Abstract
Background:
Segmental mandibulectomy impairs health-related quality of life(QoL), by altering speech, mastication, swallowing, and facial esthetics. Fibula free-flap(FFF), used for mandible reconstruction is known to improve outcomes; however, minimal information exists in the literature regarding patient-reported outcomes (PRO). We aim to assess how current studies evaluate patient perception following segmental mandibulectomy and FFF mandible reconstruction.
Methods:
Following PRISMA guidelines, a search was conducted for publications involving FFF mandible reconstruction between 2005–2017 using PubMed, Cochrane, EMBASE, Web of Science, and PsychInfo.
Results:
Of 2,212 articles identified initially, only seven studies were deemed suitable. Six studies used UWQoL questionnaire; three OHIP, and one used EORTC-H&N35.
Conclusions:
There is a paucity of information in published reports on QoL outcomes following mandible reconstruction with FFF. In the era of patient-centered healthcare, observations warrant attention from researchers for physician-assessed patient-reported measures to factor in QoL expectation during surgical decision-making about the choice of reconstruction.
INTRODUCTION
Segmental mandibulectomy, often employed for resection of a tumor, and occasionally for trauma, osteoradionecrosis, osteomyelitis, or congenital abnormalities, adversely affects patient’s quality of life (QoL) to a varying degree.(1) It inflicts a significant defect in the head and neck region, impacting on facial appearance, and the functions of speech, mal occlusion, mastication, swallowing and health-related QoL. Mandible resection thus creates a significant impact on a patient`s life, both esthetically as well as functionally.
Restoration of the defects following resection of any part of the mandible presents a challenging problem for the reconstructive surgeons. Since the introduction of fibula free flap (FFF), by Taylor in 1975, it has become the most popular choice for mandible reconstruction. (2) Hidalgo popularized the FFF, since 1989 and reported on its versatility with satisfactory outcomes. (3) (4, 5) The utility and techniques of free flap mandible reconstruction have advanced in the past two decades (6) with success rate up from 82.6–100%. As the longest bone segment available for reconstructive purpose, FFF is known for its wide variety of applications, following mandible resection, including, angle-to-angle reconstruction. Additionally, it offers a desirable range of width and to some extent height for placement of osseointegrated implants (7). While the survival of the flap has been achieved in nearly all patients, reports in the literature mostly deal with esthetic restoration of facial contour, but are lacking on functional outcomes and particularly patient reported outcomes on satisfaction with functional restoration. Thus, there has not been much progress noted in the utilization and documentation of patient-reported outcomes (PROs) in patients with FFF reconstruction after segmental mandibulectomy.
Despite a good structural and esthetic outcome achieved following reconstruction, minimal information is available regarding QoL of patients undergoing FFF reconstruction following segmental mandibulectomy. In an era when patient autonomy plays a crucial role in healthcare along with the expanding awareness of self-directed care(8), outcomes beyond survival are equally important metrics of health service research. Moreover, postoperative health-related QoL is reported to be associated with the anatomical location of the surgical resection(9). Given this knowledge, a better understanding of the QoL and changes associated with FFF mandible reconstruction is needed to help patients make informed decisions about their surgical options.
Although many generic QoL measurements have been developed over the past 30 years, there is no questionnaire that has clearly been identified as a gold standard. The tool measuring health-related QoL must be clinically relevant and scientifically robust. Patient questionnaires, if not formally developed, tested and validated, may lack reliability quotient. The goal of this review is to assess how current studies are established to evaluate patient perception via validated instruments measuring functional and aesthetic outcomes following segmental mandibulectomy and reconstruction with FFF.
MATERIAL AND METHODS
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for this review(10).
Search strategy
A comprehensive online literature search of published studies was initiated in Jun 19, 2015 and updated until April 4, 2017, in all languages using the electronic data base of PubMed, Cochrane via Wiley, EMBASE provided by Elsevier, Web of Science with Thomson Reuters and PsychInfo on the OVID platform for the years 2005–2017. Additional filters included: clinical trial, meta-analysis, multicenter study, observational study, randomized controlled trial, controlled clinical trial, systematic reviews, twin study, and validation studies. Relevant search terms for the patient reported outcomes (PROs), fibula free flap reconstruction following segmental mandibulectomy in oncologic patients were used (Table 1.) Grey literature was also searched and results on meeting abstracts were generated on BIOSIS, another database provided by Thomson Reuters. Three broad concept categories were searched, and results were combined using the appropriate Boolean operators (AND, OR). The broad categories included: mandible reconstruction, patient reported outcomes and validated assessment tools. Related terms were also incorporated into the search strategy to ensure all relevant papers were retrieved (Table 1). To find relevant articles not detected in the electronic bibliographic search, a follow-up review of references was performed. After an examination of titles and abstracts, we examined reference lists, tables and texts in the pertinent articles to find all patient-reported outcome questionnaires evaluating QoL among patients who had mandibulectomy followed by primary reconstruction using fibula free flap.
Table 1.
