Abstract
Introduction:
Significant heterogeneity exists in traumatic brain injury (TBI) outcomes. In the United States, TBI remains a primary driver of injury-related mortality and morbidity. Prior work has suggested that disparity exists in rural areas; our objective was to evaluate potential differences in TBI mortality across urban and rural areas on a national scale.
Methods:
Age-adjusted TBI fatality rates were obtained at the county level across the U.S. from 2008 to 2014. To evaluate geography, urban influence codes (UIC) were also obtained at the county level. UIC codes range from 1 (most urban) to 12 (most rural). Metropolitan counties are defined as those with an UIC ≤2, while nonmetropolitan counties are defined as an UIC ≥3. County-level fatality rates and UIC classification were geospatially mapped. Linear regression was used to evaluate the change in TBI fatality rate at each category of UIC. The median TBI fatality rate was also compared between metropolitan and nonmetropolitan counties.
Results:
Geospatial analysis demonstrated higher fatality rates distributed among nonmetropolitan counties across the United States. The TBI fatality rate was 13.00 deaths per 100,000 persons higher in the most rural UIC category compared to the most urban UIC category (95% confidence interval 12.15, 13.86; P < 0.001). The median TBI rate for nonmetropolitan counties was significantly higher than metropolitan counties (22.32 vs. 18.22 deaths per 100,000 persons, P < 0.001).
Conclusions:
TBI fatality rates are higher in rural areas of the United States. Additional studies to evaluate the mechanisms and solutions to this disparity are warranted and may have implications for lower-and middle-income countries.
KEYWORDS: Disparity, geographic, lower-middle-income countries, rural, traumatic brain injury
INTRODUCTION
Significant disparities exist across the spectrum of care for traumatic brain injury (TBI); this is due primarily to heterogeneity in available resources, with resulting disparities in postinjury outcomes.[1] Lack of access to prehospital care, high-level trauma, neurosurgical interventions, and postdischarge rehabilitative services have all been associated with increased mortality and poor functional outcome.[2,3,4,5,6]
The burden of injury is disproportionately borne by populations in rural areas, where resources are limited in comparison to urban areas. Multiple studies have found a higher risk of TBI and TBI-related mortality in the U.S. rural regions.[7,8,9] Given that 60 million people (19.3% of the total U.S. population) reside in rural America, the impact of suboptimal resource distribution and management of TBI is a public health concern affecting a considerable segment of the American population.[10]
Several studies examining rural and urban differences within individual states have found disparities in TBI treatments and outcomes.[7,11] However, it is not known whether treatments and outcomes for patients with TBI differ between rural and urban environments on a national scale. The primary objective of this study was to evaluate the relationship between TBI mortality and rural geography across the United States. We hypothesized that TBI mortality would be higher in rural areas of the United States than in urban areas.
METHODS
Data sources
The Centers for Disease Control Web-based Injury Statistics Query and Reporting System was queried to identify the age-adjusted TBI-specific fatality rate per 100,000 population from 2008 to 2014 for the United States at the county level.[12] TBI was defined based on the International Classification of Disease, 10th Revision (ICD-10) codes. These codes represent patient-level diagnoses of specific injuries. The codes used for this study represent concussion or internal head injuries including the following codes: S01.0–S01.9, S02.0, S02.1, S02.3, S02.7–S02.9, S04.0, S06.0–S06.9, S07.0, S07.1, S07.8, S07.9, S09.7–S09.9, T90.1, T90.2, T90.4, T90.5, T90.8, and T90.9. Age adjustment was performed using the direct method across 5-year age categories against the standard United States population in the year 2000.[13] These rates were also geospatially smoothed to account for areas with fewer than 20 deaths over the period. This method calculates the rate for the counties with fewer than 20 deaths, using the county deaths and deaths in counties that border it, and to develop a local neighborhood rate for the small geographic locale of typically six–eight counties.[14]
County-level urban influence codes (UIC) as developed by the U.S. Department of Agriculture were then merged with U.S. counties.[15] The UIC scale ranges from 1 to 12, with one representing the most urban counties with a metro area of 1+ million residents, and 12 representing the most rural counties without a town of at least 2500 residents. The UIC is based on both geographic adjacencies to large metro areas as well as the percent of population in a county that commutes to metro areas. Metropolitan counties are defined as those with a UIC ≤2, while nonmetropolitan counties are defined as those with a UIC ≥3.
