ABSTRACT
Background and Objective: Millions of children and adolescents worldwide suffer from post-traumatic stress disorder (PTSD) and other problems due to prolonged exposure to traumatizing events. Forms of cognitive-behavioural therapy are the most commonly used treatment for PTSD, but evidence from sophisticated studies in clinical settings among children is limited.
Method: This multicentre, parallel, non-blinded, pragmatic randomized controlled trial assessed the effectiveness of narrative exposure therapy (NET) in traumatized children and adolescents. Fifty 9–17-year-old participants, who had experienced prolonged traumatic conditions in the form of refugeedom or family violence and suffered from PTSD symptoms, were randomized into NET (n = 29) and treatment as usual (TAU; n = 21) active control groups. The objective was to determine whether NET can be feasibly implemented within the existing healthcare system of a high-income country and whether it would reduce mental health problems, especially PTSD, and increase resilience, in children and adolescents with multiple traumas more effectively than TAU. We hypothesized that NET would be more effective than TAU in reducing symptoms and increasing resilience.
Results: Analysis of variance revealed that PTSD and psychological distress, but not depression symptoms, decreased regardless of treatment group. Resilience increased in both groups. Within-group analyses showed that the decrease in PTSD symptoms was significant in the NET group only. The effect sizes were large in NET but small in TAU. Concerning PTSD symptom cut-off scores, the reduction in the share of participants with clinical-level PTSD was significant in the NET group only. Intention-to-treat analyses using linear mixed models confirmed these results.
Conclusions: Despite its shortcomings, this study gives preliminary support for the safety, effectiveness, and usefulness of NET among multiply traumatized children and adolescents in clinical settings. Close attention must be paid to the implementation of the new intervention as an everyday tool in healthcare.
KEYWORDS: Refugee, maltreatment, children, adolescents, narrative exposure therapy, PTSD
HIGHLIGHTS
• Narrative exposure therapy (NET) is a safe and useful method for treating children with multiple violence-related traumas.• Intrusive symptoms may be more effectively treated with NET than with non-exposure-based methods.• Close attention must be paid to the implementation of new interventions for trauma-related symptoms as everyday tools in typical healthcare settings.
Tratando a niños y adolescentes con múltiples traumas- un estudio clínico randomizado de terapia de exposición narrativa
Antecedentes y Objetivo: Millones de niños y adolescentes en todo el mundo sufren de trastorno de Estrés Postraumático (TEPT) y otros problemas debido a exposición prolongada a eventos traumáticos. Formas de terapia cognitivo-conductual son las más comúnmente usadas para tratar el TEPT, pero evidencias con diseños sofisticados con niños en ambientes clínicos son limitados.
Métodos: Condujimos un estudio multicéntrico, paralelo, no ciego, pragmático aleatoriamente controlado y estudiamos la efectividad de la Terapia de Exposición Narrativa (NET) en niños y adolescentes traumatizados. Un total de 50 participantes entre 9 y 17 años, quienes habían experimentado condiciones traumáticas prolongadas como refugiados o violencia familiar y sufrido de síntomas de TEPT, fueron puestos en forma aleatoria en grupos de NET (n= 29) y tratamiento usual como control (TAU por sus siglas en inglés; n= 21). El objetivo del estudio era encontrar si la NET puede ser implementada de manera factible en el sistema de salud existente de un país de altos ingresos y si puede reducir los problemas de salud mental, especialmente TEPT, y aumentar la resiliencia, en niños y adolescentes con múltiples traumas más efectivamente que el TAU. Nuestra hipótesis era que la NET sería más efectiva en reducir los síntomas y aumentaría más la resiliencia que el TAU.
Resultados: los resultados ANOVA revelaron que el TEPT y la angustia psicológica, pero no los síntomas depresivos, disminuyeron sin importar el grupo en el cual fueron tratados. La resiliencia aumentó en ambos grupos. Los análisis intra-grupo mostraron que hubo una disminución significativa en los síntomas de TEPT solo en el grupo de la NET. Los tamaños del efecto fueron grandes en la NET, pero pequeños en el TAU. En lo que concierne a los síntomas de TEPT los puntos de corte, una reducción en la proporción de participantes con un nivel clínico de TEPT fue significativa sólo en el grupo de NET. El análisis de con la intención de tratar empleando modelos lineales mixtos confirmó estos resultados.
Conclusiones: A pesar de las limitaciones del estudio actual, nos da un apoyo preliminar para la seguridad, efectividad y utilidad de la NET entre múltiples niños y adolescentes traumatizados en ambientes clínicos. Se deberá prestar mucha atención a la implementación de la nueva intervención como una herramienta del día a día en el sistema de salud.
PALABRAS CLAVES: refugiados, maltrato, niños, adolescentes, Terapia de Exposición Narrativa, TEPT
Abstract
背景和目标: 全世界上百万的儿童和青少年患有创伤后应激障碍(PTSD)和长期接触创伤事件导致的其他问题。认知行为疗法是PTSD最常用的治疗形式,但设计成熟的儿童临床情境提供的证据还尚有限。
方法:我们进行了一项多中心、平行、非盲法( non-blinded)、务实的随机对照试验,并研究了叙事暴露疗法(NET)在创伤儿童和青少年中的有效性。总共50名9-17岁的被试,他们经历了避难所或家庭里的暴力,在经历长期创伤性疾病后患有PTSD症状。 被试被随机分入NET(n = 29)和照常治疗主动控制(TAU; n = 21)组。该研究的目的是考查NET是否可以在高收入国家的现有医疗保健系统中切实可行地实施,以及是否能够比TAU更有效地帮助多发创伤的儿童青少年减少心理健康问题(尤其是创伤后应激障碍),并提高韧性。我们假设NET比TAU更有效地减轻症状和增加弹性。
结果:ANOVA结果显示,不论哪个治疗组,PTSD和心理痛苦有所减轻,但抑郁症状不变。两组的恢复力均有所提高。组内分析显示,仅在NET组中PTSD症状的减少是显著的。 NET的效果大小很大,但TAU的效果很小。考虑PTSD症状临界分,仅在NET组中临床PTSD被试比例的降低是显著的。使用线性混合模型的治疗意向分析(Intention-to-treat analyses)证实了这些结果。
结论:尽管本研究存在缺陷,但它为NET在临床环境中对多发创伤儿童和青少年群体中的安全性、有效性和可用性提供了初步支持。我们必须密切关注这种新干预措施作为医疗保健日常工具的使用情况。
关键词: 难民, 虐待, 儿童, 青少年, 叙事暴露疗法, 创伤后应激障碍
1. Introduction
Exposure to multiple traumas during childhood is a major challenge for mental health throughout the lifespan. In particular, a strong association between violence-related traumatic events and post-traumatic symptoms has been established (Evans, Davies, & DiLillo, 2008; Johnson & Thompson, 2008). Findings on the prevalence of post-traumatic stress disorder (PTSD) among refugee children have varied between 19% and 54% (for a review, see Bornstein & Montgomery, 2011). Rates as high as 37% and 65% were found in studies among children and adolescents resettled into high-income countries (Buchmüller, Lembcke, Busch, Kumsta, & Leyendecker, 2018; Gandham, Gunasekera, Isaacs, & Britton, 2017). At the same time, a great number of children living in high-income countries are exposed to family violence, and 13–50% of them suffer from PTSD (Rossman, Hughes, & Rosenberg, 2000). This study included children and adolescents exposed to violence either in war or refugeedom or within the family.
For traumatized children and adolescents in general, cognitive-behavioural therapy (CBT), especially its trauma-focused forms, has been repeatedly found to be effective in reducing PTSD and other mental health symptoms (Gillies, Taylor, Gray, O’Brien, & D’Abrew, 2012; Stallard, 2006). A review by de Arellano et al. (2014) showed that the most studied intervention package, trauma-focused cognitive behavioural therapy (TF-CBT), is indeed able to reduce symptoms of PTSD. The TF-CBT method has mainly been studied among sexually abused children, with both active control groups and waiting-list control groups.