Search Strategies and Keywords Used
| Medical Subject Headings (MeSH) | Keyword terms |
|---|---|
| (Mandibular Reconstruction[Mesh] OR Mandibular Osteotomy[Mesh] OR Mandibular Neoplasms[Mesh] OR Mandibular Neoplasms[Mesh] OR Mandibular Neoplasms[Mesh] OR Mandibular Diseases[Mesh] OR Mouth Neoplasms[Mesh] OR Surgery, Oral[Mesh] OR Surgical Flaps[Mesh]) AND (“Outcome Assessment (Health Care)”[Mesh] OR Quality of Life[Mesh] OR Quality-Adjusted Life Years[Mesh] OR “Health Status”[Mesh] OR “Personal Satisfaction”[Mesh] OR Patient Satisfaction[Mesh] OR Patient Compliance”[Mesh] OR “Patient Preference[Mesh] OR Attitude[Mesh] OR Pain[Mesh] OR “Body Image”[Mesh] OR Social Adjustment[Mesh] OR Social Behavior[Mesh] OR Shyness[Mesh] OR Social Distance[Mesh] OR Social Isolation[Mesh] OR Fear[Mesh] OR Frustration[Mesh] OR Personal Autonomy[Mesh] OR Self Concept[Mesh] OR Social Adjustment[Mesh] OR Adaptation, Psychological[Mesh] OR Stress, Psychological[Mesh] OR Emotions[Mesh] OR Esthetics[Mesh]) AND (“Questionnaires”[Mesh] OR Interviews as Topic[Mesh] OR Observation[Mesh]) | (“mandibular neoplasms” OR “mandibular cancer” OR “mandibular carcinoma” OR “mandibular tumor” OR “mandibular tumour” OR “mandible malignancies” OR “mandible malignancy” OR “oral cancer” OR “oral carcinoma” OR “oral neoplasm” OR “oral tumor” OR “oral tumour” OR “oral malignancies” OR “oral malignancy” OR “mandibular reconstruction” OR mandibulectomy OR “mandibular resection” OR “maxillofacial surgery” OR “fibular flap reconstruction” OR “surgical flap” OR “free fibula flap”) AND (“outcome assessment” OR “quality of life” OR QOL OR “Health related quality of life” OR HRQOL OR “quality adjusted life years” OR QALY OR “health status” OR “functional status” OR “functional outcome” OR “well-being” OR “personal satisfaction” OR “patient satisfaction” OR “patient compliance” OR preference OR attitude OR perspective OR “patient reported outcome” OR pain OR disability OR disabilities OR disabled OR “body image” OR “social function” OR “social behavior” OR “social behaviour” OR shyness OR “social distance” OR “social isolation” OR fear OR frustration OR autonomy OR “self-concept” OR adaptation OR adjustment OR coping OR stress OR emotion OR aesthetic OR esthetics OR appearance) AND questionnaires OR survey OR assessment OR instrument OR validated tool OR interview OR observation OR evaluation OR measure OR feedback OR scales) |
Selection Process
Results of the search were imported into EndNote database. Publications were screened for inclusion in three phases. In the first phase, two authors independently reviewed titles and abstracts for duplicates and poor fit with focus on systematic review. If at least one author coded the title to continue in the next round, three authors then independently reviewed the full text of the article and classified the articles based on the eligibility criteria. The selected full text of the article was recommended for full data extraction. Discrepancies were discussed at the full text review stage until a consensus was reached.
Selection criteria
All instruments cited in the articles were assessed for evidence with respect to their development or validation criteria. Papers with questionnaires not developed and/or validated in an oncologic head and neck surgery patient population were excluded. The inclusion criteria accepted all publications from a retrospective study, prospective study, longitudinal study, systematic review, meta-analysis, studies with populations that include patients that had only segmental or hemi mandibulectomy performed with primary FFF reconstruction, studies that report on patient’s perception of outcomes by validated questionnaires, and articles in English language (Table 2). Exclusion criteria were: case reports, studies with patients without mandibulectomy and FFF reconstruction, studies that report patient’s perception of outcomes by not validated questionnaires, article not on English (Table 2). Two reviewers independently reviewed all article (IP, PDD). All potentially relevant abstracts were examined in detail. Disagreements were resolved by consensus with the lead author (JS) acting as a mediator.
Table 2.
Study Selection criteria
Inclusion criteria:
|
Exclusion Criteria:
|
Data extraction
Three authors independently extracted data from all eligible studies and discrepancies were reconciled as necessary (IP, PDD, JS). Data was collected and summarized regarding study characteristics, patient characteristics, information of the treatment modality (segmental mandibulectomy reconstructed with FFF), and outcome measures regarding functional outcomes and quality of life (speech, swallowing, chewing, taste, saliva, esthetic outcome, activity, pain, mood).
Institutional review board exempted the study protocol.