Geospatial analysis
County-level TBI fatality rates were mapped across the United States [Figure 1], represented by color ramp (high values red; low values tan), to evaluate the specific geographic pattern of TBI fatalities and geographic location in the country. In addition, a patterned overlay was added to indicate whether the county is classified as metropolitan or nonmetropolitan based on the UIC as described above to allow visual inspection of TBI fatality rates and rurality across the U.S. [Figure 2]. All geospatial analyses were performed using ArcGIS v10.5 (ESRI, Redlands, CA).
Figure 1.
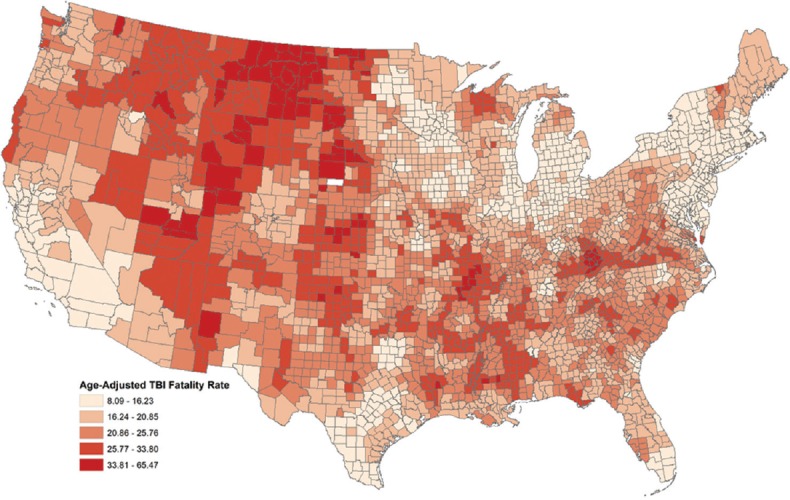
County traumatic brain injury fatality rate per 100,000 persons across the United States. The traumatic brain injury fatality rate is represented by color ramp, with higher values represented in red and lower values represented in tan
Figure 2.
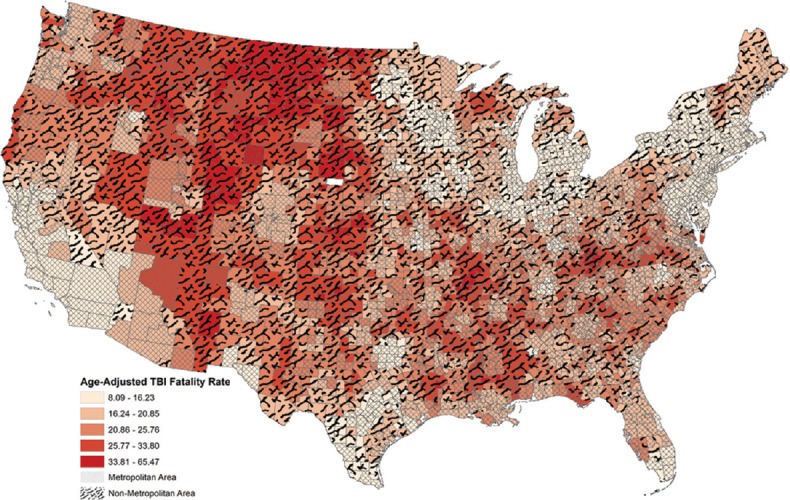
County traumatic brain injury fatality rate per 100,000 persons across the US. Higher traumatic brain injury fatality rates are represented in red and lower values in tan. The black overlay pattern represents rural nonmetropolitan counties, and the light cross-hatch pattern represents urban metropolitan counties
Statistical analysis
The mean TBI fatality rate was calculated within each UIC category and plotted over UIC to evaluate the relationship between TBI fatality rate and incrementally more rural areas in the United States. Linear regression was used to evaluate the change in TBI fatality rate at each category of UIC with the most urban UIC category as the reference. Regression coefficients for the most rural UIC category compared to the most urban UIC category are presented below. The median TBI fatality rate was also compared between metropolitan versus nonmetropolitan counties (defined above) by UIC, using the Wilcoxon rank-sum test. These evaluations were stratified by all TBI deaths, unintentional TBI deaths, and TBI deaths as a result of violence. The intention of TBI deaths was determined using the ICD-10 external cause of injury code matrix. Data analysis was conducted using Stata v15 (StataCorp; College Station, TX, USA).