Narrative exposure therapy (NET) is also based on CBT principles but its development has been influenced by exposure-based and testimonial therapies (Schauer, Neuner, & Elbert, 2011). It is a manualized, individual, short-term intervention programme for the treatment of PTSD resulting from exposure to organized violence or other repeated traumatic events. When treating children and adolescents with multiple traumas, it may be important not only to tackle one event in their traumatic history, but to process all events that still cause PTSD symptoms (Mørkved et al., 2014; Mørkved & Thorp, 2018; Schauer et al., 2011). The clinical model of repeated traumatization underlying NET draws on (1) dual representation theories of PTSD (Brewin, Dalgleish, & Josep, 1996; Brewin, 2014) and (2) emotional processing theory and the idea of fear networks (Foa, Hupper, & Cahill, 2006). KIDNET is a child-friendly version with some adaptations to the original model to help children to construct their story and express their emotions (Schauer, Neuner, & Elbert, 2017).
Although good evidence on the effectiveness of NET already exists for adults (McPherson, 2012; Robjant & Fazel, 2010), only four trials are available among children and adolescents: one for refugee children and adolescents in Germany (Ruf et al., 2010), one among former child soldiers in Uganda, including also young adults (Ertl, Pfeiffer, Schauer, Elbert, & Neuner, 2011), one among Sri Lankan adolescents affected by both war and a natural disaster (Catani et al., 2009), and one among Rwandan genocide orphans (Schaal, Elbert, & Neuner, 2009). The only trial with refugee children in a high-income country did not include an active control group and none of the earlier studies was conducted as a pragmatic clinical trial (PCT), where intervention delivery and participant follow-up would be closely aligned with usual care in order to understand the real-world implications of the intervention (Thorpe et al., 2009; Zwarenstein et al., 2008). None of the earlier studies included children exposed exclusively to family violence, even though they had often experienced multiple traumatization.
Among adults, a single pragmatic trial exists on the effectiveness of NET versus treatment as usual (TAU) among adult refugees and asylum seekers (Halvorsen, Stenmark, Neuner & Nordahl, 2014). It showed the superiority of NET in treating PTSD symptoms over TAU, although symptoms decreased in both groups. A clear gap exists in understanding the effectiveness of NET as part of everyday clinical work among multiply traumatized children. We aimed to contribute to the field by conducting a PCT in the context of the existing healthcare system of a high-income country.
In this study, we ask: (1) Can NET be feasibly implemented within the existing healthcare system of a high-income country (Finland)? (2) Does NET reduce (a) PTSD symptoms, (b) depressive symptoms, or (c) psychological distress, or improve (d) resilience in children and adolescents with multiple traumas more effectively than TAU? We hypothesize that NET is more effective than TAU in reducing the symptoms and increasing resilience.
2. Method
2.1. Design and procedure
We carried out a multicentre, parallel-group, randomized, controlled pragmatic trial comparing NET to TAU at several treatment units located around Finland. This study was registered at ClinicalTrials.gov (NCT02425280) before data collection started and the study protocol was published beforehand (Kangaslampi, Garoff & Peltonen, 2015). Since publication of the protocol, the study was extended to also include participants suffering from violence in the family. Other changes that were necessary to the protocol during the study are noted later. This paper presents findings on the primary outcomes described in the study protocol.
Participants’ mental health was assessed before and after the 3 month intervention period as well as 3 months after the intervention ended. Unfortunately, the very limited data gathered at follow-up prevented their use in primary analyses of effectiveness. However, these data were utilized in intention-to-treat analyses.
A total of 51 experienced mental health professionals were trained to use NET and recruited as therapists. With 51 trained therapists, we aimed at 80 participants to be recruited for the study, taking into account dropouts. The goal was to include units responsible for children’s and adolescents’ trauma treatment at all levels (primary, secondary, and specialized units). The therapists also acted as assessors, collecting data from the patient they were treating largely in the same way as they would assess the patient’s symptoms and effects of treatment in general. In other words, the researchers were involved in the treatment practice as little as possible.
A 3 day NET training was organized in three consecutive years (2014–2016). The recruitment took place between January 2015 and June 2017. The data collection started in January 2015 and ended in February 2018. To maintain NET skills, the trained therapists participated in tailored peer-group meetings organized within their own units as the interventions proceeded. When conducting TAU, therapists received the usual work counselling which is statutory in psychiatric work in Finland.
NET consisted of seven to 10 weekly sessions lasting for 90 minutes each. Treatment length could be adjusted, but was advised not to exceed 10 sessions. NET was conducted according to the manual as outlined by Schauer, Neuner & Elbert (2011) and translated into Finnish (Peltonen, 2015). With younger participants, the treatment included elements from KIDNET with creative elements, especially as part of the lifeline construction (Schauer, Neuner & Elbert, 2017). The purpose of this pragmatic trial was to study the NET method as a part of everyday clinical practice, implemented in the existing healthcare framework, thus reflecting typical, not necessarily ideal or perfect, use of the method. However, treatment adherence and competence was monitored and ensured through (1) group supervision, where all cases were reviewed and discussed, (2) a self-report questionnaire, where the therapists had to report the patient’s life events that had been part of the intervention, and (3) use of the Subjective Units of Distress Scale (SUDS) administered to the client to ensure that exposure really took place during sessions where it was intended to happen. No major deviations from the NET protocol as described by Schauer et al. (2011) were identified.
In the TAU condition, the therapists were instructed to use any intervention that they would normally use. No specific instructions were given as to what TAU should entail, apart from not including elements specific to NET. No extra resources were added to the usual care settings to implement the interventions. The TAU varied in intensity from weekly to monthly meetings, reflecting the typical level of care provided by each unit. The session duration varied between 45 and 90 minutes, and treatment was delivered by a single therapist (excluding network meetings). Based on information gathered through a self-report questionnaire, TAU mainly consisted of the following components (in order of prevalence): (1) network meetings with the child’s family and involved professionals (such as social workers and teachers); (2) discussions about current problems and life situations such as sleep difficulties, problems related to the asylum procedure, and practical matters; (3) psychosocial support and monitoring; and (4) family therapeutic sessions. One TAU case was reported to include one session of exposure to a traumatic event.
The ethical boards of the Pirkanmaa Hospital District, Tampere City Welfare Services, the Helsinki Diaconess Institute, and the Hospital District of Southwest Finland approved the study. Age-specific brochures with information about the study were given to the participants and their parents. Written consent was requested from both parents or guardians and the participants themselves.
2.2. Participants
The sample consisted of 50 participants recruited among the patients and clients of the participating clinics. The participants were between 9 and 17 years of age (mean age 13.2, SD = 3.2), who attended NET or TAU for post-traumatic stress symptoms. Boys made up slightly more than half (58%) of the sample. Three-quarters of the participants were refugees or asylum seekers (n = 37) and one-quarter were Finnish children and adolescents with experiences of family violence (n = 13). The refugee children and adolescents were from Iraq (n = 14), Afghanistan (n = 14), and various other countries (from other Middle Eastern countries and from African countries, n = 9).
The inclusion criteria were: (1) 9–17 years of age; (2) exposure to violence either in war or refugeedom or within the family; (3) the child being referred to a participating clinic because of trauma symptoms; and (4) active post-traumatic stress symptoms, as confirmed by the therapist at the participating unit based on his or her evaluation and the Children’s Revised Impact of Event Scale (CRIES) (Horowitz, 1986; Smith, Perrin, Dyregrov, & Yule, 2003). All children and adolescents were subjected to a clinical evaluation, but a diagnosis of PTSD was not necessary for participation in the study. The exclusion criteria were: (1) psychotic disorders; (2) current severe substance abuse; (3) severe suicidal ideations; and (4) intellectual disability. Four adolescents declined to participate. Three of them were unaccompanied minors, who were sceptical about the confidentiality of the research even though it was explained to them, and for one child, the parents were hesitant to start treatment at all.
