Abstract
Background
Antibodies targeting malaria blood-stage antigens are important targets of naturally acquired immunity, and may act as valuable biomarkers of malaria exposure.
Methods
Six-hundred and one young Malawian children from a randomized trial of prenatal nutrient supplementation with iron and folic acid or pre- and postnatal multiple micronutrients or lipid-based nutrient supplements were followed up weekly at home and febrile episodes were investigated for malaria from birth to 18 months of age. Antibodies were measured for 601 children against merozoite surface proteins (MSP1 19kD, MSP2), erythrocyte binding antigen 175 (EBA175), reticulocyte binding protein homologue 2 (Rh2A9), schizont extract and variant surface antigens expressed by Plasmodium falciparum-infected erythrocytes (IE) at 18 months of age. The antibody measurement data was related to concurrent malaria infection and to documented episodes of clinical malaria.
Results
At 18 months of age, antibodies were significantly higher among parasitaemic than aparasitaemic children. Antibody levels against MSP1 19kD, MSP2, schizont extract, and IE variant surface antigens were significantly higher in children who had documented episodes of malaria than in children who did not. Antibody levels did not differ between children with single or multiple malaria episodes before 18 months, nor between children who had malaria before 6 months of age or between 6 and 18 months.
Conclusions
Antibodies to merozoite and IE surface antigens increased following infection in early childhood, but neither age at first infection nor number of malaria episodes substantially affected antibody acquisition. These findings have implications for malaria surveillance during early childhood in the context of elimination.
Trials registration Clinical Trials Registration: NCT01239693 (Date of registration: 11-10-2010). URL: http://www.ilins.org
Keywords: Episodes, Nutrient supplements, Randomized controlled trial, Merozoite antigens, Variant surface antigens, Seroprevalence
Background
Malaria is one of the leading causes of childhood morbidity and mortality, and Plasmodium falciparum infection is responsible for nearly all malaria deaths. The World Health Organization estimated that in 2017 there were 435,000 deaths due to malaria of which around 61% were in children below 5 years of age [1]. Children in malaria-endemic areas become most vulnerable to malarial infection at 4 to 6 months of age as maternally transferred antibodies wane [2] and they then begin to acquire their own antibodies in response to repeated infection. Naturally acquired immunity to malaria develops over time with continuous exposure to infection [3].
Antibodies play a crucial role in mediating acquired immunity to malaria. Blood stage merozoite antigens and variant surface antigens (VSA) expressed on infected erythrocytes (IE) are important targets of this protective immunity. Antibodies to merozoite antigens inhibit invasion of red blood cells (RBCs), prevent intra-erythrocytic growth [4], and promote opsonization for phagocytic clearance [5] and complement fixation [6]. Antibodies to merozoite antigens of sufficient magnitude and function appear to contribute to immunity [7]. In young children or those with limited malaria exposure, they may instead act as biomarkers of malaria exposure [8, 9], with potential to inform surveillance and control activities [10]. Among the tested antigens, merozoite surface protein 1 (MSP1) is the most copious protein found on the surface of the merozoite [11]. Crucial for the primary interaction between merozoites and RBCs in parasite invasion [12], MSP1 is a major target of opsonizing following natural exposure [13]. MSP2 is another abundant, GPI-anchored surface protein necessary for merozoite invasion. Increased IgG level against MSP2 was associated with increasing age, higher haemoglobin level and reduced parasitaemia suggesting its protective effect [14]. Erythrocyte binding antigen 175 (EBA175) is released from micronemes [15] and aggregates at the apical region of the merozoite surface. Antibodies to the RIII-V region of EBA175 have also been associated with protection from malaria [16–18]. Rhoptry-derived Rh2A9 help binding to the RBC receptors after the primary interaction between the RBC and merozoite surface proteins is completed. The level of IgG against Rh2A9 in children (5–14 years) was associated with lower risk of malaria [19].
Antibodies to VSA diminish malaria risk by obstructing cytoadhesion to different host receptors [20, 21] and initiating phagocytic clearance of IE [22]. Several studies have reported associations between levels of anti-VSA antibodies and protection against symptomatic malaria [23–26] but few studies have examined the dynamics of naturally occurring anti-VSA IgG in infants in a malaria-endemic setting [27, 28]. In one study [27], children up to 24 months of age did not acquire antibodies to VSA but in a high-transmission area of Tanzania [29], children had dramatic increases in antibodies to VSA from 1 to 2 years of age. Recent studies in Papua New Guinea suggest that acquired antibodies to VSA play an earlier role in immunity to malaria than antibodies to merozoite antigens [30]. These contradictory findings indicate the need for further studies to investigate the dynamics of naturally acquired immunity targeting both merozoite antigens and VSA in very young children.
This study examines the dynamics of antibody acquisition to multiple merozoite antigens, schizont extract and VSA in young children in response to ongoing exposure to malaria. The study was part of the International Lipid-based Nutrient Supplement (iLiNS) Project DYAD-Malawi randomized controlled trial (clinicaltrials.gov registration number NCT01239693). The original study reported that nutrient supplementation did not have any significant impact on anthropometric indices in 18 months old children [31]. Another sub-study from the same cohort [32] reported that malaria antibody acquisition (against the same antigens reported here) in early infancy was not improved by additional lipid-based nutrient supplementation. For this report, malaria antibody measurement at 18 months of age was related to concurrent malaria infection and to documented episodes of clinical malaria during early childhood to understand the impact of exposure on antibody acquisition.
Methods
Study location and participants
The study participants were 601 infants of 18 months of age from rural Malawi, participants in the iLiNS Project DYAD-Malawi trial. Detailed description of the trial design and supplements has been published elsewhere [33]. Briefly, pregnant women were randomly allocated to supplementation groups that received either iron and folic acid (IFA), multiple micronutrients (MMN) or 20 g of lipid based nutrient supplements (LNS) daily. After delivery, women in the IFA group received placebo, whereas MMN and LNS supplementation was sustained for 6 months post-partum. From 6 to 18 months of age, children in the LNS group received 10 g LNS twice daily.
Detection of malaria
Children were followed up weekly at home and febrile episodes were investigated for malaria. Clinical malaria was defined as fever with axillary temperature above 37.5 °C and parasitaemia was confirmed by microscopy or rapid diagnostic test (RDT). For microscopy, slides were examined under 100× magnification and parasites were counted against 200 leucocytes. The RDT was the Clearview® Malaria Combo (British Biocell International Ltd, Dundee, UK) which detects the proteins P. falciparum lactate dehydrogenase and histidine-rich protein 2.
Preparation of plasma samples
Blood from participants was collected at the 18-month study visit. Plasma was separated by centrifugation and stored at − 80 °C prior to shipping on dry ice to Australia. Samples were thawed, heat inactivated at 57 °C for 45 min, and were stored at − 80 °C until assayed.
Maintenance of parasite culture
Three P. falciparum lines were cultured as previously described [34]. The E8B-ICAM line binds to ICAM-1 and CD36 [35], and expresses group B/C var genes [36]. Rosetting line R29 expresses var genes from group A [37]. A 3D7-derived line had a group A var gene as its dominant transcript, but its binding phenotype was not defined [30]. Cultures were synchronized by hypotonic lysis using 5% sorbitol, and by regular gelatin flotation [38]. To select R29 for high levels of rosetting, it was subject to two rounds of gelatin flotation. After the first round, the pellet was collected and resuspended in gelatin with heparin lithium salt, (0.05 mg/ml Sigma Aldrich), added to disrupt rosettes, and the supernatant was collected.
