45% of the study participants belonged to food unsecured households. Overall, 21% of the respondents were identified as “potential psychiatric case,” which was found to be associated with higher age, illiteracy, divorcee female, and people living in households without food security.
Conclusion:
Study results reflecting high prevalence (21%) of “potential psychiatric case” with various correlates such as age, sex, education, marital status, and HHFS among the slum dweller of Bankura town may be helpful in formulating policies for combating mental health morbidities.
Key words: Adult slum population, female, food insecurity, illiteracy, mental disorder
INTRODUCTION
Mental and behavioral disorders are important causes of morbidity in primary care settings and produce considerable disability.[1,2] The overall Disability Adjusted Life Years (DALYs) burden for neuropsychiatric disorders is projected to increase to 15% by the year 2020.[3] As per the report of the National mental health survey of India 2015–16, the overall current mental morbidity was found to be 10.6%.[4] India is implementing a national level program of integrating mental health with primary health care. However, psychiatric epidemiology lags behind other branches of epidemiology because of difficulties encountered in conceptualizing, diagnosing, defining a case, sampling, selecting an instrument, and lack of resources and stigma, especially in developing countries. Although mental health problems in developing countries are highly prevalent, such issues are not yet adequately addressed in these countries, where a growing number of residents live in slums. Little is known about the spectrum of mental illnesses in urban slums, and adequate research on the mental illnesses of the slum dwellers is lacking.[5]
Food insecurity is a major health problem that has devastating effects on various aspects of human life. In particular, there are compelling theoretical and empirical reasons to expect that food insecurity may be directly related to mental health morbidities and may be quantifiable in developing country settings.[6] There is evidence of an association between insecurity of income flow and common mental disorders (CMD).[7] The knowledge of the relationship that food insufficiency and mental health have, may help reduce the burden of common mental disorders, as this may be relatively amenable to intervention unlike a number of other major risk factors for mental illness. There have been studies on the association between household food security (HHFS) and various factors such as underweight children, growth faltering in children, maternal anxiety, etc.[8] However, the association between HHFS and mental morbidity of the household has not been adequately studied in our country. With this backdrop, this study was conducted to estimate the prevalence of mental morbidities among the adult population in the study area and to find out the factors associated with mental morbidity, including HHFS.
MATERIALS AND METHODS
A community-based cross-sectional survey was carried out, for a period of 2 months (from 7th August 2012 to 6th October 2012), involving permanent inhabitants of Bokultala slum of Bankura Municipality of Bankura district, West Bengal under the field practice area of Bankura Sammilani Medical College (BSMC). People aged ≥18 years and ≤60 years, without any serious illness and willing to participate in the study, were included in the study after being selected using two-stage simple random sampling technique with a sample size of 152 calculated according to a formula n = (Zα2*p*q)/d2; where, Zα=1.96 (two-tailed) at 95% confidence level, p (prevalence) = 0.4, q=(1 − p) = 0.6, d = allowable error = 20% of “p” assuming, and possible non-response rate of 5%.[9]
Baseline information as well as data pertaining to the mental morbidity and HHFS were collected through house-house interview using a predesigned, pretested, and semi-structured questionnaire, self-reporting questionnaire (SRQ) in Bengali version,[10] and 6-item household food security scale (HFSS) in Bengali version.[8]
The SRQ (Harding et al. 1980) is a standardized self-reporting questionnaire used to screen for common mental disorders and has been widely used in primary care. It indicates if the responder is a “potential psychiatric case.” The SRQ was originally developed by the WHO as a screening research instrument for the detection of psychiatric morbidity across different cultures by validating, including Bengali version.[7]
To measure HHFS, 6-item HFSS was used. It was developed by the United States Department of Agriculture and has been extensively studied in the United States[11,12] as well as a few other countries[13] and found very effective in measuring food insecurity. Its validated Bengali version was used successfully in a study in Bankura.[8]
Out of the 73 slums in Bankura municipality, One slum was first selected using simple random sampling technique.[14] There were 195 households in the chosen “Bokultala slum.” The list of the households, along with names of their members, was collected from family folders, and a sampling frame was made by serially arranging the population of ≥18 years and ≤60 year age group. Further, the study subjects were selected by using a computer-generated random number table till a sample size of 152 was reached. It came to a total of 58 families.
