Abstract
Stem cells drive embryonic and fetal development. In several adult tissues, they retain the ability to self-renew and differentiate into a variety of specialized cells, thus contributing to tissue homeostasis and repair throughout life span. Alcohol consumption is associated with an increased risk for several diseases and conditions. Growing and developing tissues are particularly vulnerable to alcohol’s influence, suggesting that stem- and progenitor-cell function could be affected. Accordingly, recent studies have revealed the possible relevance of alcohol exposure in impairing stem-cell properties, consequently affecting organ development and injury response in different tissues. Here, we review the main studies describing the effects of alcohol on different types of progenitor/stem cells including neuronal, hepatic, intestinal and adventitial progenitor cells, bone-marrow-derived stromal cell, dental pulp, embryonic and hematopoietic stem cells, and tumor-initiating cells. A better understanding of the nature of the cellular damage induced by chronic and episodic heavy (binge) drinking is critical for the improvement of current therapeutic strategies designed to treat patients suffering from alcohol-related disorders.
Keywords: Alcoholic beverages, Mesenchymal stromal cells, Alcohol-related disorders, Fetal alcohol spectrum disorders, Alcohol dehydrogenase, Acetaldehyde
Introduction
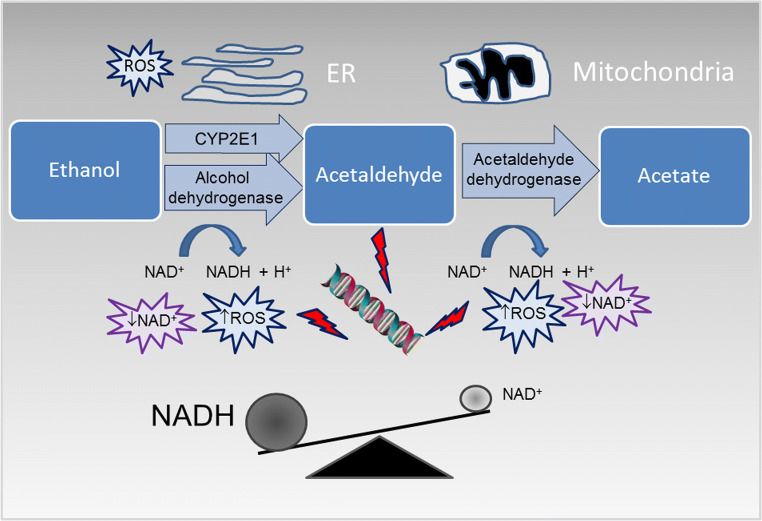
According to the World Health Organization, approximately half of the global adult population consumes alcoholic beverages; nevertheless, alcohol consumption represents one of the most important risk factor for public health and the third leading cause of premature death [1]. Alcohol use is associated with chronic and acute diseases including several types of cancers, cardiovascular diseases, diabetes, pneumonia, immunologic alterations, liver cirrhosis, and reduced healing after traumatic injury [2]. Moreover, alcohol exposure during prenatal gestation determines a wide array of harmful effects on the developing fetus, collectively indicated as fetal alcohol spectrum disorders (FASD). Whether moderate alcohol consumption is potentially preventative against cardiovascular diseases [3] is an object of ongoing scientific debate [4]. The quantity, type, and quality of the alcoholic beverages and the pattern of drinking habits can modify the effects of alcohol misuse. Moreover, several other factors, such as genetic background, gender, age, ethnicity, diet, hormone status, as well as interactions with additional risk factors such as smoking and obesity, can have an impact on modulating alcohol response [5]. In addition, the rate of alcohol metabolism contributes to the development of alcohol-associated diseases. Ingested alcohol is rapidly absorbed throughout the gastrointestinal tract into the bloodstream, and then, the majority (more than 90%) is metabolized in the liver. The most important hepatic ethanol metabolic pathway involves the oxidation by the enzymatic activity of alcohol dehydrogenase (ADH), which converts alcohol to acetaldehyde, and acetaldehyde dehydrogenase (ALDH), which converts acetaldehyde to acetate (Fig. 1). As an ultimate step, acetate is further metabolized to carbon dioxide and water before being eliminated from the body. The kinetic of the process may be altered in the presence of different polymorphic variants of these enzymes [6]. Overall, alcohol metabolism results in: production of acetaldehyde, which is a known carcinogen; generation of reactive oxygen species (ROS), contributing to oxidative stress; production of acetate, which affects several metabolic processes; and in a significant alteration of the cellular redox balance, in particular through a change of the ratio of the oxidized and reduced forms of nicotinamide adenine dinucleotide (NAD+/NADH) [7].
Fig. 1.
Main pathways of alcohol oxidative metabolism. Ethanol is converted into acetaldehyde by the cytosolic enzyme alcohol dehydrogenase and by the microsomal cytochrome P450 2E1 (CYP2E1); acetaldehyde is then oxidized into acetate by the mitochondrial enzyme aldehyde dehydrogenase 2. Alcohol metabolism increases the ratio of the reduced nicotinamide adenine dinucleotide (NADH) to the oxidized nicotinamide adenine dinucleotide (NAD+) and promotes reactive oxygen species (ROS) production
Ethanol has an impact on virtually all tissues, and some effects can persist long after stopping alcohol intake. Growing and developing tissues are remarkably susceptible to alcohol due to incomplete antioxidant protection. In fact, epidemiologic studies have provided evidence that drinking during adolescence can be dangerous for brain development, possibly inducing irreversible damage. Most importantly, alcohol exposure in pregnancy affects embryo development and can cause permanent birth defects. Similarly, early postnatal alcohol exposure might result in immunological and neurological disorders in later life. Accordingly, teen and prenatal alcohol drinking are serious social and health problems with increasing incidence. While the fact that acute and chronic alcohol abuse severely damages tissue and organ functions is well-established, only recently the role of ethanol exposure in deteriorating stem-cell properties has been investigated. Different organs of an individual may have different sensitivities to alcohol. The hypothesis that ethanol has nefarious consequences on stem cells in different tissues is consistent with alcohol’s widespread, long-term effects observed in the developing and adult human organisms.
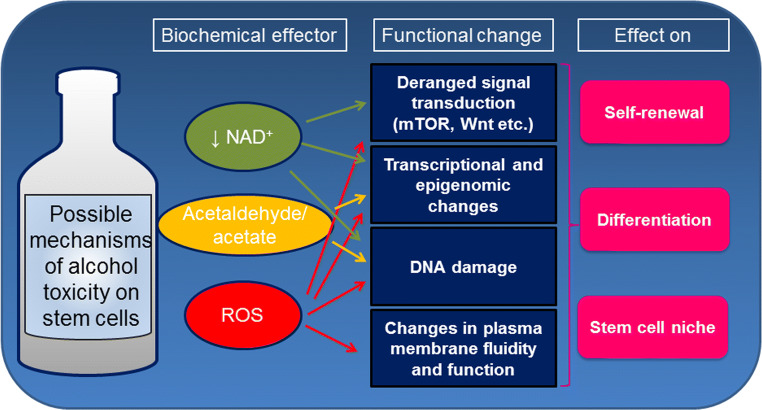
Evidence of direct toxicity of ethanol and/or its metabolites on stem and progenitor cells in different tissues offers a new perspective on the biological consequences of alcohol intake (Fig. 2). Accordingly, due to the profound perturbation of alcohol on stem-cell biology in the developing fetus, Mahnke et al. have provocatively proposed to classify FASD as a “stem cellopathy” [8]. However, the exact mechanisms causing ethanol deleterious effects remain to be completely investigated. Alcohol susceptibility may depend on the target cell and may be influenced by the dose and duration of exposure. Adult stem cells reside in a quiescent state in specialized niches within multiple different tissues. In response to an injury stem cells are able to exit quiescence, renew themselves and differentiate into different cell types [9]. The maintenance of quiescence for a prolonged period of time is functional to preserve stem-cell proliferative potential and genomic integrity throughout the lifetime of the organism. On the other hand, long-lived stem cells are continuously exposed to endogenous and exogenous genotoxic agents, leading to accumulation of DNA damage. Accumulating evidences, suggest that alcohol may impact key aspect of stem cell biology, such as the function of the niche, maintenance of potency and differentiation. In the following sections, we review the main studies describing the effects of alcohol on different types of stem cells (Table 1).
Fig. 2.
Possible mechanisms of alcohol toxicity on stem cell biology
Table 1.
Effects of alcohol on stem cells
| Cell type | Observed changes | Main references |
|---|---|---|
| Neural progenitors cells | Reduced proliferation; effects on cell fate determination | [10, 16, 17, 20] |
| Hepatic stem cells | Reduced proliferation; promotion of mesenchymal transition | [43] |
| Intestinal stem cells | Decreased the expression of stem cell markers, | [46] |
| BM-derived MSC | Reduced osteogenic differentiation; adipogenic effect; induction of senescence | [34, 52, 57, 59] |
| Dental pulp stem cells | Dysregulation of odontogenic/osteogenic differentiation. | [58, 63, 64] |
| Adventitial progenitor cells | Decreased proliferation; reduced myogenic differentiation | [69] |
| Embryonic stem cells | Inhibition of differentiation; apoptosis induction | [78, 86] |
| Hematopietic progenitors | Effects on cell fate determination; DNA damage | [91–93, 97] |
| Cancer stem cells | Phenotypic changes; microenvironmental alterations. | [105, 108] |
BM bone marrow, MSC mesenchymal stromal cells
Effects of alcohol on different types of stem cells
Neural stem cells
The devastating effects of fetal exposure to ethanol on brain development and function in the context of FASD conceivably reflect major consequences of alcohol on early neuronal maturation and by extension on proliferation, differentiation and survival of embryonic neural stem and progenitor cells (NSC) [8, 10]. Furthermore, ethanol can also impact on adult NSC activity in some brain areas, primarily in the subgranular zone of the hippocampus, where neurogenesis persists throughout the entire lifetime [11], or at least until early postnatal life [12]. Adult neurogenesis has been documented in nearly all animal models investigated so far, including rodents and primates, supporting a limited degree of cell renewal within brain structures which has been estimated in 1.7% annual turnover in the human hippocampus [13]. Adult neurogenesis contributes to higher cognitive phenomena, from pattern discrimination to memory consolidation/extinction and mood changes [14]. Thus, deranged adult neurogenesis may contribute to the neurologic decline and neurodegenerative changes observed in chronic alcoholism [15–17]. Accordingly, studies in adolescent and adult rodents under a binge ethanol exposure have shown a consistent reduction in neural progenitors proliferation and survival, as assessed by bromodeoxyuridine (BrdU) labeling at both 1 and 28 days after treatment [18, 19]. A similar, albeit transient (maximum at 3 days with recovery at 30 days), reduction of dentate gyrus (DG) progenitors has been described in rats subjected to chronic, voluntary ethanol assumption in the drinking water [20]. Conversely, neurogenesis increases in rats during chronic abstinence from alcohol [21], a phenomenon possibly related to the return of human cognitive function and brain volume associated with recovery from addiction. Of note, brain damage and epilepsy, two conditions experimentally associated with enhanced hippocampal neurogenesis [22], are also major consequences of ethanol abuse on human brain.
