Abstract
Objective
Cesarean section (CS) is one of the most common surgical procedures in the world. In developed and developing countries, CS has grown significantly over the past decades. The Iranian Ministry of Health and Medical Education has developed a health transformation plan (HTP) in order to reduce CS rate and promote vaginal delivery. This study was conducted with the aim of reviewing the results of published studies on the impact of the HTP on CS in Iran.
Results
We searched Embase, PubMed/MEDLINE, ISI/Web of Sciences, Scopus, as well as Iranian databases (MagIran, SID and Barakatkns), from May 2014 to October 2018. To assess the quality of studies, the checklist “A Cochrane Risk of Bias Assessment Tool: for Non-Randomized Studies of Interventions” was utilized. Twelve studies were selected. Seven studies reported statistically significant results, showing a positive impact of the implementation of the HTP on CS reduction. Despite the decreased CS rate in Iran after about 4 years of the implementation of this policy, the goal of a yearly reduction by 10% has not been achieved yet. Increasing access to maternity services and community-based education through mass media could help changing the attitudes of Iranian mothers towards CS.
Keywords: Cesarean section, Health transformation plan, Health policy, Iran
Introduction
Health is a valuable global capital, and, hence, health policy- and decision-makers are working to improve it, ensuring the delivery of better health provisions, a fair and just access to healthcare facilities and implementing effective policies [1]. Most countries are developing, evaluating and re-programming health policies, and, therefore, health system reforms can be considered as a continuous improvement cycle to achieve better health levels [2]. In its 2000 report, the World Health Organization (WHO) has stated that public organisms and organizations should promote health and well-being, meeting with the expectations of the users, guaranteeing access to services and protecting against increasing health costs [3].
Iran, one of the Eastern Mediterranean Regional Office (EMRO) countries, has suffered from various health problems due to economic-financial issues, causing people to be dissatisfied with the services of various sectors of the healthcare system. Following the establishment of President Rouhani, the Ministry of Health and Medical Education (MoHME) of Iran has developed a health sector evolution plan (“health transformation plan”, HTP). The HTP, which has sought to financially protect people against healthcare costs, has significantly improved the quality of health services and has increased their access. It has been implemented in public hospitals nationwide since May 5, 2014 [4].
One of the indicators of proper healthcare provisions is the rate of cesarean section (CS). CS is one of the most common surgical procedures worldwide. In developed and developing countries, CS has grown significantly over the past decades [5, 6]. In 1985, the WHO announced that the acceptable rate of CS should be in the range 5–15% [7]. According to a meta-analysis, CS rate in Iran was estimated to be 48% [8]. This high, unacceptable figure can be seen as a warning, which should foster the implementation of adequate policies to reduce CS in Iran.
Unnecessary CS can have adverse consequences on health both for the mother and the infant. A WHO study showed that maternal mortality was higher for CS than for vaginal delivery [9], also indicating that there is a very strong relationship between CS and infant mortality [10]. Furthermore, unnecessary CS imposes financial costs both for households and the entire healthcare system [5].
Health policy- and decision-makers in Iran in the past have proposed several plans to reduce CS rate [11]. Lack of proper knowledge of the complications of CS, fear of pain, psychological stress, and shortened delivery time are the major factors contributing to the choice of having CS [12, 13].
A comprehensive package for the promotion of vaginal delivery aimed at promoting maternal and infant health in public hospitals was included in the HTP. According to this policy, all hospitals were required to curb the CS rate by 10% per year. In order to encourage mothers to undergo normal vaginal delivery, this was offered in public state hospitals free of charge. In addition, to protect the mother’s privacy and the pleasantness of the delivery process, the environment, in which the delivery was performed, was optimized. Encouraging public agencies and service providers to deliver methods for reducing labor pain, including pharmacological and non-pharmacological methods, was also implemented by the plan. In addition, to support the culture of pregnancy and childbirth, the provision of maternity-ready classes for pregnant mothers and the empowerment of service providers were among the other measures taken for the promotion of vaginal delivery. To investigate the effect of the HTP on CS after its implementation, different studies have been carried out. Pooling these investigations together can help assessing the overall effect of the HTP on CS rate, as well as improving decision making for developing and providing more suitable and effective programs. Therefore, this study was conducted with the aim of systematically reviewing the results of published studies on the impact of the HTP on CS in Iran.