Verbal informed consent was obtained from each participant before collecting information. SRQ consisted of 24 short questions that required a “yes” or “no” response, depending on the presence or absence of symptoms. The respondent was considered to be a potential psychiatric case if the total number of “yes” answers to the first 20 questions (non-psychotic items) reached a value ≥7 (cut-off point), or if there was at least one “yes” answer to any of the four remaining “psychotic” items, or if both criteria were met.[15]
Six-item HFSS was used to assess the HHFS. Responses of “often” or “sometimes” on questions HH3 and HH4 and “yes” on AD1, AD2, and AD3 were coded as affirmative (yes). Responses of “almost every month” and “some months but not every month” on AD1a were coded as affirmative (yes). The sum of affirmative responses to the six questions in the module was taken as the household's raw score on the scale.
Food security status was assigned as follows:
Raw score 0–1: High or marginal food security
Raw score 2–4: Low food security
Raw score 5–6: Very low food security.
Further, the food security of households with raw score 0–1 was described as “food secured,” and the two categories “low food security” and “very low food security” in combination was referred to as “food unsecured.”
The study was initiated after obtaining clearance from the Institutional ethics committee of BSMC, Bankura on 6th August 2012. A pilot study was conducted in a similar community setting to assess the feasibility, acceptability, and reliability of the tool.
Data were described by mean, standard deviation (SD), and percentage and was displayed by tables and charts. Inferential statistical tests such as Omnibus Chi-square (χ2) were followed by Chi-square of independence/Fisher exact test using partitioning approach to investigate further statistically significant Omnibus Chi-square test result.[16] Odds ratio (OR) with 95% confidence interval were used to analyze the different factors associated with “potential psychiatric case” along with the bearing of HHFS on it as well. A P value of <0.05 was taken as the criteria for significance.
RESULTS
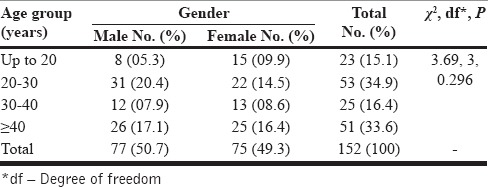
Approximately, 34.9% of the study population belonged to age group 20–30 years, closely followed by 40–60 years. There was no significant difference in the male-female ratio across the age groups (P = 0.296) [Table 1]. The mean age of the participants was estimated to be 29 ± 4.7 years.
Table 1.
Distribution of study population according to age and gender (n=152)
However, 46.1% of the study participants were daily wage earners, followed by homemakers who constituted 26.3%; 15.1% and 12.5% of the respondents were students and unemployed, respectively.
Moreover, 39.5% were literate, with low level (1–4 years of schooling) of formal education, and 36.8% were illiterate. Formal education for 5–0 years and >10 years was received by 19.1% and 4.6%, respectively. Overall, 63.9% were married, and 6.6% were widow/divorcee, and 45.4% belonged to food unsecured households. In total, 21.1% were “potential psychiatric cases.”
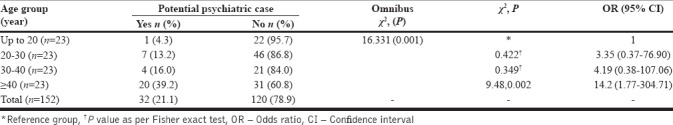
Statistically significant association was found between the age of the individual and possibility of being a “potential psychiatric case” (P = 0.001). Those aged 40–60 years were four times more likely to develop psychiatric illness (χ2 for linear trend 14.722, P = 0.0001, OR = 4.0). The Chi-square test revealed that people of 40–60 years age group are nine times more likely to psychiatric illness compared to the youngest age group, i.e., 18–20 years age group [Table 2].
