Abstract
Objectives
To estimate rates and national trends of initiation of new psychotropic medications without a psychiatric diagnosis and to identify demographic and clinical correlates independently associated with such use among US adults in outpatient settings.
Data Source
Data were gathered from the 2006‐2015 National Ambulatory Medical Care Survey (NAMCS), a nationally representative sample of office‐based U.S. outpatient care. The sample was limited to adults aged 18 or older who received a new psychotropic drug prescription (n = 8618 unweighted).
Study Design
Using a repeated cross‐sectional design with survey sampling techniques, we estimated prescription initiation rates and national trends. Multivariable‐adjusted logistic regression analysis was used to identify correlates independently associated with initiation of new psychotropic prescriptions without a psychiatric diagnosis.
Data Collection/Extraction Methods
Data were publicly available, and we extracted them from the Centers for Disease Control and Prevention website.
Principal Findings
Altogether, at 60.4% of visits at which a new psychotropic prescription was initiated, no psychiatric diagnosis was recorded for the visit. Overall, the rate increased from 59.1% in 2006‐2007 to 67.7% in 2008‐2009 and then decreased to 52.0% in 2014‐2015. Visits to psychiatrists were associated with very low odds of having no psychiatric diagnosis when compared to primary care visits (OR = 0.02; 95% CI, 0.01‐0.04). Visits to non‐psychiatric specialists showed 6.90 times greater odds of not having a psychiatric diagnosis when compared to primary care visits (95% CI, 5.38‐8.86).
Conclusion
New psychotropic medications are commonly initiated without any psychiatric diagnosis, especially by non‐psychiatrist physicians. Non‐psychiatrists should document relevant diagnoses more vigilantly to prevent potentially inappropriate use or misuse.
Keywords: prescribing patterns, prescription, psychiatric diagnosis, psychotropic
1. INTRODUCTION
The use of prescription psychotropic medications has increased steadily over the past two decades,1, 2, 3, 4 driven, in large part, by the increased prescribing of these medications by non‐psychiatrists.5, 6 In 2013, about one in six U.S. adults reported taking psychotropic medications at least once.4 Since 2010, the Food and Drug Administration (FDA) has approved at least 15 new or existing psychotropic drugs for psychiatric diagnoses,7 and average nationwide annual spending for all psychotropic medications as a proportion of all health costs estimated to be around 3% per year.8
Previous studies have reported, unexpectedly, that a large proportion of psychotropics are prescribed to patients who do not have any psychiatric diagnosis, even without consideration of whether the particular psychiatric diagnosis represents a specific approved indication for the specific prescribed drug.3, 9, 10 One study investigating national antidepressant prescribing trends found that the proportion of visits in which antidepressants were prescribed without any accompanying psychiatric diagnosis increased from 59.5% to 72.7% between 1996 and 2007 in office‐based care settings.3 Similarly, a study using 2009 MarketScan® commercial claims data reported that 58% of individuals aged 18 to 64 with psychotropic prescriptions did not have a psychiatric diagnosis during the year in which the medication was prescribed.9 Similar findings were found using 2010 national data from the Veterans Health Administration.10
Such prescribing practices generate concern for several reasons. First, the lack of any psychiatric diagnostic indication may reflect off‐label or unjustified use of medications that may not be effective for a given problem and which impose a risk of significant adverse drug events. For example, many psychotropics have strong anticholinergic properties that can cause constipation, urinary retention, or delirium in older adults.11, 12 In addition, both first‐ and second‐generation antipsychotics require careful drug administration, as they can cause significant sedation, metabolic morbidity, and even mortality in older adults with dementia, for example.13, 14 Third, in the absence of a psychiatric diagnosis, it is possible that addictive psychotropics are being used without justification and may pose an unnecessary risk of abuse to population health.
Earlier studies acknowledged several methodological limitations.3, 9, 10, 15, 16, 17 First, these studies did not distinguish between psychotropic prescriptions that represented initiation of a new drug as contrasted with renewal or continuation of an old one. While some long continuing prescriptions may understandably have been renewed without specification of a justifying psychiatric diagnosis, the initiation of new psychotropic use without any, even remotely, relevant diagnosis suggests either careless prescribing or frank misuse of medications, issues of great concern.3, 9, 10, 15, 16, 17 Second, some studies only investigated the antidepressant drug class3, 15, 16, 17 and did not evaluate other psychotropic classes such as antipsychotics and anxiolytics that may represent even greater risks. Third, some of these studies were limited to younger adult populations,9 or focused on older male veterans,10 and thus have limited generalizability in terms of population or study settings. Finally, all of these studies used data from years prior to 2010, and time trends need updating.
To address these gaps in the literature, we used data from the specific visits at which new psychotropic medications in three classes (antidepressants, antipsychotics, and anxiolytics) were initiated to answer the following questions: (a) What were the national rates of initiating psychotropic prescriptions in these classes without a psychiatric diagnosis in the years from 2006 to 2015? (b) For which medical specialties and psychotropic medication classes was prescription in these classes without a diagnosis most common? And finally, (c) What other demographic and clinical characteristics are independently associated with the initiation of new psychotropic prescriptions in these classes without a psychiatric diagnosis? This is thus the first pharmacoepidemiologic study to investigate national trends in the initiation of new psychotropic prescriptions without a concurrent psychiatric diagnosis in office‐based outpatient settings, and provides a benchmark for tracking future use of psychiatric diagnosis and for developing policies that promote more diligent prescribing.