Main text
Literature search
This review has been performed according to the “The Meta-analysis of Observational Studies in Epidemiology” (MOOSE) guidelines [14]. Two authors independently searched several scholarly databases, including Embase, PubMed/MEDLINE, ISI/Web of Sciences (WOS), Scopus, as well as Iranian thesauri (such as MagIran, SID and Barakatkns), from May 2014 to October 2018. The search strategy was: (“cesarean” OR “cesarean section” OR “caesarean delivery” OR “childbirth”) AND (“health system reform” OR “health reform” OR “health sector evolution plan” OR “health transition” OR “health transition plan” OR “health transformation” OR “health transformation plan”) AND (Iran). The search strategy was developed by consulting an expert librarian. The reference list of each eligible article was also reviewed for potentially relevant studies. Any disagreements were resolved through discussion.
Inclusion and exclusion criteria
Studies investigating the effect of the HTP on CS in the form of cross-sectional, cohort, time-series studies written in English or Persian were included. Those studies whose results were not clear, or designed as letters to editor, editorials, case-reports, case-series, commentaries or conference abstracts were excluded.
Quality assessment
To assess the quality of studies included in the present systematic review, the checklist “A Cochrane Risk of Bias Assessment Tool: for Non-Randomized Studies of Interventions” (ACROBAT-NRSI) was utilized [15].
Data extraction
The surname of the first author, the year of publication, the location of the study, the study design, the number of participants, and the most important findings of the included studies were independently extracted by 2 authors. Any discrepancy was solved through discussion.
Results
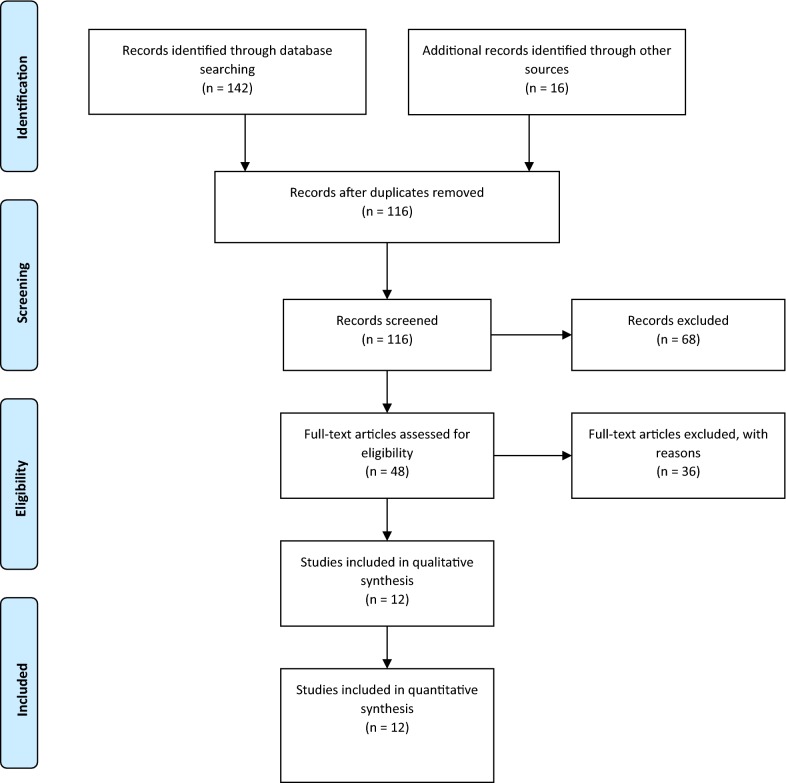
In the initial search, 158 studies were found. Then, 42 duplicate studies were deleted. After reviewing the title, 68 studies were excluded. In the next step, the abstract of the studies was assessed and, finally, 12 studies meeting with the previously stated inclusion criteria were selected [16–27], as shown in Fig. 1.