Table 2.
Distribution of study population according to potential psychiatric case and age of the individual (n=152)
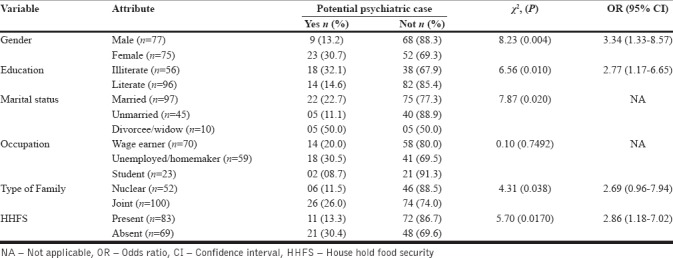
Females were three times more likely to be “potential psychiatric cases.” Similarly, illiterate divorcee females having lack of food security were more likely to be “potential psychiatric case” [Table 3].
Table 3.
Distribution of respondents according to potential psychiatric case and socio-demographics (n=152)
Although a higher proportion of tobacco consumers were “potential psychiatric case” compared to tobacco non-users (23.9% vs. 18.5%), this difference was not statistically significant (P = 0.413). Similarly, alcohol consumption was found to be unrelated to the potentiality to be affected by psychiatric illness (22.2% vs. 20.8% with P = 0.869).
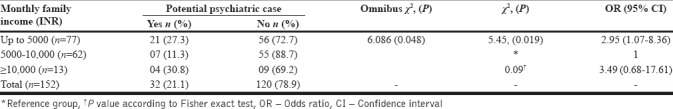
The proportion of “potential psychiatric case” was significantly higher among those with monthly family income up to INR 5,000 than those with monthly family income INR 5,001–10,000/(27.3% vs. 11.3%). The difference was statistically significant (P = 0.019) [Table 4].
Table 4.
Distribution of participants according to their potentiality to develop into a psychiatric case and monthly family income (n=152)
DISCUSSION
The socio-physical environment of slums is diverse and can compromise health in a variety of ways. This study determined the prevalence of mental morbidity and analyzed the determinants of being a “potential psychiatric case” among the slum dwellers in the town of Bankura in the South-Western zone of West Bengal. It was found that mental morbidity was unequally distributed among the population. The prevalence of household food insecurity was also determined as it is of dynamic concern in urban India and was found to be one of the prime reasons for mental distress.
Maximum participants were aged 20–30 years, followed by 40–60 years. Majority of males were aged 20–30 years, whereas maximum females belonged to the 40–60 years group. The male-female ratio was found to be almost one, which is one of the positive aspects of this study. This might be because of the increasing consciousness regarding the saving of girl child and higher life expectancy of the females. Approximately, 46.1% of the participants were wage earners, and 26.3% were homemakers. It was because a good proportion of women were cook s and maids, engaged in wage-based work for patients admitted to the nearby BSMC and Hospital. However, 39.5% of participants reportedly had 1–4 years of schooling, and 36.8% were illiterate. Only one graduate was found in the study subjects, reflecting the typical educational status of a slum in a district town.
On assessment by the SRQ, it was found that 21.1% of the participants were “potential psychiatric cases”. As per the report of the National Mental Health Survey of India 2015–16, the overall current mental morbidity was found to be 10.6%.[4] In a study conducted in Brazil on a population of 1,277 using SRQ, Lima et al. showed that 22.7% of people were suffering from mental morbidity, which is quite close to the value obtained here.[17] However, not many studies using the SRQ have been conducted in this part of the world. Hence, still, it might be concluded that the prevalence of “potential psychiatric case” was significantly high, and various factors might be associated with this high prevalence. Lund et al. observed that variables such as education, food insecurity, housing, social class, socio-economic status, and financial stress exhibit a relatively consistent and strong association with CMD.[18]
The prevalence of “potential psychiatric case” was 39.2% in 40–60 years age group and 16.0% in 30–40 years age group. This was followed by 13.2% for people aged 20–30 years. It was the least in 18–20 years age group. Statistically significant association was found between the age of the individual and likelihood of being a “potential psychiatric case.”