2. METHODS
2.1. Data source and study sample
Data were obtained from the 2006‐2015 National Ambulatory Medical Care Surveys (NAMCS), administrated by National Center for Health Statistics of the Centers for Disease Control and Prevention.18 The NAMCS is an annual, cross‐sectional survey of visits to office‐based physicians in outpatient settings and nationally represents office‐based outpatient medical care in the United States.18 We limited the sample to adults ages 18 or older who received new psychotropic medication prescriptions (n = 9467 unweighted). We further excluded observations with any missing covariates (9.0%), presumed to be missing at random, leaving a final sample size of 8618. Because we used publicly available deidentified data, this study was exempted by the Institutional Review Board (#2000021850) at Yale School of Medicine. Further details of the survey, including descriptions, questionnaires, sampling methodology, and datasets, are publicly available on the NAMCS website.19
2.2. Measures
2.2.1. Psychotropic medications
The NAMCS collected up to eight medications prescribed in 2006‐2011, up to 10 medications in 2012‐2013, and up to 30 medications in 2014‐2015. We examined the first eight medications listed as prescribed for each visit, ensuring consistency across years.3, 20, 21, 22 For each medication, there is a status indicator variable whether the prescribed medication is newly prescribed at that visit, continued from previous visits, or unknown. We considered new prescribed psychotropic medications to represent the “initiation” of psychotropic treatment at the visit in question. We classified psychotropic prescriptions considered in this study into three groups using the following generic names:23 (a) Antipsychotics included haloperidol, chlorpromazine, fluphenazine, perphenazine, prochlorperazine, thioridazine, trifluoperazine, thiothixene, loxapine, molindone, pimozide, aripiprazole, asenapine, clozapine, iloperidone, lurasidone, olanzapine, paliperidone, quetiapine, risperidone, and ziprasidone; (b) antidepressants included amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, maprotiline, nortriptyline, protriptyline, trimipramine, nefazodone, trazodone, vilazodone, vortioxetine, citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline, phenelzine, tranylcypromine, rasagiline, selegiline, desvenlafaxine, duloxetine, levomilnacipran, venlafaxine, milnacipran, bupropion, and mirtazapine; and (c) anxiolytics included amobarbital sodium, butabarbital sodium, pentobarbital, phenobarbital, secobarbital, alprazolam, chlordiazepoxide, clorazepate, diazepam, estazolam, flurazepam, lorazepam, midazolam HCL, oxazepam, quazepam, temazepam, triazolam, clonazepam, buspirone HCL, chloral hydrate, dexmedetomidine, droperidol, hydroxyzine, meprobamate, promethazine, suvorexant, diphenhydramine HCL, doxylamine, and propofol.
2.2.2. Mental health conditions
The NAMCS collects up to three clinical diagnoses using the International Classification of Diseases, 9th edition, Clinical Modification (ICD‐9‐CM) diagnostic codes. We constructed several indicator variables for clinical indications most relevant to psychotropic prescriptions. Psychiatric diagnoses were classified into five groups: (a) major depressive disorder (MDD; 296.20‐296.30); (b) depressive disorders other than MDD (296.90, 296.99, 301‐10‐301.13, 300.4, 311); (c) anxiety disorder (300.00‐300.09); (d) post‐traumatic stress disorder (309.81); and (e) others, including dementia (290, 294.10‐294.11, 294.20‐294.21, 331.19, 331.82, 331.0), mild cognitive impairment (331.83), schizophrenia (295), bipolar disorders (296.00‐296.16, 296.40‐296.80, 296.89), adjustment disorders (309.0‐309.4, 309.82‐309.9), personality disorders (301.0, 301.20‐301.22, 301.3, 301.4, 301.50, 301.59, 301.6, 301.7, 301.8‐301.9), other psychoses (297‐299), and psychiatric diagnoses otherwise (290‐319), all of which were identified for less than 1% of patient visits. For substance use disorders, we constructed variables for seven specific substance use disorders (alcohol, opiates, cocaine, cannabis, barbiturates, amphetamines, and hallucinogens) using ICD‐9‐CM diagnostic codes.24 We also constructed an indicator variable representing non‐psychiatric FDA‐approved indications for psychotropic drugs (eg, off‐label use), which included seizures (345, 780.31‐780.39), insomnia (780.51‐780.52, 327.0), migraine and headache (346, 784.0), pain and neuropathy (250.6, 357.2, 337.1, 338, 719.4, 780.96, 729.1, 728.85, 781.0, 053.12, 729.2, 352.1, 350.1), narcolepsy (347), nausea and vomiting (787.0), and pruritus (698) (I. L. Petrakis, M. Sofuoglu, R. A. Rosenheck, under review).
2.2.3. Covariates
Demographic variables documented age (18‐44, 45‐64, 65‐74, 75+), gender, race/ethnicity (non‐Hispanic white, non‐Hispanic black, Hispanics, or other), region of residence (Northeast, Midwest, South, or West), primary source of payment (Private, Medicare, Medicaid, or other), reason for visit (acute problem, routine chronic problem, preventive care, or pre‐ or post‐surgery care), and number of repeat visits within the past 12 months (none, 1‐2, 3‐5, or 6+). Additional characteristics documented included physician specialty (primary care, psychiatry, or other), metropolitan statistical area (MSA) status (yes/no), receipt of psychotherapy or mental health counseling (yes/no), time spent with a doctor (<15, 15‐20, 21‐30, or >30 min), number of chronic conditions (1, 2‐3, or 4+), and the total number of medications documented on the NAMCS (0‐3, 4‐5, or 6+). The number of chronic conditions was based on 14 chronic conditions (yes/no) collected by the NAMCS (eg, arthritis, congestive heart failure, and diabetes).
