Abstract
Objective:
The absence of a centralized health system has limited epidemiological research surrounding vestibular schwannoma (VS) in the United States. The Rochester Epidemiology Project (REP) comprises a unique medical consortium that covers a complete population of all ages in a well-defined geographic region over the past half-century. The objective of this study was to characterize the incidence of sporadic VS over this extended period of time.
Study Design:
Population-based study.
Setting:
Olmsted County, Minnesota.
Subjects and Methods:
Review of all VS diagnosed between 1/1/1966 and 12/31/2016 using the REP medical records-linkage system.
Results:
One hundred fifty-three incident cases of VS were identified. The incidence of VS significantly increased over the past half-century from 1.5 per 100,000 person-years during the first decade to 4.2 in the last decade (p<0.001). Incidence increased with age (p<0.001); those aged 70+ exhibited the highest incidence rate at 18.3 per 100,000 person-years in the last decade. Age at diagnosis significantly increased from a median of 52 years in the first decade to 62 in the last (p<0.001). Despite presenting with fewer symptoms and smaller tumors, the time delay between symptom onset and diagnosis significantly decreased over the past five decades (all p<0.05). Almost one in four patients was diagnosed incidentally in the last decade.
Conclusion:
The incidence of VS increased significantly over the past half-century to a rate greater than previously reported. Patients’ ease-of-access to medical care in Olmsted County and the comprehensive REP system likely contributed to this elevated detection rate of VS.
Keywords: vestibular schwannoma, acoustic neuroma, sporadic, incidence, incidental, epidemiology, Rochester epidemiology project, Olmsted County
INTRODUCTION
Arising from Schwann cells of the eighth cranial nerve, vestibular schwannoma (VS) constitutes the most common neoplasm of the cerebellopontine angle and internal auditory canal. Epidemiological research over recent decades suggests that the incidence of VS is increasing, likely secondary to improved access to modern diagnostic imaging and more widespread screening of asymmetrical sensorineural hearing loss.1–3 However, within the United States, the absence of a centralized health system has limited epidemiological research surrounding VS.
Prior to the Benign Brain Tumor Cancer Registries Amendment Act of 2004 (Public Law 107–260), registration of VS was not nationally mandated. Recent research using the Central Brain Tumor Registry of the United States (CBTRUS) suggests that the incidence of VS from 2004 to 2010 was 1.09 per 100,000 person-years.4 Similarly, a recent study from the Surveillance, Epidemiology, and End Results (SEER) program reported the incidence of VS to be 1.1 per 100,000 person-years between 2004 and 2011.5 Despite these advancements in the understanding of VS epidemiology within the United States, the restricted historical depth, heterogeneous geographic coverage, and variability in data collection of current national medical databases limits prior research. What is more, radiological and autopsy studies suggest that the true incidence of VS may be much higher.3 For instance, a retrospective analysis of 46,000 magnetic resonance imaging (MRI) studies performed for unrelated indications identified 8 previously undiagnosed VS – a prevalence rate of 2 VS per 10,000 individuals studied.6 An even higher rate was observed during a post-mortem study of 893 temporal bones where 0.9% of people were found to have occult VS.7 The combination of limited past epidemiological research and the observed high detection rate of radiological and autopsy studies underscore the importance of further investigation into VS epidemiology.
With inception dating back to 1966, the Rochester Epidemiology Project (REP) was founded when Dr. Leonard T. Kurland initiated collaboration for a medical consortium that linked patient data from all health care providers in Olmsted County to the Mayo Clinic.8 Supporting over 2,500 publications to-date, the REP comprises a unique medical records-linkage system that covers a complete population in a well-defined geographic region and spans the past half-century.9 Furthermore, given its healthcare-driven economy, Olmsted County’s health literacy and ease-of-access to medical care provide a unique patient cohort for research.10 For these reasons, we hypothesized that the incidence of VS within this catchment area would be greater than previous epidemiological reports. As such, the primary objective of this study was to characterize the epidemiology of VS since 1966 using the comprehensive REP consortium.
