Abstract
Background and aims This study aimed to evaluate the performance of Macroscopic On-site Evaluation (MOSE) using a novel endoscopic ultrasound (EUS) fine needle biopsy (FNB) needle (22-G Franseen-tip needle, Acquire, Boston Scientific Incorporated, Boston, Massachusetts, United States), and without using Rapid On-Site Evaluation (ROSE).
Method Between May 2016 and August 2016, all consecutive patients referred to our center for EUS tissue acquisition (TA) for solid lesions underwent EUS-FNB with the 22-G Franseen-tip needle unless contra-indicated. The operator performed MOSE. If no macroscopic core was visualized, a second pass was performed. The final diagnosis was defined as unequivocal histology from EUS-TA with compatible 18 months follow-up, surgical resection, or both. We retrospectively analyzed the performance of MOSE.
Results A total of 46 consecutive patients was included, and 54 solid lesions were biopsied. The endosonographer visualized core tissue in 93 % (50/54) of targets with a single pass, of which the pathologist confirmed histologic core fragments in 94 % (47/50). Four lesions required two passes, and the overall correlation between MOSE and histologic core fragments was 94 % (48/51). Diagnostic adequacy was 98 % (53/54) with one biliary target biopsied without significant material. The overall diagnostic accuracy was 94 %. Sensitivity, specificity, positive predictive value, and negative predictive value for malignancy were 92 %, 100 %, 100 %, and 81 %, respectively. No adverse events were reported.
Conclusion Our study demonstrated that MOSE using the 22-G Franseen-tip needle could limit needle passes by accurately estimating histologic core fragments. It also demonstrated that high diagnostic adequacy and accuracy of > 90 % could be achieved without ROSE.
Introduction
Endoscopic ultrasound guided tissue acquisition (EUS-TA) has become the procedure of choice in obtaining diagnostic samples for lesions within the gastrointestinal tract and adjacent organs 1 2 3 . Its purpose is to acquire a diagnostic sample with the least number of passes to increase efficiency and decrease the cost and complications of the procedure. The diagnostic accuracy of EUS-TA is highly variable ranging from 50 % to 98 % 1 2 3 4 5 . It relies on multiple factors including operator expertise, location, and characteristic of the target lesion, needle choice, and the availability of Rapid On-Site Cytologic Evaluation (ROSE) 6 .
Although EUS fine needle aspiration (EUS-FNA) procures cytology, it presents several deficiencies. Firstly, it does not provide core tissue with the preserved architecture necessary to assess diseases such as lymphoma, gastrointestinal stromal tumors (GIST), and autoimmune pancreatitis 1 7 . Tissue quality is also insufficient for molecular profiling of pancreatic adenocarcinoma, which is performed on both the tumor and stromal cells 8 9 . Finally, EUS-FNA requires ROSE to improve diagnostic adequacy with fewer needle passes 6 10 ; however, this is not readily available outside tertiary centers in the United States. Furthermore, it increases the cost and duration of the procedure.
Novel EUS fine needle biopsy (EUS-FNB) needles developed to obtain a core biopsy specimen have been designed to overcome these limitations 11 12 13 14 15 . Studies comparing EUS-FNA to EUS-FNB needles have reached different conclusions 16 17 18 19 . Recent data including new generation EUS-FNB needles suggest that, in the absence of ROSE, EUS-FNB provides better diagnostic adequacy with fewer passes than EUS-FNA 18 . A few studies also indicate that Macroscopic On-Site Evaluation (MOSE) by the endosonographer could be a comparable alternative to ROSE when performed using EUS core tissue biopsy needles 20 21 .
In April 2016, EUS-FNB with the novel 22-G Acquire needle (Boston Scientific Incorporated, Boston, Massachusetts, United States), also called the 22-G Franseen-tip needle, was tested on solid lesions in our center. A visible tan-pink core tissue specimen was readily seen using this needle, and appeared to correlate with histologic core fragments. We speculated that MOSE could be reliable to determine tissue adequacy.
This retrospective study aimed to assess the performance of MOSE using the EUS-FNB 22-G Franseen-tip needle.
