ABSTRACT
Objectives: To preliminarily investigate in patients with a primary complaint of non-acute knee pain for ≥ 1 month: 1) the proportion of patients with non-acute knee pain classified by Mechanical Diagnosis and Therapy (MDT) as Spinal Derangements, 2) the number of sessions taken to identify the concluding classification, and 3) the ability of MDT classifications, demographics, and symptomatic baselines to predict pain reduction at 1-month follow-up.Methods: This study reviewed data from outpatients managed with MDT. For modeling knee pain reduction at the 1-month follow-up, 3 MDT provisional or concluding classifications (Spinal Derangement, Knee Derangement, and Non-Derangement) and the following variables were included: 1) gender, 2) symptom duration, 3) presence of low back pain (LBP), 4) the Japanese Knee Osteoarthritis Measure, 5) average pain intensity at the initial session using a 0–10 numerical rating scale, and 6) the Kellgren–Lawrence grade.Results: Data from 101 patients were extracted. The percentage of patients with the concluding classification of Spinal Derangement was 44.6%. This was greater in those patient’s reporting concomitant LBP (p = .002) and without radiographic findings of knee osteoarthritis (p < .001). A concluding classification was determined by the fourth session in 80% of patients. Multiple regression modeling demonstrated that only the concluding classification significantly predicted the knee pain reduction at the 1-month follow-up.Discussion: These findings suggest the importance of careful screening assessments of the lumbar spine and the importance of detecting Derangements throughout the follow-up sessions for patients with a primary complaint of knee pain.
KEYWORDS: Classification, cohort studies, knee, lumbar spine, McKenzie, musculoskeletal pain, physical therapy specialty, self-care
Background
The McKenzie Method of Mechanical Diagnosis and Therapy (MDT) is a conservative classification and treatment-based system for musculoskeletal disorders. MDT focuses on mechanical loading strategies and patient education within a psychosocial framework [1,2]. While MDT is reported as the most commonly used approach for spinal conditions [3–5], its application to extremity problems is less well recognized. However, research has been ongoing [6] addressing the application of MDT to the knee. Rosedale et al. [7] reported a randomized controlled trial (RCT) using patients with knee osteoarthritis and Lynch and May [8] reported a case study using a patient with an apparent meniscal injury. In MDT, management strategies are guided by the identification of specific subgroups that respond to a specific management strategy. There have been several reliability studies examining the agreement of subgroup classification between therapists [9–12]. It is argued that identifying a subgroup is useful to maximize therapeutic effectiveness [13,14] as the average treatment effect is modest when patients are treated as if they are a homogeneous group [13]. It is well understood that there is an unclear relationship between pathoanatomy and symptoms, and the prevalence of pathology in asymptomatic individuals is widely reported [15–17]. Hence, when MDT algorithms are utilized to identify subgroups, it is not pathoanatomy but symptom and functional responses to mechanical loadings that are used as primary factors for decision-making. MDT focuses on identifying appropriate management strategies using specific subgroups rather than on attempting to identify an underlying pathoanatomical cause of the symptoms.
Six classifications (with various subgroups included) can be considered in the MDT evaluation for extremity pain, features of each are detailed elsewhere [12,18,19]. Of particular interest is the classification of the Derangement Syndrome, where mechanical loading in a specific direction, termed the ‘directional preference’ (DP), results in symptomatic and functional improvements that rapidly occur and last after loading. Thus, early identification of the Derangement Syndrome in the spine (Spinal Derangement) and the knee (Knee Derangement) should result in improved treatment efficacy and cost-effectiveness. For the purposes of this study, the classification of Spinal Derangement is made when spinal DP exercises, sustained loading and/or hands-on techniques results in an improvement of knee symptoms, functional baselines, and, ultimately, improved outcomes. Similarly, with a Knee Derangement, mechanical loading to the knee in the DP results in improvement of knee symptoms, functional levels, and ultimately improved outcomes.
In the MDT evaluation algorithm, the possibility of a Spinal Derangement causing the patient’s reported extremity pain is explored first. In a case study, Menon and May [20] reported on a patient diagnosed with an magnetic resonance imaging (MRI) confirmed rotator cuff tear referred to therapy by their physician. Following a mechanical evaluation of the cervical spine, the problem was classified as a Spinal Derangement and the patient completely resolved with purely mechanical loading to the cervical spine. As illustrated in this case study, it may not be uncommon for an extremity problem to be diagnosed and referred to physiotherapy for management, especially if the patient has no spinal symptoms and with abnormal imaging that correspond with the patient’s complaint. It would, therefore, be important to undertake a careful screening of the spine for patients with an extremity complaint to provide patients with effective management. It is unknown what percentage of patients with a primary complaint of knee pain, who are classified as Spinal Derangements, have abnormal knee imaging or have no complaint of low back pain (LBP). Investigating such proportions would provide useful information for clinicians in regard to the importance of spinal screening in patients with primary knee pain. If the proportion was significant, this would also discourage choosing a management strategy based on imaging findings alone as pathological findings do not always correspond with symptoms [15–17].
In MDT, detailed assessments of the extremity are undertaken after the MDT screening for a Spinal Derangement. Therefore, it may take several sessions for MDT therapists to be clear regarding the patient’s presentation and response before concluding on a classification. Heidar Abady et al. [21] in a cohort study reported that 36.6% of patients with shoulder pain had a change in classification over the course of treatment. It is unknown how many sessions it took to identify a concluding classification. Such information would be useful for clinician’s in their decision-making and, therefore, should be investigated.