The chance of being “potential psychiatry case” was found to be higher in females, in concurrence to the somewhat similar result found in a study on gender and mental health in Kerala.[19]
However, psychiatric disorders were more common in women aged 25–34 years than those aged 35–44 years. The increase in mental distress in the age of 40–60 years might be attributed to the fact that people of higher age group are more prone to psychological problems, especially depression; the most common geriatric psychiatric disorder might have started in the late fifties. The well-being of the elderly woman is also affected by widowhood in old age. The fact that age was related to mental well-being was also depicted in a study on mental health done in the slums of Dhaka.[20] In a study on “Stress and psychiatric disorder in urban Rawalpindi,” the mean Bradford somatic inventory (BSI) scores were revealed to increase with age in both men and women.[21] This was also comparable to the observations made in a study on the prevalence of depression among pre-university college students in an urban area of South India.[22]
The prevalence of “potential psychiatric case” among illiterate was 32.1%, whereas for literate it was about 14.6% which was less than half the prevalence in illiterate. Statistically significant association was found between the educational status of the individual and likelihood of being a “potential psychiatric case” (P = 0.010). Thus, as one would expect, education was revealed to have a positive influence on the well-being of subjects. This fact was also supported by the study on “Gender and mental health in Kerala,” which showed that the higher the level of educational attainment, the higher is the sense of well-being.[19] The fact that a sense of well-being comes with literacy was also shown in a study of depression among elderly persons in Surat.[23] Lower levels of education were associated with higher BSI in a study on stress and psychiatric disorder in urban Rawalpindi.[19] Patel et al. in their review, also showed an association between indicators of poverty and the risk of mental disorders, the most consistent association being with low levels of education.[24]
Unlike what was shown in the study on “Gender and mental health” in Kerala,[19] here it was the broken marriage or widowhood, instead of married or unmarried status, which seemed to have a negative impact on the sense of well-being. The prevalence of “potential psychiatric case” was 22.7% and 11.1% for married and unmarried participants, respectively, whereas in divorcee/widow it was 50.0%. There was a significant difference in prevalence between unmarried and divorcees (Fisher exact; P = 0.011 at df 1) and between married plus unmarried and divorcee plus widow (Fisher exact; P = 0.035 at df 1). This might partly be because of the stress that arises as a result of responsibilities as well as the stress of separate life. However, the higher the prevalence of “potential psychiatric case” seen in divorcee/widow group might also be linked to the increase in “potential psychiatric case” with age and small sample size in this group.
Statistically significant association was not found between the occupation of the individual and likelihood of being a “potential psychiatric case.” As one would expect in connection to the occupation, unemployment among adult is associated with mental morbidity, whereas it was lower in wage earners and least in the young minds of students.
Similarly, although there was a higher proportion of “potential psychiatry cases” among those who reported tobacco-alcohol consumption, the difference was not statistically significant. It might be because of the fact that the grade of alcohol-tobacco consumption was not to the level that can induce psychiatric disorders could be considered an inducer or indicator of depression.
The prevalence of likelihood of being a “potential psychiatric case” in a joint family was greater than double the prevalence in a nuclear family (P = 0.038). This might be attributed to an increase in the number of family members and the presence of in-laws. There might also be the distribution of income in the joint family among a greater number of family members, leading to such results.