RESULTS
It was observed that higher fatality rates were distributed among mid-Western and Southern counties, representing more rural areas of the United States (dark red) [Figure 1]. Applying the metropolitan/nonmetropolitan overlay (black pattern) also demonstrated higher fatality rates distributed among nonmetropolitan counties across the U.S. [Figure 2].
There was a direct relationship between mean TBI fatality rates and UIC demonstrating higher TBI fatality rates across all intentions for more rural counties [Figure 3]. For all TBI, the fatality rate was 13.00 deaths per 100,000 persons higher in the most rural UIC category compared to the most urban UIC category (95% confidence interval [CI] 12.15, 13.86; P < 0.001). The TBI fatality rate was 9.34 deaths per 100,000 persons (95% CI 8.75, 9.93; P < 0.001) higher in the most rural category for unintentional injury and 4.61 deaths per 100,000 persons (95% CI 4.12, 5.11; P < 0.001) higher in the most rural category for violent injury. The median TBI fatality rate was also significantly higher in nonmetropolitan counties compared to metropolitan counties [Figure 4]. The median TBI fatality rate from all causes was 23% higher in rural relative to urban America (P < 0.001), while the median TBI fatality rate was 30% higher from unintentional injury and 16% higher from violent injury in rural relative to urban American areas (P < 0.001, respectively).
Figure 3.
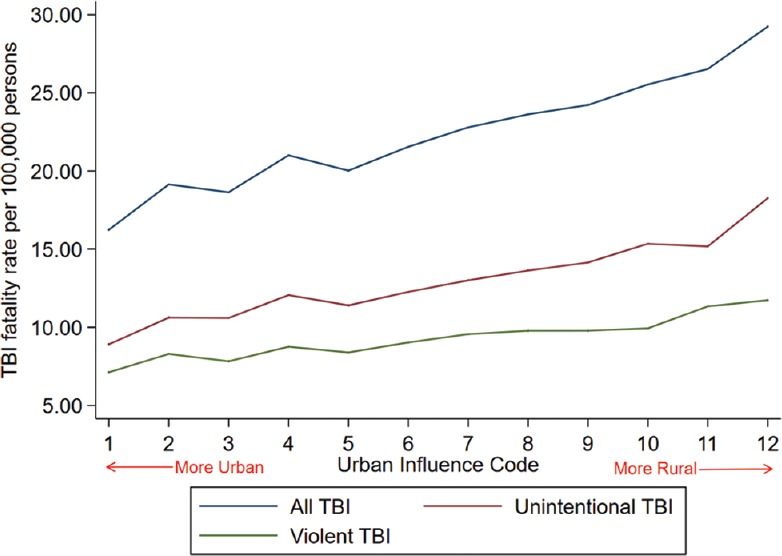
Mean traumatic brain injury fatality rate per 100,000 persons at each urban influence code category across all traumatic brain injury deaths, unintentional traumatic brain injury deaths, and violent traumatic brain injury deaths. Higher urban influence codes indicate more rural US counties
Figure 4.