Patients and method
Study population
Between May 2016 and August 2016, all consecutive patients referred to our center for EUS-TA for solid lesions underwent EUS-FNB with the 22-G Franseen-tip needle and were included prospectively in a database. Patients with interposing vessels or ducts were excluded. Patient inclusion ended in August 2016 to allow presentation at the French digestive meeting (abstracts in September 2016, meeting in March 2017). All patients were followed up to surgery, death or 18 months follow-up. Collected data were patient demographics, target lesion type and location, procedure specifics, histology, diagnostic adequacy, and adverse events. In February 2018, we retrospectively reviewed all included cases.
We obtained written informed consent from all patients. The Institutional Ethics Committee of Ramsay Générale de Santé approved the study protocol (IRB: COS-RGDS-2017-11-02). All procedures performed in human participants were per the moral, ethical, and scientific principles governing clinical research as set out in the Declaration of Helsinki (1989).
Definition of end points
The primary end point was histologic core tissue of the targeted organ correlated with macroscopically visualized core tissue. Architecturally intact fragments with various non-dissociated cellular components defined the histologic core tissue.
The secondary end points were:
Technical success defined as successful sampling of the lesion.
Diagnostic adequacy defined as the presence of targeted tissue confirmed on histopathology.
Overall diagnostic accuracy defined as the correct identification of the final diagnosis (benign or malignant) by EUS-FNB.
Sensitivity, specificity, PPV, and NPV calculated using malignancy as a positive sample, and a benign lesion as a negative sample.
Reference standard diagnosis
The final diagnosis was defined as unequivocal histology from EUS-FNB with compatible 18 months follow-up, surgical resection, or both.
Procedure
In total, five experienced endosonographers, each of whom had performed more than 1000 EUS-TA, performed all procedures. EUS-FNB was performed under sedation with a curvilinear array echoendoscope (GF-UCT 180, Olympus) and the 22-G Acquire needle. The tip of the 22-G Acquire needle has a Franseen three-plane symmetric design in which the inclination and included angles are a constant thus enabling an optimal geometry for both tissue penetration and cutting 22 . Furthermore, the long insertion length and area at the crown tip should augment acquired tissue. The needle has an outer and inner diameter of 0.72 mm and 0.56 mm, respectively, and an adjustable working length of 137.5 – 141.5 cm.
All procedures were performed with the stylet in place. After advancing the needle beyond the scope channel and sheath, the stylet was retracted a few millimeters before puncturing the target lesion. The stylet was maximally advanced inside the needle to remove potential tissue plugs. The stylet was subsequently removed from the needle. The needle was then used to puncture the target lesion in a standardized fashion using a “fanning” technique and with a total of 10 strokes. No suction was applied during the first needle pass. The needle content was flushed in a formalin flask. If the endosonographer identified a tan-pink core tissue by gross visual inspection, no further passes were performed; however, if the specimen was deemed only bloody or without any core tissue, a second pass was completed, either with no suction and five strokes if the initial sample was bloody, or with 10 mL suction if no material was present.
Recording of adverse events was as per standard protocol in the center. Immediate adverse events were noted at the center during, and up to 4 hours following the procedure. The patient and the referring physicians notified any delayed adverse events within 72 hours.
Specimen preparation and evaluation
Core biopsy samples were collected in 10 % buffered formalin solution for cellblock preparation. Each block underwent hematoxylin-phloxine-saffron staining as per standard pathology protocol. A single designated pathologist (AIL) processed and examined all specimens. Tissue fragments were counted manually. Length of tissue was estimated based on × 200 magnification field corresponding to 1.1 mm. The width of tissue was determined based on the × 400 magnification field corresponding to 0.55 mm. In pancreatic adenocarcinoma, the pathologist estimated the ratio of tumor cellularity to total cellularity using an area of ≥ 2 mm 2 , in a zone deemed of highest cellularity. The presence of stroma was noted, and the ratio of stroma to overall tumor cellularity was estimated.
Unequivocal histopathologic diagnosis was given when possible, otherwise it was designated suspicious or inconclusive.