2.3. Data analysis
First, we compared patients for whom new psychotropic medications were initiated who had a psychiatric diagnosis with patients who did not have a psychiatric diagnosis. Due to the large sample size, bivariate significance testing (eg, Pearson's chi‐square statistic) can be misleading because even small or trivial differences are likely to produce statistically significance results (P < 0.001). For this reason, we reported risk ratios to quantify effect size.25 A risk ratio of 1.0 indicates no difference in risk of having no psychiatric diagnosis between the two groups defined by a particular characteristics. Greater than 1.0 indicates that those with the characteristic had a higher likelihood of initiating psychotropic medications without a diagnosis than those with a diagnosis.
Second, we estimated prescription initiation rates of psychotropic medications without a psychiatric diagnosis over the years from 2006 to 2015. We further stratified these trends by psychotropic class to investigate prescribing trends without a psychiatric diagnosis for each class of medications. Lastly, we used multivariable‐adjusted logistic regression analysis to identify demographic and clinical correlates independently associated with having a new psychotropic medication prescribed with no psychiatric diagnosis. In this analysis, we only included variables that had risk ratios greater than 1.20 or less than 0.80. We used Stata 15.1 (Stata Corp., College Station, TX, USA)26 for all analyses, and we employed the svy commands in Stata to account for the complex survey sampling design of the NAMCS (ie, unequal probability of selection, clustering, and stratification).
3. RESULTS
3.1. Selected characteristics of the sample
Of all visits by U.S. adults, psychotropic prescriptions were written at 19.4% of visits between 2006 and 2015. Altogether, 60.4% of visits at which a new psychotropic prescription was initiated did not record any psychiatric diagnosis at that visit. Tables 1 and 2 present demographic and clinical characteristics of visits initiated new psychotropic medication use without a psychiatric diagnosis. Overall, the majority of visits were made by younger adults ages between 18 and 64 (74.9%). However, adults aged 65 or older had a risk ratio of 1.47 or higher for receiving psychotropic prescriptions without a psychiatric diagnosis when compared to adults aged 18‐44 (Table 1). Considering physician specialty, visits to psychiatrists had a risk ratio of only 0.04 of receiving a psychotropic prescription without a psychiatric diagnosis when compared to the reference group, primary care visits. Visits with specialists other than psychiatrists had a risk ratio of 1.57 of receiving psychotropic prescriptions without a psychiatric diagnosis when compared to primary care visits. Having three to five and six or more concomitant medications prescribed was associated with risk ratios of 1.39 and 1.76 of receiving a psychotropic prescription without a psychiatric diagnosis, respectively, when compared to <3 medications concomitantly prescribed.
Table 1.
Weighted selected characteristics of US adults aged 18 or older with initiation of psychotropic prescriptions in office‐based outpatient settings, 2006‐2015 NAMCS
| All visits (N) | Column percentage of all visits | Without a psychiatric diagnosis (n) | Row percentage of no psychiatric diagnosis of all visits (%) | Risk ratio (reference condition = 1.00) | |
|---|---|---|---|---|---|
| Sample size (row %) | |||||
| Unweighted sample | 8618 | 100.0 | 5227 | 60.7 | |
| Weighted visits | 22 498 475 | 100.0 | 13 584 867 | 60.4 | |
| Age | |||||
| 18‐44 | 9 067 847 | 32.9 | 4 475 391 | 49.4 | Reference |
| 45‐64 | 8 767 848 | 42.0 | 5 711 662 | 65.1 | 1.32 |
| 65‐74 | 2 510 135 | 13.4 | 1 819 667 | 72.5 | 1.47 |
| 75+ | 2 152 644 | 11.6 | 1 578 147 | 73.3 | 1.49 |
| Gender | |||||
| Male | 7 527 092 | 31.9 | 4 998 501 | 66.4 | Reference |
| Female | 14 971 383 | 68.1 | 10 270 274 | 68.6 | 1.03 |
| Race/ethnicity | |||||
| Non‐Hispanic white | 17 295 675 | 76.8 | 10 427 975 | 60.3 | Reference |
| Non‐Hispanic black | 2 028 931 | 8.8 | 1 195 120 | 58.9 | 0.98 |
| Hispanic | 2 225 878 | 10.3 | 1 393 968 | 62.6 | 1.04 |
| Othera | 947 990 | 4.2 | 567 804 | 59.9 | 0.99 |
| Region | |||||
| Northeast | 4 148 797 | 18.4 | 2 452 795 | 59.1 | Reference |
| Midwest | 4 528 529 | 19.9 | 2 720 545 | 60.1 | 1.02 |