Interestingly, compromised adult neurogenesis may also be implicated in the long-term neural consequences of fetal exposure to ethanol. In particular, adult neurogenesis appears preserved [23] or even increased in adult rodents prenatally exposed to ethanol [24], with higher number of immature neurons in DG, a possible compensatory mechanism to alcohol-induced neuronal loss. In contrast, a decrease in hippocampal neurogenesis has been specifically detected in aged rats exposed to the same experimental paradigm [25]. While the mechanisms underlying these age-specific effect of fetal ethanol exposure on adult neurogenesis are still ill–defined, alcohol-induced epigenetic changes involving the neural stem cell pool [26–28], as well as non-cell autonomous changes affecting neural stem cell niche [29] have been considered.
Molecular cascades connecting exposure to ethanol with the defects in NSC proliferation, differentiation and survival that overall result in impaired developmental and adult neurogenesis are still elusive. A reduction of brain-derived neurotrophic factor (BDNF), a major neurogenic neurotrophin, has been reported in plasma of alcohol-addicted patients [30]. Consistently, BDNF as well as insulin-like growth factor-1 have been shown to ameliorate the inhibition of rat embryonic NSC differentiation induced by ethanol in vitro (20–100 mM) [31]. Moreover, physical exercise, that reportedly increases hippocampal BDNF, was able to attenuate the long-lasting hippocampal neurogenic deficits in a rat model of FASD [32]. Downstream of neurotrophin receptors, the mammalian target of rapamycin (mTOR) and its effectors have been recognized key roles in the modulation of NSC functions [33], but their specific involvement in ethanol effects on neurogenesis have been little investigated. Ethanol metabolism promotes the microsomal and mitochondrial generation of ROS in several cell models including stem/progenitor cells [34]; on the other hand, increased levels of oxygen species inhibit mTOR activity and promote autophagy in neurons via a peroxisome–tuberous sclerosis complex 2 circuitry [35]. Thus, ethanol-induced proliferative defects of NSC involve impaired signaling capacity along the mTOR cascade. With this respect, it is of note that ethanol activates autophagy in the developing brain, and that autophagic preconditioning alleviates ethanol-induced ROS and neuronal damage [36].
Liver stem/progenitor cells
Alcohol consumption causes a wide spectrum of hepatic disorders ranging from mild fatty liver (steatosis) to more severe steatohepatitis, progressive fibrosis, cirrhosis and hepatocellular carcinoma, which are collectively recognized as alcoholic liver disease (ALD) [37]. The high prevalence of ALD has a deep impact on public health; nonetheless, the pathogenesis of the disease remains poorly understood. Alcohol-induced alteration of the intestinal barrier integrity results in the translocation of bacteria, endotoxins and peptidoglycans into the systemic and portal circulation, potentially promoting liver inflammation and injury; this hepatic response to intestinal inflammation is known as the gut-liver axis [38]. Liver responds to an insult inducing mature hepatocytes proliferation; therefore, physiologic hepatic regeneration occurs with minimal involvement from liver stem cells. Hepatic ethanol metabolism increases the production of reactive oxygen species, which enhance oxidative stress and inhibit hepatocyte proliferation [39]. Accordingly, both acute and chronic ethanol exposure impair liver regeneration [40]. Reduction of the capacity of the hepatocytes to replace damaged tissue parallels the induction of proliferation of the hepatic stem cells located in the Canals of Hering. This phenomenon, referred as ductular reaction, has been linked to alcohol hepatitis progression and severity [41], increased pro-fibrogenic response and tumor development [42].
In addition, in vitro studies suggest an hepatotoxic effect of alcohol exposure on hepatic stem cells [43]. Primary and immortalized human liver stem cells exposed in vitro to ethanol (tested dose range 25–100 mM, for 72 h) show reduced proliferation rate, decreased differentiation towards a hepatocyte phenotype and induction of mesenchymal transition [43]. Taken together, these results suggest that the effect of alcohol consumption on hepatic stem cells might be multifaceted: on the one hand, alcohol and/or its metabolites might exert their toxic effects directly on hepatocytes, damaging their function and limiting their proliferative capacity; on the other hand via the gut-liver axis alcohol might stimulate inflammatory signals leading to extensive proliferation of liver stem cells, which in turn promotes fibrosis at expense of hepatic regeneration.
Intestinal stem cells
Alcohol ingestion causes alteration of the intestinal microbiota composition and the disruption of intestinal barriers promoting local and systemic inflammation and tissue injury [44]. Intestinal epithelium cells’ turnover is rapid, supported by continuous replication of undifferentiated intestinal stem cells located within the crypts, which generate cells undergoing subsequent differentiation during the migration along the crypt-villus axis [45]. Intestinal damage persists long after alcohol consumption, suggesting that the damage may involve intestinal stem cells [46]. In vivo studies on a mouse model of alcohol chronic consumption and ex vivo organoid culture, demonstrated that alcohol exposure impairs intestinal stem-cell homeostasis, reducing their proliferation rate via deregulation of the β-catenin pathway [46]. Interestingly, alcohol exposure also significantly modifies the expression of intestinal stem-cell markers, including the leucine-rich repeat-containing G-protein coupled receptor 5 (Lgr5), which is known to be required to maintain the adult intestine epithelial cell proliferation [47]. Therefore, by limiting mucosal repair capacity alcohol-induced damage of intestinal stem cells may contribute to the alteration of intestinal barriers observed in acute and chronic drinkers [48].
Bone-marrow-derived mesenchymal stromal cells
Alcohol abuse is associated with impaired bone homeostasis leading to pathologic remodeling and impaired healing of bone fractures [49, 50]. Bone-marrow-derived stromal/stem cells are involved in the process of physiological maintenance of bones. Alcohol imbalances the process of bone remodeling by impairing bone-marrow stromal cell osteoblastic differentiation and promoting adipogenesis, therefore, contributing to bone loss. Mechanistically, alcohol and its main metabolite acetaldehyde affect the redox state of mesenchymal stem cell niche determining the downregulation of the Wnt/β-catenin signaling pathway, which directs osteoblast and chondrocyte cells differentiation from a common mesenchymal stem cell precursor [34, 51–53]. Deregulation of Wnt signaling due to alcohol exposure before bone injury persists up to 2 week post-fracture. Consequently, differentiation of mesenchymal precursors into bone and cartilage-forming cells is impaired, inhibiting the formation of the external callus [54].
A crosstalk between the Wnt/β-catenin and the mammalian target of rapamycin (mTOR) signaling has been identified in maintenance of bone-marrow-derived [55] and epithelial stem cells [56]. Alcohol impairs bone-marrow-derived mesenchymal cells osteogenic differentiation by activation of the mTOR pathway [57], consistently with a similar effect observed on odontoblastic differentiation of dental pulp cells [58]. Moreover, in vitro exposure to 50 mM ethanol promotes a shift in bone-marrow stromal cell differentiation towards the adipocyte lineage via up-regulation of the peroxisome proliferator-activated receptor (PPAR)γ2 signaling [59].
Interestingly, the effects of chronic alcohol intoxication on bone remodeling are not permanent and can be improved by abstinence [60]. A better understanding of the molecular pathways involved in the development of alcohol-induced bone disease may help the identification of targets for pharmacological therapies. For instance, treatment with mTOR inhibitors such as rapamycin might be useful for reducing the impact of alcohol-induced bone disease [57].
Dental pulp stem cells
Alcohol abuse, in association with other co-morbidity factors such as poor nutrition, vitamin deficiencies, and smoking, may lead to periodontal disease [61]. Dental mesenchymal stromal cells contribute to tooth homeostasis and repair of damaged dentine. These cells are present in adult dental pulp and can differentiate into osteogenic and odontogenic lineages depositing mineral matrix and trans-differentiate into neuronal cells [62]. Acute exposure of cultured human dental pulp stem cells to increasing concentration of ethanol (tested dose range 1–50 mM, for 24–48 h) results in transcriptional changes [63] and in DNA methylation pattern alterations [64]. Specifically, ethanol exposure reduces the expression profile of genes involved in the mineralization process, such as alkaline phosphatase, bone morphogenic protein 2 and 4, osteocalcin and osteopontin. The mammalian target of rapamycin (mTOR) plays a pivotal role in regulating proliferation and cell fate of mesenchymal stromal cells [65]. Accordingly, ethanol-mediated activation of the mTOR signaling pathway reduces odontoblastic differentiation of dental pulp cells [58]. Moreover, ethanol exposure leads to significant dysregulation of the lysine specific histone demethylase 6B (KDM6B) that epigenetically regulates odontogenic differentiation of dental mesenchymal stromal cells [66]. Therefore, epigenetic changes leading to altered gene expression profile may represent one of the molecular mechanisms underlying the effect on dental mesenchymal stromal cells contributing to ethanol-associated periodontal disease.
Adventitial progenitor cells
The vessel wall contains a heterogeneous population of stem cells, referred as adventitial stem/progenitor cells, able to differentiate into vascular and non-vascular cells [67]. These stem cells are involved in the process of vascular remodeling in response to arterial injury and disease. Alcohol consumption has a complex effect on the cardiovascular system; several evidences indicate that low drinking is associated with a beneficial effect on the pathophysiologic mechanisms involved in most cardiovascular disorders [3], while alcohol abuse has been linked to an increased risk [68]. Interestingly, Fitzpatrick et al. has recently demonstrated on a murine model that ethanol exposure equivalent to two drinks daily reduces stem cell antigen (Sca)-1 positive adventitial progenitor-cell proliferation via inhibition of the sonic hedgehog pathway [69]. Therefore, moderate drinking, acting on vascular stem cells, may contribute in attenuating pathologic arterial remodeling [70]. However, possible positives effect of moderate drinking on the cardiovascular system might be outweighed by the harmful impact of alcohol on other tissues and organs, implying that “no level of alcohol consumption improves health” [4, 71].
