Abstract
Background
There are several meta-analyses on the genetic relationship between the rs1695 polymorphism within the GSTP1 (glutathione S-transferase pi 1) gene and the risk of different SCC (squamous cell carcinoma) diseases, such as ESCC (oesophageal SCC), HNSCC (head and neck SCC), LSCC (lung SCC), and SSCC (skin SCC). Nevertheless, no unified conclusions have been drawn.
Methods
Herein, an updated meta-analysis was performed to evaluate the probable impact of GSTP1 rs1695 on the susceptibility to different SCC diseases under six genetic models (allele, carrier, homozygote, heterozygote, dominant, and recessive). Three online databases, namely, PubMed, WOS (Web of Science), and Embase (Excerpta Medica Database), were searched.
Results
Initially, we obtained a total of 497 articles. Based on our selection criteria, we eventually included 52 case-control studies (9763 cases/15,028 controls) from 47 eligible articles. As shown in the pooling analysis, there was no difference in the risk of overall SCC disease between cases and controls [allele, Pa (P value of association test) = 0.601; carrier, Pa = 0.587; homozygote, Pa = 0.689; heterozygote, Pa = 0.167; dominant, Pa = 0.289; dominant, Pa = 0.548]. Similar results were obtained after stratification by race (Asian/Caucasian), genotyping, control source, and disease type (ESCC/HNSCC/LSCC/SSCC) (all Pa > 0.05).
Conclusion
The rs1695 polymorphism within the GSTP1 gene is not associated with the risk of overall SCC or a specific SCC type, including ESCC, HNSCC, LSCC, and SSCC.
Keywords: GSTP1, Polymorphism, Squamous cell carcinoma, Susceptibility
Background
SCC (squamous cell carcinoma), also termed “epidermal carcinoma,” is a malignant tumour that takes part in epidermis or adnexal cells and exhibits distinct degrees of keratosis [1–3]. SCC exists in the squamous epithelium of several places, e.g., skin, mouth, lung, lips, oesophagus, cervix, and vagina [4–6]. Based on GWAS (genome-wide association study) data, more and more reported genetic polymorphisms are believed to contribute to the aetiologies of different SCC types. For instance, a series of genes, including CADM1 (cell adhesion molecule 1), AHR (aryl hydrocarbon receptor), and SEC16A (SEC16 homolog A, endoplasmic reticulum export factor), may be related with the risk of SCC [7]. Two variants within the KLF5 (Kruppel-like factor 5) gene on chromosome 13q22.1, namely, rs1924966 and rs115797771, may be relevant to ESCC (oesophageal SCC) susceptibility [8]. Herein, we determined whether GSTP1 (glutathione S-transferase pi 1) gene polymorphism is associated with the susceptibility to different SCC patterns.
GSTP1, a member of the GST (glutathione S-transferase) family in humans, is associated with the biological detoxification or biotransformation process through catalysing the conjugation of many hydrophobic and electrophilic compounds with reduced glutathione [9, 10]. The GSTP1 gene, which is located on human chromosome 11q13, comprises seven exons and six introns [11]. Two common polymorphisms, namely, rs1695 A/G polymorphism in exon five (p.Ile105Val) and rs1138272 C/T polymorphism in exon six (p.Ala114Val), have been reported [12, 13].
Several SCC/GSTP1 rs1695-associated meta-analyses with conflicting conclusions have been reported. For instance, in 2009, Zendehdel et al. enrolled three case-control studies [14–16], performed a meta-analysis to assess the association between GSTP1 rs1695 and ESCC risk in Caucasian populations, and found a borderline significant association [16]. In 2014, Song et al. enrolled 21 case-control studies to perform a meta-analysis concerning the role of the GSTP1 rs1695 polymorphism in the risk of oesophageal cancers, including EAC (oesophageal adenocarcinoma) and ESCC [17]. The subgroup meta-analysis of ESCC containing thirteen case-control studies showed a positive correlation, particularly in the Caucasian population [17]. However, in 2015, Tan et al. performed another meta-analysis with twenty case-control studies on overall oesophageal cancer and reported negative results in both ESCC and EAC subgroups [18]. Accordingly, we performed an updated meta-analysis with a relatively larger sample size to reevaluate the potential impact of the GSTP1 rs1695 A/G polymorphism on the susceptibility to SCC diseases, mainly including ESCC, SSCC, HNSCC (head and neck SCC), and LSCC (lung SCC).
Methods
Electronic database retrieval
We reviewed three on-line databases, including PubMed, WOS (Web of Science), and Embase (Excerpta Medica Database), through January 2018 using the following main search keywords: Carcinoma, Squamous Cell; Carcinomas, Squamous Cell; Squamous Cell Carcinomas; Squamous Cell Carcinoma; Carcinoma, Squamous; Carcinomas, Squamous; Squamous Carcinoma; Squamous Carcinomas; Carcinoma, Epidermoid; Carcinomas, Epidermoid; Epidermoid Carcinoma; Epidermoid Carcinomas; Carcinoma, Planocellular; Carcinomas, Planocellular; Planocellular Carcinoma; Planocellular Carcinomas; SCC; GSTP1; Glutathione S-Transferase pi; Glutathione S Transferase pi; GST Class-phi; Class-phi, GST; GST Class phi; Glutathione Transferase P1–1; Glutathione Transferase P1 1; Transferase P1–1, Glutathione; GSTP1 Glutathione D-Transferase; D-Transferase, GSTP1 Glutathione; GSTP1 Glutathione D Transferase; Glutathione D-Transferase, GSTP1; Polymorphism; Polymorphism, Genetic; Polymorphisms, Genetic; Genetic Polymorphisms; Genetic Polymorphism; Polymorphism (Genetics); Polymorphisms (Genetics); and Polymorphism; Polymorphisms.
Eligible article screening
We performed a literature search and screened the retrieved articles as per the PRISMA (preferred reporting items for systematic reviews and meta-analyses) guidelines [19]. Selection criteria included duplicated articles; data from animal or cell experiments; meeting abstract or meta-analysis; review, trials or case reports; data of GSTP1 expression; not SCC or GSTP1; lack confirmed histopathological data; combined GA + AA genotype frequency; without the control data; and P value of HWE (Hardy-Weinberg equilibrium) less than 0.05. Eligible case-control studies provided sufficient genotype frequency data of the GSTP1 gene rs1695 polymorphism in each case and control group.
Data extraction
Two investigators independently extracted the data and evaluated the methodological quality of each article by means of the NOS (Newcastle-Ottawa Scale) system. One table contains the following basic information: first author, publication year, region, race, genotyping assay, genotype frequency, disease type, control source, P values of HWE, study number, and sample size of the case/control.
Data synthesis
We utilized STATA software (StataCorp LP, College Station, TX, USA) for the following statistical analyses. The allele (allele G vs. A), carrier (carrier G vs. A), homozygote (GG vs. AA), heterozygote (AG vs. AA), dominant (AG + GG vs. AA), and recessive (GG vs. AA+AG) models were utilized to target the GSTP1 gene rs1695 G/A polymorphism. We calculated the OR (odds ratio), 95% CIs (confidence intervals) and Pa (P value of association test) values to estimate the association. When the Ph (P value of heterogeneity) was > 0.1 or I2 was < 50.0%, a fixed-effects model was adopted. Otherwise, a random-effects model was selected.
Considering the factors of race, genotyping assay, control source, and disease type, we performed the corresponding subgroup meta-analyses. We also carried out Egger’s/Begg’s tests to determine a potential publication bias. The presence of a publication bias was considered when PE (P value of Egger’s test) and PB (P value of Begg’s test) were below 0.05. Sensitivity analysis was applied to assess data stability and robustness.
Results
Article retrieval and screening
The article retrieval and selection processes during our meta-analysis were conducted as described in the flow chart shown in Fig. 1. After our literature search, a total of 497 articles were obtained. Then, 168 articles with duplicated data and 214 articles meeting the exclusion criteria were excluded. Next, we assessed the eligibility of the remaining 115 full-text articles. After the exclusion of 68 ineligible articles, a total of 47 articles containing 52 case-control studies [14–16, 20–63] were ultimately recruited for our meta-analysis. Table 1 summarizes the extracted basic information.
Fig. 1.