2.3. Randomization
Each participant was randomized into one of two groups. One group received NET, acting as the study group, and the other group, receiving TAU, acted as a positive control group. The trial was parallel group in nature.
At the start of the study, before any participants were recruited, the participating clinics were provided with folders by the research group, each containing all the relevant research material, questionnaires, and measurements for one participant. A sealed, opaque envelope was placed by the research team in each folder with a piece of paper inside. Half of these papers were marked ‘NET’ and the other half ‘TAU’. Each trained therapist was provided with two folders, one for NET and one for TAU, forming an allocation ratio of 1:1 (Schulz & Grimes, 2002). Whenever a child was identified as a potential participant by a clinician at one of the cooperating units, information concerning the intervention and the related research was provided both to the participant and to his or her parents. If they were willing to participate in the research, informed consent was requested from the child and his or her parents. The envelope was then to be opened and its content would determine whether the participant received NET or TAU. However, as Figure 1 shows, the final distribution to NET and TAU groups was not even. This was due to difficulties in the planned recruitment procedure of participants. One-third of the trained therapists could not find any eligible patients to participate in the study and 41% recruited one participant instead of two. Irregularities in the randomization process were not identified, but cannot be completely ruled out as additional explanations for the imbalance.
Figure 1.
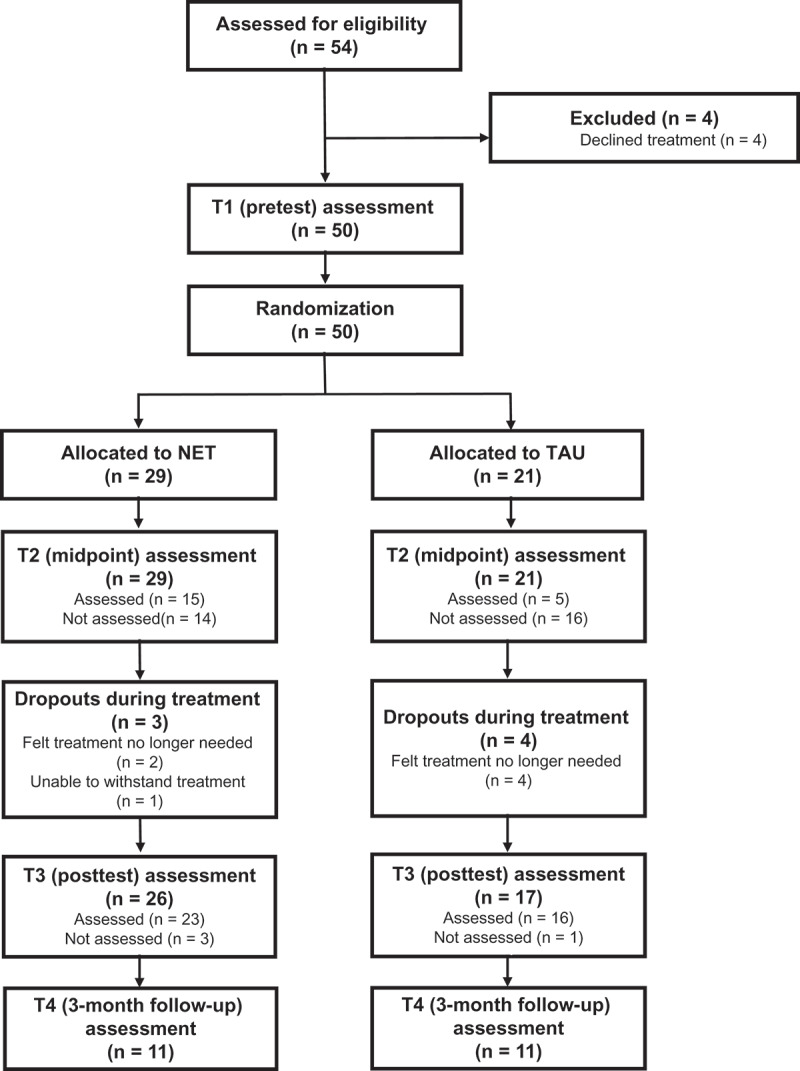
Adapted CONsolidated Standards of Reporting Trials (CONSORT) flow diagram of data collection. NET, narrative exposure therapy; TAU, treatment as usual.
Two out of 10 dropouts were Finnish children with a background of family violence, while the others had a refugee background. Dropouts were due to discontinuation of treatment in seven cases. Of those, one participant belonged to the TAU and six to the NET group. The reason for dropout in six cases was either the child’s/adolescent’s or his or her parents’ decision not to continue the treatment because they felt that the treatment was no longer needed (in all cases the therapists had a different opinion). Only one NET client reported that it was too hard to go through the traumatic events and wanted to quit. Three NET cases are further considered as dropouts in the absence of collected post-test data, although they completed the treatment.
2.4. Measures
In line with PCT principles, the measurement tools were selected so that they could be easily employed as part of the therapists’ everyday practice. Most of the measures were already in use in participating clinics before the study. All therapists were familiar with administering self-report questionnaires prior to the study, and the importance of not interfering when the children were filling the questionnaires was emphasized when training the therapists. All measures were either already available in the most common languages spoken by the participants (Finnish, English, Dari, Sorani, and Arabic), or translated into these languages as part of this study. For those participants who did not speak any of these languages, an interpreter read out the questions and response alternatives to them.
2.4.1. Traumatic experiences
Exposure to traumatic experiences was measured by checklists capturing typical violent and traumatic events during war or refugeedom (nine items) and violence in the family (nine items). The checklists were prepared for the purposes of this study but were based on the Event Checklist for War, Detention, and Torture Experiences (Schauer et al., 2011), the Child and Adolescent Intake Form of the Center for Victims of Torture, and adverse childhood experiences studies (Dong et al., 2004; Duke, Pettingell, McMorris, & Borowsky, 2010).
2.4.2. PTSD
PTSD symptoms were measured at T1 (pretest), T2 (midway), T3 (post-test), and T4 (follow-up), using the children’s version of the Revised Impact of Event Scale (CRIES) (Horowitz, 1986; Smith et al., 2003). CRIES consists of 13 items covering the re-experiencing, avoidance, and hyperarousal symptom dimensions. Participants estimate the occurrence of each symptom on a four-point scale (0 = not at all, 1 = rarely, 3 = sometimes, 5 = often). CRIES has been found to have good reliability among war-affected children and adolescents (Smith et al., 2003). In this study, the PTSD Total score, together with the subscales of Intrusions, Avoidance, and Arousal, was used. In addition, the cut-off score of 17, calculated from the Intrusions and Avoidance subscales, was used as a measurement of high probability of obtaining a diagnosis of PTSD, as recommended by Smith et al. (2003). Because the questions in the CRIES refer to a certain traumatic event, and participants in our sample had been exposed to many events, they were advised to think about the worst or most disturbing event in their trauma history when answering the questionnaire. The reliabilities were α = .81 at pretest and α = .86 at post-test for the PTSD Total score, α = .64 at pretest and α = .83 at post-test for Intrusions, α = .74 at pretest and α = .80 at post-test for Avoidance, and α = .76 at pretest and α = .83 at post-test for Arousal.
2.4.3. Depression
Depressive symptoms were measured at T1, T3, and T4, using the Depression Self-Rating Scale for Children (DSRS) (Birleson, Hudson, Buchanan, & Wolff, 1987). The measure includes 18 items that assess the cognitive, affective, and behavioural dimensions of depression. For each item, participants estimate on a three-point scale whether they have experienced the symptom over the preceding 2 weeks (0 = not at all, 1 = sometimes, 2 = all the time). The reliabilities were α = .89 at pretest and α = .89 at post-test.
