Abstract
BACKGROUND:
Excessive opioid prescribing is common in surgical oncology with 72% of prescribed opioids going unused after curative-intent surgery. In this study, we sought to reduce opioid prescribing after breast and melanoma procedures by designing and implementing an intervention focused on education and prescribing guidelines. We then evaluated the impact of this intervention.
METHODS:
In this single-institution study, we designed and implemented an intervention targeting key factors identified in qualitative interviews. This included mandatory education for prescribers, evidence-based prescribing guidelines, and standardized patient instructions. After the intervention, interrupted time series analysis was used to compare the mean quantity of opioid prescribed before and after the intervention (July 2016-September 2017). We also evaluated the frequency of opioid prescription refills.
RESULTS:
During the study, 847 patients underwent breast or melanoma procedures and received an opioid prescription. For mastectomy or wide local excision for melanoma, the mean quantity of opioid prescribed immediately decreased by 37% after the intervention (P=0.03), equivalent to 13 tablets of 5mg oxycodone. For lumpectomy or breast biopsy, the mean quantity of opioid prescribed decreased by 42% or 12 tablets of 5mg oxycodone (P=0.07). Furthermore, opioid prescription refills did not significantly change for mastectomy/wide local excision (13% vs. 14%, P=0.8), or lumpectomy/breast biopsy (4% vs. 5%, P=0.7).
CONCLUSIONS:
Education and prescribing guidelines reduced opioid prescribing for breast and melanoma procedures without increasing the need for refills. This suggests further reductions in opioid prescribing may be possible, and provides rationale for implementing similar interventions for other procedures and practice settings.
INTRODUCTION
Surgeons frequently overprescribe opioids with 67 – 92% of patients having unused opioids after common elective procedures.1–9 Unfortunately, excessive opioid prescribing can have serious consequences for surgical patients. Among previously opioid-naïve patients undergoing common elective procedures, 6 – 10% develop new persistent opioid use and continue filling opioid prescriptions 3 – 6 months after surgery.10–12 Patients with cancer undergoing curative-intent surgery are particularly vulnerable with 10% developing new persistent opioid use.10 Many factors likely contribute to this increased risk, including frequent overprescribing of opioids in surgical oncology,2,13 uncoordinated prescribing from multiple specialties,14 high levels of psychosocial distress15–17 leading to increased opioid consumption,18,19 and side effects from chemotherapy.10,20–23
Despite these risks, little is known about effective strategies for improving the safety of postoperative opioid prescribing for patients with cancer. On one hand, many states have enacted legislation limiting opioid prescribing to surgical patients.24 Unfortunately, these limits are still much higher than the actual needs of surgical oncology patients,2,13 and often have vague exemptions for patients with cancer.24 On the other hand, our previous work has demonstrated education and prescribing guidelines are likely to change opioid prescribing behavior in surgical oncology.25 The effectiveness of these proposed interventions, however, has yet to be evaluated.
In this context, we designed and implemented an intervention to reduce opioid prescribing for patients undergoing breast and melanoma procedures. We then evaluated the impact of this intervention on the quantity of opioid prescribed. We hypothesized opioid prescribing would be significantly reduced after the intervention.
METHODS
Design of the intervention
The University of Michigan Institutional Review Board approved this study. We designed our intervention based on previous qualitative work, which identified education and prescribing guidelines as interventions likely to change opioid prescribing behavior in surgical oncology.25 Figure 1 shows the specific components of the intervention. Each component of the intervention is described in detail below:
-
1.
Mandatory education for prescribers: Prescribers in surgical oncology received a written protocol (Supplemental Figure 1) and attended mandatory educational conferences three times per year. Conferences focused on illustrating how the quantity of opioid prescribed far exceeds patient needs, and described data underlying the new opioid prescribing guidelines.
-
2.