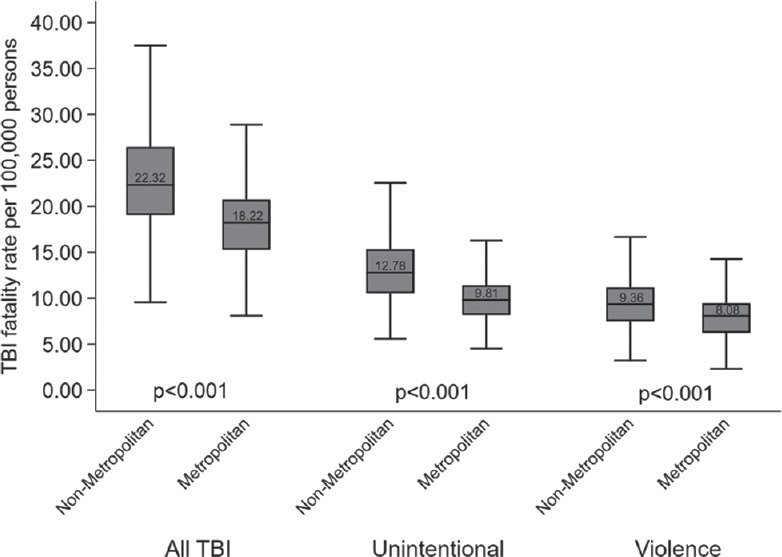
Box plot of traumatic brain injury fatality rate per 100,000 persons comparing unintentional, violent, and all traumatic brain injury deaths in nonmetropolitan and metropolitan counties. Middle line represents the median rate. Ends of the box represent the 75th and 25th percentiles. Whiskers represent 1.5 times the interquartile range
DISCUSSION
TBI is a critical global public health concern that is both widespread and costly: an estimated 69 million new cases occur annually, at a global cost of $400 billion USD.[16,17] The incidence of TBI is rising, with disproportionate increases in lower- and middle-income countries (LMICs).[16] The World Health Organization estimates that it will become the third major cause of death and disability by 2020.[18]
Even, within the United States, a high-income country (HIC), TBI remains a significant cause of morbidity and mortality. In 2010, an estimated 2.5 million TBI-related emergency department visits, hospitalizations, and deaths occurred in the U.S., and one-third of all injury-related deaths were TBI-related; these figures are believed to underestimate the true incidence.[19] An estimated 4.6 million cases occur annually in the U.S. and Canada, and up to 5.3 million people in the U.S. live with the sequelae of TBI.[16,19] For Americans, TBI carries an estimated lifetime cost of $396,000 per person.[20]
This study contributes important information to the growing body of evidence that patients, who sustain TBI in rural, predominantly low-resource environments have a significantly higher risk of death than those in urban, high-resource environments. This finding has been demonstrated in previous work by comparing outcomes from TBI in LMICs and HICs.[9,21,22] In this study, within the HIC of the United States, the disparity in outcomes from TBI for patients in rural versus urban environments is clearly demonstrated; all-cause mortality from TBI is 23% higher in rural areas relative to urban areas of the United States.
Guidelines for the management of TBI have been shown to reduce the burden of mortality and morbidity in mature, resource-rich environments.[6,23,24] Multiple studies have found that adherence to the most widely adopted guidelines for TBI management, developed by the Brain Trauma Foundation, has helped to reduce TBI-related mortality.[25,26] These evidence-based guidelines have now been available for the past 20 years.[27,28,29] However, their clinical application remains limited for two major reasons.
First, the treatment recommendations can only be generated where evidence is available. The recent update of the Guidelines for the Management of Severe TBI provides 28 recommendations as follows: one Level I, 18 Level II, and nine Level III.[29] These recommendations provide some information that can be used for a “bedside” clinical protocol, but major gaps remain; to create a complete clinical protocol, it is necessary to fill those gaps using consensus from clinical experts.[30]
Second, the guidelines are mainly derived from studies conducted in HICs, and as such are specific to high-resource environments. They have limited applicability in resource-poor settings, a common scenario in LMICs.[1,17] LMICs and rural populations within the U.S. also have unique epidemiological characteristics and capacity-building constraints that limit the optimal implementation of existing TBI guidelines.[31] Most guidelines do not address costs and barriers to implementation or epidemiologic factors that may influence the outcome.[1,32,33] As such, recent efforts to implement well-validated, guideline-recommended interventions in LMICs have yielded mixed results.[1,34] As the recognition of these limitations has grown, multiple efforts have been undertaken to develop evidence-based practices for low-resource environments. Till date, many of these efforts are country-specific or region-specific, for example, Sub-Saharan Africa, Hungary, and Colombia.[35,36,37]
There is evidence that even within the United States, unequal distribution of healthcare facilities and resources exists.[5,25,26,38] Similarly, adoption of evidence-based guidelines for TBI is not uniform across the U.S., with resource-limited, rural areas demonstrating lower levels of adherence than their comparatively wealthier urban counterparts.[8,9,26] Taken together, the lack of evidence for complete clinical protocols and the lack of evidence specific to low-resource environments render currently available evidence-based guidelines of questionable generalizability in both LMICs and rural areas of HICs.