It is hypothesized that patients with a primary complaint of knee pain with a Spinal Derangement or a Knee Derangement would obtain better treatment effects than patients in other classifications (Non-Derangement) since mechanical loading in the DP rapidly results in symptomatic and functional improvements in the Derangement Syndrome. However, it is unknown if demographics or symptomatic baselines outcomes can also predict pain relief through MDT for patients with non-acute knee pain. It would be ideal to include a wait-and-see intervention group with an RCT design to fully understand the contributing factors resulting in pain relief, because spontaneous recovery may occur, particularly in the acute-phase (<1 month) [22]. However, RCTs require substantial cost and effort and it is prudent to undertake a preliminary study with other designs to identify promising factors to develop a final prediction model.
Thus, the purpose of this study was to preliminarily investigate the following five questions: (1) What is the percentage of patients who are classified as having a Spinal Derangement as a cause of their non-acute knee pain?; (2) How many patients classified as having a Spinal Derangement have current LBP?; (3) How many patients classified as Spinal Derangement have abnormalities on knee imaging?; (4) How many sessions are needed to identify a concluding classification for patients with non-acute knee pain?; and (5) Can variables related to demographics, symptoms and MDT provisional, and concluding classification predict a change in reported pain levels in patients managed with MDT with non-acute knee pain?
Methods
Design overview
The study design was a retrospective chart review. Pre-recorded medical records in the Minami Shinjuku Orthopedic Clinic from March 2012 to December 2016 were reviewed. The Minami Shinjuku Orthopedic Clinic is a certified McKenzie clinic in Japan, where MDT is routinely used. The patients’ identifying information was not used in this study and ethical approval was granted by the Saitama Prefectural University.
Patients
Eligibility criteria for patients for the current chart review were: 1) outpatients with a primary complaint of knee pain, seen in the Minami Shinjuku Orthopedic Clinic, 2) knee pain lasting for more than 1 month, and 3) undertaking MDT for two or more sessions. Patients with a history of surgical intervention for the spine or knee, patients with knee pain following trauma, including a fracture or ligament injury, and patients with any infection of the knee or spine were not considered eligible. Patients with a change of medication or having an intra-articular injection over the course of MDT intervention were also not considered eligible as the change of medications or intra-articular injections could have affected the knee symptoms over the course of the MDT interventions.
Interventions and MDT classifications
Evaluations and interventions were undertaken by three credentialed MDT therapists, who the McKenzie Institute International certifies as having at least a minimum level of skill in MDT and/or a diploma MDT therapist, who the McKenzie Institute International certifies as having the highest level of skill in MDT. The evaluation and interventions were 20–60 min per session. For the purposes of this study, two classifications of Spinal Derangement and Knee Derangement were used, along with one ‘Non-Derangement’ classification. The Derangements were further subgrouped that are dependent upon their DP; Spinal Derangement with a DP of extension, Spinal Derangement with a DP of flexion, Spinal Derangement with a DP of lateral, Knee Derangement with a DP of extension, and Knee Derangement with a DP of flexion. The ‘Non-Derangement’ classifications included Knee Contractile Dysfunction, Knee Articular Dysfunction, and OTHERs. For the purposes of this study, subgroups of the OTHERs were designated as one classification, as not all MDT therapists had been using the latest MDT extremity classifications of OTHER published in 2016 [12]. MDT assessments and treatments were undertaken, and a provisional classification was determined at the initial consultation. MDT assessments and treatments are composed of a detailed history and physical examination, including observation of symptoms and mobility in response to mechanical loading to the problem area. In this study, baselines including pain, range of motion, and function were assessed with all patients. Subsequently, they undertook screening assessments using mechanical loading to the lumbar spine before the knee. Knee symptoms and mobility were used as baselines to determine the classification. Details of the mechanical loading strategies are explained in a previous study [7]. When a DP was found, Derangement Syndrome was diagnosed and self-treatment exercises with the mechanical loading in the DP were prescribed. When a DP was not found, the most likely provisional classification was chosen taking into account the history and the response to loading strategies in the physical examination. Appropriate management was given dependent upon the specific classification. For example, if a Knee Contractile Dysfunction was diagnosed, a progressive resisted strategy for the contractile tissue would be initiated. The MDT therapist had a chance to alter the classification based on the patient’s symptom and functional changes at each follow-up. The concluding classification in this study was confirmed when a clear management strategy was determined and no further change of the classification was undertaken through the course of MDT management.
Other outcome measures
Any change in the MDT classifications throughout the course of MDT was noted. The number of sessions taken to identify a concluding classification was extracted.
Average knee pain intensity over 24 h was assessed with the 0–10 Numerical Rating Scale (NRS) (0, no pain; 10, pain as bad as it could be). At each session, NRS was assessed immediately before initiating evaluations and treatments. Knee pain NRS data were extracted at the following time points: 1) before the initial consultation and 2) 1 month after the initial consultation. When NRS data were only available before the initial consultation due to discharge before the 1-month follow-up, the NRS at the 1-month follow-up were inputted with the NRS at the time of discharge.
A plain radiograph was routinely taken and the severity of knee osteoarthritis was evaluated using the Kellgren–Lawrence grade for knee osteoarthritis [23] by an experienced orthopedic surgeon (SH). Considering the original cut-off of Grade 2 for the diagnosis of knee osteoarthritis, a 4-grading system was used in the current study: Grade 0–1, Grade 2, Grade 3 and Grade 4. In patients with MRI of the knee, data of any meniscus tear and cartilage pathology (except degenerative changes) were extracted, though no scoring was undertaken. Diagnosis was made by an experienced orthopedic surgeon (SH) and a radiologist. The findings were presented to both the patient and the therapist.