2.4.4. Resilience
Resilience was assessed using a questionnaire measuring individual resilience among war-traumatized children, developed for this study, at T1, T3, and T4. It was used after considering a well-validated Child and Youth Resilience Measure (CYRM) (Ungar & Liebenberg, 2011), but finding some of its items difficult for the target group. The questionnaire consists of 10 items measuring the positive individual resources of children and adolescents (e.g. ‘I have a skill which I am particularly good at’; ‘I feel that I am important to someone’). Participants evaluated on a three-point scale how well the description fit them (0 = not at all, 1 = somewhat, 2 = yes, fits well). Reliability was estimated at α = .89 at pretest and α = .75 at post-test.
2.4.5. Psychological distress
Psychological distress (child and guardian-rated) was measured using the Strengths and Difficulties Questionnaire (SDQ) (Goodman, 1997). A total score composed of emotional, behavioural, and relational problems, as well as hyperactivity, was used, as suggested by Goodman (1997). Each of the dimensions consists of five items rated on a three-point scale on how well the description fits the participants (0 = not at all, 1 = somewhat, 2 = yes, fits well). Reliability was α = .82 for children’s self-reports and α = .81 for parents’ reports at pretest, and α = .76 for children’s self-reports and α = .83 for parents’ reports at post-test.
2.4.6. Life changes during therapy
To take into account the possible effects of life changes occurring during therapy, we asked at post-test whether participants had had negative or positive changes in living arrangements after the intervention had started.
2.5. Statistical analyses
Two sets of analyses were carried out: first, an analysis of changes from pretest to post-test with treatment completers for whom data on symptoms were available at T3, and, secondly, intention-to-treat analyses employing all available data (T1, T2, T3, and T4). In the first and primary analysis, repeated measures analyses of variance (ANOVA) in SPSS 24 were used, with time as a two-level within-subject variable and treatment as a two-level between-subjects variable for PTSD symptom Total score and its subscales (Intrusion, Avoidance, and Arousal), as well as for depression symptoms, resilience, and psychological distress. To compare the clinical significance of symptom reduction, we used the cut-off score of 17 for the Avoidance and Intrusion subscales combined, and explored the share of participants who recovered from clinical-level PTSD to levels below this cut-off during the treatments they received. For this, we used related samples McNemar tests for both groups (NET and TAU) with pretest and post-test data of actual treatment completers.
For intention-to-treat analyses, we used linear mixed-effects modelling with the nlme package (Pinheiro, Bates, DebRoy, Sarkar, & Core Team, 2018) in R 3.4.3 (R Core Team, 2017), employing all available data from all points of measurement. The effect of time was modelled as weeks elapsed since the pretest assessment, and time × treatment interactions were examined for evidence of dissimilar treatment effects. Improvements in model fit were indicated by the Akaike information criteria and likelihood ratio tests, and 95% confidence intervals (CIs) were computed for particular effects. Visual inspection of residual plots showed no evidence of heteroscedasticity or significant deviation from normality.
A total of 34 individual item-level responses were missing from otherwise completed measures. These individual missing values were replaced by the response closest to that participant’s mean answer to other questions of the measure. Otherwise, owing to the pragmatic nature of the trial, only partial measurements were available for a large minority of participants. T1 measurements were available on PTSD symptoms for 47 participants, on depressive symptoms for 34 participants, on resilience for 41 participants, on self-evaluated psychological distress for 33 participants, and on guardian-evaluated psychological distress for 28 participants. At the T2 time-point used only for intention-to-treat analyses, PTSD symptoms were assessed for 19 participants. At T3, measurements were available as follows: PTSD symptoms, 38 participants; depressive symptoms, 25 participants; resilience, 26 participants; self-evaluated psychological distress, 21 participants; and guardian-evaluated psychological distress, 21 participants. Finally, at T4, measurements were available as follows: PTSD symptoms, 20 participants; depressive symptoms, 17 participants; resilience, 14 participants; self-evaluated psychological distress, 12 participants; and guardian-evaluated psychological distress, 13 participants. Little’s test indicated that data were missing at random in T1 and T3 [χ2(214) = 208.83, p = .587].
3. Results
3.1. Implementation
Out of 51 trained therapists, 35 (67%) contributed data to the study. This means that 33% of trained therapists could not find an eligible patient to participate in the study over the 1–3 year (depending on the training date) recruitment period. Only four patients refused to participate in the study. The aim was that every therapist would recruit two participants, one for NET and one for TAU, in random order. This was achieved by 59% of the contributing therapists, while 41% of them recruited one participant (allocated randomly to NET or TAU). The biggest obstacle expressed for recruiting participants was problems deciding on the timing of trauma treatment overall. In many cases, therapists considered that the child would not be ready to be exposed to his or her trauma history (which would be part of the treatment if allocated to NET) and it was therefore not possible to recruit the child to the study. Thus, in practice, additional exclusion criteria began to be applied by the therapists during the study.
Interpreters were used in 73% (n = 22) of cases with children of refugee background, and were present during all assessments and treatment. With one exception, the same interpreter worked with the same child in all NET or TAU sessions. The quality of interpretation varied, according to the professionals’ reports, but was at a satisfactory or good level at all times.
The majority of the interventions were conducted at outpatient clinics by psychologists and psychiatric nurses. Treatment fidelity among participating clinicians was good and no major deviations from the NET protocol described by Schauer et al. (2005) were identified. Tables 1 and 2 describe the included units, the number of trained therapists at each level, with information on their educational background, as well as the number of professionals who eventually started either the NET or a TAU intervention with their clients.
Table 1.
Number of therapists trained, as well as interventions started and completed at different types of treatment units.
| Unit | Therapists trained | Interventions started | Interventions completed |
|---|---|---|---|
| Primary healthcare | 10 | 4 | 4 |
| Specialized healthcare: outpatient clinics | 27 | 30 | 24 |
| Specialized healthcare: inpatient clinic | 4 | 0 | 0 |
| Third sector (trauma unit) | 7 | 10 | 6 |
| Housing unit | 3 | 6 | 5 |
| Total | 51 | 50 | 39 |
Table 2.
Number of therapists trained, as well as interventions started and completed, by occupation of therapist.
| Occupation | Therapists trained | Interventions started | Interventions completed |
|---|---|---|---|
| Psychiatric nurse | 13 | 16 | 14 |
| Social worker | 4 | 3 | 2 |
| Psychologist | 29 | 24 | 16 |
| Psychiatrist | 5 | 7 | 7 |
| Total | 51 | 50 | 39 |
3.2. Descriptive statistics
A minority (23% and 30%) of participants in both groups were Finnish children with a background of family violence, while the other participants had a refugee background. The vast majority (over 80%) of children in both groups had received psychiatric care before the current intervention. As confirmed by χ2 tests and t tests, there were no systematic group differences in any of the sociodemographic characteristics, or in baseline levels of the outcome variables (Table 3).
Table 3.
Demographic variables and baseline levels of mental health variables for all randomized participants.
| Demographic variables | NET (n = 30) N (%) M (SD) | TAU (n = 20) N (%) M (SD) | Difference |
|---|---|---|---|
| Gender | ns | ||
| Girl | 12 (40%) | 9 (45%) | |
| Boy | 18 (60%) | 11 (55%) | |
| Age | 13.4 (2.7) | 13.0 (3.3) | ns |
| Country of origin | ns | ||
| Finland | 7 (23%) | 6 (30%) | |
| Afghanistan | 8 (27%) | 6 (30%) | |
| Iraq | 8 (27%) | 6 (30%) | |
| Other | 6 (20%) | 3 (10%) | |
| Previous psychiatric treatment (yes) | 25 (83%) | 17 (85%) | ns |
| Post-traumatic stress symptoms | 38.0 (14.3) | 37.0 (13.0) | ns |
| Depressive symptoms | 14.0 (9.0) | 12.9 (4.8) | ns |
| Psychological distress, self-evaluated | 14.2 (7.2) | 15.8 (5.3) | ns |
| Psychological distress, guardian-evaluated | 17.1 (7.7) | 17.4 (6.6) | ns |
| Resilience | 14.1 (4.8) | 13.2 (4.5) | ns |
NET, narrative exposure therapy; TAU, treatment as usual; ns, no significant difference at p < .05, according to t test. Post-traumatic stress symptoms were measured with the Children’s Revised Impact of Event Scale (theoretical range 0–65). Depressive symptoms were measured by the Depression Self-Rating Scale for Children (theoretical range 0–36). Psychological distress was measured by the Strengths and Difficulties Questionnaire Total Difficulties scale (theoretical range 0–40). Resilience was measured by a custom 10-item measure (theoretical range 0–20).