METHODS
Patient Data & the Rochester Epidemiology Project
After obtaining approval from the Mayo Clinic and Olmsted Medical Center institutional review boards, we conducted a retrospective review of all residents of Olmsted County, Minnesota who were diagnosed with VS between January 1, 1966 and December 31, 2016 using the infrastructure provided by the REP medical records-linkage system. Since 1966, virtually all residents of Olmsted County have been prospectively registered within the REP system by either their date of birth or first health care visit.10 Patients with VS were identified through a diagnostic code search of all medical records in Olmsted County using the REP, and each case of VS was confirmed by pathology report following excision or by characteristic imaging findings for patients diagnosed during the CT or MRI era who did not undergo surgery. Research authorization and residency status at the time of diagnosis was verified upon medical record review. Hearing data and tumor size were reported in accordance with the American Academy of Otolaryngology–Head and Neck Surgery committee guidelines.11 Several studies have previously validated the accuracy of the REP’s medical records-linkage system; the rate of under-inclusion of one or more records from a given patient’s chart is estimated to be 1.3%.12 Validation of routine follow-up indicated that 80% of Olmsted County residents are seen at least once within one year and 93% of residents within three years.9
Statistical Methods
Continuous features were summarized with medians and interquartile ranges (IQRs); categorical features were summarized with frequency counts and percentages. Changes in features over time were evaluated using Spearman rank correlation coefficients, Kruskal-Wallis tests, and Wilcoxon rank sum tests. Incidence rates per 100,000 person-years were calculated using incident cases of VS as the numerator and age- and sex-specific counts of the population of Olmsted County, Minnesota as the denominator. The denominators were obtained from a complete enumeration of the Olmsted County population.12 Incidence rates were age- and sex-adjusted to the structure of the 2000 United States population. Incident cases were grouped by age into 0–19, 20–29, 30–39, 40–49, 50–59, 60–69, and 70+ years old, and were grouped by year of diagnosis into 1966–1975, 1976–1985, 1986–1995, 1996–2005, and 2006–2016. The relationships of age, sex, and year of diagnosis with incidence rates were assessed by fitting Poisson regression models using the SAS procedure GENMOD. Statistical analyses were performed using version 9.4 of the SAS software package (SAS Institute; Cary, NC). All tests were two-sided and p-values <0.05 were considered statistically significant.
RESULTS
Evolution of Patient Characteristics & Presenting Symptomatology at Diagnosis
One hundred fifty-three incident cases of sporadic VS were identified over a period that spanned 5.9 million person-years. The number of residents and thus number of people at risk for the development of VS in Olmsted County was 88,913 in 1970, 109,868 in 1990, and 148,201 in 2010. All incident cases of VS in patients with neurofibromatosis type 2 were excluded from analysis. The evolution of patient characteristics and presenting symptomatology of individuals diagnosed with sporadic VS are presented in Table 1. The time to diagnosis from the onset of symptoms decreased significantly from a median of 25 months in the first decade to 12 months in the last (p=0.028). Age at diagnosis also significantly increased over the study period, from a median of 52 years in the first decade to 62 in the last (p<0.001). Patients diagnosed in the most recent two decades were significantly more likely to present with audiovestibular symptoms alone and less hearing loss (both p<0.05). Sudden hearing loss was experienced in 10% of patients over the entire study period. Over the first two decades, only one case of VS was diagnosed incidentally compared to 24% of total cases over the most recent decade.
Table 1.
Patient characteristics and presenting symptomatology at the time of diagnosis across the past five decades.