In regression modeling for research question five, the three MDT provisional or concluding classifications (Spinal Derangement, Knee Derangement, Non-Derangement) were used as independent variables (MDT classification variables). The following demographics and symptom variables were also included as independent variables: 1) age, as it is a potential effect modifier [24], 2) symptom duration, 3) presence of LBP, 4) Japanese Knee Osteoarthritis Measure (JKOM) at the initial intervention, 5) the NRS at the initial consultation, and 6) the Kellgren–Lawrence grade for the knee osteoarthritis. Kellgren–Lawrence grade may influence symptom change overtime although it does not predict symptom severity [25]. The JKOM is a reliable and valid self-reporting questionnaire including 25 items (e.g. pain in level walking, standing or climbing stairs, physical function related to activities of daily living and social functioning) [26]. Low total scores indicate good function. The dependent variable was the percentage reduction of the NRS at 1-month follow-up. When patients were discharged before the 1-month follow-up, the percentage reduction of the NRS at 1-month follow-up was calculated using the NRS at the time of discharge.
Additionally, the number of patients taking medication for their knee complaint or having received an intra-articular injection over the course of MDT intervention was noted for supplemental data.
Data analysis
Descriptive statistics were used to summarize characteristics of the patients. SPSS version 21.0 (IBM Corporation, New York, USA) was used for statistical analyses. Alpha value was set at 5% unless specified.
For research questions 1–3, a two-tailed Fisher’s Exact test was used to compare proportions of Spinal Derangements between patients with and without LBP, with and without the Kellgren–Lawrence grades ≥2, and with and without abnormality on the knee MRI in either the provisional or concluding classification as long as each cell was greater than zero. For research question four, the cumulated proportion of the patients with a concluding classification was plotted over sessions. For research question five, the multiple imputation technique was used for missing values. A multiple regression model was built to investigate whether the MDT classification variables and the demographic and symptom variables contributed to the percentage reduction of the NRS at 1-month follow-up. Univariate regression analysis was run between the percentage reduction of the NRS at 1-month follow-up and demographics and symptom variables to minimize independent variables for final modeling. Demographics and symptom variables with a p-value of ≥.1 were excluded from the final modeling.
Results
Data of 101 patients were extracted. There were 27 instances of missing data for the JKOM. Most patients (68.3%) did not take medication or have an intra-articular injection over the course of the MDT intervention (Appendix 1). No patients reported increased NRS over 1 month.
Research question 1
Table 1 presents the characteristics of the patients. A concluding classification of Spinal Derangement was seen in 44.6% of 101 patients with a primary complaint of non-acute knee pain.
Table 1.
Demographics of the 101 patients with knee pain.
| Age (yr), mean (SD) | 56.4 (14.5) |
| Gender, n males (%) | 36 (35.6) |
| Symptom duration (mo), mean (SD) | 20.9 (35.2) |
| Presence of low back pain, n (%) | 52 (51.5) |
| Japanese Knee Osteoarthritis Measure (0–100), mean (SD)* | 25.7 (17.9) |
| NRS of average pain intensity at the initial consultation (0–10), mean (SD) | 5.6 (2.1) |
| NRS of average pain intensity at the 1-month follow-up (0–10), mean (SD)† | 2.7 (2.1) |
| Kellgren–Lawrence grading scale | |
| Grade 0–1, n (%) | 63 (61.8) |
| Grade 2, n (%) | 17 (16.7) |
| Grade 3, n (%) | 16 (16.6) |
| Grade 4, n (%) | 5 (4.9) |
| Patients with Magnetic Resonance Imaging | 23 (22.8) |
| Negative finding of abnormality on Magnetic Resonance Imaging | 2 (8.7†) |
| Positive finding of abnormality on Magnetic Resonance Imaging | 21 (91.3†) |
| MDT concluding subgroup | |
| Spinal Derangement with directional preference of extension, n (%) | 35 (34.7) |
| Spinal Derangement with directional preference of flexion, n (%) | 1 (1.0) |
| Spinal Derangement with directional preference of lateral, n (%) | 9 (8.9) |
| Knee Derangement with directional preference of extension, n (%) | 19 (18.8) |
| Knee Derangement with directional preference of flexion, n (%) | 8 (7.9) |
| Knee Contractile Dysfunction, n (%) | 4 (3.9) |
| Knee Articular Dysfunction, n (%) | 3 (3.0) |
| OTHERs, n (%) | 22 (21.8) |
NRS = Numerical Rating Scale, MDT = Mechanical Diagnosis and Therapy.
*n = 74
†out of n = 23
Research question 2
In regard to the presence of LBP, there was no difference in the proportion of patients with a provisional classification of Spinal Derangement (p = .19) but a difference in the proportion of patients with the concluding classification of Spinal Derangement (p = .002) (Table 2).
Table 2.
Proportions of patients with Derangement Syndrome of the spine as the provisional or concluding classification considering presence/absence of low back pain.
| Provisional or concluding classification of Spinal Derangement | Provisional classification of Spinal Derangement, n (%) | Concluding classification of Spinal Derangement, n (%) |
|---|---|---|
| Patients without low back pain (n = 49) |
36 (73.5) | 14 (28.6) |
| Patients with low back pain (n = 52) |
43 (82.7) | 31 (59.6) |
Research question 3
For the presence of the Kellgren–Lawrence grades ≥2, there was no difference in the proportion of patients with the provisional classification of Spinal Derangement (p = .19) but a difference in the proportion of patients with a concluding classification of Spinal Derangement (p < .001). The statistical test was not undertaken for the presence of any knee MRI abnormality, as one cell was zero in the cross-table (Table 3). Detailed information is presented in Appendix 2.
