Abstract
Background:
The majority of people with anxiety tend to seek help in primary care. Patients' illness perception regarding their own anxiety can influence the assessment, treatment processes, and outcomes. This cross-sectional study explored possible relationships between patients' illness perception of their anxiety and the severity of their anxiety.
Materials and Methods:
Ninety-five patients with anxiety were recruited at two primary care clinics in Singapore. Their responses to the generalized anxiety disorder-7 (GAD-7) and illness perception questionnaire mental health (IPQ-MH) were examined with Spearman's rho correlation coefficients and multiple regression analyses.
Results:
Four illness perception subscales, i.e., consequences (rs = 0.23), personal control (rs = –0.27), coherence (rs = –0.22), and biological (rs = 0.34) significantly correlated to anxiety (P < 0.05). A multiple regression analysis identified that attribution to biological factors (β = 0.348, P =0.001) and attribution to personal control (β = -0.262, P =0.008) were significantly associated with anxiety.
Conclusions:
Interventions for anxiety reduction in primary care can be enhanced with methods that promote (1) patients' awareness of the reasons for their anxiety beyond mostly bodily ones to include psychosocial ones and (2) patients' confidence in their own capacity to influence their recovery.
Key words: Anxiety, biological attribution, cross-sectional study, illness perception, personal control, primary care, regression analysis, Singapore
INTRODUCTION
A significant population of people with anxiety seeks help in primary care.[1,2,3] They may present with medical issues associated with anxiety such as irritable bowel syndrome, asthma, cardiovascular disease, and chronic pain.[4,5] In Singapore, the lifetime prevalence of anxiety was estimated to be 0.9%.[6] Anxiety is likely to compromise the quality of life[7] and treatment adherence.[8] For instance, early treatment drop out was observed among patients with anxiety symptoms.[2,9] This highlights the importance of establishing and delivering brief and effective treatment for anxiety patients, especially in primary care.
Understanding patients' perception of their illness is essential to enhancing the assessment and treatment of patients with anxiety. Illness perception is a cognitive model of how patients process information about their own health threat. The self-regulation model (SRM)[10,11] has been one of the most empirically tested models in clinical health psychology, psychiatry, and medicine. There are five components in the model, including identity (i.e., the perceived nature of the symptoms of the illness), causes (i.e., attributions regarding the reasons of the presence of the illness), timeline (i.e., the expected duration of the illness), consequences (i.e., the perceived impact of the illness), and cure/control (i.e., the perceived efficacy of attempts at managing the illness).
Studies have shown that illness perception may influence patients' response to their illness and treatment outcomes. In particular, treatment adherence may be related to perceived negative consequences and sense of personal control.[12] Causal attributions could determine patients' motivation in acquiring coping skills. For example, most patients who ceased their smoking habit had also attributed chronic obstructive pulmonary disease to smoking.[13] Evidence has shown that negative illness perception is associated with complications in the recovery process,[14,15] low health status,[16] and poor quality of life.[17]
Studies on illness perception related to anxiety tend to be conducted for patients with a specific disease such as type-2 diabetes mellitus,[18,19] chronic obstructive pulmonary disease,[20,21] chronic pain,[22] and heart failure.[23] However, illness perception studies on anxiety as a primary presenting problem appear to be underrepresented. In Singapore, anxiety is a common presenting problem, for which illness perception may enhance clinicians' formulations of its underlying factors and development of targeted interventions for the local population.
The aims of the present study were to (1) explore the illness perception of patients with anxiety in primary care in Singapore and (2) investigate the relationships between illness perception and anxiety. Given that past studies reported a significant relationship between illness perceptions and various presentations of anxiety, significant relationships between illness perception and anxiety were hypothesized for the local primary care population.
MATERIALS AND METHODS
Study design
The present study was a cross-sectional study.
Setting
The study was conducted in two primary care clinics in Singapore. Participants of this study were referred by their general physicians to consult a colocated clinical psychologist for anxiety. The clinical psychologists identified patients who were eligible to participate in this study and invited them to participate. The recruitment and data collection were ongoing from December 1, 2015 till July 29, 2016. All data were collected on a single occasion, and no follow-up was required.