RESULTS
Summary of the selected articles and patient population
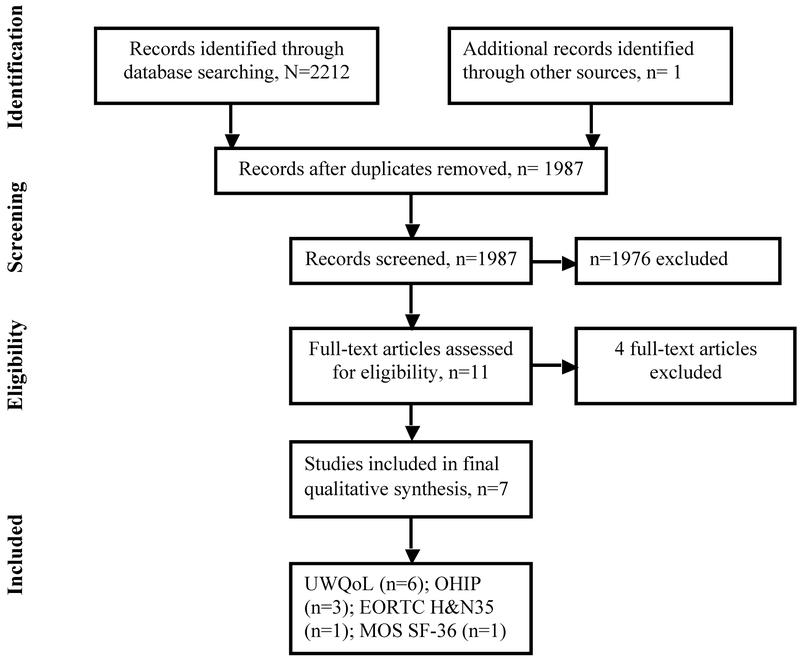
Of the total of 2212 articles identified initially by the search engines and reviewed by two individual investigators, only 11 studies had used validated PRO instruments. Of total eligible studies, eight unique studies satisfied our selection criteria (Figure 1). One of the eight articles was excluded from the study due to missing tables, which we were unable to obtain from the authors.(6)
Figure 1:
Flow diagram demonstrating search strategy and selection process
A total of seven were finally selected for the review. All seven studies were retrospective case series(5, 11–14). In all reviewed papers, total 245 patients were described who underwent segmental resection of the mandible followed by FFF reconstruction and whose quality of life functions were assessed by a validated tool. Among all, the median response rate of patients who returned the QoL questionnaire was 73.8% with a range of 65.0 to 100% (Table 3). A total of 194 patients (127 male and 67 female) answered the QoL assessment questionnaire that was given to them prospectively, on the day of follow-up or by phone (Table 3). Indications for mandible resection included, oral squamous cell carcinoma, adenoid cystic carcinoma, ameloblastoma and osteoradionecrosis. The number of patients per study ranged from 14 to 35 (median=32) and their age ranged from 10–75 years (weighted mean, 19 years). From the total articles reviewed, 4 validated questionnaires were used including University of Washington Quality of Life (UWQoL), Oral Health Impact Profile (OHIP), European Organization for Research and Treatment of Cancer Quality of life Questionnaire Head and Neck (EORTC QLQ-H&N 35), and Medical Outcomes Study Short Form 36 (MOS SF-36).
Table 3:
Patient characteristics
| Study | Total | Total | Sex | Age, years | Diagnosis | Follow-up, months |
|---|---|---|---|---|---|---|
| Ni | Nr | M/F | Med (Min–Max) |
Mean/med (Min-Max) |
||
| Wang, L. et al, 2009 | 15 | 15 | 8/7 | 48 (34–62) | ORN | 28 (6–60) |
| Zhang, X. et al, 2013 | 42 | 31 | 18/13 | 58 (31–75) | Malignancy | 44 (12–72) |
| Li, X. et al, 2014 | 54 | 35 | 23/12 | 17 (10–24) | AB | -- (12–32) |
| Luo, R. et al, 2014 | 47 | 32 | 23/9 | 21 (10–30) | AB | -- (16–123) |
| Yang, W. et al, 2014 | 34 | 34 | 25/9 | 53 (28–65) | SCC | 27 (12–48) |
| Zhu, J. et al, 2014 | 45 | 33 | 24/9 | 43 (26–58) | AB | 23 (14–60) |
| Hundepool et al. 2008 | 18 | 14 | 6/8 | 58(19–77) | Mixed* | 39(6–89) |
| Total | 245 | 194 | 127/67 | 48 (10–77) | --(6–123) |
Ni Number of patients invited to participate in the study; Nr Number of patients who responded the questionnaires, ORN osteoradionecrosis, AB Ameloblastoma, SCC Squamous cell carcinoma, * 8SCC, 3AB, 3ORN, 1 adenoid cystic carcinoma
8SCC, 3AB, 3ORN, 1 adenoid cystic carcinoma
University of Washington Quality of Life (UWQoL)(15)
From the total selected studies, six studies used UWQoL. Results from these studies were reviewed and summarized (Table 4).(5, 11–14, 16) All studies included UWQoL questionnaire containing 15 domains, 12 of which are disease specific including pain, appearance, activity, recreation, swallowing, chewing, speech, shoulder function, taste, saliva, mood and anxiety, and 3 are global questions. The domains are scored on a scale ranging from 0 (worst) to 100 (best). Summary of the UWQoL responses is displayed in Table 4.