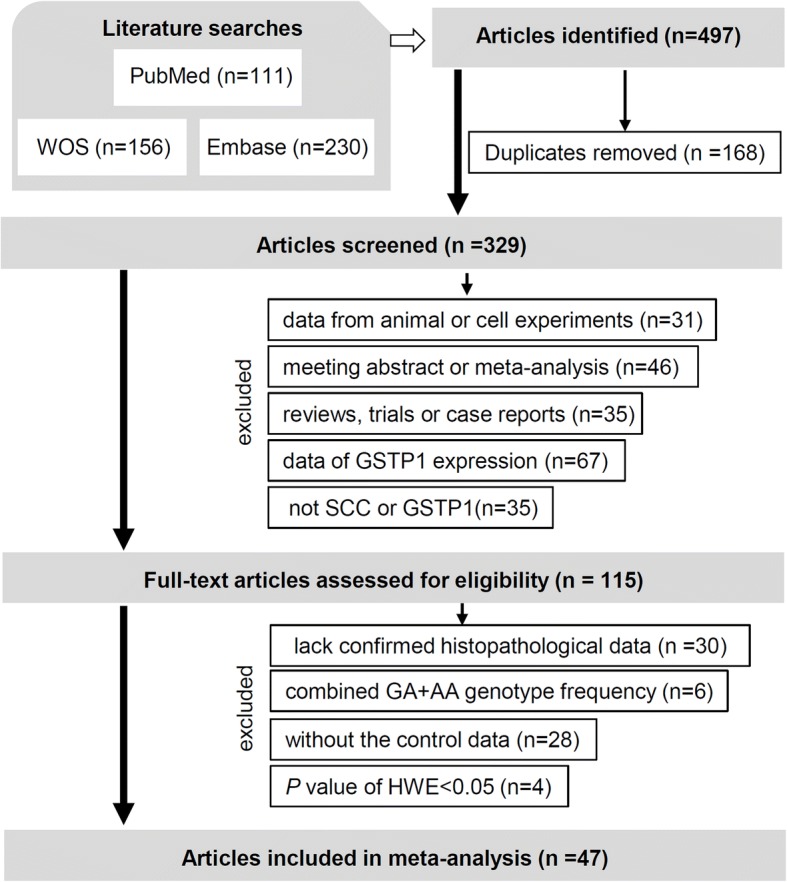
Flow chart of eligible article selection
Table 1.
Basic information of the eligible articles in the meta-analysis
| First author | Year | Region | Race | Assay | Case | Disease type | Control | Control source | P HWE | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AA | AG | GG | AA | AG | GG | ||||||||
| Abbas | 2004 | France | Caucasian | PCR-RFLP | 21 | 21 | 3 | ESCC | 59 | 56 | 9 | PB | 0.38 |
| Cabelguenne | 2001 | France | Caucasian | PCR-RFLP | 89 | 57 | 16 | HNSCC | 146 | 139 | 25 | HB | 0.31 |
| Cai | 2006 | China | Asian | PCR-RFLP | 143 | 58 | 3 | ESCC | 265 | 116 | 12 | PB | 0.87 |
| Cho | 2006 | Korea | Asian | Gene sequencing | 201 | 85 | 7 | HNSCC | 211 | 112 | 10 | HB | 0.29 |
| Dura | 2013 | Netherlands | Caucasian | PCR | 48 | 42 | 15 | ESCC | 246 | 261 | 84 | PB | 0.27 |
| Dzian | 2012 | Netherlands | Caucasian | PCR-RFLP | 56 | 45 | 11 | LSCC | 153 | 115 | 22 | PB/HB | 0.95 |
| Evans | 2004 | USA | Caucasian | PCR-RFLP | 123 | 132 | 27 | HNSCC | 97 | 85 | 24 | PB | 0.42 |
| Fryer | 2005 | Australia | Caucasian | PCR-RFLP | 59 | 51 | 18 | SSCC | 95 | 90 | 25 | HB | 0.60 |
| Harth | 2008 | Germany | Caucasian | PCR-melting-curve | 145 | 122 | 45 | HNSCC | 130 | 138 | 32 | HB | 0.62 |
| Jain | 2006 | India | Asian | PCR-RFLP | 46 | 23 | 7 | ESCC | 72 | 56 | 9 | HB | 0.67 |
| Jourenkova | 1999a | France | Caucasian | PCR-RFLP | 49 | 53 | 15 | HNSCC | 86 | 64 | 22 | HB | 0.07 |
| Jourenkova | 1999b | France | Caucasian | PCR-RFLP | 62 | 52 | 15 | HNSCC | 86 | 64 | 22 | HB | 0.07 |
| Jourenkova | 1998 | France | Caucasian | PCR-RFLP | 46 | 41 | 11 | LSCC | 86 | 64 | 22 | HB | 0.07 |
| Kelders | 2002 | Netherlands | Caucasian | PCR-RFLP | 36 | 38 | 13 | HNSCC | 26 | 18 | 7 | HB | 0.20 |
| Kihara | 1999 | Japan | Asian | PCR-RFLP | 84 | 32 | 9 | LSCC | 184 | 65 | 8 | HB | 0.45 |
| Larsen | 2006 | Australia | Caucasian | PCR-RFLP | 230 | 213 | 51 | LSCC | 161 | 169 | 49a | HB | 0.66 |
| Australia | Caucasian | PCR-RFLP | 230 | 213 | 51 | LSCC | 112 | 100 | 35b | PB | 0.11 | ||
| Leichsenring | 2006 | Brazil | Mixed | PCR-RFLP | 30 | 34 | 8 | HNSCC | 30 | 25 | 5 | PB | 0.95 |
| Leite | 2007 | Brazil | Mixed | PCR-RFLP | 14 | 13 | 2 | SSCC | 60 | 46 | 18 | PB | 0.07 |
| Lewis | 2002 | UK | Caucasian | PCR-RFLP | 14 | 17 | 1 | LSCC | 64 | 74 | 13 | HB | 0.19 |
| Li | 2010 | South African | Black African | PCR-RFLP | 56 | 59 | 26 | ESCC | 76 | 83 | 27 | PB | 0.58 |
| Mixed | PCR-RFLP | 34 | 52 | 11 | ESCC | 30 | 51 | 13 | PB | 0.24 | |||
| Li | 2007 | USA | Caucasian | PCR-RFLP | 336 | 356 | 111 | HNSCC | 333 | 385 | 121 | PB | 0.57 |
| Liang | 2005 | China | Asian | diASA-AMP | 58 | 32 | 4 | LSCC | 132 | 86 | 9 | HB | 0.27 |
| Liu | 2010 | China | Asian | PCR-RFLP | 66 | 29 | 0 | ESCC | 61 | 27 | 3 | PB | 1.00 |
| Malik | 2010 | India | Asian | PCR-RFLP | 53 | 36 | 14 | ESCC | 111 | 75 | 9 | PB | 0.41 |
| Matejcic | 2011 | South African | Black African | TaqMan genotyping | 79 | 155 | 91 | ESCC | 100 | 242 | 132 | PB | 0.57 |
| South African | Mixed | TaqMan genotyping | 69 | 112 | 48 | ESCC | 145 | 191 | 92 | PB | 0.05 | ||
| McWilliams | 2000 | USA | Mixed | PCR-RFLP | 60 | 73 | 13 | HNSCC | 58 | 51 | 15 | HB | 0.47 |
| Miller | 2006 | USA | Caucasian | PCR-RFLP | 190 | 173 | 49 | LSCC | 579 | 623 | 141 | PB | 0.16 |
| Moaven | 2010 | Iran | Asian | PCR-RFLP | 84 | 50 | 14 | ESCC | 74 | 54 | 8 | PB | 0.65 |
| Nazar | 2003 | USA | Mixed | PCR-RFLP | 35 | 29 | 9 | LSCC | 199 | 234 | 54 | PB | 0.23 |
| Olshan | 2000 | USA | Mixed | PCR-RFLP | 40 | 62 | 7 | HNSCC | 68 | 80 | 20 | HBc | 0.63 |
| USA | Mixed | PCR-RFLP | 18 | 38 | 7 | HNSCC | 7 | 13 | 5 | HBd | 0.82 | ||
| Oude | 2003 | Netherlands | Caucasian | PCR-RFLP | 116 | 90 | 29 | HNSCC | 125 | 121 | 39 | PB | 0.27 |
| Peters | 2006 | USA | Mixed | PCR-RFLP | 303 | 311 | 76 | HNSCC | 333 | 329 | 86 | PB | 0.73 |
| Ramsay | 2001 | UK | Caucasian | SSCP | 10 | 10 | 0 | SSCC | 53 | 71 | 17 | HB | 0.36 |
| Risch | 2001 | Germany | Caucasian | PCR-RFLP | 76 | 77 | 18 | LSCC | 167 | 151 | 35 | HB | 0.92 |
| Rossini | 2007 | Brazil | Mixed | PCR-RFLP | 42 | 65 | 18 | ESCC | 116 | 108 | 28 | PB | 0.71 |
| Ruwali | 2009 | India | Caucasian | PCR-RFLP | 224 | 112 | 14 | HNSCC | 199 | 138 | 13 | PB | 0.06 |
| Ruwali | 2011 | India | Caucasian | PCR-RFLP | 316 | 162 | 22 | HNSCC | 285 | 195 | 20 | PB | 0.06 |
| Ryberg | 1997 | Norway | Caucasian | PCR-RFLP | 20 | 34 | 13 | LSCC | 153 | 117 | 27 | PB | 0.50 |
| Schneider | 2004 | Germany | Caucasian | PCR-melting-curve | 81 | 75 | 27 | LSCC | 298 | 254 | 70 | PB/HB | 0.16 |
| Soucek | 2010 | Czech/Polish | Caucasian | TaqMan drug metabolism genotyping | 56 | 53 | 7 | HNSCC | 57 | 50 | 10 | PB | 0.52 |
| Soya | 2007 | India | Asian | PCR-RFLP | 219 | 162 | 27 | UADTSCC | 120 | 88 | 12 | PB | 0.42 |
| Stücker | 2002 | France | Caucasian | PCR-RFLP | 54 | 46 | 15 | LSCC | 124 | 120 | 20 | HB | 0.22 |
| Tan | 2000 | China | Asian | PCR-RFLP | 93 | 48 | 9 | ESCC | 91 | 53 | 6 | PB | 0.62 |
| To | 2002 | Spain | Caucasian | PCR-RFLP | 101 | 84 | 19 | HNSCC | 100 | 78 | 23 | PB | 0.20 |
| To | 1999 | Spain | Caucasian | PCR-RFLP | 29 | 20 | 3 | LSCC | 64 | 54 | 14 | PBb | 0.61 |
| Spain | Caucasian | PCR-RFLP | 29 | 20 | 3 | LSCC | 90 | 90 | 20 | PBe | 0.72 | ||
| van | 1999 | Netherlands | Caucasian | PCR-RFLP | 5 | 6 | 2 | ESCC | 146 | 89 | 12 | PB | 0.74 |