Evidence-based prescribing guidelines:Specific prescribing guidelines are shown in detail in Table 1. Prescribing guidelines specific to each procedure were created based on previously published studies2,13 and patient-reported opioid consumption data from our institution. These guidelines were distributed to surgical residents as a written protocol (Supplemental Figure 1) with an online module at the beginning of their rotations on the surgical oncology service. The online module consisted of a 10-minute video that summarized the role of surgeons in the opioid epidemic, described key data underlying the new opioid prescribing guidelines, and described how to integrate the new prescribing guidelines and patient instructions into the existing clinical workflow. The online module also provided links to key studies for the prescribing guidelines and patient instructions.
-
3.
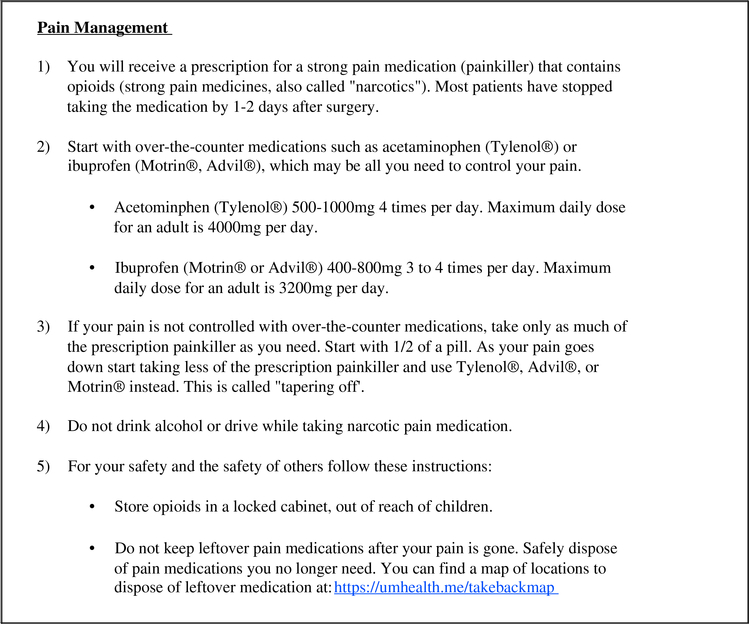
Standardized patient instructions:The specific instructions used for this study are shown in Figure 2. Patient instructions focused on using non-opioid analgesics first with opioids only for breakthrough pain, safe storage of opioids, and safe disposal of unused opioids.
Figure 1: Intervention for opioid prescribing.
The intervention was designed based on previous qualitative work, which identified education and prescribing guidelines as interventions likely to change opioid prescribing behavior in surgical oncology. The intervention had three components: 1) mandatory education for prescribers including educational conferences and written protocols; 2) evidence-based prescribing guidelines specific to each procedure based on previously published studies and patient-reported opioid consumption data from our institution; and 3) standardized patient instructions emphasizing using non-opioid analgesics first with opioids only for breakthrough pain, safe storage of opioids, and safe disposal of unused opioids.
Table 1.
Evidence-based opioid prescribing guidelines
| Procedure | Recommended Prescription |
|---|---|
| Melanoma wide local excision ± sentinel lymph node biopsy | 20 tablets of 5 mg oxycodone |
| Simple mastectomy ± sentinel lymph node biopsy | 20 tablets of 5 mg oxycodone |
| Sentinel lymph node biopsy only | 10 tablets of 5 mg oxycodone |
| Lumpectomy with sentinel lymph node biopsy | 10 tablets of 5 mg oxycodone |
| Breast biopsy or lumpectomy without sentinel lymph node biopsy | 5 tablets of 5 mg oxycodonea |
During the study, the recommended prescription was 10 tablets of 5 mg oxycodone. After the study, this was reduced to 5 tablets based on patient-reported opioid consumption data from our institution and other studies.13
Figure 2: Standardized patient instructions for pain management.
All patients were provided with standardized written instructions for pain management. The instructions were also explained in-person by nursing staff. Key topics reviewed included using nonopioid analgesics first with opioids only for breakthrough pain, safe storage of opioids, and safe disposal of unused opioids.