| 1966–1975 | 1976–1985 | 1986–1995 | 1996–2005 | 2006–2016 | ||
|---|---|---|---|---|---|---|
| N=9 | N=9 | N=19 | N=40 | N=76 | ||
| Feature | Median (IQR) | P-value | ||||
| Age at diagnosis in years | 52 (46–67) | 50 (47–56) | 55 (46–67) | 53 (43–62.5) | 62 (52.5–71) | <0.001 |
| Time to diagnosis from onset of symptoms in months (N=120) | 25 (12–132) | 36 (21–51) | 17 (7–60) | 12 (4–36) | 12 (5–35) | 0.028 |
| SRT in affected ear in dB (N=130) | 80 (50–135) | 50 (28–64) | 25 (20–35) | 30 (20–47.5) | 27.5 (15–45) | 0.016 |
| WRS in affected ear in % (N=128) | 8 (0–18) | 36 (12–52) | 69.5 (36–92) | 75 (40–96) | 80 (37–100) | 0.007 |
| Sex | N (%) | |||||
| Women | 6 (67) | 4 (44) | 11 (58) | 23 (58) | 38 (50) | 0.41 |
| Men | 3 (33) | 5 (56) | 8 (42) | 17 (43) | 38 (50) | |
| Race (N=145) | ||||||
| All others | 0 | 1 (17) | 0 | 1 (3) | 5 (6) | 0.38 |
| White | 7 (100) | 5 (83) | 17 (100) | 38 (97) | 71 (93) | |
| Side (N=152) | ||||||
| Left | 8 (89) | 4 (44) | 11 (61) | 17 (43) | 38 (50) | 0.31 |
| Right | 1 (11) | 5 (56) | 7 (39) | 23 (58) | 38 (50) | |
| Sudden hearing loss (N=150) | 0 | 0 | 2 (12) | 7 (18) | 6 (8) | 0.87 |
| Gradual hearing loss (N=150) | 7 (88) | 9 (100) | 11 (65) | 25 (63) | 47 (62) | 0.094 |
| Tonal tinnitus (N=144) | 4 (50) | 7 (88) | 9 (56) | 21 (54) | 43 (59) | 0.90 |
| Aural fullness (N=145) | 0 | 1 (13) | 2 (13) | 9 (23) | 12 (16) | 0.71 |
| Dizziness (N=152) | 4 (44) | 2 (22) | 8 (44) | 22 (55) | 34 (45) | 0.85 |
| Dysguesia (N=149) | 1 (11) | 1 (11) | 1 (6) | 1 (3) | 1 (1) | 0.065 |
| Facial spasm (N=150) | 0 | 0 | 0 | 0 | 1 (1) | NE |
| Facial paresis or paralysis (N=152) | 2 (22) | 1 (11) | 0 | 1 (3) | 0 | NE |
| Facial numbness (N=151) | 1 (11) | 2 (22) | 4 (24) | 2 (5) | 2 (3) | 0.006 |
| Trigeminal neuralgia (N=151) | 1 (11) | 0 | 0 | 0 | 0 | NE |
| Headache with hydrocephalus (N=151) | 1 (13) | 0 | 3 (17) | 1 (3) | 0 | 0.007 |
| Other cranial nerve symptoms (N=152) | 1 (11) | 0 | 2 (11) | 1 (3) | 0 | NE |
| Symptom classification (N=152) | ||||||
| None (incidental cases) | 1 (11) | 0 | 3 (17) | 5 (13) | 18 (24) | <0.00 |
| Cranial nerve symptoms | 6 (67) | 3 (33) | 6 (33) | 3 (8) | 3 (4) | 1 |
| Audiovestibular symptoms alone | 2 (22) | 6 (67) | 9 (50) | 32 (80) | 55 (72) | |
| Chronic loud noise exposure (N=116) | 1 (17) | 2 (25) | 3 (20) | 8 (26) | 12 (21) | 0.95 |
Abbreviations: SRT = speech reception threshold | WRS = word recognition score | NE = not examined
Incidence of Vestibular Schwannoma Over the Past Half-Century
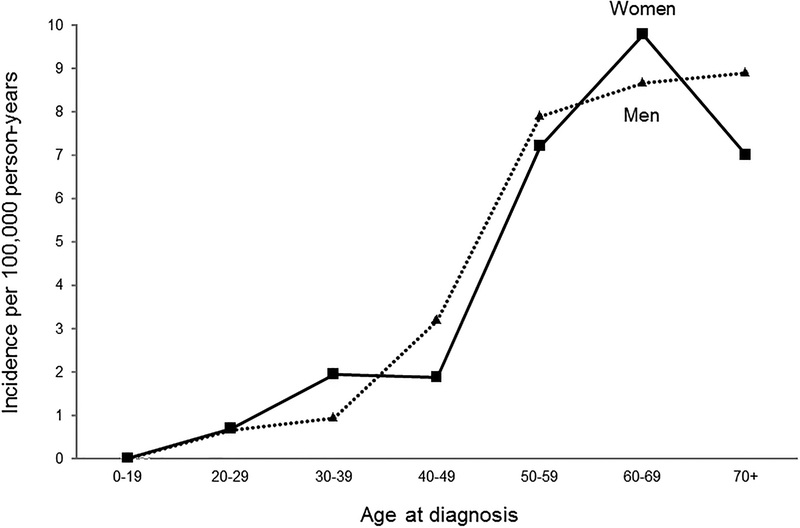
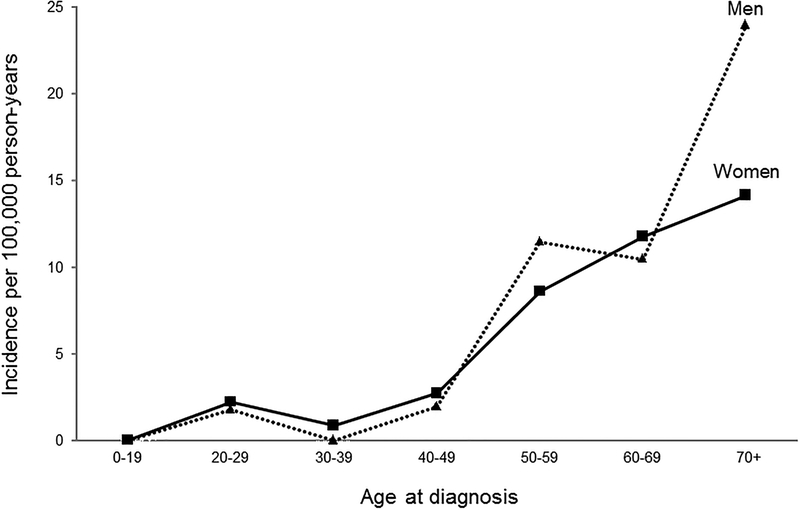