Table 3.
Proportions of patients with Derangement Syndrome of the spine as the provisional or concluding classification considering presence/absence of abnormalities on knee imaging.
| Provisional or concluding classification of Spinal Derangement | Provisional classification of Spinal Derangement, n (%) | Concluding classification of Spinal Derangement, n (%) |
|---|---|---|
| Patients with the Kellgren–Lawrence grades ≥2 (n = 38) | 32 (84.2) | 8 (21.1) |
| Patients with the Kellgren-Lawrence grades 0–1 (n = 63) | 47 (74.6) | 37 (58.7) |
| Patients with positive finding of abnormality on Magnetic Resonance Imaging (n = 21) | 14 (66.7) | 7 (33.4) |
| Patients with negative finding of abnormality on Magnetic Resonance Imaging (n = 2) | 2 (100) | 2 (100) |
Research question 4
Figure 1 presents the cumulated proportion of the 101 patients with a concluding classification over the MDT sessions. A concluding MDT classification was determined by the fourth session in more than 80% of 101 patients.
Figure 1.
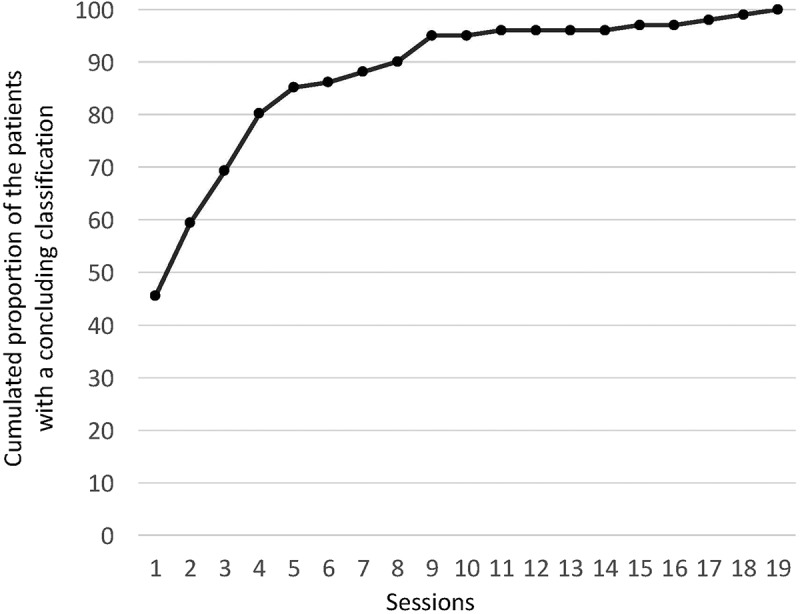
Sessions to achieve a concluding mechanical diagnosis and therapy classification.
Research question 5
In the univariate regression analyses for the percentage reduction of the NRS at 1-month follow-up, the criteria for the final modeling were satisfied for symptom duration (r = −0.36, p < .001) and the Kellgren–Lawrence grade (r = −0.37, p < .001).
Modeling with the MDT provisional classification, symptom duration and the Kellgren–Lawrence grade explained a significant proportion of variance in the percentage reduction of the NRS at 1-month follow-up, R2 = 0.45, F(4, 96) = 6.22, p < .001. The analysis showed that the percentage reduction of the NRS at 1-month follow-up was significantly predicted by symptom duration (β = −0.007, t(96) = −2.30, p = .02) and by the Kellgren–Lawrence grade (β = −8.46, t(96) = −2.27, p = .02). However, the analysis showed that MDT provisional classification did not significantly predict the percentage reduction of the NRS at 1-month follow-up: β = 10.22, t(96) = 8.21, p = .21 (Spinal Derangement); β = 24.21, t(96) = 13.01, p = .06 (Knee Derangement) for dummy variables of the Spinal Derangement and Knee Derangement and β = −14.00, t(96) = 11.20, p = .21 (Spinal Derangement); β = −24.21, t(96) = 13.01, p = .06 (Non-Derangement) for dummy variables of the Spinal Derangement and Non-Derangement. A post-hoc power analysis for the regression model comprised of MDT provisional classification, symptom duration and Kellgren–Lawrence grade for our 101 patients was 99%.
Modeling with the MDT concluding classification, symptom duration and the Kellgren–Lawrence grade explained a significant proportion of variance in the percentage reduction of the NRS at 1-month follow-up, R2 = 0.60, F(4, 96) = 13.72, p < .001. The analysis showed that the percentage reduction of the NRS at 1-month follow-up was not significantly predicted by symptom duration (β = −0.004, t(96) = −1.34, p = .18) and by the Kellgren–Lawrence grade (β = −2.39, t(96) = −0.68, p = .50). However, the analysis showed that the MDT concluding classification significantly predicted the percentage reduction of the NRS at 1-month follow-up: β = 39.60, t(96) = 7.62, p < .001 (Spinal Derangement); β = −18.84, t(96) = −7.71, p = .01 (Knee Derangement) for dummy variables of the Spinal Derangement and Knee Derangement and β = 20.75, t(96) = 6.53, p = .001 (Spinal Derangement); β = −18.84, t(96) = 7.71, p = .01 (Non-Derangement) for dummy variables of the Spinal Derangement and Non-Derangement. A post-hoc power analysis for the regression model comprised of MDT concluding classification, symptom duration and Kellgren–Lawrence grade for our 101 patients was 99%.