Study cohort, data source, and study outcomes
After the intervention was implemented on November 3, 2016, we performed a retrospective analysis of all patients undergoing an eligible breast or melanoma procedure before and after the intervention (July 2016 – September 2017). This included breast biopsy, lumpectomy, sentinel lymph node biopsy, simple mastectomy, and wide local excision for melanoma. Patient and opioid prescription data were obtained from an automated report generated from the electronic medical record, which automatically records all prescriptions provided by prescribers at our institution. The primary outcome for this study was the quantity of opioid for the initial postoperative opioid prescription provided to the patient at discharge. This was converted to oral morphine equivalents (OME),26 then standardized to the equivalent number of tablets of 5 mg oxycodone for ease of interpretation. A secondary outcome for the study was the percentage of patients requiring an opioid prescription refill. This was defined as being provided another opioid prescription in the 30 days after surgery. Patients who underwent another procedure within 30 days of their index procedure were excluded for this part of the analysis. In addition, we evaluated the percentage of patients with opioid prescriptions in compliance with the prescribing guidelines (less than equal to the recommended quantity of opioid for that procedure).
Statistical analysis
Patients were divided into two groups based on procedure type and the recommended quantity of opioid to prescribe: 1) 20 tablets for simple mastectomy or wide local excision for melanoma ± sentinel lymph node biopsy; and 2) 5 – 10 tablets for breast biopsy or lumpectomy ± sentinel lymph node biopsy. For each group, we calculated the mean quantity of opioid prescribed (OME) every month. We then used interrupted times series analysis to evaluate the change in the mean quantity of opioid prescribed after the intervention. Interrupted time series analysis is a well-established method for evaluating the impact of public health interventions by accounting for preintervention and post-intervention trends in the outcome of interest.27
Because interrupted time series analysis does not account for variation at each individual time point, we also compared summary statistics for the pre-intervention period (four months before the intervention), transition period (seven months after the intervention), and post-intervention period (four months after the transition period). The seven-month transition period was chosen to allow sufficient time for new practice patterns to stabilize. The mean quantity of opioid prescribed was compared using Student’s t-test. The percentage of patients requiring opioid prescription refills and the percentage of patients with opioid prescriptions in compliance with the prescribing guidelines was compared using Fisher’s exact test. All analyses were performed using Stata version 14.2 (StataCorp LLC, College Station, Texas). Two-sided P values less than 0.05 were considered statistically significant.
RESULTS
In this study, 847 patients underwent an eligible breast or melanoma procedure and received an opioid prescription. Of these, 340 patients (40%) underwent simple mastectomy or wide local excision for melanoma. The remaining 507 patients (60%) underwent lumpectomy or breast biopsy. For simple mastectomy or wide local excision for melanoma, 103 patients (30%) underwent surgery before the intervention and 237 patients (70%) underwent surgery after the intervention. For breast biopsy or lumpectomy, 137 patients (27%) underwent surgery before the intervention and 370 patients (73%) underwent surgery after the intervention. A total of 61 unique prescribers wrote opioid prescriptions during the study period. Surgical residents wrote the vast majority (91%) of opioid prescriptions during the study. In contrast, surgical fellows wrote only 8% of opioid prescriptions, and attending surgeons wrote only 1% of opioid prescriptions.
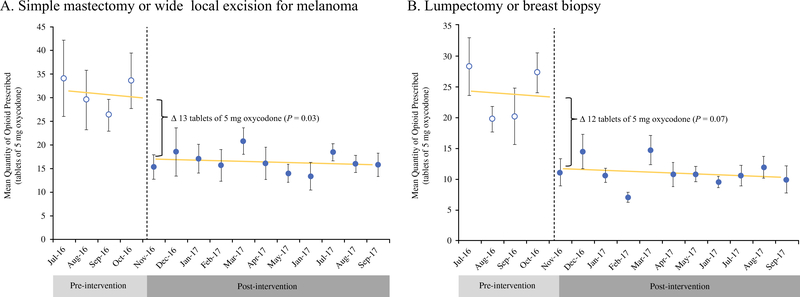
Figure 3 compares the mean quantity of opioid prescribed each month before and after the intervention using interrupted time series analysis. For simple mastectomy or wide local excision for melanoma (Figure 3A), the mean quantity of opioid prescribed was declining slowly prior to the intervention (– 0.4 tablets of 5 mg oxycodone per month), but this trend was not statistically significant (P = 0.8). After the intervention, the mean quantity of opioid prescribed immediately decreased by 37%, equivalent to 13 tablets of 5 mg oxycodone (P = 0.03). The mean quantity of opioid prescribed continued to decline slowly after the intervention (– 0.1 tablets of 5 mg oxycodone per month), but this trend was not statistically significant (P = 0.4). The change in the pre-intervention and post-intervention trend was also not statistically significant (P = 0.9).
