ABSTRACT
Background: Studies on mental health following disasters have primarily focused on post-traumatic stress disorder (PTSD), yet severe, enduring, and disabling grief [i.e. complicated grief (CG)] also appears relevant.
Objective: The present study examines symptom profiles of PTSD and CG among bereaved Sichuan earthquake survivors 1 year after the disaster.
Method: Self-report measures of demographic, disaster, and loss-related characteristics and symptoms of PTSD and CG were administered among 803 survivors (63% women; mean age = 46.7 years). Latent class analysis (LCA) was performed to identify subgroups of people with different PTSD and CG symptom profiles.
Results: The LCA demonstrated that a five-class solution yielded the best fit, consisting of a CG class with low PTSD and high CG (N = 208), a combined class with high PTSD and high CG (N = 205), a class with low PTSD and partial CG (N = 145), a class with partial PTSD and CG (N = 136), and a resilient class with low PTSD and CG (N = 108). Being a woman (vs man), losing a child or spouse (vs other), being injured (vs non-injured), and/or having a missing family member (vs non-missing) predicted membership of the CG class compared to other classes.
Conclusions: CG appears to be a unique consequence of disasters involving many casualties. Disaster survivors should be screened for CG and provided with appropriate psychological treatment.
KEYWORDS: Prolonged grief disorder, persistent complex bereavement disorder, bereavement, trauma, Wenchuan earthquake
HIGHLIGHTS
• Earthquakes elicit post-traumatic stress disorder (PTSD) and complicated grief (CG), but research on CG is still limited.• We performed the first latent class analysis on PTSD and CG among bereaved earthquake survivors.• The analysis demonstrated a five-class solution, which includes a CG class and a resilient class• The results suggest that disaster mental health services should screen for CG and offer CG-specific therapies.
Abstract
Antecedentes: Los estudios en la salud mental luego de desastres se ha centrado principalmente en el trastorno de estrés postraumático (TEPT), pero el duelo discapacitante y permanente (por ejemplo, duelo complicado, DC) también pareciera ser importante.
Objetivo: El presente estudio examina los perfiles de síntomas de TEPT y DC entre los sobrevivientes del terremoto de Sichuan que perdieron a un ser querido, un año después del desastre.
Método: A los 803 sobrevivientes (63% mujeres, edad media = 46,7 años), se les administraron medidas de auto-reporte sobre las características demográficas, del desastre, y relacionadas a la pérdida como también síntomas de TEPT y DC. El análisis de clases latentes (LCA en sus siglas en inglés) fue llevado a cabo para identificar subgrupos de personas con diferentes perfiles de TEPT y DC.
Resultados: El LCA demostró que una solución de cinco clases presentó el mejor ajuste, consistiendo de una clase de DC con bajo TEPT y alto DC (N = 208), una clase combinada de alto TEPT y alto DC (N = 205), una clase de bajo TEPT y DC parcial (N = 145), una clase con TEPT y DC parciales (N = 136), y una clase resiliente con bajo TEPT y DC (N = 108). Ser mujer (vs. hombre), perder un hijo/a o cónyuge (vs. otro), estar lesionado/a (vs. no lesionado/a), y/o tener a un familiar perdido (vs. no perdido) predijeron la pertenencia a la clase del DC comparado a las otras clases.
Conclusiones: El DC surge como una consecuencia única de los desastres involucrando a muchas víctimas. Los sobrevivientes de desastres deberían ser pesquisados por DC y tener acceso a tratamiento psicológico adecuado.
PALABRAS CLAVES: Trastorno de duelo prolongado, trastorno de duelo complejo persistente, duelo, trauma, terremoto de Wenchuan
四川地震丧亲者的复杂哀伤与创伤后应激症状剖面图:来自潜在类别分析的结果
背景:有关灾难的研究通常都关注创伤后应激障碍(PTSD),然而持续而强烈的哀伤(即,复杂哀伤,CG)也同样值得关注。
目的:本研究探索四川地震一年以后,失去亲人的灾民们的PTSD 和CG症状情况。
方法:共有803名丧亲的灾民(63%是女性,平均年龄47岁)完成了自我报告的问卷,内容包括人口学变量,与灾难和丧失有关的情况,以及测量PTSD与CG的问卷。用潜分类分析(LCA)来检测被试的PTSD与CG 症状分组情况。
结果:分析结果表明被试的最佳分类是5组,包括CG组:低PTSD和高CG (N = 208),混合组:高PTSD及高CG (N = 205),一组低PTSD和部分CG(N =145),一组部分PTSD和CG (N = 136),以及复原组:低PTSD低CG(N = 108)。女性(相比男性),失去孩子或配偶(相比失去其他人),有家庭成员失踪(相比无失踪),有家庭成员失踪(相比无失踪)能预测CG组(相对于其他组而言)。
结论:在有人员伤亡的灾难中,CG是单独呈现的一组症状。灾难幸存者的CG情况应该被筛查并给予相应的支持。
1. Introduction
Ten years after the 2008 Sichuan earthquake, it is time to consolidate what we have learned from this disaster. Measuring 8.0 on the Richter scale, it was one of the most devastating earthquakes in recent history, with 87,000 people either killed or missing, and around 374,000 people injured. The earthquake destroyed an estimated 6.5 million houses, and severely damaged commercial areas and infrastructure, resulting in substantial interpersonal and economic losses. About 46 million people were affected, 15 million people were evacuated from their homes, and more than 5 million farmers lost their harvests (e.g. Kun et al., 2009; Li, Chow, Shi, & Chan, 2015).
Survivors of disasters such as the Sichuan earthquake commonly experience a variety of major stressful life events, including but not limited to being injured; exposure to dead bodies; losing homes, communities, and jobs; and sudden and/or traumatic bereavement of family members, friends, neighbours, and colleagues. As a consequence, survivors may be at an elevated risk of developing stress-related disorders, such as post-traumatic stress disorder (PTSD). Indeed, multiple studies have demonstrated that high prevalence rates of PTSD are found in survivors of human-made disasters, such as boat and aeroplane accidents (e.g. Gouweloos et al., 2016; Lee, Kim, Noh, & Chae, 2018), and terrorist attacks (e.g. Bowler et al., 2010), and natural disasters, such as the 2004 tsunami (e.g. Kristensen, Weisæth, Hussain, & Heir, 2015; Thienkrua et al., 2006), floods (e.g. Liu et al., 2006; Norris, Murphy, Baker, & Perilla, 2004), and earthquakes (e.g. Chan et al., 2012; Goenjian et al., 2000; Roussos et al., 2005). Notable in the context of the present study, a recent review demonstrated that 1 year after the Sichuan earthquake, PTSD prevalence rates ranged from 21.5% to 41.0% among people directly or indirectly affected by the earthquake (Liang, Cheng, Ruzek, & Liu, 2019).
Substantially less attention has been devoted to post-disaster development of severe, persistent, and disabling grief, also termed prolonged grief or complicated grief (CG). Even for bereaved disaster survivors, concerns about PTSD appear to have overshadowed concerns about CG. This may be due, in part, to the fact that CG has until recently not been formally established as a disorder in diagnostic classification manuals. However, it is currently included as persistent complex bereavement disorder (PCBD) in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), as a proposed disorder requiring further empirical study (American Psychiatric Association, 2013). Moreover, a related but distinct disorder, prolonged grief disorder (PGD), has been included in the 11th edition of the International Classification of Diseases (ICD-11) as a stress-related disorder (World Health Organization, 2018). These recent developments suggest that it is prudent to investigate the extent to which disasters involving massive casualties lead to the development of CG, and whether CG symptomatology represents a unique disaster outcome that can be distinguished from PTSD.