| South | 9 073 191 | 40.4 | 5 574 362 | 61.4 | 1.04 |
| West | 4 747 958 | 21.4 | 2 837 166 | 59.8 | 1.01 |
| Source of payment | |||||
| Private | 13 193 467 | 58.8 | 7 986 879 | 60.5 | Reference |
| Medicare | 5 052 891 | 25.2 | 3 426 054 | 67.8 | 1.12 |
| Medicaid | 2 004 322 | 7.4 | 1 011 244 | 50.5 | 0.83 |
| Otherb | 2 247 796 | 8.5 | 1 160 690 | 51.6 | 0.85 |
| Reason for visit | |||||
| Acute problem | 8 325 426 | 37.2 | 5 562 728 | 66.8 | Reference |
| Routine chronic problem | 10 532 579 | 46.4 | 5 432 677 | 51.6 | 0.77 |
| Preventive care | 2 941 596 | 13.3 | 1 927 061 | 65.5 | 0.98 |
| Pre‐ or post‐surgery | 698 875 | 3.1 | 662 401 | 94.8 | 1.42 |
| Repeat of visits in the past 12 mo | |||||
| 0 visit | 1 531 633 | 7.2 | 981 289 | 64.1 | Reference |
| 1‐2 visits | 8 217 303 | 36.4 | 4 943 891 | 60.2 | 0.94 |
| 3‐5 visits | 7 015 176 | 31.6 | 4 291 595 | 61.2 | 0.95 |
| 6+ visits | 5 734 363 | 24.8 | 3 368 093 | 58.7 | 0.92 |
| Physician specialty | |||||
| Primary care | 13 343 476 | 56.4 | 7 660 805 | 57.4 | Reference |
| Psychiatry | 2 632 497 | 0.4 | 56 044 | 2.1 | 0.04 |
| Otherc | 6 522 502 | 43.2 | 5 868 018 | 90.0 | 1.57 |
| Metropolitan statistical area (MSA) | |||||
| MSA | 19 877 253 | 89.0 | 12 092 027 | 60.8 | Reference |
| Non‐MSA | 2 621 222 | 11.0 | 1 492 840 | 57.0 | 0.94 |
| Mental health counseling and psychotherapy | |||||
| No | 20 249 204 | 99.0 | 13 446 934 | 66.4 | Reference |
| Yes | 2 249 271 | 1.0 | 137 933 | 6.1 | 0.09 |
| Time spent with doctor | |||||
| <15 min | 3 397 901 | 15.0 | 2 042 805 | 60.1 | Reference |
| 15‐20 min | 10 238 764 | 47.3 | 6 425 729 | 62.8 | 1.04 |
| 21‐30 min | 5 187 371 | 23.6 | 3 200 891 | 61.7 | 1.03 |
| >30 min | 3 674 439 | 14.1 | 1 915 442 | 52.1 | 0.87 |
| Multiple chronic conditions | |||||
| None | 5 804 526 | 30.6 | 4 151 811 | 71.5 | Reference |
| 1 | 7 743 151 | 28.6 | 3 882 490 | 50.1 | 0.70 |
| 2‐3 | 7 101 673 | 30.9 | 4 202 545 | 59.2 | 0.83 |
| 4+ | 1 849 125 | 9.9 | 1 348 020 | 72.9 | 1.02 |
| Number of medications | |||||
| <3 | 7 854 367 | 25.8 | 3 498 788 | 44.5 | Reference |
| 3‐5 | 8 610 092 | 39.3 | 5 342 083 | 62.0 | 1.39 |
| 6+ | 6 034 016 | 34.9 | 4 743 997 | 78.6 | 1.76 |
Asians, American Indian/Alaska Natives (AIANs), Native Hawaiian or Other Pacific Islanders (NHOPI), and other mixed racial groups.
Worker's compensation, self‐pay, no charge, and others.
General surgery, obstetrics/gynecology, orthopedic surgery, cardiovascular diseases, dermatology, urology, neurology, ophthalmology, otolaryngology, and others.
Table 2.
Weighted characteristics of initiating psychotropic medication use without a psychiatric diagnosis in US adults aged 18 or in office‐based outpatient settings, 2006‐2015 NAMCS
| All visits (N) | Column percentage of all visits (%) | Without a psychiatric diagnosis (n) | Row percentage of no psychiatric diagnosis of all visits (%) | Column percentage of no psychiatric diagnosis of all visits (%) | Bivariate risk ratio for having no psychiatric diagnosis | |
|---|---|---|---|---|---|---|
| Sample size | ||||||
| Unweighted sample | 8618 | 100.0 | 5227 | 60.7 | ||
| Weighted visits | 22 498 475 | 100.0 | 13 584 867 | 60.4 | ||
| FDA‐approved non‐psychiatric indications | 3 165 849 | 14.1 | 2 182 922 | 69.0 | 16.1 | 1.46 |
| Total number of psychotropics prescribed | ||||||
| One | 4 445 464 | 21.3 | 2 891 614 | 65.0 | 21.3 | 1.22 |
| Two | 12 645 752 | 62.2 | 8 449 328 | 66.8 | 62.2 | 1.32 |
| Three | 1 889 445 | 6.3 | 859 357 | 45.5 | 6.3 | 0.55 |
| Four or more | 3 517 814 | 10.2 | 1 384 568 | 39.4 | 10.2 | 0.43 |
| Psychotropic class | ||||||
| Antipsychotic | 2 121 106 | 5.9 | 795 923 | 37.5 | 5.9 | 0.39 |
| Antidepressant | 14 226 981 | 56.5 | 7 671 438 | 53.9 | 56.5 | 0.77 |
| Anxiolytic | 10 802 382 | 51.3 | 6 968 650 | 64.5 | 51.3 | 1.19 |
| Overall | 27 150 469 | 15 436 011 | ||||
Turning to clinical characteristics (Table 2), FDA‐approved non‐psychiatric indications for psychotropic use (including insomnia), as expected, was associated with a risk ratio of 1.46 for receiving a psychotropic prescription without a psychiatric diagnosis. Among individual psychotropic drug classes, both antipsychotics and antidepressants had risk ratios of 0.39 and 0.77 of having psychotropic prescriptions without a psychiatric diagnosis, respectively. Anxiolytics had a risk ratio of 1.19 of having psychotropic prescriptions without a psychiatric diagnosis.