Figure 3: Impact of the intervention on quantity of opioid prescribed.
Interrupted time series analysis was used to evaluate the impact of the intervention on the mean quantity of opioid prescribed each month. Error bars show 95% confidence intervals for each mean. [A] For simple mastectomy or wide local excision for melanoma, the mean quantity of opioid prescribed immediately decreased by 37% after the intervention, equivalent to 13 tablets of 5 mg oxycodone (P = 0.03). [B] For lumpectomy or breast biopsy, the mean quantity of opioid prescribed immediately decreased by 42% after the intervention, equivalent to 12 tablets of 5 mg oxycodone (P = 0.07).
For lumpectomy or breast biopsy (Figure 3B), the mean quantity of opioid prescribed was declining slowly prior to the intervention (– 0.2 tablets of 5 mg oxycodone per month), but this trend was not statistically significant (P = 0.9). After the intervention, the mean quantity of opioid prescribed immediately decreased by 42%, equivalent to 12 tablets of 5 mg oxycodone (P = 0.07). The mean quantity of opioid prescribed continued to decline slowly after the intervention (– 0.1 tablets of 5 mg oxycodone per month), but this trend was not statistically significant (P = 0.5). The change in the pre-intervention and post-intervention trend was also not statistically significant (P = 1.0).
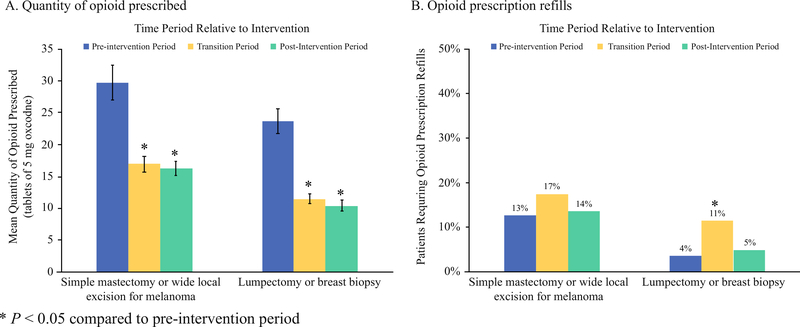
Figure 4 compares the mean quantity of opioid prescribed and the percentage of patients requiring opioid prescription refills during the pre-intervention, transition, and post-intervention periods. The mean quantity of opioid prescribed decreased immediately during the transition period and remained low during the post-intervention period (Figure 4A). The mean quantity of opioid prescribed during the post-intervention period was significantly reduced compared to the pre-intervention period for simple mastectomy or wide local excision for melanoma (30 vs. 16 tablets of 5 mg oxycodone, P < 0.001) and lumpectomy or breast biopsy (24 vs. 10 tablets of 5 mg oxycodone, P < 0.001). Opioid prescription refills initially increased during the transition period for both procedure groups, but subsequently returned to pre-intervention levels (Figure 4B).
Figure 4: Quantity of opioid prescribed and opioid prescription refills.
Study outcomes were compared during the pre-intervention period (four months before the intervention), transition period (seven months after the intervention), and postintervention period (four months after the transition period). [A] Errors bars show 95% confidence intervals for each mean. The mean quantity of opioid prescribed during the post-intervention period was significantly reduced compared to the pre-intervention period for simple mastectomy or wide local excision for melanoma (30 vs. 16 tablets of 5 mg oxycodone, P < 0.001) and lumpectomy or breast biopsy (24 vs. 10 tablets of 5 mg oxycodone, P < 0.001). [B] Opioid prescription refills during the post-intervention period were not significantly different compared to the pre-intervention period for simple mastectomy or wide local excision for melanoma (13% vs. 14%, P = 0.8) and lumpectomy or breast biopsy (4% vs. 5%, P = 0.7).