The incidence of VS significantly increased over the past half-century from 1.5 per 100,000 person-years during the first decade to 4.2 in the last decade (p<0.001; Table 2 and Figure 1). Incidence increased significantly with age (p<0.001); since 1966, individuals aged 60–69 exhibited the highest overall incidence rate at 9.3 per 100,000 person-years (Table 3.a). However, over the most recent decade, individuals 70 years and older exhibited the highest incidence rate at 18.3 per 100,000 person years (Table 3.b). The change in incidence rate per 100,000 person-years by age group and sex is depicted in Figure 2.
Table 2.
Incidence of sporadic vestibular schwannoma from 1966–2016 in Olmsted County, Minnesota by year of diagnosis.
| Women | Men | Total | ||||
|---|---|---|---|---|---|---|
| Year of diagnosis | N | Rate* | N | Rate* | N | Rate† |
| 1966–1975 | 6 | 1.8 | 3 | 1.4 | 9 | 1.5 |
| 1976–1985 | 4 | 1.0 | 5 | 1.5 | 9 | 1.3 |
| 1986–1995 | 11 | 2.3 | 8 | 1.7 | 19 | 2.1 |
| 1996–2005 | 23 | 3.5 | 17 | 2.9 | 40 | 3.2 |
| 2006–2016 | 38 | 3.9 | 38 | 4.7 | 76 | 4.2 |
| Total | 82 | 2.8 | 71 | 3.0 | 153 | 2.9 |
Incidence per 100,000 person-years age-adjusted to 2000 United States population.
Incidence per 100,000 person-years age- and sex-adjusted to 2000 United States population.
Figure 1.
Incidence of sporadic vestibular schwannoma from 1966–2016 in Olmsted County, Minnesota by year of diagnosis.
Table 3.
Incidence of sporadic vestibular schwannoma in Olmsted County, Minnesota by age at diagnosis (a) from 1966 through 2016 and (b) from 2006 through 2016.
| (A) | ||||||
|---|---|---|---|---|---|---|
| Women | Men | Total | ||||
| Age at diagnosis | N | Rate* | N | Rate* | N | Rate* |
| 0–19 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| 20–29 | 4 | 0.7 | 3 | 0.7 | 7 | 0.7 |
| 30–39 | 9 | 1.9 | 4 | 0.9 | 13 | 1.5 |
| 40–49 | 7 | 1.9 | 11 | 3.2 | 18 | 2.5 |
| 50–59 | 22 | 7.2 | 22 | 7.9 | 44 | 7.5 |
| 60–69 | 21 | 9.8 | 16 | 8.7 | 37 | 9.3 |
| 70+ | 19 | 7.0 | 15 | 8.9 | 34 | 7.7 |
| Total | 82 | 2.8† | 71 | 3.0† | 153 | 2.9‡ |
| (B) | ||||||
|---|---|---|---|---|---|---|
| Women | Men | Total | ||||
| Age at diagnosis | N | Rate* | N | Rate* | N | Rate* |
| 0–19 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| 20–29 | 3 | 2.2 | 2 | 1.8 | 5 | 2.0 |
| 30–39 | 1 | 0.8 | 0 | 0.0 | 1 | 0.4 |
| 40–49 | 3 | 2.7 | 2 | 2.0 | 5 | 2.3 |
| 50–59 | 10 | 8.6 | 12 | 11.5 | 22 | 9.9 |
| 60–69 | 9 | 11.7 | 7 | 10.4 | 16 | 11.1 |
| 70+ | 12 | 14.1 | 15 | 23.9 | 27 | 18.3 |
| Total | 38 | 3.9† | 38 | 4.7† | 76 | 4.2‡ |
Incidence per 100,000 person-years.