Participants
Inclusion criteria for this study were age 21 years and above, and the presence of anxiety symptoms with total score of 5 (i.e., mild anxiety) and above on the generalized anxiety disorder-7 (GAD-7).[24] Patients who exhibited suicide risk or psychotic symptoms were excluded. Participants were recruited by the end of their psychology consultation with a clinical psychologist. They were given adequate time to consider. They were told that their participation was completely voluntary, and they were assured that they would receive treatment as usual in their future consultations even if they did not participate. After written consent was obtained, they were sent to an independent coinvestigator who administered the questionnaires. The coinvestigator collected all data.
The ethical approval (2015/00658) was obtained from the National Healthcare Group Domain Specific Review Board (DSRB) in Singapore. Written consent to participate in this study was obtained from all participants.
Study size
According to the G*Power analysis (based on the effect size of 0.15 as reported by past studies), at least 74 participants were required for this study.
Measures of assessment
Generalized anxiety disorder-7 (GAD-7).[24] The GAD-7 was used to assess the severity of the participant's anxiety. It is a self-report questionnaire that comprises seven items. Respondents are asked if they are affected by seven anxiety symptoms over the past 2 weeks. The response to each item (e.g., “not being able to stop or control worrying”) is rated on a 4-point Likert scale. The reliability and validity of GAD-7 have been supported by research.[25,26]
Illness perception questionnaire mental health (IPQ-MH).[27] The IPQ-MH was used to assess patients' illness perception of anxiety. It consists of 12 subscales: identity, timeline chronic, timeline cyclical, consequences, personal control, treatment control, coherence, emotional representation, psychosocial causes, biological causes, structural causes, and stress causes. It reportedly has good internal reliability.[27] In the present study, all subscales of the IPQ-MH showed adequate internal reliability (Cronbach's alpha ≥0.70), except the stress causes subscale. Their Cronbach's alpha values ranged from 0.69 (stress causes subscale) to 0.98 (treatment control subscale).
The IPQ-MH has a total of 67 items that utilize a 5-point Likert scale. The identity subscale includes items that ask whether the participants' main complaints belong to “social and/or relational problems” or “a reaction to circumstances or events.” Under the structure subscales, the timeline chronic items include “These problems will pass quickly.” The timeline cyclical items include “My problems are very unpredictable.” The consequences items include “My action cause difficulties for those who are close to me.” The personal control items include “My actions will have effect on the course of my problems.” The treatment control items include “The negative effects of my problems can be prevented (avoided) by my treatment.” The coherence items include “My problems don't make any sense to me.” The emotional representation items include “When I think about my problems, I get upset.” The causes subscales include the psychological subscale (e.g., “unresolved feelings resulting from the past”), biological subscale (e.g., “a chemical imbalance inside my brain”), structural subscale (e.g., “the lack of supportive communities”), stress subscale (e.g., “experience of serious marital conflict”).
Analysis
Data were analyzed by SPSS Version 20.0 for Mac. Shapiro–Wilk tests showed that other than the identity and timeline chronic subscales in the IPQ-MH, the data were not normally distributed (P < 0.05). Therefore, nonparametric tests were used for the analysis. Spearman's rho correlation coefficients were applied to explore not only the relationships between the IPQ-MH subscales and the GAD-7 total scores but also, separately, within the IPQ-MH subscales themselves.
To further analyze the relationship between illness perception and anxiety, a multiple regression analysis was conducted with the IPQ-MH subscales (i.e., identity, timeline chronic, timeline cyclical, consequences, personal control, treatment control, coherence, emotional representation, psychosocial causes, biological causes, structural causes, and stress causes) as the potential independent variables and GAD-7 total scores as the dependent variable.
RESULTS
Participant characteristics
A total of 110 patients were screened, and 95 participants were recruited. The median age of the participants (64 females and 31 males) was 51 years (interquartile range was 28). A total of 70 participants reported mild anxiety, 22 reported moderate anxiety and three reported severe anxiety. The median score for anxiety was 8.00, and the interquartile range was 5.00. No significant relationships were found between anxiety and age (Rs = –0.045, P = 0.668) or gender (Rs = 0.010, P = 0.920).