Fig. 1.
Process of studies retrieval and selection
Studies were conducted between 2015 and 2018. In most studies, the HTP was implemented in public hospitals, whereas in 3 and 2 studies in private and health ministry hospitals, respectively. According to the study design, 4 and 6 investigations were cross-sectional and descriptive-analytic studies, 1 was a time series analysis and 1 a quasi-experimental investigation. Seven studies reported statistically significant results. An overall decrease in CS rate was observed for public hospitals, whereas the effect of the HTP on CS in private hospitals was mixed, with 1 study reporting a significant increase, 1 study computing a significant decrease and a further study reporting unclear findings (Table 1).
Table 1.
The main findings of the studies included in the present systematic review
| First author/references | Year of publication | Location | Study design | Method of study | Main findings |
|---|---|---|---|---|---|
| Zarei [16] | 2015 | Tehran | Cross-sectional | A public hospital was selected and information from 2013 and 2014 was compared | Physicians were able to reduce CS by 3 to 7% compared to last year |
| Piroozi [17] | 2016 | Kurdistan | Descriptive-analytic | Data were collected in 2013 and 1 year after the implementation of the HTP in public hospitals, Social Security Hospitals and 1 private hospital | CS decreased by 14.62% compared to the year before the plan was implemented in 9 public state hospitals. In social welfare hospitals, CS rate worsened in 2 hospitals. In the private hospital, a 0.21% increase in CS was observed. Results were statistically significant |
| Seidali [18] | 2016 | Khuzestan | Descriptive-analytic | Data were collected 6 months after the implementation of the plan and compared with the previous year in public hospitals | After implementation of the HTP, CS rate decreased from 49.56% to 32.10%. Results were statistically significant |
| Rooeintan [19] | 2016 | Fars | Cross-sectional | Information was collected from private and public hospitals between 2013 and 2014 | CS dropped from 64.7% to 58.6%. Findings about the decrease or increase in private hospitals were unclear. The results were not statistically significant |
| Dehghan [20] | 2017 | Yazd | Descriptive-analytic | Information was collected and compared between 2013 and 2014 in 15 public and private hospitals | CS decreased from 52.64% to 47.37%. In public hospitals, it decreased from 45.2% to 36.71% and in private hospitals from 56.7% to 54.36%. Results were statistically significant |
| Fouladi [21] | 2017 | Qom | Descriptive-analytic | Two public hospitals were selected and data were compared 2 years before and 2 years after the implementation of the plan | The rate of CS in hospital A decreased from 49.43% to 41% and in hospital B from 46.76% to 43.36%. Results were not statistically significant |
| Zaboli [22] | 2017 | Kerman | Cross-sectional | Seven public hospitals were selected and information was reviewed 6 months before the plan and 6 months after | CS decreased from 48.02% to 43.43%. Results were not statistically significant |
| Zandian [23] | 2017 | Ardabil | Cross-sectional | Information between 2013 and 2015 was collected from a public hospital | CS decreased from 60.5% to 43%. Results were statistically significant |
| Karami Matin [24] | 2018 | Kermanshah | Time series analysis | Information from 15 public hospitals was reviewed between 2012 and 2016 | CS dropped by 11% a month after the implementation of the plan, and after the implementation of the plan, the monthly increase was 0.0017%. Results showed that the plan was not effective in reducing CS. |
| Rezaie [25] | 2018 | Fars | Descriptive-analytic | Between 2014 and 2015, information was collected from a public hospital | CS was reduced from 47.57% to 38.70%. Results were statistically significant |
| Yusefi [26] | 2018 | Fars | Descriptive-analytic | Information was collected from 10 public hospitals between 2013 and 2015 | CS decreased. Results were statistically significant |
| Jabbari [27] | 2018 | Isfahan | Quasi-experimental | Data was collected from 22 public and 6 private hospitals in 6 months before and after the implementation of the HTP | CS decreased. Results were statistically significant |
The quality of the studies based on the ACROBAT-NRSI is presented in Table 2. More in detail, bias due to confounding was low for all studies, whilst bias in selection of participants was generally low but moderate for 2 studies. Bias in measurement of interventions was moderate for 3 studies, as well as bias due to departures from intended intervention. Bias due to missing data was moderate for 4 studies. Bias in measurement of outcomes was moderate for 5 studies, whereas bias in selection of reported results resulted moderate for 6 studies.