ROSE was not used in any of the cases.
Statistical analysis
This was a retrospective study using descriptive statistics. Sensitivity, specificity as well as positive predictive value (PPV), negative predictive value (NPV), and accuracy were calculated using the final diagnosis. Continuous data were presented with median and IQR, whereas quantitative data were presented as mean and standard deviation.
Results
Patient and lesion characteristics
In total, 46 consecutive patients were included, and 54 solid target lesions were biopsied ( Table 1 ). One excluded patient had an interposing vessel over the target lesion. The median patient age was 70 years old (IQR 61 – 78), and 34/46 (74 %) were male patients.
Table 1. Outcome by lesion type.
| Lesion type | n | Mean lesion size and range, mm | Fragments/length, mm | Diagnostic adequacy, % | Accuracy, % | Final diagnosis |
| Pancreas | 31 | 27 ± 12 (6 – 60) | 2 – 15/0.5 – 10 | 31/31 (100) | 30/31 (97) | 20 adenocarcinoma (1 FN) |
|
18 | 10 – 35 | 5 NET | |||
|
2 | 6 – 36 | 2 AIP | |||
|
7 | 10 – 60 | 1 lymphoma | |||
|
4 | 20 – 35 | 3 chronic pancreatitis | |||
| SMT | 4 | 34 ± 24 (21 – 70) | 2 – 10/0.5 – 4 | 4/4 (100) | 4/4 (100) | |
|
2 | 21 | 10/1 – 3 | 1 GIST | ||
| 23 | 3/1 – 4 | 1 schwannoma | ||||
|
1 | 20 | 8/1 – 4 | NET | ||
|
1 | 70 | 2/0.5 | Solitary fibrous tumor | ||
| Gastric wall thickening | 2 | 4/1 – 8 | 2/2 (100 %) | 2/2 (100 %) | 2 gastric linitis | |
| Lymph node | 9 | 31 ± 12 (15 – 50) | 2 – 5/0.5 – 5 | 9/9 (100) | 7/7 (100) | 3 metastases (2 adenocarcinomas, 1 NET) |
| 2 NE | 2 sarcoidosis | |||||
| 1 tuberculosis | ||||||
| 1 lymphoma | ||||||
| Other | 8 | 11 ± 6 (5 – 20) | 6 – 12/0.1 – 7 | 7/8 (87.5) | 5/7 (71) | |
|
2 | 13 ± 11 (5 – 20) | 10/1 – 2 | 1 NC | Cholangiocarcinoma | |
| AIC | ||||||
|
5 | 7 ± 2 (5 – 10) | 6 – 12/0.1 – 5 | 1 NE | 4 liver metastases (1 FN) | |
|
1 | 18 | 10/1 – 7 | 1 pleural hamartoma |
SMT, sub-mucosal tumor; NET, neuroendocrine tumor; GIST, gastrointestinal stromal tumor; AIP, autoimmune pancreatitis; AIC, autoimmune cholangitis; NE, non-evaluable; FN, false negative; NC, non-contributive.
Target lesions were pancreas (n = 31), biliary tract (n = 2), liver (n = 5), lymph node (n = 9), sub-mucosal (n = 4), wall thickening (n = 2), and pleura (n = 1). Mean lesion size was 24.5 ± 13.8 mm.
Technical aspects
Technical success was 100 % (54/54). A median of 1 needle pass per target was performed. A single needle pass procured a tan-pink core ( Fig. 1 ) upon gross inspection in 50/54 targets (93 %). A second needle pass was required in 4/54 cases: 2/54 due to insufficient initial material and 2/54 due to initial hemorrhagic “core” ( Fig. 2 ). Only 1/4 of the second passes procured a macroscopic core upon MOSE. Overall visible core with one or two passes was 51/54 (94 %). There were no adverse events reported.
Fig. 1.