Illness perception
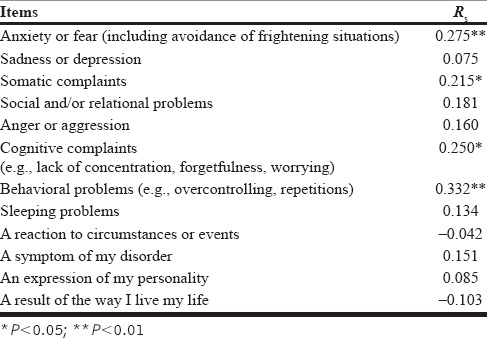
In the identity subscale, all symptoms were identified by at least one participant as important psychological symptoms. The mean score was 34.67 (SD = 7.44). Anxiety or fear (including avoidance of frightening situations), somatic complaints, cognitive complaints (e.g., lack of concentration, forgetfulness, worrying), and behavioral problems (e.g., overcontrolling, repetitions) were found to be significantly correlated to anxiety [Table 1].
Table 1.
Correlations between identity items and anxiety
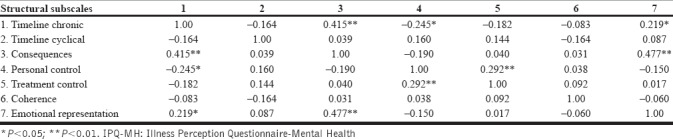
The median scores and interquartile ranges for other subscales are presented in Table 2. There were several significant correlations detected among the structuralsubscales themselves [Table 3]. Timeline chronic positively correlated with consequences and emotional representation but negatively correlated with personal control. Consequences positively correlated with emotional representation. Personal control positively correlated with treatment control.
Table 2.
Correlations between IPQ-MH subscales and anxiety
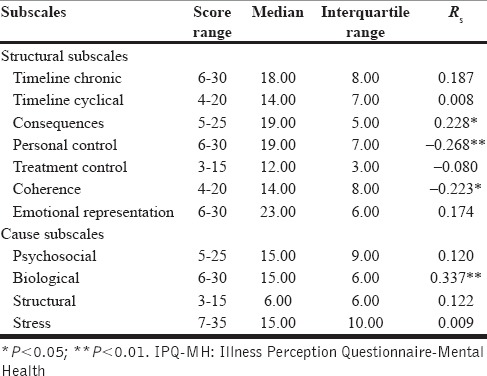
Table 3.
Correlations between structural subscales in IPQ-MH
Further, consequences positively correlated with anxiety, whereas personal control and coherence negatively correlated with anxiety [Table 2].
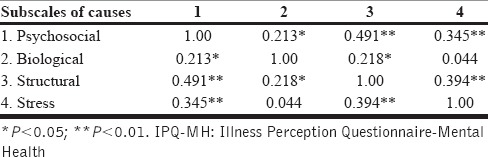
There were several significant correlations among the causes subscales themselves [Table 4]. The psychosocial subscale positively correlated with the biological, structural, and stress subscales. The biological subscale positively correlated with the structural subscale. The structural subscale positively correlated with the stress subscale. Among the causes subscales, only the biological subscale correlated with anxiety [Table 3].
Table 4.
Correlations between subscales of causes in IPQ-MH
Further, consequences, personal control, coherence, and biological subscales were included in a standard regression analysis to explore their association with anxiety. The model was statistically significant [F (4, 90) = 6.244, P < 0.0001] and accounted for approximately 18% of the variance of anxiety (R2 = 0.217, Adjusted R2 = 0.182). Anxiety was found to be significantly associated with personal control (β = -0.262, P = 0.008) and biological causes (β = 0.348, P = 0.001).