| Zendehdel | 2009 | Sweden | Caucasian | Pyrosequencing | 26 | 42 | 10 | ESCC | 208 | 207 | 38 | PB | 0.18 |
PCR polymerase chain reaction, PCR-RFLP polymerase chain reaction-restriction fragment length polymorphism, diASA-AMP di-allele-specific-amplification with artificially modified primers assay, SSCP Single-stranded conformational polymorphism, ESCC oesophageal squamous cell carcinoma, HNSCC head and neck squamous cell carcinoma, LSCC lung squamous cell carcinoma, SSCC skin squamous cell carcinoma, OSCC oral squamous cell carcinoma, UADTSCC upper aerodigestive tract squamous cell carcinoma, PB population-based, HB hospital-based, PHWE P value of hardy-weinberg equilibrium
aCOPD patients without LSCC, bhealthy smokers; ccontrol from Caucasian population; dcontrol from Black African population; econtrol from general population
Overall meta-analysis
First, we performed the overall meta-analysis, which included 52 case-control studies with 9763 cases and 15,028 controls (Table 2). The fixed-effects model was applied in all meta-analyses, because no substantial between-study heterogeneity was detected [Table 2, I2 value < 50.0%, Ph > 0.1]. As shown in Table 2, no altered susceptibility to SCC disease in cases was observed compared with controls [allele, Pa = 0.601; carrier, Pa = 0.587; homozygote, Pa = 0.689; heterozygote, Pa = 0.167; dominant, Pa = 0.289; dominant, Pa = 0.548]. These data suggest that the rs1695 polymorphism within the GSTP1 gene does not contribute to the risk of overall SCC.
Table 2.
Meta-analysis of the GSTP1 rs1695 A/G polymorphism
| Statistical analysis | Index | Allele | Carrier | Homozygote | Heterozygote | Dominant | Recessive |
|---|---|---|---|---|---|---|---|
| Association | OR | 0.99 | 0.99 | 1.02 | 0.96 | 0.97 | 1.03 |
| 95% CIs | 0.95~1.03 | 0.94~1.03 | 0.93~1.12 | 0.91~1.02 | 0.92~1.03 | 0.94~1.12 | |
| P a | 0.601 | 0.587 | 0.689 | 0.167 | 0.289 | 0.548 | |
| Sample size | case | 9763 | 9763 | 9763 | 9763 | 9763 | 9763 |
| control | 15,028 | 15,028 | 15,028 | 15,028 | 15,028 | 15,028 | |
| study | 52 | 52 | 52 | 52 | 52 | 52 | |
| Heterogeneity | I2 | 15.5% | 0.0% | 9.7% | 7.7% | 11.8% | 1.2% |
| P h | 0.174 | 0.999 | 0.278 | 0.318 | 0.239 | 0.450 | |
| Model | Fixed | Fixed | Fixed | Fixed | Fixed | Fixed | |
| Egger’s test | t | 1.14 | 1.38 | 0.13 | 2.36 | 2.16 | −0.31 |
| P E | 0.259 | 0.175 | 0.899 | 0.022 | 0.036 | 0.760 | |
| Begg’s test | z | 0.53 | 0.84 | 0.77 | 1.96 | 1.82 | 1.29 |
| P B | 0.597 | 0.398 | 0.444 | 0.049 | 0.068 | 0.198 |
OR odds ratio, CIs confidence intervals, Pa, P value of association test, Ph, P value of heterogeneity test, PE, P value of Egger’s test, PB, P value of Begg’s test
Subgroup analysis
Next, we performed additional subgroup meta-analyses according to the factors of race (Asian/Caucasian), genotyping assay (PCR-RFLP), control source (PB/HB), and disease type (ESCC/HNSCC/LSCC/SSCC). As shown in Tables 3 and 4, there were no significant associations in any subgroup analysis for all genetic models tested (all Pa > 0.05). The forest plot of the subgroup analysis by disease type under the allele model is shown in Fig. 2.
Table 3.
Subgroup analysis of the GSTP1 rs1695 A/G polymorphism by race, genotyping assay and control source
| Factor | Subgroup | Index | Allele | Carrier | Homozygote | Heterozygote | Dominant | Recessive |
|---|---|---|---|---|---|---|---|---|
| Race | Asian | OR (95% CIs) | 1.00 (0.89~1.12) | 0.98 (0.86~1.11) | 1.29 (0.94~1.76) | 0.90 (0.78~1.04) | 0.94 (0.82~1.08) | 1.35 (0.99~1.83) |
| P a | 0.948 | 0.716 | 0.114 | 0.139 | 0.361 | 0.058 | ||
| Case/control | 1696/2139 | 1696/2139 | 1696/2139 | 1696/2139 | 1696/2139 | 1696/2139 | ||
| Study number | 10 | 10 | 10 | 10 | 10 | 10 | ||
| Race | Caucasian | OR (95% CIs) | 0.98 (0.93~1.03) | 0.98 (0.82~1.04) | 1.00 (0.89~1.12) | 0.94 (0.87~1.01) | 0.95 (0.89~1.02) | 1.02 (0.91~1.14) |
| P a | 0.358 | 0.447 | 0.984 | 0.099 | 0.153 | 0.716 | ||
| Case/control | 5968/9719 | 5968/9719 | 5968/9719 | 5968/9719 | 5968/9719 | 5968/9719 | ||
| Study number | 30 | 30 | 30 | 30 | 30 | 30 | ||
| genotyping assay | PCR-RFLP | OR (95% CIs) | 0.99 (0.94~1.03) | 0.99 (0.93~1.04) | 1.01 (0.91~1.12) | 0.96 (0.90~1.03) | 0.97 (0.91~1.03) | 1.01 (0.91~1.12) |
| P a | 0.542 | 0.579 | 0.874 | 0.260 | 0.351 | 0.824 | ||
| Case/control | 8008/11,342 | 8008/11,342 | 8008/11,342 | 8008/11,342 | 8008/11,342 | 8008/11,342 | ||
| Study number | 42 | 42 | 42 | 42 | 42 | 42 | ||
| control source | PB | OR (95% CIs) | 0.98 (0.94~1.03) | 0.98 (0.93~1.04) | 1.00 (0.90~1.12) | 0.96 (0.89~1.03) | 0.96 (0.90~1.03) | 1.02 (0.92~1.13) |
| P a | 0.519 | 0.572 | 0.943 | 0.214 | 0.287 | 0.751 | ||
| Case/control | 6697/10,170 | 6697/10,170 | 6697/10,170 | 6697/10,170 | 6697/10,170 | 6697/10,170 | ||
| Study number | 31 | 31 | 31 | 31 | 31 | 31 | ||
| control source | HB | OR (95% CIs) | 0.98 (0.91~1.06) | 0.98 (0.90~1.07) | 1.00 (0.84~1.20) | 0.95 (0.86~1.06) | 0.96 (0.87~1.07) | 1.01 (0.85~1.19) |
| P a | 0.586 | 0.638 | 0.977 | 0.377 | 0.461 | 0.944 | ||
| Case/control | 2771/3946 | 2771/3946 | 2771/3946 | 2771/3946 | 2771/3946 | 2771/3946 | ||
| Study number | 19 | 19 | 19 | 19 | 19 | 19 |
Pa, P value of association test
PCR-RFLP polymerase chain reaction-restriction fragment length polymorphism, PB population-based, HB hospital-based, OR odds ratio, CIs confidence intervals
Table 4.