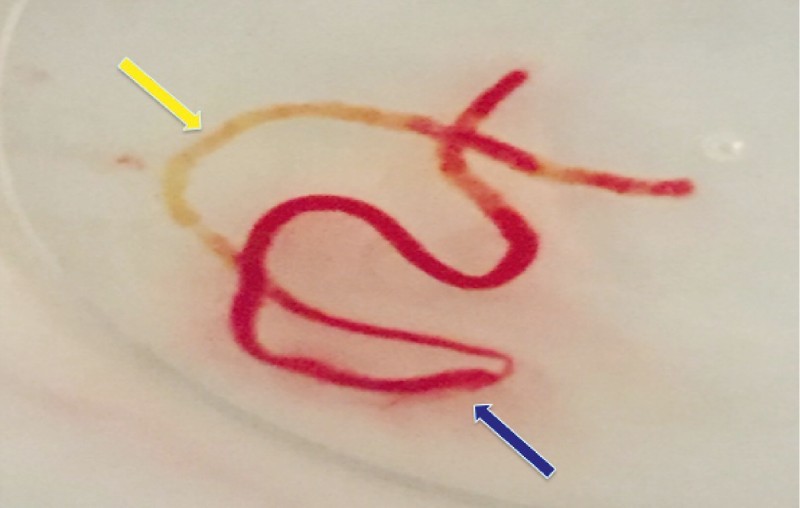
Macroscopic onsite evaluation (MOSE): single needle pass. Yellow arrow = tan-pink core; blue arrow = hemorrhagic core.
Fig. 2.
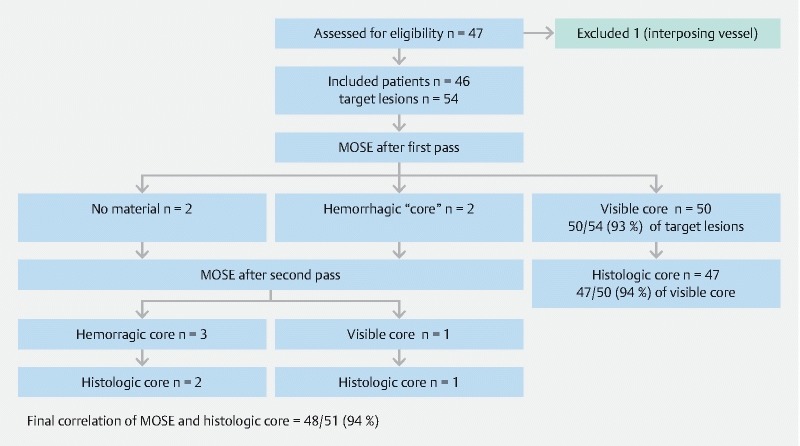
Study flow chart.
Histologic assessment
Of the biopsied targets with a visible core on MOSE after a single pass by the endosonographer, the pathologist confirmed histologic core fragments in 47/50 cases (94 %). In one target, the histopathologic examination showed no contributive tissue, and in two targets, it showed only dissociated cells in contaminated tissue. For the latter two targets, cytological examination confirmed the diagnosis of a pancreatic adenocarcinoma and a pancreatic neuroendocrine tumor.
For those targets requiring two passes, core histologic fragments were present in 3/4 targets. Only one target, an adenopathy that required two passes (both hemorrhagic) showed neither a visible macroscopic core nor histologic core tissue. The pathologist confirmed histologic core fragments in visible core on MOSE with one or two passes, in 48/51 (94 %) targets ( Fig. 2 ).
Overall core histology obtained in this study for all targets was 50/54 (93 %). Overall diagnostic adequacy was 98 % (53/54) with one biliary target biopsied without significant material.
There was a median of 6 (IQR 4 – 10) tissue fragments per target. Size of fragments ranged from 0.1 mm to 10 mm in length. The width of tissue fragments was consistent in all evaluable specimens measuring 0.4 – 0.5 mm.
For pancreatic adenocarcinomas, tumor cellularity was present in 95 % and represented at least 30 % of cells in 25 % of cases. Stroma was noted in 71 % and represented at least 50 % of the tumor volume in 50 % of cases ( Fig. 3a,b ).
Fig. 3 a.