As Table 4 shows, exposure to violence was massive among the participants. Over 80% of participants with a refugee background had experienced violence by an unknown person and over 20% of them physical abuse by their caretakers. Over 70% of family members of refugee participants had experienced violence and/or torture, and for 35% of them a family member had been killed. Finnish children with a family violence background had experiences of physical (100%), psychological (70%), and sexual (46%) violence. None of the children was experiencing violence at the time of the study.
Table 4.
Exposure to different types of traumatic events for children with refugee or family violence backgrounds.
| Traumatic event | Refugee (n = 37) | Family violence (n = 13) |
|---|---|---|
| Stayed at refugee camp | 6 (16%) | |
| Been imprisoned or held in enclosed space against will | 13 (35%) | |
| Experienced violence by a stranger | 30 (81%) | |
| Family members imprisoned or taken away against their will | 17 (46%) | |
| Family members experienced violence or been tortured | 27 (73%) | |
| Family members died due to armed conflict | 13 (35%) | |
| Family members injured due to armed conflict | 9 (24%) | |
| Been separated from family members due to armed conflict | 20 (54%) | |
| Family members missing | 13 (35%) | |
| Experienced physical abuse by caretakers | 21 (57%) | 13 (100%) |
| Experienced psychological abuse by caretakers | 20 (54%) | 9 (69%) |
| Experienced sexual abuse by caretakers | 7 (19%) | 6 (46%) |
| Neglected | 10 (27%) | 7 (54%) |
Exploration of the possible effects of life changes occurring during therapy showed that two participants in the NET group had had negative and one had had positive changes in living arrangements after the intervention started. Other participants reported no changes.
3.3. Effectiveness
3.3.1. Short-term effects among treatment completers
Table 5 shows the levels of all primary outcomes at T1 and T3, the mean change in them, and effect sizes. ANOVA results, presented in Tables 6 and 7, indicated a significant main effect of time for PTSD Total score [F(1,35) = 12.93, p < .001], as well as for the subscales of Intrusions [F(1,35) = 21.77, p < .001] and Arousal [F(1,35) = 8.16, p = .007], but not for Avoidance. As presented in Table 6, the main effect of time was also significant for psychological distress reported by the child [F(1,18) = 4.97, p < .039] and the guardian [F(1,17) = 5.94, p < .026], as well as for resilience [F(1,23) = 5.14, p < .033], but not for depression. The main effects of group and time × treatment interaction were not significant for any of the outcome variables.
Table 5.
Levels of primary outcomes at pretreatment and post-treatment for treatment completers, with mean changes and effect sizes.
| Pretreatment |
Post-treatment |
Change |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NET |
TAU |
NET |
TAU |
NET |
TAU |
|||||||||
| Outcome | n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) | n | M (SD) | gav | n | M (SD) | gav |
| Post-traumatic stress symptoms | 22 | 16 | 22 | 16 | 21 | 16 | ||||||||
| Hyperarousal | 13.4 (7.6) | 11.0 (6.5) | 10.3 (7.1) | 9.7 (5.9) | −3.52 (6.45) | 0.46 | −2.00 (5.24) | 0.32 | ||||||
| Intrusions | 12.1 (4.4) | 10.9 (5.2) | 7.5 (5.3) | 8.8 (6.5) | −4.81 (4.26) | 0.97 | −2.63 (5.44) | 0.43 | ||||||
| Avoidance | 12.8 (5.0) | 13.7 (5.8) | 10.5 (6.1) | 13.6 (5.7) | −2.00 (5.86) | 0.35 | +0.31 (5.04) | 0.05 | ||||||
| Total | 38.3 (14.4) | 35.6 (12.2) | 28.2 (15.2) | 32.1 (14.9) | −10.33 (12.70) | 0.68 | −4.31 (12.1) | 0.30 | ||||||
| Depressive symptoms | 18 | 13.1 (9.2) | 12 | 12.8 (5.0) | 14 | 13.0 (8.6) | 11 | 12.1 (6.4) | 13 | −2.08 (6.87) | 0.22 | 11 | −0.91 (3.73) | 0.14 |
| Resilience | 18 | 14.6 (4.9) | 13 | 13.3 (5.2) | 15 | 15.1 (4.1) | 11 | 15.0 (2.5) | 14 | +1.57 (3.61) | 0.32 | 11 | +2.00 (4.27) | 0.43 |
| Psychological distress | ||||||||||||||
| Self-evaluated | 18 | 14.6 (7.2) | 10 | 15.4 (5.7) | 12 | 14.7 (5.8) | 9 | 13.4 (5.2) | 12 | −2.25 (4.69) | 0.33 | 8 | −2.50 (4.63) | 0.39 |
| Guardian-evaluated | 13 | 18.0 (7.4) | 10 | 17.3 (7.3) | 10 | 15.0 (9.1) | 11 | 15.8 (5.3) | 10 | −3.10 (5.80) | 0.33 | 9 | −3.33 (5.68) | 0.50 |
NET, narrative exposure therapy; TAU, treatment as usual; gav, effect size as Hedges’ g using average variance.
Table 6.
Repeated measures analysis of variance results for changes in post-traumatic stress disorder (PTSD) (n = 39) from pretest to post-test.
| PTSD Total score |
Intrusions |
Avoidance |
Arousal |
|||||
|---|---|---|---|---|---|---|---|---|
| F | p | F | p | F | p | F | p | |
| Time | 12.93 | < .001 | 21.77 | < .001 | 1.15 | .291 | 8.15 | .007 |
| Group | 0.00 | .949 | 0.00 | .996 | 1.15 | .290 | 0.51 | .478 |
| Time*Group | 1.98 | .168 | 1.88 | .179 | 1.30 | .262 | 0.68 | .416 |
df = (1,35). PTSD Total score, Intrusions, Avoidance, and Arousal subscales of the Children’s Revised Impact of Event scale.
Table 7.
Repeated measures analysis of variance results for changes in resilience (n = 26), psychological distress reported by the child (n = 21) and guardian (n = 21), and depression (n = 25) from pretest to post-test.
| Resilience |
Psychological Distress, Self |
Psychological Distress, Guardian |
Depression |
|||||
| |
F |
p |
F |
p |
F |
p |
F |
p |
| Time | 5.14 | .033 | 4.970 | .039 | 5.940 | .026 | 1.66 | .212 |
| Group | 0.07 | .794 | 0.471 | .501 | 1.15 | .290 | 0.00 | .949 |
| Time*Group | 0.07 | .168 | 0.150 | .908 | 0.011 | .971 | 0.25 | .620 |
df: Resilience (1,23), Psychological Distress Self-Evaluated (1,18), Psychological Distress, Guardian (1,17), Depression (1,22).