Embryonic and induced pluripotent stem cells
Embryonic stem cells (ESCs), which are derived from the inner cell mass of blastocysts, and induced pluripotent stem cells (iPSCs), which are adult cells genetically reprogrammed to an embryonic stem cell-like state, represent attractive in vitro models for the study of human developmental studies [72, 73]. Alcohol exposure alters the gene expression and methylation profiles in ESCs [74]. Human embryonic cells can model the ethanol-mediated developmental toxicity [75, 76] and different lines of evidence consistently show that alcohol exposure deregulate the differentiation properties of ESCs derived from both murine and primate sources. In particular, human ESCs hepatic differentiation is impaired by alcohol-mediated inhibition (tested dose range 25–100 mM) of the mitogen-activated protein kinase/extracellular-signal-regulated kinase (MAPK/ERK) and WNT signaling pathways [77]. Similarly, ethanol (tested dose range 17.1–51.4 mM) suppresses cardiac differentiation of murine ESCs by inhibiting Wnt signaling [78, 79]. In addition, neurological differentiation of ESCs is compromised by ethanol exposure (tested dose range 25–100 mM) via alteration of the equilibrium of the expression of Sox2, Oct4, and Nanog [80, 81]. In addition, alcohol exposure induces gene expression changes in hESC-derived cortical neurons, including a significant up-regulation of N-methyl-d-aspartate (NMDA) receptor subunit gene expression [82]. Alcohol-mediated changes in NMDA receptor function was also assessed in iPS-derived neural cells [83], indicating that iPSCs may offer a novel approach for better understanding the molecular mechanisms of alcohol use disorders [73, 84]. Exposure of iPSc to alcohol (100 mM) was also demonstrated to induce apoptosis and impair hepatic differentiation [85].
Collectively these data suggest that ESCs are more sensitive to ethanol than differentiated cells [75, 86] providing a possible mechanism by which prenatal alcohol exposure exerts its toxic effect on different target organs. It should be considered that during physiological embryonic development, ESCs are present for a limited period, so the effect of alcohol on development may be directly due to the effect on ESCs but most probably also on their progeny at different stages of differentiation [86].
Hematopoietic stem cells
Alcoholic patients may experience anemia, bleeding disorders, and compromised immune response [87]. Alterations in the hematologic profile have been also observed in short-term moderate alcohol drinkers. Hematopoiesis is a coordinated process of cell proliferation, self-renewal, and differentiation from a small population of bone-marrow (BM) hematopoietic stem cells (HSCs) to lineage-specific terminally differentiated cells. Nutritional deficiencies associated with alcoholism may negatively influence the production and function of various blood cells. On the other hand, direct effects of alcohol toxicity may target the BM, leading to the generation of abnormal blood cell precursors that cannot mature into functional cells [87]. In line with this hypothesis, the formation of vacuoles, which interfere with cells’ functionality, has been observed in red and white blood cells precursors [88]. In physiological conditions only a small fraction of HSCs enter cell cycling for self-renewal and/or proliferation, while the majority are maintained in the quiescent state. Prolonged quiescence exposes HSCs to endogenous and exogenous genotoxic agents promoting accumulation of a severe mutation burden with harmful effects, possibly leading to anemia, increased risk of developing cancer and cellular ageing [89]. Alcohol as such is not mutagenic but its metabolism produces ROS and acetaldehyde, that is mutagenic and carcinogenic via induction of DNA damage, interference with DNA replication and formation of DNA adducts [90]. It has been elegantly demonstrated that endogenous aldehydes, such as the ones produced during ethanol metabolism, are genotoxic to cells of the hematopoietic system. In the absence of the protective role of the Fanconi anemia DNA repair pathway and the activity of an isoform of aldehyde dehydrogenase (ALDH), the genotoxic effect of acetaldehyde results in a severe depletion of the HSC pool [91]. The same authors extended their findings establishing a key role of p53 in response to aldehyde-induced DNA damage to promote HSCs loss [92]. Collectively, the seminal work performed by Garaycoechea and collaborators improved our knowledge on the impact of alcohol consumption on human health, providing the molecular link between alcohol exposure and HSC damage. Consistently, formaldehyde produced by the metabolism of methanol, which may be also present in alcoholic beverages, exerts a genotoxic effect on HSCs [93].
Alcoholic patients may experience also reduced granulocyte levels and show weakened host immune defense against bacterial infection [94]. It has been demonstrated that alcohol administration alters the molecular cues needed for HSC activation and production of granulocytes, compromising the immune response against pathogens [95, 96]. In addition, in utero alcohol exposure affects the transcriptional regulation of B cell development from hematopoietic progenitors [97].
Hematopoiesis also involves the interaction of the developing cells with the BM stroma, which provides the microenvironment suitable for cells differentiation. Besides damaging HSC directly ethanol could affect the BM progenitor cells also in an indirect fashion by altering their microenvironment. Alcohol has a detrimental effect also on BM stromal cells, which has been associated with the reduction of bone mass and decreased bone formation observed in alcoholics [52]. In addition, alcohol-mediated liver injury promotes mobilization of BM-derived CD34+ stem cells which mainly contain hematopoietic and endothelial progenitor cells. Hepatic recruitment of CD34+ stem cells correlates with liver fibrosis [98]. Therefore, alcohol promotes dysfunctional hematopoiesis acting on bone-marrow cells at various stages of lineage commitment.
Cancer stem cells
Alcohol beverages consumption is classified as carcinogenic by the World Health Organization. In particular, acetaldehyde, the first compound of alcohol metabolism, is a known carcinogen and a key generator of free radicals which can promote cancer development through multiple mechanisms [99]. Ethanol exposure results in reduction of inflammatory mediators, with immunologic alterations leading to reduced healing after traumatic injury, increased susceptibility to infection and tumor formation in the upper aero-digestive tract, colorectum, liver and breast [100]. It has been estimated that approximately 6% of all cancer deaths are attributable to alcohol, with a loss of about 19 years of potential life for each victim [101]. Alcohol may influence cancer incidence by modulating the initiation, promotion, progression or metastasis of tumors. Suggested mechanisms by which alcohol consumption increases the risk of cancer include: a tumorigenic effect of the ethanol metabolite acetaldehyde; increased levels of estrogen, which can cause breast cancer; liver cirrhosis leading to hepatocellular carcinoma; increased level of reactive oxygen species, which may damage DNA; inhibition of DNA methylation; higher solubility of tobacco carcinogenic chemicals in the mouth and throat; adverse effect on folate metabolism, with increased risk of colorectal cancer; direct or indirect alteration of oncogenic or regulatory pathways [100]. The exact cellular and molecular processes and their contribution to alcohol-associated carcinogenesis are not fully elucidated [99]. Interestingly, in a mouse model of ethanol intoxication, loss of the tumor suppressor p53 promoted alcohol-induced dysplastic changes while abrogating cell death, suggesting that p53-dependent apoptosis restrains the tumorigenic effect of ethanol on liver cells [102].
According to the cancer stem cell hypothesis, only a small subgroup of tumorigenic stem-like cells within a highly heterogeneous cancerous cell population initiates and drives tumor growth [103]. These cells, referred also as tumor-initiating cells, have characteristics similar to normal adult stem cells having both the capacity to self-renew and to differentiate into multiple cell types. Studies aimed at the identification and analysis of cancer stem cells are limited by the lack of specific cancer stem-cell markers [104]. Nonetheless, it has been proposed that alcohol may impinge on cancer stem-cell properties [105, 106]. The molecular mechanism by which ethanol metabolism contributes to tumorigenesis may be associated to the production of ROS which play a pivotal role in cancer stem-cell maintenance and differentiation [105, 107]. Indeed, alcohol promotes migration, invasion and propagation of breast cancer stem cell population via the ErbB2/p38γ MAPK axis [108]. Alcohol-mediated induction of hepatic cancer stem cells via the activation of the toll-like receptor 4 (TLR4)-Nanog pathway has also been described [109]. Moreover, a possible role of alcohol in promoting expansion of a cancer stem cell-like population in oro-esophageal squamous cell carcinoma has been recently postulated [110]. Cancer stem-cell-directed therapeutic approaches might represent an important strategy to improve cancer therapy. Therefore, improved knowledge of how and to which extent cancer stem cell biology is modified by alcohol may prove valuable for reducing the risk of ethanol-induced tumors.
Alcohol toxicity on stem cells: in search for molecular mechanisms
Despite intensive research, the mechanisms leading to alcohol toxicity are still largely unclear. In the following sections, we review the main putative mechanisms by which alcohol might exert negative effects on stem cells (Fig. 2).
Increased production of reactive oxygen species
Endogenous reactive metabolites, such as ROS and aldehydes produced during ethanol metabolism, are key players in induction of mutagenesis and ageing. In particular, high cellular levels of ROS can be detrimental, leading to lipid peroxidation and DNA damage. Alcohol intake can lead to ROS production by several mechanisms including ethanol and acetaldehyde oxidation by the ADH and ALDH, cytochrome P450 2E1 (CYP2E1) induction, raise in the cellular amount of free iron, conversion of xanthine dehydrogenase to xanthine oxidase [111]. Increased ROS production, impaired levels of antioxidant defense and consequent induction of oxidative stress have a causative role in FASD [112]. On the other hand, ROS are implicated in the long-term maintenance of different stem cell pools, regulating stem cell renewal, commitment and differentiation [113]. The overall amount of ROS in stem cells is determined by the balance between production and scavenging systems finely tuned by complex regulatory mechanisms. Therefore, alcohol alteration of the ROS balance may lead to functional stem cell decline which may affect organ and tissue development and regeneration [114].