3.2. Trends of psychotropic prescription initiation without a psychiatric diagnosis
Figure 1 presents initiation of new psychotropic prescribing trends without a psychiatric diagnosis from 2006 to 2015. Overall, the rate increased from 59.1% in 2006‐2007 to 67.7% in 2008‐2009, and then decreased to 52.0% in 2014‐2015. When stratified by psychotropic drug class, anxiolytics had the highest prescribing rate over time, which increased from 65.9% in 2006‐2007 to 69.6% in 2008‐2009, and then decreased to 55.5% in 2014‐2015. Antipsychotics had the lowest rate of being prescribed without a psychiatric diagnosis over time.
Figure 1.
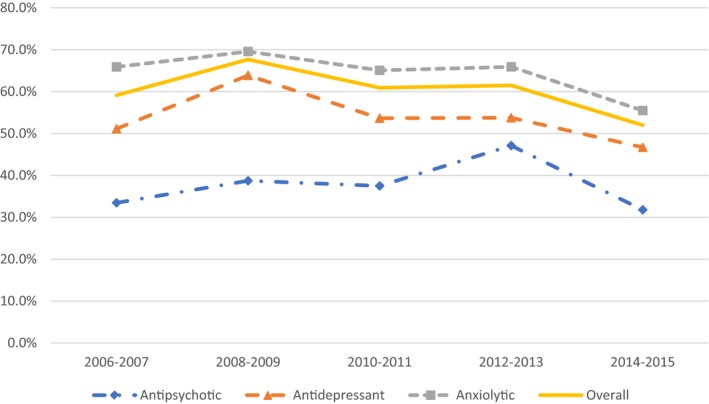
Initiation of psychotropic prescription without a psychiatric diagnosis among US adults aged 18 or older, 2006‐2015 NAMCS [Color figure can be viewed at wileyonlinelibrary.com]
Note: Overall psychotropic prescriptions increased from 59.1% in 2006‐2007 to 67.7% in 2008‐2009 and then decreased to 52.0% in 2014‐2015 (P = 0.041). Individual psychotropic class did not show significant time trends from 2006 to 2015.
3.3. Multivariable logistic regression analysis
Table 3 presents the results of multivariable‐adjusted logistic regression analysis, which estimated the odds of receiving a new psychotropic medication without a concurrent psychiatric diagnosis, independent of other factors. Overall, being older, for example, 45‐64 was associated with 1.57 times higher odds of not having a psychiatric diagnosis, when compared to a reference group of those aged 18‐44 (P < 0.001; 95% CI, 1.30‐1.90). Visits to psychiatrists were associated with very low odds of having no psychiatric diagnosis when compared to primary care visits (OR = 0.02; P < 0.001; 95% CI, 0.01‐0.04). Visits to non‐psychiatric specialties had 6.90 times greater odds of not having a psychiatric diagnosis when compared to primary care visits (P < 0.001; 95% CI, 5.38‐8.86). Having three or more concomitant medications prescribed was also associated with higher odds of lacking a psychiatric diagnosis (P < 0.001).
Table 3.
Adjusted odds ratios (AOR) of no psychiatric diagnosis among adults ages 18 or older with initiation of psychotropic prescription in office‐based outpatient settings by psychotropic class, 2006‐2015 NAMCS
| (Reference group in parentheses) | Overall | Antipsychotic | Antidepressant | Anxiolytic | ||||
|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| Age (18‐44) | ||||||||
| 45‐64 | 1.57*** | 1.30‐1.90 | 1.39 | 0.73‐2.67 | 1.52*** | 1.20‐1.93 | 1.32 | 0.99‐1.74 |
| 65+ | 1.68*** | 1.30‐2.18 | 2.26 | 0.78‐6.53 | 1.60* | 1.03‐2.47 | 1.42 | 0.96‐2.11 |
| Physician specialty (primary care) | ||||||||
| Psychiatry | 0.02*** | 0.01‐0.04 | 0.01*** | 0.00‐0.06 | 0.03*** | 0.01‐0.07 | 0.01*** | 0.00‐0.04 |
| Othera | 6.90*** | 5.38‐8.86 | 3.23** | 1.61‐6.47 | 6.47*** | 5.03‐8.31 | 7.38*** | 5.08‐10.71 |
| Number of medications (<3) | ||||||||
| 3‐5 | 2.20*** | 1.79‐2.71 | 1.81 | 0.85‐3.84 | 2.92*** | 2.33‐3.67 | 2.01*** | 1.43‐2.83 |
| 6+ | 3.38*** | 2.44‐4.69 | 4.41*** | 2.08‐9.37 | 5.84*** | 3.82‐8.92 | 3.99*** | 2.41‐6.60 |
| FDA‐approved non‐psychiatric indications (no) | ||||||||
| Yes | 1.38** | 1.11‐1.72 | 0.52 | 0.20‐1.37 | 1.47** | 1.14‐1.91 | 1.31 | 0.94‐1.81 |
| Psychotropic use | ||||||||
| Antipsychotic (no) | 1.00 | Reference | — | — | 0.59 | 0.24‐1.48 | 0.67 | 0.18‐2.40 |
| Antidepressant (no) | 1.22 | 0.77‐1.88 | 0.48* | 0.25‐0.95 | — | — | 0.32*** | 0.22‐0.48 |
| Anxiolytic (no) | 1.46 | 0.93‐2.29 | 0.68 | 0.32‐1.45 | 0.48*** | 0.33‐0.71 | — | — |
| Sample size | ||||||||
| Unweighted sample | 9129 | 899 | 5464 | 4043 | ||||
| Weighted visits | 23 964 669 | 2 121 106 | 14 226 981 | 10 802 382 | ||||
aGeneral surgery, obstetrics/gynecology, orthopedic surgery, cardiovascular diseases, dermatology, urology, neurology, ophthalmology, otolaryngology, and others.