DISCUSSION
The present findings highlighted the illness perception of patients with anxiety in primary care. Majority of the participants were concerned about mental health symptoms including fear, somatic complaints, cognitive complaints (e.g., lack of concentration, forgetfulness, worrying), and behavioral problems (e.g., overcontrolling, repetitions). Overall, the participants perceived their conditions as moderately chronic with some fluctuations overtime. The participants' tendency to perceive their anxiety as chronic might suggest that they had experienced the anxiety symptoms for some time before seeking professional help. Any fluctuations of anxiety might have contributed to delay in seeking professional help, as they might not think they needed help while they felt better. Similarly, they generally reported a high degree of negative consequences, which could be a reflection of the duration of their condition and emotional distress. They also described themselves as having a meaningful understanding of their anxiety condition. In addition, they expressed a relatively greater sense of personal control and positive perception toward treatment, and both correlated with each other. The negative correlation between personal control and perceived chronicity was consistent with certain negative associations detected in cardiology between self-efficacy and the “stability” component of a pessimistic attributional style.[28]
The present findings highlighted that the four illness perception subscales (consequences, personal control, coherence, and biological) are significantly correlated to anxiety. The participants experienced higher anxiety when they perceived a greater negative impact of anxiety on their lives (i.e., consequences), lacked confidence in managing their own anxiety symptoms (i.e., personal control), held a deficient understanding about their anxiety condition (i.e., coherence), or believed that their anxiety resulted from physiological abnormality (i.e., biological attribution). Taken together, consequences, personal control, coherence, and biological attribution explained 18% of the variance in the anxiety severity. In particular, both personal control and biological attribution were significantly associated to anxiety, with the latter showing a stronger association.
In contrast to the findings from Costa et al.[22] that all structure subscales of illness perception were significantly and moderately associated with anxiety in patients with chronic pain, only three structure subscales (i.e., consequences, personal control, and coherence) significantly (albeit less than moderately) correlated to anxiety for the Singaporean participants in this study. Findings from this study were consistent with the results reported by Paschalides et al.[18] in diabetic patients, which showed marginal correlations between consequences and anxiety as well as personal control and anxiety, although the significant relationship between timeline and anxiety that was reported in their study did not emerge in our study. Further, the findings of Morgan et al.,[23] who reported a delicate but significant relationship between personal control and anxiety in patients with heart failure, was replicated in the present study. The present findings are also similar to those by Howard et al.[20] who reported a subtle but significant relationship between consequences and anxiety in patients with chronic obstructive pulmonary disease.
Limitations and recommendations
We did not rule out possible comorbidities with anxiety (i.e., anxiety potentially accompanied by other psychiatric conditions or physical diseases). To fine-tune the generalizability of the findings from this study to other primary care settings, it would be necessary to capture larger sample sizes from a more diverse range of primary care clinics with relevant comorbidity information.
Given this preliminary study's cross-sectional design, the test-retest reliability of IPQ-MH was not explored in this study, and the consistency of the patients' illness perception patterns over time could not be determined. Hence, conclusions should not be drawn about causal relationships between illness perception and anxiety severity. As illness perception might impact the severity of anxiety, the illness perception might as well have reciprocally resulted from the anxiety. This study can serve as a basis for longitudinal or even randomized controlled studies that attempt to examine patients' illness perception profiles overtime and the directionality between anxiety and illness perception. In addition, as anxiety was only partially explained by illness perception, qualitative studies would be a justifiable and promising approach to uncovering other important factors associated with primary care patients' anxiety.
Implications
This preliminary study demonstrated that meaningful patterns of patients' views and experiences of anxiety in primary care in Singapore could be detected and analyzed with IPQ-MH. Patients' perception toward consequences, personal control, understanding of the condition, and attribution to biological factors were shown to be associated with the severity of anxiety, with biological attribution, and personal control as significant contributing factors of anxiety severity.