Several studies have demonstrated that CG is highly prevalent after natural and human-made disasters involving the death of significant others (e.g. Ghaffari-Nejad, Ahmadi-Mousavi, Gandomkar, & Reihani-Kermani, 2007; Johannesson, Lundin, Fröjd, Hultman, & Michel, 2011; Kristensen, Weisæth, & Heir, 2009; Li et al., 2015; Neria et al., 2007; Shear et al., 2011). The few large-scale comparative studies on mental health outcomes of people bereaved through disasters to date have even shown that CG may have a higher prevalence than PTSD (e.g. Li et al., 2015; Neria et al., 2007), but for a study showing contradictory results see Kristensen et al. (2009). Most notably, an investigation of a large sample of Chinese Sichuan earthquake survivors found the estimated prevalence of CG (71%) to be much higher than that of PTSD (39%) (Li et al., 2015). In summary, these findings appear to indicate that CG may be a distinct mental health problem in people who have experienced a disaster with a large number of casualties. However, it is unclear to what extent comorbidity of PTSD and CG exists, and how many people typically demonstrate resilient responses following disasters.
One way to shed light on this issue is by identifying symptom profiles in people bereaved through disasters, by applying latent class analysis (LCA), a statistical technique which identifies unobserved subgroups of individuals based on predefined indicators (e.g. presence of symptoms of specific disorders). In contrast to prior epidemiological studies (for a review, see Kristensen, Weisæth, & Heir, 2012) whereby PTSD and CG are considered either absent or present based on questionnaire cut-off scores or structured clinical interviews, LCA can reveal subtypes of (comorbid) disorders. For instance, LCA studies in various samples of people exposed to stressful life events have identified several PTSD subtypes that differ in terms of severity of symptoms (e.g. classes with low, intermediate, and high PTSD levels) (Breslau, Reboussin, Anthony, & Storr, 2005; Lenferink, de Keijser, van Denderen, & Boelen, in press), but also in the combination of different subsets of symptoms (e.g. low PTSD and dissociation symptoms, PTSD with dissociation symptoms, and PTSD without dissociation symptoms) (Hansen, Ross, & Armour, 2017).
A notable preliminary investigation applied LCA to assess whether classes of 167 people bereaved through the 2014 MH-17 aeroplane crash could be distinguished based on their symptom clusters of depression, PTSD, and PGD approximately 1 year after the crash (Lenferink, de Keijser, Smid, Djelantik, & Boelen, 2017). In that study, it was found that three classes provided the best fit. The first class (resilient class; 20%) was predominantly characterized by a low probability of PGD, major depressive disorder (MDD), and PTSD symptom clusters; the second class (PGD class; 42%) by a moderate to high probability of the presence of PGD without comorbidity; and the third class (combined class; 38%) by a moderate to high probability of the presence of PGD, MDD, and PTSD symptom clusters. While this pioneering work was invaluable in showing that CG without comorbidity may be a unique and prevalent symptom class following a disaster, the small sample size made it impossible to investigate individual symptom profiles and therefore it was limited to an analysis of symptom clusters (e.g. for PTSD: re-experiencing, avoidance, alterations in cognition and mood, and alterations in arousal and reactivity). In addition, it is unclear if the results from this investigation can be generalized to people who have been exposed to a natural disaster (involving exposure to a higher number of potentially traumatic events, e.g. witnessing violent death, being injured, having a missing relative) or to people living in non-Western countries.
Two other relevant studies applied LCA on PTSD and CG symptoms (not clusters) in non-Western forcibly displaced people who reported multiple traumatic events and bereavement. These studies consistently reported four distinct PTSD and CG symptom classes (Heeke, Stammel, Heinrich, & Knaevelsrud, 2017; Nickerson et al., 2014). For instance, Nickerson et al. (2014) showed that one class was resilient (43%), one class presented with high PTSD symptoms only (25%), one class predominantly showed high CG symptoms (16%), and one combined class scored high on CG and PTSD (16%). However, these samples differ from natural disaster samples because mental health problems in these samples were not the consequence of one central event, but rather of an accumulation of negative life events over a longer period.
Therefore, the present study aimed to critically extend the current knowledge base on this topic by conducting a symptom-based LCA of PTSD and CG in 803 survivors of the Sichuan earthquake 1 year after the disaster. Based on the only study applying LCA in disaster-bereaved people (Lenferink et al., 2017), we predicted that we would discern a resilient class, a high CG class without comorbid PTSD, and a combined class with high PTSD and CG. Furthermore, we aimed to explore potential correlates of class membership, including demographic variables (e.g. age and gender), loss-related variables (i.e. relationship to the deceased), and disaster-related variables (e.g. being injured in the earthquake).
2. Materials and methods
2.1. Procedure and participants
Ethical approval for this study was granted by the Human Research Ethics Committee for Non-Clinical Faculties of the University of Hong Kong.
Twelve to 13 months after the Sichuan earthquake, a cross-sectional survey was conducted in a temporary shelter community (Li et al., 2015). Most community members were former residents of Beichuan county, which was graded one of the 10 most earthquake-affected areas by the Chinese government. According to official statistics, at least 8605 residents in that county were killed in the earthquake. Death and injury rates in Beichuan country were 5% and 6%, respectively (Zhao, Cui, Yu, & Zhong, 2012). To avoid bias, only one competent person in each household, meaning someone who has no difficulty in understanding questions or communicating, was recruited. Owing to the concerns of the medical ethical review board that people with severe mental health problems (e.g. schizophrenia) may be negatively affected by the interview or may not fully understand questions, and a lack of study resources to conduct formal psychiatric assessments, participants who indicated that they had been diagnosed with a psychiatric disorder prior to the earthquake were excluded from participation. However, it should be noted that the estimated prevalence of diagnosed mental disorders in the largest city in the earthquake-affected area prior to the disaster was very low (0.4%) and therefore few people were excluded for this reason (Wei, Hu, & Chen, 1994). The purpose and significance of the study were explained to participants, and their oral consent was obtained before starting the interview. Only participants who had lost at least one significant other (including family members and friends) in the earthquake were invited to answer the questions. Originally, 859 bereaved people were interviewed; however, 56 of them had to be excluded from the present analysis because more than one-fifth of the data to be analysed were missing.
The participants’ mean age was 46.72 years (SD = 15.51) and 63% of the participants were women. For the majority of participants, the highest educational level was primary school (42.2%) or junior high school (35.9%). For 19.5%, the highest educational level was high school or technical secondary school, and 2.4% had acquired higher education. More than half of the participants (52.8%) were of the Qiang ethnic minority group and 4.6% were members of other minority groups. The remaining 42.6% were Han Chinese. Most participants (74.3%) did not hold any religious beliefs. One-fifth (20.7%) of the sample practised Buddhism and 5.0% practised another religion. All of the participants had lost significant others in the earthquake and many people had experienced multiple losses; 21.3% had lost a spouse, 33.4% had lost one or more children, 79.7% had lost one or more other family members, and almost everyone (98.4%) had lost one or more friends or colleagues. Table 1 shows all the sample characteristics.
Table 1.