Table 2.
Result of the quality assessment of the studies included in the present systematic review
| Study | Domains of bias | ||||||
|---|---|---|---|---|---|---|---|
| Bias due to confounding | Bias in selection of participants | Bias in measurement of interventions | Bias due to departures from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of reported results | |
| Zarei | Low risk | Moderate risk | Low risk | Low risk | Moderate risk | Low risk | Moderate risk |
| Piroozi | Low risk | Low risk | Low risk | Moderate risk | Low risk | Low risk | Low risk |
| Seidali | Low risk | Low risk | Low risk | Low risk | Moderate risk | Moderate risk | Low risk |
| Rooeintan | Low risk | Low risk | Moderate risk | Low risk | Moderate risk | Low risk | Moderate risk |
| Dehghan | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | Moderate risk |
| Fouladi | Low risk | Moderate risk | Moderate risk | Low risk | Low risk | Moderate risk | Moderate risk |
| Zaboli | Low risk | Low risk | Low risk | Low risk | Moderate risk | Low risk | Low risk |
| Zandian | Low risk | Low risk | Moderate risk | Low risk | Low risk | Moderate risk | Moderate risk |
| Karami Matin | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
| Rezaie | Low risk | Low risk | Low risk | Moderate risk | Low risk | Low risk | Low risk |
| Yusefi | Low risk | Low risk | Low risk | Moderate risk | Low risk | Moderate risk | Moderate risk |
| Jabbari | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk |
Discussion
To the best of our knowledge, this study is the first systematic review of the impact of the implementation of the HTP on the CS rate in Iran. According to a meta-analytical study in 2014, the rate of CS was estimated to be 48% [8], comparable with the rate computed for Lebanon (49%) [6], but higher than the rate found for Pakistan (9.2%) [28]. In a study published in 2016, the temporal trend of CS between 1990 and 2014 has been studied. The highest percentages were found in Latin America and the Caribbean, whereas in Asia, Oceania, Europe and Africa a rate of 15.1%, 14.1%, 13.8%, and 4.5% was computed, respectively. CS had a worrying upward trend in most countries of the world. Therefore, policy- and decision-makers should take effective health policies and strategies to reduce this trend [29].
Health policy-makers in Iran should be aware that CS is a surgical operation that has its own complications and may have long-term effects and serious consequences for future pregnancies in women [30, 31]. Promotion of vaginal delivery and reduction of CS are the main priorities of the MoHME [11], which aims at ensuring a high quality maternal care. Therefore, the HTP was designed to reduce the rate of CS.
The present review showed that CS exhibited a decreasing trend after the implementation of the HTP, also because vaginal delivery was offered free of charge. Paying attention to financial issues in health system reform is, indeed, very important, and, on the other hand, the cost of CS directly impacts on the cost of health care [32]. Increasing the offer of CS would increase direct payments and out-of-pocket (OOP) expenditure, dramatically weakening the sustainability of the healthcare system. In a study by Moradi and collaborators, assessing the effectiveness of the package for the promotion of vaginal delivery, midwives and physicians said that free-of-charge offer represented a major incentive for choosing natural delivery, besides the reduced maternity services tariffs [33]. On the other hand, doctors and providers of maternity services have less legal responsibilities in performing normal labor compared to CS [34, 35].
