Dear Editor,
Prostate cancer is an important disease worldwide.1 In 2015 it was the third most common cancer diagnosed in male in Hong Kong (China) and the incidence of prostate cancer has been rising in the past 15 years.2 Meanwhile, with increasing public awareness, health education, presentation, and detection of prostate cancer may be changed. Therefore, we would like to review how the epidemiology of prostate cancer in Hong Kong (China) had changed in the past two decades.
We have retrospectively reviewed all prostate cancer patients who were managed at public hospitals of the New Territories East Cluster in Hong Kong, China (Prince of Wales Hospital, Alice Ho Miu Ling Nethersole Hospital, and North District Hospital). The study was approved by The Joint Chinese University of Hong Kong (China) – New Territories East Cluster Clinical Research Ethics Committee. Patient consent was not required in this retrospective review. Four 2-year historical cohorts (1997–1998, 2002–2003, 2007–2008, and 2012–2013) were selected. Characteristics of the patients and cancer, treatment approach and survival of these periods were reviewed through patient medical records.
A total of 945 patients were included in this study (Table 1). Across four cohorts, there was a significant increase in the number of newly diagnosed prostate cancer (109, 184, 263, and 389 patients, respectively, for each cohort, P < 0.001). The mean age was 71.2 (standard deviation [s.d.]: 8.43) years, without significant difference between the four cohorts (P = 0.232).
Table 1.
Demographic information, survival, and hazard ratio of the four cohorts of patients
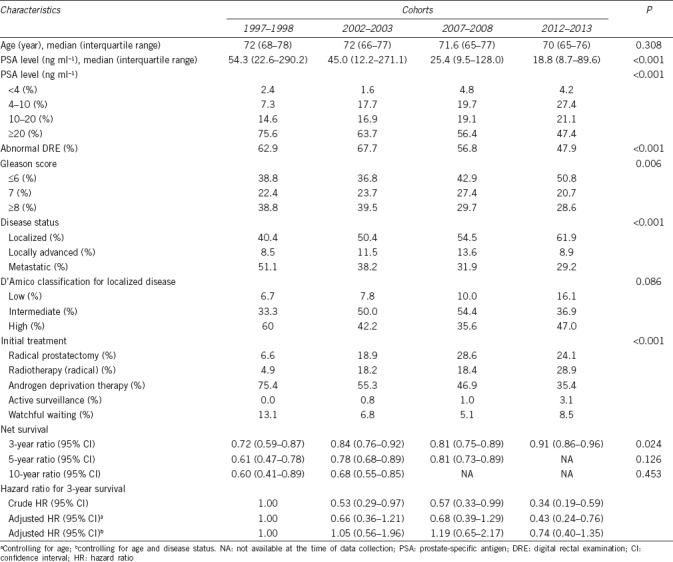
Using the cohort 1997–1998 as the control, prostate-specific antigen (PSA) level was decreasing across the cohorts (median: 57.5, 44.5, 25.5, and 18.4 ng ml−1, respectively, P < 0.001). Prostate cancer was increasingly diagnosed with normal digital rectal examination (P < 0.001). For the pathological information, there were more cases with Gleason sum <7 (P = 0.002), diagnosed at the stage of localized disease and less metastatic disease at the later cohorts (P < 0.001).
Among those patients with localized disease, we observed that an increasing proportion of patients had received radical treatment including radical prostatectomy or radiotherapy. There was also a rising trend for patients who were managed with active surveillance.
There was also statistically significant improvement in the survival of prostate cancer patients across the cohorts (Log-rank test, P = 0.0018). There appeared to be a trend of gradual improvement in net survival. The crude hazard ratios for later cohorts were all significantly <1, indicating a better 3-year survival than the reference cohort (1997–1998). However, the 3-year survival did not differ between the cohorts after adjusted for age and disease status.