Measurement of IgG to merozoite antigens and schizont extract
Merozoite antigens MSP119kD, MSP2 (FC27 clone), EBA 175, and P. falciparum reticulocyte binding protein homologue 2 (Rh2A9) were expressed and purified as previously described [16, 19, 32, 39, 40], and schizont extract was prepared as previously described [41]. ELISAs were performed as previously described [32].
Measurement of IgG levels against VSA
IgG antibody levels against VSA were measured by flow cytometry as previously described [32], and flow cytometry data were analysed as described [42].
Data analysis
Data were analysed using Stata version 13.0 (StataCorp, Texas, USA) and graphed using GraphPad Prism version 5 (La Jolla, CA, USA). Antibody levels were measured as optical density (OD) for schizont and merozoite antigens, or as geometric mean fluorescence intensity (MFI) for VSA. They were expressed relative to the positive control which was a pooled plasma sample from malaria exposed individuals from Africa.
Seroprevalence was specified as the percentage of children whose relative antibody level was greater than the mean plus three standard deviations of the negative controls’ antibody levels. Negative controls were a panel of malaria-naïve Melbourne blood donors. Socio-economic status (SES) was derived from an inventory of key household assets (HHA) adapted from [43]. Chi squared tests were performed to test the differences in seropositivity. Mann–Whitney tests were performed for comparing antibody levels between two groups and Kruskal–Wallis tests were performed to compare the antibody levels among more than two groups.
The association between malaria episodes and antibody seroprevalence in 18 months old children was investigated using logistic regression, and linear regression was performed to study the association of malaria episodes with antibody levels. Linear regression was done by transforming antibody levels to their natural logarithm; these were back transformed for reporting descriptive results. Multivariate regression adjusted for the covariates duration of gestation, HIV infection, gender of the child and maternal anaemia.
Results
Study population characteristics
A total of 601 samples from 18 months old children were tested (48.8% male and 51.2% female). The nutrient supplements received by their mothers were IFA in 33.6%, MMN in 33.4%, and 32.9% received LNS. The mean haemoglobin level was 10.8 ± 1.5 g/dl with a prevalence of anaemia (haemoglobin level ≤ 10.9 g/dl) of 46.3%. The percentage of children having P. falciparum parasitaemia at the 18-month visit was 6.5% by microscopy and 9.9% by RDT (Table 1).
Table 1.
Study population characteristics
| Characteristics of the participants | Number (%) [n = 601] |
|---|---|
| Female | 308 (51.2) |
| Blood haemoglobin concentration, mean ± SD, g/dl | 10.8 ± 1.5 |
| Anaemiaa | 278 (46.3) |
| Parasitaemia by microscopy | 39 (6.5) |
| Parasitaemia by RDTb | 60 (9.9) |
| Number of children with malarial episodes | 144 (23.9) |
| Single episode | 119 (19.8) |
| Multiple episodes | 25 (4.2) |
| Low socio-economic status | 357 (59.4) |
| Mother’s education below median | 321 (53.4) |
aAnaemia defined as Hb ≤ 10.9 g/dl
bRapid diagnostic test
Magnitude and prevalence of antibodies and IgG responses in parasitaemic and aparasitaemic children at 18 months
Antibody seroprevalence against merozoite antigens, schizont extract and VSA was measured for all the tested children (Table 2). The seropositivity was highest for MSP1 (54.4%), followed by schizont extract (54.1%). However, IgG against VSA for all the tested parasite lines were very low and few children were seropositive.
Table 2.
Magnitude and prevalence of antibodies and IgG responses in parasitaemic and aparasitaemic children at 18 months
| Antigen tested/parasite isolate | Median antibody levela (IQRb) Number of seropositivec children (%) |
p valued | ||
|---|---|---|---|---|
| All children; (n = 601) | Parasitaemic children; (n = 60) | Aparasitaemic children; (n = 541) | ||
| MSP1 19kDe | 2.80 (0.65, 7.09) | 12.31 (4.38, 28.79) | 2.37 (0.56, 6.08) | < 0.0001 |
| 327 (54.4) | 53 (88.3) | 274 (50.7) | < 0.0001 | |
| MSP2f | 2.91 (0.87, 9.04) | 15.14 (3.47, 35.16) | 2.62 (0.79, 7.28) | < 0.0001 |
| 162 (26.9) | 36 (60.0) | 126 (23.3) | < 0.0001 | |
| EBA175g | 3.38 (1.95, 16.09) | 5.89 (2.89, 21.37) | 3.24 (1.92, 15.89) | 0.0228 |
| 69 (11.5) | 15 (25.0) | 54 (9.9) | 0.001 | |
| Rh2A9h | 7.17 (2.1, 25.3) | 8.59 (3.28, 19.24) | 7.11 (4.05, 13.27) | 0.5630 |
| 151 (25.1) | 23 (38.3) | 128 (23.7) | 0.013 | |
| Schizont | 3.30 (1.27, 8.09) | 17.31 (5.22, 48.66) | 2.95 (1.09, 6.98) | < 0.0001 |
| 325 (54.1) | 58 (96.7) | 267 (49.4) | < 0.0001 | |
| E8Bi | 0 (0, 0.20) | 0.15 (0, 0.86) | 0 (0, 0.16) | < 0.0001 |
| 43 (7.2) | 9 (15.0) | 34 (6.3) | 0.013 | |
| R29i | 0 (0, 0.07) | 0 (0, 1.12) | 0 (0, 0.002) | < 0.0001 |
| 21 (3.5) | 9 (15.0) | 12 (2.2) | < 0.0001 | |
| 3D7i | 0 (0, 0.35) | 0.30 (0, 2.08) | 0 (0, 0.29) | < 0.0001 |
| 50 (8.3) | 17 (28.3) | 33 (6.1) | < 0.0001 | |
Significant p value in italic format
aAntibody levels expressed as units relative to positive control
bInterquartile range
cSamples defined as antibody positive if levels greater than mean + 3SD of negative controls
dp value between parasitaemic and aparasitaemic children calculated by Mann–Whitney test or Chi squared test for antibody level or seropositivity, respectively
eMerozoite surface protein 1
fMerozoite surface protein 2
gErythrocyte binding antigen 175
hReticulocyte binding protein homologue 2A
iVariant surface antigen antibody responses
Children who were parasitaemic (n = 60) by RDT (9.9%) at the time of sample collection at 18 months had higher antibody levels than aparasitaemic children, and differences were statistically significant for all the tested antigens except Rh2A9. The seroprevalence data were also in accordance with the antibody level data and parasitaemic children were more frequently seropositive for all the antigens than the aparasitaemic children (Table 2). Children who were parasitaemic at 6 months (n = 57) were somewhat more likely to experience malarial episodes from 6 to 18 months of age; 14 out of 57 (24.6%) parasitaemic children at 6 months had episodes between 6 to 18 months compared to 99 out of 544 (18.2%) aparasitaemic children (p = 0.24, Chi square).