Role of the mammalian target of rapamycin
The mTOR–mitochondria–ROS axis plays a pivotal role in regulating stem-cell quiescence and self-renewal [115]. Ethanol activation of mTOR has been described in different stem cells leading to impaired differentiation [57, 58]. Moreover, in a mouse model of tuberous sclerosis, deregulated mTOR signaling led to enhanced generation of subventricular zone neural progeny, followed by premature differentiation and impaired maturation during both embryonic and postnatal development [116], a phenotype somehow reminiscent of neurogenic changes described in young mice following prenatal exposure to ethanol [24]. Furthermore, mTOR-dependent inhibition of autophagy promotes proinflammatory signaling via reduced inflammasome clearance [117]. Along these lines it has been recently reported that ethanol exposure (70 mM) activates the NLRP3 inflammasome in induced pluripotent stem cells (iPSCs) and iPSC-derived neural progenitor cells [118]. These results suggest that inflammation, a hallmark of alcohol-mediated tissue damage, may also participate in neurogenesis derangement by ethanol. Taken together, the above cues strongly call for further research in the role of the mTOR cascade, amenable of pharmacological control, in ethanol effects on NSC function and by extension on ethanol-related stem cell failure.
Effects on nicotinamide adenine dinucleotide
Hepatic ethanol oxidation causes a significant change of the ratio between the oxidized and reduced forms of nicotinamide adenine dinucleotide (NAD+/NADH), leading to altered gene expression and epigenetic changes [119, 120]. Interestingly, it has been demonstrated that low levels of NAD+ determine a reduction of self-renewal and differentiation capabilities of neural stem cells [121]. Consistently, NAD+ repletion has been associated with improved retention of muscular, neural and melanocyte stem cell pools in aged mice [122] and with attenuation of alcohol-associated hepatic lesions [123]. NAD+ beneficial effects likely involve several NAD-dependent pathways and effectors, including sirtuins, a class of protein deacylase extensively linked to extended longevity in model organisms and to health span in mammals through antioxidant, prosurvival and metabolism-regulating functions [124]. Interestingly, sirtuins have been identified as potential targets of ethanol in both animal and human models of hepatocellular carcinoma [125, 126]. In conclusion, by causing a reduction of the intracellular NAD+ levels ethanol may negatively impact on the preservation of adult stem cells and by extension on tissue regenerative capacity, while pharmacologic treatments aiming at increasing intracellular NAD+ content may help to prevent stem-cell functional decline upon alcohol intake.
Acetaldehyde production and aldehyde dehydrogenases 2 activity
Ethanol metabolism produces acetaldehyde which is genotoxic, interferes with DNA replication, induces DNA damage and formation of DNA adducts [127]. Different, partially redundant, DNA repair mechanisms have been evolved to protect cells from DNA damage. In particular, the Fanconi anemia pathway is involved in the repair of DNA damage induced by acetaldehyde. Concomitant inactivation of the Fanconi anemia DNA repair pathway and the aldehyde catabolism enzyme ALDH2 results in HSC chromosome damage and loss [91, 92, 128]. This observation, originally demonstrated on murine models, was clinically corroborated by the discovery of a higher prevalence of bone-marrow failure in patients affected by Fanconi anemia harboring also a dominant negative polymorphism in the ALDH2 gene which is frequent in the Asian population [129]. Moreover, the expression BRCA1 and BRCA2 tumor suppressors genes, known to contribute to DNA repair [130], has been associated to a protective role against endogenous acetaldehyde toxicity [131]. Consequently, endogenous aldehydes may be implicated in triggering carcinogenesis in BRCA2 mutation carriers [132].
The mitochondrial ALDH2 is the member of the aldehyde dehydrogenase (ALDH) family which provides the main detoxification activity against acetaldehyde. Moreover, ALDH affects HSCs self-renewal via inhibition of the retinoic acid signaling [133]. Noteworthy, elevated ALDH expression has been reported also in tumor-initiating cells, suggesting a functional role of ALDH activity in determining resistance to current cancer therapies and promoting expansion of cancer stem cells [134]. Therefore, aldehyde dehydrogenase activity has a key role in stem-cell self-protection, maintenance and differentiation. Exposure to ethanol is likely to alter ALDH2 expression levels and functions in stem cells as observed in esophageal epithelium [135]; along similar lines of speculation, it is possible that diverse ALDH levels in subpopulations of stem cells may dictate unique vulnerability to alcohol damage, affecting the dynamic of cell proliferation and cell fate.
Effects on cell membrane and extracellular matrix
Cell membrane-mediated interactions play a pivotal role in regulating stem cell proliferation and differentiation [136]. Ethanol interacts both with the phospholipids and proteins of the plasma membrane, thereby affecting cell structure and function [137]. Furthermore, ROS production associated with alcohol metabolism results in lipid peroxidation, further affecting membrane behavior. In addition, several studies have demonstrated that alcohol deregulates the extracellular matrix (ECM) deposition in different organs including liver, brain, skeletal and cardiac muscle [138–140]. Stem cells rely on mechanical cues from their niche to drive and regulate cell fate [141, 142]. Therefore, by modifying cell membrane fluidity, inducing conformational changes in membrane proteins and altering ECM remodeling alcohol may perturb stem cell maintenance and differentiation.
Epigenetic mechanisms and microRNAs
Stem-cell differentiation is a strictly orchestrated process involving multiple regulatory pathways. A complex network of soluble factors such as cytokines, hormones and growth factors, regulates stem cell fate [143]. Alcohol intake is known to disrupt cytokine balance and functions, possibly interfering with stem cell proliferation and differentiation [144]. In addition, dynamic epigenetic mechanisms such as histone modifications, changes in DNA methylation, chromatin remodeling, and non-coding RNAs signaling, play a significant role in stem-cell control of self-renewal and differentiation into tissue-specific lineages [145]. Alcohol metabolism has a profound impact on cellular gene expression via modification in the epigenetic machinery [119, 146, 147]. Extensive epigenetic alteration subsequent to alcohol exposure may interfere with the molecular switches needed for the coordinated process of stem cell differentiation. Indeed, perturbation of the epigenetic profile by alcohol exposure leads to alteration of gene expression of specific genes implicated in neuronal stem-cell maintenance and differentiation [148, 149]. Alteration of chromatin structure promoted by prenatal alcohol exposure has been linked to altered neuron and astrocyte differentiation and FASD [27]. In contrast, a recent large cohort study failed to detect any evidence that maternal alcohol consumption during pregnancy is associated with offspring cord blood DNA methylation [150]. Therefore, the role of epigenetic changes and chromatin structure in the context of FASD is far from being fully elucidated.
In addition, broad alcohol‐mediated changes in microRNA (miRNA) and miRNA‐target gene expression have been observed in utero, possibly contributing to the harmful effects on the developing fetus [151]. Consequently, it has been proposed that alcohol-sensitive circulating miRNAs may represent a promising theranostic marker for FASD [152]. Interestingly, alcohol intake can promote defined changes in the content of miRNA enclosed into extracellular vesicles (EVs) [153], which play a pivotal role in intracellular communication. Therefore, EV cargo analysis might represent a sensitive tool for monitoring progression of alcohol addiction disorders [154].
Conclusions
Emerging evidence for the impact of ethanol on stem and progenitor cells has added a new layer of biological complexity to our understanding of how alcohol misuse affects adult and developing tissues and especially fetal brain. However, the underlying biochemical mechanisms appear manifold, complex and overall incompletely identified. Hopefully, intense research aimed at delineating the pathogenic molecular interactions that link ethanol intake to stem-cell damage will in the next few years provide the immediate benefit of uncovering the processes leading (or at least contributing) to alcohol toxicity. This will be in turn instrumental to develop novel therapeutic strategies to reverse or prevent the effects of alcohol intoxication.
Acknowledgements
The work was supported by ERAB: the European Foundation for Alcohol Research (Grant # EA 17 19 to G.T.). We gratefully acknowledge also Ministero della Salute (Ricerca Finalizzata Grant # RF-2011-02347907 to G.T.) and Istituto Regina Elena Cinque per Mille (IRE 5x1000 2014).