Table 4:
Functional outcomes assessment using UWQoL, n=6
| Study | Pain | Shoulder | Activity | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | GS (%) | Imp (%) | RO | Mean SD) | GS (%) | Imp (%) | RO | Mean (SD) | GS (%) | Imp (%) | RO | |
| Wang L. et al. 2009 | 86.7 (16.0) | 53 | 7 | 6 | 82.0 (15.2) | 40 | 0 | 8 | 76.7 (22.1) | 40 | 0 | 8 |
| Zhang X. et al. 2013 | 87.6 (10.2) | -- | 7 | 8 | 92.5 (3.1) | --- | 3 | 9 | 72.4 (8.5) | -- | 0 | 11 |
| Li X. et al. 2014 | 82.2 (5.8) | 43 | 0 | 11 | 80.3 (9.0) | 40 | 0 | 11 | 69.5 (7.6) | 9 | 17 | 7 |
| Luo R. et al. 2014 | 80.6 (7.5) | 44 | 0 | 8 | 82.3 (3.1) | 44 | 0 | 8 | 66.2 (9.1) | 6 | 38 | 4 |
| Yang W. et al. 2014 | 67.4 (7.5) | -- | 6 | 9 | 65.9 (7.1) | --- | 0 | 10 | 56.5 (9.1) | -- | 41 | 4 |
| Zhu J. et al. 2014 | 76.4 (6.5) | 42 | 0 | 9 | 81.1 (5.5) | 46 | 0 | 9 | 64.1 (8.3) | 6 | 58 | 3 |
| Speech | Chewing | Swallowing | ||||||||||
| Wang L. et al. 2009 | 53.3 (34.1) | 20 | 46 | 3 | 36.7 (22.8) | 0 | 53 | 2 | 48.7 (26.9) | 7 | 93 | 1 |
| Zhang X. et al. 2013 | 47.9 (1.2) | -- | 68 | 2 | 42.2 (2.6) | -- | 90 | 1 | 83.7(1.6) | -- | 13 | 7 |
| Li X. et al. 2014 | 71.3 (12.6) | 23 | 54 | 2 | 28.5 (3.2) | 0 | 77 | 1 | 77.3 (6.8) | 29 | 6 | 10 |
| Luo R. et al. 2014 | 66.4 (7.8) | 3 | 25 | 5 | 30.3 (2.7) | 0 | 94 | 1 | 78.1 (5.1) | 28 | 3 | 7 |
| Yang W. et al. 2014 | 55.3 (10.3) | -- | 53 | 2 | 33.1 (16.1) | -- | 71 | 1 | 52.8 (9.1) | -- | 47 | 3 |
| Zhu J. et al. 2014 | 68.8 (9.9) | 15 | 30 | 4 | 32.4 (1.8) | 0 | 76 | 1 | 79.9 (7.2) | 49 | 0 | 9 |
| Saliva | Taste | Appearance | ||||||||||
| Wang L. et al. 2009 | 58.7 (28.2) | 13 | 40 | 4 | 80.7 (24.9) | 53 | 0 | - | 66.7 (29.4) | 20 | 20 | 5 |
| Zhang X. et al. 2013 | 70.8 (1.6) | -- | 26 | 4 | 90.3 (1.8) | -- | 3 | 9 | 58.5 (2.1) | -- | 55 | 3 |
| Li X. et al. 2014 | 60.0 (7.6) | 42 | 23 | 5 | 71.2 (8.8) | 26 | 11 | 9 | 78.1(11.6) | 26 | 49 | 3 |
| Luo R. et al. 2014 | 74.09 (8.0) | 22 | 0 | 8 | 78.7 (7.5) | 40 | 3 | 7 | 76.3 (8.7) | 31 | 50 | 3 |
| Yang W. et al. 2014 | 47.83 (8.9) | -- | 24 | 6 | 55.6 (6.0) | -- | 29 | 5 | 70.1 (6.6) | -- | 18 | 7 |
| Zhu J. et al. 2014 | 75.0 (9.7) | 42 | 12 | 8 | 80.5 (5.5) | 33 | 0 | 9 | 74.6 (9.6) | 36 | 67 | 2 |
| Mood | Anxiety | Recreation | ||||||||||
| Wang L. et al. 2009 | 71.7 (31.1) | 40 | 0 | 8 | 64.7 (66.7) | 40 | 7 | 6 | 65 (33.8) | 33 | 0 | 8 |
| Zhang X. et al. 2013 | 85.3 (7.9) | -- | 16 | 6 | 69.8 (6.3) | -- | 19 | 5 | 75.91 (6.1) | -- | 0 | 11 |
| Li X. et al. 2014 | 67.1 (1.2) | 11 | 20 | 6 | 55.8 (8.2) | 0 | 29 | 4 | 68.2 (10.6) | 0 | 14 | 8 |
| Luo R. et al. 2014 | 60.1 (3.0) | 3 | 13 | 6 | 45.3 (9.6) | 0 | 63 | 2 | 69.39 (7.1) | 6 | 13 | 6 |
| Yang W. et al. 2014 | 73.4(11.5) | -- | 0 | 10 | 50.8(14.3) | -- | 12 | 8 | 60.09 (9.1) | -- | 0 | 10 |
| Zhu J. et al. 2014 | 67.1 (1.2) | 9 | 18 | 6 | 65.2 (8.6) | 0 | 24 | 5 | 65.6 (8.7) | 3 | 15 | 7 |
UWQoL, University of Washington Quality of Life; GS, Good score; Imp, importance of the domains; RO, Rank Order of the domain;
Averaging respective mean domain scores of all 6 studies, pain (80.2) and shoulder function (80.7) scored the highest, followed by taste (76.2), mood (70.8), swallowing (70.1), activity (67.6), recreation (67.4), saliva (64.4), speech (60.5), Anxiety (58.6), and chewing (33.9). Among all patients assessed using UWQoL, 77% indicated chewing as an important domain, 46% speech, 27% swallowing, and 26% indicated activity as important functions. 11–21% reported mood and saliva as important functions; whereas, less than 10% of the cohort considered taste, recreation, pain and shoulder function of importance (Table 4).
Chewing scored the lowest with mean score ranging from 30–42, and ranked first as the most important function in all but one study (Table-4). Speech, which scored 53–71, ranked from second to fifth in the order of importance. Swallowing function, which scored 49–84, had the highest variability with importance rank ranging from first to tenth. Mood (score: 60–85) and recreation (score: 65–76) were the least important functions ranking from 6–10 and 6–11, respectively.