Despite the decreased CS rate, the target of a yearly reduction by 10% was not achieved, probably for a variety of reasons, not currently well understood, including cultural, social and economic factors [29]. In a study, for instance, mothers have expressed concerns and pain of normal labor, including fear of rupture, deformation and relaxation of the genitalia [36].
Furthermore, the findings of the present study showed that, after the implementation of the HTP, the rate of CS increased in some private hospitals. This is consistent with the literature and studies performed in other countries. For example, in a study conducted in Peru, after reforming the health sector, and changing the payment mechanisms, CS rate increased from 28 to 53% [37]. Also, another study in Uruguay showed that, due to increased payments to doctors in the private sector, CS rate was twice as high as in the public sector [38], due to financial incentives for physicians and reimbursement of costs by insurers [39–41]. In many cases, insurance covers the cost of CS in the private sector, which makes mothers not worried about the costs. In a meta-analysis, the results showed that mothers with private insurance had a greater tendency for choosing CS in the private sector [42].
Conclusions
Overall, a positive impact of the implementation of the HTP on CS reduction was shown in the existing scholarly literature. However, despite the decreased CS rate in Iran, the goal of a yearly reduction by 10% has not been achieved yet.
Recommendation
Extensive efforts should be made to properly implement health policies, and, in this regard, support should be granted to all stakeholders and groups that can contribute to the effective implementation. If the process of implementation of a policy is accompanied by a slowdown and encounters problems, negotiation, training and various strategies should be taken as proper measures and interventions [43].
Health policy- and decision-makers have implemented a package for promoting natural delivery and reducing CS rate. To further explore the effect of this policy, more studies are needed in all Iranian provinces in public and, especially, private hospitals. To achieve the goal of reducing CS, all individuals and groups should be involved. Encouraging physicians to perform vaginal delivery through reforming the payment mechanisms, and increasing access to maternity services and community-based education through mass media could help changing the attitude of Iranian mothers towards CS.
Limitations
This study has some limitations that should be properly mentioned: there is a dearth of studies aimed at evaluating the effectiveness of this policy on the reduction of CS in many Iranian provinces, especially the provinces with the highest rates of CS. Also, there is a need of qualitative studies on the tendency of mothers to choose CS rather than normal delivery, as well as investigations related to the opinions of physicians and midwives after the implementation of the HTP. Most studies merely collected information from public hospitals and less from private hospitals. Another shortcoming of the present review is the publication bias, due to the fact that gray literature was not searched.
Authors’ contributions
AB and MaB designed the study. MeB and AB searched databases, extracted data and performed study selection. MaB, FG, SAand NLB performed data analysis. MeB, AB, FG, and NLB interpreted the results. MaB wrote the manuscript. AB, MaB, MS, and NLB have been involved in drafting the manuscript or revising it critically for important intellectual content. MaB, AB and NLB carried out a final revision and grammar editing. All authors read and approved the final version of the manuscript.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The raw data (primary literature) is publicly available.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- HTP
health transformation plan
- CS
cesarean section
- MoHME
Ministry of Health and Medical Education
- ACROBAT-NRSI
A Cochrane Risk of Bias Assessment Tool: for Non-Randomized Studies of Interventions
- WHO
World Health Organization
- EMRO
Eastern Mediterranean Regional Office
- OOP
out-of-pocket
Contributor Information
Meysam Behzadifar, Email: m_behzadifar67@yahoo.com.
Masoud Behzadifar, Email: behzadifar.m@tak.iums.ac.ir, Email: masoudbehzadifar@gmail.com.
