Abstract
Many processes in the human body — including brain function — are regulated over the 24-hour cycle, and there are strong associations between disrupted circadian rhythms (for example, sleep–wake cycles) and disorders of the CNS. Brain disorders such as autism, depression and Parkinson disease typically develop at certain stages of life, and circadian rhythms are important during each stage of life for the regulation of processes that may influence the development of these disorders. Here, we describe circadian disruptions observed in various brain disorders throughout the human lifespan and highlight emerging evidence suggesting these disruptions affect the brain. Currently, much of the evidence linking brain disorders and circadian dysfunction is correlational, and so whether and what kind of causal relationships might exist are unclear. We therefore identify remaining questions that may direct future research towards a better understanding of the links between circadian disruption and CNS disorders.
Circadian rhythms are near-24-hour oscillations found in essentially every physiological process in the human brain and body1. The suprachiasmatic nucleus (SCN) in the hypothalamus serves as the master pacemaker that sets the timing of rhythms by regulating neuronal activity, body temperature and hormonal signals2 (FIG. 1).
Fig. 1 |. The circadian timing system.
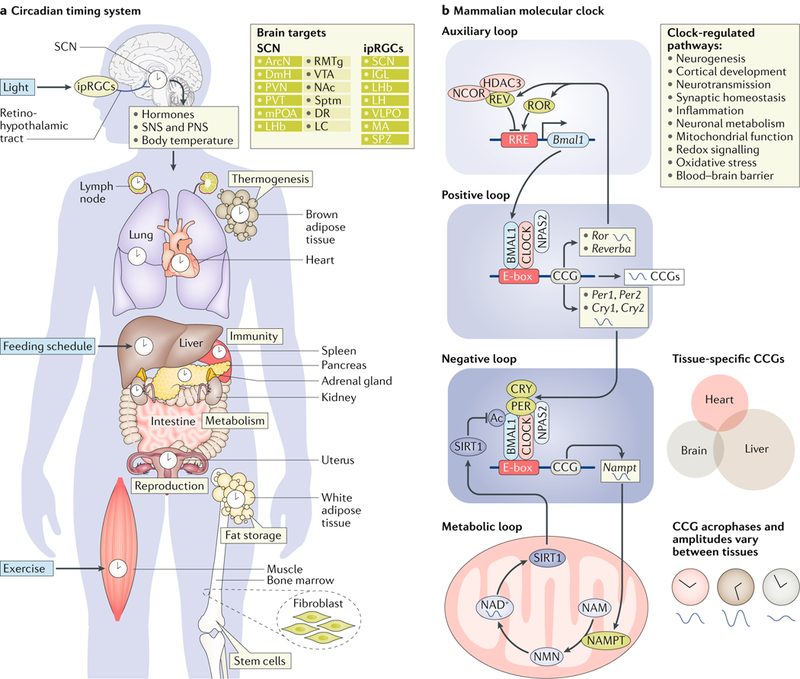
a | The circadian timing system synchronizes clocks across the entire body to adapt and optimize physiology to changes in our environment. Light is received by specialized melanopsin-producing photoreceptive retinal ganglion cells (ipRGCs) in the eye. These ipRGCs project through the retinohypothalamic tract to the suprachiasmatic nucleus (SCN), among other brain regions. The SCN relays timing information to other areas of the brain via direct projections (dark green boxes) and indirect projections (light green boxes). Humoral signals and the peripheral nervous system (that is, the sympathetic nervous system (SNS) and parasympathetic nervous system (PNS)) convey information from the SCN to orchestrate peripheral clocks. Feeding schedules and exercise can also entrain central and peripheral clocks. Circadian rhythms are key regulators of thermogenesis, immune function, metabolism, reproduction and stem cell development. b | The mammalian molecular clock is composed of transcriptional and translational feedback loops that oscillate with a near-24-hour cycle. The positive loop is driven by the heterodimerization of either circadian locomotor output cycles protein kaput (CLOCK) or neuronal PAS domain-containing protein 2 (NPAS2) with brain and muscle ARNT-like 1 (BMAL1) in the nucleus. The resulting heterodimers bind to enhancer boxes (E-boxes) in gene promoters to regulate the transcription of clock-controlled genes (CCGs), including those encoding period (PER) proteins and cryptochrome (CRY) proteins. PER and CRY proteins accumulate in the cytoplasm during the circadian cycle, eventually dimerizing and shuttling to the nucleus to inhibit their own transcription, thus closing the negative-feedback loop. The auxiliary loop includes the nuclear retinoic acid receptor-related orphan receptors (RORα and RORβ) and REV-ERBs (REV-ERBα and REV-ERBβ), which are also transcriptionally regulated by CLOCK–BMAL1 heterodimers. REV-ERBα (REV in the figure) and RORα repress and activate the transcription of Bmal1, respectively, by inhibiting and activating the ROR or REV-ERB response elements (RREs). CLOCK–BMAL1 complexes also control the expression of nicotinamide phosphori-bosyltransferase (NAMPT), which is the rate-limiting enzyme of NAD+ biosynthesis from nicotinamide (NAM). NAM is modified by NAMPT to produce nicotinamide mononucleotide (NMN), which in turn is converted to NAD+ by several adenyltransferases. Thus, NAMPT oscillations control circadian fluctuations in NAD+ levels, which in turn modulate sirtuin 1 (SIRT1) activity and signalling. High levels of NAD+ promote SIRT1 activation. SIRT1 interacts directly with CLOCK–BMAL1 to deacetylate BMAL1 and inhibit CLOCK-driven transcription. Between tissues and cell types, CCGs and other molecular and cellular rhythms may be expressed with different acrophases (phase of peak expression), amplitudes and even periodicities. ArcN, arcuate nucleus; DmH, dorsomedial hypothalamus; DR, dorsal raphe; IGL, intergeniculate leaflet; LC, locus coeruleus; LH, lateral hypothalamus; LHb, lateral habenula; MA, medial amygdala; mPOA, medial preoptic area; NAc, nucleus accumbens; PVN, paraventricular nucleus of the hypothalamus; PVT, paraventricular nucleus of the thalamus; RMTg, rostromedial tegmental nucleus; Sptm, septum; SPZ, subparaventricular zone; VLPO, ventrolateral preoptic nucleus; VTA, ventral tegmental area.
In individual cells, molecular rhythms are generated by a transcriptional–translational feedback loop involving core transcriptional activators — circadian locomotor output cycles kaput (CLOCK), the closely related neuronal PAS domain protein 2 (NPAS2) and brain and muscle ARNT-like protein 1 (BMAL1) — that regulate the expression of many genes, including those encoding period (PER) and cryptochrome (CRY)1, which, once translated, inhibit their own transcription. Many other proteins, including various kinases, phosphatases and other transcriptional cofactors, regulate this core molecular clock (FIG. 1).
Circadian rhythms are set by both genetic and environmental factors. Most people have sleep–wake and activity rhythms that, in the absence of environmental cues, are slightly longer than 24 hours3,4, but the length of this period can be affected by circadian gene variants5. Environmental factors such as light exposure, social cues, meal times and work schedules also influence the period, phase and amplitude of these rhythms6,7.
Circadian rhythms emerge during early infancy but undergo various changes through the lifespan and with ageing (FIG. 2). In general, the timing of sleep onset and waking and other biological rhythms (for example, fluctuations in melatonin levels) is earlier relative to adults during early childhood8,9 and shifts later during adolescence, and this shift in timing may be conserved among rodents and non-human primates (NHPs)10. In older adults, rhythms often return to being substantially earlier, and this shift may be accompanied by a weakening of circadian rhythms11,12.
Fig. 2 |. rhythms across the lifespan.
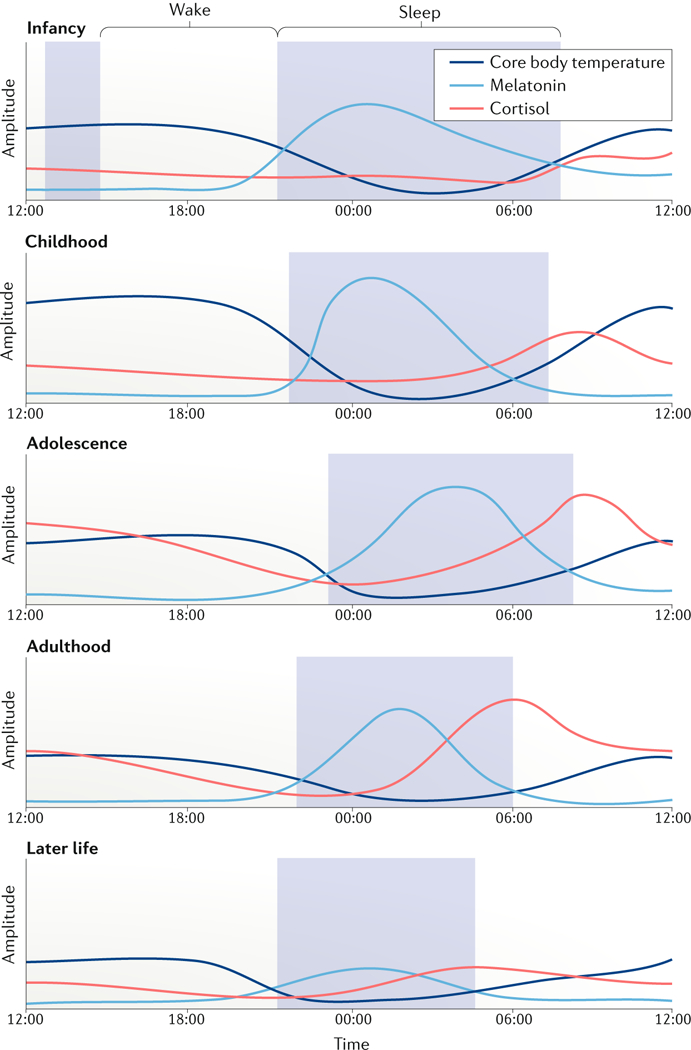
Schematic of circadian rhythm changes from infancy, adolescence, adulthood and older age. During infancy, sleep–wake rhythms are ultradian and consolidate during the first year of development. From childhood to adolescence, there is a marked shift from an early to a late chronotype, which subsequently becomes earlier during adulthood, with shorter sleep durations through adulthood. Rhythms undergo a gradual loss of amplitude with ageing. Temperature rhythms peak during childhood, and amplitudes steadily reduce during ageing. Melatonin rhythms are delayed during adolescence, with overall levels peaking during childhood and considerably decreasing during ageing. Similarly, rodent studies have demonstrated that suprachiasmatic nucleus (SCN) activity rhythms gradually decline with ageing (not shown). Cortisol rhythms peak earlier in the morning during childhood and, with age, gradually widen and reduce in overall amplitude. The amplitude of rhythmic gene expression in the brain and other tissues is reduced during ageing, affecting tissue homeostasis and function (not shown).
Circadian dysfunction is observed in several brain disorders, typically emerging at different stages of life. Disruption of circadian rhythms is associated with higher risk of brain disorders. For example, chronic shift-workers (workers with rotating schedules or consistent night shifts) are vulnerable to various diseases13,14, including psychiatric disorders such as depression15–19. Much of the currently available evidence linking brain disorders to circadian dysfunction is correlational and may not be surprising, given the importance of circadian rhythms for brain function20. Identifying causal relationships between rhythm dysfunction and psychiatric disorders may have important implications for the treatment of disorders.
In psychiatry, neurology and behavioural medicine, novel circadian-based interventions are rare and often overlooked. Even in cases in which circadian disruption is not a primary cause of a disorder, stabilizing sleep–wake patterns using behavioural, environmental or pharmacological tools might, for example, ease symptoms. Understanding the extent to which circadian rhythms are involved in normal functioning and pathological processes requires systems-biology approaches. Such approaches have proved valuable for investigating the complex relationships between rhythms and metabolic disorders21 and continue to provide strong translational potential for treating metabolic disorders and premature ageing through molecular and behavioural therapeutics targeting the circadian system22. In this Review, we describe the changes in circadian rhythms that occur with human development into adulthood and with ageing and highlight evidence suggesting that circadian disruptions at different life stages may be associated with certain brain disorders that typically emerge during these life periods, such as neurodevelopmental, psychiatric or neurodegenerative disorders. As most of the research linking circadian disruption and brain disorders is correlational, we emphasize key findings with a particular focus on mechanism and causality. In addition, we discuss implications for treatments and interventions.
Prenatal period and early childhood
Many of our insights into the development of the circadian system are from laboratory investigations of rodents and NHPs. By mid-to-late gestation, rhythms of metabolic activity and gene expression are evident in the SCN of rodents and NHPs23–25; however, the functional importance of early prenatal development of the SCN for fetal rhythms and physiology is less well understood. In humans, melatonin and dopamine receptors appear as early as gestational week 18 in the fetal SCN26–28, suggesting melatonin and dopamine may serve as the primary communicators of circadian information for the fetus29,30. Melatonin from the mother readily passes through the placenta and the fetal blood–brain barrier and may thus be the predominant relay of time-of-day information to the fetus, particularly during the transition from dusk to night, as circulating melatonin rises31–34. Circadian rhythms of melatonin along with corticosteroid are detectable in the umbilical artery and vein, along with fetal circulation35,36. Fetal rhythms are also entrained by maternal core body temperature, feeding and hormone release27 (FIG. 3).
Fig. 3 |. Maternal and fetal rhythms.
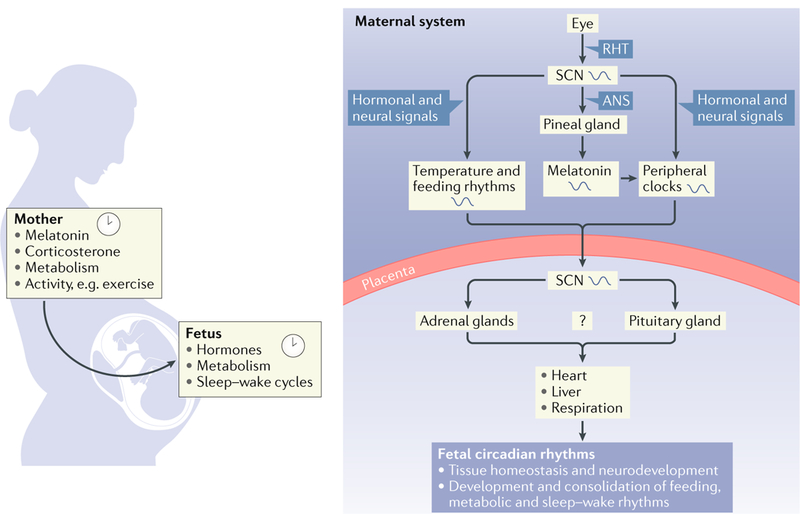
Fetal tissues such as adrenal glands and the suprachiasmatic nucleus (SCN) may be entrained by rhythms of maternal feeding schedules, core body temperature and melatonin. Entraining signals, including melatonin and glucocorticoids, may cross the placental barrier to entrain, modulate or aid the development of fetal circadian rhythms among brain and peripheral tissues. ANS, autonomic nervous system; RHT, retinohypothalamic tract.
Prenatal and maternal rhythms.
Epidemiological studies report increased risks of preterm delivery, low birthweights and miscarriage in pregnant women who are chronic shift-workers37–40. Abnormal sleep, feeding and work schedules might disrupt maternal rhythms, such as melatonin fluctuations, and thus desynchronize the maternal SCN from peripheral oscillators and lead to deleterious effects of shift-work on the fetus. Pregnant rats exposed to simulated shift-work (that is, complete reversal of the light–dark cycle every 3–4 days for several weeks) showed substantially reduced weight gain during early pregnancy and reduced fat-pad and liver weights, and also exhibited lower-amplitude rhythms of corticosterone, glucose, insulin and leptin levels41. The same manipulation also affected metabolic and circadian gene expression rhythms in the fetal liver, but did not affect placental or fetal growth41. Exposing pregnant NHPs to constant light suppresses the emergence of melatonin and body temperature rhythms in their offspring following birth42–44, suggesting that maternal rhythms are important for the early brain development of fetal circadian systems45. Moreover, the rhythms of the expression of circadian genes (specifically, Bmal1 (also known as Arntl) and Per2) and genes encoding NMDA receptor subunits (including Grin1b, Grin3a and Grin3b) are suppressed in the hippocampus of adult offspring of rats exposed to constant light during pregnancy46. Alterations in the rhythms of circadian gene expression are also associated with impaired spatial memory in these offspring46,47, and these memory deficits can be prevented by regularly scheduled supplementation of melatonin to the mother46. Gestational circadian disruption also promotes social avoidance and hyperactivity behaviours in pups, even when they are cross-fostered by non-disrupted mothers48, further highlighting the importance of circadian stability during pregnancy on the mother and offspring.