***<0.001; **<0.01; *<0.05.
Having a non‐psychiatric indication for the FDA‐approved use of psychotropic medications, which included insomnia, was associated with 1.38 times higher odds of not having a psychiatric diagnosis (P < 0.001; 95% CI, 1.11‐1.72). Among psychotropic drug classes, antidepressants and anxiolytics were associated with 1.22 and 1.46 times higher odds of not having a psychiatric diagnosis, respectively, when compared to antipsychotic prescriptions. Reported odds ratios, however, were not statistically significant.
When stratified by individual psychotropic class, similar associations were found in terms of age, physician specialty, and the number of medications concomitantly prescribed. The antidepressant class was distinctive; having FDA‐approved non‐psychiatric indications was associated with 1.47 times greater odds of not having a psychiatric diagnosis (P < 0.01; 95% CI, 1.14‐1.91). In each psychotropic class, being prescribed other psychotropic medications was associated with lower odds of not having psychiatric diagnosis. For example, having an anxiolytic prescribed was associated with 0.52 times lower odds of not having a psychiatric diagnosis in the antidepressant class (P < 0.001; 95% CI, 0.33‐0.71).
4. DISCUSSION
This is the first pharmacoepidemiologic study investigating rates, correlates, and national trends in the initiation of new psychotropic prescriptions in the absence of a concurrent psychiatric diagnosis among adults in office‐based outpatient physician visits. From 2006 to 2015, new psychotropic medications were initiated at approximately 22.4 million visits, and 60.4% of these visits did not have any associated psychiatric diagnosis. The rate is comparable to previous studies, which reported rates ranging from 42% to 72.7%.3, 9, 15, 16 While these rates are not directly comparable due to differences in databases, inclusion criteria for psychotropics, or study settings, the rate remains consistently high, and raises a potential concern as to whether the use of psychotropic medications often fails to be grounded on clinical evidence or conventional practice.
When stratified by psychotropic drug class, anxiolytics had the highest rates of prescribing without a psychiatric diagnosis, a finding which is similar to that of a previous study.9 One possible explanation is that these medications may have been prescribed to patients on the basis of complaints or symptoms rather than clinical diagnoses. An alternative explanation is the potential influence of direct‐to‐consumer advertising. As previous studies suggest,27, 28, 29 psychotropics are heavily marketed through mass media, and about 42% of psychotropic prescriptions are reported to have been initiated through medication‐specific patient requests.29
In the multivariable‐adjusted logistic regression analysis, being older was associated with a higher likelihood of initiating psychotropic prescriptions without a psychiatric diagnosis, as found in a previous study.10 This is of special concern because older adults are especially vulnerable to side effects due in part to multimorbidity and to polypharmacy. In addition, non‐psychiatrist specialists had a sharply higher likelihood of initiating psychotropic prescriptions without a psychiatric diagnosis, and these patterns are also similar to those of previous studies.3, 10, 15, 16, 17 Non‐psychiatrists may approve psychotropic drug use for patients who do not necessarily have psychiatric disorders, but still have mild mood or anxiety symptoms which do not meet the criteria for a psychiatric disorders.3 Non‐psychiatrists may also incur a risk of liability claim due to such practices because “proper documentation of clinical interactions is critical in the defense of a malpractice claim.”30 (p. 117) Non‐psychiatrists should, perhaps, either be more cautious in using these medications or initiate psychotropic medication use with more thorough documentation.
Having three or more medications concomitantly prescribed was also associated with a higher likelihood of initiating psychotropic prescriptions without a psychiatric diagnosis. While some combinations of medications may be supported by clinical trials, many of them are of unproven efficacy or increased risk of side effects due to drug‐drug interactions.1 Finally, when compared to antipsychotic medications, other psychotropic medications classes presented higher likelihoods of being initiated without a psychiatric diagnosis, although they were not statistically significant. Since antipsychotic drugs have had boxed warnings from the FDA since the mid‐2000s13, 14 and are most often prescribed by psychiatrists, it is not surprising that they were least likely to be prescribed without a diagnosis. Furthermore, as shown in the multivariable analyses, drugs with FDA‐approved non‐psychiatric indications (eg, neuropathic pain) were associated with a higher likelihood of initiating new antidepressants or anxiolytics without a psychiatric diagnosis. This reflects the fact that both antidepressant and anxiolytic classes are prescribed for both approved uses, as in insomnia, but are often used for off‐label reasons such as various forms of non‐specific distress, for which their use may not be justified.