The likelihood of being a “potential psychiatric case” was significantly higher in individuals with monthly family income of <INR 5,000 and INR >10,000 than the group with monthly family income to the range of INR 5,000–10,000. This might be possible, as during the study it was seen that most families with family income >10,000 were joint families. An association between poverty and the risk of mental disorders was also reported by Patel et al. in a review.[7]
Approximately, 45.4% belonged to food secured household. According to a mid-term status report on progress of Millennium Development Goals of West Bengal, 6–11 household out of 1,000 did not have enough food everyday during the months of July 2004 and June 2005.[24] It was found that HHFS had a positive impact on the vulnerability to be a “potential psychiatric case” (P = 0.017). A study in four ethnic groups in two communities of rural Tanzania also examined the association of food insecurity with mental anxiety and depression, with similar results.[6]
The study had some limitations. As it had a cross-sectional design, the assessment of seasonal variations of the impact of food insecurity could not be done. A longitudinal study would help better in this regard. The sample was taken from a single slum that might not be representative of the whole population of slums of Bankura town. The prevalence of “potential psychiatric case” was estimated using only SRQ, and no further assessment after SRQ was done to confirm caseness.
CONCLUSION
The present study reported a high prevalence (21.1%) of “potential psychiatric case” with various correlates such as age, sex, education, marital status, and HHFS among the slum dwellers of Bankura town. These results may be utilized in formulating policies for combating the forward march of mental health morbidities that are of great concern in this 21st century. Strategies should be formulated to cope up with psychiatric disorders and induce a sense of well-being among the vulnerable individuals. Grass root level workers may be deployed to increase the awareness toward the necessity of addressing household food insecurity to alleviate not only its physical consequences but also mental morbidities. However, the results of a large-scale multi-centric study would have played a better role in framing future policy as well as implementing the existing ones.
Financial support and sponsorship
INR 10000/sponsorship from ICMR.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
It was an Indian Council of Medical Research (ICMR) sponsored “short-term studentship” (STS) project.
REFERENCES
- 1.The ICD-10 classification of mental and behavioural disorders. Geneva: World Health Organization; 1992. [Google Scholar]
- 2.Sartorious N. WHO's work on the epidemiology of mental disorders. Soc Psychiatry Psychiatr Epidemiol. 1993;28:147–55. doi: 10.1007/BF00797316. [DOI] [PubMed] [Google Scholar]
- 3.Murry C, Lopez A. A Comprehensive Assessment of Mortality and Disability from Diseases, Injuries and Risk Factors in 1990 and Projected to 2020. Cambridge, MA: Harvard University press, World Health Organization; 1996. The Global Burden of Disease. [Google Scholar]
- 4.Murthy RS. National mental health survey of India 2015–2016: Editorial commentary. Indian J Psychiatry. 2017;59:21–6. doi: 10.4103/psychiatry.IndianJPsychiatry_102_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Izutsu T, Tsutsumi A, Islam AM, Kato S, Wakai S, Kurita H. Mental health, quality of life, and nutritional status of adolescents in Dhaka, Bangladesh: Comparison between an urban slum and a non-slum area. Soc Sci Med. 2006;63:1477–88. doi: 10.1016/j.socscimed.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Hadley C, Patil CL. Food insecurity in rural tanzania is associated with maternal anxiety and depression. Am J Human Biol. 2006;18:359–68. doi: 10.1002/ajhb.20505. [DOI] [PubMed] [Google Scholar]