Other studies have shown that even dim light at night has physiological and behavioural consequences on parents and offspring. For example, chronically exposing mice to dim light at night impairs adaptive immune function49 and increases depression-like behaviours50 in their offspring. Notably, these effects are evident in offspring from parents exposed to dim light at night before breeding, suggesting that repeated exposure to dim light at night leads to epigenetic modifications that can be passed between generations. Such studies are particularly important because rates of shift-work and extended work schedules have increased over the past decade, as have exposures to prolonged periods of light at night from work and social demands, and the use of electronic devices51.
Rhythms in early childhood.
Circadian rhythms gradually emerge between birth and the first several months of life. Temperature rhythms appear almost immediately after birth in full-term infants, whereas other rhythms, including rest–activity, sleep–wake and hormonal cycles, typically develop between 3 and 6 months of age23,52. During the first year of life, sleep–wake rhythms continue to consolidate, coinciding with increased melatonin secretion at sunset23. Notably, nocturnal sleep onset is coupled with sunset for the first few months after birth and then to family bedtime thereafter, suggesting that the circadian system is initially entrained by light but is subsequently entrained by social and environmental factors. Most infants, toddlers (2–3-year-olds) and young children (4–11-year-olds) display earlier sleep–wake patterns and a stronger morning preference than do adults, according to the Children’s Chronotype Questionnaire — even when considering the high intra-individual and interindividual variability of sleep onset, mid-points and wake times measured by parental report questionnaires and actigraphy8,9. However, on non-scheduled days, children tend to wake up later, substantially delaying their sleep–wake times, indicating that social and environmental factors, such as schedules imposed by school and parents, have a major influence on survey-based measures of chronotype9. Importantly, children who consistently display earlier sleep onsets on scheduled days tend to delay less than do children who have later sleep onsets and wake times9.
Social environment and scheduling demands by the parents can interact with endogenous circadian and sleep rhythms, creating a state of misalignment between social schedule, endogenous circadian physiology and sleep homeostasis. Sleep loss and consistently shorter sleep durations have been linked to inattentiveness, frustration and hyperactivity in 2–5-year-old children53,54. Interestingly, before the age of 3 years, poor sleep quality and shorter sleep durations, which could be the result of inconsistent sleep–wake cycles and less-robust circadian rhythms, are predictive of hyperactivity, cognitive deficits and impulsivity at 6 years of age55,56, even in children showing normative sleep in the interim period57. Inconsistent sleep–wake cycles during early development might be contributing to the steadily rising rates of emotional and behavioural problems in young children58–61. Additional — ideally longitudinal — studies from infancy and through early childhood are needed to better understand the interplay between environment and biology in the development of the circadian system and the rest of the brain and their potential involvement in cognitive, mood and behavioural issues. In support of this, a large twin study suggested that shared environments (rather than genetics) are the primary influencer of sleep abnormalities and behavioural problems62, although these findings do not preclude the involvement of genetic or other biological factors that shape early parenting practices.
At birth, light is the most important stimulus for entraining circadian rhythms. Rodent studies demonstrate that melanopsin photoreceptors are present prenatally, are light-responsive after gestation and undergo functional reorganization and maturation during the first few weeks of life63–69. In rats, photic inputs to the SCN are mature after postnatal day 10 (reF.64), whereas in mice, these pathways reach maturity by postnatal day 14, when the eyes fully open67,69. A few studies have shown that the eyes of infants who were born prematurely can respond to light as early as gestational week 30, suggesting that photic input pathways may be functional during the third trimester of development70,71. Studies in baboons reveal that metabolic activity and gene expression in the SCN are highly responsive to light inputs in full-term infants and can be entrained by low-intensity light, similar to human infants72–74.
Regular light–dark schedules and/or low-intensity lighting, as well as particular wave lengths of light that affect the circadian clock, may be beneficial for the over-all health of premature infants75–77. In neonatal intensive care units (NICUs) worldwide, constant lighting conditions are often used to aid the care and nursing staff to readily respond to potential emergencies and frequent health monitoring78. However, rearing premature infants (32 weeks gestational age or older) under regular light–dark schedules in the NICU leads to greater and more rapid weight gain than rearing infants under constant bright light or dim light, effectively shortening their hospital stays76,77. Premature infants kept in regular light–dark conditions also fed orally sooner and spent fewer days on ventilator assistance, but had similar motor coordination compared with infants under continuous near darkness in the NICU (28–32 weeks of gestation)79–85. Moreover, compared with infants in constant dim light, these infants cry less and are more active in the daytime81. Regular light–dark schedules also support the maturation of rest–activity, sleep–wake and melatonin rhythms earlier in premature infants71,85. Although more controlled comparative studies are necessary, these findings strongly suggest that regular light–dark and feeding schedules may substitute, in part, for the early loss of the influence of maternal rhythms and loss of the constant darkness environment in utero in premature infants. Larger multisite randomized trials will be necessary to determine the extent to which different light–dark schedules might improve long-term health outcomes in infants in the NICU.
Neurodevelopmental disorders
Sleep disturbances and circadian disruptions are associated with several neurodevelopmental disorders, including attention-deficit hyperactivity disorder (ADHD), autism spectrum disorders (ASDs), Prader–Willi syndrome (PWS) and Smith–Magenis syndrome (SMS). One of the most common neurodevelopmental disorders of childhood, ADHD, is characterized by inattentiveness, impulsivity and hyperactivity and is associated with high rates of co-occurring sleep problems and circadian alterations86. Reductions in sleep quality, delays in circadian phase and evening preference are consistently reported in children and adults with ADHD87 and may be correlated with the severity of ADHD symptoms88. In adults with ADHD, a loss of circadian gene expression rhythms in the oral mucosa accompanies delays in cortisol rhythm and reduced-amplitude melatonin rhythms89. Advancing melatonin rhythms using bright light therapy improves ADHD symptoms of hyperactivity and impulsivity in adults independent of changes in sleep time, sleep efficiency, wake time or waking during sleeping87,90.
Abnormal melatonin rhythms (for example, with phase delays and reduced amplitude) are also reported in children with ADHD87. Studies of sleep–wake cycles in children with ADHD are often complicated by the effects of stimulants used to treat the disorder91. Interestingly, modafinil, a stimulant used to treat narcolepsy and shift work disorders, may be effective for treating ADHD92 and, along with targeting dopaminergic signalling, may also target therapeutic mechanisms distinct from those targeted by amphetamine and methylphenidate, including central histamine and orexin signalling pathways, to improve sleep efficiency and quality93.
Studies have also tenuously associated dysfunction in circadian rhythms with ASD, a neurodevelopmental disorder characterized by impairments in social communication, restricted interests and repetitive behaviours. Sleep problems are very common in children with ASD94–96, although revealing any underlying circadian abnormalities has proved difficult97,98. The most consistent related finding in prepubertal children, pubertal adolescents and young adults with ASD is reduced melatonin levels in the evening99–102. A genetic basis for impaired melatonin synthesis in ASD was proposed following the finding that unaffected parents of children with ASD have lower evening melatonin levels and lower activity of the acetylserotonin methyltransferase (ASMT) enzyme102, which converts N-acetylserotonin to melatonin103. Variants identified in the promoter of the ASMT gene were specific to individuals with ASD compared with controls and were associated with reduced ASMT activity and melatonin levels102. In addition to its role in sleep and circadian rhythms, melatonin is also a potent antioxidant. Reductions in melatonin during early development have been hypothesized to lead to a build-up of oxidative stress, which is harmful to the developing nervous system and increases the risk of neurodevelopmental disorders such as ASD104. A double-blind placebo-controlled study of 125 children and adolescents (2–17.5 years of age) supports the use of melatonin supplementation to treat sleep disturbances associated with ASD105 and may lead to other therapeutic approaches targeting circadian rhythms and sleep issues, as well as other symptoms of ASD106.
Other neurodevelopmental disorders, such as PWS and SMS, are linked more directly to dysfunctional circadian rhythm pathways107,108. PWS is characterized by hypotonia and failure to thrive in infancy and early toddlerhood followed by hyperphagia and childhood obesity, intellectual impairment, hypogonadism and obsessive–compulsive-related behaviours109, and it is due to a paternal deficiency of the 15q11–13 locus110. PWS is also accompanied by shorter sleep duration and excessive daytime sleepiness71,111,112. The 15q11–13 locus contains several clusters of genes encoding small nucleolar RNAs (snoRNAs), including SNORD116, which is expressed in the brain of mice and humans113–115. In mice, paternal deletion of Snord116 increases the expression of several genes specifically during the light phase, including Ube3a, which encodes ubiquitin ligase E3A (UBE3A)116. UBE3A targets the circadian transcription factor BMAL1 for proteasomal degradation and thus is crucial for maintaining the pace of molecular clock timing117. UBE3A belongs to a cluster of imprinted genes also within the 15q11–13 locus. Specifically, genomic imprinting, a rare epigenetic mechanism of gene regulation and developmental imprinting118, leads to parent-of-origin-specific effects of deletion of the 15q11–13 locus. For example, SNORD116 is expressed exclusively from the paternally inherited allele113, whereas maternally inherited alleles of UBE3A are linked to PWS119,120. Maternal duplications of the 15q11–13 locus lead to increased expression of UBE3A and epigenetic silencing of the paternal antisense transcript, UBE3A-ATS121–124. The maternal allele of UBE3A is imprinted only in neurons and is expressed by alleles in other cell types120,125,126. In mice with maternal loss of Ube3a, period lengthening of locomotor rhythms and molecular rhythms in the brain are dependent on core clock factors, including CLOCK and BMAL1 (reF.127). Intriguingly, activation of the epigenetically silenced paternal Ube3a allele restores neuronal circadian function127, suggesting that targeting the locus may be useful for treatment and involve molecular-clock-dependent mechanisms. Thus, duplication of the 15q11–13 locus and developmental imprinting of SNORD116 and UBE3A may provide a molecular explanation for the circadian rhythm disruptions common to patients with PWS.
SMS is a rare neurodevelopmental disorder characterized by craniofacial and skeletal anomalies, metabolic problems and obesity, along with intellectual disability and stereotypical behaviours, and is a result of a heterozygous deletion of chromosomal region 17p11.2. The deleted region contains several genes, including the gene encoding retinoic acid induced one (RAI1), the loss of which is thought to be responsible for many of the disease characteristics. Symptoms of SMS also include sleep and circadian abnormalities, with the most extreme being a complete reversal of sleep–wake patterns (that is, daytime sleep and night-time wake)128–131.RAI1 is implicated in melatonin secretion, and inverted melatonin rhythms may be responsible for these sleep disturbances132. Mice with a heterozygous deletion of Rai1 display a shortened locomotor activity period133,134, although these mice are of mixed genetic background containing C57BL/6, which do not produce pineal melatonin. Introducing the mutation into another mouse background capable of generating endogenous melatonin may yield more pronounced effects on sleep and circadian rhythm phenotypes relevant for SMS. In human cells from patients with SMS and the mouse brain, RAI1 activates the transcription of CLOCK via direct binding to enhancer elements within intron 1 of the CLOCK gene135, demonstrating a possible mechanism by which loss of RAI1 may result in circadian dysfunction at the molecular and cellular level. Further study is required to definitively link molecular clock disruption observed in animal models of SMS and patients with the disorder to the reversal in melatonin secretion. Circadian, sleep and behavioural disturbances are the most severe and difficult to treat for individuals with SMS. Attenuating the rise of melatonin during the morning via pharmacological antagonism of β1-adrenergic receptors by acebutolol (as pineal melatonin production is stimulated by sympathetic nervous system activation of β1- and α1-receptors) has been effective for reducing daytime naps, improving concentration and reducing the frequency of tantrums in a sample of ten patients, aged 4–18 years136. Combining β1-adrenergic receptor antagonism with timed administration of exogenous melatonin greatly improves sleep (that is, leading to fewer sleep awakenings and better organized sleep stages) and also reduces disruptive behaviours during the daytime in children and adolescents with SMS137. Thus, therapies targeting the reversal of melatonin rhythms in patients with SMS may improve sleep, as well as behaviour, attention and learning137–139.
Adolescence
Humans, rodents and some NHPs undergo changes in circadian rhythms during adolescence140. At the onset of puberty, sleep–wake cycles and melatonin rhythms start to phase delay141 — a shift that is dependent on the presence of gonadal hormones, and that coincides with sexual maturity142,143. Environmental factors, such as social pressure from peers and/or decreasing parental involvement in bedtime routines, can also contribute to changes in adolescent sleep timing and duration140. Sensitivity to the phase-shifting effects of light may also play a role, which is especially important when considering the increasingly pervasive use of electronic devices at night and their influence on sleep timing, duration and quality144.Adolescents may be more sensitive to the ability of light exposure to shift rhythms at specific times of day. For example, light exposure during the night (23:00 h to 24:00 h) suppresses melatonin levels in adolescents, with greater suppression occurring in early adolescents (prepubertal to mid-pubertal adolescents aged 9–14 years) than in late adolescents (aged 11–15 years, in late pubertal to post-pubertal stages)145. Early-morning light exposure (between 03:00 h and 04:00 h) also reduced melatonin, although no differences were found between early and late adolescents145. Thus, the sensitivity of the circadian system to light exposure depends on the developmental stage and time of day, and early adolescents may be particularly vulnerable to the phase-delaying effects of light at night145. Although the amount of sleep needed per night is variable, the vast majority of US adolescents sleep less than the suggested 8–10 hours of sleep per night, according to the American Academy of Pediatrics146,147. Early school start times, which are typically more than an hour earlier in US high schools (ages 15–18 years) than in elementary schools (ages 9–10 years) or middle schools (ages 11–13 years), may contribute to these problems of shorter sleep10,148. On weekends, adolescents in the US tend to sleep later, both reverting to their natural sleep–wake cycle and possibly to recover from cumulative sleep loss during the school week149. Transitions from weekday to weekend compound the phase delay in the endogenous clock150,151 that is often referred to as ‘social jet-lag’148,152.
Substance use disorders.
Emerging evidence from studies in humans and animal models suggests that disruptions to sleep and circadian rhythms during adolescence have consequences on brain development and might contribute to the vulnerability to mood and substance use disorders (FIG. 4). Experimentation with substances often begins during mid-adolescence to late adolescence (ages ~14–18 years), and the frequency of use peaks during early to mid-20s153. Circadian disruptions (such as social jet-lag) during adolescence increase vulnerability to substance use, and conversely, chronic exposure to these substances can lead to long-lasting changes in the circadian and sleep networks154. Weekday–weekend differences in sleep timing and duration are associated with increased risk-taking behaviours, substance use and depressed mood155,156. Moreover, adolescents with shorter sleep duration are more likely to use substances, including caffeine, nicotine, alcohol and marijuana157–159, and to engage in other risky behaviours157,160,161. Longitudinal follow-up studies have found that weekend delay and sleep-timing variability during adolescence and young adulthood positively correlate with alcohol use 2 years later162 and the incidence of alcohol use disorder symptoms 3 and 5 years later163 and are associated with an earlier onset of alcohol use disorder164. Greater eveningness and later sleep timing in adolescents and young adults are associated with increased substance abuse and may not merely be a consequence of increased opportunity to engage in substance use later at night165–167. However, the roles of biological factors versus social influences remain unclear: social context is also important, and social networks may affect sleep duration and substance use in adolescents168.
Fig. 4 |. Effects of social constraints, sleep and circadian disruptions on adolescent brain function.
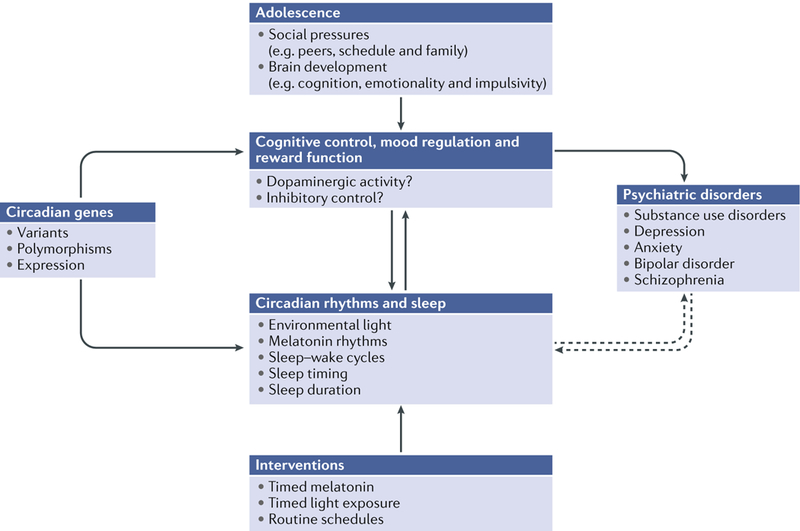
A proposed model for the associations between sleep, circadian rhythms and psychiatric disorders during adolescence. Neural circuits responsible for controlling cognition, mood and reward mature rapidly during adolescence and may be negatively affected by sleep deprivation and circadian misalignment, potentially leading to poor decision making, impulsivity and risky behaviours. Basic and clinical studies have linked circadian genes and their variants to corticostriatal dopamine and glutamatergic signalling that are important for cognition, mood and reward. These changes contribute to the vulnerability of developing psychiatric disorders. Several psychiatric disorders, including mood disorders, substance use disorders and schizophrenia, are associated with alterations in rhythms and/or sleep that affect cognition, motivation and impulsivity. Sleep and/or circadian rhythm disruptions (for example, genetic and/or environmental perturbations) are also associated with vulnerability to and the progression of psychiatric disorders. Interventions for targeting sleep and/or circadian rhythms may be therapeutically effective for treating disorders that emerge during vulnerable periods of adolescence.