Association of previous malaria episodes with antibody seroprevalence in 18 months old children
One-hundred and forty-four children (23.9%) had one or more malaria episodes before 18 months of age. Antibody seroprevalence was higher in the children with previous clinical malaria episodes than those without malaria for all the tested antigens, and differences were statistically significant for MSP1, MSP2 and schizont extract and IgG against E8B VSA (Table 3).
Table 3.
Association between malaria episodes and antibody seroprevalence in 18 months old children
| Antigen tested/parasite isolate | Seropositivesa (%) | No episode (n = 457) | Any episode within 18 months % (n = 144) |
p valueb | Single episode % (n = 119) |
p valueb | Multiple episodes % (n = 25) | p valueb | Unadjusted OR (95% CI) | p valuec | Adjusted OR (95% CI) | p valued |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MSP1 19 kDe | 327 (54.4) | 224 (49.0) | 103 (71.5) | < 0.0001 | 83 (69.8) | < 0.0001 | 20 (80.0) | 0.003 | 2.24 (1.59, 3.17) | < 0.0001 | 2.21 (1.56, 3.12) | < 0.0001 |
| MSP2f | 162 (26.9) | 113 (24.7) | 49 (34.0) | 0.028 | 40 (33.6) | 0.051 | 9 (36.0) | 0.207 | 1.41 (1.02, 1.94) | 0.034 | 1.38 (1.00, 1.90) | 0.049 |
| EBA175g | 69 (11.5) | 50 (10.9) | 19 (13.2) | 0.459 | 13 (10.9) | 0.996 | 6 (24.0) | 0.047 | 1.33 (0.87, 2.05) | 0.182 | 1.31 (0.85, 2.01) | 0.216 |
| Rh2A9h | 151 (25.1) | 108 (23.6) | 43 (29.9) | 0.133 | 34 (28.6) | 0.265 | 9 (36.0) | 0.160 | 1.32 (0.95, 1.83) | 0.095 | 1.30 (0.93,1.80) | 0.117 |
| Schizont | 325 (54.1) | 222 (48.6) | 103 (71.5) | < 0.0001 | 85 (71.4) | < 0.0001 | 18 (72.0) | 0.023 | 2.14 (1.52, 3.00) | < 0.0001 | 2.20 (1.55, 3.13) | < 0.0001 |
| E8Bi | 43 (7.2) | 24 (5.3) | 19 (13.2) | 0.001 | 17 (14.3) | 0.001 | 2 (8.0) | 0.554 | 1.85 (1.15, 2.98) | 0.010 | 1.87 (1.15, 3.04) | 0.011 |
| R29i | 21 (3.5) | 13 (2.8) | 8 (5.6) | 0.122 | 7 (5.9) | 0.107 | 1 (4.0) | 0.738 | 1.55 (0.78, 3.09) | 0.204 | 1.51 (0.75, 3.02) | 0.245 |
| 3D7i | 50 (8.3) | 36 (7.9) | 14 (9.7) | 0.485 | 10 (8.4) | 0.850 | 4 (16.0) | 0.152 | 1.31 (0.80, 2.14) | 0.278 | 1.30 (0.79, 2.14) | 0.291 |
Significant p value in italic format
aSamples defined as antibody positive if levels greater than mean + 3SD of negative controls
bp value compared to children with no episode calculated by Chi squared test
cp-value derived from logistic regression with Odds Ratios (OR) and 95% confidence intervals (CI)
dp-value derived from multivariate logistic regression with Adjusted Odds Ratios (OR) after controlling for duration of gestation, HIV infection, gender of the child, maternal anaemia
eMerozoite surface protein 1
fMerozoite surface protein 2
gErythrocyte binding antigen 175
hReticulocyte binding protein homologue 2A
iVariant surface antigen antibody responses
To determine whether the percentage of seropositivity at 18 months of age varies according to the number of malaria episodes, children were divided into groups having either a single episode of malaria or more than one episode of malaria (detected by RDT). One-hundred and nineteen children had single episodes of malaria whereas 25 children had multiple episodes recorded. Antibody seroprevalence was higher in children having a single episode or multiple episodes than those without any episode detected. For a single episode, differences in prevalence were statistically significant for MSP1, schizont extract (p ≤ 0.051) and IgG against VSA expressed by the E8B parasite line (p = 0.001). In the smaller number of children having multiple episodes, prevalence of antibody to MSP1 (0.003), EBA175 (0.047) and schizont extract (0.023) was significantly higher than in children without malaria. There were no significant differences in antibody seroprevalence between those with single or multiple episodes.
Logistic regression revealed that children with any episode of malaria from birth to 18 months of age had significantly higher odds of being seropositive for MSP1, MSP2, schizont extract and VSA against E8B parasite line in both unadjusted (p ≤ 0.034) and adjusted analysis (p ≤ 0.049) than children without any episode.
Association of previous malaria episodes with levels of antibodies in 18 months old children
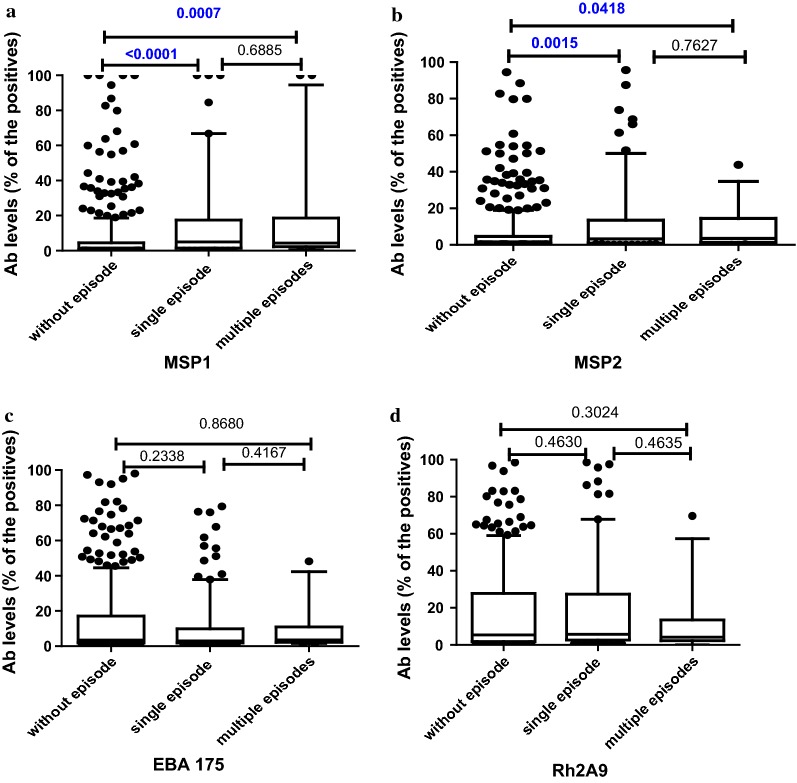
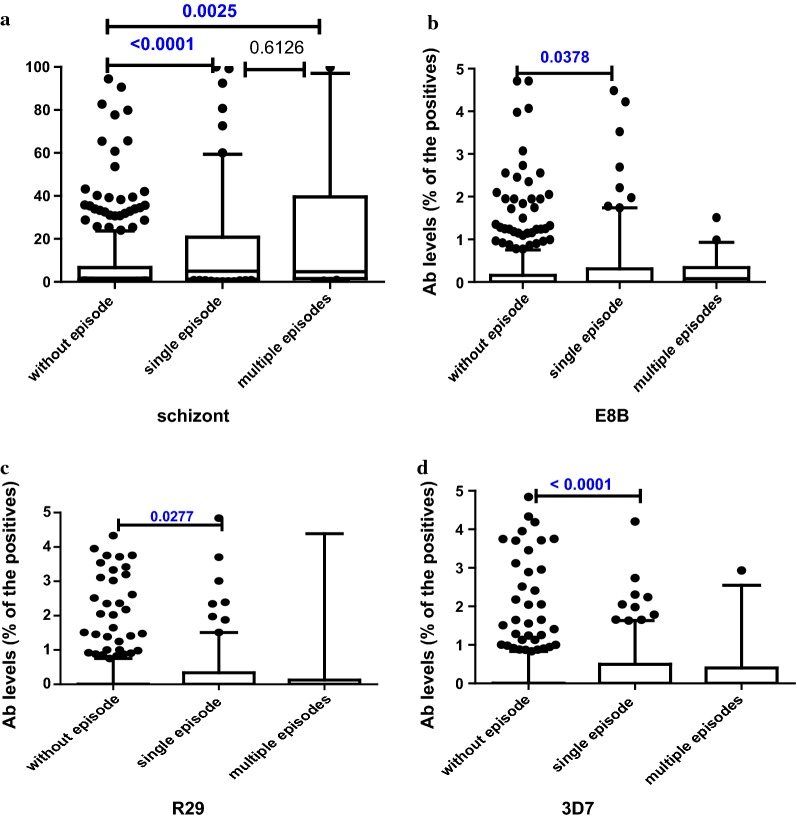
The levels of antibody to malaria antigens were compared between infants who did and did not have previous malaria episodes (Figs. 1, 2). As observed with antibody seropositivity, children having malaria episodes had higher levels of antibodies to several antigens when compared to children without malaria history, and this was significant for MSP1, MSP2 and schizont extract. However, there were no significant differences between the antibody levels of children with single or multiple episodes for any antigen.