Incidence per 100,000 person-years age-adjusted to 2000 United States population.
Incidence per 100,000 person-years age- and sex-adjusted to 2000 United States population.
Figure 2.
Incidence of sporadic vestibular schwannoma in Olmsted County, Minnesota by age at diagnosis (a) from 1966 through 2016 and (b) from 2006 through 2016.
The first year computed tomography (CT) was used for diagnosis of VS in Olmsted County was in 1978, and the first year MRI was used for diagnosis of VS was in 1984. There were 10 incident cases in the pre-CT era (1966–1977), 6 in the CT era (1978–1983), and 137 in the MRI era (1984–2016). Incidence rates for the pre-CT, CT, and MRI eras were 1.4, 1.4, and 3.3 per 100,000 person-years, respectively.
Changing Tumor Size and Location since 1966
The location of VS at diagnosis significantly changed over time, with 100% of cases between 1966 and 1985 versus only 28% of cases during the most recent decade being located in the cerebellopontine angle (p<0.001). As of 1995, the median extracanalicular size of VS was 2.5 cm, and the extracanalicular size decreased over time to a median of 1.4 cm and 1.2 cm over the most recent two decades (p=0.055). Over the most recent three decades, the size of intracanalicular tumors have steadily decreased from a median of 0.8 cm to 0.5 cm and eventually 0.4 cm in the last decade(p=0.094).
Treatment of Vestibular Schwannoma
Treatment of VS significantly changed over time, where 100% of cases from 1966–1975 underwent surgical excision but only 14% of cases from 2006–2016 underwent surgery (p<0.001; Table 4). No patients underwent observation only for management of VS during the first decade, whereas 58% of patients received observation as their only therapeutic management over the most recent decade.
Table 4.
Evolution of therapeutic strategy for sporadic vestibular schwannoma from 1966–2016.
| 1966–1975 | 1976–1985 | 1986–1995 | 1996–2005 | 2006–2016 | ||
|---|---|---|---|---|---|---|
| N=9 | N=9 | N=19 | N=40 | N=76 | ||
| Feature | N (%) | P-value | ||||
| Treatment classification (N=150) | ||||||
| Surgery only | 8 (100) | 7 (88) | 15 (83) | 21 (53) | 11 (14) | <0.001 |
| SRS only | 0 | 0 | 0 | 3 (8) | 12 (16) | |
| Observation then surgery | 0 | 0 | 0 | 3 (8) | 2 (3) | |
| Observation then SRS | 0 | 0 | 0 | 4 (10) | 7 (9) | |
| Observation only | 0 | 1 (13) | 3 (17) | 9 (23) | 44 (58) | |
| Surgical approach (N=67) | ||||||
| Middle fossa | 0 | 0 | 0 | 1 (4) | 3 (23) | <0.001 |
| Suboccipital craniectomy | 8 (100) | 7 (100) | 14 (93) | 16 (67) | 4 (31) | |
| Translabyrinthine | 0 | 0 | 1 (7) | 7 (29) | 6 (46) | |
| Extent of resection (N=66) | ||||||
| Gross total | 7 (88) | 7 (100) | 14 (100) | 23 (96) | 9 (69) | 0.10 |
| Near total | 0 | 0 | 0 | 1 (4) | 2 (15) | |
| Sub total | 1 (13) | 0 | 0 | 0 | 2 (15) | |
DISCUSSION
This study examined the epidemiology of VS over the past half-century using the REP medical records-linkage system and found that the incidence in Olmsted County, Minnesota over the last decade has increased to 4.2 per 100,000 person-years and 18.3 per 100,000 person-years in individuals 70 years and older. Patients with VS are now 10 years older at diagnosis than they were in 1966. Despite exhibiting significantly fewer symptoms at presentation, the time delay between symptom onset and diagnosis has significantly decreased over the past 50 years. Further, almost one of every four patients in the last decade was diagnosed incidentally. A significant shift towards conservative management was observed over the past half-century, in part secondary to the increased proportion of small intracanalicular tumors. This finding corresponds with a recent study analyzing the SEER registry.5 Lastly, the incidence rate of VS more than doubled following the introduction of MRI in Olmsted County circa 1985. Given that MRI is only increasingly being used in recent years, the significant increase in incidence of VS observed over the past 50 years can most likely be attributed to increased utilization of advanced imaging modalities rather than a true increase in the sporadic development of VS within the Olmsted County population.