Glossary
- ADH
Alcohol dehydrogenase
- ALD
Alcoholic liver disease
- ALDH
Acetaldehyde dehydrogenase
- BM
Bone marrow
- CYP2E1
Cytochrome P450 2E1
- DG
Dentate gyrus
- ESC
Embryonic stem cells
- EV
Extracellular vesicles
- FASD
Fetal alcohol spectrum disorders
- HSC
Hematopoietic stem cells
- MSC
Mesenchymal stromal cells
- mTOR
Mammalian target of rapamycin
- NADH
Nicotinamide adenine dinucleotide
- NSC
Neural stem and progenitor cells
- PPAR
Peroxisome proliferator-activated receptor
- ROS
Reactive oxygen species
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Poznyak V, Fleischmann A, Rekve D, Rylett M, Rehm J, Gmel G. The World Health Organization’s global monitoring system on alcohol and health. Alcohol Res. 2013;35:244–249. doi: 10.35946/arcr.v35.2.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rehm J, Baliunas D, Borges GL, Graham K, Irving H, Kehoe T, Parry CD, Patra J, Popova S, Poznyak V, et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction. 2010;105:817–843. doi: 10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sacco RL, Elkind M, Boden-Albala B, Lin IF, Kargman DE, Hauser WA, Shea S, Paik MC. The protective effect of moderate alcohol consumption on ischemic stroke. JAMA. 1999;281:53–60. doi: 10.1001/jama.281.1.53. [DOI] [PubMed] [Google Scholar]
- 4.Collaborators GA. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:1015–1035. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou Y, Zheng J, Li S, Zhou T, Zhang P, Li HB. Alcoholic beverage consumption and chronic diseases. Int J Environ Res Public Health. 2016;13:522. doi: 10.3390/ijerph13060522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crabb DW, Matsumoto M, Chang D, You M. Overview of the role of alcohol dehydrogenase and aldehyde dehydrogenase and their variants in the genesis of alcohol-related pathology. Proc Nutr Soc. 2004;63:49–63. doi: 10.1079/PNS2003327. [DOI] [PubMed] [Google Scholar]
- 7.Cederbaum AI. Alcohol metabolism. Clin Liver Dis. 2012;16:667–685. doi: 10.1016/j.cld.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahnke AH, Salem NA, Tseng AM, Fincher AS, Klopfer A, Miranda RC. Fetal alcohol spectrum disorders: a stem-cellopathy? In: Rasmussen TP, editor. Stem cells in birth defects research and developmental toxicology. Hoboken: Wiley; 2018. [Google Scholar]
- 9.Cheung TH, Rando TA. Molecular regulation of stem cell quiescence. Nat Rev Mol Cell Biol. 2013;14:329–340. doi: 10.1038/nrm3591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vangipuram SD, Lyman WD. Ethanol alters cell fate of fetal human brain-derived stem and progenitor cells. Alcohol Clin Exp Res. 2010;34:1574–1583. doi: 10.1111/j.1530-0277.2010.01242.x. [DOI] [PubMed] [Google Scholar]
- 11.Boldrini M, Fulmore CA, Tartt AN, Simeon LR, Pavlova I, Poposka V, Rosoklija GB, Stankov A, Arango V, Dwork AJ, et al. Human hippocampal neurogenesis persists throughout aging. Cell Stem Cell. 2018;22:589–599.e585. doi: 10.1016/j.stem.2018.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sorrells SF, Paredes MF, Cebrian-Silla A, Sandoval K, Qi D, Kelley KW, James D, Mayer S, Chang J, Auguste KI, et al. Human hippocampal neurogenesis drops sharply in children to undetectable levels in adults. Nature. 2018;555:377–381. doi: 10.1038/nature25975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spalding KL, Bergmann O, Alkass K, Bernard S, Salehpour M, Huttner HB, Boström E, Westerlund I, Vial C, Buchholz BA, et al. Dynamics of hippocampal neurogenesis in adult humans. Cell. 2013;153:1219–1227. doi: 10.1016/j.cell.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gage FH, Temple S. Neural stem cells: generating and regenerating the brain. Neuron. 2013;80:588–601. doi: 10.1016/j.neuron.2013.10.037. [DOI] [PubMed] [Google Scholar]
- 15.Nixon K. Alcohol and adult neurogenesis: roles in neurodegeneration and recovery in chronic alcoholism. Hippocampus. 2006;16:287–295. doi: 10.1002/hipo.20162. [DOI] [PubMed] [Google Scholar]
- 16.Campbell JC, Stipcevic T, Flores RE, Perry C, Kippin TE. Alcohol exposure inhibits adult neural stem cell proliferation. Exp Brain Res. 2014;232:2775–2784. doi: 10.1007/s00221-014-3958-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Le Maître TW, Dhanabalan G, Bogdanovic N, Alkass K, Druid H. Effects of alcohol abuse on proliferating cells, stem/progenitor cells, and immature neurons in the adult human hippocampus. Neuropsychopharmacology. 2018;43:690–699. doi: 10.1038/npp.2017.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crews FT, Mdzinarishvili A, Kim D, He J, Nixon K. Neurogenesis in adolescent brain is potently inhibited by ethanol. Neuroscience. 2006;137:437–445. doi: 10.1016/j.neuroscience.2005.08.090. [DOI] [PubMed] [Google Scholar]
- 19.Nixon K, Crews FT. Binge ethanol exposure decreases neurogenesis in adult rat hippocampus. J Neurochem. 2002;83:1087–1093. doi: 10.1046/j.1471-4159.2002.01214.x. [DOI] [PubMed] [Google Scholar]
- 20.Rice AC, Bullock MR, Shelton KL. Chronic ethanol consumption transiently reduces adult neural progenitor cell proliferation. Brain Res. 2004;1011:94–98. doi: 10.1016/j.brainres.2004.01.091. [DOI] [PubMed] [Google Scholar]
- 21.Nixon K, Crews FT. Temporally specific burst in cell proliferation increases hippocampal neurogenesis in protracted abstinence from alcohol. J Neurosci. 2004;24:9714–9722. doi: 10.1523/JNEUROSCI.3063-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jessberger S, Parent JM. Epilepsy and adult neurogenesis. Cold Spring Harb Perspect Biol. 2015 doi: 10.1101/cshperspect.a020677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamilton GF, Bucko PJ, Miller DS, DeAngelis RS, Krebs CP, Rhodes JS. Behavioral deficits induced by third-trimester equivalent alcohol exposure in male C57BL/6J mice are not associated with reduced adult hippocampal neurogenesis but are still rescued with voluntary exercise. Behav Brain Res. 2016;314:96–105. doi: 10.1016/j.bbr.2016.07.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gil-Mohapel J, Boehme F, Patten A, Cox A, Kainer L, Giles E, Brocardo PS, Christie BR. Altered adult hippocampal neuronal maturation in a rat model of fetal alcohol syndrome. Brain Res. 2011;1384:29–41. doi: 10.1016/j.brainres.2011.01.116. [DOI] [PubMed] [Google Scholar]
- 25.Gil-Mohapel J, Titterness AK, Patten AR, Taylor S, Ratzlaff A, Ratzlaff T, Helfer J, Christie BR. Prenatal ethanol exposure differentially affects hippocampal neurogenesis in the adolescent and aged brain. Neuroscience. 2014;273:174–188. doi: 10.1016/j.neuroscience.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 26.Ungerer M, Knezovich J, Ramsay M. In utero alcohol exposure, epigenetic changes, and their consequences. Alcohol Res. 2013;35:37–46. doi: 10.35946/arcr.v35.1.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gavin DP, Grayson DR, Varghese SP, Guizzetti M. Chromatin switches during neural cell differentiation and their dysregulation by prenatal alcohol exposure. Genes (Basel) 2017;8:137. doi: 10.3390/genes8050137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burrowes SG, Salem NA, Tseng AM, Balaraman S, Pinson MR, Garcia C, Miranda RC. The BAF (BRG1/BRM-Associated Factor) chromatin-remodeling complex exhibits ethanol sensitivity in fetal neural progenitor cells and regulates transcription at the miR-9-2 encoding gene locus. Alcohol. 2017;60:149–158. doi: 10.1016/j.alcohol.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gil-Mohapel J, Boehme F, Kainer L, Christie BR. Hippocampal cell loss and neurogenesis after fetal alcohol exposure: insights from different rodent models. Brain Res Rev. 2010;64:283–303. doi: 10.1016/j.brainresrev.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 30.Zanardini R, Fontana A, Pagano R, Mazzaro E, Bergamasco F, Romagnosi G, Gennarelli M, Bocchio-Chiavetto L. Alterations of brain-derived neurotrophic factor serum levels in patients with alcohol dependence. Alcohol Clin Exp Res. 2011;35:1529–1533. doi: 10.1111/j.1530-0277.2011.01489.x. [DOI] [PubMed] [Google Scholar]
- 31.Tateno M, Ukai W, Ozawa H, Yamamoto M, Toki S, Ikeda H, Saito T. Ethanol inhibition of neural stem cell differentiation is reduced by neurotrophic factors. Alcohol Clin Exp Res. 2004;28:134S–138S. doi: 10.1097/01.ALC.0000133538.40841.36. [DOI] [PubMed] [Google Scholar]
- 32.Redila VA, Olson AK, Swann SE, Mohades G, Webber AJ, Weinberg J, Christie BR. Hippocampal cell proliferation is reduced following prenatal ethanol exposure but can be rescued with voluntary exercise. Hippocampus. 2006;16:305–311. doi: 10.1002/hipo.20164. [DOI] [PubMed] [Google Scholar]
- 33.Tee AR, Sampson JR, Pal DK, Bateman JM. The role of mTOR signalling in neurogenesis, insights from tuberous sclerosis complex. Semin Cell Dev Biol. 2016;52:12–20. doi: 10.1016/j.semcdb.2016.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen X, Li M, Yan J, Liu T, Pan G, Yang H, Pei M, He F. Alcohol induces cellular senescence and impairs osteogenic potential in bone marrow-derived mesenchymal stem cells. Alcohol Alcohol. 2017;52:289–297. doi: 10.1093/alcalc/agx006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang J, Kim J, Alexander A, Cai S, Tripathi DN, Dere R, Tee AR, Tait-Mulder J, Di Nardo A, Han JM, et al. A tuberous sclerosis complex signalling node at the peroxisome regulates mTORC1 and autophagy in response to ROS. Nat Cell Biol. 2013;15:1186–1196. doi: 10.1038/ncb2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luo J. Autophagy and ethanol neurotoxicity. Autophagy. 2014;10:2099–2108. doi: 10.4161/15548627.2014.981916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Magdaleno F, Blajszczak CC, Nieto N. Key events participating in the pathogenesis of alcoholic liver disease. Biomolecules. 2017 doi: 10.3390/biom7010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stärkel P, Leclercq S, de Timary P, Schnabl B. Intestinal dysbiosis and permeability: the yin and yang in alcohol dependence and alcoholic liver disease. Clin Sci (Lond) 2018;132:199–212. doi: 10.1042/CS20171055. [DOI] [PubMed] [Google Scholar]