Subgroup analysis of the GSTP1 rs1695 A/G polymorphism by SCC type
| Subgroup | Index | Allele | Carrier | Homozygote | Heterozygote | Dominant | Recessive |
|---|---|---|---|---|---|---|---|
| ESCC | OR (95% CIs) | 1.05 (0.96~1.15) | 1.03 (0.93~1.14) | 1.15 (0.95~1.39) | 1.00 (0.88~1.14) | 1.03 (0.92~1.17) | 1.13 (0.95~1.34) |
| P a | 0.263 | 0.568 | 0.155 | 0.970 | 0.575 | 0.160 | |
| Case/control | 1934/3951 | 1934/3951 | 1934/3951 | 1934/3951 | 1934/3951 | 1934/3951 | |
| Study number | 15 | 15 | 15 | 15 | 15 | 15 | |
| HNSCC | OR (95% CIs) | 0.95 (0.89~1.01) | 0.96 (0.89~1.03) | 0.94 (0.82~1.09) | 0.94 (0.87~1.02) | 0.93 (0.86~1.01) | 0.95 (0.83~1.09) |
| P a | 0.112 | 0.247 | 0.408 | 0.131 | 0.102 | 0.459 | |
| Case/control | 4671/4961 | 4671/4961 | 4671/4961 | 4671/4961 | 4671/4961 | 4671/4961 | |
| Study number | 18 | 18 | 18 | 18 | 18 | 18 | |
| LSCC | OR (95% CIs) | 1.00 (0.93~1.08) | 1.00 (0.92~1.09) | 1.04 (0.88~1.24) | 0.97 (0.87~1.07) | 0.98 (0.89~1.09) | 1.06 (0.90~1.25) |
| P a | 0.940 | 0.973 | 0.616 | 0.526 | 0.741 | 0.485 | |
| Case/control | 2574/5421 | 2574/5421 | 2574/5421 | 2574/5421 | 2574/5421 | 2574/5421 | |
| Study number | 15 | 15 | 15 | 15 | 15 | 15 | |
| SSCC | OR (95% CIs) | 0.91 (0.70~1.19) | 0.94 (0.69~1.28) | 0.83 (0.46~1.49) | 0.94 (0.64~1.36) | 0.91 (0.64~1.30) | 0.86 (0.49~1.51) |
| P a | 0.493 | 0.688 | 0.532 | 0.728 | 0.605 | 0.597 | |
| Case/control | 177/475 | 177/475 | 177/475 | 177/475 | 177/475 | 177/475 | |
| Study number | 3 | 3 | 3 | 3 | 3 | 3 |
ESCC oesophageal squamous cell carcinoma, HNSCC head and neck squamous cell carcinoma, LSCC lung squamous cell carcinoma, SSCC skin squamous cell carcinoma, OR odds ratio, CIs confidence intervals, Pa, P value of association test
Fig. 2.
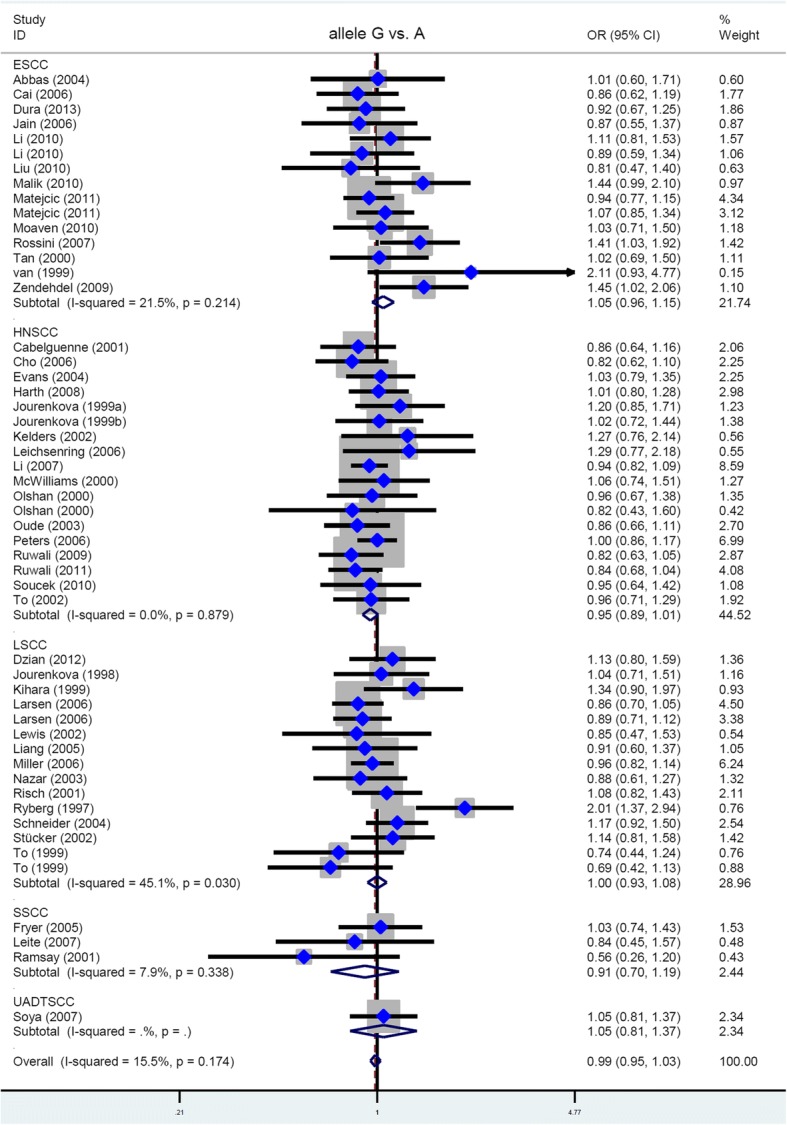
Data of subgroup analysis by SCC type (allele model)
Furthermore, we included all case-controls studies regarding the specific SCC type and conducted a series of subgroup analyses by race and control source. However, similar results were obtained (data not shown). As a result, the GSTP1 gene rs1695 polymorphism is not likely related to the genetic susceptibility of a specific SCC type, including ESCC, HNSCC, LSCC, and SSCC.