Sample characteristics.
| Gender, valid N (%) | |
| Male | 273 (63.1) |
| Female | 466 (36.9) |
| Age (years), M (SD), range | 46.72 (15.51), 16–98 |
| Educational level, valid N (%) | |
| Primary school | 335 (42.2) |
| Junior high school | 285 (35.9) |
| High school | 96 (12.1) |
| Technical secondary school | 59 (7.4) |
| College/university | 19 (2.4) |
| Ethnic minority group, valid N (%) | |
| Qiang | 421 (52.8) |
| Han | 340 (42.6) |
| Other | 42 (4.6) |
| Religious beliefs, valid N (%) | |
| No religion | 570 (74.3) |
| Buddhism | 159 (20.7) |
| Other | 38 (5.0) |
| Deceased person(s) is/are, valid N (%)a | |
| Partner | 170 (21.3) |
| Child(ren) | 268 (33.4) |
| Other family members | 636 (79.7) |
| Friends or colleagues | 789 (98.4) |
| Family members missing, valid N (%) | 373 (46.6) |
| Physical injury, valid N (%) | 379 (47.4) |
a Categories are not mutually exclusive.
2.2. Measures
Demographic, loss-related, and disaster-related characteristics were assessed with a self-constructed questionnaire. The following variables were used as correlates of class membership: the demographic variables gender (0 = male, 1 = female), highest educational level (coded as 0 = primary school or lower, 1 = junior high school or higher), age (in years), and religious beliefs (0 = no, 1 = yes); the loss-related variable relationship to the deceased [coded as 0 = the deceased relative(s) is/are not a child or spouse, 1 = at least one deceased relative is a child or spouse]; and two disaster-related variables, namely whether any family member is still missing due to the earthquake (0 = no, 1 = yes), and whether the participant was physically injured in the earthquake (0 = no, 1 = yes).
PTSD symptoms in accordance with the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) criteria were assessed with the 17-item Chinese PTSD Checklist – Civilian version (PCL-C) (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Chinese translation: Wu, Chan, & Yiu, 2008). Each item describes a symptom of PTSD, corresponding to the three DSM-IV symptom clusters of PTSD (re-experiencing, avoidance, and hyperarousal). Participants were asked to rate to what extent they had experienced each symptom over the past month on a five-point scale in response to the anchor event (in this study, the earthquake), ranging from not at all (1) to extremely (5). The reliability of the PCL-C in the current sample was excellent, at α = 0.95.
The 19-item Chinese version of the Inventory of Complicated Grief (ICG) was used to assess CG symptoms (Prigerson et al., 1995; Chinese translation: Li & Prigerson, 2016). It contains 19 items reflecting proposed indicators of CG. Participants rated the frequency with which they experienced each individual symptom over the previous month on a five-point scale ranging from never (0) to always (4). The internal consistency of the ICG in the present sample was excellent, at α = 0.96.
2.3. Analyses
The LCA was performed using dichotomized indicators of PTSD and CG. For PTSD, items scored as 1 = ‘not at all’ or 2 = ‘a little bit’ were coded as symptom absent, and items scored as 3 = ‘moderately’, 4 = ‘quite a bit’, or 5 = ‘extremely’ were coded as symptom present. For CG, items scored as 0 = ‘never’ or 1 = ‘rarely’ were coded as symptom absent, and items scored as 2 = ‘sometimes’, 3 = ‘often’, or 4 = ‘always’ were coded as symptom present.
A one-class up to a six-class model was estimated (Nickerson et al., 2014). Based on the fit indices of these six models, the most optimal class solution was selected. The (sample-size adjusted) Bayesian information criterion [(SA-)BIC] and Akaike information criterion (AIC) of the models were compared; lower values for these criteria indicate a better fit (Nylund, Asparouhov, & Muthén, 2007). The entropy index of each model was inspected, which has a value between 0 and 1. A higher entropy index indicates that people are classified with more confidence (van de Schoot, Sijbrandij, Winter, Depaoli, & Vermunt, 2017). Entropy values > .80 are considered acceptable (Muthén & Muthén, 2007). The p-value of the bootstrap likelihood ratio test (BLRt) was computed. A p-value below .05 indicates a significant improvement of the fit of the current model relative to the model with one less class (Nylund et al., 2007). Following the recommendations of Nylund et al. (2007), we did not solely rely on fit indices in selecting the optimal class solution; the class sizes and interpretation of the class solutions were also considered. Models with too small class sizes were avoided, because they can result in computational difficulties when estimating the correlates of class membership (e.g. too few observations within cells). With regard to the interpretation of the classes, solutions with fewer classes that were interpretable because they were in line with previous research and/or theory were preferred over solutions with more classes that were uninterpretable.
After selecting the most optimal class solution, people were allocated to the class with the highest classification proportion. The classification error resulting from assigning people to classes was taken into account when examining the correlates of class membership, using the three-step approach (Vermunt, 2010). The association between, on the one hand, demographic (four variables), loss-related (one variable), and disaster-related variables (two variables), and, on the other hand, class membership was examined simultaneously in a multivariate logistic regression model by including these variables as covariates in the model and the classification probabilities as dependent variables. Following recommendations from Vermunt (2010), a maximum likelihood estimation-based correction method was used. A univariate approach was used to examine the associations between symptom levels of PTSD and CG and class membership. The 95% confidence intervals (CIs) were computed for each contrast. When zero was not included in the 95% CI, the difference between the classes was considered significant. Odds ratios (ORs) were computed for each significant contrast, while taking the classification error into account. A maximum of 2.0% of the data per PTSD and CG item was missing and this was handled using maximum likelihood estimation. Latent Gold version 5.0 was used to analyse the data (Vermunt & Magidson, 2013).
3. Results
3.1. Selection of an optimal class solution
Table 2 shows the fit indices of the one- to six-class models. The six-class model yielded the lowest (SA-)BIC and AIC values. All models showed acceptable entropy values. The significant BLRt p-value of the five-class model indicated that this model is preferred over the four-class model. Because the p-value of the six-class model was non-significant and the six-class model could not be interpreted meaningfully, we chose to select the five-class model as the optimal class solution.
Table 2.
Goodness-of-fit statistics for one- to six-class models (N = 803).
| Model | LL | SA-BIC | BIC | AIC | BLRt p | Entropy R2 | Smallest class size |
|---|---|---|---|---|---|---|---|
| One-class | −18,244.05 | 36,614.55 | 36,728.87 | 36,560.09 | |||
| Two-class | −15,161.71 | 30,579.85 | 30,811.67 | 30,469.42 | <.001 | .95 | 306 |
| Three-class | −13,881.28 | 28,148.96 | 28,498.27 | 27,982.55 | <.001 | .94 | 229 |
| Four-class | −13,374.07 | 27,264.53 | 27,731.33 | 27,042.15 | .002 | .94 | 114 |
| Five-class | −13,013.21 | 26,672.78 | 27,257.08 | 26,394.42 | .036 | .93 | 108 |
| Six-class | −12,689.33 | 26,154.99 | 26,856.79 | 25,820.66 | .068 | .94 | 79 |
LL, log-likelihood; SA-BIC, sample-size adjusted Bayesian information criterion; BIC, Bayesian information criterion; AIC, Akaike information criterion; BLRt, bootstrap likelihood ratio test.