- 39.Dey A, Cederbaum AI. Alcohol and oxidative liver injury. Hepatology. 2006;43:S63–74. doi: 10.1002/hep.20957. [DOI] [PubMed] [Google Scholar]
- 40.Wands JR, Carter EA, Bucher NL, Isselbacher KJ. Effect of acute and chronic ethanol intoxication on hepatic regeneration. Adv Exp Med Biol. 1980;132:663–670. doi: 10.1007/978-1-4757-1419-7_69. [DOI] [PubMed] [Google Scholar]
- 41.Sancho-Bru P, Altamirano J, Rodrigo-Torres D, Coll M, Millán C, José Lozano J, Miquel R, Arroyo V, Caballería J, Ginès P, et al. Liver progenitor cell markers correlate with liver damage and predict short-term mortality in patients with alcoholic hepatitis. Hepatology. 2012;55:1931–1941. doi: 10.1002/hep.25614. [DOI] [PubMed] [Google Scholar]
- 42.Lukacs-Kornek V, Lammert F. The progenitor cell dilemma: cellular and functional heterogeneity in assistance or escalation of liver injury. J Hepatol. 2017;66:619–630. doi: 10.1016/j.jhep.2016.10.033. [DOI] [PubMed] [Google Scholar]
- 43.Shi X, Chang CC, Basson MD, Upham BL, Wei L, Zhang P. Alcohol disrupts human liver stem/progenitor cell proliferation and differentiation. J Stem Cell Res Ther. 2014 doi: 10.4172/2157-7633.1000205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Patel S, Behara R, Swanson GR, Forsyth CB, Voigt RM, Keshavarzian A. Alcohol and the intestine. Biomolecules. 2015;5:2573–2588. doi: 10.3390/biom5042573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Umar S. Intestinal stem cells. Curr Gastroenterol Rep. 2010;12:340–348. doi: 10.1007/s11894-010-0130-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lu R, Voigt RM, Zhang Y, Kato I, Xia Y, Forsyth CB, Keshavarzian A, Sun J. Alcohol injury damages intestinal stem cells. Alcohol Clin Exp Res. 2017;41:727–734. doi: 10.1111/acer.13351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–1007. doi: 10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- 48.Keshavarzian A, Fields JZ, Vaeth J, Holmes EW. The differing effects of acute and chronic alcohol on gastric and intestinal permeability. Am J Gastroenterol. 1994;89:2205–2211. [PubMed] [Google Scholar]
- 49.González-Reimers E, Quintero-Platt G, Rodríguez-Rodríguez E, Martínez-Riera A, Alvisa-Negrín J, Santolaria-Fernández F. Bone changes in alcoholic liver disease. World J Hepatol. 2015;7:1258–1264. doi: 10.4254/wjh.v7.i9.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chakkalakal DA. Alcohol-induced bone loss and deficient bone repair. Alcohol Clin Exp Res. 2005;29:2077–2090. doi: 10.1097/01.alc.0000192039.21305.55. [DOI] [PubMed] [Google Scholar]
- 51.Chen JR, Lazarenko OP, Shankar K, Blackburn ML, Badger TM, Ronis MJ. A role for ethanol-induced oxidative stress in controlling lineage commitment of mesenchymal stromal cells through inhibition of Wnt/beta-catenin signaling. J Bone Miner Res. 2010;25:1117–1127. doi: 10.1002/jbmr.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gong Z, Wezeman FH. Inhibitory effect of alcohol on osteogenic differentiation in human bone marrow-derived mesenchymal stem cells. Alcohol Clin Exp Res. 2004;28:468–479. doi: 10.1097/01.ALC.0000118315.58404.C1. [DOI] [PubMed] [Google Scholar]
- 53.Giuliani N, Girasole G, Vescovi PP, Passeri G, Pedrazzoni M. Ethanol and acetaldehyde inhibit the formation of early osteoblast progenitors in murine and human bone marrow cultures. Alcohol Clin Exp Res. 1999;23:381–385. doi: 10.1111/j.1530-0277.1999.tb04126.x. [DOI] [PubMed] [Google Scholar]
- 54.Lauing KL, Roper PM, Nauer RK, Callaci JJ. Acute alcohol exposure impairs fracture healing and deregulates β-catenin signaling in the fracture callus. Alcohol Clin Exp Res. 2012;36:2095–2103. doi: 10.1111/j.1530-0277.2012.01830.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huang J, Nguyen-McCarty M, Hexner EO, Danet-Desnoyers G, Klein PS. Maintenance of hematopoietic stem cells through regulation of Wnt and mTOR pathways. Nat Med. 2012;18:1778–1785. doi: 10.1038/nm.2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Castilho RM, Squarize CH, Chodosh LA, Williams BO, Gutkind JS. mTOR mediates Wnt-induced epidermal stem cell exhaustion and aging. Cell Stem Cell. 2009;5:279–289. doi: 10.1016/j.stem.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Liu Y, Kou X, Chen C, Yu W, Su Y, Kim Y, Shi S. Chronic high dose alcohol induces osteopenia via activation of mTOR signaling in bone marrow mesenchymal stem cells. Stem Cells. 2016;34:2157–2168. doi: 10.1002/stem.2392. [DOI] [PubMed] [Google Scholar]
- 58.Qin W, Huang QT, Weir MD, Song Z, Fouad AF, Lin ZM, Zhao L, Xu HHK. Alcohol inhibits odontogenic differentiation of human dental pulp cells by activating mTOR signaling. Stem Cells Int. 2017;2017:8717454. doi: 10.1155/2017/8717454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wezeman FH, Gong Z. Adipogenic effect of alcohol on human bone marrow-derived mesenchymal stem cells. Alcohol Clin Exp Res. 2004;28:1091–1101. doi: 10.1097/01.ALC.0000130808.49262.F5. [DOI] [PubMed] [Google Scholar]
- 60.Peris P, Parés A, Guañabens N, Del Río L, Pons F, Martínez de Osaba MJ, Monegal A, Caballería J, Rodés J, Muñoz-Gómez J. Bone mass improves in alcoholics after 2 years of abstinence. J Bone Miner Res. 1994;9:1607–1612. doi: 10.1002/jbmr.5650091014. [DOI] [PubMed] [Google Scholar]
- 61.Tezal M, Grossi SG, Ho AW, Genco RJ. The effect of alcohol consumption on periodontal disease. J Periodontol. 2001;72:183–189. doi: 10.1902/jop.2001.72.2.183. [DOI] [PubMed] [Google Scholar]
- 62.Sharpe PT. Dental mesenchymal stem cells. Development. 2016;143:2273–2280. doi: 10.1242/dev.134189. [DOI] [PubMed] [Google Scholar]
- 63.Khalid O, Kim JJ, Duan L, Hoang M, Elashoff D, Kim Y. Genome-wide transcriptomic alterations induced by ethanol treatment in human dental pulp stem cells (DPSCs) Genom Data. 2014;2:127–131. doi: 10.1016/j.gdata.2014.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hoang M, Kim JJ, Kim Y, Tong E, Trammell B, Liu Y, Shi S, Lee CR, Hong C, Wang CY. Alcohol-induced suppression of KDM6B dysregulates the mineralization potential in dental pulp stem cells. Stem Cell Res. 2016;17:111–121. doi: 10.1016/j.scr.2016.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martin SK, Fitter S, Dutta AK, Matthews MP, Walkley CR, Hall MN, Ruegg MA, Gronthos S, Zannettino AC. Brief report: the differential roles of mTORC1 and mTORC2 in mesenchymal stem cell differentiation. Stem Cells. 2015;33:1359–1365. doi: 10.1002/stem.1931. [DOI] [PubMed] [Google Scholar]
- 66.Xu J, Yu B, Hong C, Wang CY. KDM6B epigenetically regulates odontogenic differentiation of dental mesenchymal stem cells. Int J Oral Sci. 2013;5:200–205. doi: 10.1038/ijos.2013.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wörsdörfer P, Mekala SR, Bauer J, Edenhofer F, Kuerten S, Ergün S. The vascular adventitia: an endogenous, omnipresent source of stem cells in the body. Pharmacol Ther. 2017;171:13–29. doi: 10.1016/j.pharmthera.2016.07.017. [DOI] [PubMed] [Google Scholar]
- 68.Piano MR. Alcohol’s effects on the cardiovascular system. Alcohol Res. 2017;38:219–241. doi: 10.35946/arcr.v38.2.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fitzpatrick E, Han X, Liu W, Corcoran E, Burtenshaw D, Morrow D, Helt JC, Cahill PA, Redmond EM. Alcohol reduces arterial remodeling by inhibiting sonic hedgehog-stimulated stem cell antigen-1 positive progenitor stem cell expansion. Alcohol Clin Exp Res. 2017;41:2051–2065. doi: 10.1111/acer.13499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shirpoor A. Ethanol and the cardiovascular system: friend or enemy? Alcohol Clin Exp Res. 2018;42:244–247. doi: 10.1111/acer.13548. [DOI] [PubMed] [Google Scholar]
- 71.Burton R, Sheron N. No level of alcohol consumption improves health. Lancet. 2018;392:987–988. doi: 10.1016/S0140-6736(18)31571-X. [DOI] [PubMed] [Google Scholar]
- 72.Zhu Z, Huangfu D. Human pluripotent stem cells: an emerging model in developmental biology. Development. 2013;140:705–717. doi: 10.1242/dev.086165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Prytkova I, Goate A, Hart RP, Slesinger PA. Genetics of alcohol use disorder: a role for induced pluripotent stem cells? Alcohol Clin Exp Res. 2018;42:1572–1590. doi: 10.1111/acer.13811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Khalid O, Kim JJ, Kim HS, Hoang M, Tu TG, Elie O, Lee C, Vu C, Horvath S, Spigelman I, et al. Gene expression signatures affected by alcohol-induced DNA methylomic deregulation in human embryonic stem cells. Stem Cell Res. 2014;12:791–806. doi: 10.1016/j.scr.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nash R, Krishnamoorthy M, Jenkins A, Csete M. Human embryonic stem cell model of ethanol-mediated early developmental toxicity. Exp Neurol. 2012;234:127–135. doi: 10.1016/j.expneurol.2011.12.022. [DOI] [PubMed] [Google Scholar]
- 76.Bosnjak ZJ. Developmental neurotoxicity screening using human embryonic stem cells. Exp Neurol. 2012;237:207–210. doi: 10.1016/j.expneurol.2012.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gao W, Zhou P, Ma X, Tschudy-Seney B, Chen J, Magner NL, Revzin A, Nolta JA, Zern MA, Duan Y. Ethanol negatively regulates hepatic differentiation of hESC by inhibition of the MAPK/ERK signaling pathway in vitro. PLoS One. 2014;9:e112698. doi: 10.1371/journal.pone.0112698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang Q, Song JW, Liu Y, Zhao XX. Involvement of Wnt pathway in ethanol-induced inhibition of mouse embryonic stem cell differentiation. Alcohol. 2017;58:13–18. doi: 10.1016/j.alcohol.2016.11.006. [DOI] [PubMed] [Google Scholar]
