Abstract
Background:
Primary stability is one of the prerequisites of immediate loading. The aim of this study was to compare the primary stability of four different implant systems in low-density bone models.
Materials and Methods:
In this in vitro experimental study, 20 fixtures from four implant body designs were selected: Zimmer Tapered Screw-Vent (ZTSV), NobleReplace Tapered (NRT), Replace Select Tapered (RST), and Dentium SuperLine (DSL). Fixtures were inserted in low-density bone models according to manufacturer drilling protocol by one surgeon. Measurement of insertion torque value (ITV), resonance frequency analysis (implant stability quotient [ISQ]), and reverse torque value (RTV) was recorded for each fixture. The data were analyzed with one-way ANOVA and post hoc tests (Tukey honestly significant difference) (P < 0.05).
Results:
ZTSV had significantly lower amount of insertion torque in comparison to other systems (P = 0.045). RTV was significantly lower in ZTSV in comparison to DSL and NRT (P = 0.004). ISQ value in NRT (ISQ = 67) was significantly higher than other systems (P = 0.000). The lowest amount of ISQ was in RST system (ISQ = 53) with significant difference (P = 0.000).
Conclusion:
This study demonstrated that primary stability of different implant systems was not comparable and implant design was effective on ITV, RTV, and ISQ.
Keywords: Dental implants, immediate dental implant loading, resonance frequency analysis, torque
INTRODUCTION
Immediate loading in dental implants has been become more popular due to patients’ demand of having teeth in the period of osseointegration. Immediate loading is defined as restoration of implant with fixed functional interim prosthesis at the time of implant insertion up to 48 hours later.[1]
There are some essential prerequisites for the possibility of immediate loading: (1) selection of an implant system with great primary stability, (2) high bone implant surface contact,[2] and (3) reduction of micro-motion to <100 μm.[3]
Implant primary stability is a mechanical fact, defined as the absence of clinical mobility at the time of insertion, and has an important role on immediate loading success because instability leads to fibrous encapsulation and implant failure.[4]
Primary stability is related to implant design, method of implant insertion, quality and quantity of surrounding bone.[4] Some surgical methods are suggested to increase primary stability such as bicortical implant placement,[5] under-sized bed preparation,[6] and bone compression technique.[7] Some implant designs result in more stability such as conical fixtures[8] and wide diameter implants.[9] High-density bone provides more stability and in case of low-density bone, exact selection of implant design and surgical protocol is more important.[10]
Methods of evaluation of implant stability are classified to invasive and noninvasive. Invasive techniques include histological analysis (evaluation of bone-implant contact in specimen), removal torque analysis, tensional and push out, pull out test. These methods are limited to nonclinical experimental because of ethical concerns. Noninvasive methods are surgeon's perception, radiographic analysis, cutting torque resistance, insertion or seating torque measurement, vibration test, percussion test, pulsed oscillation waveform, periotest, resonance frequency analysis (RFA), and magnetic technology.[11]
To achieve the proper primary stability, bone quality has an important role, which is not changeable. Surgical methods of increasing stability are successful in some extent although they are not feasible in all cases and they require surgeon experience and dexterity. It seems that the most promising and logical way for getting higher stability in weak bone is to choose appropriate implant design.[10] The purpose of this study was to compare primary stability of four different popular implant designs, which are recommended by their companies for immediate loading. Primary stability in each design was determined through measuring insertion torque value (ITV), RFA and reverse torque value (RTV). It is hypothesized that primary stability of all of the implants would be equal.
MATERIALS AND METHODS
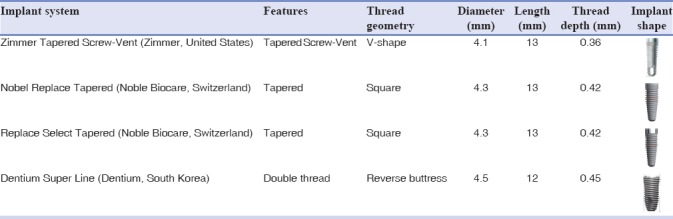
In this in vitro experimental, 20 dental implant with four different designs were selected. The sample size was determined at least five sample in each group according to Lachmann et al. study[12] by Minitab software, with α = 0.05 and β = 0.2 and standard deviation of 4.4. Selected dental implants were the factory recommended type for immediate loading: Zimmer Tapered Screw-Vent (ZTSV), Noble Replace Tapered (NRT), Replace Select Tapered (RST), and Dentium Super Line (DSL). Implant features are shown in Table 1.