Ahad Bakhtiari, Email: ah.bakhtyari@gmail.com.
Samad Azari, Email: samadazari1010@gmail.com.
Mandana Saki, Email: mandana_saki@yahoo.com.
Farnaz Golbabayi, Email: farnaz2006_1000@yahoo.com.
Nicola Luigi Bragazzi, Email: robertobragazzi@gmail.com.
References
- 1.Van der Wees PJ, Zaslavsky AM, Ayanian JZ. Improvements in Health Status after Massachusetts Health Care Reform. Milbank Q. 2013;91(4):663–689. doi: 10.1111/1468-0009.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frenk J. The global health system: strengthening national health systems as the next step for global progress. PLoS Med. 2010;7(1):e1000089. doi: 10.1371/journal.pmed.1000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. The world health report 2000—Health systems: improving performance. 2000. http://www.who.int/whr/2000/en/. Accessed 24 Apr 2018.
- 4.Moradi-Lakeh M, Vosoogh-Moghaddam A. Health sector evolution plan in Iran; equity and sustainability concerns. Int J Health Policy Manag. 2015;4(10):637–640. doi: 10.15171/ijhpm.2015.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neuman M, Alcock G, Azad K, Kuddus A, Osrin D, Shah More S, et al. Prevalence and determinants of caesarean section in private and public health facilities in underserved South Asian communities: cross-sectional analysis of data from Bangladesh, India and Nepal. BMJ Open. 2014;4(12):e005982. doi: 10.1136/bmjopen-2014-005982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zgheib SM, Kacim M, Kostev K. Prevalence of and risk factors associated with cesarean section in Lebanon—a retrospective study based on a sample of 29,270 women. Women Birth. 2017;30(6):e265–e271. doi: 10.1016/j.wombi.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization Appropriate technology for birth. Lancet. 1985;2(8452):436–437. [PubMed] [Google Scholar]
- 8.Azami-Aghdash S, Ghojazadeh M, Dehdilani N, Mohammadi M. Prevalence and causes of cesarean section in Iran: systematic review and meta-analysis. Iran J Public Health. 2014;43(5):545–555. [PMC free article] [PubMed] [Google Scholar]
- 9.Souza J, Gülmezoglu A, Lumbiganon P, Laopaiboon M, Carroli G, Fawole B, et al. Caesarean section without medical indications is associated with an increased risk of adverse short-term maternal outcomes: the 2004–2008 WHO Global Survey on Maternal and Perinatal Health. BMC Med. 2010;8:71. doi: 10.1186/1741-7015-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kyu HH, Shannon HS, Georgiades K, Boyle MH. Caesarian delivery and neonatal mortality rates in 46 low- and middle-income countries: a propensity score matching and meta-analysis of demographic health survey data. Int J Epidemiol. 2013;42(3):781–791. doi: 10.1093/ije/dyt081. [DOI] [PubMed] [Google Scholar]
- 11.Shahshahan Z, Heshmati B, Akbari M, Sabet F. Caesarean section in Iran. Lancet. 2016;388(10039):29–30. doi: 10.1016/S0140-6736(16)30899-6. [DOI] [PubMed] [Google Scholar]
- 12.Gholami A, Rezaof M, Shakeri M, Gazerani A, Khojastehpour M. Cesarean preference rate and factors associated with it among pregnant women with previous vaginal delivery in Neyshabur, Iran. J Rafsanjan Univ Med Sci. 2013;12(6):437–446. [Google Scholar]
- 13.Yazdizadeh B, Nedjat S, Mohammad K, Rashidian A, Changizi N, Majdzadeh R. Cesarean section rate in Iran, multidimensional approaches for behavioral change of providers: a qualitative study. BMC Health Serv Res. 2011;11:159. doi: 10.1186/1472-6963-11-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Metaanalysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 15.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zarei E, Majidi S, Bay V. Achievement of health sector evolution objectives in the vaginal delivery promotion plan: a study in a large public hospital in Tehran. J Health Field. 2015;3(2):2–32. [Google Scholar]