During adolescence, many developmental changes occur in the frontostriatal reward circuitry, which includes the ventral striatum (VS; including the nucleus accumbens), dorsal striatum (DS) and medial prefrontal cortex (mPFC)169,170. These changes include increases in synaptic pruning and myelination107,171, as well as increases in the availability of dopamine in the limbic circuitry172,173. The combination of heightened activity in reward-related circuits and underdeveloped cognitive control centres contributes to greater emotionality, impulsivity and reward-seeking behaviour174,175. Circadian and sleep disruptions may amplify these responses by further reducing cortical control and increasing the activity of reward circuitry in human adolescents. Chronic exposure to drugs of abuse can lead to epigenetic changes affecting the molecular clock that may then alter function of the reward circuitry for long periods of time, creating more vulnerability for future drug abuse176.
Functional MRI studies reveal that the activation (that is, glucose uptake) of striatal and prefrontal brain regions during monetary reward tasks is greater in the afternoon or evening than in the morning in late adolescents and young adults (aged 19–24 years)177, and is related to morningness and eveningness chronotypes in adults178. In an age-matched cohort of late adolescents, greater VS responses to reward outcome and reduced mPFC responses to reward anticipation are associated with eveningness179 and may predict alcohol dependence167, further suggesting that certain circadian phenotypes emerging during early to late adolescence could contribute to vulnerability to substance use. In fact, larger weekday–weekend advances of sleep onset (for example, similar to the transition from early school start times to weekend schedules) are associated with lower mPFC reactivity to the anticipation and receipt of monetary reward in early adolescents (aged 11–13 years), even after adjusting for puberty, sex and total sleep time149. Lower responsivity of the PFC could lead to impaired inhibition of striatal circuits and related behaviours, including impulsivity and risk-taking. Whether these relationships between neural responses to reward and alcohol use are attributable to circadian misalignment or other factors, some of which may affect chronotype, remains unclear. For example, sleep deprivation can also alter neural reward circuitry: a single night of total sleep deprivation leads to decreases in mPFC activity and increases in VS activity in response to rewarding stimuli in young adults (aged 18–25 years)180. Further investigations in humans and animals are necessary to determine how circadian misalignment and/or disruption, along with sleep deprivation, independently and together, may affect the development of reward and cognitive neural systems and whether interventions that target these systems are clinically beneficial. A recent meta-analysis performed on nine studies investigated the impact of insomnia treatment on alcohol use disorder181. Behavioural (but not pharmacological) interventions for insomnia improved sleep quality and reduced symptoms of depression; however, there was no evidence that these interventions improved rates of alcohol abstinence, suggesting that improving sleep quality alone is not sufficient to prevent relapse. Determining whether chronobiological interventions can reduce the risk of developing substance use disorders or treat individuals with these disorders is an important and translationally relevant avenue of future research.
Mood disorders.
Adolescence is a time during which serious psychiatric disorders, including major depression, bipolar disorder and schizophrenia, tend to emerge. The overall prevalence of disorders with severe impairment and/or distress during this developmental period is 22.2%182, and the median age of onset for mood disorders is 13 years of age182. A major component of many mood, anxiety and psychotic disorders is a disrupted sleep–wake cycle183–188. In addition, circadian disruptions can precipitate mood and psychotic episodes in individuals who already have psychiatric disorders189–191. Mood symptoms can also occur in a seasonal pattern, as in seasonal affective disorder and in many cases of bipolar disorder192,193; symptoms may be related to the amount, duration and intensity of light varying across the seasons (that is, short versus long days)194. However, these disorders are very heterogeneous, and any association with disruptions in the sleep–wake cycle can be highly variable from individual to individual. Thus, similar to genetic studies, identifying a common circadian or sleep-related mechanism that is causal for all bipolar disorder or major depression is unlikely.
Similar to substance use disorders, delayed rhythms during adolescence and early adulthood are strongly associated with depression and the severity of mood symptoms195,196. More recent work has shown that circadian disruptions in adolescents who are at high risk of psychosis (that is, subthreshold symptoms of psychosis, social impairment and higher suspicion–paranoia)197 and individuals with mood disorders predict worse prognosis and symptoms in longitudinal studies198,199. Together, these findings suggest that circadian and sleep disruptions may have a role in the vulnerability to mood disorders and the precipitation of disorder symptoms.
Although the mechanisms underlying these associations remain to be elucidated, one possibility is that disrupted sleep and circadian rhythms affect the synaptic pruning and maturation of neural circuits during adolescence3,4,107,108,200. Many of these selective synaptic pruning and refinement processes occur during sleep, and sleep is crucial for proper circuit maturation and long-term memory formation in humans and animals201–204. In addition, slow-wave activity during sleep dramatically decreases specifically during adolescence; this reduction is suggested to result directly from synaptic refinement, further demonstrating important links between sleep and synaptic changes107,108. Excessive pruning or too little pruning during adolescence may be linked to the development of psychiatric disorders205,206; for example, 5 days of 50% sleep restriction in rats during early adolescence led to alterations in the fractions of projections from the motor cortex to other regions of the brain207. Therefore, insults during adolescence that affect sleep and circadian stability may contribute to the pathophysiology underlying the vulnerability and progression of these diseases later in life107,108. As an estimated 7% of adolescents meet clinical criteria for delayed sleep phase syndrome, and the majority of adolescents are reported to be sleep deprived208–210, delaying school start times should be universally considered as a potential intervention for curbing the effect of these conditions211.
Treatments to amplify, phase advance or delay circadian rhythms have been developed for potential use in psychiatric disorders in adults. These treatments include bright light therapy, acute sleep deprivation, interpersonal and social rhythm therapy and therapeutic melatonin agonists (such as agomelatine)189,212–214. Moreover, antidepressant and mood-stabilizing medications, such as lithium, valproic acid and selective serotonin reuptake inhibitors (SSRIs), all have dramatic effects on gene expression rhythms that may, at least in part, underlie their therapeutic efficacy215–217. Additionally, the rapid and lasting antidepressant effects of low-dose ketamine can be predicted based on measures of locomotor activity rhythms before treatment and on how well the treatment strengthens low-amplitude activity rhythms, suggesting that the therapeutic effects are directly related to the strengthening of the circadian system218. Thus, rhythm alignment and amplification are important therapeutic approaches to helping prevent or treat psychiatric disorders. Such chronotherapy for these disorders, however, is in its infancy and needs to be evidence-based. Chronotherapies may also need to be personalized based on the particular needs of the individual; for example, subjects with depression are more responsive to light therapy combined with wake therapy and sleep-time stabilization if they are evening chronotypes and have a positive diurnal variation in mood, with the best mood occurring in the evening219.
Adulthood
For most people, there is a gradual shift towards an earlier chronotype from adolescence into adulthood141. Between 20 and 50 years of age, men continue to have greater evening preference on average than women141,220,221, and these sex differences disappear after the age of 50 years, coinciding with menopause in women141,220,222. However, these measures of chronotype are also affected by social and work schedules, and some individuals may never shift back to a morning preference after adolescence223. Mutations in clock genes such as CRY1, NFIL3 and RORC have been linked to extreme phase delay (that is, delayed sleep–wake phase disorder) in genetic studies of families224,225. The risk of depression is increased in people with this disorder and particularly in those with a biological circadian misalignment (as measured by the dim light melatonin onset (DLMO) phase). Moreover, most people who are diagnosed with bipolar disorder have an evening chronotype that persists after adolescence191,226.
Shift-work disorder and chronic jet-lag.
Our 24-hour society depends on both shift-work and frequent travel across time zones. Shift-work has been associated with increased risk of cancer, obesity, heart disease, gastrointestinal dysfunction, sleep disorders, diabetes and depression227. A large study of 11,450 Canadian nurses found that the strongest relationship between work schedule and depression was in those who work rapidly rotating schedules and undefined rotating schedules (as opposed to slowly rotating schedules)228. This study suggests more severe circadian disruptions are associated with a greater likelihood of developing depression. Another study of ~14,000 workers in electronics manufacturing in South Korea revealed that, compared with daytime workers, shift-workers showed higher rates of insomnia, depression and suicidal ideation (with the strongest association with insomnia)229.
A survey of ~4,000 flight attendants as part of the US National Health and Nutrition Survey (NHANES) found that, compared with the general population, flight attendants are 2–5.7-fold more likely to have sleep disorders, depression, anxiety and/or fatigue230. Female flight attendants also have a higher prevalence of reproductive cancers, skin cancers and other conditions such as chronic bronchitis and heart disease230,231, probably as a consequence of carcinogens in cabin environments, including cosmic radiation and poor aircraft ventilation, but perhaps also exacerbated by night shift-work, irregular schedules and frequent crossing of time zones232,233. Taken together, many health problems during adulthood, including sleep problems, depression and anxiety, are linked to circadian disruptions that are caused by shift work or other environmental or genetic disruptions to the sleep–wake cycle.
Later life
Older people (ages ~65 years and older) generally sleep less and have poorer sleep efficiency, increased night-time awakening, increased sleep latency and greater levels of daytime sleepiness234–236. Several studies have reported declines in melatonin levels with ageing, although others find no difference compared with younger people in a healthy population237,238. When other circadian outputs are measured, older individuals show lower-amplitude body temperature rhythms, with the minimum of the endogenous phase occurring nearly 2 hours earlier than in younger individuals239.
Importantly, measures of activity and physiological rhythms in older people can be confounded by health problems, medications and eye problems such as cataracts that can reduce light input to the central clock. In humans and rodent models, the amplitude of peripheral oscillatory rhythms dampens with age, but whether this effect is due to a loss of intrinsic core clock function, to dysfunction of SCN signalling and connections240,241 or to a deficit in entrainment to the environment is unclear242. The number of vasopressin-expressing cells in the SCN in humans243,244 and rodents245,246 reduces with age, possibly altering SCN output. Moreover, some SCN cells become silent in older animals (as measured in vitro), and SCN neurons lose phase coherence with age247,248. These SCN network changes result in desynchronization and a reduction in the amplitude of neuronal activity rhythms248,249 and, ultimately, physiological and behavioural rhythms241.
In addition to SCN changes, gene expression rhythms in the human mPFC also decline with age; however, surprisingly, a separate set of genes becomes newly rhythmic in older people (aged 65 years and older)11. These rhythmic genes might be protective, as the individuals in this post-mortem study did not experience psychiatric or neurodegenerative disorders before death. There is also accumulating evidence linking disrupted sleep and circadian rhythms to neurodegenerative disorders in humans and animal models235,236.
Neurodegenerative disorders.
In older adults, less-robust circadian rhythms and more fragmented patterns of activity are risk factors for the development of dementia250. Moreover, the incidence of single-nucleotide polymorphisms (SNPs) in CLOCK and BMAL1, and in BMAL1 and PER1, are associated with increased risk of Alzheimer disease (AD) and Parkinson disease (PD), respectively251–253. Compared with healthy aged people, individuals with AD or PD show considerably lower melatonin rhythm amplitudes and excessive sleepiness, as well as other sleep–wake cycle disturbances, such as later sleep onsets254–258. In individuals with PD, these sleep–wake symptoms often precede the development of motor or cognitive symptoms and may even be useful as a diagnostic biomarker259,260, whereas in patients with AD, sleep disruptions tend to begin after diagnosis261. AD brains show marked loss of neurons in the SCN243,244,262, and SCN neuronal loss correlates with reductions in the amplitude of motor activity rhythms in the same individuals before death240. In addition, although individuals with AD still show cycling clock gene expression in multiple brain regions, they lose typical phase coherence within and across regions263.
In mice, SCN levels of sirtuin 1 (SIRT1), a metabolic sensing protein and mediator of CLOCK and BMAL1 function (FIG. 1), decline with age, potentially explaining the increase in circadian rhythm disruptions in older people241. Indeed, brain-specific knockout of Sirt1 in rodents is sufficient to phenocopy the effects of ageing on the SCN and circadian behaviour, whereas overexpression of Sirt1 is protective241. Recent studies revealed that SIRT1 binds to CLOCK at the promoter of the gene encoding tyrosine hydroxylase (TH) in dopaminergic neurons to control rhythms in TH expression and, ultimately, dopamine synthesis264 (FIG. 5). When iron is present in the cytosol (as may occur more frequently with ageing)265,266, dopamine can be oxidized into dopamine quinone (DAQ), which is highly reactive and toxic267,268. DAQ has been found in human induced pluripotent stem cell-derived dopaminergic neurons that carry mutations associated with PD269. Thus, deficits in SIRT1 may contribute to toxic levels of DAQ and neurodegeneration.
Fig. 5 |. circadian regulation of dopamine.
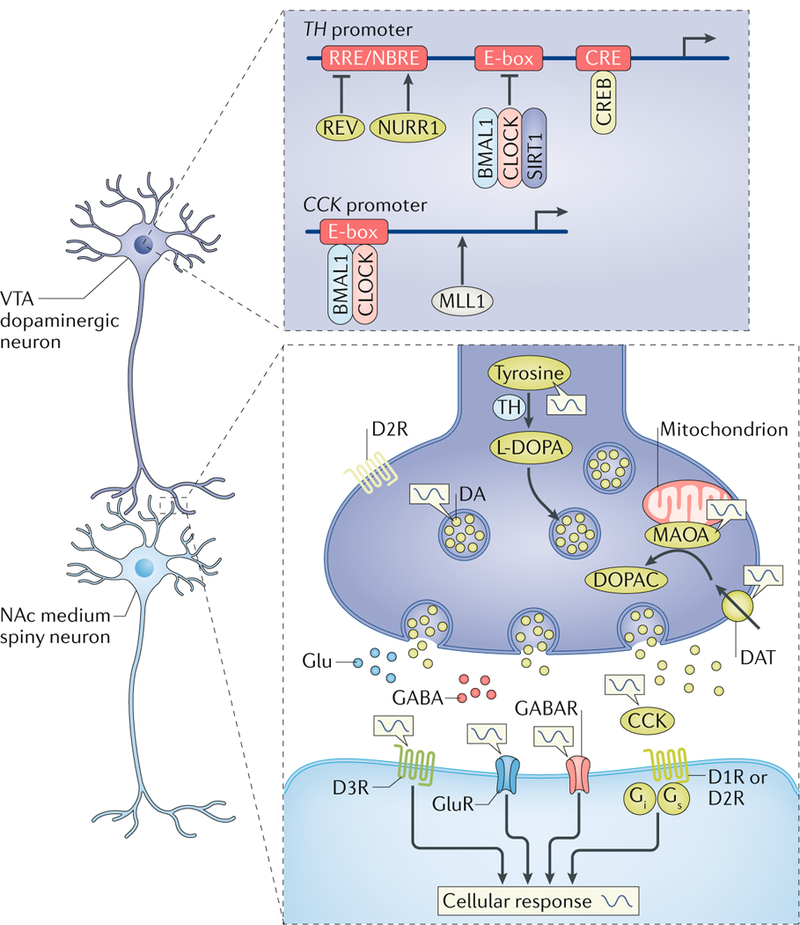
The ventral tegmental area (VTA)–nucleus accumbens (NAc) circuitry is regulated by a local molecular clock, which controls the transcription of genes involved in the dopamine (DA) signalling pathway, including those encoding: tyrosine hydroxylase (TH), the major rate-limiting enzyme converting tyrosine to the DA precursor l-dihydroxyphenylalanine (l-DOPA); cholecystokinin (CCK), a neuropeptide released from presynaptic DA terminals to suppress further DA release; and monoamine oxidase A (MAOA), a mitochondrial enzyme used to metabolize monoamine neurotransmitters, including DA. For example, the circadian transcription factors of circadian locomotor output cycles protein kaput (CLOCK) and brain and muscle ARNT-like 1 (BMAL1) form heterodimers and recruit the metabolic sensor and histone acetylase sirtuin 1 (SIRT1) to the enhancer box (E-box) within the TH promoter to repress transcription by cAMP response element-binding protein (CREB). CREB activates TH transcription via the CRE site, located proximal to the transcription start site and the circadian E-box. In addition, CLOCK is capable of binding the E-box within the Cck promoter to promote the transcription of Cck in the VTA. Mixed lineage leukaemia protein 1 (MLL1) is also recruited to CLOCK–BMAL1 heterodimers to promote the transcription of target genes via histone acetylation. REV-ERBα (REV) also represses transcription by binding the REV-ERB response element (RRE) promoter site in antiphase with the transcription factor NURR1 at the NURR1 binding motif, NBRE. Presynaptic dopamine 2 receptors (D2Rs) may also be regulated by the molecular clock. Diurnal rhythms of dopamine, glutamate and GABA levels, as well as of the expression and activity of their receptors, are present in the NAc, potentially temporally gating and promoting neuronal responses during certain times of day. DAT, DA transporter; DOPAC, 3–4-dihydroxyphenylacetic acid; GABAR, GABA receptor; Glu, glutamate; GluR, glutamate receptor (ionotropic).