We conducted further within-group analyses for PTSD symptoms, as the interventions were specifically targeted to trauma. They showed that the decrease in symptoms was significant for all PTSD symptom scales excluding Avoidance in NET, but not in the TAU group, and the effect sizes were large in NET, but small in TAU [NET: for PTSD Total score, t(20) = 3.79, p < .01, Cohen’s dz = 0.83; for Intrusions, t(20) = 5.17; p < .001, dz = 1.13; for Avoidance, t(20) = 1.56, p = .13, dz = 0.34; for Arousal t(20) = 2.59; p = .017, dz = 0.57; TAU: for PTSD Total score, t(15) = 1.46, p = .164, Cohen’s dz = 0.37; for Intrusions, t(15) = 1.93, p = .07, dz = 0.48; for Avoidance, F(15) = 0.052; p = .96, dz = 0.01; for Arousal, t(15) = 1.53; p = .148, dz = 0.38]. Figure 2 illustrates the changes in symptoms in the NET and TAU groups separately.
Figure 2.
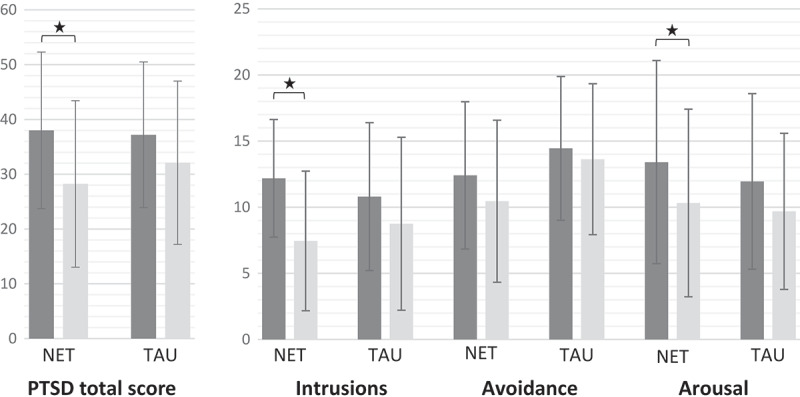
Levels of total post-traumatic stress disorder (PTSD) symptoms, and the Intrusions, Avoidance, and Arousal subscales at pretest (dark grey bars) and post-test (light grey bars). Mean group scores on the Children’s Revised Impact of Event Scale are presented, with 95% confidence intervals. NET, narrative exposure therapy; TAU, treatment as usual. *Significant difference according to t tests at p < .05.
3.3.2. Clinically significant change
At T1, 80% (16/20) of participants in the TAU group and 85% (23/27) of participants in the NET group had clinical levels of PTSD. After the intervention, the proportion of participants exceeding the cut-off level had dropped to 45% (10/22) in the NET group, while in the TAU group 75% (12/16) of participants still exceeded the cut-off. McNemar tests showed that the difference between the share of participants with clinical-level PTSD at pretest versus post-test was significant in the NET (p = .008) but not in the TAU (p = 1.00) group. Five participants in the TAU group and six in the NET group did not exceed the clinical cut-off in T1. Two (TAU) and three (NET) of them experienced a decrease in PTSD symptoms, one in the TAU group remained at the same level, and one in the NET group experienced an increase in symptoms. Three of these children were among the dropouts.
3.3.3. Intention-to-treat analyses including follow-up
In linear mixed models for PTSD symptoms, adding random intercepts and slopes and accounting for autocorrelation significantly improved model fit. Final models confirmed that PTSD symptoms decreased over time (b = −0.32, 95% CI −0.48, −0.15, SE = 0.081, p < .001). However, adding a time × treatment interaction effect did not improve model fit and the interaction was not significant. For depressive symptoms, estimation of random slopes was not possible owing to limited data. Models with random intercepts confirmed no significant effect of time or time × treatment interaction.
For resilience, random slopes or autocorrelations did not improve model fit. In a model with random intercepts, there was a trend towards an increase in resilience over time (b = 0.04, 95% CI −0.0036, 0.089, SE = 0.023, p = .070). Adding a time × treatment interaction effect did not improve model fit and the interaction was not significant.
For both self-evaluated and guardian-evaluated psychological distress, random slopes or autocorrelations did not improve model fit. In models with random intercepts, psychological distress decreased over time both when self-evaluated (b = −0.091, 95% CI −0.16, −0.09, SE = 0.033, p = .0097) and when evaluated by the guardian (b = −0.11, 95% CI −0.20, −0.11, SE = 0.045, p = .021). Adding a time × treatment interaction effect did not improve model fit for either outcome and the interactions were not significant.
3.4. Safety of interventions
Child safety was closely monitored during the interventions by the routine procedures existing at each participating clinic. None of the clients was referred to inpatient clinics during or immediately after the study and there were no suicide attempts or other serious adverse events. We asked participants about negative and positive changes during the intervention. Two participants in the TAU group and three participants in the NET group reported negative changes related to family relations during the therapy. One participant in the NET group reported negative changes related to school during the intervention. These changes were discussed with the therapist after the intervention.
4. Discussion
Millions of children and adolescents around the world suffer from post-traumatic stress symptoms due to experiences of military and/or family violence, and providing them with the most effective forms of evidence-based help is a crucial, global concern. The participants in the current study were severely traumatized. Their PTSD symptom levels were very high (83% with clinical levels of PTSD) at the start of treatment, although most (84%) had already received prior psychiatric care for their mental health problems. Refugee children in particular face atrocities, insecurity, and deprivation of basic needs, premigration, in transit, as well as postmigration (Zimmerman, Kiss, & Hossain, 2011). Earlier research has shown that such experiences increase the risk for post-traumatic symptoms (Barber, 2013; Mels, Derluyn, Broekaert, & Rosseel, 2010). We still have limited evidence, especially from randomized controlled trials (RCTs), on the effectiveness of interventions targeted at children and adolescents exposed to multiple traumas. Concerning refugee children in high-income countries, such evidence is nearly non-existent. At the same time, there is growing concern that results obtained from clinical research may not always apply to ‘real-world’ situations, because research is often carried out under artificial conditions with no active control groups (Ionnidis, 2005).
We found no evidence for superior effects of NET versus TAU on our primary outcome of reduction in levels of PTSD symptoms. However, looking at the changes observed in more detail, we found suggestions that NET was superior to TAU in some respects, although the limited follow-up measurements inhibit us from making strong conclusions. The results are promising for finding an effective tool to treat multiply traumatized children and adolescents, a patient group with whom many clinicians feel they lack suitable options. Although there was a decrease in PTSD symptoms regardless of treatment condition, within-group analyses showed that the decrease was significant in the NET group only. The effect sizes of decreases in Total PTSD and Intrusive symptoms were large with NET, but small in TAU. In addition, more participants in the NET group moved from ‘clinical’ to ‘non-clinical’ levels of symptoms at post-test. These results differ somewhat from those of Catani et al. (2009), who compared a meditation-relaxation protocol with KIDNET. That study found out that in both treatment conditions PTSD symptoms were significantly reduced, the effect sizes were large in both groups, and about the same number of children in both groups moved from ‘clinical’ to ‘non-clinical’ levels of symptoms at post-test. Since the TAU interventions in this study were resource demanding, such as family therapy and network meetings, the results are generalizable to other high-income countries but not to care environments where significantly fewer resources are available for the provision of healthcare.
A closer look at the changes showed that the difference from pretest to post-test was largest in intrusion symptoms in the NET group. Further research is needed to elucidate whether children and adolescents with flashbacks and nightmares are the ones who might especially benefit from NET or other exposure-based treatments. For the first time, this NET trial also included children and adolescents who were exposed to family violence exclusively. The finding that NET can be used and is safe among this group is important.
Psychological distress decreased and individual resilience increased in both groups, although these results must be interpreted with caution owing to the limited amount of data available for those measures. However, this can be seen as a cautious sign of more general rehabilitation among children who receive treatment for their trauma. There was no change in depressive symptoms in either group. The search for possible reciprocal effects, however, was outside the scope of the current article and should be explored in further studies with better follow-up data, such as Mauritz et al. (2016). Reduction in PTSD symptoms has been shown to lead to reductions in depression in exposure-based therapy among adolescents (McLean, Su, Carpenter, & Foa, 2015).