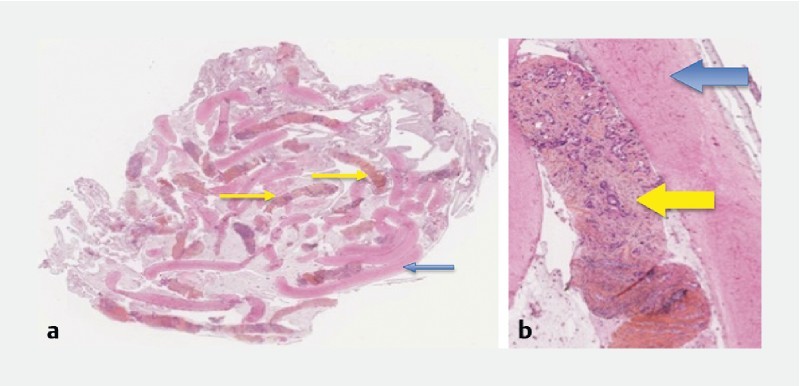
Pancreatic adenocarcinoma. Cellblock section with hematin – eosin staining. Yellow arrows = pancreatic tumor core (orange): 0.4 mm wide, 3 – 5 cm long; blue arrow = blood clot (pink). b Pancreatic adenocarcinoma. Cellblock section with hematin – eosin staining. Yellow arrow = pancreatic tumor core (orange): carcinomatous glands in tumoral stoma; blue arrow = blood clot (pink).
Final diagnosis
In three patients with pancreatic adenocarcinoma, the evaluation of the second target (two lymph nodes, one liver lesion) was not possible. In these cases, histology showed normal or benign tissue, but final diagnosis could not be established, as the patients did not have surgery, or significant evolution of the targets before their death. For the 51 remaining targets, final diagnosis was based on surgery (n = 11), and results of EUS-FNB with 18 months follow-up (n = 40).
In total, 22/24 patients had died of related underlying disease at 18 months follow-up. Their diagnoses were 16 pancreatic adenocarcinomas, 1 poorly differentiated pancreatic neuroendocrine tumor, 3 metastatic adenocarcinomas, 1 aggressive lymphoma, and 1 cholangiocarcinoma. Two patients died of unrelated diseases: 1 with a benign lymph node, and 1 with a GIST.
The diagnosis correlated with EUS-FNB results in 48 targets including 35 malignant and 13 benign lesions. In total, 3 EUS-FNB with benign histopathology were false negatives after follow-up: 1 liver metastasis, 1 cholangiocarcinoma, and 1 pancreatic adenocarcinoma ( Table 1 ). Overall diagnostic accuracy was 94 % (48/51). Sensitivity, specificity, PPV, and NPV for the diagnosis of malignancy were 92 %, 100 %, 100 %, and 81 %, respectively.
Discussion
In the era of EUS core biopsy needles, the role of ROSE remains unclear. A recent review showed that EUS-FNB without ROSE offered similar diagnostic adequacy and accuracy to EUS-FNB with ROSE for solid pancreatic lesions 23 . In the ROSE group, sensitivity, specificity, overall diagnostic adequacy, and overall diagnostic accuracy were 96 %, 100 %, 86.5 %, and 85.5 %, respectively, while in the no-ROSE group, they were 86.6 %, 100 %, 89.5 %, and 86.1 %, respectively. In another randomized controlled trial comparing the 22-G Franseen-tip and 22-G Fork-tip needles (SharkCore, Medtronic), diagnostic cellblock in > 90 % of patients suggested that ROSE was not necessary 24 .
A potential practical alternative to ROSE is MOSE; however, evidence for its usefulness in EUS-TA remains limited and conflicting 2 21 . Our results showed that MOSE using the 22-G Franseen-tip needle was able to procure a visible core tissue in 93 % of target lesions with a single pass, which correlates with histologic core fragments in 94 % of these lesions. Recent needle studies and guidelines suggest that second-generation EUS-FNB needles can reduce the number of needle passes to a minimum of two passes 2 12 14 . Our results indicate that MOSE using the 22-G Franseen-tip needle could have a further impact on reducing the number of passes required to reach adequate diagnostic performance as it may be a practical and objective measure of specimen adequacy.