3.2. Five-class solution
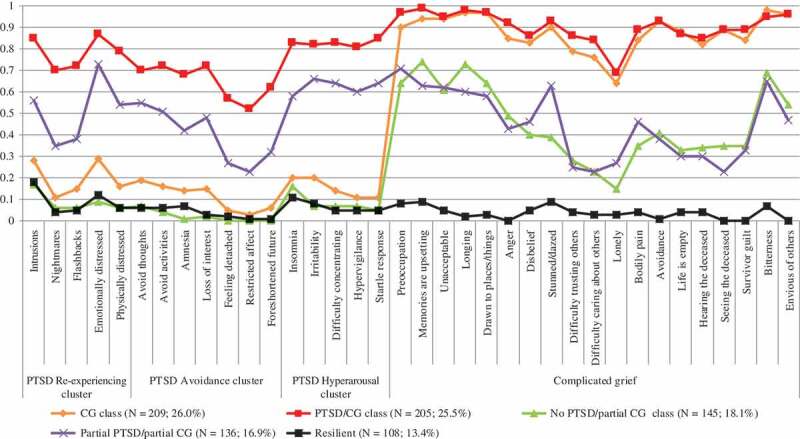
Table 3 and Figure 1 show the conditional probability estimates of the PTSD and CG symptoms, i.e. the frequencies of the presence of PTSD and CG symptoms per class (e.g. 18.0% of the people assigned to the Resilient class endorsed the PTSD symptom ‘Intrusions’). Following previous research (Lenferink et al., 2017; Nickerson et al., 2014), probability rates below .15 were considered low and rates of .60 or higher were considered high. Probabilities falling between these values were considered moderate.
Table 3.
Probability estimates of symptom endorsement for all participants and per class (N = 803).
| Overall symptom frequency (N = 803) |
CG class (n = 209; 26.0%) |
PTSD/CG class (n = 205; 25.5%) |
No PTSD/Partial CG class (n = 145; 18.1%) |
Partial PTSD/CG class (n = 136; 16.9%) |
Resilient class (n = 108; 13.4%) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | n | % | Prob. | SE | Prob. | SE | Prob. | SE | Prob. | SE | Prob. | SE | |
| PTSD Re-experiencing cluster | Intrusions | 335 | 44.3 | .28 | .03 | .85 | .03 | .17 | .03 | .56 | .04 | .18 | .04 |
| Nightmares | 227 | 28.5 | .11 | .03 | .70 | .04 | .06 | .02 | .35 | .04 | .04 | .02 | |
| Flashbacks | 242 | 30.6 | .15 | .03 | .72 | .03 | .06 | .02 | .38 | .05 | .05 | .02 | |
| Emotionally distressed | 361 | 45.4 | .29 | .04 | .87 | .03 | .09 | .03 | .73 | .04 | .12 | .03 | |
| Physically distressed | 283 | 35.3 | .16 | .03 | .79 | .03 | .06 | .02 | .54 | .05 | .06 | .03 | |
| PTSD Avoidance cluster | Avoid thoughts | 273 | 34.1 | .19 | .03 | .70 | .03 | .07 | .02 | .55 | .05 | .06 | .02 |
| Avoid activities | 261 | 32.7 | .16 | .03 | .72 | .03 | .04 | .02 | .51 | .05 | .06 | .02 | |
| Amnesia | 233 | 29.3 | .14 | .03 | .68 | .03 | .01 | .01 | .42 | .05 | .07 | .02 | |
| Loss of interest | 246 | 30.9 | .15 | .03 | .72 | .03 | .02 | .02 | .48 | .05 | .03 | .02 | |
| Feeling detached | 167 | 20.8 | .05 | .02 | .57 | .04 | .00 | .00 | .27 | .04 | .02 | .02 | |
| Restricted affect | 147 | 18.3 | .03 | .02 | .52 | .04 | .00 | .00 | .23 | .04 | .01 | .01 | |
| Foreshortened future | 183 | 22.9 | .06 | .02 | .62 | .04 | .00 | .00 | .32 | .04 | .01 | .01 | |
| PTSD Hyperarousal cluster | Insomnia | 324 | 40.4 | .20 | .04 | .83 | .03 | .16 | .03 | .58 | .05 | .11 | .03 |
| Irritability | 317 | 39.5 | .20 | .03 | .82 | .03 | .07 | .02 | .66 | .04 | .08 | .03 | |
| Difficulty concentrating | 304 | 37.9 | .14 | .03 | .83 | .03 | .07 | .03 | .64 | .04 | .05 | .02 | |
| Hypervigilance | 284 | 35.6 | .11 | .03 | .81 | .03 | .07 | .02 | .60 | .05 | .05 | .02 | |
| Startle response | 296 | 37.1 | .11 | .03 | .85 | .03 | .05 | .02 | .64 | .05 | .05 | .02 | |
| CG | Preoccupation with the person who died | 581 | 72.8 | .90 | .02 | .97 | .01 | .64 | .04 | .71 | .04 | .08 | .03 |
| Memories of the person who died are upsetting | 598 | 74.9 | .94 | .02 | .99 | .01 | .74 | .04 | .63 | .05 | .09 | .03 | |
| The death is unacceptable | 568 | 71.0 | .94 | .02 | .95 | .02 | .61 | .04 | .62 | .05 | .05 | .02 | |
| Longing for the person who died | 579 | 73.6 | .97 | .01 | .98 | .01 | .73 | .04 | .60 | .05 | .02 | .01 | |
| Drawn to places and things associated with the person who died | 575 | 71.9 | .97 | .01 | .97 | .01 | .64 | .04 | .58 | .05 | .03 | .02 | |
| Anger about the death | 492 | 61.6 | .85 | .03 | .92 | .02 | .49 | .04 | .43 | .05 | .00 | .00 | |
| Disbelief | 473 | 59.1 | .83 | .03 | .86 | .03 | .40 | .04 | .46 | .05 | .05 | .02 | |
| Feeling stunned or dazed | 527 | 66.0 | .90 | .02 | .93 | .02 | .39 | .04 | .63 | .05 | .09 | .03 | |
| Difficulty trusting others | 414 | 52.1 | .79 | .03 | .86 | .03 | .28 | .04 | .25 | .04 | .04 | .02 | |
| Difficulty caring about others | 396 | 49.4 | .76 | .04 | .84 | .03 | .23 | .04 | .23 | .04 | .03 | .02 | |
| Lonely | 336 | 42.0 | .64 | .04 | .69 | .03 | .15 | .03 | .27 | .04 | .03 | .02 | |
| Pain in the same area of the body | 473 | 59.2 | .84 | .03 | .89 | .02 | .35 | .04 | .46 | .05 | .04 | .02 | |
| Avoidance of reminders of the person who died | 492 | 61.7 | .93 | .02 | .93 | .02 | .41 | .04 | .38 | .05 | .01 | .01 | |
| Feeling that life is empty | 451 | 56.5 | .88 | .03 | .87 | .02 | .33 | .04 | .30 | .05 | .04 | .02 | |
| Hearing the voice of the person who died | 439 | 54.7 | .82 | .03 | .85 | .03 | .34 | .04 | .30 | .05 | .04 | .02 | |
| Seeing the person who died | 449 | 56.1 | .89 | .03 | .89 | .02 | .35 | .04 | .23 | .04 | .00 | .00 | |
| Feeling it is unfair to live when the other person has died | 452 | 56.6 | .84 | .03 | .89 | .02 | .35 | .04 | .33 | .05 | .00 | .01 | |
| Bitter about the death | 590 | 74.0 | .98 | .01 | .95 | .02 | .69 | .04 | .65 | .05 | .07 | .02 | |
| Envious of others | 540 | 67.2 | .96 | .02 | .96 | .01 | .54 | .04 | .47 | .05 | .00 | .00 | |
PTSD, post-traumatic stress disorder; CG, complicated grief.
Figure 1.
Estimated post-traumatic stress disorder (PTSD) and complicated grief (CG) symptom probabilities for the five-class latent class analysis solution.