Publication bias and sensitivity analysis
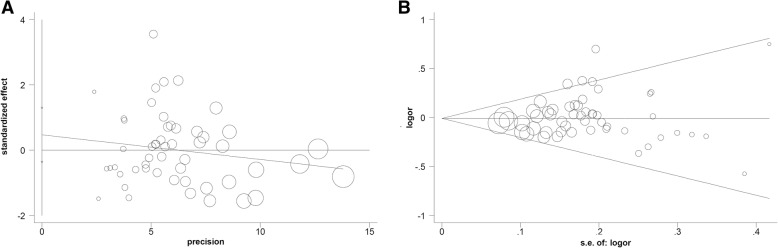
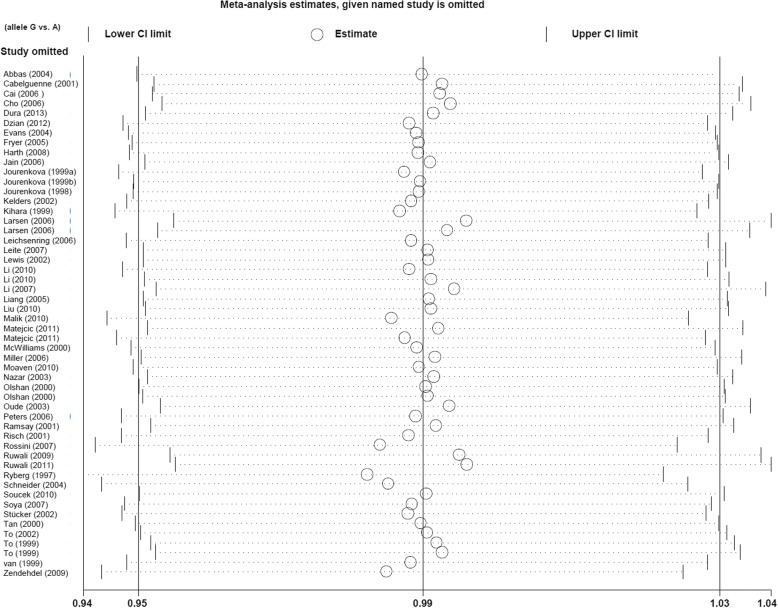
The publication bias analysis data obtained from Egger’s and Begg’s tests are shown in Table 2. There was no remarkable publication bias in most genetic models (PE > 0.05, PB > 0.05), except for the heterozygote (PE = 0.022, PB = 0.049) and dominant (PE = 0.036) models. The funnel plot (allele model) is displayed in Fig. 3a-b. Moreover, our sensitivity analysis led us to consider the stability of the data. Figure 4 shows a representative example of the sensitivity analysis (allele model).
Fig. 3.
Funnel plot of publication bias analysis. a Egger’s test; b Begg’s test
Fig. 4.
Sensitivity analysis data (allele model)
Discussion
In the current meta-analysis, we first focused on the genetic relationship between the GSTP1 rs1695 A/G polymorphism and the risk of overall SCC and then conducted subgroup analyses by the specific histological status. After rigorous screening, four main types of SCC, namely, ESCC, HNSCC, ESCC, and SSCC, were targeted.
ESCC, a type of squamous epithelium differentiation of a malignant tumour within the oesophagus, accounts for the vast majority of oesophageal cancers [64, 65]. ESCC often presents in physiological or pathological stenosis of the oesophagus, and genetic factors, carcinogens, and/or chronic irritants may contribute to the pathogenesis of ESCC [64, 65]. The GSTP1 rs1695 A/G polymorphism is significantly related to the risk of ESCC in the Kashmiri population [42]. Similarly, GSTP1 rs1695 may be an independent risk factor for ESCC in Western populations [53]. Nevertheless, different associations were detected in other reports. For instance, no difference between unrelated controls and ESCC cases was observed in a French population [14] or a Chinese population [61]. Therefore, a meta-analysis was required to comprehensively evaluate the role of the GSTP1 rs1695 A/G polymorphism in ESCC risk. Herein, we recruited 15 case-control studies involving 1934 cases and 3951 controls and performed a new meta-analysis to examine the association between the GSTP1 rs1695 A/G polymorphism and ESCC susceptibility. The carrier (carrier G vs. A) model, as well as the allele, homozygote, heterozygote, dominant and recessive genetic models, was used. Our results in the stratified analysis of specific ESCCs are consistent with the data of Tan et al. [18].
Similarly, inconsistent results regarding an association between the GSTP1 rs1695 A/G polymorphism and LSCC risk have been reported in different races and geographical locations [24, 31, 33, 34, 37, 40, 45, 47, 52, 56, 57, 60, 63]. Here, we failed to detect a positive correlation between GSTP1 rs1695 and LSCC susceptibility, consistent with the prior meta-analysis of Feng in 2013 [66] and Xu in 2014 [67].
Head and neck cancer comprises cancers of the mouth, nose, sinuses, salivary glands, throat, and lymph nodes in the neck, and HNSCC is the major pathologic type [68]. In 2012, Lang et al. enrolled 28 case-control studies to perform a meta-analysis regarding the genetic effect of the GSTP1 rs1695 A/G polymorphism on overall head and neck cancer [69]. The authors were unable to identify a positive association between the GSTP1 rs1695 A/G polymorphism and the risk of overall head and neck cancer. Nevertheless, the potential role of GSTP1 rs1695 in the susceptibility to HNSCC was not assessed. Therefore, we performed a subgroup meta-analysis of HNSCC involving 18 case-control studies, but did not identify an association between GSTP1 rs1695 and HNSCC risk.
SSCC, SBCC (skin basal cell carcinoma) and (MM malignant melanoma) are the three main types of cutaneous cancer [4]. Herein, we did not identify an association between the GSTP1 rs1695 A/G polymorphism and SSCC risk, consistent with the prior meta-analyses regarding the correlation between GSTP1 rs1695 and the susceptibility to cutaneous cancer in 2015 [70, 71].
Human GST family genes, mainly including GSTA (glutathione S-transferase alpha), GSTM1 (glutathione S-transferase mu 1), GSTT1 (glutathione S-transferase theta 1) and GSTP1, encode phase II enzymes and are thus important for the body defence, metabolic detoxification of mutagens or chemical drugs, or cellular elimination of carcinogens [9, 10]. The rs1695 A/G polymorphism within the GSTP1 gene can result in the substitution of Ile (isoleucine) for Val (valine) at amino acid position 105, which may lower the cytosolic enzyme activity of GSTP1 protein [72, 73]. Although significant associations were not obtained in our overall meta-analysis or subgroup analyses by pathological type, we cannot rule out the potential genetic effect of the GSTP1 rs1695 A/G polymorphism.
There are still some limitations to our meta-analysis that should be clarified. Even though our findings were considered reliable by our sensitivity analysis and publication bias assessment, more eligible investigations are still warranted to further enhance the statistical power. We note that population-based controls were not utilized in each case-control study. The currently available data of genotypic and allelic frequency from the on-line databases led us to only target the rs1695 polymorphism of the GSTP1 gene. Other possible functional polymorphisms of the GSTP1 gene, such as rs1138272, or relative haplotypes will be important to examine in the future. We should also pay attention to the genetic relationship between GSTP1/GSTM1/GSTT1 polymorphisms and the risk of SCC.
Conclusion
In general, based on the currently published data, the GSTP1 gene rs1695 polymorphism is not associated with the susceptibility to overall SCC diseases, including ESCC, HNSCC, LSCC, and skin SCC. The confirmation or refutation of this conclusion merits further evidence.
Acknowledgements
Not applicable.
Funding
This study was supported in part by a grant of Science Foundation from Tianjin Municipal Commission of Health and Family Planning (2015KY11).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AHR
Aryl hydrocarbon receptor
- CADM1
Cell adhesion molecule 1
- diASA-AMP
Di-allele-specific- amplification with artificially modified primers assay
- Embase
Excerpta Medica Database
- ESCC
Oesophageal squamous cell carcinoma
- GST
Glutathione S-transferase
- GSTA
Glutathione S-transferase alpha
- GSTM1
Glutathione S-transferase mu 1
- GSTP1
Glutathione S-transferase pi 1
- GSTT1
Glutathione S-transferase theta 1
- GWAS
Genome-wide association study
- HB
Hospital-based
- HNSCC
Head and neck squamous cell carcinoma
- HWE
Hardy-Weinberg equilibrium
- KLF5
Kruppel like factor 5
- LSCC
Lung squamous cell carcinoma
- MM
Malignant melanoma
- OSCC
Oral squamous cell carcinoma
- PB
Population-based
- PCR
Polymerase chain reaction
- PCR-RFLP
Polymerase chain reaction-restriction fragment length polymorphism
- SBCC
Skin basal cell carcinoma
- SCC
Squamous cell carcinoma
- SEC16A
SEC16 homolog A, endoplasmic reticulum export factor
- SSCC
Skin squamous cell carcinoma
- SSCP
Single-stranded conformational polymorphism
- UADTSCC
Upper aerodigestive tract squamous cell carcinoma
- WOS
Web of Science
Authors’ contributions
SW and ZB designed the study. SW, JZ and FJ extracted, analyzed, and interpreted the data. SW and ZB drafted the manuscript. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shuang Wang, Email: willa770612@163.com.
Jingqi Zhang, Email: zjq20071029@163.com.
Fan Jun, Email: feixueyizu1981@163.com.
Zhijie Bai, Email: bzjky1127@126.com.