Fig. 1.
Levels of antibody at 18 months for a MSP1, b MSP2, c EBA175 and d Rh2A9, by history of episodes of malaria; (N; Without episode = 457, Single episode = 119, Multiple episodes = 25). Data presented as box plots with the Y axis representing antibody levels as a percentage of positive control (pooled plasma of malaria immune adults). The boxes denote the 25th to 75th percentile while the whiskers denote the 10th and the 90th percentile with outliers. p value calculated using Mann–Whitney test between the two groups indicated by the line
Fig. 2.
Levels of antibody at 18 months for a schizont extract, b E8B, c R29 and d 3D7 parasite line, by history of episodes of malaria; (N; Without episode = 457, Single episode = 119, Multiple episodes = 25). Data presented as box plots with the Y axis representing antibody levels as a percentage of positive control (pooled plasma of malaria immune adults). The boxes denote the 25th to 75th percentile while the whiskers denote the 10th and the 90th percentile with outliers. p value calculated using Mann–Whitney test between the two groups indicated by the line
Levels of IgG against VSA were significantly higher for all the tested parasite lines in children having single malaria episode than those who had none (p value 0.038 for E8B, 0.028 for R29 and < 0.0001 for 3D7).
Linear regression (Table 4) indicated that having single or multiple episodes of malaria from birth to 18 months of age was associated with significantly higher antibody levels for MSP1, MSP2 and schizont extract in unadjusted analysis (p ≤ 0.047) and for MSP1 and schizont extract in adjusted analysis (p < 0.0001) for 18 months old children.
Table 4.
Association between number of malaria episodes and antibody level in 18 months old children
| Antigen tested/parasite isolate | Unadjusted coefficient (95% CI) | p valuea | Adjusted coefficient (95% CI) | p valueb |
|---|---|---|---|---|
| MSP1 19 kDc | 1.85 (1.43, 2.41) | < 0.0001 | 1.83 (1.41, 2.37) | < 0.0001 |
| MSP2d | 1.28 (1.00, 1.63) | 0.047 | 1.26 (0.99, 1.61) | 0.057 |
| EBA175e | 0.92 (0.75, 1.11) | 0.399 | 0.91 (0.76, 1.10) | 0.378 |
| Rh2A9f | 1.14 (0.98, 1.33) | 0.074 | 1.14 (0.98, 1.33) | 0.082 |
| Schizont | 1.52 (1.21, 1.91) | < 0.0001 | 1.50 (1.19, 1.87) | < 0.0001 |
| E8Bg | 1.06 (0.75, 1.50) | 0.719 | 1.03 (0.73, 1.46) | 0.826 |
| R29h | 1.33 (0.79, 2.24) | 0.267 | 1.39 (0.81, 2.40) | 0.222 |
| 3D7h | 1.16 (0.79, 1.72) | 0.434 | 1.13 (0.77, 1.67) | 0.508 |
Significant p value in italic format
ap-value derived from linear regression of antibody levels and reported as coefficient and 95% confidence intervals (CI)
bp-value calculated using multivariate linear regression of antibody levels reporting coefficient and 95% confidence intervals (CI) while adjusting for duration of gestation, HIV infection, gender of the child, maternal anaemia
cMerozoite surface protein 1
dMerozoite surface protein 2
eErythrocyte binding antigen 175
fReticulocyte binding protein homologue 2A
gVariant surface antigen antibody responses
Association of age at the time of malaria episode on antibody levels and seroprevalence in 18 months old children
To investigate whether age at the time of clinical malaria affected antibody levels or seroprevalence at 18 months, antibody levels and seroprevalence were compared between children who had malarial episodes prior to 6 months and those who had them between 6 and 18 months of age (Table 5). Both children who had malaria episodes before 6 months of age and those who had malaria episodes from 6 to 18 months had higher antibody levels and seropositivity to multiple antigens compared to those without any history of clinical malaria. However, antibody level or seroprevalence for all of the tested antigens did not differ between children who had malaria before 6 months or from 6 to 18 months.
Table 5.