Several factors could have contributed to the observed detection rate of VS. First, Olmsted County represents a unique geographic region with an economy driven by healthcare. For instance, according to the 2015 American Community Survey of Olmsted County performed by the United States Census, more people work in the healthcare and social assistance industry than the next four most populated industries combined. The healthcare and social assistance industry accounts for almost 40% of the workforce in Olmsted County compared to approximately 10% of the workforce across the United States. This demographic feature of Olmsted Country undoubtedly influences overall health literacy, and the underlying economy facilitates uniquely easy access to medical care and thus advanced diagnostic imaging. To this end, the significant decrease in time to diagnosis following the onset of symptoms that was observed in this study points to a heightened health literacy surrounding asymmetrical hearing loss and growing access to modern medical diagnostic capabilities.
Further substantiating this rationale, the findings of the current study parallel a study by Schwartz et al. that evaluated the incidence of VS in Beverly Hills, California, a municipality with a high level of healthcare access. In this conference paper, the authors identified 11 cases over a six year period from 1999 to 2004, for a calculated incidence of 5.4 per 100,000 person-years. Also similar to the current study, most patients had small tumors with minimal symptomatology.13
Longitudinal data from a national database in Denmark described the incidence rate of VS to be 2.3 per 100,000 person-years in 2004 with the incidence plateauing and eventually decreasing to 1.9 per 100,000 person-years by 2008.2,14 In contrast, data from our study indicated that the incidence rate in Olmsted County as of 2005 was 3.2 per 100,000 person-years, and the incidence rate only increased over the most recent decade to a rate of 4.2 per 100,000 person-years. Another notable difference between studies was that just 12% of patients diagnosed in the last period in Denmark were 70 years or older, whereas 36% of patients diagnosed in the last decade in Olmsted County were 70 years or older; and, this age group actually displayed the highest incidence rates of any age group at 18.3 per 100,000 person-years. Given that a recent study estimated the incidence rate of VS in this age group to be 3 per 100,000 person-years,4 the fact individuals 70 years and older exhibited an incidence rate of almost 2 in 10,000 represents perhaps the most surprising finding of the current study. In both the Denmark data and the current study, MRI was introduced circa 1985 for diagnosis of VS. Danish research found that the proportion of intracanalicular tumors increased from 3% in the pre-MRI era to 29% by 2001. The present study similarly found that no cases prior to the introduction of MRI were diagnosed intracanalicularly; however, by the last decade, 72% of patients had intracanalicular tumors at the time of diagnosis.14 Lastly, the age at diagnosis in Denmark has steadily increased since 1976 to a mean age of 58 years in 2008. These findings coincide with the current study where the median age at diagnosis increased to 62 years over the most recent decade.14 Importantly, given the trend towards an aging population within the United States, the increasing age at diagnosis of VS could bear important national healthcare implications in the coming years.
Several past studies have attempted to estimate the prevalence of asymptomatic VS.3,6 MRI studies have suggested the prevalence rate of incidental VS to affect up to 0.07% of the population,15 and autopsy studies of selected temporal bones have reported the prevalence to potentially affect 2.4% of the population.3 However, controversy exists within the literature surrounding incidental (ie, asymptomatic) VS as subsequent incidence estimations based off of these autopsy findings concluded that the incidence rate of VS would have to be unrealistically high at 800 per 100,000 person-years.2 Remarkably, within the most recent decade in Olmsted County, almost a quarter of all sporadic VS were diagnosed incidentally after individuals obtained head imaging for unrelated indications. This suggests that the incidence rate of incidental tumors approximates 1 per 100,000 person-years.