As data have shown, prostate cancer is one of the most common cancers among males in Hong Kong (China).3 In our study, we observed a statistically significant increase in the diagnosis of prostate cancer. When comparing against the cohort 1997–1998, across the four cohorts, there was a significant increase in the number of newly diagnosed prostate cancer (109, 184, 263, and 389 patients, respectively, P < 0.001). This implies that long-term planning addressing prostate cancer is essential to maintain the standard of healthcare, and more resources would be needed.
We observed several important trends of prostate cancer in the past two decades. First, more patients presented with an earlier clinical stage, i.e., more patients were found to have normal digital rectal examination (T1c) at the time of diagnosis. Meanwhile, the median serum PSA level at the time of diagnosis was decreasing across our cohorts. Moreover, the proportion of metastatic disease was also found to be decreasing. These suggested that prostate cancers were detected at an earlier stage. It could be attributed by increasing awareness and health checking in Hong Kong (China).
Although the trend of earlier detection of prostate cancer was observed, from our study, the 3-year survival was not found to differ between the cohorts after adjusted for age and disease status. The relatively good survival outcome of prostate cancer could account for such observation. The potential advantage of earlier prostate cancer detection may not be reflected in our 3-year survival data.
The trend of earlier diagnosis was also observed. The median ages of diagnosis in 1997–1998 and 2012–2013 were 72 and 80 years, respectively, although it was not statistically significant across four cohorts. While this is still higher than that in the Western countries, where patients usually have prostate cancer diagnosed in their 60s, the longer life expectancy in Hong Kong (China) makes radical treatment still an option to many prostate cancer patients.
An increasing number of less aggressive prostate cancer were noted with lower PSA, lower Gleason score and less abnormal digital rectal examination. It would imply that more patients would be suitable candidates for active surveillance. In fact, we observed the trend. With the increase of suitable candidates, the improvement of public awareness and acceptance of the concept of active surveillance, it is expected that there would be more patients adopting this approach. Guidelines development for active surveillance for our population would be needed in the near future.
The overall prostate cancer survival had been improved in the past two decades. It can be attributed to the early detection of disease and improvement in cancer management. With the new evidence on the treatment of metastatic prostate cancer, patients with later stages of prostate cancer would also be expected to have further improvement in survival.4,5
There were several limitations to our study. First, it is a retrospective study. There were missing or incomplete data for cases especially in the early cohorts. Second, we retrospectively reviewed prostate cancer cases who were managed in one of the seven clusters of public hospitals in Hong Kong (China). Cases being followed up in the private sector would be missed. Third, our study was limited by the short follow-up time in terms of survival. The time for evaluating survival for prostate cancer is short for cases diagnosed in the latest cohort. However, by including these cases, we could have a better overall picture in evaluating the change in disease pattern and the initial management. Despite the aforementioned limitations, our study provides a large-scale comprehensive local data for Hong Kong (China), which may guide our service planning and resources allocation.
In conclusion, prostate cancer was increasingly diagnosed at an earlier stage in recent years in Hong Kong (China). Training and service planning are needed to maintain the treatment standard to the upcoming challenge.
AUTHOR CONTRIBUTIONS
HFW and CFN conceived of the study. HFW, CHY, JYCT, SYSC, PKFC, HYC, SSMH, and CFN participated in data collection and analysis. HFW and CHY drafted the manuscript. All authors read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
COMPETING INTERESTS
All authors declare no competing interests.
REFERENCES
- 1.Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, et al. GLOBOCAN 2012 v1.0, cancer incidence and mortality worldwide: IARC cancer base no. 11 [Internet]. International Agency for Research on Cancer, Lyon. Int J Cancer J Int Du Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Hospital Authority: Hong Kong Cancer Registry. [Last accessed on 2018 Aug 27]. Available from: http://www3.ha.org. hk/cancereg/statistics.html .
- 3.Yee CH, Ng CF. Urological malignancy in Hong Kong: the trend and the practice. Jpn J Clin Oncol. 2015;45:1103–6. doi: 10.1093/jjco/hyv145. [DOI] [PubMed] [Google Scholar]
- 4.Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373:737–46. doi: 10.1056/NEJMoa1503747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387:1163–77. doi: 10.1016/S0140-6736(15)01037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