Association between age at the time of malaria episode and antibody levels and seroprevalence in 18 months old children
| Antigen tested/parasite isolate | No episodea (n = 457) | ≥ 1 episode before 6 months of agea (n = 31) | p valueb | ≥ 1 episode between 6 and 18 months of agea (n = 113) | p valueb |
|---|---|---|---|---|---|
| MSP1 19 kDc | 2.36 (0.51, 5.73) | 6.16 (1.92, 11.16) | 0.0071 | 4.71 (1.43, 21.25) | < 0.0001 |
| 224 (49.0) | 24 (77.5) | 0.002 | 79 (69.9) | < 0.0001 | |
| MSP2d | 2.76 (0.79, 8.23) | 5.76 (1.01, 10.55) | 0.1043 | 3.06 (1.06, 13.97) | 0.3165 |
| 113 (24.7) | 12 (38.8) | 0.084 | 37 (32.7) | 0.083 | |
| EBA175e | 3.49 (1.96, 17.05) | 3.25 (1.89, 8.79) | 0.5785 | 3.19 (1.93, 9.91) | 0.3753 |
| 50 (10.9) | 3 (9.7) | 0.827 | 16 (14.2) | 0.338 | |
| Rh2A9f | 7.03 (3.97, 13.13) | 8.24 (4.41, 17.32) | 0.3790 | 7.92 (4.12, 15.87) | 0.2223 |
| 108 (23.6) | 10 (32.3) | 0.278 | 33 (29.2) | 0.219 | |
| Schizont | 2.95 (1.02, 7.24) | 7.40 (2.24, 13.97) | 0.0211 | 4.70 (1.77, 14.87) | 0.0018 |
| 222 (48.6) | 23 (74.2) | 0.006 | 80 (70.8) | < 0.0001 | |
| E8Bg | 0 (0, 0.15) | 0.03 (0, 1.11) | 0.0177 | 0 (0, 0.26) | 0.0967 |
| 24 (5.3) | 10 (32.3) | < 0.0001 | 9 (7.9) | 0.269 | |
| R29g | 0 (0, 0.002) | 0 (0, 0.43) | 0.0424 | 0 (0, 0.24) | 0.2341 |
| 13 (2.8) | 5 (16.2) | < 0.0001 | 3 (2.6) | 0.913 | |
| 3D7g | 0 (0, 0.33) | 0.01 (0, 0.37) | 0.4718 | 0 (0, 0.42) | 0.8673 |
| 36 (7.9) | 4 (12.9) | 0.324 | 10 (8.9) | 0.734 |
Significant p value in italic format
aFor each antigen represented, row 1: median antibody level (interquartile range); row 2: number of seropositive children (%)
bp value calculated by Mann–Whitney test or Chi squared test for antibody level or seropositivity, respectively
cMerozoite surface protein 1
dMerozoite surface protein 2
eErythrocyte binding antigen 175
fReticulocyte binding protein homologue 2A
gVariant surface antigen antibody responses
Discussion
Naturally acquired immunity to malaria is achieved with ongoing exposure to infections and subsequent acquisition of anti-malarial antibodies. Antibodies against merozoite antigens and VSA are thought to play key roles in conferring immunity against malaria [26, 44]. The aim of this study was to examine how asymptomatic parasitaemia at the time of blood sampling and episodes of clinical malaria in young children affect the early development of antibodies against merozoite antigens and VSA. This study investigated whether the number of episodes in early life, or the age at which they occurred, influenced the development of antibody. The study found that at 18 months of age children who were parasitaemic had significantly higher levels of antibodies and seroprevalence to all the tested VSA and merozoite antigens than the aparasitaemic children, with the exception of antibody to Rh2A9. Children who had experienced clinical malaria episodes before 18 months of age had higher antibody levels and seroprevalence for the tested antigens than children who did not have any episode, and the levels and seroprevalence of antibodies at 18 months of age did not differ depending on the age of the child at the time of malaria episodes. This knowledge is relevant to informing vaccine development and strategies for sero-surveillance of malaria [10].
Previous studies have shown that newborn babies and young infants are relatively protected from symptomatic malaria [45, 46], and this has been attributed mainly to maternally transferred antibodies present in the first few months of life [2, 47]. Young children become most susceptible to infection as maternally derived antibodies wane, and then gradually begin to acquire antibody in response to infections, thus developing naturally acquired immunity to malaria [2, 3].
The present study examined the effect of clinical malaria episodes and parasitaemia on acquisition of antibodies by 18 months of age. At this time, little or no placentally transferred antibody remains, so antibodies elicited are likely to reflect naturally acquired immunity [47]. Antibody levels against all the tested antigens were relatively low, in agreement with earlier studies showing the age dependent acquisition of antibody [48, 49]. The proportion of children with detectable antibodies was highest for MSP1 (54.4%) and schizont extract (54.1%) perhaps because schizont extract acts as a crude marker of blood stage malaria infection whereas MSP1 is the most abundant merozoite surface protein [11]. Antibodies to VSA expressed by IE predominantly consist of antibodies to PfEMP1, the main antigen on the IE surface [50]. Antibodies to VSA are largely strain-specific and repeated exposure leads to the acquisition of a repertoire of antibodies to different variants [51]. Slow acquisition of variant-specific antibody, and possible lack of infection with variants similar to those tested, could explain the very low prevalence of detected antibodies to VSA.
Children who were parasitaemic at the time of sample collection at 18 months had significantly higher levels of antibodies and seroprevalence to all the tested VSA and merozoite antigens (except Rh2A9) than the aparasitaemic children. This finding is consistent with studies from Kenya in which antibodies to VSA [52] and to merozoite antigens [53] were higher in currently parasitaemic individuals. In the latter study, there were more dramatic differences in IgG levels between parasitaemic and aparasitaemic children, than between parasitaemic and aparasitaemic adults. Over two time periods of higher and lower transmission, parasitaemia was strongly associated with higher antibody levels for MSP2 and Rh2A9 (and to other antigens including AMA1 and MSP4), and weakly with antibody to MSP1, EBA175 and schizont extract [53]. In Malawi, by contrast, antibodies to all tested antigens except Rh2A9 were strongly associated with parasitaemia. However, it is possible that some infected children may have been missed because parasitaemia was detected using RDT, which may miss low density infections. Selecting antibody targets for surveillance of malaria exposure [10] will require evaluation in multiple populations and age groups.
The relationship between antibody levels or seroprevalence and history of clinical malaria infections was also investigated. Both measures were higher in children who had experienced clinical malaria episodes before 18 months of age than children who did not, and the differences were significant for MSP1 19 kd, MSP2, schizont extract, and (for antibody levels, but not seroprevalence) for IgG against all tested parasite lines. This is in accordance with other studies that report antibody boosting following exposure to clinical malaria [9, 27, 53–55], and suggests that merozoite (and VSA) antibodies act primarily as biomarkers of exposure in very young children [8, 9]. Some children with no malaria episodes detected did have antibodies; this likely reflects the occurrence of low-density asymptomatic infections that were not detected during follow up and were sufficient to generate antibodies to some antigens.
When the cohort was divided into children with single or multiple malaria episodes, those with single malaria episodes had significantly higher levels of antibody against MSP1, MSP2, schizont extract (≤ 0.0015) and IgG against VSA for all three tested parasite lines (≤ 0.028) compared to those without episodes. Fewer children had multiple episodes, limiting statistical power, but these children also had significantly higher antibody levels against MSP1, MSP2 and schizont extract (≤ 0.0418) than those who did not have malaria. There was no relationship between the number of clinical episodes and either antibody levels or prevalence. These findings suggested that antibodies to MSP1, MSP2 or schizont extract were useful markers of history of clinical malaria, but antibodies to EBA175 and Rh2A9 were not. In Kenyan children 1–8 years old, MSP1, MSP2, Rh2A9 and schizont extract also showed moderate induction following malaria episodes in the previous year, while EBA175 did not [53]. In sum, antibodies to MSP1, MSP2 and schizont protein extract may serve as good biomarkers for sero-surveillance of malaria [10, 56], although other antigens such as AMA1 and MSP4 [53] warrant further evaluation.