As a post-hoc analysis, the percentage reduction of the NRS at 1-month follow-up was compared among the three MDT concluding classifications using the one-way ANOVA with post-hoc analyses using Bonferroni corrections (Table 4). There were significant differences (p < .05) in the percentage reduction of the NRS at 1-month follow-up between Spinal Derangement, Knee Derangement, and Non-Derangement.
Table 4.
Results of the one-way ANOVA and post-hoc analyses using the Bonferroni corrections for the % reduction of the NRS at 1-month follow-up between the three concluding MDT subgroups.
| Primary outcome measure | Spinal Derangement (n = 45) | Knee Derangement (n = 28) | Non-Derangement (n = 28) |
|---|---|---|---|
| % reduction of the NRS at 1-month follow-up, mean (SD) | 68.8 (25.7) | 49.0 (32.5) | 24.4 (24.4) |
NRS = Numerical Rating Scale
One-way ANOVA for the 1-month % reduction of pain, F(2,98), p < .001.
Spinal Derangement vs Knee Derangement in the % reduction of the NRS at 1-month follow-up; p = .01 (95CIs of differences: 3.7 to 35.9).
Spinal Derangement vs Non-Derangement in the % reduction of the NRS at 1-month follow-up; p < .001 (95CIs of differences: 28.4 to 60.5)
Knee Derangement vs Non-Derangement in the % reduction of the NRS at 1-month follow-up; p = .003 (95CIs of differences: 6.8 to 42.5)
Discussion
The current study suggests that a spinal screening assessment in the non-acute knee pain population may provide useful information for identifying a concluding classification. The results of each research question provide the foundation for future studies.
Research questions 1–3
Notably, 44.6% of patients with a primary complaint of non-acute knee pain responded to mechanical loading to the lumbar spine and were categorized into the concluding subgroup of the Spinal Derangement regardless of the presence of LBP and pathologic findings on imaging. Not surprisingly, the percentage of the Spinal Derangement is greater in individuals with LBP than ones without LBP and in individuals with negligible pathologic findings on imaging than ones with apparent pathologic findings. These findings indicate that knowledge of a history of LBP and of imaging findings would be meaningful for the clinical reasoning process to identify the concluding classification of Spinal Derangement.
In 28.6% of patients, the concluding classification was a Spinal Derangement with the patients reporting no LBP. In 21.1% of patients, the concluding classification was a Spinal Derangement and the Kellgren–Lawrence grade was ≥ 2. In 33.4% of patients with a positive finding of abnormality on MRI, the concluding classification was Spinal Derangement. These percentages are not negligible.
The potential reasons for this finding of knee pain of apparent spinal origin are unclear and not the focus of the current study, but the following three possibilities may be considered. There may be a contribution from the altered mechanical loading to the knee by changing dynamic alignment of the lumbar spine through repeated mechanical loading. As a second possibility, Yabuki and Kikuchi [27] and Kunoki et al. [28] reported on contributions of the L4 nerve root to painful knee osteoarthritis. Thus, it may be possible that the knee pain that responded to mechanical loading primarily to the lumbar spine actually originated from the lumbar spine. The third possibility is the contribution of a hypoalgesic effect of applying mechanical loading to the spine on the knee pain. A systematic review demonstrated hyperalgesia in people with knee osteoarthritis [29] and discussed the hypoalgesic effect of spinal mobilization [30].
Research question 4
Approximately 55% of patients had their classification changed between the initial consultation and discharge. This finding may explain why inter-examiner reliability for the provisional MDT classification at one session in a successive reliability designed study was poor [12]. It was found that the number of patients with a concluding classification increased over the first few sessions. These findings indicate the importance of determining the concluding classification through follow-up sessions rather than just at the initial session. The current study should provoke discussion and be a stimulus for further research regarding the accuracy of identifying a treatment classification in just one session [31–36].
The cumulated proportion of the patients with a concluding MDT classification increased to 80% in the first four sessions. This finding indicates that classification becomes clarified overtime in MDT as it does in clinical practice guidelines that recommend monitoring changes in the patient’s status throughout the course of treatment [37,38]. However, the cumulated proportion increased only 10% over the following five sessions and generally plateaued after the 10th session. It is unclear whether confirmation of the concluding classification in 80% of patients at the fourth session and in 90% at the ninth session is appropriate or whether this is an issue in clinical practice.
Research question 5
The current study found that neither the MDT provisional classification nor the demographic and symptom variables could predict the % reduction of the NRS at 1-month follow-up, only the concluding classification was predictive. Further, the percentage reduction of the NRS at 1-month follow-up was the greatest when the concluding classification was Spinal Derangement, followed by Knee Derangement and least in the Non-Derangement classification. These findings indicate the importance of exploring the possibility of Derangement Syndrome first to maximize the efficiency and efficacy of the treatment. These findings also reinforce the importance of utilizing a system that has ongoing evaluations to determine the concluding classification through follow-up sessions.