Opioid prescription refills during the post-intervention period were not significantly different compared to the pre-intervention period for simple mastectomy or wide local excision for melanoma (13% vs. 14%, P = 0.8) and lumpectomy or breast biopsy (4% vs. 5%, P = 0.7). In addition, the percentage of patients with opioid prescriptions in compliance with the prescribing guidelines during the post-intervention period increased significantly compared to the pre-intervention period for simple mastectomy or wide local excision of melanoma (36% vs. 97%, P < 0.001) and lumpectomy or breast biopsy (8% vs. 83%, P < 0.001).
DISCUSSION
This study has two key findings. First, education and prescribing guidelines effectively reduced the quantity of opioid prescribed for patients undergoing breast and melanoma procedures at a single academic institution. Second, this reduction in opioid prescribing occurred without increasing the need for opioid prescription refills. Although opioid prescription refills transiently increased during the transition period, they returned to baseline levels during the post-intervention period. This transient increase opioid prescription refills was likely due to ineffective patient education on strategies to minimize opioid use, such as using non-opioid analgesics first with opioids only for severe breakthrough pain. This was discovered during discussions with clinic nurses answering telephone calls from patients requesting refills. In response, more time was spent educating prescribers on how to counsel patients on specific strategies to minimize opioid use.
The findings of this study have important implications. First, similar interventions could be implemented at other academic teaching hospitals to reduce opioid prescribing for surgical oncology. We have provided the prescribing guidelines and patient education materials used in this study for institutions potentially interested in implementing this type of intervention. The procedure-specific prescribing guidelines are also publicly available online along with prescribing guidelines for other procedures based on prospective statewide data on patient-reported opioid consumption.28 Future work should focus on evaluating the effectiveness of these interventions across multiple settings of care, including private practice and non-teaching hospitals. In fact, these interventions could be even more effective in these settings given the lack of frequent turnover of surgical trainees, who often perform the majority of opioid prescribing at teaching hospitals. Second, because reductions in opioid prescribing were not associated with an increase in opioid prescription refills, it may be possible to further reduce opioid prescribing. In fact, previous studies have demonstrated that the initial quantity of opioid prescribed is not associated with the frequency of opioid prescription refills29 or patient satisfaction scores.1,30 Finally, these interventions may help reduce the supply of unused prescription opioids in the community, which is a major contributor to the current epidemic of prescription opioid misuse.31
It is possible that education and prescribing guidelines will also be effective for other surgical procedures. In fact, two previous studies have demonstrated this type of intervention is effective for reducing opioid prescribing for laparoscopic cholecystectomy and hernia repair.1,13 In contrast to these proven interventions, 19 states have passed laws limiting opioid prescriptions for acute pain to a seven-day supply.24 While well-intentioned, these laws have no proven effectiveness for reducing opioid prescribing, and do not provide sufficient limits on opioid prescribing. For example, a seven-day limit still allows for 28 – 84 tablets of oxycodone (1–2 tablets every 4–6 hours × 7 days), which still far exceeds the needs of most surgical patients.1–4,13 These laws also do not account for potential differences in opioid prescribing practices for primary care, surgery, and emergency medicine. In addition to these laws, surgeons should consider implementing interventions described in this study and others,1,13 which are known be effective for reducing opioid prescribing.