As suggested by the learning health system approach by the Institute of Medicine (2015), the current trial was embedded within an existing system of healthcare, aiming at a cycle in which evidence is rapidly and continually fed back into clinical care, and clinical care itself informs the further development of the intervention. However, there were unexpected difficulties in recruiting participants. The biggest obstacle expressed by the trained therapists was the timing of trauma treatment. In many cases, they considered that the child would not be ready to be exposed to his or her trauma history and it was seen as better to continue stabilization as the treatment method. However, Ter Heide, Moore, van de Schoot, and De Jongh (2016) showed that there were no differences in safety or efficacy between exposure-based therapy and stabilization as usual for refugees. This means that trauma-focused treatments are often well tolerated and can be provided for patients with multiple traumas, albeit based on individual assessment. As descriptions of the TAU methods showed, therapists in participating units do not regularly use exposure-based methods with multiply traumatized children and adolescents in Finland. This is in line with Cahill, Foa, Hembree, Marshall, and Nacash (2006), who concluded that most patients with PTSD do not receive treatments consistent with expert consensus guidelines, as well as with Pottie et al. (2011) showing that there is a mismatch between refugee adolescents’ needs and customs and the provided services. Thus, we assume that the problems in recruitment may reflect the more general hesitation concerning clinical interventions with severely and complexly traumatized children.
4.1. Limitations
The underpowered nature of the trial, high number of dropouts and missing data restrict the conclusions that can be drawn from this study. In addition, the analyses focusing mainly on the post-assessment point of time restrict the evidence for long-term effects. In two earlier NET trials among similarly aged children, recovery rates remained stable over a 6 month post-treatment period (Catani et al., 2009; Ruf et al., 2010), similar to our mixed-model-analyses including the 3 month follow-up. However, in a study by Schaal et al. (2009), the changes in symptom scores indicating long-term success of NET over an active control group were evidenced only 6 months after the treatments ended.
Another challenge for the trial was its reliance on mostly child-evaluated measures. Given the challenges faced by the parents of the participants, it was difficult to engage them in the study. However, parental report of psychological distress was included. In addition, as clinicians acted as assessors in this trial, the battery of measures and instruments had to be kept simple and manageable in scope.
The difficulties in finding eligible participants caused a challenge to the balanced block randomization (Schulz & Grimes, 2002). Irregularities in the randomization process were not identified, but cannot be completely ruled out as additional explanations for the imbalance in group sizes. However, the NET and TAU groups did not otherwise differ in the studied variables.
In the original study protocol (Kangaslampi, Garoff, & Peltonen, 2015), spontaneous recovery was planned to be controlled for by including a waiting-list control condition, utilizing the time spent in treatment queues. However, such queues did not exist at the treatment units participating in the study, and it was considered unethical to include a group with no treatment at all. This resulted in the lack of a passive control group.
Children who were included in the study based on referral and therapist’s evaluation of traumatization but did not exceed the clinical cut-off in CRIES experienced mixed results, possibly suggesting that clinical-level PTSD symptoms are an important criterion when considering trauma treatment. Unfortunately, the SUDS was not used by all therapists to ensure that exposure really happened in those sessions where it was intended to happen.
Because the participating clinicians acted as both treatment providers and assessors, blinding them to the treatment status of each participant beyond randomization (after T0) was not possible. The participants themselves could not be blinded to the intervention, as the differences between TAU and NET made it obvious to them which group they belonged to. Finally, assessment of the safety of the intervention could have included systematic reporting of side effects.
4.2. Conclusions
In typical clinical use, it appears that NET is at least as effective as trauma treatments currently in use in the Finnish healthcare system. For some severely traumatized children and adolescents, NET and other exposure-based methods may even be a superior treatment method to methods that do not include exposure. However, more research with larger samples and follow-ups are needed to confirm this finding. Close attention must be paid to the implementation of the new method. We should aim to improve clinicians’ understanding of the safety and limited risks of exposure-based methods and diminish prejudices against such methods. Peer as well as supervisory support is needed when using the method with the first clients. Increasing confidence in the effectiveness of exposure-based methods, as evidenced by many RCTs, should inform the selection of treatment approaches for multiply traumatized children and adolescents.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Barber B. K. (2013). Annual research review: The experience of youth with political conflict: Challenging notions of resilience. Journal of Child Psychology and Psychiatry, 54, 461–13. [DOI] [PubMed] [Google Scholar]
- Birleson P., Hudson I., Buchanan D. G., & Wolff S. (1987). Clinical evaluation of a self-rating scale for depressive disorder in childhood (Depression Self-Rating Scale). Journal of Child Psychology and Psychiatry, 28, 43–60. [DOI] [PubMed] [Google Scholar]
- Bornstein I., & Montgomery P. (2011). Psychological distress in refugee children: A systematic review. Clinical Child and Family Psychology Review, 14(1), 44–56. [DOI] [PubMed] [Google Scholar]
- Brewin C. R. (2014). Episodic memory, perceptual memory, and their interaction: Foundations for a theory of posttraumatic stress disorder. Psychological Bulletin, 140, 69–97. [DOI] [PubMed] [Google Scholar]
- Brewin C.R, Dalgleish T, & Joseph S. (1996). A dual representation theory of post-traumatic stress disorder. Psychological Review, 103, 670-686. doi: 10.1037/0033-295X.103.4.670 [DOI] [PubMed] [Google Scholar]
- Buchmüller T., Lembcke H., Busch J., Kumsta R., & Leyendecker B. (2018). Exploring mental health status and syndrome patterns among young refugee children in Germany. Frontiers in Psychiatry, 9, 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill S. P., Foa E. B., Hembree E. A., Marshall R. D., & Nacash N. (2006). Dissemination of exposure therapy in the treatment of posttraumatic stress disorder. Journal of Traumatic Stress, 19, 597–610. [DOI] [PubMed] [Google Scholar]
- Catani C., Kohiladevy M., Ruf M., Schauer E., Elbert T., & Neuner F. (2009). Treating children traumatized by war and tsunami: A comparison between exposure therapy and meditation relaxation in North-East Sri Lanka. BMC Psychiatry, 9, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Arellano R., Lyman D. R., Jobe-Shields L., George P., Dougherty R. H., Daniels A. S., … Delphin-Rittmon M. E. (2014). Trauma-focused cognitive behavioral therapy: Assessing the evidence. Psychiatric Service, 65(5), 591–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong M., Anda R. F., Felitti V. J., Dube S. R., Williamson D. F., Thompson T. J., … Giles W. H. (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse & Neglect, 28, 771–784. [DOI] [PubMed] [Google Scholar]
- Duke N., Pettingell S. L., McMorris B. J., & Borowsky I. W. (2010). Adolescent violence perpetration: Associations with multiple types of adverse childhood experiences. Pediatrics, 125, 778–786. [DOI] [PubMed] [Google Scholar]
- Ertl V., Pfeiffer A., Schauer E., Elbert T., & Neuner F. (2011). Community-implemented trauma therapy for former child soldiers in Northern Uganda: A randomized controlled trial. JAMA, 306, 503–512. [DOI] [PubMed] [Google Scholar]