Our results evaluating this EUS-FNB needle are concordant with other recently published series 11 12 13 14 15 . In the series by Bang et al. 12 , two passes were performed for all lesions, and ROSE was performed in all cases with overall diagnostic adequacy of 96.6 %. Our series produced similar results (diagnostic adequacy of 98 %, accuracy of 94 %) with MOSE and a single needle pass.
Until recently, histologic core tissue has been difficult to obtain from EUS-TA. First-generation core biopsy needles such as the reverse bevel biopsy needle ProCore 22-G (Cook Medical) were not shown to differ from standard FNA needles in histology procurement, sample adequacy, or diagnostic accuracy 17 . The number of comparative studies of EUS-FNA with second-generation EUS-FNB needles is still limited but show promising results in favor of EUS-FNB 11 15 18 19 . In a case-control study by Kandel et al. 15 , diagnostic adequacy was significantly higher using the 22-G Fork-tip needle compared to the standard FNA needle (95 % vs. 59 %, P = 0.01). Furthermore, a sample was achieved with fewer needle passes (average of 2 vs. 4 passes, P = 0.001). In a randomized trial by Bang et al. 11 , diagnostic adequacy was significantly higher using the 22-G Franseen-tip needle compared to the 22-G standard bevel FNA needle in pancreatic masses (97.8 % vs. 82 %, P = 0.03). Finally, Li et al. 19 recently published a meta-analysis of randomized controlled trials showing that EUS-FNB was superior to EUS-FNA with regard to diagnostic adequacy and accuracy in the sampling of pancreatic masses. Interestingly, in our study, the high diagnostic accuracy was maintained for sub-epithelial lesions and thickened gastrointestinal wall (6/6, 100 %), which notoriously pose a diagnostic challenge in EUS-TA 1 . This finding could be due to the high percentage of tumor cells in tissue procured by EUS-FNB and is consistent with results in previous core needle publications 12 14 .
An even more salient point is that EUS-FNB significantly improves the quality of the histologic material. In our study, the method of histologic processing and analysis was standardized and centrally reviewed by a single pathologist to optimize the congruency of interpretation. We were able to determine the quality of histologic sampling in several ways. Firstly, the pathologist saw core fragments in 94 % of target lesions. Secondly, all fragments consistently presented a width of 0.4 – 0.5 mm corresponding to the adjusted inner width of the 22-G Franseen-tip needle after 20 – 30 % shrinkage from the fixation with formalin. Thirdly, tumor cellularity in pancreatic adenocarcinoma was present in 95 % and represented at least 30 % of cells in 25 % of cases. Although we did not electronically calculate the percentage of tumor cells in tissue, our results are consistent with the recent findings of Bang et al. (percentage of tumor in tissue, 73.9 % [IQR = 44 – 97.6]) 12 . Moreover, we observed stroma in 71 % of cases of pancreatic adenocarcinomas with at least 50 % of tumor tissue in 50 % of these cases. This is particularly important as pancreatic adenocarcinomas may be relatively hypocellular while both tumor cells and desmoplastic stroma are required for molecular profiling 8 9 . The latter is becoming increasingly important as it could facilitate evaluating patient prognosis and the tailoring of adjuvant chemotherapy 25 .
In our study, we experienced no adverse events although overall reported adverse event rate for EUS-TA is 2 % in the literature 26 . Our low adverse event rate could be due to operator expertise, the limited needle passes, and the excluding of patients with interposing large vessels between the needle and the target lesion.
Our study had some limitations including the small number of biopsied lesions per subtype, the single referral center population, and the inherent shortcomings of a retrospective design. We also did not study the use of molecular profiling. Larger prospective trials comparing EUS-FNB needles could be performed to confirm our findings.
In conclusion, our study demonstrated that MOSE using the 22-G Franseen-tip needle could limit needle passes by accurately estimating histologic core fragments. It also demonstrated that high diagnostic adequacy and accuracy of > 90 % could be achieved without ROSE.