References
- 1.Que SKT, Zwald FO, Schmults CD. Cutaneous squamous cell carcinoma: management of advanced and high-stage tumors. J Am Acad Dermatol. 2018;78(2):249–261. doi: 10.1016/j.jaad.2017.08.058. [DOI] [PubMed] [Google Scholar]
- 2.Wang C, Wang J, Chen Z, Gao Y, He J. Immunohistochemical prognostic markers of esophageal squamous cell carcinoma: a systematic review. Chin J Cancer. 2017;36(1):65. doi: 10.1186/s40880-017-0232-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bann DV, Deschler DG, Goyal N. Novel Immunotherapeutic Approaches for Head and Neck Squamous Cell Carcinoma. Cancers (Basel). 2016;8(10). [DOI] [PMC free article] [PubMed]
- 4.Liu N, Liu GJ, Liu J. Genetic association between TNF-alpha promoter polymorphism and susceptibility to squamous cell carcinoma, basal cell carcinoma, and melanoma: a meta-analysis. Oncotarget. 2017;8(32):53873–53885. doi: 10.18632/oncotarget.17179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang X, He R, Ren F, Tang R, Chen G. Association of miR-146a rs2910164 polymorphism with squamous cell carcinoma risk: a meta-analysis. J buon. 2015;20(3):829–841. [PubMed] [Google Scholar]
- 6.Yu H, Li H, Zhang J, Liu G. Influence of MDM2 polymorphisms on squamous cell carcinoma susceptibility: a meta-analysis. Onco Targets Ther. 2016;9:6211–6224. doi: 10.2147/OTT.S113417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chahal HS, Lin Y, Ransohoff KJ, Hinds DA, Wu W, Dai HJ, Qureshi AA, Li WQ, Kraft P, Tang JY, et al. Genome-wide association study identifies novel susceptibility loci for cutaneous squamous cell carcinoma. Nat Commun. 2016;7:12048. doi: 10.1038/ncomms12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang J, Wei L, Miao X, Yu D, Tan W, Zhang X, Wu C, Lin D. Two novel variants on 13q22.1 are associated with risk of esophageal squamous cell carcinoma. Cancer Epidemiol Biomark Prev. 2015;24(11):1774–1780. doi: 10.1158/1055-9965.EPI-15-0154-T. [DOI] [PubMed] [Google Scholar]
- 9.Schnekenburger M, Karius T, Diederich M. Regulation of epigenetic traits of the glutathione S-transferase P1 gene: from detoxification toward cancer prevention and diagnosis. Front Pharmacol. 2014;5:170. doi: 10.3389/fphar.2014.00170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marchewka Z, Piwowar A, Ruzik S, Dlugosz A. Glutathione S - transferases class pi and mi and their significance in oncology. Postepy Hig Med Dosw (Online) 2017;71(0):541–550. doi: 10.5604/01.3001.0010.3835. [DOI] [PubMed] [Google Scholar]
- 11.Yuan Y, Qian ZR, Sano T, Asa SL, Yamada S, Kagawa N, Kudo E. Reduction of GSTP1 expression by DNA methylation correlates with clinicopathological features in pituitary adenomas. Mod Pathol. 2008;21(7):856–865. doi: 10.1038/modpathol.2008.60. [DOI] [PubMed] [Google Scholar]
- 12.Hollman AL, Tchounwou PB, Huang HC. The association between Gene-environment interactions and diseases involving the human GST superfamily with SNP variants. Int J Environ Res Public Health. 2016;13(4):379. doi: 10.3390/ijerph13040379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karaca S, Karaca M, Cesuroglu T, Erge S, Polimanti R. GSTM1, GSTP1, and GSTT1 genetic variability in Turkish and worldwide populations. Am J Hum Biol. 2015;27(3):310–316. doi: 10.1002/ajhb.22671. [DOI] [PubMed] [Google Scholar]
- 14.Abbas A, Delvinquiere K, Lechevrel M, Lebailly P, Gauduchon P, Launoy G, Sichel F. GSTM1, GSTT1, GSTP1 and CYP1A1 genetic polymorphisms and susceptibility to esophageal cancer in a French population: different pattern of squamous cell carcinoma and adenocarcinoma. World J Gastroenterol. 2004;10(23):3389–3393. doi: 10.3748/wjg.v10.i23.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Lieshout EM, Roelofs HM, Dekker S, Mulder CJ, Wobbes T, Jansen JB, Peters WH. Polymorphic expression of the glutathione S-transferase P1 gene and its susceptibility to Barrett's esophagus and esophageal carcinoma. Cancer Res. 1999;59(3):586–589. [PubMed] [Google Scholar]
- 16.Zendehdel K, Bahmanyar S, McCarthy S, Nyren O, Andersson B, Ye W. Genetic polymorphisms of glutathione S-transferase genes GSTP1, GSTM1, and GSTT1 and risk of esophageal and gastric cardia cancers. Cancer Causes Control. 2009;20(10):2031–2038. doi: 10.1007/s10552-009-9399-7. [DOI] [PubMed] [Google Scholar]
- 17.Song Y, Du Y, Zhou Q, Ma J, Yu J, Tao X, Zhang F. Association of GSTP1 Ile105Val polymorphism with risk of esophageal cancer: a meta-analysis of 21 case-control studies. Int J Clin Exp Med. 2014;7(10):3215–3224. [PMC free article] [PubMed] [Google Scholar]
- 18.Tan X, Chen M. Association between glutathione S-transferases P1 Ile105Val polymorphism and susceptibility to esophageal cancer: evidence from 20 case-control studies. Mol Biol Rep. 2015;42(2):399–408. doi: 10.1007/s11033-014-3781-6. [DOI] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cabelguenne A, Loriot MA, Stucker I, Blons H, Koum-Besson E, Brasnu D, Beaune P, Laccourreye O, Laurent-Puig P, De Waziers I. Glutathione-associated enzymes in head and neck squamous cell carcinoma and response to cisplatin-based neoadjuvant chemotherapy. Int J Cancer. 2001;93(5):725–730. doi: 10.1002/ijc.1392. [DOI] [PubMed] [Google Scholar]
- 21.Cai L, Mu LN, Lu H, Lu QY, You NC, Yu SZ, Le AD, Zhao J, Zhou XF, Marshall J, et al. Dietary selenium intake and genetic polymorphisms of the GSTP1 and p53 genes on the risk of esophageal squamous cell carcinoma. Cancer Epidemiol Biomark Prev. 2006;15(2):294–300. doi: 10.1158/1055-9965.EPI-05-0680. [DOI] [PubMed] [Google Scholar]
- 22.Cho CG, Lee SK, Nam SY, Lee MS, Lee SW, Choi EK, Park HJ, Kim SY. Association of the GSTP1 and NQO1 polymorphisms and head and neck squamous cell carcinoma risk. J Korean Med Sci. 2006;21(6):1075–1079. doi: 10.3346/jkms.2006.21.6.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dura P, Salomon J, Te Morsche RH, Roelofs HM, Kristinsson JO, Wobbes T, Witteman BJ, Tan AC, Drenth JP, Peters WH. No role for glutathione S-transferase genotypes in Caucasian esophageal squamous cell or adenocarcinoma etiology: an European case-control study. BMC Gastroenterol. 2013;13:97. doi: 10.1186/1471-230X-13-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dzian A, Halasova E, Matakova T, Kavcova E, Smolar M, Dobrota D, Hamzik J, Mistuna D. Lung adenocarcinoma and squamous cell carcinoma in association with genetic polymorphisms of GSTs in Slovak population. Neoplasma. 2012;59(2):160–167. doi: 10.4149/neo_2012_021. [DOI] [PubMed] [Google Scholar]
- 25.Evans AJ, Henner WD, Eilers KM, Montalto MA, Wersinger EM, Andersen PE, Cohen JI, Everts EC, McWilliams JE, Beer TM. Polymorphisms of GSTT1 and related genes in head and neck cancer risk. Head Neck. 2004;26(1):63–70. doi: 10.1002/hed.10342. [DOI] [PubMed] [Google Scholar]
- 26.Fryer AA, Ramsay HM, Lovatt TJ, Jones PW, Hawley CM, Nicol DL, Strange RC, Harden PN. Polymorphisms in glutathione S-transferases and non-melanoma skin cancer risk in Australian renal transplant recipients. Carcinogenesis. 2005;26(1):185–191. doi: 10.1093/carcin/bgh291. [DOI] [PubMed] [Google Scholar]