- 7.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81:609–15. [PMC free article] [PubMed] [Google Scholar]
- 8.Mukhopadhyay DK, Biswas AB. Food security and anthropometric failure among tribal children in Bankura, West Bengal. Indian J Pediatr. 2011;48:11–4. doi: 10.1007/s13312-011-0057-2. [DOI] [PubMed] [Google Scholar]
- 9.Kumar S, Jeyaseelan L, Suresh S, Ahuja RC. Domestic violence and its mental health correlates in Indian women. Br J Psychiatry. 2005;187:62–7. doi: 10.1192/bjp.187.1.62. [DOI] [PubMed] [Google Scholar]
- 10.Choudhury AN, Brahma A, Sanyal D. The validation of the Bengali version of the self reporting questionnaires (SRQ) Indian J Clin Psychiatry. 2003;30:56–61. [Google Scholar]
- 11.Bickel G, Nord M, Hamilton W, Cook J. Guide to Measuring Household Food Security: Revised 2000. U.S. Department of Agriculture, Food and Nutrition Service, Alexandria VA. 2000 [Google Scholar]
- 12.Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the household food security scale. Am J Public Health. 1999;89:1231–4. doi: 10.2105/ajph.89.8.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Webb P, Coates J, Frongillo EA, Rogers BL, Swindale A, Bilinsky P. Measuring household food security: Why it's so important and yet so difficult to do. J Nutr. 2006;136:1404S–8S. doi: 10.1093/jn/136.5.1404S. [DOI] [PubMed] [Google Scholar]
- 14.Integrated housing and slum developmental programme (IHSDP) Bankura municipality. [Last accessed on 2012 Nov 18]. Available from: www.bankuramunicipality.org .
- 15.Al-Subaie A, Mohammed K, Al-Malik T. The Arabic self-reporting questionnaire (SRQ) as a psychiatric screening instrument in medical patients. Ann Saudi Med. 1998;18:308–10. doi: 10.5144/0256-4947.1998.308. [DOI] [PubMed] [Google Scholar]
- 16.Sharpe D. Your Chi-Square Test is Statistically Significant: Now What? [Last accessed on 2018 Oct 14];Practical Assessment, Research & Evaluation. 2015 20:1–9. Available from: http://pareonline.net/getvn.asp?v=20&n=8 . [Google Scholar]
- 17.Lima MS, Beria JU, Tomasi E, Conceicao AT, Mari JJ. Stressful life events and minor psychiatric disorders: An estimate of the population attributable fraction in a Brazilian community-based study. Int J Psychiatry Med. 1996;26:213–24. doi: 10.2190/W4U4-TCTX-164J-KMAB. [DOI] [PubMed] [Google Scholar]
- 18.Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, et al. Poverty and common mental disorders in low and middle income countries: A systematic review. Soc Sci Med. 2010;71:517–28. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohamed E, Rajan SI, Kumar KA, Mohammed PMS. Gender and Mental health in Kerala. 2002 Dec [Google Scholar]
- 20.Gruebner O, Khan MM, Lautenbach S, Müller D, Krämer A, Lakes T, et al. Mental health in the slums of Dhaka-a geoepidemiological study. BMC Public Health. 2012;12:177. doi: 10.1186/1471-2458-12-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mumford DB, Minhas FA, Akhtar I, Akhter S, Mubbashar MH. Stress and psychiatric disorder in urban Rawalpindi. Community Survey. Br J Psychiatry. 2000;177:557–62. doi: 10.1192/bjp.177.6.557. [DOI] [PubMed] [Google Scholar]
- 22.Joseph N. Prevalence of depression among pre-university college students in an urban area of South India. Int JCurr Res. 2011;3:439–42. [Google Scholar]
- 23.Jariwala V, Bansal RK, Patel S, Tamakuwala B. A study of depression among aged in Surat city. [Last accessed on 2018 Jun 12];National Journal of Community Medicine. 2010 1:47–9. Available from: http://www.njcmindia.org/uploads/01-01_47-49.pdf . [Google Scholar]
- 24.A mid – Term status report on progress of Millennium Development Goals of West Bengal. WADA NA TODO, WEST BENGAL. C/O IMSE, 195 JODHPUR PARK KOLKATA. [Last access on 2018 Dec 13]. p. p.14. Available from: http://wadanatodo.net/wp-content/uploads/2014/11/MDG-Report-West-Bengal-2007.pdf .