This study adds to previous work describing postoperative opioid use, which has demonstrated three key findings: 1) patients with cancer undergoing curative-intent surgery are at risk of developing new persistent opioid use;10,11 2) opioids are frequently overprescribed for surgical oncology procedures;2 and 3) education and prescribing guidelines are likely to change healthcare provider behavior for opioid prescribing in surgical oncology.25 The findings of this study confirm that education and guidelines are indeed an effective strategy for reducing opioid prescribing in this vulnerable population. In addition, this study further supports the effectiveness of using education and prescribing guidelines to reduce opioid prescribing in surgical patients, which was also demonstrated in two previous single institution studies.1,13 It also reports the success of this intervention for melanoma patients undergoing wide local excision, which has not been reported in previous studies of opioid prescribing for surgical patients.2–4,8,13,32,33 Our findings also provide evidence to directly refute common misconceptions about opioid prescribing. For example, surgical oncology providers frequently report overprescribing opioids in an effort to reduce patient requests for refills.25 This study shows that reducing the quantity of opioid prescribed does not increase the frequency of refills, which is in agreement with other studies demonstrating no association between the quantity of opioid prescribed and refills or patient satisfaction.1,29,30
This study has several limitations. First, it was limited to a single academic teaching hospital, which limits the generalizability of the results. For example, over 99% of opioid prescriptions in this study were provided by surgical trainees. Because of this, our analysis was not adequately powered to evaluate differences in the success of the intervention when comparing trainees with attending surgeons. Nevertheless, we expect our results to be reproducible in similar settings of care. In fact, two other studies at academic teaching hospitals have reported significant reductions in opioid prescribing using a similar approach.1,13 This study was also limited in that we did not account for all potential confounding factors, such as differences in age, race, socioeconomic status, and comorbidities. Previous work, however, has shown that these variables are not significantly associated with opioid prescribing.29 Because of this, it is unlikely that adjusting for these variables would change the findings of this study. We also did not account for the potential effect of other interventions (formal or informal) during the 7month transition period after the intervention. Nevertheless, the interrupted times series analysis in this study demonstrated an immediate significant decrease in the mean quantity of opioid prescribed with a non-significant post-intervention trend. This makes it less likely that other interventions during the 7-month transition period played a significant role in changing the study outcome.
This study was also limited because patients were not randomized, which makes it difficult to measure the true effect of the intervention. For example, opioid prescribing may have already been decreasing before the intervention. To account for this, we used interrupted time series analysis to evaluate any pre-intervention trend, which was found to be insignificant. Furthermore, randomization was not possible due to the lack of clinical equipoise for the intervention. Another limitation was that the intervention was limited to surgeons only. Unfortunately, patients with cancer are frequently exposed to uncoordinated opioid prescribing from multiple specialties.14,34 Future work will focus on facilitating more effective transitions of care for surgical patients to prevent uncoordinated opioid prescribing. Finally, although we compared opioid prescription refills before and after the intervention, this study was limited because we did not evaluate patient-reported outcomes such as pain and overall satisfaction. These important outcomes are the focus of ongoing work in our group. In addition, because our electronic medical record does not record opioid prescriptions obtained from prescribers at other institutions, our study may underestimate the frequency of opioid prescription refills. We also did not specifically evaluate requests for opioid prescriptions refills, which could be inconsistently documented in the medical record. Future studies will prospectively measure this to evaluate potential increases in workload for clinic staff.
In conclusion, we found that education and prescribing guidelines significantly reduced the quantity of opioid prescribed for breast and melanoma procedures without increasing the need for refills. These findings suggest further reductions in opioid prescribing may be possible, and provides rationale for implementing similar interventions for other procedures and practice settings. Given the known risks of opioids10 and pervasive overprescribing of opioids to surgical oncology patients,2 surgical oncology providers should strongly consider implementing similar interventions to reduce opioid prescribing and improve the quality of care for cancer survivors.
Supplementary Material
Supplemental Figure 1: Surgical Oncology Service Protocol for Postoperative Pain Medications. All prescribers in surgical oncology received a written protocol describing the new opioid prescribing guidelines and key points for patient education. The protocol also described strategies to optimize pain control while minimizing the need for opioids, such as infiltration of long-acting local anesthetic prior to incision.
SYNOPSIS.
In this study, we evaluated the impact of mandatory education and prescribing guidelines on opioid prescribing after breast and melanoma procedures. This intervention significantly reduced the quantity of opioid prescribed without increasing the frequency of opioid prescription refills.
Acknowledgments
Research Support: Dr. Lee is a National Research Service Award postdoctoral fellow supported by the National Cancer Institute (5T32 CA009672–23). Drs. Englesbe, Waljee, and Brummett receive funding from the Michigan Department of Health and Human Services and the National Institute on Drug Abuse (RO1 DA042859). The content of this study is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Michigan Department of Health and Human Services.