Table 1.
Features of implants used in the study groups
Polyurethane blocks (General Plastics manufacture Co, WA, USA) with density of 0.3 cm3/g was chose for bone model, which is categorized as low-density type according to ASTM F1839 (American Society for Testing and Materials).[13] This density is similar to type D4 of Lekholm classification and simulate thin layer of cortical bone surrounding a core of low-density trabecular bone.[14] Five polyurethane blocks were prepared in size of 40 mm in length, 30 mm in width, and 30 mm in height and divided into 4 equal rectangular. The center of each rectangular was the insertion place of each implant, and therefore, four type of implant were inserted in each blocks [Figure 1].
Figure 1.
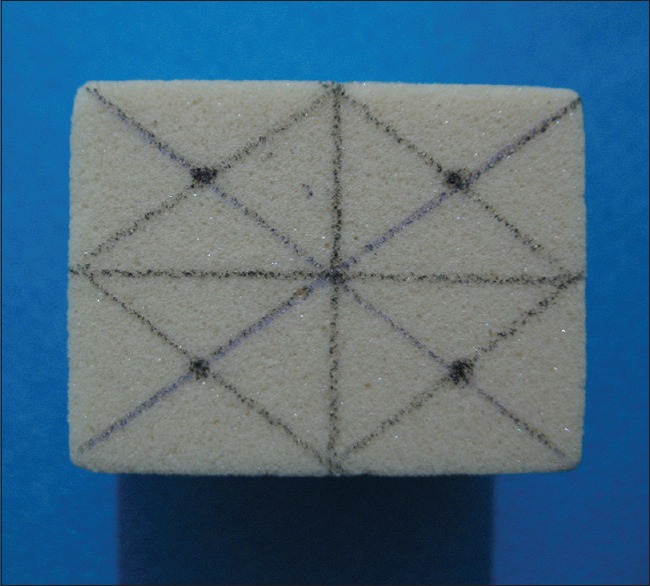
Prepared polyurethane block to place four types of implant.
All the fixtures were inserted according to the manufacturer's protocol by one expert clinician.
The ITV was measured with connecting torque meter probe to superior part of fixtures to seat in prepared socket. Then, Osstell Mentor device (Osstell, Integration Diagnostic AB, GoteborgSvagen, Sweden) was used to measure the implant stability in implant stability quotient (ISQ). The appropriate smart peg of the instrument was selected according to company catalog in relation to size and type of implant and attached to fixture, to determine the primary stability of each implant according to the RFA values.
Then, the least RTV needed for unscrewing the fixture was measured with torque meter (TQ 8800, Lutron Electronic Enterprise CO, Taipei, Taiwan) [Figure 2].
Figure 2.
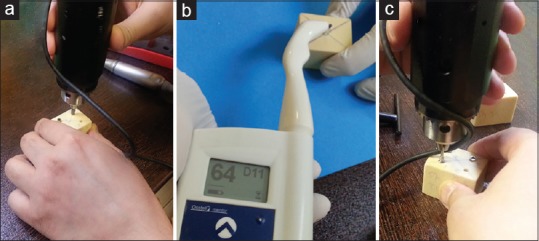
Measuring insertion torque value (a), resonance frequency analysis value (b), reverse torque value (c).
Data analysis was done with SPSS (SPSS for Windows Inc. Version 22. Chicago, Illinois, IBM Corporation, USA). Normality of data was proved according to Kolmogorov–Smirnov analysis. One-way ANOVA was used to compare data in each group. Multiple comparison was done with post hoc test (Tukey honestly significant difference [HSD] type). P < 0.05 was considered as statistically significant.
RESULTS
The mean, maximum, minimum, and standard deviation of variables of each group is summarized in Table 2.
Table 2.