The largest class (n = 209; 26.0%) was characterized by a low probability of endorsement of eight PTSD symptoms and a moderate probability of endorsement of nine PTSD symptoms, but a high probability of endorsement of all CG symptoms. This class was therefore labelled the ‘CG class’. The second class (n = 205; 25.5%) was characterized by a high probability of endorsement of all CG symptoms and 15 out of 17 PTSD symptoms. We labelled this the ‘PTSD/CG class’. The third class (n = 145; 18.1%) was characterized by a low probability of endorsement of 15 out of 17 PTSD symptoms, a high probability of endorsement of six out of 19 CG symptoms (i.e. ‘Preoccupation’, ‘Memories are upsetting’, ‘Unacceptable’, ‘Longing’, ‘Drawn to places/things’, and ‘Bitterness’), and a moderate probability of the other CG symptoms. This class was labelled the ‘No PTSD/Partial CG class’. The fourth class (n = 136; 16.9%) was characterized by a similar CG symptom pattern to the third class, but differed from the third class with respect to the PTSD symptom pattern. More specifically, five PTSD (mostly hyperarousal) symptoms were highly present in the fourth class and 12 PTSD symptoms were moderately present. This class was therefore labelled the ‘Partial PTSD/CG class’. The smallest class (n = 108; 13.4%) was characterized by a low probability of endorsement of all PTSD and CG symptoms, except for one PTSD symptom (‘Intrusions’) that had a moderate probability rate. This class was therefore labelled the ‘Resilient class’.
3.3. Symptom severity across the five classes
Altogether, 248 people (30.9%) in the total sample scored above the clinically relevant threshold of 44 for PTSD (Ruggiero et al., 2003). Of these people, the CG class contained five (2.4%), the PTSD/CG class 179 (87.7%), the Partial CG class zero (0.0%), the Partial PTSD/CG class 63 (46.7%), and the Resilient class one (0.9%). Furthermore, 565 people (70.4%) scored above the clinically relevant threshold of 25 on the ICG (Prigerson et al., 1995). All people in the CG class and PTSD/CG class scored above this threshold; 72 people (49.7%) and 79 people (58.1%) scored above this threshold in the No PTSD/Partial CG class and Partial PTSD/CG class, respectively; and none of the people in the Resilient class scored above this threshold.
We further examined differences between the classes with respect to PTSD and CG symptom levels (Table 4). To limit the number of tests, we focused on the differences between the modal response and other symptom profiles. The CG class was therefore used as the reference category. Average PTSD scores were significantly lower in the CG class (M = 32.68, SD = 6.23) than in the PTSD/CG class (M = 54.67, SD = 10.94) and Partial PTSD/CG class (M = 44.52, SD = 9.32). PTSD scores were, on average, significantly higher in the CG class than in the No PTSD/Partial CG class (M = 27.45, SD = 4.73) and Resilient class (M = 26.31, SD = 6.34). For CG scores, the average scores were significantly lower in the CG class (M = 43.19, SD = 9.07) than in the PTSD/CG class (M = 50.84, SD = 9.73), but significantly higher in the CG class than in the No PTSD/Partial CG class (M = 25.03, SD = 6.95), Partial PTSD/CG class (M = 25.68, SD = 10.43), and Resilient class (M = 5.40, SD = 6.10).
Table 4.
Univariate differences in complicated grief (CG) and post-traumatic stress disorder (PTSD) symptom levels between the classes (N = 803).
| CG vs PTSD/CG class |
CG vs No PTSD/Partial CG class |
CG vs Partial PTSD/CG class |
CG vs Resilient class |
Main effect |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | p | |
| ICG total score | 0.09 | 0.02 | 0.06, 0.13 | −0.44 | 0.04 | −0.52, −0.36 | −0.43 | 0.04 | −0.52, −0.35 | −0.71 | 0.05 | −0.81, −0.61 | <.001 |
| PCL-C total score | 0.48 | 0.03 | 0.42, 0.55 | −0.16 | 0.02 | −0.20, −0.12 | 0.35 | 0.03 | 0.29, 0.41 | −0.20 | 0.03 | −0.26, −0.15 | <.001 |
ICG, Inventory of Complicated Grief; PCL-C, PTSD Checklist – Civilian version; CI, confidence interval.
3.4. Correlates of class membership
Table 5 shows the results of the tests examining differences between the classes with respect to the seven demographic, disaster-related, and loss-related variables. As mentioned, the CG class was used as the reference category.
Table 5.
Parameter estimates for the latent class model with covariates included simultaneously (N = 699a).
| CG vs PTSD/CG class |
CG vs No PTSD/Partial CG class |
CG vs Partial PTSD/CG class |
CG vs Resilient class |
Main effect |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Covariates | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | p |
| Gender (0 = male) | 0.10 | 0.26 | −0.41, 0.60 | −0.48 | 0.27 | −1.02, 0.05 | −0.50 | 0.28 | −1.05, 0.05 | −0.67 | 0.31 | −1.27, −0.07 | .055 |
| Educational level (0 = primary school or lower) | −0.18 | 0.28 | −0.72, 0.36 | 0.32 | 0.30 | −0.27, 0.90 | 0.83 | 0.34 | 0.16, 1.51 | −0.09 | 0.34 | −0.75, 0.57 | .033 |
| Age (years) | 0.00 | 0.01 | −0.02, 0.02 | 0.00 | 0.01 | −0.02, 0.02 | −0.01 | 0.01 | −0.03, 0.02 | 0.01 | 0.01 | −0.01, 0.03 | .660 |
| Religion (0 = no) | 0.33 | 0.26 | −0.18, 0.84 | −0.52 | 0.31 | −1.13, 0.10 | −0.19 | 0.32 | −0.81, 0.44 | −0.73 | 0.36 | −1.43, −0.03 | .027 |
| Relationship to the deceased (0 = other than spouse or child) | 0.08 | 0.26 | −0.43, 0.59 | −1.49 | 0.28 | −2.04, −0.94 | −1.33 | 0.31 | −1.93, −0.73 | −3.04 | 0.42 | −3.87, −2.21 | <.001 |
| Missing family member (0 = no) | 0.98 | 0.24 | 0.52, 1.44 | −0.10 | 0.26 | −0.62, 0.41 | −0.17 | 0.29 | −0.73, 0.39 | −0.80 | 0.31 | −1.41, −0.19 | <.001 |
| Physically injured (0 = no) | 0.27 | 0.23 | −0.19, 0.72 | −0.58 | 0.27 | −1.10, −0.06 | −0.09 | 0.27 | −0.61, 0.44 | −0.82 | 0.31 | −1.42, −0.22 | .002 |
a The sample size is 699 instead of 803 because people with missing responses on the covariates were excluded from these analyses. CG, complicated grief; PTSD, post-traumatic stress disorder; CI, confidence interval.
People in the CG class differed significantly from the Resilient class with respect to five out of seven correlates. Compared to the Resilient class, people in the CG class were more likely to be women (69.5% vs 54.4%; OR = 1.91), have religious beliefs (27.4% vs 18.8%; OR = 1.63), have lost at least a spouse or child [vs other relatives(s) or friend(s); 64.9% vs 8.8%; OR = 19.24], report that any of their family members were missing in the earthquake (45.6% vs 24.1%; OR = 2.64), and be physically injured because of the earthquake (51.5% vs 30.6%; OR = 2.41). Regarding the differences between the CG class and the Partial PTSD/CG class, people in the CG class were less likely to have a higher educational level than people in the Partial PTSD/CG class (51.3% vs 76.7%; OR = 0.32) and were more likely to have lost their spouse or one or more children [vs other relatives(s) or friend(s); 64.9% vs 30.8%; OR = 4.15]. The CG class differed significantly from the No PTSD/Partial CG class with respect to kinship to the deceased and being physically injured because of the earthquake. More specifically, people in the CG class were more likely to have lost at least a spouse or child [vs other relatives(s) or friend(s); 64.9% vs 29.3%; OR = 4.46] and be physically injured because of the earthquake (51.5% vs 34.6%; OR = 2.01). Lastly, people in the CG class differed significantly from people in the PTSD/CG class with respect to only one variable. Specifically, people in the PTSD/CG class were more likely to report that any of their family members were missing in the earthquake than people in the CG class (69.5% vs 45.6%; OR = 2.72).