- 27.Harth V, Schafer M, Abel J, Maintz L, Neuhaus T, Besuden M, Primke R, Wilkesmann A, Thier R, Vetter H, et al. Head and neck squamous-cell cancer and its association with polymorphic enzymes of xenobiotic metabolism and repair. J Toxicol Environ Health A. 2008;71(13–14):887–897. doi: 10.1080/15287390801988160. [DOI] [PubMed] [Google Scholar]
- 28.Jain M, Kumar S, Rastogi N, Lal P, Ghoshal UC, Tiwari A, Pant MC, Baiq MQ, Mittal B. GSTT1, GSTM1 and GSTP1 genetic polymorphisms and interaction with tobacco, alcohol and occupational exposure in esophageal cancer patients from North India. Cancer Lett. 2006;242(1):60–67. doi: 10.1016/j.canlet.2005.10.034. [DOI] [PubMed] [Google Scholar]
- 29.Jourenkova-Mironova N, Voho A, Bouchardy C, Wikman H, Dayer P, Benhamou S, Hirvonen A. Glutathione S-transferase GSTM1, GSTM3, GSTP1 and GSTT1 genotypes and the risk of smoking-related oral and pharyngeal cancers. Int J Cancer. 1999;81(1):44–48. doi: 10.1002/(sici)1097-0215(19990331)81:1<44::aid-ijc9>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 30.Jourenkova-Mironova N, Voho A, Bouchardy C, Wikman H, Dayer P, Benhamou S, Hirvonen A. Glutathione S-transferase GSTM3 and GSTP1 genotypes and larynx cancer risk. Cancer Epidemiol Biomark Prev. 1999;8(2):185–188. [PubMed] [Google Scholar]
- 31.Jourenkova-Mironova N, Wikman H, Bouchardy C, Voho A, Dayer P, Benhamou S, Hirvonen A. Role of glutathione S-transferase GSTM1, GSTM3, GSTP1 and GSTT1 genotypes in modulating susceptibility to smoking-related lung cancer. Pharmacogenetics. 1998;8(6):495–502. doi: 10.1097/00008571-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Kelders WP, Oude Ophuis MB, Roelofs HM, Peters WH, Manni JJ. The association between glutathione S-transferase P1 genotype and plasma level in head and neck cancer. Laryngoscope. 2002;112(3):462–466. doi: 10.1097/00005537-200203000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Kihara M, Kihara M, Noda K. Lung cancer risk of the GSTM1 null genotype is enhanced in the presence of the GSTP1 mutated genotype in male Japanese smokers. Cancer Lett. 1999;137(1):53–60. doi: 10.1016/s0304-3835(98)00337-1. [DOI] [PubMed] [Google Scholar]
- 34.Larsen JE, Colosimo ML, Yang IA, Bowman R, Zimmerman PV, Fong KM. CYP1A1 Ile462Val and MPO G-463A interact to increase risk of adenocarcinoma but not squamous cell carcinoma of the lung. Carcinogenesis. 2006;27(3):525–532. doi: 10.1093/carcin/bgi227. [DOI] [PubMed] [Google Scholar]
- 35.Leichsenring A, Losi-Guembarovski R, Maciel ME, Losi-Guembarovski A, Oliveira BW, Ramos G, Cavalcanti TC, Bicalho MG, Cavalli IJ, Colus IM, et al. CYP1A1 and GSTP1 polymorphisms in an oral cancer case-control study. Braz J Med Biol Res. 2006;39(12):1569–1574. doi: 10.1590/s0100-879x2006001200007. [DOI] [PubMed] [Google Scholar]
- 36.Leite JL, Morari EC, Granja F, Campos GM, Guilhen AC, Ward LS. Influence of the glutathione s-transferase gene polymorphisms on the susceptibility to basal cell skin carcinoma. Rev Med Chil. 2007;135(3):301–306. doi: 10.4067/s0034-98872007000300004. [DOI] [PubMed] [Google Scholar]
- 37.Lewis SJ, Cherry NM, Niven RM, Barber PV, Povey AC. GSTM1, GSTT1 and GSTP1 polymorphisms and lung cancer risk. Cancer Lett. 2002;180(2):165–171. doi: 10.1016/s0304-3835(02)00028-9. [DOI] [PubMed] [Google Scholar]
- 38.Li D, Dandara C, Parker MI. The 341C/T polymorphism in the GSTP1 gene is associated with increased risk of oesophageal cancer. BMC Genet. 2010;11:47. doi: 10.1186/1471-2156-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li DH, Wang LE, Chang P, El-Naggar AK, Sturgis EM, Wei QY. In vitro benzo a pyrene diol epoxide-induced DNA adducts and risk of squamous cell carcinoma of head and neck. Cancer Res. 2007;67(12):5628–5634. doi: 10.1158/0008-5472.CAN-07-0983. [DOI] [PubMed] [Google Scholar]
- 40.Liang G, Pu Y, Yin L. Rapid detection of single nucleotide polymorphisms related with lung cancer susceptibility of Chinese population. Cancer Lett. 2005;223(2):265–274. doi: 10.1016/j.canlet.2004.12.042. [DOI] [PubMed] [Google Scholar]
- 41.Liu R, Yin L, Pu Y, Li Y, Liang G, Zhang J, Li X. Functional alterations in the glutathione S-transferase family associated with enhanced occurrence of esophageal carcinoma in China. J Toxicol Environ Health A. 2010;73(7):471–482. doi: 10.1080/15287390903523394. [DOI] [PubMed] [Google Scholar]
- 42.Malik MA, Upadhyay R, Mittal RD, Zargar SA, Mittal B. Association of xenobiotic metabolizing enzymes genetic polymorphisms with esophageal cancer in Kashmir Valley and influence of environmental factors. Nutr Cancer. 2010;62(6):734–742. doi: 10.1080/01635581003605904. [DOI] [PubMed] [Google Scholar]
- 43.Matejcic M, Li D, Prescott NJ, Lewis CM, Mathew CG, Parker MI. Association of a deletion of GSTT2B with an altered risk of oesophageal squamous cell carcinoma in a south African population: a case-control study. PLoS One. 2011;6(12):e29366. doi: 10.1371/journal.pone.0029366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McWilliams JE, Evans AJ, Beer TM, Andersen PE, Cohen JI, Everts EC, Henner WD. Genetic polymorphisms in head and neck cancer risk. Head Neck. 2000;22(6):609–617. doi: 10.1002/1097-0347(200009)22:6<609::aid-hed10>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 45.Miller DP, Asomaning K, Liu G, Wain JC, Lynch TJ, Neuberg D, Su L, Christiani DC. An association between glutathione S-transferase P1 gene polymorphism and younger age at onset of lung carcinoma. Cancer. 2006;107(7):1570–1577. doi: 10.1002/cncr.22124. [DOI] [PubMed] [Google Scholar]
- 46.Moaven O, Raziee HR, Sima HR, Ganji A, Malekzadeh R, A'Rabi A, Abdollahi A, Memar B, Sotoudeh M, Naseh H, et al. Interactions between glutathione-S-transferase M1, T1 and P1 polymorphisms and smoking, and increased susceptibility to esophageal squamous cell carcinoma. Cancer Epidemiol. 2010;34(3):285–290. doi: 10.1016/j.canep.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 47.Nazar-Stewart V, Vaughan TL, Stapleton P, Van Loo J, Nicol-Blades B, Eaton DL. A population-based study of glutathione S-transferase M1, T1 and P1 genotypes and risk for lung cancer. Lung Cancer. 2003;40(3):247–258. doi: 10.1016/s0169-5002(03)00076-x. [DOI] [PubMed] [Google Scholar]
- 48.Olshan AF, Weissler MC, Watson MA, Bell DA. GSTM1, GSTT1, GSTP1, CYP1A1, and NAT1 polymorphisms, tobacco use, and the risk of head and neck cancer. Cancer Epidemiol Biomark Prev. 2000;9(2):185–191. [PubMed] [Google Scholar]
- 49.Oude Ophuis MB, Roelofs HM, van den Brandt PA, Peters WH, Manni JJ. Polymorphisms of the glutathione S-transferase P1 gene and head and neck cancer susceptibility. Head Neck. 2003;25(1):37–43. doi: 10.1002/hed.10182. [DOI] [PubMed] [Google Scholar]