For the most part, efforts to implement and assess clinical protocols that are specific to low-resource environments have taken place in LMICs.[1,39,40,41] The feasibility of conducting such a study in a HIC, however, is limited. For example, although 60 million people live in rural areas of the U.S., the number of patients per center presenting with severe TBI is low.[4,8,31] To collect a meaningful sample size in the U.S., it would be necessary to recruit many centers in many regions of the country and collect data over an extended period. The costs of such a multicenter study would be prohibitively high and the logistical and organizational challenges expansive. A low-resource environment with a high percent census of severe TBI patients would allow for a more efficient and less costly means of collecting data that can address which interventions are most effective in improving outcomes from severe TBI in low-resource environments.
Granted, differences exist between LMICs and rural areas of HICs regarding characteristics such as demographics, epidemiological factors, prevailing injury patterns, and availability of treatment resources – These differences may limit the generalizability of findings from populations in an LMIC to populations in rural areas of HICs. Nevertheless, a well-controlled study in an LMIC with a sample size sufficient to utilize robust and flexible analytic methods may provide information that would be useful to rural regions of HICs.[42]
CONCLUSIONS
TBI fatality rates are higher in rural areas of the United States relative to urban areas. This disparity is likely due in part to differences in resource availability. Additional studies are needed to (1) better characterize the unmet needs of rural Americans who sustain TBI and (2) develop treatment guidelines that can effectively address the unique conditions and resource limitations contributing to poorer outcomes from TBI in these communities. Similarly, investigations done in resource-constrained LMICs may have important implications for improving outcomes from TBI in rural areas of HICs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rubiano AM, Carney N, Chesnut R, Puyana JC. Global neurotrauma research challenges and opportunities. Nature. 2015;527:S193–7. doi: 10.1038/nature16035. [DOI] [PubMed] [Google Scholar]
- 2.Rudehill A, Bellander BM, Weitzberg E, Bredbacka S, Backheden M, Gordon E, et al. Outcome of traumatic brain injuries in 1,508 patients: Impact of prehospital care. J Neurotrauma. 2002;19:855–68. doi: 10.1089/08977150260190447. [DOI] [PubMed] [Google Scholar]
- 3.Nielsen K, Mock C, Joshipura M, Rubiano AM, Zakariah A, Rivara F, et al. Assessment of the status of prehospital care in 13 low- and middle-income countries. Prehosp Emerg Care. 2012;16:381–9. doi: 10.3109/10903127.2012.664245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alkhoury F, Courtney J. Outcomes after severe head injury: A national trauma data bank-based comparison of level I and level II trauma centers. Am Surg. 2011;77:277–80. [PubMed] [Google Scholar]
- 5.DuBose JJ, Browder T, Inaba K, Teixeira PG, Chan LS, Demetriades D, et al. Effect of trauma center designation on outcome in patients with severe traumatic brain injury. Arch Surg. 2008;143:1213–7. doi: 10.1001/archsurg.143.12.1213. [DOI] [PubMed] [Google Scholar]
- 6.Gupta D, Sharma D, Kannan N, Prapruettham S, Mock C, Wang J, et al. Guideline adherence and outcomes in severe adult traumatic brain injury for the CHIRAG (Collaborative head injury and guidelines) study. World Neurosurg. 2016;89:169–79. doi: 10.1016/j.wneu.2015.12.097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gabella B, Marine WW, Hoffman RE. Brain injuries in Colorado. Brain. 1997;7:207–12. doi: 10.1016/s1047-2797(96)00150-0. [DOI] [PubMed] [Google Scholar]
- 8.Tiesman H, Young T, Torner JC, McMahon M, Peek-Asa C, Fiedler J, et al. Effects of a rural trauma system on traumatic brain injuries. J Neurotrauma. 2007;24:1189–97. doi: 10.1089/neu.2006.0196. [DOI] [PubMed] [Google Scholar]