Acknowledgments
The authors wish to thank Mrs Stéphanie Girodet (research nurse at Hôpital Privé Jean Mermoz) for her contribution to conducting this study.
Footnotes
Competing interests Dr Napoleon and Dr Fumex declare having received educational fees and research support from Boston.
References
- 1.Dumonceau J M, Deprez P H, Jenssen C et al. Indications, results and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline – updated January 2017. Endoscopy. 2017;49:695–714. doi: 10.1055/s-0043-109021. [DOI] [PubMed] [Google Scholar]
- 2.Polkowski M, Jenssen C, Kaye P et al. Technical aspects of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) technical guidelines – March 2017. Endoscopy. 2017;49:989–1006. doi: 10.1055/s-0043-119219. [DOI] [PubMed] [Google Scholar]
- 3.ASGE Standards of Practice Committee . Eloubeidi M A, Decker G A, Chandrasekhara V et al. The role of endoscopy in the evaluation and management of patients with solid pancreatic neoplasia. Gastrointest Endosc. 2016;83:17–28. doi: 10.1016/j.gie.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Hewitt M J, McPhail M J, Possamai L et al. EUS-guided FNA for diagnosis of solid pancreatic neoplasms: a meta-analysis. Gastrointest Endosc. 2012;275:319–331. doi: 10.1016/j.gie.2011.08.049. [DOI] [PubMed] [Google Scholar]
- 5.Puli S R, Bechtold M L, Buxbaum J L et al. How good is endoscopic ultrasound-guided fine-needle aspiration in diagnosing the correct etiology for a solid pancreatic mass? A meta-analysis and systematic review. Pancreas. 2013;42:20–26. doi: 10.1097/MPA.0b013e3182546e79. [DOI] [PubMed] [Google Scholar]
- 6.Holt B A, Varadarajulu S, Herbert-Magee S. High-quality endoscopic ultrasound-guided fine needle aspiration tissue acquisition. Adv Ther. 2014;31:696–707. doi: 10.1007/s12325-014-0129-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deshpande V, Mino-Kenudson M, Brugge W R et al. Endoscopic ultrasound guided fine needle aspiration biopsy of autoimmune pancreatitis: diagnostic criteria and pitfalls. Am J Surg Pathol. 2005;29:1464–1471. doi: 10.1097/01.pas.0000173656.49557.48. [DOI] [PubMed] [Google Scholar]
- 8.Brais R J, Davies S E, O’Donovan M et al. Direct histological processing of EUS biopsies enables rapid molecular biomarker analysis for interventional pancreatic cancer trials. Pancreatology. 2012;12:8–15. doi: 10.1016/j.pan.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 9.Moffitt R A, Marayati R, Flate E L et al. Virtual microdissection identifies distinct tumor and stroma specific subtypes of pancreatic ductal adenocarcinoma. Nat Genet. 2015;47:1168–1178. doi: 10.1038/ng.3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hébert-Magee S, Bae S, Varadarajulu S et al. The presence of a cytopathologist increases the diagnostic accuracy of endoscopic ultrasound-guided fine-needle aspiration cytology for pancreatic adenocarcinoma: a meta-analysis. Cytopathology. 2013;24:159–171. doi: 10.1111/cyt.12071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bang J Y, Herbert-Magee S, Navaneethan Uet al. EUS-guided fine needle biopsy of pancreatic masses can yield true histology: results of a randomized trial Gut 2017 10.1136/gutjnl-2017-315154[Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bang J Y, Hebert-Magee S, Hasan M K et al. EUS-guided biopsy using a Franseen needle design: An initial assessment. Dig Endosc. 2016;29:338–346. doi: 10.1111/den.12769. [DOI] [PubMed] [Google Scholar]