PD, in particular, is strongly associated with rapid eye moment (reM) sleep behaviour disorder (RBD), as well as excessive daytime sleepiness, insomnia and restless legs syndrome270–273. In fact, more than 80% of people with RBD are later diagnosed with PD or dementia274,275. Transgenic mice overexpressing α-synuclein (a model of PD) show greater fragmentation and amplitude reduction in locomotor activity rhythms during the active phase, and these effects progress with age276. SCN neuronal firing is also reduced in these mice from young adulthood and progressively worsens with age, suggesting a weakened circadian pacemaker276 and a potential loss of dopaminergic modulation of circadian rhythms via midbrain, striatal and SCN circuits277,278. MitoPark transgenic mice also show a profound disruption of locomotor rhythms in constant conditions and are more vulnerable to changes in the light–dark cycle279.
Sundowning syndrome is prevalent in people with dementia and is characterized by increases in aggression, restlessness, delirium and agitation specifically in the late afternoon or early evening280,281. Clinical and preclinical data suggest that a lack of appropriate light–dark cues, disturbances in sleep (particularly, reductions in reM sleep) and a deterioration of the SCN pacemaker and its outputs all contribute to sundowning syndrome281. Phase delays and reductions in the amplitude of body temperature rhythms correlate with the severity of sundowning symptoms, suggesting that a breakdown of the circadian system may be responsible282. Aggression, for example, may be modulated by the circadian system. A recent study in mice revealed that rhythms in the propensity of aggressive behaviours are modulated via a polysynaptic circuit from VIP neurons in the SCN to GABAergic neurons of the subparaventricular zone, which in turn innervate the ventromedial hypothalamus, an area known to regulate aggression283. Further studies are needed to fully elucidate the biological mechanisms that underlie this syndrome, which affects many elderly people and their families.
Several processes regulated by the circadian clock could contribute to neurodegeneration, including the regulation of oxidative stress, inflammation, dopamine synthesis and cellular metabolism. One simple hypothesis is that disruptions in circadian rhythms disrupt sleep, in turn resulting in reduced clearance of misfolded and aggregated proteins that contribute to neurodegenerative disorders from the brain. A recent study found that even one night of sleep deprivation led to accumulation of amyloid-β (Aβ; one of the proteins that is pathologically accumulated in the brain in AD) in the right hippocampus and thalamus in the human brain284. These increases were negatively correlated with mood but were not associated with a particular AD-linked genotype (that is, the APOE genotype). In line with the clearance hypothesis, during sleep, the glymphatic system285 exchanges cerebrospinal fluid with interstitial fluid and clears Aβ286. Sleep deprivation increases interstitial fluid levels of Aβ and increases plaque formation in mice and flies287,288, whereas in Drosophila, genetically increasing sleep reduces Aβ deposition288. However, based on estimates of anatomical and fluid dynamic parameters, the plausibility of periarterial flow and glymphatic circulation is controversial; thus, further characterization of this system is needed289.
The build-up and expulsion of reactive oxygen species (ROS) also follow a circadian pattern. In diurnal species (including humans), ROS accumulate during the day owing to neuronal activity while awake; at night, antioxidants safely remove excess ROS during the day owing to neuronal activity while awake; at night, antioxidants safely remove excess ROS during sleep236,290. Bmal1−/− mice, which lack a functional molecular clock, show premature ageing, neurodegeneration and a reduced lifespan291. ROS accumulation is considerably higher in Bmal1−/− mice and correlates with increases in astrocytosis and levels of oxidative damage markers in the brain. Treating Bmal1−/− mice with the antioxidant N-acetyl-l-cysteine partially rescues their lifespan and prevents age-dependent pathology292. Interestingly, mice with a brain-specific Bmal1 deletion also exhibit increased astrocytosis, despite having mostly normal locomotor circadian rhythms and sleep–wake cycling (that is, relatively normal clock function in the SCN); thus, these neurodegenerative effects are probably due to loss of the local control of cellular metabolism in specific regions of the brain that is normally mediated by BMAL1, independently or as part of the molecular clock, in these cells291.
Whether circadian rhythm and sleep disruptions are primarily causal to neurodegenerative disorders remains unclear, but environmental and biological disruptions to these systems do seem to worsen progression of these diseases293–295. Thus, therapies that stabilize circadian and sleep rhythms may at least slow the progression of these disorders. Indeed, some studies indicate that morning light therapy may improve circadian rhythms and Mini-Mental State examination (MMSE), Cohen-Mansfield Agitation Inventory (CMAI) and Behaviour Pathology in AD Rating Scale (BEHAVEAD) scores, particularly in the early stages of dementia, and that, even in severe cases of dementia, it improves circadian and behavioural symptoms, most notably agitation and overall cognitive function296,297. Care centres for patients with dementia are often dimly lit298–300, and a randomized control trial of 189 participants found that increasing illumination levels in elderly care centres during daytime hours leads to a slower decline in MMSE scores, reduced depression scores and reduced functional impairment in individuals with dementia over a 1.5-year period301. Moreover, a double-blind, multicentre study in 157 individuals with AD showed that evening melatonin treatment improved cognition, decreased nocturnal activity and increased sleep302. Importantly, melatonin treatment must be carefully timed to that of normal endogenous melatonin synthesis, as other studies that provided melatonin later in the evening did not find beneficial effects302,303.
Conclusions
Throughout the lifespan, sleep and circadian rhythm disruptions are strongly linked to the pathophysiology of specific psychiatric and neurodegenerative disorders. Though most clinical studies are still correlational, animal model studies are beginning to examine potential causal relationships between disrupted circadian rhythms and multiple brain disorders and are starting to identify molecular mechanisms. Although the central clock in the SCN seems to be key, circadian genes in other brain regions outside of this central pace-maker also contribute locally to the control of neuronal metabolism, neurotransmitter synthesis and activity, and the disruption of these functions might contribute to brain disorders264,304–315. We are only beginning to understand the role of peripheral oscillators in multiple regions of the brain, how they are entrained and what other functions circadian transcription factors have that might be independent of the control of daily rhythms. These points should certainly be the focus of future study.
We need to better understand the bidirectional relationships between circadian rhythms and environmental perturbations, such as stress or drugs of abuse, and how circadian rhythms are intimately connected to neurotransmission, metabolism, immunity and other processes. Circadian disruptions may promote vulnerability to or the progression of certain disorders, within a developmental context. With development, changes occur in the sensitivity of the brain to light input, in the inputs and outputs of the SCN, and in the functions of the molecular clock in specific cell types in the brain and in other tissues. In later life, certain disorders exhibit a defined trajectory, with sleep and circadian problems often preceding the development of other symptoms. These findings provide an opening for future, in-depth investigation of the causal relationships between sleep and/or circadian disruption and neurodegeneration.
Recent studies have demonstrated that elements of the molecular circadian clock directly regulate cellular metabolism and mitochondrial function in the liver and other tissues316–318. Further studies should determine the molecular mechanisms by which circadian genes may control the metabolism, mitochondrial function, redox state, antioxidant response and activity of neurons and glia, as dysfunction of each of these processes and states can contribute to neurodegeneration. In addition, future studies should determine the circadian rhythm of the expression of drug targets. For example, drugs that target certain neurotransmitters and their receptors may have higher therapeutic efficacy or more adverse effects depending on the time of day the medication is administered and on the endogenous rhythm of neurotransmission and receptor expression.
The evidence for associations between circadian disruptions and brain disorders in humans is mostly epidemiological and correlational. Studies in preclinical models have supported these findings while also offering insights into the bidirectionality, in which circadian disruption leads to certain disease-related phenotypes, and the environmental factors that can alter rhythms, such as stress or exposure to drugs of abuse, can lead to the exacerbation or progression of certain symptoms. Future research will require the continuation of experimental investigation of causality using translational approaches. For example, investigators are beginning to implement laboratory manipulations in humans to misalign the environmental schedule with an individual’s endogenous sleep–wake and melatonin rhythms to assess the impact of circadian alignment on cognitive, reward and memory functions, as well as their related neural circuits. Considering these hypotheses within a developmental context will be necessary, as certain developmental periods (for example, adolescence) may be vulnerable to these disruptions. Larger-scale, more in-depth assessments of chronotype utilizing novel biological assays319, combined with longitudinal follow-ups, could further clarify the predictive associations between eveningness or delayed chronotypes andbrain disorders such as depression, bipolar disorder and addiction. Recent genome-wide association studies with more than 100,000 subjects have identified novel loci associated with sleep duration, chronotype and metabolic phenotypes (for example, body mass index)320,321. The role of these environmental and genetic factors underlying circadian rhythms and brain disorders can be further experimentally interrogated using cell-based assays and preclinical models. Manipulation of specific circadian genes within neural cell types and regions will begin to dissect the involvement of molecular and cellular clocks in neural circuits and relevant physiological and behavioural end points. Optogenetic and chemogenetic tools can be used to tease apart the function of light-input pathways to the brain that are dependent on, or independent from, SCN connections in regulating neural activity, as has recently been demonstrated for mood-related behaviours322–324. With the advent of new tools and resources in neuroscience, and building on a greater understanding of the relationships between circadian rhythms, physiology and behaviour, research in humans and animals is equipped to investigate causal relationships between circadian disruption and various brain disorders. These findings may lead to effective therapeutics and interventions with improved clinical outcomes.
Chronotherapeutic strategies of specifically timing the delivery of certain drugs are now being used in the treatment of certain cancers325 and may be therapeutically beneficial across various diseases326. Time-restricted feeding is also now being used to help treat and/or prevent obesity, as well as metabolic, cardiac and liver disorders327,328. Several first-line pharmacological treatments for psychiatric disorders, such as lithium for bipolar disorder and SSRIs for major depressive disorders, modulate the circadian clock216,217,329–331. Although these effects were identified later, they suggest that targeting rhythms or components of the clock using pharmacological agents might be therapeutically beneficial215,216,331. Many of the most effective treatments for brain disorders and other diseases modulate clock function216,326,330,332,333. Importantly, treatments and interventions that target the circadian system may have therapeutic efficacy and improve clinical symptoms and daily functioning for the individual. Such approaches, if considered, could even be added as adjunct therapies to first-line medications or treatments to further improve therapeutic outcomes. There is much interest in the implementation of regular social, sleep and activity schedules in children and adolescents with developmental disorders, as stable environmental schedules seem to ameliorate daytime sleepiness and daytime behavioural problems in individuals with ASD or ADHD. The increased use of wearable activity and sleep-tracking devices has also brought about new possibilities in terms of diagnostic analysis and personalized treatment plans334. The field is poised to align multiple approaches, including tracking of brain function, receptor levels and internal rhythms, that could be valuable for treating psychiatric and neurological disorders in the future.
Peripheral oscillators.
Circadian ‘clocks’ in other parts of the brain and in peripheral organs that are driven by the suprachiasmatic nucleus and various other nonphotic cues and stimuli.
Actigraphy.
The monitoring of physical activity patterns (that is, rest–activity cycles) over many days, weeks or months, typically using non-invasive devices, such as wrist actometers.
Chronotype.
The preference for early or late activities (translating to morning or evening chronotypes, respectively) during the 24-hour cycle.
Sleep homeostasis.
A type of homeostasis by which prolonged periods of wakefulness lead to increases in the intensity and duration of subsequent sleep, in compensation for a sleep deficit or deprivation.
Melanopsin photoreceptors.
Opsin class g protein-coupled receptors expressed in a small percentage (~2%) of photosensitive mammalian retinal ganglion cells.
Bright light therapy.
A therapy for mood and sleep disorders that involves the use of bright light, typically in the morning, to shift and stabilize endogenous circadian timing.
Sleep efficiency.
A measure of the integrity of sleep architecture and quality of sleep, consisting of the ratio of total sleep time to the amount of time spent in bed.
Narcolepsy.
A chronic neurological disorder characterized by excessive daytime sleepiness, with many individuals experiencing intermittent, uncontrollable episodes of cataplexy (a sudden loss of muscle tone during wakefulness).
Amphetamine.
A potent stimulant drug that can be used in the treatment of attention-deficit hyperactivity disorder.
Methylphenidate.
A stimulant drug primarily used in the treatment of attention-deficit hyperactivity disorder.
Eveningness.
The preference for activity in the evening and later bed times, related to endogenous circadian phase, and akin to evening chronotype.
Frontostriatal reward circuitry.
Neural pathways that connect frontal regions with basal ganglia and mediate reward value and motivation.
Slow-wave activity.
An electrophysiological measure of slow (0.5–4 Hz), synchronized oscillatory activity primarily expressed during non-rapid eye movement sleep.
Delayed sleep phase syndrome.
A circadian rhythm disorder in which sleep timing is shifted later by 2 or more hours relative to normative sleep–wake cycles and often accompanied by similar shifts in body-temperature and hormone rhythms.
Acute sleep deprivation.
A partial night or full night of sleep restriction. This approach can produce a short-term antidepressant effect.
Interpersonal and social rhythm therapy.
A cognitive behavioural therapy often used for bipolar disorder that acts to stabilize sleep–wake and social schedules.
Dim light melatonin onset (DLMO).
A marker of endogenous circadian phase that can be used for research or to determine the appropriate timing of treatments.
Fatigue.
The feeling of exhaustion and lack of energy.
REM sleep behaviour disorder.
(RBD). A disorder in which there is a loss of the paralysis that normally occurs during rapid eye movement sleep, allowing the person to physically ‘act out’ their dreams.
Restless legs syndrome.
A condition marked by uncomfortable sensations in the legs accompanied by the urge to move them.
MitoPark transgenic mice.
A mouse model of Parkinson disease in which dopamine neurons are deficient in mitochondrial function through inactivation of mitochondrial transcription factor A.
REM sleep.
A phase of sleep characterized by rapid movement of the eyes, low muscle tone and dreams that can later be recollected.
Glymphatic system.
A functional waste clearance system in the brain that is active during sleep.
Astrocytosis.
An abnormal increase in the number of astrocytes, attributable to the death of nearby neurons.
Mini-Mental State Examination (MMSe).
A standardized set of 11 questions with a maximal score of 30 (≤23 indicating cognitive impairment) used to assess five cognitive functional areas: orientation, registration, attention and calculation, recall and language.
Acknowledgements
Figures were initially designed using BioRender software (biorender.io). Funding for the studies discussed from the authors’ group was obtained from NARSAD, International Mental Health Research Organization (IMHRO), MH106460, DA039865, DA037636, MH082876 and DA023988 to C.A.M. and from NARSAD, DA038654 and DA041872 to R.W.L.
Footnotes
Competing interests
The authors declare no competing interests.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reviewer information
Nature Reviews Neuroscience thanks A. Phillips, K. Wulff and the other anonymous reviewer(s) for their contribution to the peer review of this work.
References
- 1.Reppert SM & Weaver DR Coordination of circadian timing in mammals. Nature 418, 935–941 (2002). [DOI] [PubMed] [Google Scholar]
- 2.Colwell CS Linking neural activity and molecular oscillations in the SCN. Nat. Rev. Neurosci 12, 553–569 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Selemon LD A role for synaptic plasticity in the adolescent development of executive function. Transl Psychiatry 3, e238 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mighdoll MI, Tao R, Kleinman JE & Hyde TM Myelin, myelin-related disorders, and psychosis. Schizophr. Res 161, 85–93 (2015). [DOI] [PubMed] [Google Scholar]
- 5.Hsu PK, Ptacek LJ & Fu YH Genetics of human sleep behavioral phenotypes. Methods Enzymol 552, 309–324 (2015). [DOI] [PubMed] [Google Scholar]
- 6.Roenneberg T & Merrow M Entrainment of the human circadian clock. Cold Spring Harb. Symp. Quant. Biol 72, 293–299 (2007). [DOI] [PubMed] [Google Scholar]
- 7.Foster RG et al. Sleep and circadian rhythm disruption in social jetlag and mental illness. Prog. Mol. Biol. Transl Sci 119, 325–346 (2013). [DOI] [PubMed] [Google Scholar]
- 8.Werner H, Lebourgeois MK, Geiger A & Jenni OG Assessment of chronotype in four-to eleven-year-old children: reliability and validity of the Children’s Chronotype Questionnaire (CCTQ). Chronobiol. Int 26, 992–1014 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simpkin CT et al. Chronotype is associated with the timing of the circadian clock and sleep in toddlers. J. Sleep Res 23, 397–405 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crowley SJ et al. A longitudinal assessment of sleep timing, circadian phase, and phase angle of entrainment across human adolescence. PLOS ONE 9, e112199 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen CY et al. Effects of aging on circadian patterns of gene expression in the human prefrontal cortex. Proc. Natl Acad. Sci. USA 113, 206–211 (2015).This is the largest-scale study of circadian rhythms of gene expression in human post-mortem brain tissue, revealing age-related decline in the expression of core circadian genes and the emergence of other rhythmic pathways in older subjects.