These findings can enhance clinical formulation and interventions for patients with anxiety. Psychoeducation on their anxiety condition that equally emphasizes biological, psychological, and social factors would be helpful in making their largely physiologically inclined views less rigid and thus more balanced and resourceful in addressing other determinants of their anxiety as well. While interventions that target physiological reactions to anxiety (e.g., relaxation techniques and pharmacological prescriptions) may be routinely recommended for primary care patients, their personal control can be heightened with strategies that capitalize on the patients' sense of internal locus of control (i.e., confidence in their own capacity to influence outcomes of their anxiety condition). Accordingly, psychotherapeutic approaches such as strength-based cognitive-behavioral therapy[29] and solution-focused therapy[30] may foster patients' own confidence and problem-solving capabilities in attaining sustainable anxiety reduction.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States. Results from the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:629–40. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 2.Seekles W, Cuijpers P, Kok R, Beekman A, van Marwijk H, van Straten A. Psychological treatment of anxiety in primary care: A meta-analysis. Psychol Med. 2013;43:351–61. doi: 10.1017/S0033291712000670. [DOI] [PubMed] [Google Scholar]
- 3.Combs H, Markman J. Anxiety disorders in primary care. Med Clin N Am. 2014;98:1007–23. doi: 10.1016/j.mcna.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Roy-Byrne PP, Davidson KW, Kessler RC, Asmundson GJ, Goodwin RD, Kubzansky L, et al. Anxiety disorders and comorbid medical illness. Gen Hosp Psychiatry. 2008;30:208–25. doi: 10.1016/j.genhosppsych.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Gates K, Petterson S, Wingrove P, Miller B, Klink K. You can't treat what you don't diagnose: An analysis of the recognition of somatic presentations of depression and anxiety in primary care. Fam Syst Health. 2016;34:317–29. doi: 10.1037/fsh0000229. [DOI] [PubMed] [Google Scholar]
- 6.Chong SA, Abdin E, Vaingankar JA, Heng D, Sherbourne C, Yap M, et al. A population-based survey of mental disorders in Singapore. Ann Acad Med Singapore. 2012;41:49–66. [PubMed] [Google Scholar]
- 7.Bautista LE, Vera-Cala LM, Colombo C, Smith P. Symptoms of depression and anxiety and adherence to antihypertensive medication. Am J Hypertens. 2012;25:505–11. doi: 10.1038/ajh.2011.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim L, Jin AZ, Ng TP. Anxiety and depression, chronic physical conditions, and quality of life in an urban population sample study. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1047–53. doi: 10.1007/s00127-011-0420-6. [DOI] [PubMed] [Google Scholar]
- 9.Young BJ, Beidel DC, Turner SM, Ammerman RT, McGraw K, Coaston SC. Pretreatment attrition and childhood social phobia: Parental concerns about medication. J Anxiety Disord. 2006;20:1133–47. doi: 10.1016/j.janxdis.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Leventhal H, Nerenz DR, Steele DF. Illness representation and coping with health threats. In: Baum A, Taylor SE, Singer JE, editors. Handbook of psychology and health. Vol IV. Social psychological aspects of health. Hillsdale (NJ): Erlbaum; 1984. pp. 219–52. [Google Scholar]
- 11.Baines T, Wittkowski A. A systematic review of the literature exploring illness perceptions in mental health utilising the self-regulation model. J Clin Psychol Med Settings. 2013;20:263–74. doi: 10.1007/s10880-012-9337-9. [DOI] [PubMed] [Google Scholar]
- 12.Schüz B, Wolff JK, Warner LM, Ziegelmann JP, Wurm S. Multiple illness perceptions in older adults: Effects on physical functioning and medication adherence. Psychol Health. 2014;29:442–57. doi: 10.1080/08870446.2013.863884. [DOI] [PubMed] [Google Scholar]