Infants’ immune systems are rapidly developing, and responses to infection may differ between younger and older children in magnitude or longevity. To investigate this, antibody levels and prevalence at 18 months were compared between children having malaria before 6 months of age, or from 6 to 18 months. Symptomatic malaria is uncommon in very young infants [3], and only 31 participants (5.15%) had clinical malaria before 6 months of age, whereas 113 (18.8%) had malaria from 6 to 18 months of age. The levels and seroprevalence of antibodies at 18 months of age did not differ between these two groups, and both children with malaria before 6 months of age and children with malaria from 6 to 18 months had higher levels of antibody (except to EBA175) than children with no malaria. This is in keeping with observations suggesting that the time of first exposure to malaria or previous malaria episodes have no effect on the acquisition of antibodies to MSP1, EBA175 and VSA [27, 28], although an earlier longitudinal study of antibody to MSP1 in infants showed highly dynamic antibody responses, with generally short-lived IgG peaks that correlated with symptomatic or asymptomatic infection [47]. Development and persistence of malaria antibody responses in infancy require further exploration.
The strengths of this study include the longitudinal design, with home-based monitoring of children with weekly home visits to 18 months of age and prompt detection and diagnosis of clinical malaria, and the number of antibody assays performed in a large group of over 600 well-characterized infants. The study provides unique insight into the development of antibody responses to VSA in relation to clinical malaria in infancy. Possible study weaknesses include the infrequent blood sampling of asymptomatic children, which gave only limited insights into the relationship between asymptomatic infection and antibody acquisition.
Conclusions
The study provides a considerable insight on the acquisition of antibodies in early infancy in response to concurrent parasitaemia and clinical malaria. This study found that antibodies to tested merozoite and IE surface antigens increased following infection in early childhood and in response to concurrent parasitaemia at 18 months of age, but neither age at first infection nor number of malaria episodes substantially affected the antibody acquisition. The result provides strong evidence that antibodies to blood stage malaria antigens may be biomarkers of infection in early life and this knowledge is relevant to informing vaccine development and strategies for sero-surveillance of malaria.
Authors’ contributions
SJR and PA designed the laboratory studies. PA and KM designed the intervention trial. PB performed laboratory work. PB, SJR, PA and JGB analysed the data. PB and SJR drafted the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to thank Ulla Ashorn, Jaden Bendabenda and Andrew Matchado for collecting the morbidity data for the children, Jack Richards and Wina Hasang for advice and technical support, Kathryn Dewey for comments on the manuscript, Freya Fowkes for comments on the statistical analysis, and Upeksha P. Chandrasiri for providing the clinical database, and Christine Langer for protein expression. We are also thankful to the University of Melbourne Flow Cytometry Core Platform. We acknowledge all the study participants, the local communities, the health services staff and our research personnel at the study sites as well as members of the trial’s data safety and monitoring board, and the International Lipid-based Nutrient Supplementation (iLiNS)-Project Steering Committee (http://www.ilins.org/) for their positive attitude, support and help in all stages of the study.
Competing interests
The author declares that they have no competing interests.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Participating pregnant women provided informed consent for themselves and after delivery for their infants. College of Medicine Research and Ethics Committee, Malawi, and Tampere University Hospital Ethics Committee, Finland granted the ethical approval for the trial and the laboratory work. The laboratory work reported here was also approved by the Melbourne Health Human Research Ethics Committee.
Funding
This work was supported by a grant from the Office of Health, Infectious Diseases, and Nutrition, Bureau for Global Health, U.S. Agency for International Development (USAID) under terms of Cooperative Agreement No. AID-OAA-A-12-00005, through the Food and Nutrition Technical Assistance III Project (FANTA), managed by FHI 360 and additional funding from a grant to the University of California, Davis from the Bill & Melinda Gates Foundation [Grant Number 49817] and the Academy of Finland [Grant Number 252075]. SJR and JGB are supported by a Program Grant from the National Health and Medical Research Council of Australia (NHMRC) [Grant Number 1092789], and NHMRC Senior Research Fellowship [to JGB; APP1077636]. The Burnet Institute is supported by an Operational Infrastructure Support grant from the Victorian State Government, Australia, and the NHMRC Independent Research Institute Infrastructure Support Scheme. PB is supported by Melbourne International Fee Remission Scholarship (MIFRS) and Melbourne Research Scholarship program.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- EBA
erythrocyte binding antigen
- HHA
household assets
- IE
infected erythrocytes
- IFA
iron and folic acid
- iLiNS
International Lipid-based Nutrient Supplement
- LNS
lipid-rich nutrient supplement
- MMN
multiple micronutrients
- MSP
merozoite surface protein
- OR
odds ratio
- PfEMP1
P. falciparum erythrocyte membrane protein-1
- RDT
rapid diagnostic test
- Rh2A9
reticulocyte binding protein homologue 2A
- SES
socio-economic status
- VSA
variant surface antigen
References
- 1.World Health Organization . World malaria report, 2018. Geneva: World Health Organization; 2018. [Google Scholar]
- 2.Dobbs KR, Dent AE. Plasmodium malaria and antimalarial antibodies in the first year of life. Parasitology. 2016;143:129–138. doi: 10.1017/S0031182015001626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Doolan DL, Dobano C, Baird JK. Acquired immunity to malaria. Clin Microbiol Rev. 2009;22:13–36. doi: 10.1128/CMR.00025-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Richards JS, Beeson JG. The future for blood-stage vaccines against malaria. Immunol Cell Biol. 2009;87:377–390. doi: 10.1038/icb.2009.27. [DOI] [PubMed] [Google Scholar]