- 12.Cornelissen G & Otsuka K Chronobiology of aging: a mini-review. Gerontology 63, 118–128 (2017). [DOI] [PubMed] [Google Scholar]
- 13.Drake CL, Roehrs T, Richardson G, Walsh JK & Roth T Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep 27, 1453–1462 (2004). [DOI] [PubMed] [Google Scholar]
- 14.Ramin C et al. Night shift work at specific age ranges and chronic disease risk factors. Occup. Environ. Med 72, 100–107 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bedrosian TA & Nelson RJ Timing of light exposure affects mood and brain circuits. Transl Psychiatry 7, e1017 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bedrosian TA & Nelson RJ Influence of the modern light environment on mood. Mol. Psychiatry 18, 751–757 (2013). [DOI] [PubMed] [Google Scholar]
- 17.Nakata A et al. Association of sickness absence with poor sleep and depressive symptoms in shift workers. Chronobiol. Int 21, 899–912 (2004). [DOI] [PubMed] [Google Scholar]
- 18.Roth T Shift work disorder: overview and diagnosis. J. Clin. Psychiatry 73, e09 (2012). [DOI] [PubMed] [Google Scholar]
- 19.Wright KP Jr, Bogan RK & Wyatt JK Shift work and the assessment and management of shift work disorder (SWD). Sleep Med. Rev 17, 41–54 (2012). [DOI] [PubMed] [Google Scholar]
- 20.Benca R et al. Biological rhythms, higher brain function, and behavior: gaps, opportunities, and challenges. Brain Res. Rev 62, 57–70 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poggiogalle E, Jamshed H & Peterson CM Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism 84, 11–27 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chaudhari A, Gupta R, Makwana K & Kondratov R Circadian clocks, diets and aging. Nutr. Healthy Aging 4, 101–112 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rivkees SA Developing circadian rhythmicity in infants. Pediatr. Endocrinol. Rev 1, 38–45 (2003). [PubMed] [Google Scholar]
- 24.Swaab DF Development of the human hypothalamus. Neurochem. Res 20, 509–519 (1995). [DOI] [PubMed] [Google Scholar]
- 25.VanDunk C, Hunter LA & Gray PA Development, maturation, and necessity of transcription factors in the mouse suprachiasmatic nucleus. J. Neurosci 31, 6457–6467 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reppert SM Pre-natal development of a hypothalamic biological clock. Progress Brain Res 93, 119–131; discussion 132 (1992). [DOI] [PubMed] [Google Scholar]
- 27.Reppert SM Interaction between the circadian clocks of mother and fetus. Ciba Found. Symp 183, 198–207; discussion 207–111 (1995). [DOI] [PubMed] [Google Scholar]
- 28.Reppert SM, Weaver DR & Rivkees SA Maternal communication of circadian phase to the developing mammal. Psychoneuroendocrinology 13, 63–78 (1988). [DOI] [PubMed] [Google Scholar]
- 29.Shearman LP, Zeitzer J & Weaver DR Widespread expression of functional D1-dopamine receptors in fetal rat brain. Brain Res. Dev. Brain Res 102, 105–115 (1997). [DOI] [PubMed] [Google Scholar]
- 30.Reiter RJ, Tan DX, Korkmaz A & Rosales-Corral SA Melatonin and stable circadian rhythms optimize maternal, placental and fetal physiology. Hum. Reprod. Update 20, 293–307 (2014). [DOI] [PubMed] [Google Scholar]
- 31.Okatani Y et al. Maternal–fetal transfer of melatonin in pregnant women near term. J. Pineal Res 25, 129–134 (1998). [DOI] [PubMed] [Google Scholar]
- 32.Schenker S et al. Antioxidant transport by the human placenta. Clin. Nutr 17, 159–167 (1998). [DOI] [PubMed] [Google Scholar]
- 33.Davis FC & Mannion J Entrainment of hamster pup circadian rhythms by prenatal melatonin injections to the mother. Am. J. Physiol 255, R439–R448 (1988). [DOI] [PubMed] [Google Scholar]
- 34.Seron-Ferre M et al. Circadian rhythms in the fetus. Mol. Cell. Endocrinol 349, 68–75 (2012). [DOI] [PubMed] [Google Scholar]
- 35.Seron-Ferre M, Riffo R, Valenzuela GJ & Germain AM Twenty-four-hour pattern of cortisol in the human fetus at term. Am. J. Obstet. Gynecol 184, 1278–1283 (2001). [DOI] [PubMed] [Google Scholar]
- 36.Kennaway DJ, Goble FC & Stamp GE Factors influencing the development of melatonin rhythmicity in humans. J. Clin. Endocrinol. Metab 81, 1525–1532 (1996). [DOI] [PubMed] [Google Scholar]
- 37.Bisanti L, Olsen J, Basso O, Thonneau P & Karmaus W Shift work and subfecundity: a European multicenter study. European Study Group on Infertility and Subfecundity. J. Occup. Environ. Med 38, 352–358 (1996). [DOI] [PubMed] [Google Scholar]
- 38.Aspholm R et al. Spontaneous abortions among Finnish flight attendants. J. Occup. Environ. Med 41, 486–491 (1999). [DOI] [PubMed] [Google Scholar]
- 39.Cone JE, Vaughan LM, Huete A & Samuels SJ Reproductive health outcomes among female flight attendants: an exploratory study. J. Occup. Environ. Med 40, 210–216 (1998). [DOI] [PubMed] [Google Scholar]
- 40.Mahoney MM Shift work, jet lag, and female reproduction. Int. J. Endocrinol 2010, 813764 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Varcoe TJ et al. Characterisation of the maternal response to chronic phase shifts during gestation in the rat: implications for fetal metabolic programming. PLOS ONE 8, e53800 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Torres-Farfan C et al. Maternal melatonin selectively inhibits cortisol production in the primate fetal adrenal gland. J. Physiol 554, 841–856 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Seron-Ferre M et al. Impact of chronodisruption during primate pregnancy on the maternal and newborn temperature rhythms. PLOS ONE 8, e57710 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Matsumoto T et al. Circadian myometrial and endocrine rhythms in the pregnant rhesus macaque: effects of constant light and timed melatonin infusion. Am. J. Obstet. Gynecol 165, 1777–1784 (1991). [DOI] [PubMed] [Google Scholar]
- 45.Novakova M, Sladek M & Sumova A Exposure of pregnant rats to restricted feeding schedule synchronizes the SCN clocks of their fetuses under constant light but not under a light-dark regime. J. Biol. Rhythms 25, 350–360 (2010). [DOI] [PubMed] [Google Scholar]
- 46.Vilches N et al. Gestational chronodisruption impairs hippocampal expression of NMDA receptor subunits Grin1b/Grin3a and spatial memory in the adult offspring. PLOS ONE 9, e91313 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Voiculescu SE et al. Behavioral and molecular effects of prenatal continuous light exposure in the adult rat. Brain Res 1650, 51–59 (2016). [DOI] [PubMed] [Google Scholar]
- 48.Smarr BL, Grant AD, Perez L, Zucker I & Kriegsfeld LJ Maternal and early-life circadian disruption have long-lasting negative consequences on offspring development and adult behavior in mice. Sci. Rep 7, 3326 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cisse YM, Russart KL & Nelson RJ Parental exposure to dim light at night prior to mating alters offspring adaptive immunity. Sci. Rep 7, 45497 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cisse YM, Russart KLG & Nelson RJ Depressive-like behavior is elevated among offspring of parents exposed to dim light at night prior to mating. Psychoneuroendocrinology 83, 182–186 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lunn RM et al. Health consequences of electric lighting practices in the modern world: a report on the National Toxicology Program’s workshop on shift work at night, artificial light at night, and circadian disruption. Sci. Total Environ 607–608, 1073–1084 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kennaway DJ, Stamp GE & Goble FC Development of melatonin production in infants and the impact of prematurity. J. Clin. Endocrinol. Metab 75, 367–369 (1992). [DOI] [PubMed] [Google Scholar]
- 53.Davis KF, Parker KP & Montgomery GL Sleep in infants and young children: part two: common sleep problems. J. Pediatr. Health Care 18, 130–137 (2004). [DOI] [PubMed] [Google Scholar]
- 54.Dahl RE Sleep, learning, and the developing brain: early-to-bed as a healthy and wise choice for school aged children. Sleep 28, 1498–1499 (2005). [PubMed] [Google Scholar]
- 55.Wolke D, Meyer R, Ohrt B & Riegel K Incidence and persistence of problems at sleep onset and sleep continuation in the preschool period: results of a prospective study of a representative sample in Bavaria [German]. Prax Kinderpsychol. Kinderpsychiatr 43, 331–339 (1994). [PubMed] [Google Scholar]
- 56.Gaylor EE, Burnham MM, Goodlin-Jones BL & Anders TF A longitudinal follow-up study of young children’s sleep patterns using a developmental classification system. Behav. Sleep Med 3, 44–61 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Touchette E et al. Associations between sleep duration patterns and behavioral/cognitive functioning at school entry. Sleep 30, 1213–1219 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kobayashi K et al. Poor toddler-age sleep schedules predict school-age behavioral disorders in a longitudinal survey. Brain Dev 37, 572–578 (2015). [DOI] [PubMed] [Google Scholar]
- 59.Gregory AM et al. Prospective longitudinal associations between persistent sleep problems in childhood and anxiety and depression disorders in adulthood. J. Abnorm. Child Psychol 33, 157–163 (2005). [DOI] [PubMed] [Google Scholar]
- 60.Gregory AM, Caspi A, Moffitt TE & Poulton R Sleep problems in childhood predict neuropsychological functioning in adolescence. Pediatrics 123, 1171–1176 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hysing M, Sivertsen B, Garthus-Niegel S & Eberhard-Gran M Pediatric sleep problems and social-emotional problems. A population-based study. Infant Behav. Dev 42, 111–118 (2016). [DOI] [PubMed] [Google Scholar]
- 62.Gregory AM, Eley TC, O’Connor TG & Plomin R Etiologies of associations between childhood sleep and behavioral problems in a large twin sample. J. Am. Acad. Child Adolesc. Psychiatry 43, 744–751 (2004). [DOI] [PubMed] [Google Scholar]
- 63.Bendova Z, Sumova A & Illnerova H Development of circadian rhythmicity and photoperiodic response in subdivisions of the rat suprachiasmatic nucleus. Brain Res. Dev. Brain Res 148, 105–112 (2004). [DOI] [PubMed] [Google Scholar]
- 64.Duncan MJ, Banister MJ & Reppert SM Developmental appearance of light–dark entrainment in the rat. Brain Res 369, 326–330 (1986). [DOI] [PubMed] [Google Scholar]
- 65.Fahrenkrug J, Nielsen HS & Hannibal J Expression of melanopsin during development of the rat retina. Neuroreport 15, 781–784 (2004). [DOI] [PubMed] [Google Scholar]
- 66.Gonzalez-Menendez I, Contreras F, Cernuda-Cernuda R & Garcia-Fernandez JM Daily rhythm of melanopsin-expressing cells in the mouse retina. Front. Cell Neurosci 3, 3 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Landgraf D, Koch CE & Oster H Embryonic development of circadian clocks in the mammalian suprachiasmatic nuclei. Front. Neuroanat 8, 143 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Leard LE, Macdonald ES, Heller HC & Kilduff TS Ontogeny of photic-induced c-fos mRNA expression in rat suprachiasmatic nuclei. Neuroreport 5, 2683–2687 (1994). [DOI] [PubMed] [Google Scholar]
- 69.Tarttelin EE et al. Expression of opsin genes early in ocular development of humans and mice. Exp. Eye Res 76, 393–396 (2003). [DOI] [PubMed] [Google Scholar]
- 70.Rivkees SA The development of circadian rhythms: from animals to Humans. Sleep Med. Clin 2, 331–341 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Guyer C et al. Very preterm infants show earlier emergence of 24-hour sleep-wake rhythms compared to term infants. Early Hum. Dev 91, 37–42 (2015). [DOI] [PubMed] [Google Scholar]
- 72.Boivin DB, Duffy JF, Kronauer RE & Czeisler CA Dose-response relationships for resetting of human circadian clock by light. Nature 379, 540–542 (1996). [DOI] [PubMed] [Google Scholar]
- 73.Rivkees SA, Hofman PL & Fortman J Newborn primate infants are entrained by low intensity lighting. Proc. Natl Acad. Sci. USA 94, 292–297 (1997). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shanahan TL & Czeisler CA Physiological effects of light on the human circadian pacemaker. Semin. Perinatol 24, 299–320 (2000). [DOI] [PubMed] [Google Scholar]
- 75.Watanabe S et al. Designing artificial environments for preterm infants based on circadian studies on pregnant uterus. Front. Endocrinol 4, 113 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Morag I & Ohlsson A Cycled light in the intensive care unit for preterm and low birth weight infants. Cochrane Database Syst. Rev 8, CD006982 (2013). [DOI] [PubMed] [Google Scholar]
- 77.Vasquez-Ruiz S et al. A light/dark cycle in the NICU accelerates body weight gain and shortens time to discharge in preterm infants. Early Hum. Dev 90, 535–540 (2014). [DOI] [PubMed] [Google Scholar]
- 78.Mirmira M. & Ariagn RL. Influence of light in the NICU on the development of circadian rhythms in preterm infants. Semin. Perinatol 24, 247–257 (2000). [DOI] [PubMed] [Google Scholar]
- 79.Boo NY, Chee SC & Rohana J Randomized controlled study of the effects of different durations of light exposure on weight gain by preterm infants in a neonatal intensive care unit. Acta Paediatr 91, 674–679 (2002). [DOI] [PubMed] [Google Scholar]
- 80.Brandon DH, Holditch-Davis D & Belyea M Preterm infants born at less than 31 weeks’ gestation have improved growth in cycled light compared with continuous near darkness. J. Pediatr 140, 192–199 (2002).This randomized intervention study reports that preterm infants (<31 weeks) receiving cycled light (11 hours on and 11 hours off, with 1 transition hour for shift changes) during hospital care (~4 weeks) gained weight faster than age-matched infants receiving near darkness.