There are limitations to the data presented in this study. First, Olmsted County represents a homogenous racial sampling. As such, the incidence rates reported in this study may not be directly transferrable to other racial backgrounds. Specifically, when interpreting the data from the current study, past research suggests that the incidence rates of VS could be higher in Asian Pacific Islanders and lower in Native/American Indians and African Americans.4 Similarly, Olmsted County represents a small subset of the entire United States’ population. Therefore, these data cannot be extrapolated to the general United States’ population. However, they do suggest that the true incidence of VS may be much higher than reported in previous epidemiological studies. Next, given the limitations of diagnostic code searches, it is possible that not every case of VS in Olmsted Country over the study period was reviewed. In this way, the incidence rates reported would underestimate the true incidence of sporadic VS in this geographic region. The impact of this potential systematic error is likely to be extremely low, as evidenced by previous validations of the REP medical records-linkage system.8,10,12 Lastly, compared to reports from national databases, the sample size in this study is relatively small. However, the calculation of incidence rates is not affected by sample size, and the ability to detect significant changes in incidence rates over time in this study was not affected by the sample size (ie, p<0.001).
CONCLUSION
The incidence of sporadic VS in Olmsted County, Minnesota has significantly increased over the past half-century from 1.5 per 100,000 person-years during the first decade to 4.2 in the last decade. Over the last 50 years, the median age at diagnosis has increased by 10 years, the median tumor size has decreased, more patients present with less severe symptoms or incidentally, the time delay between symptom onset and diagnosis has shortened, and more cases are managed with observation. The combination of patients’ ease-of-access to medical care in Olmsted County and the comprehensive REP system likely contributed to this elevated detection rate of VS.
ACKNOWLEDGEMENTS
This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest: The authors report no conflict of interest in submitting this article for publication.
The currently submitted manuscript represents original research that has not been previously submitted and is not under consideration for publication elsewhere. The associated abstract was submitted to the 2018 AAO-HNS meeting for oral presentation. We performed this research with approval from the Mayo Clinic and Olmsted County Medical Center Institutional Review Boards (IRB 15–006036 and 050-OMC-15, respectively).
REFERENCES
- 1.Morris Z, Whiteley WN, Longstreth WT Jr., et al. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. Bmj 2009;339:b3016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tos M, Stangerup SE, Caye-Thomasen P, et al. What is the real incidence of vestibular schwannoma? Arch Otolaryngol Head Neck Surg 2004;130:216–20. [DOI] [PubMed] [Google Scholar]
- 3.Schmidt RF, Boghani Z, Choudhry OJ, et al. Incidental vestibular schwannomas: a review of prevalence, growth rate, and management challenges. Neurosurg Focus 2012;33:E4. [DOI] [PubMed] [Google Scholar]
- 4.Kshettry VR, Hsieh JK, Ostrom QT, et al. Incidence of vestibular schwannomas in the United States. J Neurooncol 2015;124:223–8. [DOI] [PubMed] [Google Scholar]
- 5.Carlson ML, Habermann EB, Wagie AE, et al. The Changing Landscape of Vestibular Schwannoma Management in the United States--A Shift Toward Conservatism. Otolaryngol Head Neck Surg 2015;153:440–6. [DOI] [PubMed] [Google Scholar]
- 6.Lin D, Hegarty JL, Fischbein NJ, et al. The prevalence of “incidental” acoustic neuroma. Arch Otolaryngol Head Neck Surg 2005;131:241–4. [DOI] [PubMed] [Google Scholar]
- 7.Stewart TJ, Liland J, Schuknecht HF. Occult schwannomas of the vestibular nerve. Arch Otolaryngol 1975;101:91–5. [DOI] [PubMed] [Google Scholar]
- 8.Rocca WA, Yawn BP, St Sauver JL, et al. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc 2012;87:1202–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol 2012;41:1614–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.St Sauver JL, Grossardt BR, Leibson CL, et al. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc 2012;87:151–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Committee on Hearing and Equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma). American Academy of Otolaryngology-Head and Neck Surgery Foundation, INC. Otolaryngol Head Neck Surg 1995;113:179–80. [DOI] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, et al. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol 2011;173:1059–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwartz M, Fisher L. Incidence and Clinical Characteristics of Acoustic Neuroma in Beverly Hills; 2006. [Google Scholar]
- 14.Stangerup SE, Tos M, Thomsen J, et al. True incidence of vestibular schwannoma? Neurosurgery 2010;67:1335–40; [DOI] [PubMed] [Google Scholar]
- 15.Anderson TD, Loevner LA, Bigelow DC, et al. Prevalence of unsuspected acoustic neuroma found by magnetic resonance imaging. Otolaryngol Head Neck Surg 2000;122:643–6. [DOI] [PubMed] [Google Scholar]