- 5.Osier FH, Feng G, Boyle MJ, Langer C, Zhou J, Richards JS, et al. Opsonic phagocytosis of Plasmodium falciparum merozoites: mechanism in human immunity and a correlate of protection against malaria. BMC Med. 2014;12:108. doi: 10.1186/1741-7015-12-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyle MJ, Reiling L, Feng G, Langer C, Osier FH, Aspeling-Jones H, et al. Human antibodies fix complement to inhibit Plasmodium falciparum invasion of erythrocytes and are associated with protection against malaria. Immunity. 2015;42:580–590. doi: 10.1016/j.immuni.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richards JS, Arumugam TU, Reiling L, Healer J, Hodder AN, Fowkes FJ, et al. Identification and prioritization of merozoite antigens as targets of protective human immunity to Plasmodium falciparum malaria for vaccine and biomarker development. J Immunol. 2013;191:795–809. doi: 10.4049/jimmunol.1300778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Riley EM, Wagner GE, Ofori MF, Wheeler JG, Akanmori BD, Tetteh K, et al. Lack of association between maternal antibody and protection of African infants from malaria infection. Infect Immun. 2000;68:5856–5863. doi: 10.1128/IAI.68.10.5856-5863.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stanisic DI, Fowkes FJ, Koinari M, Javati S, Lin E, Kiniboro B, et al. Acquisition of antibodies against Plasmodium falciparum merozoites and malaria immunity in young children and the influence of age, force of infection, and magnitude of response. Infect Immun. 2015;83:646–660. doi: 10.1128/IAI.02398-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elliott SR, Fowkes FJI, Richards JS, Reiling L, Drew DR, Beeson JG. Research priorities for the development and implementation of serological tools for malaria surveillance. F1000Prime Rep. 2014;6:100. doi: 10.12703/P6-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gilson PR, Nebl T, Vukcevic D, Moritz RL, Sargeant T, Speed TP, et al. Identification and stoichiometry of glycosylphosphatidylinositol-anchored membrane proteins of the human malaria parasite Plasmodium falciparum. Mol Cell Proteomics. 2006;5:1286–1299. doi: 10.1074/mcp.M600035-MCP200. [DOI] [PubMed] [Google Scholar]
- 12.Baldwin MR, Li X, Hanada T, Liu S-C, Chishti AH. Merozoite surface protein 1 recognition of host glycophorin A mediates malaria parasite invasion of red blood cells. Blood. 2015;125:2704–2711. doi: 10.1182/blood-2014-11-611707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jaschke A, Coulibaly B, Remarque EJ, Bujard H, Epp C. Merozoite surface protein 1 from Plasmodium falciparum is a major target of opsonizing antibodies in individuals with acquired immunity against malaria. Clin Vaccine Immunol. 2017;24:e00155-17. doi: 10.1128/CVI.00155-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khosravi A, Hommel M, Sayemiri K. Age-dependent antibody response to Plasmodium falciparum merozoite surface protein 2 (MSP-2) Parasite Immunol. 2011;33:145–157. doi: 10.1111/j.1365-3024.2010.01260.x. [DOI] [PubMed] [Google Scholar]
- 15.Sim BK, Toyoshima T, Haynes JD, Aikawa M. Localization of the 175-kilodalton erythrocyte binding antigen in micronemes of Plasmodium falciparum merozoites. Mol Biochem Parasitol. 1992;51:157–159. doi: 10.1016/0166-6851(92)90211-2. [DOI] [PubMed] [Google Scholar]
- 16.Richards JS, Stanisic DI, Fowkes FJ, Tavul L, Dabod E, Thompson JK, et al. Association between naturally acquired antibodies to erythrocyte-binding antigens of Plasmodium falciparum and protection from malaria and high-density parasitemia. Clin Infect Dis. 2010;51:e50–e60. doi: 10.1086/656413. [DOI] [PubMed] [Google Scholar]
- 17.Toure FS, Bisseye C, Mavoungou E. Imbalanced distribution of Plasmodium falciparum EBA-175 genotypes related to clinical status in children from Bakoumba, Gabon. Clin Med Res. 2006;4:7–11. doi: 10.3121/cmr.4.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiu CY, White MT, Healer J, Thompson JK, Siba PM, Mueller I, et al. Different regions of Plasmodium falciparum erythrocyte-binding antigen 175 induce antibody responses to infection of varied efficacy. J Infect Dis. 2016;214:96–104. doi: 10.1093/infdis/jiw119. [DOI] [PubMed] [Google Scholar]
- 19.Reiling L, Richards JS, Fowkes FJI, Barry AE, Triglia T, Chokejindachai W, et al. Evidence that the erythrocyte invasion ligand PfRh2 is a target of protective immunity against Plasmodium falciparum malaria. J Immunol. 2010;185:6157–6167. doi: 10.4049/jimmunol.1001555. [DOI] [PubMed] [Google Scholar]
- 20.Claessens A, Adams Y, Ghumra A, Lindergard G, Buchan CC, Andisi C, et al. A subset of group A-like var genes encodes the malaria parasite ligands for binding to human brain endothelial cells. Proc Natl Acad Sci USA. 2012;109:E1772–E1781. doi: 10.1073/pnas.1120461109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oleinikov AV, Amos E, Frye IT, Rossnagle E, Mutabingwa TK, Fried M, et al. High throughput functional assays of the variant antigen PfEMP1 reveal a single domain in the 3D7 Plasmodium falciparum genome that binds ICAM1 with high affinity and is targeted by naturally acquired neutralizing antibodies. PLoS Pathog. 2009;5:e1000386. doi: 10.1371/journal.ppat.1000386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Celada A, Cruchaud A, Perrin LH. Opsonic activity of human immune serum on in vitro phagocytosis of Plasmodium falciparum infected red blood cells by monocytes. Clin Exp Immunol. 1982;47:635–644. [PMC free article] [PubMed] [Google Scholar]
- 23.Bull PC, Lowe BS, Kortok M, Molyneux CS, Newbold CI, Marsh K. Parasite antigens on the infected red cell surface are targets for naturally acquired immunity to malaria. Nat Med. 1998;4:358. doi: 10.1038/nm0398-358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dodoo D, Staalsoe T, Giha H, Kurtzhals JA, Akanmori BD, Koram K, et al. Antibodies to variant antigens on the surfaces of infected erythrocytes are associated with protection from malaria in Ghanaian children. Infect Immun. 2001;69:3713–3718. doi: 10.1128/IAI.69.6.3713-3718.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giha HA, Staalsoe T, Dodoo D, Roper C, Satti GM, Arnot DE, et al. Antibodies to variable Plasmodium falciparum-infected erythrocyte surface antigens are associated with protection from novel malaria infections. Immun Lett. 2000;71:117–126. doi: 10.1016/S0165-2478(99)00173-X. [DOI] [PubMed] [Google Scholar]
- 26.Chan JA, Fowkes FJI, Beeson JG. Surface antigens of Plasmodium falciparum-infected erythrocytes as immune targets and malaria vaccine candidates. Cell Mol Life Sci. 2014;71:3633–3657. doi: 10.1007/s00018-014-1614-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nhabomba AJ, Guinovart C, Jimenez A, Manaca MN, Quinto L, Cistero P, et al. Impact of age of first exposure to Plasmodium falciparum on antibody responses to malaria in children: a randomized, controlled trial in Mozambique. Malar J. 2014;13:121. doi: 10.1186/1475-2875-13-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quelhas D, Jimenez A, Quinto L, Serra-Casas E, Mayor A, Cistero P, et al. IgG against Plasmodium falciparum variant surface antigens and growth inhibitory antibodies in Mozambican children receiving intermittent preventive treatment with sulfadoxine-pyrimethamine. Immunobiol. 2011;216:793–802. doi: 10.1016/j.imbio.2010.12.010. [DOI] [PubMed] [Google Scholar]
- 29.Vestergaard LS, Lusingu JP, Nielsen MA, Mmbando BP, Dodoo D, Akanmori BD, et al. Differences in human antibody reactivity to Plasmodium falciparum variant surface antigens are dependent on age and malaria transmission intensity in northeastern Tanzania. Infect Immun. 2008;76:2706–2714. doi: 10.1128/IAI.01401-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chan JA, Stanisic DI, Duffy MF, Robinson LJ, Lin E, Kazura JW, et al. Patterns of protective associations differ for antibodies to P. falciparum-infected erythrocytes and merozoites in immunity against malaria in children. Eur J Immunol. 2017;47:2124–2136. doi: 10.1002/eji.201747032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ashorn P, Alho L, Ashorn U, Cheung YB, Dewey KG, Gondwe A, et al. Supplementation of maternal diets during pregnancy and for 6 months postpartum and infant diets thereafter with small-quantity lipid-based nutrient supplements does not promote child growth by 18 months of age in rural Malawi: a randomized controlled trial. J Nutr. 2015;145:1345–1353. doi: 10.3945/jn.114.207225. [DOI] [PubMed] [Google Scholar]