Presented at the Society of Surgical Oncology 71st Annual Cancer Symposium, Chicago, IL, March 2018.
REFERENCES
- 1.Howard R, Waljee J, Brummett C, Englesbe M, Lee J. Reduction in Opioid Prescribing Through Evidence-Based Prescribing Guidelines. JAMA Surg. 2018;153(3):285–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hill MV, McMahon ML, Stucke RS, Barth RJ, Jr. Wide Variation and Excessive Dosage of Opioid Prescriptions for Common General Surgical Procedures. Ann Surg. 2017;265(4):709–714. [DOI] [PubMed] [Google Scholar]
- 3.Feinberg AE, Chesney TR, Srikandarajah S, Acuna SA, McLeod RS, Best Practice in Surgery G. Opioid Use After Discharge in Postoperative Patients: A Systematic Review. Ann Surg. 2017. [DOI] [PubMed] [Google Scholar]
- 4.Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription Opioid Analgesics Commonly Unused After Surgery: A Systematic Review. JAMA Surg. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maughan BC, Hersh EV, Shofer FS, et al. Unused opioid analgesics and drug disposal following outpatient dental surgery: A randomized controlled trial. Drug Alcohol Depend. 2016;168(1879–0046 (Electronic)):328–334. [DOI] [PubMed] [Google Scholar]
- 6.Bartels K, Mayes LM, Dingmann C, Bullard KJ, Hopfer CJ, Binswanger IA. Opioid Use and Storage Patterns by Patients after Hospital Discharge following Surgery. PLoS ONE. 2016;11(1):e0147972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris K, Curtis J, Larsen B, et al. Opioid Pain Medication Use After Dermatologic Surgery A Prospective Observational Study of 212 Dermatologic Surgery Patients. Jama Dermatology. 2013;149(3):317–321. [DOI] [PubMed] [Google Scholar]
- 8.Rodgers J, Cunningham K, Fitzgerald K, Finnerty E. Opioid consumption following outpatient upper extremity surgery. J Hand Surg Am. 2012;37(4):645–650. [DOI] [PubMed] [Google Scholar]
- 9.Bates C, Laciak R, Southwick A, Bishoff J. Overprescription of postoperative narcotics: a look at postoperative pain medication delivery, consumption and disposal in urological practice. J Urol. 2011;185(2):551–555. [DOI] [PubMed] [Google Scholar]
- 10.Lee JS, Hu HM, Edelman AL, et al. New Persistent Opioid Use Among Patients With Cancer After Curative-Intent Surgery. J Clin Oncol. 2017;35(36):4042–4049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brummett CM, Waljee JF, Goesling J, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg. 2017;152(6):e170504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goesling J, Moser SE, Zaidi B, et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. PAIN. 2016;157(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hill MV, Stucke RS, McMahon ML, Beeman JL, Barth RJ, Jr., An Educational Intervention Decreases Opioid Prescribing After General Surgical Operations. Ann Surg. 2017. [DOI] [PubMed] [Google Scholar]
- 14.Dreyer T, Rontal R, Gabriel K, Udow-Phillips M, Uncoordinated Prescription Opioid Use in Michigan. Ann Arbor, MI: Center for Healthcare Research & Transformation, December 2015. 2015. http://www.chrt.org/publication/uncoordinated-prescription-opioid-use-inmichigan/. Accessed March 30, 2018. [Google Scholar]
- 15.Fann JR, Ell K, Sharpe M. Integrating psychosocial care into cancer services. J Clin Oncol. 2012;30(11):1178–1186. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12(2):160–174. [DOI] [PubMed] [Google Scholar]
- 17.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10(1):19–28. [DOI] [PubMed] [Google Scholar]
- 18.Brummett CM, Janda AM, Schueller CM, et al. Survey criteria for fibromyalgia independently predict increased postoperative opioid consumption after lowerextremity joint arthroplasty: a prospective, observational cohort study. Anesthesiology. 2013;119(6):1434–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Janda AM, As-Sanie S, Rajala B, et al. Fibromyalgia Survey Criteria Is Associated with Increased Postoperative Opioid Consumption in Women Undergoing Hysterectomy. Anesthesiology. 2015. [DOI] [PubMed] [Google Scholar]