4. Discussion
The aim of the present study was to assess, for the first time, whether unique symptom profiles of PTSD and CG can be distinguished in a sample of bereaved earthquake survivors, using LCA. In line with expectations and prior LCA research among (disaster-)bereaved people (e.g. Djelantik, Smid, Kleber, & Boelen, 2017; Lenferink et al., 2017; Maccallum & Bryant, in press), the five-class LCA solution included a large CG group (26.0%, characterized by low PTSD and high CG symptoms), a large PTSD/CG group (25.5% with moderate to high CG symptoms and high PTSD symptoms), and a resilient group (13.4% with low PTSD and low CG symptoms). However, two additional groups could also be identified: one partial PTSD/CG group (16.9% with moderate to high PTSD and CG symptoms) and one group with partial CG (18.1% with low PTSD and moderate to high CG symptoms).
In addition, we set out to explore correlates of class membership. Key findings were that people were more likely to be members of the CG group relative to the Resilient group if they were female, bereaved of a spouse and/or one or more children, had themselves been physically injured during the earthquake, or had relatives who were missing due to the earthquake. People were more likely to be part of the CG group relative to both the Partial PTSD/CG group and the Partial CG group if they had lost a spouse or one or more children. Lastly, people reporting that any family member went missing during the earthquake were less likely to be part of the CG group compared to the PTSD/CG group.
Turning to the primary results first, our findings on class membership are partially in line with one previous study on people bereaved through the MH-17 aeroplane disaster (Lenferink et al., 2017). However, in addition to a CG class, a comorbid PTSD/CG class, and a resilient class, we identified two additional classes, namely partial PTSD/CG and partial CG. The increased specificity offered by a symptom-based instead of a cluster-based LCA in a much larger disaster-bereaved sample has probably allowed for the detection of these two additional classes. Both of these partial CG classes showed high probabilities for a number of grief symptoms that are currently considered to be core symptoms of ICD-11 PGD (World Health Organization, 2018) and DSM-5 PCBD (American Psychiatric Association, 2013), and reporting only these symptoms (e.g. longing, cognitive preoccupation, non-acceptance) would qualify a person to receive a diagnosis of PGD, but not PCBD. Potentially, the current lenient criteria for PGD in ICD-11 would yield higher prevalence rates of pathological grief among disaster-bereaved individuals than the stricter PCBD criteria, as has been shown in other bereaved samples (Boelen, Lenferink, Nickerson, & Smid, 2018; Mauro et al., in press; for a discussion, see Eisma & Lenferink, 2017).
The identification of partial (or subthreshold) PTSD and CG classes in the present study is notable. While little is known about the correlates of subthreshold CG, a systematic review demonstrated that the experience of subthreshold PTSD is associated with a wide range of negative outcomes, including higher healthcare utilization, increased feelings of hopelessness, and an increased risk of suicidality (Brancu et al., 2016). Moreover, subthreshold PTSD may persist over long periods of time and could eventually evolve into delayed-onset PTSD (Cukor, Wyka, Jayasinghe, & Difede, 2010; Smid, Mooren, van der Mast, Gersons, & Kleber, 2009). The identification of people experiencing partial PTSD and/or CG following disasters, and increasing attention for the treatment of these distinct symptom patterns, appears to be a worthwhile goal for future research.
Comparing our results against two studies including forcibly displaced people who had experienced multiple potentially traumatic events, including (traumatic) losses of significant others, one notable difference is that we found no evidence for a fourth PTSD-only class reported in these studies (Heeke et al., 2017; Nickerson et al., 2014). Possibly, the high number of repeated traumatic stressful events experienced by forcibly displaced people, such as torture, imprisonment, and kidnapping, could result in an additional group uniquely presenting with PTSD symptoms, whereas a natural disaster, involving sudden and often multiple deaths of family members and friends, does not result in this specific class. However, it may also be that cultural differences between samples, to some extent, account for these different results. Perhaps findings in Arabic and Columbian people exposed to armed conflict simply do not generalize to natural disaster survivors from China.
With regard to the correlates of class membership, the finding that female gender differentiated the CG class from the Resilient class, and that the loss of a spouse and/or one or more children (compared to other types of loss) is associated with a higher likelihood of CG class membership compared to the Resilient class, the Partial PTSD/CG class, and the Partial CG class, is largely compatible with findings from a review on risk factors for CG following bereavement (Burke & Neimeyer, 2013). The disappearance of a significant other was the only factor associated with (a reduced) likelihood of being in the CG class compared to the PTSD/CG class, which corresponds with a growing body of research demonstrating the severe mental health consequences that may ensue following this ambiguous type of loss (for a review, see Lenferink, de Keijser, Wessel, de Vries, & Boelen, in press). Given that all participants in this study had also experienced bereavement, our study uniquely demonstrates that having a missing relative in addition to bereavement may be a risk factor for the development of comorbid CG and PTSD. Future studies on disaster-related mental health should also assess both types of losses separately, to take such effects into account. Being physically injured during the earthquake was further demonstrated to be associated with membership of the CG symptom class compared to the Resilient and Partial CG classes. It is not so clear why injuries are also related to CG class membership. One explanation may be that people who are injured in the earthquake are also more likely to experience and be witness to the violent deaths of people who were in the same place as them when the earthquake struck, such as their family members, friends, and colleagues. It could also be that coping with physical injury leaves fewer resources available to effectively cope with bereavement.
This study has some clear clinical implications. It provides strong evidence that exclusively screening for PTSD in survivors of a natural disaster with massive casualties may yield an incomplete picture of the mental health problems experienced by this group. Survivors of earthquakes commonly report very high prevalence rates of CG (Li et al., 2015; Neria et al., 2007), and the present study extends this finding by showing that distinct subgroups (e.g. experiencing CG but no comorbid PTSD symptoms) may be missed if disaster mental health services focus solely on assessing and treating PTSD. This may be particularly problematic as some previous research indicates that grief-specific treatments are more effective in treating people suffering from CG than treatments developed for other disorders, such as depression (e.g. Shear, Frank, Houck, & Reynolds, 2005). Specifically, evidence is mounting that therapist-guided internet-based and face-to-face cognitive–behavioural treatment for CG, which may consist of loss-related exposure, challenging negative loss-related cognitions, and behavioural activation and/or goal setting, is efficacious (for a review, see Doering & Eisma, 2016). Based on the present data, we recommend that mental health services for survivors of natural disasters involving massive casualties are systematically screened for CG. Should survivors with CG indicate a need for treatment, one group may require eclectic PTSD and CG treatment, one group could fare best with CG-specific treatments, and partial PTSD/CG and partial CG groups could potentially benefit from other approaches, focused on the prevention of more severe mental health problems (e.g. Litz et al., 2014).