- 17.Piroozi B, Moradi G, Esmail Nasab N, Ghasri H, Farshadi S, Farhadifar F. Evaluating the effect of health sector evolution plan on cesarean rate and the average costs paid by mothers: a case study in Kurdistan province between 2013–2015. Hayat. 2016;22(3):245–254. [Google Scholar]
- 18.Seidali A, Namazi N. Assessment of changes in cesarean indications before and after the implementation of health sector evolution plan in pregnant women referred to Nezam-Mafi hospital, Shoush, Khoozestan province in 2013–2014. Pejouhandeh. 2016;20(6):315–319. [Google Scholar]
- 19.Rooeintan F, Borzabad PA, Yazdanpanah A. The impact of healthcare reform plan on the rate of vaginal delivery and cesarean section in Shiraz (Iran) in 2015. Electron Phys. 2016;8(10):3076–3080. doi: 10.19082/3076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dehghan A, Mirjalily MR, Zare Mehrjardi MH, Raghebian M, Samiyezargar A, Kazemeini SK. Epidemiology of caesarean sections performed in academic and nonacademic hospitals in Yazd between 2013 and 2014. J Shahid Sadoughi Univ Med Sci. 2017;24(10):810–817. [Google Scholar]
- 21.Fouladi Z, Shoarbafchi Zadeh N, Shaikhvaisi Y, Alimoradnuri M, Bagheri F. The effect of healthcare reform plan to reduce the rate of cesarean in hospitals affiliated to Qom University of Medical Sciences. Mil Caring Sci. 2017;4(3):207–212. [Google Scholar]
- 22.Zaboli R, Malmoon Z, Soltanizerandi M. The rate of normal vaginal delivery and cesarean section in two six month periods before and after the health reform project in hospitals affiliated to Kerman University of Medical Sciences. J Health Dev. 2017;6(3):182–190. [Google Scholar]
- 23.Zandian H, Tourani S, Moradi F, Zahirian Moghadam T. Effect of health sector evolution plan on the prevalence and costs of caesarean section and natural childbirth. Payesh. 2017;16(4):411–419. [Google Scholar]
- 24.Karami Matin B, Hajizadeh M, Najafi F, Homaie Rad E, Piroozi B, Rezaei S. The impact of health sector evolution plan on hospitalization and cesarean section rates in Iran: an interrupted time series analysis. Int J Qual Health Care. 2018;30(1):75–79. doi: 10.1093/intqhc/mzx169. [DOI] [PubMed] [Google Scholar]
- 25.Rezaie M, Dakhesh S, Fazli H. Comparison of frequency of cesarean section and its causes before and after implementation of the health system reform plan in Jahrom, Iran. JJUMS. 2018;15(4):43–50. [Google Scholar]
- 26.Yusefi AR, Bastani P, Bordbar S, Sadeghi A, Hesami SZ. The effects of health transformation plan implementation on the performance indicators of public hospitals. Health Scope. 2018;7(S):e62566. doi: 10.5812/jhealthscope.62566. [DOI] [Google Scholar]
- 27.Jabbari A, Yarmohamadian MH, Hadian M. Iran’s struggling health system: an increase in natural childbirth: a case study. Int J Prev Med. 2018;9:47. doi: 10.4103/ijpvm.IJPVM_82_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mumtaz S, Bahk J, Khang Y-H. Rising trends and inequalities in cesarean section rates in Pakistan: evidence from Pakistan Demographic and Health Surveys, 1990–2013. PLoS ONE. 2017;12(10):e0186563. doi: 10.1371/journal.pone.0186563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Betrán AP, Ye J, Moller A-B, Zhang J, Gülmezoglu AM, Torloni MR. The increasing trend in caesarean section rates: global, regional and national estimates: 1990–2014. PLoS ONE. 2016;11(2):e0148343. doi: 10.1371/journal.pone.0148343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gregory KD, Jackson S, Korst L, Fridman M. Cesarean versus vaginal delivery: whose risks? Whose benefits? Am J Perinatol. 2012;29(1):7–18. doi: 10.1055/s-0031-1285829. [DOI] [PubMed] [Google Scholar]