- 79.Worley SL, Vaughn BJ, Terry AI, Gardiner CS, DeKrey GK. Time- and dose-dependent effects of ethanol on mouse embryonic stem cells. Reprod Toxicol. 2015;57:157–164. doi: 10.1016/j.reprotox.2015.06.044. [DOI] [PubMed] [Google Scholar]
- 80.Sánchez-Alvarez R, Gayen S, Vadigepalli R, Anni H. Ethanol diverts early neuronal differentiation trajectory of embryonic stem cells by disrupting the balance of lineage specifiers. PLoS One. 2013;8:e63794. doi: 10.1371/journal.pone.0063794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ogony JW, Malahias E, Vadigepalli R, Anni H. Ethanol alters the balance of Sox2, Oct4, and Nanog expression in distinct subpopulations during differentiation of embryonic stem cells. Stem Cells Dev. 2013;22:2196–2210. doi: 10.1089/scd.2012.0513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Xiang Y, Kim KY, Gelernter J, Park IH, Zhang H. Ethanol upregulates NMDA receptor subunit gene expression in human embryonic stem cell-derived cortical neurons. PLoS One. 2015;10:e0134907. doi: 10.1371/journal.pone.0134907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lieberman R, Levine ES, Kranzler HR, Abreu C, Covault J. Pilot study of iPS-derived neural cells to examine biologic effects of alcohol on human neurons in vitro. Alcohol Clin Exp Res. 2012;36:1678–1687. doi: 10.1111/j.1530-0277.2012.01792.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Scarnati MS, Halikere A, Pang ZP. Using human stem cells as a model system to understand the neural mechanisms of alcohol use disorders: current status and outlook. Alcohol. 2018 doi: 10.1016/j.alcohol.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tian L, Prasad N, Jang YY. In vitro modeling of alcohol-induced liver injury using human-induced pluripotent stem cells. Methods Mol Biol. 2016;1353:271–283. doi: 10.1007/7651_2014_168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Arzumnayan A, Arzumanyan A, Anni H, Rubin R, Rubin E. Effects of ethanol on mouse embryonic stem cells. Alcohol Clin Exp Res. 2009;33:2172–2179. doi: 10.1111/j.1530-0277.2009.01057.x. [DOI] [PubMed] [Google Scholar]
- 87.Ballard HS. The hematological complications of alcoholism. Alcohol Health Res World. 1997;21:42–52. [PMC free article] [PubMed] [Google Scholar]
- 88.Yeung KY, Klug PP, Lessin LS. Alcohol-induced vacuolization in bone marrow cells: ultrastructure and mechanism of formation. Blood Cells. 1988;13:487–502. [PubMed] [Google Scholar]
- 89.Mohrin M, Bourke E, Alexander D, Warr MR, Barry-Holson K, Le Beau MM, Morrison CG, Passegué E. Hematopoietic stem cell quiescence promotes error-prone DNA repair and mutagenesis. Cell Stem Cell. 2010;7:174–185. doi: 10.1016/j.stem.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Albano E. Alcohol, oxidative stress and free radical damage. Proc Nutr Soc. 2006;65:278–290. doi: 10.1079/PNS2006496. [DOI] [PubMed] [Google Scholar]
- 91.Garaycoechea JI, Crossan GP, Langevin F, Daly M, Arends MJ, Patel KJ. Genotoxic consequences of endogenous aldehydes on mouse haematopoietic stem cell function. Nature. 2012;489:571–575. doi: 10.1038/nature11368. [DOI] [PubMed] [Google Scholar]
- 92.Garaycoechea JI, Crossan GP, Langevin F, Mulderrig L, Louzada S, Yang F, Guilbaud G, Park N, Roerink S, Nik-Zainal S, et al. Alcohol and endogenous aldehydes damage chromosomes and mutate stem cells. Nature. 2018;553:171–177. doi: 10.1038/nature25154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pontel LB, Rosado IV, Burgos-Barragan G, Garaycoechea JI, Yu R, Arends MJ, Chandrasekaran G, Broecker V, Wei W, Liu L, et al. Endogenous formaldehyde is a hematopoietic stem cell genotoxin and metabolic carcinogen. Mol Cell. 2015;60:177–188. doi: 10.1016/j.molcel.2015.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Szabo G. Consequences of alcohol consumption on host defence. Alcohol Alcohol. 1999;34:830–841. doi: 10.1093/alcalc/34.6.830. [DOI] [PubMed] [Google Scholar]
- 95.Shi X, Lin YP, Gao B, Zhang P. Impairment of hematopoietic precursor cell activation during the granulopoietic response to bacteremia in mice with chronic-plus-binge alcohol administration. Infect Immun. 2017;85:00369-17. doi: 10.1128/IAI.00369-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhang P, Welsh DA, Siggins RW, Bagby GJ, Raasch CE, Happel KI, Nelson S. Acute alcohol intoxication inhibits the lineage-c-kit + Sca-1 + cell response to Escherichia coli bacteremia. J Immunol. 2009;182:1568–1576. doi: 10.4049/jimmunol.182.3.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wang H, Zhou H, Moscatello KM, Dixon C, Brunson LE, Chervenak R, Chervenak DC, Zhao X, Wolcott RM. In utero exposure to alcohol alters cell fate decisions by hematopoietic progenitors in the bone marrow of offspring mice during neonatal development. Cell Immunol. 2006;239:75–85. doi: 10.1016/j.cellimm.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 98.Dalakas E, Newsome PN, Boyle S, Brown R, Pryde A, McCall S, Hayes PC, Bickmore WA, Harrison DJ, Plevris JN. Bone marrow stem cells contribute to alcohol liver fibrosis in humans. Stem Cells Dev. 2010;19:1417–1425. doi: 10.1089/scd.2009.0387. [DOI] [PubMed] [Google Scholar]
- 99.Seitz HK, Stickel F. Molecular mechanisms of alcohol-mediated carcinogenesis. Nat Rev Cancer. 2007;7:599–612. doi: 10.1038/nrc2191. [DOI] [PubMed] [Google Scholar]
- 100.Boffetta P, Hashibe M. Alcohol and cancer. Lancet Oncol. 2006;7:149–156. doi: 10.1016/S1470-2045(06)70577-0. [DOI] [PubMed] [Google Scholar]
- 101.LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and cancer: a statement of the American Society of Clinical Oncology. J Clin Oncol. 2018;36:83–93. doi: 10.1200/JCO.2017.76.1155. [DOI] [PubMed] [Google Scholar]
- 102.Pani G, Fusco S, Colavitti R, Borrello S, Maggiano N, Cravero AA, Farré SM, Galeotti T, Koch OR. Abrogation of hepatocyte apoptosis and early appearance of liver dysplasia in ethanol-fed p53-deficient mice. Biochem Biophys Res Commun. 2004;325:97–100. doi: 10.1016/j.bbrc.2004.09.213. [DOI] [PubMed] [Google Scholar]
- 103.Shackleton M, Quintana E, Fearon ER, Morrison SJ. Heterogeneity in cancer: cancer stem cells versus clonal evolution. Cell. 2009;138:822–829. doi: 10.1016/j.cell.2009.08.017. [DOI] [PubMed] [Google Scholar]
- 104.Singh AK, Arya RK, Maheshwari S, Singh A, Meena S, Pandey P, Dormond O, Datta D. Tumor heterogeneity and cancer stem cell paradigm: updates in concept, controversies and clinical relevance. Int J Cancer. 2015;136:1991–2000. doi: 10.1002/ijc.28804. [DOI] [PubMed] [Google Scholar]
- 105.Xu M, Luo J. Alcohol and cancer stem cells. Cancers (Basel) 2017;9:158. doi: 10.3390/cancers9110158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gu S, Nguyen BN, Rao S, Li S, Shetty K, Rashid A, Shukla V, Deng CX, Mishra L, Mishra B. Alcohol, stem cells and cancer. Genes Cancer. 2017;8:695–700. doi: 10.18632/genesandcancer.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ding S, Li C, Cheng N, Cui X, Xu X, Zhou G. Redox regulation in cancer stem cells. Oxid Med Cell Longev. 2015;2015:750798. doi: 10.1155/2015/750798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Xu M, Ren Z, Wang X, Comer A, Frank JA, Ke ZJ, Huang Y, Zhang Z, Shi X, Wang S, et al. ErbB2 and p38γ MAPK mediate alcohol-induced increase in breast cancer stem cells and metastasis. Mol Cancer. 2016;15:52. doi: 10.1186/s12943-016-0532-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Machida K, Chen CL, Liu JC, Kashiwabara C, Feldman D, French SW, Sher L, Hyeongnam JJ, Tsukamoto H. Cancer stem cells generated by alcohol, diabetes, and hepatitis C virus. J Gastroenterol Hepatol. 2012;27(Suppl 2):19–22. doi: 10.1111/j.1440-1746.2011.07010.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fujihara KM, Clemons NJ. Bridging the molecular divide: alcohol-induced downregulation of PAX9 and tumour development. J Pathol. 2018;244:386–388. doi: 10.1002/path.5041. [DOI] [PubMed] [Google Scholar]
- 111.Wu D, Cederbaum AI. Alcohol, oxidative stress, and free radical damage. Alcohol Res Health. 2003;27:277–284. [PMC free article] [PubMed] [Google Scholar]
- 112.Brocardo PS, Gil-Mohapel J, Christie BR. The role of oxidative stress in fetal alcohol spectrum disorders. Brain Res Rev. 2011;67:209–225. doi: 10.1016/j.brainresrev.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 113.Khacho M, Slack RS. Mitochondrial and reactive oxygen species signaling coordinate stem cell fate decisions and life long maintenance. Antioxid Redox Signal. 2017;4:10. doi: 10.1089/ars.2017.7228. [DOI] [PubMed] [Google Scholar]
- 114.Liang R, Ghaffari S. Stem cells, redox signaling, and stem cell aging. Antioxid Redox Signal. 2014;20:1902–1916. doi: 10.1089/ars.2013.5300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chen C, Liu Y, Zheng P. The axis of mTOR-mitochondria-ROS and stemness of the hematopoietic stem cells. Cell Cycle. 2009;8:1158–1160. doi: 10.4161/cc.8.8.8139. [DOI] [PubMed] [Google Scholar]