Oral Health Impact Profile (OHIP)
Three studies had used OHIP as an outcome measure(5, 13, 14). The OHIP provides a comprehensive measure of dysfunction, discomfort, and disability attributed to oral conditions. OHIP-14 consists of 14 items and OHIP-49 consists of 49 items organized into 7 domains: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap. Each item is scored as 0: never, 1: hardly ever, 2: sometimes, 3: fairly often, and 4: very often. The domains are scored in a scale ranging from 0 (best) to 100 (worst). Higher score inversely correlates to the patient´s state of health.
Summary of the OHIP scores reported by three studies is displayed in Table 5. The best domain mean scores for the three studies that used OHIP were 35.7 for handicap, followed by social disability (38.3), psychological disability (48.9), and physical pain (51.0). The worst scores were reported for physical disability (72.4) and functional limitations (54.5) (13).
Table 5.
Summary of OHIP questionnaire scores
| STUDY | Luo, R. et al. 2014** | Yang, W. et al. 2014* | Zhu J. et al. 2014* | ||
|---|---|---|---|---|---|
| OHIP Domain | Mean (SD) | %<20 | Mean | Mean (SD) | % ≤40 |
| Physical disability | 76.1(3.4) | 0 | 70.12 (8.22) | 71.1(9.5) | 0 |
| Physical pain | 35.4(3.4) | 22 | 63.31 (3.85) | 54.2(1.9) | 18 |
| Functional limitations | 56.2(5.8) | 9 | 55.14 (2.43) | 52.1 (1.7) | 12 |
| Psychological discomfort | 44.4(1.8) | 0 | 51.35 (1.55) | 46.3(1.2) | 21 |
| Psychological disability | 52.1(6.7) | 3 | 45.27 (1.54) | 48.9(2.0) | 46 |
| Handicap | 36.4(2.9) | 25 | 36.33 (1.08) | 34.3(1.2) | 63 |
| Social disability | 38.8(1.9) | 19 | 35.32 (2.19) | 40.8(1.3) | 49 |
OHIP Oral Health Impact Profile, OHIP score ranges from 0(best) to 100 (worst).
OHIP-14,
OHIP-49;
percentage of patients who scored 40 or lower;
Good score percentages indicates percentage of patients who scored below 20.
European Organization for Research and Treatment of Cancer Quality of life Questionnaire Head and Neck (EORTC QLQ-H&N 35)
Only one study reported scores of EORTC H&N35.(7) Head and Neck Module of the European Organization for Research and Treatment of Cancer is a Quality of Life Head and Neck cancer-specific quality of life questionnaire. EORTC QLQ-H&N 35 incorporates different scales aimed to assess symptoms and side effects of treatment such as trouble with eating, social function, and body images/sexuality, and is specifically designed for patients undergoing surgery, chemotherapy, and radiotherapy. EORTC- H&N 35 module contains items exploring side effects and symptoms of treatment on a scale of 0–100 with higher score representing worse outcomes. Hundepool et al. reported EORTC H&N35 scores of 14 patients who responded to the questionnaire containing 12 domains described in Table 6. The authors also used this tool to compare pre- and post-implant status. While these scores varied across the domains, over time after dental rehabilitation, the scores remained equivalent, except for social function, which improved significantly after dental rehabilitation (61 vs. 25, p <0.001; Table 6).
Table 6:
Functional assessment and quality of life using EORTC H&N35 Questionnaire
| EORTC H&N 35 | Hundepool et al. 2013 | |
|---|---|---|
| Domains | Pre- Ti | Post-Ti |
| Soreness mouth | 52 | 48 |
| Swallowing | 53 | 37 |
| Swallowing liquids | 31 | 29 |
| Swallowing pureed food | 21 | 20 |
| Swallowing solid food | 55 | 48 |
| Opening mouth | 49 | 45 |
| Dry mouth | 84 | 75 |
| Senses of taste | 44 | 43 |
| Social* | 61 | 25 |
| Talking | 61 | 49 |
| Chewing | 62 | 59 |
| Nutritional supplements/feeding tube | 32 | 32 |
P <0.001 (Wilcoxon matched-pairs signed rank test). Pre-Ti, before dental rehabilitation, Post-Ti, after dental rehabilitation; H&N35 scales ranges from 0–100 with 100 implying maximum impairment in the function of interest.
Medical Outcomes Study Short Form 36 (MOS SF-36)
The distributions of MOS SF-36 domain scores are shown in Table 7. Only one study, Zhang et al., used this tool and reported the outcomes. (11) The score ranges from 0–100, with 100 being the best score. Physical role was the best scoring domain followed by bodily pain, physical functioning, emotion, mental health, social functioning. Domains including vitality and general health scored the least suggesting worse outcome (Table 7).