- 9.Jarman MP, Castillo RC, Carlini AR, Kodadek LM, Haider AH. Rural risk: Geographic disparities in trauma mortality. Surgery. 2016;160:1551–9. doi: 10.1016/j.surg.2016.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Public Information Office. New Census Data Show Differences between Urban and Rural Populations. Washington, DC: U.S. Census Bureau; 2016. [Last accessed on 2016 Dec 08]. Available from: https://www.census.gov/newsroom/press-releases/2016/cb16-210.html . [Google Scholar]
- 11.Schootman M, Fuortes L. Functional status following traumatic brain injuries: Population-based rural-urban differences. Brain Inj. 1999;13:995–1004. doi: 10.1080/026990599121007. [DOI] [PubMed] [Google Scholar]
- 12.Injury Prevention and Control: Data and Statistics (WISQARS): Fatal Injury Data. Atlanta: Centres for Disease Control and Prevention; 2008-2018. [Last accessed on 2018 Feb 05; Last accessed on 2018 May 15]. Available from: http://www.cdc.gov/injury/wisqars/fatal.html . [Google Scholar]
- 13.Klein RJ, Schoenborn CA. Age-Adjustment Using the 2000 Projected U.S. Population. Statistical Notes; No. 20. Hyattsville, Maryland: National Center for Health Statistics; 2001. [PubMed] [Google Scholar]
- 14.WISQARS Fatal Injury Mapping Help Menu. 3.3 Smoothed Rate Calculations. Atlanta: Centres for Disease Control and Prevention; c2008-2018; [Last accessed on 2018 Jul 21; Last accessed on 2018 Aug 15]. Available from: https://www.cdc.gov/injury/wisqars/mapping_help/smoothed_rate.html . [Google Scholar]
- 15.Hall SA, Kaufman JS, Ricketts TC. Defining urban and rural areas in U.S. Epidemiologic studies. J Urban Health. 2006;83:162–75. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dewan MC, Rattani A, Gupta S, Baticulon RE, Hung YC, Punchak M, et al. Estimating the global incidence of traumatic brain injury. J Neurosurg. 2018;128:1–18. doi: 10.3171/2017.10.JNS17352. [DOI] [PubMed] [Google Scholar]
- 17.Maas AIR, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A, et al. Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16:987–1048. doi: 10.1016/S1474-4422(17)30371-X. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Neurological Disorders: Public Health Challenges. Geneva: World Health Organization; 2006. [Google Scholar]
- 19.Atlanta, GA: Centres for Disease Control and Prevention; 2015. National Center for Injury Prevention and Control. Division of Unintentional Injury Prevention. Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. [Google Scholar]
- 20.Faul M, Wald MM, Rutland-Brown W, Sullivent EE, Sattin RW. Using a cost-benefit analysis to estimate outcomes of a clinical treatment guideline: Testing the brain trauma foundation guidelines for the treatment of severe traumatic brain injury. J Trauma. 2007;63:1271–8. doi: 10.1097/TA.0b013e3181493080. [DOI] [PubMed] [Google Scholar]
- 21.De Silva MJ, Roberts I, Perel P, Edwards P, Kenward MG, Fernandes J, et al. Patient outcome after traumatic brain injury in high-, middle- and low-income countries: Analysis of data on 8927 patients in 46 countries. Int J Epidemiol. 2009;38:452–8. doi: 10.1093/ije/dyn189. [DOI] [PubMed] [Google Scholar]
- 22.Mauritz W, Wilbacher I, Majdan M, Leitgeb J, Janciak I, Brazinova A, et al. Epidemiology, treatment and outcome of patients after severe traumatic brain injury in European regions with different economic status. Eur J Public Health. 2008;18:575–80. doi: 10.1093/eurpub/ckn079. [DOI] [PubMed] [Google Scholar]
- 23.Alarcon JD, Rubiano AM, Chirinos MS, Valderrama A, Gich I, Bonfill X, et al. Clinical practice guidelines for the care of patients with severe traumatic brain injury: A systematic evaluation of their quality. J Trauma Acute Care Surg. 2013;75:311–9. doi: 10.1097/TA.0b013e3182924bf8. [DOI] [PubMed] [Google Scholar]
- 24.Arabi YM, Haddad S, Tamim HM, Al-Dawood A, Al-Qahtani S, Ferayan A, et al. Mortality reduction after implementing a clinical practice guidelines-based management protocol for severe traumatic brain injury. J Crit Care. 2010;25:190–5. doi: 10.1016/j.jcrc.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Fakhry SM, Trask AL, Waller MA, Watts DD IRTC Neurotrauma Task Force. Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. J Trauma. 2004;56:492–9. doi: 10.1097/01.ta.0000115650.07193.66. [DOI] [PubMed] [Google Scholar]