- 32.Barua P, Chandrasiri UP, Beeson JG, Dewey KG, Maleta K, Ashorn P, et al. Effect of nutrient supplementation on the acquisition of humoral immunity to Plasmodium falciparum in young Malawian children. Malar J. 2018;17:74. doi: 10.1186/s12936-018-2224-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ashorn P, Alho L, Ashorn U, Cheung YB, Dewey KG, Harjunmaa U, et al. The impact of lipid-based nutrient supplement provision to pregnant women on newborn size in rural Malawi: a randomized controlled trial. Am J Clin Nutr. 2015;101:387–397. doi: 10.3945/ajcn.114.088617. [DOI] [PubMed] [Google Scholar]
- 34.Chandrasiri UP, Randall LM, Saad AA, Bashir AM, Rogerson SJ, Adam I. Low antibody levels to pregnancy-specific malaria antigens and heightened cytokine responses associated with severe malaria in pregnancy. J Infect Dis. 2014;209:1408–1417. doi: 10.1093/infdis/jit646. [DOI] [PubMed] [Google Scholar]
- 35.Biggs BA, Anders RF, Dillon HE, Davern KM, Martin M, Petersen C, et al. Adherence of infected erythrocytes to venular endothelium selects for antigenic variants of Plasmodium falciparum. J Immunol. 1992;149:2047–2054. [PubMed] [Google Scholar]
- 36.Duffy MF, Byrne TJ, Carret C, Ivens A, Brown GV. Ectopic recombination of a malaria var gene during mitosis associated with an altered var switch rate. J Mol Biol. 2009;389:453–469. doi: 10.1016/j.jmb.2009.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rowe JA, Moulds JM, Newbold CI, Miller LHP. falciparum rosetting mediated by a parasite-variant erythrocyte membrane protein and complement-receptor 1. Nature. 1997;388:292–295. doi: 10.1038/40888. [DOI] [PubMed] [Google Scholar]
- 38.Goodyer ID, Johnson J, Eisenthal R, Hayes DJ. Purification of mature-stage Plasmodium falciparum by gelatine flotation. Ann Trop Med Parasitol. 1994;88:209–211. doi: 10.1080/00034983.1994.11812859. [DOI] [PubMed] [Google Scholar]
- 39.Stanisic DI, Richards JS, McCallum FJ, Michon P, King CL, Schoepflin S, et al. Immunoglobulin G subclass-specific responses against Plasmodium falciparum merozoite antigens are associated with control of parasitemia and protection from symptomatic illness. Infect Immun. 2009;77:1165–1174. doi: 10.1128/IAI.01129-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Triglia T, Chen L, Lopaticki S, Dekiwadia C, Riglar DT, Hodder AN, et al. Plasmodium falciparum merozoite invasion is inhibited by antibodies that target the PfRh2a and b binding domains. PLoS Pathog. 2011;7:e1002075. doi: 10.1371/journal.ppat.1002075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Persson KEM, McCallum FJ, Reiling L, Lister NA, Stubbs J, Cowman AF, et al. Variation in use of erythrocyte invasion pathways by Plasmodium falciparum mediates evasion of human inhibitory antibodies. J Clin Invest. 2008;118:342–351. doi: 10.1172/JCI32138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Teo A, Hasang W, Rogerson S. Evaluating IgG antibody to variant surface antigens expressed on Plasmodium falciparum infected erythrocytes using flow cytometry. Methods Mol Biol. 2015;1325:207–213. doi: 10.1007/978-1-4939-2815-6_17. [DOI] [PubMed] [Google Scholar]
- 43.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- 44.Beeson JG, Drew DR, Boyle MJ, Feng G, Fowkes FJ, Richards JS. Merozoite surface proteins in red blood cell invasion, immunity and vaccines against malaria. FEMS Microbiol Rev. 2016;40:343–372. doi: 10.1093/femsre/fuw001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brabin B. An analysis of malaria parasite rates in infants: 40 years after Macdonald. Trop Dis Bull. 1990;87:1–21. [PubMed] [Google Scholar]
- 46.Macdonald G. The analysis of malaria parasite rates in infants. Trop Dis Bull. 1950;47:915–938. [PubMed] [Google Scholar]
- 47.Branch OH, Udhayakumar V, Hightower AW, Oloo AJ, Hawley WA, Nahlen BL, et al. A longitudinal investigation of IgG and IgM antibody responses to the merozoite surface protein-1 19-kiloDalton domain of Plasmodium falciparum in pregnant women and infants: associations with febrile illness, parasitemia, and anemia. Am J Trop Med Hyg. 1998;58:211–219. doi: 10.4269/ajtmh.1998.58.211. [DOI] [PubMed] [Google Scholar]
- 48.Agnandji ST, Lell B, Soulanoudjingar SS, Fernandes JF, Abossolo BP, Conzelmann C, et al. First results of phase 3 trial of RTS, S/AS01 malaria vaccine in African children. New Engl J Med. 2011;365:1863–1875. doi: 10.1056/NEJMoa1102287. [DOI] [PubMed] [Google Scholar]
- 49.Branch OH, Oloo AJ, Nahlen BL, Kaslow D, Lal AA. Anti-merozoite surface protein-1 19-kDa IgG in mother-infant pairs naturally exposed to Plasmodium falciparum: subclass analysis with age, exposure to asexual parasitemia, and protection against malaria. V. The Asembo Bay Cohort Project. J Infect Dis. 2000;181:1746–1752. doi: 10.1086/315424. [DOI] [PubMed] [Google Scholar]
- 50.Chan J-A, Howell KB, Langer C, Maier AG, Hasang W, Rogerson SJ, et al. A single point in protein trafficking by Plasmodium falciparum determines the expression of major antigens on the surface of infected erythrocytes targeted by human antibodies. Cell Mol Life Sci. 2016;73:4141–4158. doi: 10.1007/s00018-016-2267-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bull PC, Lowe BS, Kortok M, Marsh K. Antibody recognition of Plasmodium falciparum erythrocyte surface antigens in Kenya: evidence for rare and prevalent variants. Infect Immun. 1999;67:733–739. doi: 10.1128/iai.67.2.733-739.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bull PC, Lowe BS, Kaleli N, Njuga F, Kortok M, Ross A, et al. Plasmodium falciparum infections are associated with agglutinating antibodies to parasite-infected erythrocyte surface antigens among healthy Kenyan children. J Infect Dis. 2002;185:1688–1691. doi: 10.1086/340420. [DOI] [PubMed] [Google Scholar]
- 53.McCallum FJ, Persson KE, Fowkes FJ, Reiling L, Mugyenyi CK, Richards JS, et al. Differing rates of antibody acquisition to merozoite antigens in malaria: implications for immunity and surveillance. J Leukoc Biol. 2017;101:913–925. doi: 10.1189/jlb.5MA0716-294R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dechavanne C, Sadissou I, Bouraima A, Ahouangninou C, Amoussa R, Milet J, et al. Acquisition of natural humoral immunity to P. falciparum in early life in Benin: impact of clinical, environmental and host factors. Sci Rep. 2016;6:33961. doi: 10.1038/srep33961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Helb DA, Tetteh KK, Felgner PL, Skinner J, Hubbard A, Arinaitwe E, et al. Novel serologic biomarkers provide accurate estimates of recent Plasmodium falciparum exposure for individuals and communities. Proc Natl Acad Sci USA. 2015;112:E4438–E4447. doi: 10.1073/pnas.1501705112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Corran P, Coleman P, Riley E, Drakeley C. Serology: a robust indicator of malaria transmission intensity? Trends Parasitol. 2007;23:575–582. doi: 10.1016/j.pt.2007.08.023. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included within the article and its additional files.