A greater percentage reduction of the NRS at 1-month follow-up in the classification of Derangement Syndrome compared with Non-Derangement classification is not surprising since mechanical loading in the DP rapidly results in symptomatic and functional improvements in the Derangement Syndrome. Caution is required not to overinterpret the results that MDT is not effective for patients with Non-Derangement classification. A RCT in patients with knee OA demonstrated that MDT interventions generally resulted in improved symptoms and function in patients with Non-Derangement classification, although the effect size in comparison with a wait-and-see control intervention was small [7]. Non-Derangement classification is a mixture of MDT OTHER subgroups, which require specific matched intervention and some may require a specialist referral. Further research is needed to validate the matched intervention proposed for these OTHER subgroups.
Limitations
The current study was a retrospective chart review and has weaknesses in regard to methodological robustness. Due to the study design, it is unclear if factors other than MDT might have contributed to the reduction of the knee pain, such as a spontaneous pain recovery and drag effects. However, patients with acute knee pain were not included in the retrospective chart review and most patients did not take medications. Thus, it is likely that mechanical loading to the lumbar spine contributed to the reduction of knee pain in those patients classified as Spinal Derangement. A second limitation is that the patients managed by MDT for only one session were not included in the current study, and this may have led to selection bias. A careful interpretation would be required for generalizability of the findings to other countries, but the authors believe data in the current study would reflect clinical practice at least in Japan. The current study also did not include all potential variables that may be useful for the prediction of a treatment effect. For example, it has been known that psychosocial factors could be relevant for prognosis [39,40]. A number of tools have been developed to predict the treatment effect and their usefulness has been shown in certain populations [41–44]. A well-designed study will be required to investigate factors relevant to the best responsive populations using MDT. Finally, the concluding classification in this study was determined when a clear management strategy was established and no further correction of the classification was made through the course of MDT management. However, it is clinically impossible to guarantee if the concluding classification was correct due to the lack of an established gold standard. Nevertheless, the classification was undertaken by the certified MDT therapists and the authors believe the concluding classification was correct at least with the 3-classification system (Spinal Derangement, Knee derangement, and Non-Derangement) and with the eight classification system (Spinal Derangement with a DP of extension, Spinal Derangement with a DP of flexion, Spinal Derangement with a DP of lateral component, Knee Derangement with a DP of extension, Knee Derangement with a DP of flexion, Knee Contractile Dysfunction, Knee Articular Dysfunction, and OTHERs) in the current study.
Conclusion
In the current study, 44.6% of patients with primary complaints of non-acute knee pain were classified with the concluding MDT classification of Spinal Derangement. Further, the percentage of Spinal Derangements was greater in individuals with LBP than those without LBP and in individuals with negligible pathologic findings on knee imaging than those with apparent pathologic findings on images. Four sessions were required to obtain a concluding MDT classification in more than 80% of patients with non-acute knee pain. Only the MDT concluding classification was a useful predictor of the reduction of knee pain at the 1-month follow-up. These findings suggest the importance of careful screening assessments of the lumbar spine for patients with a primary complaint of non-acute knee pain and the importance of detecting subgroups of the Derangement Syndrome through follow-up sessions. These preliminary findings will serve as a foundation for future studies.
Biographies
Sanshiro Hashimoto is an orthopedic surgeon specialized in the knee, who is also credentialed in Mechanical Diagnosis and Therapy (MDT). He has received many international awards. He is a director of Minami Shinjuku Orthopedic Clinic, which is a certified McKenzie clinic in Japan.
Masatsugu Hirokado is a physiotherapist, who is credentialed in MDT. He has presented MDT studies at national and international conferences.
Hiroshi Takasaki is a physiotherapist and an associate professor in the Department of Physical Therapy at The Saitama Prefectural University, Japan. He is credentialed in MDT, who also completed MDT diploma clinical training. He has many MDT publications in international journals and has presented many studies at international conferences. He is one of seven research advisory committee members in the McKenzie Institute International.
Appendix 1. Patients taking medication or intra-articular injection over the course of Mechanical Diagnosis and Therapy intervention
| Total (N = 101), n (%) | 32 (31.7) |
|---|---|
| Kellgren–Lawrence grading scale Grade 0–1 (n = 63), n (%) | 15 (23.8) |
| Kellgren–Lawrence grading scale Grade 2 (n = 41), n (%) | 5 (29.4) |
| Kellgren–Lawrence grading scale Grade 3 (n = 16), n (%) | 8 (50.0) |
| Kellgren–Lawrence grading scale Grade 4 (n = 5), n (%) | 4 (80.0) |