- 116.Magri L, Cambiaghi M, Cominelli M, Alfaro-Cervello C, Cursi M, Pala M, Bulfone A, Garcìa-Verdugo JM, Leocani L, Minicucci F, et al. Sustained activation of mTOR pathway in embryonic neural stem cells leads to development of tuberous sclerosis complex-associated lesions. Cell Stem Cell. 2011;9:447–462. doi: 10.1016/j.stem.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 117.Weichhart T, Hengstschläger M, Linke M. Regulation of innate immune cell function by mTOR. Nat Rev Immunol. 2015;15:599–614. doi: 10.1038/nri3901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.De Filippis L, Halikere A, McGowan H, Moore JC, Tischfield JA, Hart RP, Pang ZP. Ethanol-mediated activation of the NLRP3 inflammasome in iPS cells and iPS cells-derived neural progenitor cells. Mol Brain. 2016;9:51. doi: 10.1186/s13041-016-0221-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zakhari S. Alcohol metabolism and epigenetics changes. Alcohol Res. 2013;35:6–16. doi: 10.35946/arcr.v35.1.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.French SW. Chronic alcohol binging injures the liver and other organs by reducing NAD+ levels required for sirtuin’s deacetylase activity. Exp Mol Pathol. 2016;100:303–306. doi: 10.1016/j.yexmp.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 121.Stein LR, Imai S. Specific ablation of Nampt in adult neural stem cells recapitulates their functional defects during aging. EMBO J. 2014;33:1321–1340. doi: 10.1002/embj.201386917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zhang H, Ryu D, Wu Y, Gariani K, Wang X, Luan P, D’Amico D, Ropelle ER, Lutolf MP, Aebersold R, et al. NAD+ repletion improves mitochondrial and stem cell function and enhances life span in mice. Science. 2016;352:1436–1443. doi: 10.1126/science.aaf2693. [DOI] [PubMed] [Google Scholar]
- 123.Wang S, Wan T, Ye M, Qiu Y, Pei L, Jiang R, Pang N, Huang Y, Liang B, Ling W, et al. Nicotinamide riboside attenuates alcohol induced liver injuries via activation of SirT1/PGC-1α/mitochondrial biosynthesis pathway. Redox Biol. 2018;17:89–98. doi: 10.1016/j.redox.2018.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bonkowski MS, Sinclair DA. Slowing ageing by design: the rise of NAD. Nat Rev Mol Cell Biol. 2016;17:679–690. doi: 10.1038/nrm.2016.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.You M, Liang X, Ajmo JM, Ness GC. Involvement of mammalian sirtuin 1 in the action of ethanol in the liver. Am J Physiol Gastrointest Liver Physiol. 2008;294:G892–898. doi: 10.1152/ajpgi.00575.2007. [DOI] [PubMed] [Google Scholar]
- 126.Thompson KJ, Humphries JR, Niemeyer DJ, Sindram D, McKillop IH. The effect of alcohol on Sirt1 expression and function in animal and human models of hepatocellular carcinoma (HCC) Adv Exp Med Biol. 2015;815:361–373. doi: 10.1007/978-3-319-09614-8_21. [DOI] [PubMed] [Google Scholar]
- 127.Kotova N, Vare D, Schultz N, Gradecka Meesters D, Stepnik M, Grawé J, Helleday T, Jenssen D. Genotoxicity of alcohol is linked to DNA replication-associated damage and homologous recombination repair. Carcinogenesis. 2013;34:325–330. doi: 10.1093/carcin/bgs340. [DOI] [PubMed] [Google Scholar]
- 128.Langevin F, Crossan GP, Rosado IV, Arends MJ, Patel KJ. Fancd2 counteracts the toxic effects of naturally produced aldehydes in mice. Nature. 2011;475:53–58. doi: 10.1038/nature10192. [DOI] [PubMed] [Google Scholar]
- 129.Hira A, Yabe H, Yoshida K, Okuno Y, Shiraishi Y, Chiba K, Tanaka H, Miyano S, Nakamura J, Kojima S, et al. Variant ALDH2 is associated with accelerated progression of bone marrow failure in Japanese Fanconi anemia patients. Blood. 2013;122:3206–3209. doi: 10.1182/blood-2013-06-507962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yoshida K, Miki Y. Role of BRCA1 and BRCA2 as regulators of DNA repair, transcription, and cell cycle in response to DNA damage. Cancer Sci. 2004;95:866–871. doi: 10.1111/j.1349-7006.2004.tb02195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ray Chaudhuri A, Nussenzweig A. Thwarting endogenous stress: BRCA protects against aldehyde toxicity. EMBO Mol Med. 2017;9:1331–1333. doi: 10.15252/emmm.201708194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Tan SLW, Chadha S, Liu Y, Gabasova E, Perera D, Ahmed K, Constantinou S, Renaudin X, Lee M, Aebersold R, et al. A class of environmental and endogenous toxins induces BRCA2 haploinsufficiency and genome instability. Cell. 2017;169:1105–1118.e1115. doi: 10.1016/j.cell.2017.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Gentry T, Foster S, Winstead L, Deibert E, Fiordalisi M, Balber A. Simultaneous isolation of human BM hematopoietic, endothelial and mesenchymal progenitor cells by flow sorting based on aldehyde dehydrogenase activity: implications for cell therapy. Cytotherapy. 2007;9:259–274. doi: 10.1080/14653240701218516. [DOI] [PubMed] [Google Scholar]
- 134.Alison MR, Guppy NJ, Lim SM, Nicholson LJ. Finding cancer stem cells: are aldehyde dehydrogenases fit for purpose? J Pathol. 2010;222:335–344. doi: 10.1002/path.2772. [DOI] [PubMed] [Google Scholar]
- 135.Morita M, Oyama T, Kagawa N, Nakata S, Ono K, Sugaya M, Uramoto H, Yoshimatsu T, Hanagiri T, Sugio K, et al. Expression of aldehyde dehydrogenase 2 in the normal esophageal epithelium and alcohol consumption in patients with esophageal cancer. Front Biosci. 2005;10:2319–2324. doi: 10.2741/1700. [DOI] [PubMed] [Google Scholar]
- 136.Dainiak N. Surface membrane-associated regulation of cell assembly, differentiation, and growth. Blood. 1991;78:264–276. [PubMed] [Google Scholar]
- 137.Tóth ME, Vígh L, Sántha M. Alcohol stress, membranes, and chaperones. Cell Stress Chaperones. 2014;19:299–309. doi: 10.1007/s12192-013-0472-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Lasek AW. Effects of ethanol on brain extracellular matrix: implications for alcohol use disorder. Alcohol Clin Exp Res. 2016;40:2030–2042. doi: 10.1111/acer.13200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Steiner JL, Pruznak AM, Navaratnarajah M, Lang CH. Alcohol differentially alters extracellular matrix and adhesion molecule expression in skeletal muscle and heart. Alcohol Clin Exp Res. 2015;39:1330–1340. doi: 10.1111/acer.12771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Poole LG, Arteel GE. Transitional remodeling of the hepatic extracellular matrix in alcohol-induced liver injury. Biomed Res Int. 2016;2016:3162670. doi: 10.1155/2016/3162670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Philp D, Chen SS, Fitzgerald W, Orenstein J, Margolis L, Kleinman HK. Complex extracellular matrices promote tissue-specific stem cell differentiation. Stem Cells. 2005;23:288–296. doi: 10.1634/stemcells.2002-0109. [DOI] [PubMed] [Google Scholar]
- 142.Vining KH, Mooney DJ. Mechanical forces direct stem cell behaviour in development and regeneration. Nat Rev Mol Cell Biol. 2017;18:728–742. doi: 10.1038/nrm.2017.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Dalton S. Signaling networks in human pluripotent stem cells. Curr Opin Cell Biol. 2013;25:241–246. doi: 10.1016/j.ceb.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Crews FT, Bechara R, Brown LA, Guidot DM, Mandrekar P, Oak S, Qin L, Szabo G, Wheeler M, Zou J. Cytokines and alcohol. Alcohol Clin Exp Res. 2006;30:720–730. doi: 10.1111/j.1530-0277.2006.00084.x. [DOI] [PubMed] [Google Scholar]
- 145.Wu H, Sun YE. Epigenetic regulation of stem cell differentiation. Pediatr Res. 2006;59:21R–25R. doi: 10.1203/01.pdr.0000203565.76028.2a. [DOI] [PubMed] [Google Scholar]
- 146.Vadigepalli R, Hoek JB. Introduction to the virtual issue alcohol and epigenetic regulation: do the products of alcohol metabolism drive epigenetic control of gene expression in alcohol-related disorders? Alcohol Clin Exp Res. 2018;42:845–848. doi: 10.1111/acer.13630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Mahnke AH, Miranda RC, Homanics GE. Epigenetic mediators and consequences of excessive alcohol consumption. Alcohol. 2017;60:1–6. doi: 10.1016/j.alcohol.2017.02.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhou FC, Balaraman Y, Teng M, Liu Y, Singh RP, Nephew KP. Alcohol alters DNA methylation patterns and inhibits neural stem cell differentiation. Alcohol Clin Exp Res. 2011;35:735–746. doi: 10.1111/j.1530-0277.2010.01391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Veazey KJ, Carnahan MN, Muller D, Miranda RC, Golding MC. Alcohol-induced epigenetic alterations to developmentally crucial genes regulating neural stemness and differentiation. Alcohol Clin Exp Res. 2013;37:1111–1122. doi: 10.1111/acer.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sharp GC, Arathimos R, Reese SE, Page CM, Felix J, Küpers LK, Rifas-Shiman SL, Liu C, Burrows K, Zhao S, et al. Maternal alcohol consumption and offspring DNA methylation: findings from six general population-based birth cohorts. Epigenomics. 2018;10:27–42. doi: 10.2217/epi-2017-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Mandal C, Halder D, Jung KH, Chai YG. Maternal alcohol consumption and altered miRNAs in the developing fetus: context and future perspectives. J Appl Toxicol. 2018;38:100–107. doi: 10.1002/jat.3504. [DOI] [PubMed] [Google Scholar]
- 152.Gardiner AS, Gutierrez HL, Luo L, Davies S, Savage DD, Bakhireva LN, Perrone-Bizzozero NI. Alcohol use during pregnancy is associated with specific alterations in microRNA levels in maternal serum. Alcohol Clin Exp Res. 2016;40:826–837. doi: 10.1111/acer.13026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Saha B, Momen-Heravi F, Kodys K, Szabo G. MicroRNA cargo of extracellular vesicles from alcohol-exposed monocytes signals naive monocytes to differentiate into M2 macrophages. J Biol Chem. 2016;291:149–159. doi: 10.1074/jbc.M115.694133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Rao PSS, O’Connell K, Finnerty TK. Potential role of extracellular vesicles in the pathophysiology of drug addiction. Mol Neurobiol. 2018;55:6906–6913. doi: 10.1007/s12035-018-0912-4. [DOI] [PubMed] [Google Scholar]