This study has several notable clinical and policy implications. First, non‐psychiatrists may need additional training in psychotropic prescribing. It is also possible that stigma associated with mental illness leads to incomplete documentation of psychiatric diagnoses. However, to prevent potentially inappropriate psychotropic use and medical malpractice, prescribing practices among non‐psychiatrists should align more consistently with clinical evidence and approved indications. Second, as part of the quality assurance and performance improvement, insurers may need to re‐structure incentives in their drug formulary policies. For instance, tiers of cost‐sharing for psychotropics could be categorized by psychiatric and other related clinical diagnoses rather than by drug alone. Such drug formularies could lead to lower cost‐sharing for patients with psychiatric diagnoses, as contrasted to use when there is no indicated diagnosis.3 Alternatively, quality of care performance models (eg, pay for performance31, 32) could incorporate approved or more orthodox prescribing practices at the level of office‐based outpatient care. Such quality monitoring programs may both educate and motivate physicians to initiate psychotropic prescriptions more carefully.
Several methodological limitations deserve comment. First, NAMCS did not capture visits to hospital‐affiliated clinics or emergency departments, which account for approximately 8.5% of all outpatient visits,33 and does not include prescription orders made by phone. Second, although NAMCS collected prescription and patient information from both physician surveys and chart reviews, the data may still reflect some degree of incomplete documentation. In particular, NAMCS only collected up to three diagnoses, and therefore, all psychiatric diagnoses may not have been fully documented. For instance, there are medically complicated patients in the survey, as implied by a measure indicating that they are being prescribed five or more medications concomitantly. In such cases, psychiatric diagnoses may not be documented in NAMCS because there were three or more medical diagnoses that we deemed to be of greater importance. Third, the NAMCS does not collect dosing information, which further limits our ability to investigate appropriate or potentially inappropriate psychotropic use. Finally, we used the loose criterion of having any psychiatric diagnosis, which would not have identified as problematic any prescriptions that were written for inappropriate or unjustified psychiatric diagnoses.
Despite the limitations, this study addressed several methodological limitations of previous studies and highlights the frequent initiation of new psychotropic medication use in the absence of any concurrent psychiatric diagnosis, even after adjusting for other approved uses. In particular, these data suggest that prescribing practices by non‐psychiatrists should be better aligned with clinical evidence and standards of practice.
CONFLICT OF INTEREST
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and none were reported. All research procedures performed in this study are in accordance with the ethical standards of the Institutional Review Board at Yale University School of Medicine (#2000021850).
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: Rhee received funding support from the National Institutes of Health (NIH) (#T32AG019134). The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript, and decision to submit the manuscript for publication.
Disclaimers: Publicly available data were obtained from the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention (CDC). Analyses, interpretation, and conclusions are solely those of the author and do not necessarily reflect the views of the Division of Health Interview Statistics or NCHS of the CDC.
Rhee TG, Rosenheck RA. Initiation of new psychotropic prescriptions without a psychiatric diagnosis among US adults: Rates, correlates, and national trends from 2006 to 2015. Health Serv Res. 2019;54:139–148. 10.1111/1475-6773.13072
REFERENCES
- 1. Mojtabai R, Olfson M. National trends in psychotropic medication polypharmacy in office‐based psychiatry. Arch Gen Psychiatry. 2010;67(1):26‐36. [DOI] [PubMed] [Google Scholar]
- 2. Rhee TG, Schommer JC, Capistrant BD, Hadsall RL, Uden DL. Potentially inappropriate antidepressant prescriptions among older adults in office‐based outpatient settings: national trends from 2002 to 2012. Adm Policy Ment Health. 2018;45:224‐235. [DOI] [PubMed] [Google Scholar]
- 3. Mojtabai R, Olfson M. Proportion of antidepressants prescribed without a psychiatric diagnosis is growing. Health Aff. 2011;30(8):1434‐1442. [DOI] [PubMed] [Google Scholar]
- 4. Moore TJ, Mattison DR. Adult utilization of psychiatric drugs and differences by sex, age, and race. JAMA Intern Med. 2017;177(2):274‐275. [DOI] [PubMed] [Google Scholar]
- 5. Mark TL, Levit KR, Buck JA. Datapoints: psychotropic drug prescriptions by medical specialty. Psychiatr Serv. 2009;60(9):1167. [DOI] [PubMed] [Google Scholar]
- 6. Mojtabai R, Olfson M. National patterns in antidepressant treatment by psychiatrists and general medical providers: results from the national comorbidity survey replication. J Clin Psychiatry. 2008;69(7):1064‐1074. [DOI] [PubMed] [Google Scholar]
- 7. CenterWatch . FDA approved drugs for psychiatry/psychology. 2017. https://www.centerwatch.com/drug-information/fda-approved-drugs/therapeutic-area/17/psychiatry-psychology. Accessed November 7, 2017.