| MDT concluding subgroup of Spinal Derangement (n = 45), n (%) | 9 (20.0) |
| MDT concluding subgroup of Knee Derangement (n = 27), n (%) | 10 (37.0) |
| MDT concluding subgroup of Knee Contractile Dysfunction (n = 4), n (%) | 1 (25.0) |
| MDT concluding subgroup of Knee Articular Dysfunction (n = 3), n (%) | 1 (33.3) |
| MDT concluding subgroup of OTHERs (n = 22), n (%) | 11 (50.0) |
Appendix 2. Kellgren–Lawrence grades and Magnetic Resonance Imaging (MRI) results of the MDT concluding subgroups
|
N = 101 |
N = 23 |
|||||
|---|---|---|---|---|---|---|
| MDT concluding subgroup | Kellgren–Lawrence Grade 0–1 (n = 63) | Kellgren–Lawrence Grade 2 (n = 17) | Kellgren–Lawrence Grade 3 (n = 16) | Kellgren–Lawrence Grade 4 (n = 5) | Abnormality on MRI: Negative (n = 2) | Abnormality on MRI: Positive (n = 21) |
| Spinal Derangement with directional preference of extension, n (%) | 28 (44.4) | 5 (29.4) | 2 (12.5) | 0 (0) | 1 (50) | 7 (33.4) |
| Spinal Derangement with directional preference of flexion, n (%) | 1 (1.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Spinal Derangement with directional preference of lateral, n (%) | 8 (12.7) | 1 (5.9) | 0 (0) | 0 (0) | 1 (50) | 0 (0) |
| Knee Derangement with directional preference of extension, n (%) | 12 (19.0) | 4 (23.5) | 2 (12.5) | 1 (20.0) | 0 (0) | 6 (28.6) |
| Knee Derangement with directional preference of flexion, n (%) | 4 (6.4) | 2 (11.8) | 2 (12.5) | 0 (0) | 0 (0) | 2 (9.5) |
| Knee Contractile Dysfunction, n (%) | 3 (4.8) | 1 (5.9) | 0 (0) | 0 (0) | 0 (0) | 2 (9.5) |
| Knee Articular Dysfunction, n (%) | 1 (1.6) | 1 (5.9) | 1 (6.3) | 0 (0) | 0 (0) | 0 (0) |
| OTHERs, n (%) | 6 (9.5) | 3 (17.6) | 9 (56.2) | 4 (80.0) | 0 (0) | 4 (19.0) |
Acknowledgments
The authors wish to acknowledge Mr Richard Rosedale for peer-reviewing this paper prior to submission.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Takasaki H, Saiki T, Iwasada Y.. McKenzie therapists adhere more to evidence-based guidelines and have a more biopsychosocial perspective on the management of patients with low back pain than general physical therapists in Japan. Open J Ther Rehabil. 2014;2:173–181. [Google Scholar]
- [2].Takasaki H.Mechanical diagnosis and Therapy enhances attitude towards self-management in people with musculoskeletal disorders: a preliminary evidence with a before-after design. SAGE Open Med. 2017;5:2050312117740986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Battie MC, Cherkin DC, Dunn R, et al. Managing low back pain: attitudes and treatment preferences of physical therapists. Phys Ther. 1994;74:219–226. [DOI] [PubMed] [Google Scholar]
- [4].Foster NE, Thompson KA, Baxter GD, et al. Management of nonspecific low back pain by physiotherapists in Britain and Ireland. A descriptive questionnaire of current clinical practice. Spine (Phila Pa 1976). 1999;24:1332–1342. [DOI] [PubMed] [Google Scholar]
- [5].Davies C, Nitz AJ, Mattacola CG, et al. Practice patterns when treating patients with low back pain: a survey of physical therapists. Physiother Theory Pract. 2014;30:399–408. [DOI] [PubMed] [Google Scholar]
- [6].May SJ, Rosedale R. A survey of the McKenzie classification system in the extremities: prevalence of mechanical syndromes and preferred loading strategies. Phys Ther. 2012;92:1175–1186. [DOI] [PubMed] [Google Scholar]
- [7].Rosedale R, Rastogi R, May S, et al. Efficacy of exercise intervention as determined by the McKenzie system of mechanical diagnosis and therapy for knee osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther. 2014;44:173–181, A171–176. [DOI] [PubMed] [Google Scholar]
- [8].Lynch G, May S. Directional preference at the knee: a case report using mechanical diagnosis and therapy. J Man Manip Ther. 2013;21:60–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Takasaki H, Iwasada Y, May S. Attitude towards the use of mechanical diagnosis and therapy and reliability of classification extremity problems by credentialed therapists. J Chiropr Med. 2015;14:32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Heidar Abady A, Rosedale R, Overend TJ, et al. Inter-examiner reliability of diplomats in the mechanical diagnosis and therapy system in assessing patients with shoulder pain. J Man Manip Ther. 2014;22:199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Takasaki H, Okuyama K, Rosedale R. Inter-examiner classification reliability of mechanical diagnosis and therapy for extremity problems – systematic review. Musculoskelet Sci Pract. 2017;27:78–84. [DOI] [PubMed] [Google Scholar]
- [12].Takasaki H. Agreement of mechanical diagnosis and therapy classification in patients with extremity conditions. Phys Ther. 2016;96:1525–1532. [DOI] [PubMed] [Google Scholar]
- [13].Foster NE, Hill JC, O’Sullivan P, et al. Stratified models of care. Best Pract Res Clin Rheumatol. 2013;27:649–661. [DOI] [PubMed] [Google Scholar]
- [14].Foster NE, Dziedzic KS, Van Der Windt DAWD, et al. Research priorities for non-pharmacological therapies for common musculoskeletal problems: nationally and internationally agreed recommendations. BMC Musculoskelet Disord. 2009;10:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Guermazi A, Niu J, Hayashi D, et al. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham osteoarthritis study). BMJ. 2012;345:e5339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lederman E. The fall of the postural-structural-biomechanical model in manual and physical therapies: exemplified by lower back pain. J Bodyw Mov Ther. 2011;15:131–138. [DOI] [PubMed] [Google Scholar]