- 50.Peters ES, McClean MD, Marsit CJ, Luckett B, Kelsey KT. Glutathione S-transferase polymorphisms and the synergy of alcohol and tobacco in oral, pharyngeal, and laryngeal carcinoma. Cancer Epidemiol Biomark Prev. 2006;15(11):2196–2202. doi: 10.1158/1055-9965.EPI-06-0503. [DOI] [PubMed] [Google Scholar]
- 51.Ramsay HM, Harden PN, Reece S, Smith AG, Jones PW, Strange RC, Fryer AA. Polymorphisms in glutathione S-transferases are associated with altered risk of nonmelanoma skin cancer in renal transplant recipients: a preliminary analysis. J Invest Dermatol. 2001;117(2):251–255. doi: 10.1046/j.0022-202x.2001.01357.x. [DOI] [PubMed] [Google Scholar]
- 52.Risch A, Wikman H, Thiel S, Schmezer P, Edler L, Drings P, Dienemann H, Kayser K, Schulz V, Spiegelhalder B, et al. Glutathione-S-transferase M1, M3, T1 and P1 polymorphisms and susceptibility to non-small-cell lung cancer subtypes and hamartomas. Pharmacogenetics. 2001;11(9):757–764. doi: 10.1097/00008571-200112000-00003. [DOI] [PubMed] [Google Scholar]
- 53.Rossini A, Rapozo DCM, Soares Lima SC, Guimarães DP, Ferreira MA, Teixeira R, Kruel CDP, Barros SGS, Andreollo NA, Acatauassú R, et al. Polymorphisms of GSTP1 and GSTT1, but not of CYP2A6, CYP2E1 or GSTM1, modify the risk for esophageal cancer in a western population. Carcinogenesis. 2007;28(12):2537–2542. doi: 10.1093/carcin/bgm222. [DOI] [PubMed] [Google Scholar]
- 54.Ruwali M, Pant MC, Shah PP, Mishra BN, Parmar D. Polymorphism in cytochrome P450 2A6 and glutathione S-transferase P1 modifies head and neck cancer risk and treatment outcome. Mutat Res. 2009;669(1–2):36–41. doi: 10.1016/j.mrfmmm.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 55.Ruwali M, Singh M, Pant MC, Parmar D. Polymorphism in glutathione S-transferases: susceptibility and treatment outcome for head and neck cancer. Xenobiotica. 2011;41(12):1122–1130. doi: 10.3109/00498254.2011.614020. [DOI] [PubMed] [Google Scholar]
- 56.Ryberg D, Skaug V, Hewer A, Phillips DH, Harries LW, Wolf CR, Ogreid D, Ulvik A, Vu P, Haugen A. Genotypes of glutathione transferase M1 and P1 and their significance for lung DNA adduct levels and cancer risk. Carcinogenesis. 1997;18(7):1285–1289. doi: 10.1093/carcin/18.7.1285. [DOI] [PubMed] [Google Scholar]
- 57.Schneider J, Bernges U, Philipp M, Woitowitz HJ. GSTM1, GSTT1, and GSTP1 polymorphism and lung cancer risk in relation to tobacco smoking. Cancer Lett. 2004;208(1):65–74. doi: 10.1016/j.canlet.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 58.Soucek P, Susova S, Mohelnikova-Duchonova B, Gromadzinska J, Moraviec-Sztandera A, Vodicka P, Vodickova L. Polymorphisms in metabolizing enzymes and the risk of head and neck squamous cell carcinoma in the Slavic population of the Central Europe. Neoplasma. 2010;57(5):415–421. doi: 10.4149/neo_2010_05_415. [DOI] [PubMed] [Google Scholar]
- 59.Soya SS, Vinod T, Reddy KS, Gopalakrishnan S, Adithan C. Genetic polymorphisms of glutathione-S-transferase genes (GSTM1, GSTT1 and GSTP1) and upper aerodigestive tract cancer risk among smokers, tobacco chewers and alcoholics in an Indian population. Eur J Cancer. 2007;43(18):2698–2706. doi: 10.1016/j.ejca.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 60.Stücker I, Hirvonen A, De Waziers I, Cabelguenne A, Mitrunen K, Cénée S, Koum-Besson E, Hémon D, Beaune P, Loriot MA. Genetic polymorphisms of glutathione S-transferases as modulators of lung cancer susceptibility. Carcinogenesis. 2002;23(9):1475–1481. doi: 10.1093/carcin/23.9.1475. [DOI] [PubMed] [Google Scholar]
- 61.Tan W, Song N, Wang GQ, Liu Q, Tang HJ, Kadlubar FF, Lin DX. Impact of genetic polymorphisms in cytochrome P450 2E1 and glutathione S-transferases M1, T1, and P1 on susceptibility to esophageal cancer among high-risk individuals in China. Cancer Epidemiol Biomark Prev. 2000;9(6):551–556. [PubMed] [Google Scholar]
- 62.To-Figueras J, Gene M, Gomez-Catalan J, Pique E, Borrego N, Caballero M, Cruellas F, Raya A, Dicenta M, Corbella J. Microsomal epoxide hydrolase and glutathione S-transferase polymorphisms in relation to laryngeal carcinoma risk. Cancer Lett. 2002;187(1–2):95–101. doi: 10.1016/s0304-3835(02)00406-8. [DOI] [PubMed] [Google Scholar]
- 63.To-Figueras J, Gene M, Gomez-Catalan J, Pique E, Borrego N, Carrasco JL, Ramon J, Corbella J. Genetic polymorphism of glutathione S-transferase P1 gene and lung cancer risk. Cancer Causes Control. 1999;10(1):65–70. doi: 10.1023/a:1008811824890. [DOI] [PubMed] [Google Scholar]
- 64.Song Q, Jiang D, Wang H, Huang J, Liu Y, Xu C, Hou Y. Chromosomal and genomic variations in esophageal squamous cell carcinoma: a review of technologies, applications, and prospections. J Cancer. 2017;8(13):2492–2500. doi: 10.7150/jca.19601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Luo LN, He LJ, Gao XY, Huang XX, Shan HB, Luo GY, Li Y, Lin SY, Wang GB, Zhang R, et al. Evaluation of preoperative staging for esophageal squamous cell carcinoma. World J Gastroenterol. 2016;22(29):6683–6689. doi: 10.3748/wjg.v22.i29.6683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Feng X, Zhou HF, Zheng BS, Shi JJ, Luo C, Qin JJ. Association of glutathione S-transferase P1 gene polymorphism with the histological types of lung cancer: a meta-analysis. Mol Biol Rep. 2013;40(3):2439–2447. doi: 10.1007/s11033-012-2324-2. [DOI] [PubMed] [Google Scholar]
- 67.Xu CH, Wang Q, Zhan P, Qian Q, Yu LK. GSTP1 Ile105Val polymorphism is associated with lung cancer risk among Asian population and smokers: an updated meta-analysis. Mol Biol Rep. 2014;41(7):4199–4212. doi: 10.1007/s11033-014-3290-7. [DOI] [PubMed] [Google Scholar]
- 68.Szyszko TA, Cook GJR. PET/CT and PET/MRI in head and neck malignancy. Clin Radiol. 2018;73(1):60–69. doi: 10.1016/j.crad.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 69.Lang J, Song X, Cheng J, Zhao S, Fan J. Association of GSTP1 Ile105Val Polymorphism and Risk of Head and Neck Cancers: A Meta-Analysis of 28 Case-Control Studies. PLoS One. 2012;7(11):e48132. [DOI] [PMC free article] [PubMed]
- 70.Lei Z, Liu T, Li X, Xu X, Fan D. Contribution of glutathione S-transferase gene polymorphisms to development of skin cancer. Int J Clin Exp Med. 2015;8(1):377–386. [PMC free article] [PubMed] [Google Scholar]
- 71.Zhou CF, Ma T, Zhou DC, Shen T, Zhu QX. Association of glutathione S-transferase pi (GSTP1) Ile105Val polymorphism with the risk of skin cancer: a meta-analysis. Arch Dermatol Res. 2015;307(6):505–513. doi: 10.1007/s00403-015-1576-9. [DOI] [PubMed] [Google Scholar]
- 72.Watson MA, Stewart RK, Smith GB, Massey TE, Bell DA. Human glutathione S-transferase P1 polymorphisms: relationship to lung tissue enzyme activity and population frequency distribution. Carcinogenesis. 1998;19(2):275–280. doi: 10.1093/carcin/19.2.275. [DOI] [PubMed] [Google Scholar]
- 73.Zhong SL, Zhou SF, Chen X, Chan SY, Chan E, Ng KY, Duan W, Huang M. Relationship between genotype and enzyme activity of glutathione S-transferases M1 and P1 in Chinese. Eur J Pharm Sci. 2006;28(1–2):77–85. doi: 10.1016/j.ejps.2006.01.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.