Amount of resonance frequency analysis (implant stability quotient), insertion torque (N/Cm), and reverse torque (N/Cm) value in study groups
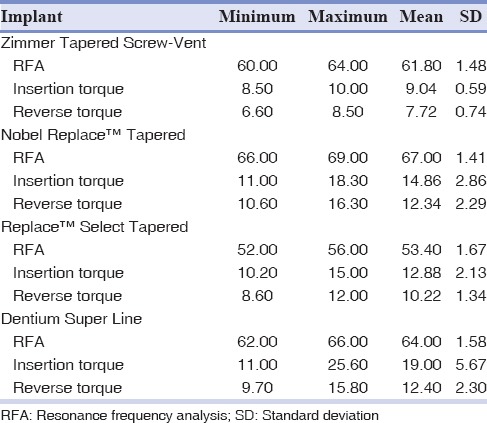
Evaluation of the ISQ, ITV, and RTV in different groups by one-way ANOVA test revealed that the study groups were different in terms of each variable (P < 0.0001).
According to post hoc analysis (Tukey HSD), the lowest amount of ISQ was in RRST with significant difference (P = 0.000). ISQ of ZTSV and DSL was equal, and the highest amount of ISQ was in NRT with significant difference with others (P = 0.000).
ZTSV had the lowest ITV with significant difference with other systems (P = 0.045). The ITV between other systems had no significant difference.
According to post hoc analysis, ZTSV had the lowest RTV, and the difference was significant (P = 0.004) with DSL and NRT implant. The RTV between other systems had no significant difference.
The multiple comparison of systems is shown in Figure 3.
Figure 3.
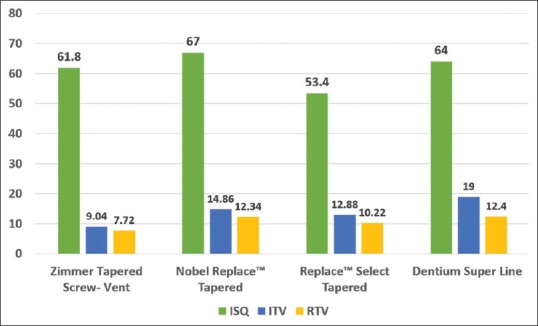
Multiple comparison of implant systems stability.
DISCUSSION
Based on the result, the study hypotheses are rejected, and primary stability of different implant systems was not equal.
Primary stability is one of the prerequisites of immediate loading. It is proved that high primary stability decreases micromotion, bone resorption, and fibrous formation.[10] The main purpose of measuring the primary stability is to evaluate the micromotion.[15] Micromotion in D1 and D2 is less and primary stability could be easily achievable but in D3 and D4 bone, reaching to primary stability is difficult.[16] In this study, primary stability of four implant designs in D4 bone model is evaluated because in this bone quality, implant design seems to be more critical[10] and the purpose is to evaluate that in compromised situation, which implant design could be more efficient.
Implant macroscopic features have great role in primary stability. Fixtures with more length provide more stability. It is proved that primary stability is in risk in fixture lengths <10 mm and length more than 15 mm does not benefit more stability.[17] Furthermore, more thread depth and width increase functional surface and stability.[18] Taper implants provide more stability than cylindrical form and are recommended to use in immediate loading[19] and when the use of short implants is necessary.[20] Although implant surface characteristic has no direct effect on primary stability, it improves bone healing and reduces micro movement because of coarse and bioactive surface, which could be effective on secondary stability.[19,21] In the present study, four popular implant designs, which are the companies recommended types for immediate loading, were selected. They contained similar features such as taper body form, length of 12 or 13 mm and regular diameters.
In this study, ISQ amount was in following sequence: NRT > ZTSV = DSL > RRST. ISQ was significantly higher in NRT system in comparison to other systems (mean = 67). Probably, it is related to double groovy (double thread) design, square form thread, with 0.42 mm depth and 0.7 mm width of threads, which increase functional surface and bone contact.[18] This result is in line with Ostman[22] Meredith[23] and Friberg et al.[24] studies, which showed the effect of macro design on ISQ value.
ISQ value in ZTSV (mean = 61.8) and DSL (mean = 64) had no significant difference. In ZTSV system, thread form was V shape and in DSL system, fixture had double thread design and reverse buttress form. The reason of the same ISQ versus these design difference could be related to more number of threads in each unit of surface in ZTSV implant, which increase functional surface and bone contact. In addition, DSL implant contains self-cutting blade in half-epical part, which increases ease of insertion but decrease ISQ value. This result is compatible with Kim et al.[25] that showed ISQ is higher in nonself-cutting blade implants.
ISQ value in RST system was significantly lower in comparison to other systems. It could be results of lacking of some specific macro design for increasing functional surface such as double thread or large number threads per unit.