- 81.Guyer C et al. Cycled light exposure reduces fussing and crying in very preterm infants. Pediatrics 130, e145–e151 (2012). [DOI] [PubMed] [Google Scholar]
- 82.Hao H & Rivkees SA The biological clock of very premature primate infants is responsive to light. Proc. Natl Acad. Sci. USA 96, 2426–2429 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lebel V, Aita M, Johnston C, Heon M & Dupuis F Effects of cycled lighting versus continuous near darkness on physiological stability and motor activity level in preterm infants. Adv. Neonatal Care 17, 282–291 (2017). [DOI] [PubMed] [Google Scholar]
- 84.Mann NP, Haddow R, Stokes L, Goodley S & Rutter N Effect of night and day on preterm infants in a newborn nursery: randomised trial. Br. Med. J. (Clin. Res. Ed.) 293, (1265–1267 (1986). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rivkees SA, Mayes L, Jacobs H & Gross I Rest-activity patterns of premature infants are regulated by cycled lighting. Pediatrics 113, 833–839 (2004). [DOI] [PubMed] [Google Scholar]
- 86.Philipsen A, Hornyak M & Riemann D Sleep and sleep disorders in adults with attention deficit/hyperactivity disorder. Sleep Med. Rev 10, 399–405 (2006). [DOI] [PubMed] [Google Scholar]
- 87.Coogan AN & McGowan NM A systematic review of circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. Atten. Defic. Hyperact. Disord 9, 129–147 (2017). [DOI] [PubMed] [Google Scholar]
- 88.Rybak YE, McNeely HE, Mackenzie BE, Jain UR & Levitan RD Seasonality and circadian preference in adult attention-deficit/hyperactivity disorder: clinical and neuropsychological correlates. Compr. Psychiatry 48, 562–571 (2007). [DOI] [PubMed] [Google Scholar]
- 89.Baird AL, Coogan AN, Siddiqui A, Donev RM & Thome J Adult attention-deficit hyperactivity disorder is associated with alterations in circadian rhythms at the behavioural, endocrine and molecular levels. Mol. Psychiatry 17, 988–995 (2012). [DOI] [PubMed] [Google Scholar]
- 90.Fargason RE et al. Correcting delayed circadian phase with bright light therapy predicts improvement in ADHD symptoms: a pilot study. J. Psychiatr. Res 91, 105–110 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Molina-Carballo A et al. Methylphenidate effects on blood serotonin and melatonin levels may help to synchronise biological rhythms in children with ADHD. J. Psychiatr. Res 47, 377–383 (2013). [DOI] [PubMed] [Google Scholar]
- 92.Wang SM et al. Modafinil for the treatment of attention-deficit/hyperactivity disorder: a meta-analysis. J. Psychiatr. Res 84, 292–300 (2017). [DOI] [PubMed] [Google Scholar]
- 93.Gerrard P & Malcolm R Mechanisms of modafinil: a review of current research. Neuropsychiatr. Dis. Treat 3, 349–364 (2007). [PMC free article] [PubMed] [Google Scholar]
- 94.Cortesi F, Giannotti F, Ivanenko A & Johnson K Sleep in children with autistic spectrum disorder. Sleep Med 11, 659–664 (2010). [DOI] [PubMed] [Google Scholar]
- 95.Richdale AL & Schreck KA Sleep problems in autism spectrum disorders: prevalence, nature, and possible biopsychosocial aetiologies. Sleep Med. Rev 13, 403–411 (2009). [DOI] [PubMed] [Google Scholar]
- 96.Giannotti F et al. An investigation of sleep characteristics, EEG abnormalities and epilepsy in developmentally regressed and non-regressed children with autism. J. Autism Dev. Disord 38, 1888–1897 (2008). [DOI] [PubMed] [Google Scholar]
- 97.Takase M, Taira M & Sasaki H Sleep–wake rhythm of autistic children. Psychiatry Clin. Neurosci 52, 181–182 (1998). [DOI] [PubMed] [Google Scholar]
- 98.Hayashi E Seasonal changes in sleep and behavioral problems in a pubescent case with autism. Psychiatry Clin. Neurosci 55, 223–224 (2001). [DOI] [PubMed] [Google Scholar]
- 99.Tordjman S, Anderson GM, Pichard N, Charbuy H & Touitou Y Nocturnal excretion of 6-sulphatoxymelatonin in children and adolescents with autistic disorder. Biol. Psychiatry 57, 134–138 (2005). [DOI] [PubMed] [Google Scholar]
- 100.Nir I et al. Brief report: circadian melatonin, thyroid-stimulating hormone, prolactin, and cortisol levels in serum of young adults with autism. J. Autism Dev. Disord 25, 641–654 (1995). [DOI] [PubMed] [Google Scholar]
- 101.Kulman G et al. Evidence of pineal endocrine hypofunction in autistic children. Neuro Endocrinol. Lett 21, 31–34 (2000). [PubMed] [Google Scholar]
- 102.Melke J et al. Abnormal melatonin synthesis in autism spectrum disorders. Mol. Psychiatry 13, 90–98 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Simonneaux V & Ribelayga C Generation of the melatonin endocrine message in mammals: a review of the complex regulation of melatonin synthesis by norepinephrine, peptides, and other pineal transmitters. Pharmacol. Rev 55, 325–395 (2003). [DOI] [PubMed] [Google Scholar]
- 104.Jin Y, Choi J, Won J & Hong Y The relationship between autism spectrum disorder and melatonin during fetal development. Molecules 23, E198 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gringras P, Nir T, Breddy J, Frydman-Marom A & Findling RL Efficacy and safety of pediatric prolonged-release melatonin for insomnia in children with autism spectrum disorder. J. Am. Acad. Child Adolesc. Psychiatry 56, 948–957 (2017). [DOI] [PubMed] [Google Scholar]
- 106.Tordjman S et al. Autism as a disorder of biological and behavioral rhythms: toward new therapeutic perspectives. Front. Pediatr 3, 1 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Hoel EP, Albantakis L, Cirelli C & Tononi G Synaptic refinement during development and its effect on slow-wave activity: a computational study. J. Neurophysiol 115, 2199–2213 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Goldstone A et al. The mediating role of cortical thickness and gray matter volume on sleep slow-wave activity during adolescence. Brain Struct. Funct 223, 669–685 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cassidy SB, Schwartz S, Miller JL & Driscoll DJ Prader–Willi syndrome. Genet. Med 14, 10–26 (2012). [DOI] [PubMed] [Google Scholar]
- 110.Sahoo T et al. Prader–Willi phenotype caused by paternal deficiency for the HBII-85C/D box small nucleolar RNA cluster. Nat. Genet 40, 719–721 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lassi G et al. Deletion of the Snord116/SNORD116 alters sleep in mice and patients with Prader–Willi syndrome. Sleep 39, 637–644 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Butler JV et al. Prevalence of, and risk factors for, physical ill-health in people with Prader–Willi syndrome: a population-based study. Dev. Med. Child Neurol 44, 248–255 (2002). [DOI] [PubMed] [Google Scholar]
- 113.Cavaille J et al. Identification of brain-specific and imprinted small nucleolar RNA genes exhibiting an unusual genomic organization. Proc. Natl Acad. Sci. USA 97, 14311–14316 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Galiveti CR, Raabe CA, Konthur Z & Rozhdestvensky TS Differential regulation of non-protein coding RNAs from Prader–Willi syndrome locus. Sci. Rep 4, 6445 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Runte M et al. The IC-SNURF-SNRPN transcript serves as a host for multiple small nucleolar RNA species and as an antisense RNA for UBE3A. Hum. Mol. Genet 10, 2687–2700 (2001). [DOI] [PubMed] [Google Scholar]
- 116.Powell WT et al. A Prader–Willi locus lncRNA cloud modulates diurnal genes and energy expenditure. Hum. Mol. Genet 22, 4318–4328 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Gossan NC et al. The E3 ubiquitin ligase UBE3A is an integral component of the molecular circadian clock through regulating the BMAL1 transcription factor. Nucleic Acids Res 42, 5765–5775 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Solter D Differential imprinting and expression of maternal and paternal genomes. Annu. Rev. Genet 22, 127–146 (1988). [DOI] [PubMed] [Google Scholar]
- 119.Martins-Taylor K et al. Imprinted expression of UBE3A in non-neuronal cells from a Prader–Willi syndrome patient with an atypical deletion. Hum. Mol. Genet 23, 2364–2373 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Rougeulle C, Glatt H & Lalande M The Angelman syndrome candidate gene, UBE3A/E6-AP, is imprinted in brain. Nat. Genet 17, 14–15 (1997). [DOI] [PubMed] [Google Scholar]
- 121.Baron CA et al. Genomic and functional profiling of duplicated chromosome 15 cell lines reveal regulatory alterations in UBE3A-associated ubiquitin-proteasome pathway processes. Hum. Mol. Genet 15, 853–869 (2006). [DOI] [PubMed] [Google Scholar]
- 122.Herzing LB, Cook EH Jr & Ledbetter DH Allele-specific expression analysis by RNA-FISH demonstrates preferential maternal expression of UBE3A and imprint maintenance within 15q11-q13 duplications. Hum. Mol. Genet 11, 1707–1718 (2002). [DOI] [PubMed] [Google Scholar]
- 123.Hogart A et al. Chromosome 15q11–13 duplication syndrome brain reveals epigenetic alterations in gene expression not predicted from copy number. J. Med. Genet 46, 86–93 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nishimura Y et al. Genome-wide expression profiling of lymphoblastoid cell lines distinguishes different forms of autism and reveals shared pathways. Hum. Mol. Genet 16, 1682–1698 (2007). [DOI] [PubMed] [Google Scholar]
- 125.Dindot SV, Antalffy BA, Bhattacharjee MB & Beaudet AL The Angelman syndrome ubiquitin ligase localizes to the synapse and nucleus, and maternal deficiency results in abnormal dendritic spine morphology. Hum. Mol. Genet 17, 111–118 (2008). [DOI] [PubMed] [Google Scholar]
- 126.Yamasaki K et al. Neurons but not glial cells show reciprocal imprinting of sense and antisense transcripts of Ube3a. Hum. Mol. Genet 12, 837–847 (2003). [DOI] [PubMed] [Google Scholar]
- 127.Shi SQ, Bichell TJ, Ihrie RA & Johnson CH Ube3a imprinting impairs circadian robustness in Angelman syndrome models. Curr. Biol 25, 537–545 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Boudreau EA et al. Review of disrupted sleep patterns in Smith–Magenis syndrome and normal melatonin secretion in a patient with an atypical interstitial 17p11.2 deletion. Am. J. Med. Genet A 149A, 1382–1391 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Greenberg F et al. Multi-disciplinary clinical study of Smith–Magenis syndrome (deletion 17p11.2). Am. J. Med. Genet 62, 247–254 (1996). [DOI] [PubMed] [Google Scholar]
- 130.Gropman AL, Elsea S, Duncan WC Jr & Smith AC New developments in Smith–Magenis syndrome (del 17p11.2). Curr. Opin. Neurol 20, 125–134 (2007). [DOI] [PubMed] [Google Scholar]
- 131.Smith AC, Dykens E & Greenberg F Sleep disturbance in Smith–Magenis syndrome (del 17p11.2). Am. J. Med. Genet 81, 186–191 (1998). [PubMed] [Google Scholar]
- 132.Boone PM et al. Abnormal circadian rhythm of melatonin in Smith–Magenis syndrome patients with RAI1 point mutations. Am. J. Med. Genet. A 155A, 2024–2027 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Walz K et al. Behavioral characterization of mouse models for Smith–Magenis syndrome and dup(17) (p11.2p11.2). Hum. Mol. Genet 13, 367–378 (2004). [DOI] [PubMed] [Google Scholar]
- 134.Lacaria M, Gu W & Lupski JR Circadian abnormalities in mouse models of Smith–Magenis syndrome: evidence for involvement of RAI1. Am. J. Med. Genet. A 161A, 1561–1568 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Williams SR, Zies D, Mullegama SV, Grotewiel MS & Elsea SH Smith–Magenis syndrome results in disruption of CLOCK gene transcription and reveals an integral role for RAI1 in the maintenance of circadian rhythmicity. Am. J. Hum. Genet 90, 941–949 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.De Leersnyder H et al. β1-adrenergic antagonists improve sleep and behavioural disturbances in a circadian disorder, Smith–Magenis syndrome. J. Med. Genet 38, 586–590 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.De Leersnyder H et al. β1-adrenergic antagonists and melatonin reset the clock and restore sleep in a circadian disorder, Smith–Magenis syndrome. J. Med. Genet 40, 74–78 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.De Leersnyder H, Claustrat B, Munnich A & Verloes A Circadian rhythm disorder in a rare disease: Smith–Magenis syndrome. Mol. Cell Endocrinol 252, 88–91 (2006). [DOI] [PubMed] [Google Scholar]
- 139.Elsea SH & Girirajan S Smith–Magenis syndrome. Eur. J. Hum. Genet 16, 412–421 (2008). [DOI] [PubMed] [Google Scholar]
- 140.Logan RW et al. Impact of sleep and circadian rhythms on addiction vulnerability in adolescents. Biol. Psychiatry 83, 987–996 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Roenneberg T et al. A marker for the end of adolescence. Curr. Biol 14, R1038–R1039 (2004). [DOI] [PubMed] [Google Scholar]
- 142.Hagenauer MH & Lee TM The neuroendocrine control of the circadian system: adolescent chronotype. Front. Neuroendocrinol 33, 211–229 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Hagenauer MH & Lee TM Adolescent sleep patterns in humans and laboratory animals. Horm. Behav 64, 270–279 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Cain N & Gradisar M Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med 11, 735–742 (2010). [DOI] [PubMed] [Google Scholar]
- 145.Crowley SJ, Cain SW, Burns AC, Acebo C & Carskadon MA Increased sensitivity of the circadian system to light in early/mid-puberty. J. Clin. Endocrinol. Metab 100, 4067–4073 (2015).This study shows that endogenous melatonin levels of prepubertal children and early adolescents are more sensitive to the suppressive effects of acute light exposure during the evening than melatonin levels in late adolescents.
- 146.Paruthi S et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J. Clin. Sleep Med 12, 785–786 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Basch CE, Basch CH, Ruggles KV & Rajan S Prevalence of sleep duration on an average school night among 4 nationally representative successive samples of American high school students, 2007–2013. Prev. Chron. Dis 11, E216 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Touitou Y Adolescent sleep misalignment: a chronic jet lag and a matter of public health. J. Physiol. Paris 107, 323–326 (2013). [DOI] [PubMed] [Google Scholar]
- 149.Hasler BP et al. Weekend-weekday advances in sleep timing are associated with altered reward-related brain function in healthy adolescents. Biol. Psychol 91, 334–341 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Skeldon AC, Phillips AJ & Dijk DJ The effects of self-selected light–dark cycles and social constraints on human sleep and circadian timing: a modeling approach. Sci. Rep 7, 45158 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Crowley SJ & Carskadon MA Modifications to weekend recovery sleep delay circadian phase in older adolescents. Chronobiol. Int 27, 1469–1492 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wittmann M, Dinich J, Merrow M & Roenneberg T Social jetlag: misalignment of biological and social time. Chronobiol. Int 23, 497–509 (2006). [DOI] [PubMed] [Google Scholar]
- 153.Chen K & Kandel DB The natural history of drug use from adolescence to the mid-thirties in a general population sample. Am. J. Publ. Health 85, 41–47 (1995). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Falcon E & McClung CA A role for the circadian genes in drug addiction. Neuropharmacology 56, 91–96 (2009). (Suppl. 1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.O’Brien EM & Mindell JA Sleep and risk-taking behavior in adolescents. Behav. Sleep Med 3, 113–133 (2005). [DOI] [PubMed] [Google Scholar]
- 156.Pasch KE, Laska MN, Lytle LA & Moe SG Adolescent sleep, risk behaviors, and depressive symptoms: are they linked? Am. J. Health Behav 34, 237–248 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.McKnight-Eily LR et al. Relationships between hours of sleep and health-risk behaviors in US adolescent students. Prev. Med 53, 271–273 (2011). [DOI] [PubMed] [Google Scholar]
- 158.Paiva T, Gaspar T & Matos MG Mutual relations between sleep deprivation, sleep stealers and risk behaviours in adolescents. Sleep Sci 9, 7–13 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Sivertsen B, Skogen JC, Jakobsen R & Hysing M Sleep and use of alcohol and drug in adolescence. A large population-based study of Norwegian adolescents aged 16 to 19 years. Drug Alcohol Depend 149, 180–186 (2015). [DOI] [PubMed] [Google Scholar]
- 160.Thomas AG, Monahan KC, Lukowski AF & Cauffman E Sleep problems across development: a pathway to adolescent risk taking through working memory. J. Youth Adolesc 44, 447–464 (2015). [DOI] [PubMed] [Google Scholar]
- 161.Wheaton AG, Olsen EO, Miller GF & Croft JB Sleep duration and injury-related risk behaviors among high school students — United States, 2007–2013. MMWR Morb. Mortal. Wkly Rep 65, 337–341 (2016). [DOI] [PubMed] [Google Scholar]
- 162.Pasch KE, Latimer LA, Cance JD, Moe SG & Lytle LA Longitudinal bidirectional relationships between sleep and youth substance use. J. Youth Adolesc 41, 1184–1196 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Hasler BP, Martin CS, Wood DS, Rosario B & Clark DB A longitudinal study of insomnia and other sleep complaints in adolescents with and without alcohol use disorders. Alcohol Clin. Exp. Res 38, 2225–2233 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hasler BP, Kirisci L & Clark DB Restless sleep and variable sleep timing during late childhood accelerate the onset of alcohol and other drug involvement. J. Stud. Alcohol Drugs 77, 649–655 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Hasler BP, Soehner AM & Clark DB Sleep and circadian contributions to adolescent alcohol use disorder. Alcohol 49, 377–387 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Tavernier R, Munroe M & Willoughby T Perceived morningness-eveningness predicts academic adjustment and substance use across university, but social jetlag is not to blame. Chronobiol. Int 32, 1233–1245 (2015). [DOI] [PubMed] [Google Scholar]
- 167.Hasler BP, Casement MD, Sitnick SL, Shaw DS & Forbes EE Eveningness among late adolescent males predicts neural reactivity to reward and alcohol dependence two years later. Behav. Brain Res 327, 112–120 (2017).This study shows that an evening chronotype during late adolescence (20 years of age) is associated with strength of activation in the VS to reward outcome, which was positively correlated with alcohol dependence 2 years later.