- 31.Timor-Tritsch IE, Monteagudo A. Unforeseen consequences of the increasing rate of cesarean deliveries: early placenta accreta and cesarean scar pregnancy. A review. Am J Obstet Gynecol. 2012;207(1):14–29. doi: 10.1016/j.ajog.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 32.Garvey M. The national birth center study II: research confirms low cesarean rates and health care costs at birth centers. Midwifery Today Int Midwife. 2013;106:40–68. [PubMed] [Google Scholar]
- 33.Moradi Gh, Farhadifar F, Piroozi B, Mohamadi Bolbanabad A. An assessment of promoting natural childbirth package in health reform plan from the opinion of stakeholders in Hospitals of Kurdistan University of Medical Science, 2015. Hakim Health Sys Res. 2016;19(2):103–110. [Google Scholar]
- 34.Simbar M, Ghafari F, Zahrani ST, Majd HA. Assessment of quality of midwifery care in labour and delivery wards of selected Kordestan Medical Science University hospitals. Int J Health Care Qual Assur. 2009;22(3):266–277. doi: 10.1108/09526860910953539. [DOI] [PubMed] [Google Scholar]
- 35.Firoozi M, Hadizadeh Talasaz F. The Survey of attitude of gynecologists and midwives about vaginal birth after caesarean delivery and barriers from their views. Ofogh-e-Danesh. 2006;12(2):26–33. [Google Scholar]
- 36.Farazmand T, Fakhr-e-Fatemi Z, Asadi RAS, Lashkardoost H. Factors associated with cesarean delivery compared to normal procedure. JNKUMS. 2015;6(4):851–860. doi: 10.29252/jnkums.6.4.851. [DOI] [Google Scholar]
- 37.Arrieta A. Health reform and cesarean sections in the private sector: the experience of Peru. Health Policy. 2011;99(2):124–130. doi: 10.1016/j.healthpol.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 38.Triunfo P, Rossi M. The effect of physicians’ remuneration system on the caesarean section rate: the Uruguayan case. Int J Health Care Finance Econ. 2009;9(4):333–345. doi: 10.1007/s10754-008-9054-y. [DOI] [PubMed] [Google Scholar]
- 39.Hoxha I, Syrogiannouli L, Luta X, Tal K, Goodman DC, da Costa BR, et al. Caesarean sections and for-profit status of hospitals: systematic review and meta-analysis. BMJ Open. 2017;7(2):e013670. doi: 10.1136/bmjopen-2016-013670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Knight M, Sullivan EA. Variation in caesarean delivery rates. BMJ. 2010;341:c5255. doi: 10.1136/bmj.c5255. [DOI] [PubMed] [Google Scholar]
- 41.Mossialos E, Allin S, Karras K, Davaki K. An investigation of Caesarean sections in three Greek hospitals: the impact of financial incentives and convenience. Eur J Public Health. 2005;15(3):288–295. doi: 10.1093/eurpub/cki002. [DOI] [PubMed] [Google Scholar]
- 42.Hoxha I, Syrogiannouli L, Braha M, Goodman DC, da Costa BR, Jüni P. Caesarean sections and private insurance: systematic review and meta-analysis. BMJ Open. 2017;7(8):e016600. doi: 10.1136/bmjopen-2017-016600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McDonnell A, Wilson R, Goodacre S. Evaluating and implementing new services. BMJ. 2006;332(7533):109–112. doi: 10.1136/bmj.332.7533.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data (primary literature) is publicly available.