Although some studies showed, that ISQ is a good evaluation of primary stability for immediate loading,[26,27] some studies mentioned that single time ISQ evaluation is not a proper determinant of stability and success of implant.[28,29] ISQ shows amount of lateral stiffness and could not demonstrate the actual implant micromotion. Micromotion should be limited to <50–100 micron unless fibrous formation and bone loss would happen around implant.[15,29] However, it is proved that there is a significant correlation between ISQ and micromotion.[29] It is reported that ISQ is more reliable in high-density bone and not trustworthy in poor quality bone (D3, D4).[30]
It is claimed that ISQ should be analyzed for each system over the time and ISQ is not reliable indicator for comparison of several systems during loading in polyurethane block or specific area of jaw.[31,32]
In this study, to assess primary stability, ITV was recorded as well. ITV is correlated with implant micromotion. Trisi et al.[33] showed maximum ITV in low- and high-density bone could be 35 N/Cm and 100 N/Cm, respectively. Each 10N/Cm increase in ITV decreases the micromotion about 4 micron. ITV can be affected by noncalibrated surgical handpiece, hand pressure of surgeon, and unstable blocks during drilling, however, it is insignificant.[34]
In this study, ITV was in following sequence: DSL > NRT = RRST > ZTSV. ZTSV had significantly lower ITV (mean = 9) in comparison to others. ZTSV has V-shaped thread, it is proved that square and reverse buttress thread shapes provide more stability than buttress and V-shaped thread.[18] Furthermore, ZTSV fixture is self-tapping which eases the insertion and reduces ITV, and the same finding of self-tapping effect is supported by Ostman[22] Javed and Romanos,[35] and Piattelli et al.[36]
DSL showed the highest ITV (mean = 19) and it could be the result of double-thread design. The effect of this macro design is compatible with Chiapasco et al.,[37] Fazel et al.,[38] and Cochran et al.[39]
RTV is an indicator of bone implant interfacial interface and was measured with torque controller device and the least torque needed to unscrew and remove the fixture was recorded.[40] RTV in ZTSV implant was lowest (mean = 7.72) with significant difference with NRT and DSL. This lower value in ZTSV system could be in association with V-shaped thread and consequently lower functional surface and lower force for detorquing.
Lachmann et al.[12] showed that removal torque value is lower in implants with self-cutting blade in half-apical part. The least removal torque value for long-term stability is reported to be 30 NCm.[22]
In this study, RTV was lower than ITV in all systems the reason could be related to deformation and compression of the surrounding bone model by lateral forces of implant placement.[33]
In this study, although all systems had high ISQ, ITV and RTV were low, and they were not proper for immediate loading in D4 bone. In comparison, DSL and NRT with higher ISQ and ITV are better choice in low-density bone to prevent failures in the early healing period.
CONCLUSION
This study demonstrated that primary stability of different implant systems was not comparable and implant design was effective on ITV, RTV, and ISQ. According to study's limitation, the lowest amount of ITV and RTV was in ZTSV with no significant difference between others. The lowest and highest amount of ISQ value was in RST and NRT, respectively.
Financial support and sponsorship
This study was supported by Deputy of Research Affairs, Faculty of Dentistry, Tehran University of Medical Sciences.
Conflicts of interest
The authors of this manuscript declare that they have no conflicts of interest, real or perceived, financial or nonfinancial in this article.
Acknowledgment
The authors wish to thank Dr. Hasan Dorriz for his kind contribution.