Table 7:
Means of scores of items and scales of SF-36 questionnaire
| Domains | Zhang X. et al. 2013 | |
|---|---|---|
| Mean (SD) | (Min-Max) | |
| Physical functioning | 87.3 (6.6) | 64–98 |
| Bodily pain | 90.0 (4.7) | 69–100 |
| General health | 66.2 (9.1) | 30–90 |
| Social functioning | 68.4 (4.1) | 44–89 |
| Role emotion | 73.0 (3.1) | 40–100 |
| Physical role | 92.8 (2.5) | 75–100 |
| Vitality | 61.3 (8.3) | 44–85 |
| Mental health | 72.2 (6.2) | 55–90 |
DISCUSSION
This systematic review revealed that there is a limited number of studies (10/1987, 0.5%; Figure 1) in the English language medical literature spanning over twelve years (2005–2017) that used one or more validated PRO tools assessing quality of life or functional outcomes following mandibulectomy and FFF reconstruction. All of these studies were retrospective cohorts or case series in nature. The data from this review highlight the lack of functional assessment and patient reported outcomes measurement in this patient population with head and neck lesions requiring segmental mandibulectomy and FFF reconstruction. Defects in the mandible following resection cause facial asymmetry, and disharmony, as well as mal occlusion and tooth loss compromising chewing and lip support. In addition, mandible also plays a major role in airway protection and support of the tongue, lower dentition, and the muscles of the floor of the mouth permitting mastication, articulation, deglutition, and respiration(17). Due to the loss of these functions as well as the increasing interest in outcomes research, the need for a region- and disease-specific validated patient-reported outcome tool is imperative. This review reveals a dearth in the utilization of patient reported outcomes for patients undergoing head and neck reconstruction following ablative surgery, and suggests that the need to expand on the PRO remains unmet in the field of head and neck reconstructive surgery. On the other hand, our findings may suggest barriers to utilization of PRO such as absence of awareness, increasing cost, patient compliance, and unavailability of treatment- or region-specific tool.
We found that the University of Washington (Seattle, WA) head and neck region specific QoL questionnaire was the most commonly used outcome tool in the studies in this review, including PROs. The original of UWQoL was developed in 1993, which has been modified multiple times(15). The current version UWQoL version 4 contains 12 QoL domains assessing pain, appearance, activity, recreation, swallowing, chewing, speech, shoulder, taste, saliva, mood, and anxiety in head and neck cancer patients. There are several advantages of this instrument such as simple and easy-to-use, validated head and neck disease-specific health-related QoL tool. UWQoL has been used and reported in the literature for patients with head and neck cancer, requiring tumor resection, and quality of life after surgery, reconstruction after maxillectomy or other flap types such as radial forearm free flap and anterolateral thigh flap used for reconstruction in the oral cavity (18–22). It has also been translated and or used in other languages including Chinese, Greek, Turkish, and German for head and neck cancer therapy albeit its use in the setting of reconstruction remains uncommon to date (23–25) However, as we found in this review, its use has not been popular in studies of patients with mandible reconstruction. Individual domain analysis within UWQoL as well as incremental assessment is claimed to provide an accurate picture of the complex functional changes associated with head and neck cancer therapy. However, this questionnaire has its own limitations such as composite QoL score, i.e. sum of the domain scores is subject to internal cancellation effect, which renders it less sensitive to overall changes when comparing treatment options. Furthermore, retrospective data collection and single center studies may not find enough information about the outcome.
Defects of head and neck region affect individuals at a personal level due to its association with appearance, personal presentation and confidence, and may lead to social isolation further deteriorating mental health. While UWQoL is specific to head and neck region, it does not cover aesthetic outcome as comprehensively as the FACE-Q, a validated PRO tool developed using international guidelines for PRO (26). It was initially developed to evaluate patients undergoing facial cosmetic operations, minimally invasive cosmetic procedures, or facial injectable and has been tested and validated in a multicenter study of over 700 patients (26). FACE-Q’s oncology module for mandibulectomy is currently under study Memorial Sloan Kettering Cancer Center, in New York. (ClinicalTrials.gov Identifier: NCT02572869). While the appearance scales ask questions about satisfaction with facial appearance, skin, lower face, jawline, chin, area under the chin, neck, and other aesthetic components of facial appearance; the mandibulectomy module also incorporates domains asking questions about salivation, taste and mastication, deglutition, speech, appearance of and sensations on the face, and oral functions. Integrating quality of life measures in the process of developing a surgical plan, in addition to post-operative complications may be a solution to challenges faced by patients treated for head and neck tumors.
The MOS SF-36 questionnaire on the other hand is not specific for head and neck region or reconstructive surgery. While generic questionnaires commonly assess health-related general wellbeing, they lack the dimensions and domains necessary to be evaluated in specific region or population such as the patients undergoing mandible resection and FFF reconstruction. Review of the responses to the SF-36 questionnaire revealed that the ‘vitality’ (61.3±8.3) and ‘general health’ (66.2±9.1) domains received significantly low scores from many patients worried about the movement of the operated limb(11). Mandibulectomy has been associated with depression by other authors(18). Most patients said that they were worried about their donor-site morbidity on the operated limb and experienced reduced vitality. The ‘physical role’ (92.8 ± 2.5) and ‘bodily pain’ (90.0 ± 4.7) components scored well. However, when using SF-36 tool, it is not possible to get an idea about specific quality measures pertaining to head and neck region such as swallowing, speech, and mastication. Despite lacking specificity SF-36 is widely used to evaluate generic patient-assessed health-outcome measure in those undergoing head-and-neck surgeries.
The oral health impact profile (OHIP), an oral-specific questionnaire, in contrast, is specific and better able to demonstrate the changes in quality of life due to oral dysfunction following surgery. In this review, the best domain mean scores for the three studies that used OHIP were for handicap, social disability and psychological disability, whereas the lowest scores were reported for physical disability and functional limitations(5, 13). These results provide evidence about the varying effect that oral cancer surgery has on oral health. Patients report that surgery has brought a lot of disability in their oral function. With chewing remaining the most important domain, assessing oral functions is critically important.