- 8. Hodgkin D, Thomas CP, O'Brien PL, et al. Projected spending on psychotropic medications 2013‐2020. Adm Policy Ment Health. 2016;43(4):497‐505. [DOI] [PubMed] [Google Scholar]
- 9. Wiechers IR, Leslie DL, Rosenheck RA. Prescribing of psychotropic medications to patients without a psychiatric diagnosis. Psychiatr Serv. 2013;64(12):1243‐1248. [DOI] [PubMed] [Google Scholar]
- 10. Wiechers IR, Kirwin PD, Rosenheck RA. Increased risk among older veterans of prescribing psychotropic medication in the absence of psychiatric diagnoses. Am J Geriatr Psychiatry. 2014;22(6):531‐539. [DOI] [PubMed] [Google Scholar]
- 11. Tune L, Carr S, Hoag E, Cooper T. Anticholinergic effects of drugs commonly prescribed for the elderly: potential means for assessing risk of delirium. Am J Psychiatry. 1992;149(10):1393‐1394. [DOI] [PubMed] [Google Scholar]
- 12. Tune LE. Anticholinergic effects of medication in elderly patients. J Clin Psychiatry. 2001;62(Suppl 21):11‐14. [PubMed] [Google Scholar]
- 13. U.S. Food and Drug Administration . Information on conventional antipsychotics. 2008. https://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm107211.htm. Accessed October 1, 2017.
- 14. U.S. Food and Drug Administration . Information for healthcare professionals: conventional antipsychotics. 2008. https://www.fda.gov/Drugs/DrugSafety/ucm124830.htm. Accessed October 9, 2017.
- 15. Larson MJ, Miller K, Fleming KJ. Treatment with antidepressant medications in private health plans. Adm Policy Ment Health. 2007;34(2):116‐126. [DOI] [PubMed] [Google Scholar]
- 16. Milea D, Verpillat P, Guelfucci F, Toumi M, Lamure M. Prescription patterns of antidepressants: findings from a US claims database. Curr Med Res Opin. 2010;26(6):1343‐1353. [DOI] [PubMed] [Google Scholar]
- 17. Pagura J, Katz LY, Mojtabai R, Druss BG, Cox B, Sareen J. Antidepressant use in the absence of common mental disorders in the general population. J Clin Psychiatry. 2011;72(4):494‐501. [DOI] [PubMed] [Google Scholar]
- 18. National Center for Health Statistics . Ambulatory health care data. 2017. https://www.cdc.gov/nchs/ahcd/index.htm.
- 19. National Center for Health Statistics . Ambulatory health care data: questionnaires, datasets, and related documentation. 2017. https://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm.
- 20. Rhee TG, Mohamed S, Rosenheck RA. Antipsychotic prescriptions among adults With major depressive disorder in office‐based outpatient settings: national trends from 2006 to 2015. J Clin Psychiatry. 2018;79(2):17m11970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rhee TG, Choi YC, Ouellet GM, Ross JS. National prescribing trends for high‐risk anticholinergic medications in older adults. J Am Geriatr Soc. 2018;66:1382‐1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maust DT, Gerlach LB, Gibson A, Kales HC, Blow FC, Olfson M. Trends in central nervous system‐active polypharmacy among older adults seen in outpatient care in the United States. JAMA Intern Med. 2017;177(4):583‐585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. American Society of Health‐System Pharmacists . American Hospital Formulary Service (AHFS) Drug Information. Bethesda, MD: American Society of Health‐System Pharmacists; 2017. [Google Scholar]
- 24. Bhalla IP, Stefanovics EA, Rosenheck RA. Clinical epidemiology of single versus multiple substance use disorders: polysubstance use disorder. Med Care. 2017;55(Suppl 9 Suppl 2):S24‐S32. [DOI] [PubMed] [Google Scholar]
- 25. Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract. 2009;40(5):532‐538. [Google Scholar]
- 26. Stata Statistical Software . Release 15 [Computer Program]. College Station, TX: StataCorp LP; 2017. [Google Scholar]
- 27. Gilbody S, Wilson P, Watt I. Direct‐to‐consumer advertising of psychotropics. An emerging and evolving form of pharmaceutical company influence. Br J Psychiatry. 2004;185:1‐2. [DOI] [PubMed] [Google Scholar]
- 28. Mintzes B, Barer ML, Kravitz RL, et al. How does direct‐to‐consumer advertising (DTCA) affect prescribing? A survey in primary care environments with and without legal DTCA. CMAJ. 2003;169(5):405‐412. [PMC free article] [PubMed] [Google Scholar]
- 29. Sleath B, Svarstad B, Roter D. Physician vs patient initiation of psychotropic prescribing in primary care settings: a content analysis of audiotapes. Soc Sci Med. 1997;44(4):541‐548. [DOI] [PubMed] [Google Scholar]
- 30. Edersheim JG, Stern TA. Liability associated with prescribing medications. Prim Care Companion J Clin Psychiatry. 2009;11(3):115‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Petersen LA, Woodard LD, Urech T, Daw C, Sookanan S. Does pay‐for‐performance improve the quality of health care? Ann Intern Med. 2006;145(4):265‐272. [DOI] [PubMed] [Google Scholar]
- 32. Van Herck P, De Smedt D, Annemans L, Remmen R, Rosenthal MB, Sermeus W. Systematic review: effects, design choices, and context of pay‐for‐performance in health care. BMC Health Serv Res. 2010;10:247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Saluja S, Woolhandler S, Himmelstein DU, Bor D, McCormick D. Unsafe drugs were prescribed more than one hundred million times in the United States before being recalled. Int J Health Serv. 2016;46(3):523‐530. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