- 13.Hoth KF, Wamboldt FS, Bowler R, Make B, Holm KE. Attributions about cause of illness in chronic obstructive pulmonary disease. J Psychosom Res. 2011;70:465–72. doi: 10.1016/j.jpsychores.2010.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cherrington CC, Moser DK, Lennie TA, Kennedy CW. Illness representation after acute myocardial infarction: Impact on in-hospital recovery. Am J Crit Care. 2004;13:136–45. [PubMed] [Google Scholar]
- 15.Hanusch BC, O'Connor DB, Ions P, Scott A, Gregg PJ. Effects of psychological distress and perceptions of illness on recovery from total knee replacement. Bone Joint J. 2014;96(B):210–6. doi: 10.1302/0301-620X.96B2.31136. [DOI] [PubMed] [Google Scholar]
- 16.Wu H, Zhao X, Fritzsche K, Salm F, Leonhart R, Jing W, et al. Negative illness perceptions associated with low mental and physical health status in general hospital outpatients in China. Psychol Health Med. 2014;19:273–85. doi: 10.1080/13548506.2013.802358. [DOI] [PubMed] [Google Scholar]
- 17.Sherwin LB, Leary E, Henderson W. Effect of illness representations and catastrophizing on quality of life in adults with irritable bowel syndrome. J Psychosoc Nurs Ment Health Serv. 2016;54:44–53. doi: 10.3928/02793695-20160803-01. [DOI] [PubMed] [Google Scholar]
- 18.Paschalides C, Wearden AJ, Dunkerley R, Bundy C, Davies R, Dickens CM. The associations of anxiety, depression and personal illness representations with glycaemic control and health-related quality of life in patients with type 2 diabetes mellitus. J Psychosom Res. 2004;57:557–64. doi: 10.1016/j.jpsychores.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 19.Hudson JL, Bundy C, Coventry P, Dickens C, Wood A, Reeves D. What are the combined effects of negative emotions and illness cognitions on self-care in people with type 2 diabetes? A longitudinal structural equation model. Psychol Health. 2016;31:873–90. doi: 10.1080/08870446.2016.1156113. [DOI] [PubMed] [Google Scholar]
- 20.Howard C, Hallas CN, Wray J, Carby M. The relationship between illness perceptions and panic in chronic obstructive pulmonary disease. Behav Res Ther. 2009;47:71–6. doi: 10.1016/j.brat.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Thakur ER, Sansgiry S, Petersen NJ, Stanley M, Kunik ME, Naik AD, et al. Cognitive and perceptual factors, not disease severity, are linked with anxiety in COPD: Results from a cross-sectional study. Int J Behav Med. 2018;25:74–84. doi: 10.1007/s12529-017-9663-2. [DOI] [PubMed] [Google Scholar]
- 22.Costa EC, Vale S, Sobral M, Graça Pereira M. Illness perceptions are the main predictors of depression and anxiety symptoms in patients with chronic pain. Psychol Health Med. 2015;11:1–13. doi: 10.1080/13548506.2015.1109673. [DOI] [PubMed] [Google Scholar]
- 23.Morgan K, Villiers-Tuthill A, Barker M, McGee H. The contribution of illness perception to psychological distress in heart failure patients. BMC Psychol. 2014;2:50. doi: 10.1186/s40359-014-0050-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 25.Ruiz MA, Zamorano E, García-Campayo J, Pardo A, Freire O, Rejas J. Validity of the GAD-7 scale as an outcome measure of disability in patients with generalized anxiety disorder in primary care. J Affect Disord. 2011;128:277–86. doi: 10.1016/j.jad.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 26.Jordan P, Shedden-Mora MC, Löwe B. Psychometric analysis of the Generalized Anxiety Disorder scale (GAD-7) in primary care using modern item response theory. PLoS One. 2017;12:e0182162. doi: 10.1371/journal.pone.0182162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Witteman C, Bolks L, Hutschemaekers G. Development of the illness perception questionnaire mental health. J Ment Health. 2011;20:115–25. doi: 10.3109/09638237.2010.507685. [DOI] [PubMed] [Google Scholar]
- 28.Bennet KK, Adams AD, Ricks JM. Pessimistic attributional style and cardiac symptom experiences: Self-efficacy as a mediator. North Am J Psychol. 2012;14 [Google Scholar]
- 29.Padesky CA, Mooney KA. Strengths-based cognitive-behavioural therapy: A four-step model to build resilience. Clin Psychol Psychother. 2012;19:283–90. doi: 10.1002/cpp.1795. [DOI] [PubMed] [Google Scholar]
- 30.Quicky EK. Solution focused anxiety management: A treatment and training manual. San Diego, CA: Academic Press; 2013. [Google Scholar]