This study had a number of limitations. First, while the focus on a non-Western sample is a major strength of this study, it is unclear to what extent the present findings generalize to people with different cultural backgrounds. Relatedly, educational levels were relatively low. We found that people in the CG class were, on average, less likely to have a high educational level than participants in the Partial PTSD/CG class, which may imply that conducting a similar study in a sample with higher educational levels would yield different findings. Secondly, while the ICG is one of the most frequently used measures for CG symptoms, it does not assess all criteria for currently established or proposed grief-related disorders, including PGD for ICD-11 (World Health Organization, 2018) or PCBD in the DSM-5 (American Psychiatric Association, 2013). Similarly, the PCL is a psychometrically valid instrument to assess PTSD, but since it is based on DSM-IV PTSD criteria, it does not correspond entirely with DSM-5 PTSD criteria. Thirdly, we considered a limited number of correlates of class membership. Future research may include other relevant variables, such as the number of traumatic events and/or losses that were experienced (Heeke et al., 2017), or therapeutically changeable variables, such as negative cognitions (Boelen, Reijntjes, Djelantik, & Smid, 2016).
In conclusion, the present investigation is the largest LCA study to date examining symptom profiles of CG and PTSD following bereavement, and to the best of our knowledge also the only study applying this technique in survivors of a natural disaster. Theoretically, the results support the viewpoint that CG is a distinct mental health problem in (traumatically) bereaved individuals. Clinically, the findings provide indications that CG may be a unique and overlooked consequence of disasters involving massive casualties, such as earthquakes. We recommend that disaster mental health services should systematically screen for CG, and treat it with established therapeutic methods when indicated.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). Arlington, VA: American Psychiatric Association Publishing. [Google Scholar]
- Blanchard E. B., Jones-Alexander J., Buckley T. C., & Forneris C. A. (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34, 669–12. [DOI] [PubMed] [Google Scholar]
- Boelen P. A., Lenferink L. I., Nickerson A., & Smid G. E. (2018). Evaluation of the factor structure, prevalence, and validity of disturbed grief in DSM-5 and ICD-11. Journal of Affective Disorders, 240, 79–87. [DOI] [PubMed] [Google Scholar]
- Boelen P. A., Reijntjes A., Djelantik A. M. J., & Smid G. E. (2016). Prolonged grief and depression after unnatural loss: Latent class analyses and cognitive correlates. Psychiatry Research, 240, 358–363. [DOI] [PubMed] [Google Scholar]
- Bowler R. M., Han H., Gocheva V., Nakagawa S., Alper H., Digrande L., & Cone J. E. (2010). Gender differences in probable posttraumatic stress disorder among police responders to the 2001 World Trade Center terrorist attack. American Journal of Industrial Medicine, 53, 1186–1196. [DOI] [PubMed] [Google Scholar]
- Brancu M., Mann-Wrobel M., Beckham J. C., Wagner H. R., Elliott A., Robbins A. T., … Runnals J. J. (2016). Subthreshold posttraumatic stress disorder: A meta-analytic review of DSM–IV prevalence and a proposed DSM–5 approach to measurement. Psychological Trauma: Theory, Research, Practice, and Policy, 8(2), 222–232. [DOI] [PubMed] [Google Scholar]
- Breslau N., Reboussin B. A., Anthony J. C., & Storr C. L. (2005). The structure of posttraumatic stress disorder: Latent class analysis in 2 community samples. Archives of General Psychiatry, 62, 1343–1351. [DOI] [PubMed] [Google Scholar]
- Burke L. A., & Neimeyer R. A. (2013). Prospective risk factors for complicated grief: A review of the empirical literature In Stroebe M. S., Schut H., & van Den Bout J. (Eds.), Complicated grief: Scientific foundations for healthcare professionals (pp. 145–161). Washington, DC: American Psychological Association. [Google Scholar]
- Chan C. L., Wang C.-W., Ho A. H., Qu Z.-Y., Wang X.-Y., Ran M.-S., … Zhang X.-L. (2012). Symptoms of posttraumatic stress disorder and depression among bereaved and non-bereaved survivors following the 2008 Sichuan earthquake. Journal of Anxiety Disorders, 26, 673–679. [DOI] [PubMed] [Google Scholar]
- Cukor J., Wyka K., Jayasinghe N., & Difede J. (2010). The nature and course of subthreshold PTSD. Journal of Anxiety Disorders, 24, 918–923. [DOI] [PubMed] [Google Scholar]
- Djelantik A. M. J., Smid G. E., Kleber R. J., & Boelen P. A. (2017). Symptoms of prolonged grief, post-traumatic stress, and depression after loss in a Dutch community sample: A latent class analysis. Psychiatry Research, 247, 276–281. [DOI] [PubMed] [Google Scholar]
- Doering B. K., & Eisma M. C. (2016). Treatment for complicated grief: State of the science and ways forward. Current Opinion in Psychiatry, 29(5), 286–291. [DOI] [PubMed] [Google Scholar]
- Eisma M. C., & Lenferink L. I. M. (2017). Response to: Prolonged grief disorder in ICD-11: The primacy of clinical utility and international applicability. European Journal of Psychotraumatology, 8(6), 1512249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaffari-Nejad A., Ahmadi-Mousavi M., Gandomkar M., & Reihani-Kermani H. (2007). The prevalence of complicated grief among Bam earthquake survivors in Iran. Archives of Iranian Medicine, 10, 525–528. [PubMed] [Google Scholar]
- Goenjian A. K., Steinberg A. M., Najarian L. M., Fairbanks L. A., Tashjian M., & Pynoos R. S. (2000). Prospective study of posttraumatic stress, anxiety, and depressive reactions after earthquake and political violence. The American Journal of Psychiatry, 157, 911–916. [DOI] [PubMed] [Google Scholar]
- Gouweloos J., Postma I. L., Te Brake H., Sijbrandij M., Kleber R. J., & Goslings J. C. (2016). The risk of PTSD and depression after an airplane crash and its potential association with physical injury: A longitudinal study. Injury, 47, 250–256. [DOI] [PubMed] [Google Scholar]
- Hansen M., Ross J., & Armour C. (2017). Evidence of the dissociative pTSD subtype: A systematic literature review of latent class and profile analytic studies of PTSD. Journal of Affective Disorders, 213, 59–69. [DOI] [PubMed] [Google Scholar]
- Heeke C., Stammel N., Heinrich M., & Knaevelsrud C. (2017). Conflict-related trauma and bereavement: Exploring differential symptom profiles of prolonged grief and posttraumatic stress disorder. BMC Psychiatry, 17, 118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johannesson K. B., Lundin T., Fröjd T., Hultman C. M., & Michel P.-O. (2011). Tsunami-exposed tourist survivors: Signs of recovery in a 3-year perspective. The Journal of Nervous and Mental Disease, 199, 162–169. [DOI] [PubMed] [Google Scholar]
- Kristensen P., Weisæth L., & Heir T. (2009). Psychiatric disorders among disaster bereaved: An interview study of individuals directly or not directly exposed to the 2004 tsunami. Depression and Anxiety, 26, 1127–1133. [DOI] [PubMed] [Google Scholar]
- Kristensen P., Weisæth L., & Heir T. (2012). Bereavement and mental health after sudden and violent losses: A review. Psychiatry: Interpersonal and Biological Processes, 75, 76–97. [DOI] [PubMed] [Google Scholar]