- 168.Mednick SC, Christakis NA & Fowler JH The spread of sleep loss influences drug use in adolescent social networks. PLOS ONE 5, e9775 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Forbes EE et al. Healthy adolescents’ neural response to reward: associations with puberty, positive affect, and depressive symptoms. J. Am. Acad. Child Adolesc. Psychiatry 49, 162–172 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Padmanabhan A, Geier CF, Ordaz SJ, Teslovich T & Luna B Developmental changes in brain function underlying the influence of reward processing on inhibitory control. Dev. Cogn. Neurosci 1, 517–529 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Frischknecht R & Gundelfinger ED The brain’s extracellular matrix and its role in synaptic plasticity. Adv. Exp. Med. Biol 970, 153–171 (2012). [DOI] [PubMed] [Google Scholar]
- 172.Luciana M & Collins PF Incentive motivation, cognitive control, and the adolescent brain: is it time for a paradigm shift? Child Dev. Perspect 6, 392–399 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Padmanabhan A & Luna B Developmental imaging genetics: linking dopamine function to adolescent behavior. Brain Cogn 89, 27–38 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ernst M & Fudge JL A developmental neurobiological model of motivated behavior: anatomy, connectivity and ontogeny of the triadic nodes. Neurosci. Biobehav. Rev 33, 367–382 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Somerville LH, Jones RM & Casey BJ A time of change: behavioral and neural correlates of adolescent sensitivity to appetitive and aversive environmental cues. Brain Cogn 72, 124–133 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Logan RW, Williams WP & McClung CA Circadian rhythms and addiction: mechanistic insights and future directions. Behav. Neurosci 128, 387–412 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hasler BP, Forbes EE & Franzen PL Time-of-day differences and short-term stability of the neural response to monetary reward: a pilot study. Psychiatry Res 224, 22–27 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Hasler BP et al. Chronotype and diurnal patterns of positive affect and affective neural circuitry in primary insomnia. J. Sleep Res 21, 515–526 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Hasler BP, Sitnick SL, Shaw DS & Forbes EE An altered neural response to reward may contribute to alcohol problems among late adolescents with an evening chronotype. Psychiatry Res 214, 357–364 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Mullin BC et al. Sleep deprivation amplifies striatal activation to monetary reward. Psychol. Med 43, 2215–2225 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Miller MB, Donahue ML, Carey KB & Scott-Sheldon LAJ Insomnia treatment in the context of alcohol use disorder: a systematic review and meta-analysis. Drug Alcohol Depend 181, 200–207 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Merikangas KR et al. Lifetime prevalence of mental disorders in U. S. adolescents: results from the National Comorbidity Survey Replication — Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 49, 980–989 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lamont EW, Coutu DL, Cermakian N & Boivin DB Circadian rhythms and clock genes in psychotic disorders. Isr. J. Psychiatry Relat. Sci 47, 27–35 (2010). [PubMed] [Google Scholar]
- 184.McClung CA How might circadian rhythms control mood? Let me count the ways. Biol. Psychiatry 74, 242–249 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Mansour HA et al. Circadian phase variation in bipolar I disorder. Chronobiol. Int 22, 571–584 (2005). [DOI] [PubMed] [Google Scholar]
- 186.McCarthy MJ & Welsh DK Cellular circadian clocks in mood disorders. J. Biol. Rhythms 27, 339–352 (2012). [DOI] [PubMed] [Google Scholar]
- 187.McClung CA Circadian rhythms and mood regulation: insights from pre-clinical models. Eur. Neuropsychopharmacol 21, S683–S693 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Wulff K, Dijk DJ, Middleton B, Foster RG & Joyce EM Sleep and circadian rhythm disruption in schizophrenia. Br. J. Psychiatry 200, 308–316 (2012).This study reports notable circadian misalignment (phase delays and advances) of sleep–wake cycles and melatonin rhythms in patients with schizophrenia despite other factors, including mood, cognitive status and pharmacological treatments.
- 189.Frank E, Swartz HA & Kupfer DJ Interpersonal and social rhythm therapy: managing the chaos of bipolar disorder. Biol. Psychiatry 48, 593–604 (2000). [DOI] [PubMed] [Google Scholar]
- 190.Malkoff-Schwartz S et al. Stressful life events and social rhythm disruption in the onset of manic and depressive bipolar episodes: a preliminary investigation. Arch. Gen. Psychiatry 55, 702–707 (1998). [DOI] [PubMed] [Google Scholar]
- 191.Melo MCA, Abreu RLC, Linhares Neto VB, de Bruin PFC & de Bruin VMS Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med. Rev 34, 46–58 (2017). [DOI] [PubMed] [Google Scholar]
- 192.Winthorst WH et al. Seasonal affective disorder and non-seasonal affective disorders: results from the NESDA study. BJPsych Open 3, 196–203 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Medici CR, Vestergaard CH, Hadzi-Pavlovic D, Munk-Jorgensen P & Parker G Seasonal variations in hospital admissions for mania: examining for associations with weather variables over time. J. Affect. Disord 205, 81–86 (2016). [DOI] [PubMed] [Google Scholar]
- 194.Young JW & Dulcis D Investigating the mechanism(s) underlying switching between states in bipolar disorder. Eur. J. Pharmacol 759, 151–162 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Raniti MB et al. Sleep duration and sleep quality: associations with depressive symptoms across adolescence. Behav. Sleep Med 15, 198–215 (2017). [DOI] [PubMed] [Google Scholar]
- 196.Lewy AJ Depressive disorders may more commonly be related to circadian phase delays rather than advances: time will tell. Sleep Med 11, 117–118 (2010). [DOI] [PubMed] [Google Scholar]
- 197.Addington J & Heinssen R Prediction and prevention of psychosis in youth at clinical high risk. Annu. Rev. Clin. Psychol 8, 269–289 (2012). [DOI] [PubMed] [Google Scholar]
- 198.Lunsford-Avery JR et al. Adolescents at clinical-high risk for psychosis: circadian rhythm disturbances predict worsened prognosis at 1-year follow-up. Schizophr. Res 189, 37–42 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Robillard R et al. Sleep–wake profiles predict longitudinal changes in manic symptoms and memory in young people with mood disorders. J. Sleep Res 25, 549–555 (2016). [DOI] [PubMed] [Google Scholar]
- 200.Crews FT, Vetreno RP, Broadwater MA & Robinson DL Adolescent alcohol exposure persistently impacts adult neurobiology and behavior. Pharmacol. Rev 68, 1074–1109 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Wei Y, Krishnan GP & Bazhenov M Synaptic mechanisms of memory consolidation during sleep slow oscillations. J. Neurosci 36, 4231–4247 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Walker MP & Stickgold R Sleep-dependent learning and memory consolidation. Neuron 44, 121–133 (2004). [DOI] [PubMed] [Google Scholar]
- 203.Havekes R, Meerlo P & Abel T Animal studies on the role of sleep in memory: from behavioral performance to molecular mechanisms. Curr. Top. Behav. Neurosci 25, 183–206 (2015). [DOI] [PubMed] [Google Scholar]
- 204.Marshall L, Helgadottir H, Molle M & Born J Boosting slow oscillations during sleep potentiates memory. Nature 444, 610–613 (2006).This study establishes the importance of slow-wave sleep during non-REM episodes that occur during the early night and shows that it promotes the retention of hippocampus-dependent declarative memories.
- 205.Selemon LD & Zecevic N Schizophrenia: a tale of two critical periods for prefrontal cortical development. Transl Psychiatry 5, e623 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Keshavan MS, Anderson S & Pettegrew JW Is schizophrenia due to excessive synaptic pruning in the prefrontal cortex? The Feinberg hypothesis revisited. J. Psychiatr. Res 28, 239–265 (1994). [DOI] [PubMed] [Google Scholar]
- 207.Billeh YN et al. Effects of chronic sleep restriction during early adolescence on the adult pattern of connectivity of mouse secondary motor cortex. eNeuro 10.1523/ENEURO.0053-16-2016 (2016). [DOI] [PMC free article] [PubMed]
- 208.Carskadon MA Patterns of sleep and sleepiness in adolescents. Pediatrician 17, 5–12 (1990). [PubMed] [Google Scholar]
- 209.Johnson EO, Roth T, Schultz L & Breslau N Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics 117, e247–e256 (2006). [DOI] [PubMed] [Google Scholar]
- 210.Sivertsen B et al. Delayed sleep phase syndrome in adolescents: prevalence and correlates in a large population based study. BMC Publ. Health 13, 1163 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Owens JA, Belon K & Moss P Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch. Pediatr. Adolesc. Med 164, 608–614 (2010). [DOI] [PubMed] [Google Scholar]
- 212.Wirz-Justice A & Terman M Chronotherapeutics (light and wake therapy) as a class of interventions for affective disorders. Handb. Clin. Neurol 106, 697–713 (2012). [DOI] [PubMed] [Google Scholar]
- 213.Srinivasan V, De Berardis D, Shillcutt SD & Brzezinski A Role of melatonin in mood disorders and the antidepressant effects of agomelatine. Expert Opin. Investig. Drugs 21, 1503–1522 (2012). [DOI] [PubMed] [Google Scholar]
- 214.Wu JC et al. Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol. Psychiatry 66, 298–301 (2009).This study demonstrates, in a cohort of 49 patients with bipolar disorder, the ability of non-invasive circadian therapy (that is, bright light therapy and sleep phase advance) and sleep (that is, acute sleep deprivation) to improve and sustain the therapeutic efficacy of lithium and antidepressants on mood symptoms.
- 215.Li J, Lu WQ, Beesley S, Loudon AS & Meng QJ Lithium impacts on the amplitude and period of the molecular circadian clockwork. PLOS ONE 7, e33292 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Johansson AS, Brask J, Owe-Larsson B, Hetta J & Lundkvist GB Valproic acid phase shifts the rhythmic expression of Period2::Luciferase. J. Biol. Rhythms 26, 541–551 (2011). [DOI] [PubMed] [Google Scholar]
- 217.Sprouse J, Braselton J & Reynolds L Fluoxetine modulates the circadian biological clock via phase advances of suprachiasmatic nucleus neuronal firing. Biol. Psychiatry 60, 896–899 (2006). [DOI] [PubMed] [Google Scholar]
- 218.Duncan WC Jr et al. Motor-activity markers of circadian timekeeping are related to ketamine’s rapid antidepressant properties. Biol. Psychiatry 82, 361–369 (2017).In a study of 51 patients with major depressive disorder or bipolar disorder, circadian activity patterns prior to and following the administration of ketamine are linked to therapeutic response of mood symptoms.
- 219.Kragh M et al. Predictors of response to combined wake and light therapy in treatment-resistant inpatients with depression. Chronobiol. Int 10.1080/07420528.2018.1468341 (2018). [DOI] [PubMed]
- 220.Adan A & Natale V Gender differences in morningness–eveningness preference. Chronobiol. Int 19, 709–720 (2002). [DOI] [PubMed] [Google Scholar]
- 221.Caci H, Deschaux O, Adan A & Natale V Comparing three morningness scales: age and gender effects, structure and cut-off criteria. Sleep Med 10, 240–245 (2009). [DOI] [PubMed] [Google Scholar]
- 222.Duarte LL et al. Chronotype ontogeny related to gender. Braz. J. Med. Biol. Res 47, 316–320 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Paine SJ, Gander PH & Travier N The epidemiology of morningness/eveningness: influence of age, gender, ethnicity, and socioeconomic factors in adults (30–49 years). J. Biol. Rhythms 21, 68–76 (2006). [DOI] [PubMed] [Google Scholar]
- 224.Patke A et al. Mutation of the human circadian clock gene CRY1 in familial delayed sleep phase disorder. Cell 169, 203–215 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Kripke DF et al. Circadian polymorphisms in night owls, in bipolars, and in non-24-hour sleep cycles. Psychiatry Invest 11, 345–362 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Murray JM et al. Prevalence of circadian misalignment and its association with depressive symptoms in delayed sleep phase disorder. Sleep 40, zsw002 (2017). [DOI] [PubMed] [Google Scholar]
- 227.James SM, Honn KA, Gaddameedhi S & Van Dongen HPA Shift work: disrupted circadian rhythms and sleep-implications for health and well-being. Curr. Sleep Med. Rep 3, 104–112 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Hall AL, Franche RL & Koehoorn M Examining exposure assessment in shift work research: a study on depression among nurses. Ann. Work Expo. Health 62, 182–194 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Kang MY, Kwon HJ, Choi KH, Kang CW & Kim H The relationship between shift work and mental health among electronics workers in South Korea: a cross-sectional study. PLOS ONE 12, e0188019 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.McNeely E et al. The self-reported health of U. S. flight attendants compared to the general population. Environ. Health 13, 13 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.McNeely E et al. Cancer prevalence among flight attendants compared to the general population. Environ. Health 17, 49 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Grajewski B, Whelan EA, Nguyen MM, Kwan L & Cole RJ Sleep disturbance in female flight attendants and teachers. Aerosp. Med. Hum. Perform 87, 638–645 (2016). [DOI] [PubMed] [Google Scholar]
- 233.McNeely E, Mordukhovich I, Tideman S, Gale S & Coull B Estimating the health consequences of flight attendant work: comparing flight attendant health to the general population in a cross-sectional study. BMC Publ. Health 18, 346 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Feinsilver SH & Hernandez AB Sleep in the elderly: unanswered questions. Clin. Geriatr. Med 33, 579–596 (2017). [DOI] [PubMed] [Google Scholar]
- 235.Mattis J & Sehgal A Circadian rhythms, sleep, and disorders of aging. Trends Endocrinol. Metab 27, 192–203 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Musiek ES & Holtzman DM Mechanisms linking circadian clocks, sleep, and neurodegeneration. Science 354, 1004–1008 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Karasek M Melatonin, human aging, and age-related diseases. Exp. Gerontol 39, 1723–1729 (2004). [DOI] [PubMed] [Google Scholar]
- 238.Zeitzer JM et al. Do plasma melatonin concentrations decline with age? Am. J. Med 107, 432–436 (1999). [DOI] [PubMed] [Google Scholar]
- 239.Czeisler CA et al. Association of sleep–wake habits in older people with changes in output of circadian pacemaker. Lancet 340, 933–936 (1992).This landmark study suggests that changes in sleep timing and consolidation driven by the circadian system underlie sleep disturbances in elderly individuals.
- 240.Wang JL et al. Suprachiasmatic neuron numbers and rest–activity circadian rhythms in older humans. Ann. Neurol 78, 317–322 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Chang HC & Guarente L SIRT1 mediates central circadian control in the SCN by a mechanism that decays with aging. Cell 153, 1448–1460 (2013).This mouse study reveals that reductions of sirtuin activity in the SCN leads to a gradual age-dependent dampening of SCN activity and locomotor rhythms.
- 242.Yamazaki S et al. Effects of aging on central and peripheral mammalian clocks. Proc. Natl Acad. Sci. USA 99, 10801–10806 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Swaab DF, Fliers E & Partiman TS The suprachiasmatic nucleus of the human brain in relation to sex, age and senile dementia. Brain Res 342, 37–44 (1985). [DOI] [PubMed] [Google Scholar]
- 244.Zhou JN, Hofman MA & Swaab DF VIP neurons in the human SCN in relation to sex, age, and Alzheimer’s disease. Neurobiol. Aging 16, 571–576 (1995). [DOI] [PubMed] [Google Scholar]
- 245.Roozendaal B, van Gool WA, Swaab DF, Hoogendijk JE & Mirmiran M Changes in vasopressin cells of the rat suprachiasmatic nucleus with aging. Brain Res 409, 259–264 (1987). [DOI] [PubMed] [Google Scholar]
- 246.Tsukahara S, Tanaka S, Ishida K, Hoshi N & Kitagawa H Age-related change and its sex differences in histoarchitecture of the hypothalamic suprachiasmatic nucleus of F344/N rats. Exp. Gerontol 40, 147–155 (2005). [DOI] [PubMed] [Google Scholar]
- 247.Nygard M, Hill RH, Wikstrom MA & Kristensson K Age-related changes in electro-physiological properties of the mouse suprachiasmatic nucleus in vitro. Brain Res. Bull 65, 149–154 (2005). [DOI] [PubMed] [Google Scholar]
- 248.Farajnia S et al. Evidence for neuronal desynchrony in the aged suprachiasmatic nucleus clock. J. Neurosci 32, 5891–5899 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Nakamura TJ et al. Age-related decline in circadian output. J. Neurosci 31, 10201–10205 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Tranah GJ et al. Circadian activity rhythms and risk of incident dementia and mild cognitive impairment in older women. Ann. Neurol 70, 722–732 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Chen HF, Huang CQ, You C, Wang ZR & Si-qing H Polymorphism of CLOCK geners 4580704C>G is associated with susceptibility of Alzheimer’s disease in a Chinese population. Arch. Med. Res 44, 203–207 (2013). [DOI] [PubMed] [Google Scholar]
- 252.Chen Q, Peng XD, Huang CQ, Hu XY & Zhang XM Association between ARNTL (BMAL1) rs2278749 polymorphism T>C and susceptibility to Alzheimer disease in a Chinese population. Genet. Mol. Res 14, 18515–18522 (2015). [DOI] [PubMed] [Google Scholar]
- 253.Gu Z et al. Association of ARNTL and PER1 genes with Parkinson’s disease: a case-control study of Han Chinese. Sci. Rep 5, 15891 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Videnovic A & Golombek D Circadian dysregulation in Parkinson’s disease. Neurobiol. Sleep Circadian Rhythms 2, 53–58 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Breen DP et al. Sleep and circadian rhythm regulation in early Parkinson disease. JAMA Neurol 71, 589–595 (2014).This study shows significantly increased sleep latency, reduced sleep efficiency and reduced REM, along with reduced melatonin levels and a loss of BMAL1 serum expression rhythms, in a cohor of 239 individuals with PD.