- 20.Gartner R, Jensen MB, Nielsen J, Ewertz M, Kroman N, Kehlet H. Prevalence of and factors associated with persistent pain following breast cancer surgery. JAMA. 2009;302(18):1985–1992. [DOI] [PubMed] [Google Scholar]
- 21.Jung BF, Herrmann D, Griggs J, Oaklander AL, Dworkin RH. Neuropathic pain associated with non-surgical treatment of breast cancer. Pain. 2005;118(1–2):10–14. [DOI] [PubMed] [Google Scholar]
- 22.Land SR, Kopec JA, Cecchini RS, et al. Neurotoxicity from oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: NSABP C-07. J Clin Oncol. 2007;25(16):2205–2211. [DOI] [PubMed] [Google Scholar]
- 23.Mols F, Beijers T, Lemmens V, van den Hurk CJ, Vreugdenhil G, van de PollFranse LV. Chemotherapy-induced neuropathy and its association with quality of life among 2- to 11-year colorectal cancer survivors: results from the population-based PROFILES registry. J Clin Oncol. 2013;31(21):2699–2707. [DOI] [PubMed] [Google Scholar]
- 24.State and Federal Legislation Surrounding Initial Opioid Prescriptions. 2017; http://www.astho.org/StatePublicHealth/State-and-Federal-Legislation-Surrounding-Initial-Opioid-Prescriptions/03-08-18/. Accessed March 22, 2018.
- 25.Lee JS, Parashar V, Miller JB, et al. Opioid Prescribing After Curative-Intent Surgery: A Qualitative Study Using the Theoretical Domains Framework. Ann Surg Oncol. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gammaitoni AR, Fine P, Alvarez N, McPherson ML, Bergmark S. Clinical application of opioid equianalgesic data. Clin J Pain. 2003;19(5):286–297. [DOI] [PubMed] [Google Scholar]
- 27.Lopez Bernal J, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michigan Opioid Prescribing Engagement Network. Opioid Prescribing Recommendations for Surgery. https://opioidprescribing.info/. Accessed March 27, 2018.
- 29.Sekhri S, Arora NS, Cottrell H, et al. Probability of Opioid Prescription Refilling After Surgery: Does Initial Prescription Dose Matter? Annals of Surgery. 2017;Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee JS, Hu HM, Brummett CM, et al. Postoperative Opioid Prescribing and the Pain Scores on Hospital Consumer Assessment of Healthcare Providers and Systems Survey. JAMA. 2017;317(19):2013–2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lipari RN, Hughes A. How People Obtain the Prescription Pain Relievers They Misuse. In: The CBHSQ Report; Rockville (MD)2017:1–7. [PubMed] [Google Scholar]
- 32.Swenson CW, Kelley AS, Fenner DE, Berger MB. Outpatient Narcotic Use After Minimally Invasive Urogynecologic Surgery. Female Pelvic Med Reconstr Surg. 2016;22(5):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim N, Matzon JL, Abboudi J, et al. A Prospective Evaluation of Opioid Utilization After Upper-Extremity Surgical Procedures: Identifying Consumption Patterns and Determining Prescribing Guidelines. The Journal of bone and joint surgery American volume. 2016;98(20):e89. [DOI] [PubMed] [Google Scholar]
- 34.Klueh MP, Hu HM, Howard RA, et al. Transitions of Care for Postoperative Opioid Prescribing in Previously Opioid-Naïve Patients in the United States: A Retrospective Review. In press. J Gen Intern Med. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Surgical Oncology Service Protocol for Postoperative Pain Medications. All prescribers in surgical oncology received a written protocol describing the new opioid prescribing guidelines and key points for patient education. The protocol also described strategies to optimize pain control while minimizing the need for opioids, such as infiltration of long-acting local anesthetic prior to incision.