One study also used EORTC-H&N35 for functional assessment, which focuses on oral functions as well as social and talking abilities. (7) EORTC H&N35 is one of the most common questionnaires used to report quality of life for patients undergoing treatment for head and neck cancer. Other reported questionnaires are EORTC-C30, which asks questions about general health, whereas, specifics such as Functional Assessment of cancer Therapy-head & neck (FACT-HN), Head and Neck Quality of Life (HNQoL) are specifically designed for head and neck cancer.(27–30) Other function or symptom specific instruments commonly used for patients with head and neck cancer encompasses Swallowing Quality of Life questionnaire (SWAL-QoL), Performance Status Scale (PSS), MD Anderson Dysphagia Inventory (MDADI) specifically for swallowing and Voice Handicap Index (VHIP) for voice; and Speech Handicap Index (SHI) for speech functions.(31, 32) However, none of these are commonly employed to assess patient satisfaction after mandible reconstruction.
Utilization of a specific validated questionnaire in the QoL armamentarium and EORTC goals is pivotal as we expand the realm of reconstructive procedures for patients undergoing resection in head and neck region. Hundepool et al. also used a visual analog scale (VAS), which measures intensity and frequency of symptoms on a scale of 0–10. The authors reported mean scores of 2.2 for discomfort and treatment impact, 3.3 for aesthetic and denture satisfaction, 4.2 for oral functioning, 3.6 for overall satisfaction indicating below 50% improvement in patients’ QoL. (7) It must be noted though that VAS is not a validated scale. Zavalishina et al. observed no significant correlation between the aesthetic expectations for face and neck appearance by patients and their dental surgeons (r=0.033) based on the VAS, suggesting that an objective measure of outcome may be imperative.(6) Moreover, the authors also noticed some degree of inter- and intra-reader variability in the appearance assessment by dentists.
This review has several strengths, but is not without limitations. We did not include papers published in languages other than English. However, most of the studies we present in this review were conducted in China. We excluded papers that did use PRO, but we did not have enough information to summarize their data.
In conclusion, our systematic review uncovered a dearth in the utility of PRO tools in assessing functional and aesthetic outcomes in patients undergoing mandible resection and reconstruction. The UWQoL was the most commonly utilized tool followed by the OHIP. Recently developed validated questionnaires such as FACE-Q mandibulectomy module may be a reasonable solution to evaluate this group of patients. In the time when health service is centered on patients’ preferences and autonomy, using region specific quality of life tool that is psychometrically robust and validated becomes imperative.
Acknowledgement:
The study was supported, in part, by NIH/NCI Cancer Center Support Grant P30 CA008748
Abbreviations:
- UWQoL
University of Washington quality of life
- OHIP
Oral health impact profile
- FFF
Free fibula flap
- EORTC
European organization for research and treatment of cancer
- QLQ-H&N
35 Quality of life Questionnaire Head and Neck
Footnotes
Financial Disclosure: None
REFERENCES
- 1.Rana M, Warraich R, Kokemuller H, et al. Reconstruction of mandibular defects - clinical retrospective research over a 10-year period. Head Neck Oncol 2011;3:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor GI, Miller GD, Ham FJ. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast Reconstr Surg 1975;55(5):533–44. [DOI] [PubMed] [Google Scholar]
- 3.Zhu J, Xiao Y, Liu F, Wang J, Yang W, Xie W. Measures of health-related quality of life and socio-cultural aspects in young patients who after mandible primary reconstruction with free fibula flap. World J Surg Oncol 2013;11:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hidalgo DA. Fibula free flap: a new method of mandible reconstruction. Plast Reconstr Surg 1989;84(1):71–9. [PubMed] [Google Scholar]
- 5.Zhu J, Yang Y, Li W. Assessment of quality of life and sociocultural aspects in patients with ameloblastoma after immediate mandibular reconstruction with a fibular free flap. Br J Oral Maxillofac Surg 2014;52(2):163–7. [DOI] [PubMed] [Google Scholar]
- 6.Zavalishina L, Karra N, Zaid WS, El-Hakim M. Quality of life assessment in patients after mandibular resection and free fibula flap reconstruction. J Oral Maxillofac Surg 2014;72(8):1616–26. [DOI] [PubMed] [Google Scholar]
- 7.Hundepool AC, Dumans AG, Hofer SO, et al. Rehabilitation after mandibular reconstruction with fibula free-flap: clinical outcome and quality of life assessment. Int J Oral Maxillofac Surg 2008;37(11):1009–13. [DOI] [PubMed] [Google Scholar]
- 8.Liu JB, Pusic AL, Temple LK, Ko CY. Patient-reported outcomes in surgery: Listening to patients improves quality of care. Bull Am Coll Surg 2017;102(3):19–23. [PubMed] [Google Scholar]
- 9.Cohen WA, Albornoz CR, Cordeiro PG, et al. Health-Related Quality of Life following Reconstruction for Common Head and Neck Surgical Defects. Plast Reconstr Surg 2016;138(6):1312–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang X, Li MJ, Fang QG, Li ZN, Li WL, Sun CF. Free fibula flap: assessment of quality of life of patients with head and neck cancer who have had defects reconstructed. J Craniofac Surg 2013;24(6):2010–3. [DOI] [PubMed] [Google Scholar]