- Evans S. E., Davies C., & DiLillo D. (2008). Exposure to domestic violence: A meta-analysis of child and adolescent outcomes. Aggression and Violent Behavior, 13, 131–140. [Google Scholar]
- Foa E. B., Hupper J. D., & Cahill S. P. (2006). Emotional processing theory: An update In Rothbaum B. O. (Ed.), Pathological anxiety: Emotional processing in etiology and treatment. (pp. 3-24). New York, NY: Guilford Press. [Google Scholar]
- Gandham S., Gunasekera H., Isaacs D., & Britton M. A. (2017). High prevalence of symptoms of post-traumatic stress in children of refugee and asylum seeker backgrounds. Journal of Pediatrics and Child Health, 53. doi: 10.1111/jpc.13596 [DOI] [Google Scholar]
- Garoff Kangaslampi, S, & Peltonen K. (2015). Narrative exposure therapy for immigrant children traumatized by war: study protocol for a randomized controlled trial of effectiveness and mechanisms of change. Bmc Psychiatry, 15, 127-141. doi: 10.1186/s12888-015-0520-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies D., Taylor F., Gray C., O’Brien L., & D’Abrew N. (2012). Psychological therapies for the treatment of posttraumatic stress disorder in children and adolescents. Cochrane Database Systematic Review, (12), CD006726. [DOI] [PubMed] [Google Scholar]
- Goodman R. (1997). The strengths and difficulties questionnaire: a research note. Journal of Child Psychology and Psychiatry, 38, 581–586. doi: 10.1111/jcpp.1997.38.issue-5 [DOI] [PubMed] [Google Scholar]
- Halvorsen J. Ø., Stenmark H., Neuner F, & Nordahl H. M (2014). Does dissociation moderate treatment outcomes of narrative exposure therapy for ptsd? a secondary analysis from a randomized controlled clinical trial. Behaviour Research and Therapy, 57, 21-28. doi: 10.1016/j.brat.2014.03.010 [DOI] [PubMed] [Google Scholar]
- Horowitz M. (1986). Stress response syndromes (2nd ed.). New York, NY: Jason Aronson; 1986. [Google Scholar]
- Institute of Medicine (2015). The learning health system series. 2015 [cited 2018. 4 October]; Available from: http://www.nap.edu/catalog/13301/the-learning-health-system-series
- Ionnidis J.P.A. (2005). “Why most published research findings are false”. PLoS Medicine, 28:e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson H., & Thompson A. (2008). The development and maintenance of post-traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: A review. Clinical Psychology Review, 28, 36–47. [DOI] [PubMed] [Google Scholar]
- Kangaslampi S. Garoff, F., & Peltonen K. (2015). Narrative exposure therapy for immigrant children traumatized by war: study protocol for a randomized controlled trial of effectiveness and mechanisms of change. BMC Psychiatry, 15, 127-141. doi: 10.1186/s12888-015-0520-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauritz M. W., Van Gaal B. G. I., Jongedijk R. A., Schoonhoven L., Nijhuis-van der Sanden M. V. G., & Goossens P. J. J. (2016). Narrative exposure therapy for posttraumatic stress disorder associated with repeated interpersonal trauma in patients with severe mental illness: A mixed methods design. European Journal of Psychotraumatology, 7, 32473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean C. P., Su Y.-J., Carpenter J. K., & Foa E. B. (2015). Changes in PTSD and depression during prolonged exposure and client-centered therapy for PTSD in adolescents. Journal of Clinical Child and Adolescent Psychology, 46, 500–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherson J. (2012). Does narrative exposure therapy reduce PTSD in survivors of mass violence? Research on Social Work Practice, 22, 29–42. [Google Scholar]
- Mels C., Derluyn I., Broekaert E., & Rosseel Y. J. (2010). The psychological impact of forced displacement and related risk factors on Eastern Congolese adolescents affected by war. Child Psychology and Psychiatry, 10, 1096–1104. [DOI] [PubMed] [Google Scholar]
- Mørkved N, Hartmann K, Aarsheim L.M, Holen D, Milde A.M, Bomyea J, & Thorp S.R (2014). A comparison of narrative exposure therapy and prolonged exposure therapy for ptsd. Clinical Psychology Review, 34,453-67. doi: 10.1016/j.cpr.2014.06.005 [DOI] [PubMed] [Google Scholar]
- Mørkved N., & Thorp S. R. (2018). The treatment of PTSD in an older adult Norwegian woman using narrative exposure therapy: A case report. European Journal of Psychotraumatology, 16, 1414561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peltonen K. (2015). Narratiivinen altistusterapia. Retrieved from https://ammattilaiset.mielenterveystalo.fi/Sivut/etusivu.aspx
- Pinheiro J., Bates D., DebRoy S., Sarkar D., & R Core Team (2018). nlme: Linear and nonlinear mixed effects models. R package version, 3.1-137, Retrieved from https://CRAN.R-project.org/package=nlme
- Pottie K., Greenaway C., Feightner J., Welch V., Swinkels H., Rashid M., … Refugee H. (2011). Evidence-based clinical guidelines for immigrants and refugees. Canadian Medical Association Journal, 183, E824–E925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2017). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from https://www.r-project.org/ [Google Scholar]
- Robjant K., & Fazel M. (2010). The emerging evidence for narrative exposure therapy: A review. Clinical Psychology Review, 30, 1030–1039. [DOI] [PubMed] [Google Scholar]
- Rossman B. B., Hughes H. M., & Rosenberg M. S. (2000). Children and interparental violence: The impact of exposure. Philadelphia, PA: Brunner, Mazel. [Google Scholar]
- Ruf M., Schauer M., Neuner F., Catani C., Schauer E., & Elbert T. (2010). Narrative exposure therapy for 7- to 16-year-olds: A randomized controlled trial with traumatized refugee children. Journal of Traumatic Stress, 23, 437–445. [DOI] [PubMed] [Google Scholar]
- Schaal S., Elbert T., & Neuner F. (2009). Narrative exposure therapy versus interpersonal psychotherapy. Psychotherapy and Psychosomatics, 78, 298–306. [DOI] [PubMed] [Google Scholar]
- Schauer M., Neuner F., & Elbert T. (2011). Narrative exposure therapy: A short-term treatment for traumatic stress disorders. (2nd ed.). Göttingen, Germany: Hogrefe. [Google Scholar]
- Schauer M., Neuner F., & Elbert T. (2017). Narrative Exposure Therapy for Children and Adolescents (KIDNET) In M. A. Landolt, M. Cloitre, & U. Schnyder (Eds.), Evidence-based treatments for trauma related disorders in children and adolescents (pp. 227–249). Switzerland: Springer International. [Google Scholar]
- Schulz K. F., & Grimes D. A. (2002). Generation of allocation sequences in randomised trials: Chance, not choice. Lancet, 359, 515–519. [DOI] [PubMed] [Google Scholar]
- Smith P., Perrin S., Dyregrov A., & Yule W. (2003). Principal components analysis of the Impact of Event Scale with children in war. Personality and Individual Differences, 34, 315–322. [Google Scholar]
- Stallard P. (2006). Psychological interventions for post-traumatic reactions in children and young people: A review of randomised controlled trials. Clinical Psychology Review, 26(7), 895–911. [DOI] [PubMed] [Google Scholar]
- Ter Heide J. J., Moore T. T. M., van de Schoot R., & De Jongh A. (2016). Eye movement desensitisation and reprocessing therapy v. stabilisation as usual for refugees: Randomised controlled trial. The British Journal of Psychiatry, 209(4), 311–318. [DOI] [PubMed] [Google Scholar]
- Thorpe K. E., Zwarenstein E., Oxman A. D., Treweek S., Furberg C. D., Altman D. G., … Chalkidou F. (2009). A Pragmatic–Explanatory Continuum Indicator Summary (PRECIS): A tool to help trial designers. Journal of Clinical Epidemiology, 62, 464–475. [DOI] [PubMed] [Google Scholar]
- Ungar M., & Liebenberg L. (2011). Assessing resilience across cultures using mixed methods: Construction of the child and youth resilience measure. Journal of Mixed Methods Research, 5, 126–149. [Google Scholar]
- Zimmerman C., Kiss L., & Hossain M. (2011). Migration and health: A framework for 21st century policy-making. PLoS Medicine, 8, e1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwarenstein M., Treweek S., Gagnier J. J., Altman D. G., Tunis S., Haynes B., … Moher D. (2008). Improving the reporting of pragmatic trials: An extension of the CONSORT statement. BMJ, 337, 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]