- 13.Di Mitri R, Rimbas M, Attili F et al. Performance of a new needle for endoscopic ultrasound-guided fine-needle biopsy in patients with pancreatic solid lesions: A retrospective multicenter study. Endosc Ultrasound. 2018;7:329–334. doi: 10.4103/eus.eus_33_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DiMaio C J, Kolb J M, Benias P C et al. Initial experience with a novel EUS-guided core biopsy needle (SharkCore): results of a large North American multicenter study. Endosc Int Open. 2016;9:E974–979. doi: 10.1055/s-0042-112581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kandel P, Tranesh G, Nassar A et al. EUS-guided fine needle biopsy sampling using a novel fork-tip needle: a case-control study. Gastrointest Endosc. 2016;84:1034–1039. doi: 10.1016/j.gie.2016.03.1405. [DOI] [PubMed] [Google Scholar]
- 16.Aadam A A, Wani S, Amick A et al. A randomized controlled cross-over trial and cost analysis comparing endoscopic ultrasound fine needle aspiration and fine needle biopsy. Endosc Int Open. 2016;4:E497–E505. doi: 10.1055/s-0042-106958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bang J W, Hawes E, Varadarajulu S. A meta-analysis comparing Pro-Core and standard fine-needle aspiration needles for endoscopic ultrasound-guided tissue acquisition. Endoscopy. 2016;48:339–349. doi: 10.1055/s-0034-1393354. [DOI] [PubMed] [Google Scholar]
- 18.Khan M A, Grimm I S, Ali B et al. A meta-analysis of endoscopic ultrasound-fine needle aspiration compared to endoscopic ultrasound-fine needle biopsy: diagnostic yield and the value of onsite cytopathological assessment. Endosc Int Open. 2017;5:E363–E375. doi: 10.1055/s-0043-101693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li H, Li W, Zhou Q Y et al. Fine needle biopsy is superior to fine needle aspiration in endoscopic ultrasound guided sampling of pancreatic masses. A meta-analysis of randomized controlled trials. Medicine (Baltimore) 2018;97:13 (e0207). doi: 10.1097/MD.0000000000010207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rodrigues-Pinto E, Jalaj S, Grimm I S et al. Impact of EUS-guided fine-needle biopsy sampling with a new core needle on the need for onsite cytopathologic assessment: a preliminary study. Gastrointest Endosc. 2016;84:1040–1046. doi: 10.1016/j.gie.2016.06.034. [DOI] [PubMed] [Google Scholar]
- 21.Iwashita T, Yasuda I, Mukai T et al. Macroscopic on-site quality evaluation of biopsy specimens to improve the diagnostic accuracy during EUS-guided FNA using a 19-gauge needle for solid lesions: a single-center prospective pilot study (MOSE study) Gastrointest Endosc. 2015;81:177–185. doi: 10.1016/j.gie.2014.08.040. [DOI] [PubMed] [Google Scholar]
- 22.Han P, Che D, Pallav K et al. Models of the cutting edge geometry of medical needles with applications to needle design. Int J Mech Sci. 2012;65:157–167. [Google Scholar]
- 23.Arena M, Eusebi L H, Pellicano R et al. Endoscopic ultrasound core needle for diagnosing of solid pancreatic lesions: is rapid on-site evaluation really necessary? Minerva Med. 2017;108:547–553. doi: 10.23736/S0026-4806.17.05327-7. [DOI] [PubMed] [Google Scholar]
- 24.Bang J Y, Hebert-Magee S, Navaneethan U et al. Randomized trial comparing the Franseen and Fork-tip needles for EUS-guided fine-needle biopsy sampling of solid pancreatic mass lesions. Gastrointest Endosc. 2018;87:1432–1438. doi: 10.1016/j.gie.2017.11.036. [DOI] [PubMed] [Google Scholar]
- 25.Chantrill L A, Nagrial A M, Watson C et al. Precision medicine for advanced pancreas cancer: the individualized molecular pancreatic cancer therapy (IMPaCT) trial. Clin Cancer Res. 2015;21:2029–2037. doi: 10.1158/1078-0432.CCR-15-0426. [DOI] [PubMed] [Google Scholar]
- 26.ASGE Standards of Practice Committee . Early D S, Acosta R D, Chandrasekhara V et al. Adverse events associated with EUS and EUS with FNA. Gastrointest Endosc. 2013;77:839–843. doi: 10.1016/j.gie.2013.02.018. [DOI] [PubMed] [Google Scholar]