- 12.Wang L, Su YX, Liao GQ. Quality of life in osteoradionecrosis patients after mandible primary reconstruction with free fibula flap. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108(2):162–8. [DOI] [PubMed] [Google Scholar]
- 13.Yang W, Zhao S, Liu F, Sun M. Health-related quality of life after mandibular resection for oral cancer: reconstruction with free fibula flap. Med Oral Patol Oral Cir Bucal 2014;19(4):e414–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luo RLP, Li W, Li Y, Qi J. Measures of Health-related Quality of Life in Huge Ameloblastoma Young Patients after Mandible Reconstruction with Free Fibula Flap. Journal of Hand Tissue Biology 2014;23(2):261–266. [Google Scholar]
- 15.Hassan SJ, Weymuller EA Jr. Assessment of quality of life in head and neck cancer patients. Head Neck 1993;15(6):485–96. [DOI] [PubMed] [Google Scholar]
- 16.Li X, Zhu K, Liu F, Li H. Assessment of quality of life in giant ameloblastoma adolescent patients who have had mandible defects reconstructed with a free fibula flap. World J Surg Oncol 2014;12:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Girish Rao S, Aditya TN, Gopinath KS, Anand K. Free fibula flap in the reconstruction of mandible: a report of six cases. J Maxillofac Oral Surg 2009;8(3):275–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.D’Antonio LL, Long SA, Zimmerman GJ, Peterman AH, Petti GH, Chonkich GD. Relationship between quality of life and depression in patients with head and neck cancer. Laryngoscope 1998;108(6):806–11. [DOI] [PubMed] [Google Scholar]
- 19.Millsopp L, Humphris G, Lowe D, Rogers SN. Patient’s response using freetext in the University of Washington Quality of Life Scale. Head Neck 2003;25(12):1042–50. [DOI] [PubMed] [Google Scholar]
- 20.Breeze J, Rennie A, Morrison A, et al. Health-related quality of life after maxillectomy: obturator rehabilitation compared with flap reconstruction. Br J Oral Maxillofac Surg 2016;54(8):857–862. [DOI] [PubMed] [Google Scholar]
- 21.Smith GI, Yeo D, Clark J, et al. Measures of health-related quality of life and functional status in survivors of oral cavity cancer who have had defects reconstructed with radial forearm free flaps. Br J Oral Maxillofac Surg 2006;44(3):187–92. [DOI] [PubMed] [Google Scholar]
- 22.Li W, Yang Y, Xu Z, et al. Assessment of quality of life of patients with oral cavity cancer who have had defects reconstructed with free anterolateral thigh perforator flaps. Br J Oral Maxillofac Surg 2013;51(6):497–501. [DOI] [PubMed] [Google Scholar]
- 23.Nemeth D, Zaleczna L, Huremovic A, et al. Importance of chewing, saliva, and swallowing function in patients with advanced oral cancer undergoing preoperative chemoradiotherapy: a prospective study of quality of life. Int J Oral Maxillofac Surg 2017;46(10):1229–1236. [DOI] [PubMed] [Google Scholar]
- 24.Senkal HA, Hayran M, Karakaya E, Yueh B, Weymuller EA Jr., Hosal AS. The validity and reliability of the Turkish version of the University of Washington Quality of Life Questionnaire for patients with head and neck cancer. Am J Otolaryngol 2012;33(4):417–26. [DOI] [PubMed] [Google Scholar]
- 25.Linardoutsos G, Rapidis AD, Lowe D, Bramis I, Rogers SN. Development of the Greek version of the University of Washington quality of life questionnaire for patients with head and neck cancer. J Craniomaxillofac Surg 2014;42(5):601–7. [DOI] [PubMed] [Google Scholar]
- 26.Klassen AF, Cano SJ, Schwitzer JA, Scott AM, Pusic AL. FACE-Q scales for health-related quality of life, early life impact, satisfaction with outcomes, and decision to have treatment: development and validation. Plast Reconstr Surg 2015;135(2):375–86. [DOI] [PubMed] [Google Scholar]
- 27.Wotherspoon RJ, Kanatas AN, Rogers SN. Review of HaNDLE-on-QoL: a database of published papers that use questionnaires to report quality of life in patients with cancer of the head and neck. Br J Oral Maxillofac Surg 2018;56(2):e5–e9. [DOI] [PubMed] [Google Scholar]
- 28.Ciocca L, Tarsitano A, Mazzoni S, Gatto MR, Marchetti C, Scotti R. Evaluation of Masticatory Efficiency and QoL Improvements After Prosthetic Rehabilitation of Mandibular Cancer Patients Reconstructed with a Fibula Free Flap. Int J Prosthodont 2015;28(4):418–24. [DOI] [PubMed] [Google Scholar]
- 29.Epstein JB, Beaumont JL, Gwede CK, et al. Longitudinal evaluation of the oral mucositis weekly questionnaire-head and neck cancer, a patient-reported outcomes questionnaire. Cancer 2007;109(9):1914–22. [DOI] [PubMed] [Google Scholar]
- 30.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 1993;11(3):570–9. [DOI] [PubMed] [Google Scholar]
- 31.Dwivedi RC, St Rose S, Roe JW, et al. First report on the reliability and validity of speech handicap index in native English-speaking patients with head and neck cancer. Head Neck 2011;33(3):341–8. [DOI] [PubMed] [Google Scholar]
- 32.Kanatas AN, Rogers SN. A guide of the questionnaires used in the measurement of health-related quality of life in head and neck oncology. Tumori 2008;94(5):724–31. [DOI] [PubMed] [Google Scholar]