- 256.Gros P & Videnovic A Sleep and circadian rhythm disorders in Parkinson’s disease. Curr. Sleep Med. Rep 3, 222–234 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Uchida K, Okamoto N, Ohara K & Morita Y Daily rhythm of serum melatonin in patients with dementia of the degenerate type. Brain Res 717, 154–159 (1996). [DOI] [PubMed] [Google Scholar]
- 258.Videnovic A et al. Circadian melatonin rhythm and excessive daytime sleepiness in Parkinson disease. JAMA Neurol 71, 463–469 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Claassen DO & Kutscher SJ Sleep disturbances in Parkinson’s disease patients and management options. Nat. Sci. Sleep 3, 125–133 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Rothman SM & Mattson MP Sleep disturbances in Alzheimer’s and Parkinson’s diseases. Neuromolecular Med 14, 194–204 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Vitiello MV, Prinz PN, Williams DE, Frommlet MS & Ries RK Sleep disturbances in patients with mild-stage Alzheimer’s disease. J. Gerontol 45, M131–M138 (1990). [DOI] [PubMed] [Google Scholar]
- 262.Stopa EG et al. Pathologic evaluation of the human suprachiasmatic nucleus in severe dementia. J. Neuropathol. Exp. Neurol 58, 29–39 (1999). [DOI] [PubMed] [Google Scholar]
- 263.Cermakian N, Lamont EW, Boudreau P & Boivin DB Circadian clock gene expression in brain regions of Alzheimer ‘s disease patients and control subjects. J. Biol. Rhythms 26, 160–170 (2011). [DOI] [PubMed] [Google Scholar]
- 264.Logan RW et al. NAD+ cellular redox and SIRT1 regulate the diurnal rhythms of tyrosine hydroxylase and conditioned cocaine reward. Mol. Psychiatry 10.1038/s41380-018-0061-1 (2018).This study demonstrates mechanistic links between circadian regulation of SIRT1-dependent metabolic signalling and dopaminergic neurotransmission in the mouse ventral tegmental area, which is important for drug reward.
- 265.Belaidi AA et al. Marked age-related changes in brain iron homeostasis in amyloid protein precursor knockout mice. Neurotherapeutics 10.1007/s13311-018-0656-x (2018). [DOI] [PMC free article] [PubMed]
- 266.Uranga RM & Salvador GA Unraveling the burden of iron in neurodegeneration: intersections with amyloid beta peptide pathology. Oxid. Med. Cell. Longev 2018, 2850341 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Graham DG Oxidative pathways for catecholamines in the genesis of neuromelanin and cytotoxic quinones. Mol. Pharmacol 14, 633–643 (1978). [PubMed] [Google Scholar]
- 268.Tse DC, McCreery RL & Adams RN Potential oxidative pathways of brain catecholamines. J. Med. Chem 19, 37–40 (1976). [DOI] [PubMed] [Google Scholar]
- 269.Burbulla LF et al. Dopamine oxidation mediates mitochondrial and lysosomal dysfunction in Parkinson’s disease. Science 357, 1255–1261 (2017).This study demonstrates that mitochondrial stress promotes the accumulation of oxidized dopamine, consequently increasing α-synuclein aggregates in neurons derived from patients with PD, an effect selective to human neurons.
- 270.Barone P et al. The PRIAMO study: a multicenter assessment of nonmotor symptoms and their impact on quality of life in Parkinson’s disease. Mov. Disord 24, 1641–1649 (2009). [DOI] [PubMed] [Google Scholar]
- 271.Chaudhuri KR et al. International multicenter pilot study of the first comprehensive self-completed nonmotor symptoms questionnaire for Parkinson’s disease: the NMSQuest study. Mov. Disord 21, 916–923 (2006). [DOI] [PubMed] [Google Scholar]
- 272.Goodman AO, Morton AJ & Barker RA Identifying sleep disturbances in Huntington’s disease using a simple disease-focused questionnaire. PLOS Curr 2, RRN1189 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Aziz NA, Anguelova GV, Marinus J, Lammers GJ & Roos RA Sleep and circadian rhythm alterations correlate with depression and cognitive impairment in Huntington’s disease. Parkinsonism Relat. Disord 16, 345–350 (2010). [DOI] [PubMed] [Google Scholar]
- 274.Iranzo A et al. Neurodegenerative disorder risk in idiopathic REM sleep behavior disorder: study in 174 patients. PLOS ONE 9, e89741 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Schenck CH, Boeve BF & Mahowald MW Delayed emergence of a parkinsonian disorder or dementia in 81% of older men initially diagnosed with idiopathic rapid eye movement sleep behavior disorder: a 16-year update on a previously reported series. Sleep Med 14, 744–748 (2013). [DOI] [PubMed] [Google Scholar]
- 276.Kudo T, Loh DH, Truong D, Wu Y & Colwell CS Circadian dysfunction in a mouse model of Parkinson’s disease. Exp. Neurol 232, 66–75 (2011). [DOI] [PubMed] [Google Scholar]
- 277.Grippo RM, Purohit AM, Zhang Q, Zweifel LS & Guler AD Direct midbrain dopamine input to the suprachiasmatic nucleus accelerates circadian entrainment. Curr. Biol 27, 2465–2475 (2017).This study shows re-entrainment of the SCN to phase shifts in the light–dark schedule is facilitated by dopaminergic projections from the ventral tegmental area to the SCN and is dependent on dopamine 1 receptor-expressing neurons in the SCN.
- 278.Korshunov KS, Blakemore LJ & Trombley PQ Dopamine: a modulator of circadian rhythms in the central nervous system. Front. Cell. Neurosci 11, 91 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Fifel K & Cooper HM Loss of dopamine disrupts circadian rhythms in a mouse model of Parkinson’s disease. Neurobiol. Dis 71, 359–369 (2014). [DOI] [PubMed] [Google Scholar]
- 280.Gnanasekaran G “Sundowning” as a biological phenomenon: current understandings and future directions: an update. Aging Clin. Exp. Res 28, 383–392 (2016). [DOI] [PubMed] [Google Scholar]
- 281.Bedrosian TA & Nelson RJ Sundowning syndrome in aging and dementia: research in mouse models. Exp. Neurol 243, 67–73 (2013). [DOI] [PubMed] [Google Scholar]
- 282.Volicer L, Harper DG, Manning BC, Goldstein R & Satlin A Sundowning and circadian rhythms in Alzheimer’s disease. Am. J. Psychiatry 158, 704–711 (2001).This study shows that patients with AD have less diurnal activity, more nocturnal activity and phase delays in body-temperature rhythms, and that the severity of sundowning is positively correlated with lower-amplitude and more-phase-delayed rhythms.
- 283.Todd WD et al. A hypothalamic circuit for the circadian control of aggression. Nat. Neurosci 21, 717–724 (2018).This chemogenetic study in mice reveals a neural circuit involving projections from the SCN to the ventromedial hypothalamus that drives time-of-day-dependent aggressive behaviours.
- 284.Shokri-Kojori E et al. β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proc. Natl Acad. Sci. USA 115, 4483–4488 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Xie L et al. Sleep drives metabolite clearance from the adult brain. Science 342, 373–377 (2013).A landmark study in mice demonstrating that wakefulness suppresses the outflow of cerebral spinal fluid from the brain, whereas sleep leads to an increase in convective fluxes of fluid, effectively promoting the clearance of neurotoxic metabolics, including Aβ.
- 286.Da Mesquita S et al. Functional aspects of meningeal lymphatics in ageing and Alzheimer’s disease. Nature 560, 185–191 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Kang JE et al. Amyloid-β dynamics are regulated by orexin and the sleep-wake cycle. Science 326, 1005–1007 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Tabuchi M et al. Sleep interacts with Aβ to modulate intrinsic neuronal excitability. Curr. Biol 25, 702–712 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Faghih MM & Sharp MK Is bulk flow plausible in perivascular, paravascular and paravenous channels? Fluids Barriers CNS 15, 17 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.McClung CA Mind your rhythms: an important role for circadian genes in neuroprotection. J. Clin. Invest 123, 4994–4996 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Musiek ES et al. Circadian clock proteins regulate neuronal redox homeostasis and neurodegeneration. J. Clin. Invest 123, 5389–5400 (2013).This preclinical investigation demonstrates that components of the molecular clock control redox state and, when disrupted, lead to oxidative stress and cell death related to neurodegeneration.
- 292.Kondratov RV, Vykhovanets O, Kondratova AA & Antoch MP Antioxidant N-acetyl-L-cysteine ameliorates symptoms of premature aging associated with the deficiency of the circadian protein BMAL1. Aging 1, 979–987 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Chauhan R, Chen KF, Kent BA & Crowther DC Central and peripheral circadian clocks and their role in Alzheimer’s disease. Dis. Model. Mech 10, 1187–1199 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Homolak J, Mudrovcic M, Vukic B & Toljan K Circadian rhythm and Alzheimer’s disease. Med. Sci 6, 52 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Huang Z et al. Circadian rhythm dysfunction accelerates disease progression in a mouse model with amyotrophic lateral sclerosis. Front. Neurol 9, 218 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Skjerve A, Bjorvatn B & Holsten F Light therapy for behavioural and psychological symptoms of dementia. Int. J. Geriatr. Psychiatry 19, 516–522 (2004). [DOI] [PubMed] [Google Scholar]
- 297.Yamadera H et al. Effects of bright light on cognitive and sleep-wake (circadian) rhythm disturbances in Alzheimer-type dementia. Psychiatry Clin. Neurosci 54, 352–353 (2000). [DOI] [PubMed] [Google Scholar]
- 298.Hanford N & Figueiro M Light therapy and Alzheimer’s disease and related dementia: past, present, and future. J. Alzheimers Dis 33, 913–922 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.De Lepeleire J, Bouwen A, De Coninck L & Buntinx F Insufficient lighting in nursing homes. J. Am. Med. Dir. Assoc 8, 314–317 (2007). [DOI] [PubMed] [Google Scholar]
- 300.Figueiro MG et al. Tailored lighting intervention improves measures of sleep, depression, and agitation in persons with Alzheimer’s disease and related dementia living in long-term care facilities. Clin. Interv. Aging 9, 1527–1537 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Riemersma-van der Lek RF et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 299, 2642–2655 (2008).This double-blinded randomized controlled trial of 189 elderly residents of a group care facility demonstrates that a combination of melatonin supplementation and scheduled light exposure improves cognitive symptoms of dementia and reduces aggression.
- 302.Singer C et al. A multicenter, placebo-controlled trial of melatonin for sleep disturbance in Alzheimer’s disease. Sleep 26, 893–901 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Coogan AN et al. The circadian system in Alzheimer’s disease: disturbances, mechanisms, and opportunities. Biol. Psychiatry 74, 333–339 (2013). [DOI] [PubMed] [Google Scholar]
- 304.Arey RN et al. An important role for cholecystokinin, a CLOCK target gene, in the development and treatment of manic-like behaviors. Mol. Psychiatry 19, 342–350 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Coque L et al. Specific role of VTA dopamine neuronal firing rates and morphology in the reversal of anxiety-related, but not depression-related behavior in the Clock∆19 mouse model of mania. Neuropsychopharmacology 36, 1478–1488 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Dzirasa K et al. Lithium ameliorates nucleus accumbens phase-signaling dysfunction in a genetic mouse model of mania. J. Neurosci 30, 16314–16323 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.McClung CA Circadian rhythms, the mesolimbic dopaminergic circuit, and drug addiction. ScientificWorldJournal 7, 194–202 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.McClung CA et al. Regulation of dopaminergic transmission and cocaine reward by the Clock gene. Proc. Natl Acad. Sci. USA 102, 9377–9381 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Ozburn AR et al. Direct regulation of diurnal Drd3 expression and cocaine reward by NPAS2. Biol. Psychiatry 77, 425–433 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Ozburn AR et al. NPAS2 regulation of anxiety-like behavior and GABAA receptors. Front. Mol. Neurosci 10, 360 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Ozburn AR, Larson EB, Self DW & McClung CA Cocaine self-administration behaviors in ClockΔ 19 mice. Psychopharmacology 223, 169–177 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Parekh PK et al. Altered GluA1 (Gria1) function and accumbal synaptic plasticity in the Clock∆19 model of bipolar mania. Biol. Psychiatry 10.1016/j.biopsych.2017.06.022 (2017). [DOI] [PMC free article] [PubMed]
- 313.Roybal K et al. Mania-like behavior induced by disruption of CLOCK. Proc. Natl Acad. Sci. USA 104, 6406–6411 (2007).This study demonstrates mice harbouring a mutation in Clock display a behavioural repertoire similar to human mania and provides evidence for CLOCK specifically in the ventral tegmental area to be important for these behaviours via modulation of dopamine cell firing.
- 314.Sidor MM et al. Daytime spikes in dopaminergic activity drive rapid mood-cycling in mice. Mol. Psychiatry 20, 1406–1419 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Spencer S et al. A mutation in CLOCK leads to altered dopamine receptor function. J. Neurochem 123, 124–134 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Neufeld-Cohen A et al. Circadian control of oscillations in mitochondrial rate-limiting enzymes and nutrient utilization by PERIOD proteins. Proc. Natl Acad. Sci. USA 113, E1673–E1682 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.O’Neill JS & Feeney KA Circadian redox and metabolic oscillations in mammalian systems. Antioxid. Redox Signal 20, 2966–2981 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Marcheva B et al. Circadian clocks and metabolism. Handb. Exp. Pharmacol 217, 127–155 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Braun R et al. Universal method for robust detection of circadian state from gene expression. Proc. Natl Acad. Sci. USA 115, E9247–E9256 (2018).This study demonstrates the use of a set of computational algorithms called TimeSignature to predict the endogenous phase of an individual based on the particular gene signatures from the blood acquired at a single timepoint.
- 320.Jones SE et al. Genome-wide association analyses in 128,266 individuals identifies new morningness and sleep duration loci. PLOS Genet 12, e1006125 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Lane JM et al. Genome-wide association analysis identifies novel loci for chronotype in 100,420 individuals from the UK Biobank. Nat. Commun 7, 10889 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.LeGates TA, Fernandez DC & Hattar S Light as a central modulator of circadian rhythms, sleep and affect. Nat. Rev. Neurosci 15, 443–454 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.LeGates TA et al. Aberrant light directly impairs mood and learning through melanopsin-expressing neurons. Nature 491, 594–598 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Fernandez DC et al. Light affects mood and learning through distinct retina-brain pathways. Cell 175, 71–84 (2018).Using mice, this study demonstrates that light input to the brain reaches neural circuits related to depression and learning through distinct projections from the retina, revealing a potential mechanism by which aberrant light exposure (for example, light at night) affects mood and cognition.
- 325.Librodo P, Buckley M, Luk M & Bisso A Chronotherapeutic drug delivery. J. Infus. Nurs 38, S18–S23 (2015). [DOI] [PubMed] [Google Scholar]
- 326.Ruben MD et al. A database of tissue-specific rhythmically expressed human genes has potential applications in circadian medicine. Sci. Transl Med 10, eaat8806 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Melkani GC & Panda S Time-restricted feeding for prevention and treatment of cardiometabolic disorders. J. Physiol 595, 3691–3700 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Mindikoglu AL, Opekun AR, Gagan SK & Devaraj S Impact of time-restricted feeding and dawn-to-sunset fasting on circadian rhythm, obesity, metabolic syndrome, and nonalcoholic fatty liver disease. Gastroenterol. Res. Pract 2017, 3932491 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Stewart KT, McEachron DL, Rosenwasser AM & Adler NT Lithium lengthens circadian period but fails to counteract behavioral helplessness in rats. Biol. Psychiatry 30, 515–518 (1991). [DOI] [PubMed] [Google Scholar]
- 330.McCarthy MJ et al. Genetic and clinical factors predict lithium’s effects on PER2 gene expression rhythms in cells from bipolar disorder patients. Transl Psychiatry 3, e318 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Sprouse J, Reynolds L, Braselton J & Schmidt A Serotonin-induced phase advances of SCN neuronal firing in vitro: a possible role for 5-HT5A receptors? Synapse 54, 111–118 (2004). [DOI] [PubMed] [Google Scholar]
- 332.Zhang R, Lahens NF, Ballance HI, Hughes ME & Hogenesch JB A circadian gene expression atlas in mammals: implications for biology and medicine. Proc. Natl Acad. Sci. USA 111, 16219–16224 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Dokucu ME, Yu L & Taghert PH Lithium- and valproate-induced alterations in circadian locomotor behavior in Drosophila. Neuropsychopharmacology 30, 2216–2224 (2005). [DOI] [PubMed] [Google Scholar]
- 334.Sathyanarayana A et al. Sleep quality prediction from wearable data using deep learning. JMIR Mhealth Uhealth 4, e125 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]