- [17].Englund M, Guermazi A, Gale D, et al. Incidental meniscal findings on knee MRI in middle-aged and elderly persons. N Engl J Med. 2008;359:1108–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].McKenzie R, May S. The human extremities: mechanical diagnosis and therapy. Raumati Beach: Spinal Publications New Zealand Ltd; 2000. [Google Scholar]
- [19].Takasaki H, May S. Mechanical diagnosis and therapy has similar effects on pain and disability as ‘wait and see’ and other approaches in people with neck pain: a systematic review. J Physiother. 2014;60:78–84. [DOI] [PubMed] [Google Scholar]
- [20].Menon A, May S. Shoulder pain: differential diagnosis with mechanical diagnosis and therapy extremity assessment - a case report. Man Ther. 2013;18:354–357. [DOI] [PubMed] [Google Scholar]
- [21].Heidar Abady AH, Rosedale R, Chesworth BM, et al. Application of McKenzie system of mechanical diagnosis and therapy (MDT) in patients with shoulder pain: a prospective longitudinal study. J Man Manip Ther. 2017;25:235–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hegmann KT, Biggs JJ, Hughes MA, et al. Knee disorders Occupational medicine practice guidelines: Evaluation and management of common health problems and functional recovery in workers. 3rd ed. Elk Grove Village: American College of Occupational and Environmental Medicine; 2015. p. 1–503. [Google Scholar]
- [23].Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Garcia AN, Costa Lda C, Hancock M, et al. Identifying patients with chronic low back pain who respond best to mechanical diagnosis and therapy: secondary analysis of a randomized controlled trial. Phys Ther. 2016;96:623–630. [DOI] [PubMed] [Google Scholar]
- [25].Schiphof D, Kerkhof HJ, Damen J, et al. Factors for pain in patients with different grades of knee osteoarthritis. Arthritis Care Res (Hoboken). 2013;65:695–702. [DOI] [PubMed] [Google Scholar]
- [26].Akai M, Doi T, Fujino K, et al. An outcome measure for Japanese people with knee osteoarthritis. J Rheumatol. 2005;32:1524–1532. [PubMed] [Google Scholar]
- [27].Yabuki S, Kikuchi S. Medical knee pain in elderly patients. Rinsho Seikei Geka (Clin Orthopaedic Surg). 1998;33:1381–1385. [Google Scholar]
- [28].Kunogi J, Hasue M, Miyoshi K, et al. Clinical study of knee pain induced by lumbar radiculopathy. Rinsho Seikei Geka (Clin Orthopaedic Surg). 1993;28:709–717. [Google Scholar]
- [29].Fingleton C, Smart K, Moloney N, et al. Pain sensitization in people with knee osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23:1043–1056. [DOI] [PubMed] [Google Scholar]
- [30].Lascurain-Aguirrebena I, Newham D, Critchley DJ. Mechanism of action of spinal mobilizations: a systematic review. Spine (Phila Pa 1976). 2016January;41(2):159–172. [DOI] [PubMed] [Google Scholar]
- [31].Sahrmann SA. Diagnosis and treatment of movement impairment syndromes. St Louis: Mosby; 2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Delitto A, Erhard RE, Bowling RW, et al. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Phys Ther. 1995;75:470–489. [DOI] [PubMed] [Google Scholar]
- [33].Fritz JM, Brennan GP. Preliminary examination of a proposed treatment-based classification system for patients receiving physical therapy interventions for neck pain. Phys Ther. 2007;87:513–524. [DOI] [PubMed] [Google Scholar]
- [34].Schäfer A, Hall T, Briffa K. Classification of low back-related leg pain-A proposed patho-mechanism-based approach. Man Ther. 2009;14:222–230. [DOI] [PubMed] [Google Scholar]
- [35].O’Sullivan PB, Beales DJ. Diagnosis and classification of pelvic girdle pain disorders—part 1: A mechanism based approach within a biopsychosocial framework. Man Ther. 2007;12:86–97. [DOI] [PubMed] [Google Scholar]
- [36].Dankaerts W, O’Sullivan P. The validity of O’Sullivan’s classification system (CS) for a sub-group of NS-CLBP with motor control impairment (MCI): overview of a series of studies and review of the literature. Man Ther. 2011;16:9–14. [DOI] [PubMed] [Google Scholar]
- [37].Logerstedt DS, Scalzitti DA, Bennell KL, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions revision 2018. J Orthop Sports Phys Ther. 2018;48:A1–A50. [DOI] [PubMed] [Google Scholar]
- [38].Logerstedt DS, Scalzitti D, Risberg MA, et al. Knee stability and movement coordination impairments: knee ligament sprain revision 2017. J Orthop Sports Phys Ther. 2017;47:A1–A47. [DOI] [PubMed] [Google Scholar]
- [39].Phyomaung PP, Dubowitz J, Cicuttini FM, et al. Are depression, anxiety and poor mental health risk factors for knee pain? A systematic review. BMC Musculoskelet Disord. 2014;15:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Urquhart DM, Phyomaung PP, Dubowitz J, et al. Are cognitive and behavioural factors associated with knee pain? A systematic review. Semin Arthritis Rheum. 2015;44:445–455. [DOI] [PubMed] [Google Scholar]
- [41].Murphy SE, Blake C, Power CK, et al. Comparison of a stratified group intervention (STarT Back) with usual group care in patients with low back pain: a nonrandomized controlled trial. Spine (Phila Pa 1976). 2016;41:645–652. [DOI] [PubMed] [Google Scholar]
- [42].Hill JC, Whitehurst DG, Lewis M, et al. Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. Lancet. 2011;378:1560–1571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Gabel CP, Burkett B, Melloh M. The shortened orebro musculoskeletal screening questionnaire: evaluation in a work-injured population. Man Ther. 2013;18:378–385. [DOI] [PubMed] [Google Scholar]
- [44].Takasaki H, Gabel CP. Cross-cultural adaptation of the 12-item Örebro musculoskeletal screening questionnaire to Japanese (ÖMSQ-12-J), reliability and clinicians’ impressions for practicality. J Phys Ther Sci. 2017;29:1409–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]