- 26.Cnossen MC, Scholten AC, Lingsma HF, Synnot A, Tavender E, Gantner D, et al. Adherence to guidelines in adult patients with traumatic brain injury: A living systematic review. J Neurotrauma. 2016;33:1–14. doi: 10.1089/neu.2015.4121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bullock R, Chesnut RM, Clifton G, Ghajar J, Marion DW, Narayan RK, et al. Guidelines for the management of severe traumatic brain injury, first edition. J Neurotrauma. 1996;13:643–734. [Google Scholar]
- 28.Bratton S, Bullock R, Carney N, Chesnut RM, Coplin W, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury, 3rd edition. J Neurotrauma. 2007;24:S1–106. [Google Scholar]
- 29.Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, 4th edition. Neurosurgery. 2017;80:6–15. doi: 10.1227/NEU.0000000000001432. [DOI] [PubMed] [Google Scholar]
- 30.Picetti E, Iaccarino C, Servadei F. Letter: Guidelines for the management of severe traumatic brain injury 4th edition. Neurosurgery. 2017;81:E2. doi: 10.1093/neuros/nyx086. [DOI] [PubMed] [Google Scholar]
- 31.Hesdorffer DC, Ghajar J, Iacono L. Predictors of compliance with the evidence-based guidelines for traumatic brain injury care: A survey of United States trauma Centers. J Trauma. 2002;52:1202–9. doi: 10.1097/00005373-200206000-00031. [DOI] [PubMed] [Google Scholar]
- 32.Patel A, Vieira MM, Abraham J, Reid N, Tran T, Tomecsek K, et al. Quality of the development of traumatic brain injury clinical practice guidelines: A systematic review. PLoS One. 2016;11:e0161554. doi: 10.1371/journal.pone.0161554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bonow RH, Barber J, Temkin NR, Videtta W, Rondina C, Petroni G, et al. The outcome of severe traumatic brain injury in Latin America. World Neurosurg. 2018;111:e82–90. doi: 10.1016/j.wneu.2017.11.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W, et al. A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med. 2012;367:2471–81. doi: 10.1056/NEJMoa1207363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eaton J, Hanif AB, Grudziak J, Charles A. Epidemiology, management, and functional outcomes of traumatic brain injury in Sub-Saharan Africa. World Neurosurg. 2017;108:650–5. doi: 10.1016/j.wneu.2017.09.084. [DOI] [PubMed] [Google Scholar]
- 36.Sorinola A, Buki A, Sandor J, Czeiter E. Effectiveness of traumatic brain injury management guideline introduction in Hungary. Turk Neurosurg. 2018;28:410–5. doi: 10.5137/1019-5149.JTN.19396-16.1. [DOI] [PubMed] [Google Scholar]
- 37.Kesinger MR, Puyana JC, Rubiano AM. Improving trauma care in low- and middle-income countries by implementing a standardized trauma protocol. World J Surg. 2014;38:1869–74. doi: 10.1007/s00268-014-2534-y. [DOI] [PubMed] [Google Scholar]
- 38.Harrison AL, Hunter EG, Thomas H, Bordy P, Stokes E, Kitzman P, et al. Living with traumatic brain injury in a rural setting: Supports and barriers across the continuum of care. Disabil Rehabil. 2017;39:2071–80. doi: 10.1080/09638288.2016.1217081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Charry JD, Rubiano AM, Puyana JC, Carney N, Adelson PD. Damage control of civilian penetrating brain injuries in environments of low neuro-monitoring resources. Br J Neurosurg. 2016;30:235–9. doi: 10.3109/02688697.2015.1096905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rubiano A, Morales P, Alarcon J. Clinical Practice Guidelines for the Diagnosis and Treatment of Adult Patients with Severe Traumatic Brain Injury. Colombia Ministry of Health; Guideline No. 2014-30. 2014 [Google Scholar]
- 41.Chesnut RM, Temkin N, Dikmen S, Rondina C, Videtta W, Petroni G, et al. A method of managing severe traumatic brain injury in the absence of intracranial pressure monitoring: The imaging and clinical examination protocol. J Neurotrauma. 2018;35:54–63. doi: 10.1089/neu.2016.4472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stukel TA, Fisher ES, Wennberg DE, Alter DA, Gottlieb DJ, Vermeulen MJ, et al. Analysis of observational studies in the presence of treatment selection bias: Effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. JAMA. 2007;297:278–85. doi: 10.1001/jama.297.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]