- Kristensen P., Weisæth L., Hussain A., & Heir T. (2015). Prevalence of psychiatric disorders and functional impairment after loss of a family member: A longitudinal study after the 2004 Tsunami. Depression and Anxiety, 32, 49–56. [DOI] [PubMed] [Google Scholar]
- Kun P., Chen X., Han S., Gong X., Chen M., Zhang W., & Yao L. (2009). Prevalence of post-traumatic stress disorder in Sichuan Province, China after the 2008 Wenchuan earthquake. Public Health, 123, 703–707. [DOI] [PubMed] [Google Scholar]
- Lee S. H., Kim E. J., Noh J.-W., & Chae J.-H. (2018). Factors associated with post-traumatic stress symptoms in students who survived 20 months after the Sewol ferry disaster in Korea. Journal of Korean Medical Science, 33, e90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenferink L. I. M., de Keijser J., Smid G. E., Djelantik A. M. J., & Boelen P. A. (2017). Prolonged grief, depression, and posttraumatic stress in disaster-bereaved individuals: Latent class analysis. European Journal of Psychotraumatology, 8, 1298311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenferink L. I. M., de Keijser J., van Denderen M., & Boelen P. A. (in press). Latent classes of posttraumatic stress symptoms in two samples of bereaved people. International Journal of Stress Management. Advance online publication. doi: 10.1037/str0000121 [DOI] [Google Scholar]
- Lenferink L. I. M, de Keijser J, Wessel I, de Vries D, & Boelen P. A. (in press). Toward a better understanding of psychological symptoms in people confronted with the disappearance of a loved one: a systematic review. Trauma, Violence, & Abuse. doi: 10.1177/1524838017699602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Chow A. Y., Shi Z., & Chan C. L. (2015). Prevalence and risk factors of complicated grief among Sichuan earthquake survivors. Journal of Affective Disorders, 175, 218–223. [DOI] [PubMed] [Google Scholar]
- Li J., & Prigerson H. G. (2016). Assessment and associated features of prolonged among Chinese bereaved individuals. Comprehensive Psychiatry, 66, 9–16. [DOI] [PubMed] [Google Scholar]
- Liang Y., Cheng J., Ruzek J. I., & Liu Z. (2019). Posttraumatic stress disorder following the 2008 Wenchuan earthquake: A 10-year systematic review among highly exposed populations in China. Journal of Affective Disorders, 243, 327–339. [DOI] [PubMed] [Google Scholar]
- Litz B. T., Schorr Y., Delaney E., Au T., Papa A., Fox A. B., … Prigerson H. G. (2014). A randomized controlled trial of an internet-based therapist-assisted indicated preventive intervention for prolonged grief disorder. Behaviour Research and Therapy, 61, 23–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu A., Tan H., Zhou J., Li S., Yang T., Wang J., … Wen S. W. (2006). An epidemiologic study of posttraumatic stress disorder in flood victims in Hunan China. The Canadian Journal of Psychiatry, 51, 350–354. [DOI] [PubMed] [Google Scholar]
- Maccallum F., & Bryant R. A. (in press). Symptoms of prolonged grief and posttraumatic stress following loss: A latent class analysis. Australian and New Zealand Journal of Psychiatry. Advance online publication. doi: 10.1177/0004867418768429 [DOI] [PubMed] [Google Scholar]
- Mauro C., Reynolds C. F., Maercker A., Skritskaya N., Simon N., Zisook S., … Shear M. K. (in press). Prolonged grief disorder: Clinical utility of ICD-11 diagnostic guidelines. Psychological Medicine. Advance online publication. doi: 10.1017/S0033291718001563 [DOI] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O. (2007). Re: What is a good value of entropy. [Online comment] Retrieved from http://www.statmodel.com/discussion/messages/13/2562.html?1237580237
- Neria Y., Gross R., Litz B., Maguen S., Insel B., Seirmarco G., … Cook J. (2007). Prevalence and psychological correlates of complicated grief among bereaved adults 2.5–3.5 years after September 11th attacks. Journal of Traumatic Stress, 20, 251–262. [DOI] [PubMed] [Google Scholar]
- Nickerson A., Liddell B. J., Maccallum F., Steel Z., Silove D., & Bryant R. A. (2014). Posttraumatic stress disorder and prolonged grief in refugees exposed to trauma and loss. BMC Psychiatry, 14, 106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris F. H., Murphy A. D., Baker C. K., & Perilla J. L. (2004). Postdisaster PTSD over four waves of a panel study of Mexico’s 1999 flood. Journal of Traumatic Stress, 17, 283–292. [DOI] [PubMed] [Google Scholar]
- Nylund K. L., Asparouhov T., & Muthén B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14, 535–569. [Google Scholar]
- Prigerson H. G., Maciejewski P. K., Reynolds C. F., Bierhals A. J., Newsom J. T., Fasiczka A., … Miller M. (1995). Inventory of Complicated Grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research, 59, 65–79. [DOI] [PubMed] [Google Scholar]
- Roussos A., Goenjian A. K., Steinberg A. M., Sotiropoulou C., Kakaki M., Kabakos C., ., & Manouras V. (2005). Posttraumatic stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia, Greece. The American Journal of Psychiatry, 162, 530–537. [DOI] [PubMed] [Google Scholar]
- Ruggiero K. J., Del Ben. K, Scotti J. R., & Rabalais A. E. (2003). Psychometric properties of the ptsd checklist—civilian version. Journal of Traumatic Stress, 16(5), 495––502.. [DOI] [PubMed] [Google Scholar]
- Shear K., Frank E., Houck P. R., & Reynolds C. F. (2005). Treatment of complicated grief: A randomized controlled trial. JAMA, 293, 2601–2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shear M. K., McLaughlin K. A., Ghesquiere A., Gruber M. J., Sampson N. A., & Kessler R. C. (2011). Complicated grief associated with Hurricane Katrina. Depression and Anxiety, 28, 648–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smid G. E., Mooren T. T., van der Mast R. C., Gersons B. P., & Kleber R. J. (2009). Delayed posttraumatic stress disorder: Systematic review, meta-analysis, and meta-regression analysis of prospective studies. The Journal of Clinical Psychiatry, 70, 1572–1582. [DOI] [PubMed] [Google Scholar]
- Thienkrua W., Cardozo B. L., Chakkraband M. S., Guadamuz T. E., Pengjuntr W., Tantipiwatanaskul P., … Varangrat A. (2006). Symptoms of posttraumatic stress disorder and depression among children in tsunami-affected areas in southern Thailand. JAMA, 296, 549–559. [DOI] [PubMed] [Google Scholar]
- van de Schoot R., Sijbrandij M., Winter S. D., Depaoli S., & Vermunt J. K. (2017). The GRoLTS-checklist: Guidelines for reporting on latent trajectory studies. Structural Equation Modeling, 24, 451–467. [Google Scholar]
- Vermunt J. K. (2010). Latent class modeling with covariates: Two improved three-step approaches. Political Analysis, 18, 450–469. [Google Scholar]
- Vermunt J. K., & Magidson J. (2013). Latent GOLD 5.0 upgrade manual. Belmont, MA: Statistical Innovations Inc. [Google Scholar]
- Wei B., Hu X., & Chen J (1994). Data analysis on the prevalence of psychiatric mental disorder in mianyang city. Sichuan Mental Health (In Chinese), 7(1), 50––51.. [Google Scholar]
- World Health Organization (2018). ICD-11 Beta Draft. Prolonged grief disorder criteria. Retrieved from https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1183832314
- Wu K., Chan S., & Yiu V. F. (2008). Psychometric properties and confirmatory factor analysis of the posttraumatic stress disorder checklist for Chinese survivors of road traffic accidents. Hong Kong Journal of Psychiatry, 18, 144–152. [Google Scholar]
- Zhao Z., Cui D., Yu S., & Zhong J. (2012). Seismic casualty assessment for Wenchuan earthquake. World Earthquake Engineering, 28, 20–25. [Google Scholar]