REFERENCES
- 1.Ghoul WE, Chidiac JJ. Prosthetic requirements for immediate implant loading: A review. J Prosthodont. 2012;21:141–54. doi: 10.1111/j.1532-849X.2011.00819.x. [DOI] [PubMed] [Google Scholar]
- 2.Romanos GE. Present status of immediate loading of oral implants. J Oral Implantol. 2004;30:189–97. doi: 10.1563/1548-1336(2004)30<189:PSOILO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Brunski JB. In vivo bone response to biomechanical loading at the bone/dental-implant interface. Adv Dent Res. 1999;13:99–119. doi: 10.1177/08959374990130012301. [DOI] [PubMed] [Google Scholar]
- 4.Mistry G, Shetty O, Shetty S, Singh RD. Measuring implant stability: A review of different methods. J Dent Implants. 2014;4:165. [Google Scholar]
- 5.Wagner W, Kunkel M, Wahlmann UW. Class D4 bone: diagnosis, problems and possible solutions for implants in a very spongy bone storage. Implantologie. 1999;2:121–7. [Google Scholar]
- 6.Tabassum A, Meijer GJ, Walboomers XF, Jansen JA. Evaluation of primary and secondary stability of titanium implants using different surgical techniques. Clin Oral Implants Res. 2014;25:487–92. doi: 10.1111/clr.12180. [DOI] [PubMed] [Google Scholar]
- 7.Friberg B, Ekestubbe A, Mellström D, Sennerby L. Brånemark implants and osteoporosis: A clinical exploratory study. Clin Implant Dent Relat Res. 2001;3:50–6. doi: 10.1111/j.1708-8208.2001.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 8.Sakoh J, Wahlmann U, Stender E, Nat R, Al-Nawas B, Wagner W, et al. Primary stability of a conical implant and a hybrid, cylindric screw-type implant in vitro . Int J Oral Maxillofac Implants. 2006;21:560–6. [PubMed] [Google Scholar]
- 9.Davarpanah M, Martinez H, Kebir M, Etienne D, Tecucianu JF. Wide-diameter implants: New concepts. Int J Periodontics Restorative Dent. 2001;21:149–59. [PubMed] [Google Scholar]
- 10.Vidyasagar L, Salms G, Apse P. Investigation of initial implant stability with different dental implant designs. Stomatologija Balt Dent Maxillofac J. 2004;6:35–9. [Google Scholar]
- 11.Swami V, Vijayaraghavan V, Swami V. Current trends to measure implant stability. J Indian Prosthodont Soc. 2016;16:124–30. doi: 10.4103/0972-4052.176539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lachmann S, Laval JY, Axmann D, Weber H. Influence of implant geometry on primary insertion stability and simulated peri-implant bone loss: An in vitro study using resonance frequency analysis and damping capacity assessment. Int J Oral Maxillofac Implants. 2011;26:347–55. [PubMed] [Google Scholar]
- 13.Calvert KL, Trumble KP, Webster TJ, Kirkpatrick LA. Characterization of commercial rigid polyurethane foams used as bone analogs for implant testing. J Mater Sci Mater Med. 2010;21:1453–61. doi: 10.1007/s10856-010-4024-6. [DOI] [PubMed] [Google Scholar]
- 14.Lekholm U, Zarb GA. Patient selection and preparation. In: Brånemark PI, Zarb GA, Albrektsson T, editors. Tissue-Integrated Prostheses-Osseointegration in Clinical Dentistry. Chicago: Quintessance Publishing Co; 1985. pp. 199–209. [Google Scholar]
- 15.Søballe K, Brockstedt-Rasmussen H, Hansen ES, Bünger C. Hydroxyapatite coating modifies implant membrane formation. Controlled micromotion studied in dogs. Acta Orthop Scand. 1992;63:128–40. doi: 10.3109/17453679209154808. [DOI] [PubMed] [Google Scholar]
- 16.Graf H. Occlusal forces during function. Occlusion Res Funct. 1975;19:90–110. [Google Scholar]
- 17.Rismanchian M, Khodaeian N, Ataei E. Review of immediate and early loading protocols in dental implants. JSSU. 2010;18:469–78. [Google Scholar]
- 18.Strong JT, Misch CE, Bidez MW. Scientific rationale for dental implant design. In: Misch CE, editor. Contemporary Implant Dentistry. 3rd ed. Ch. 11. Canada: Mosby Elsevier Publisher; 2008. [Google Scholar]
- 19.O’Sullivan D, Sennerby L, Jagger D, Meredith N. A comparison of two methods of enhancing implant primary stability. Clin Implant Dent Relat Res. 2004;6:48–57. doi: 10.1111/j.1708-8208.2004.tb00027.x. [DOI] [PubMed] [Google Scholar]
- 20.Barikani H, Rashtak S, Akbari S, Fard MK, Rokn A. The effect of shape, length and diameter of implants on primary stability based on resonance frequency analysis. Dent Res J (Isfahan) 2014;11:87–91. [PMC free article] [PubMed] [Google Scholar]
- 21.O’Sullivan D, Sennerby L, Meredith N. Measurements comparing the initial stability of five designs of dental implants: A human cadaver study. Clin Implant Dent Relat Res. 2000;2:85–92. doi: 10.1111/j.1708-8208.2000.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 22.Ostman PO. Immediate/early loading of dental implants. Clinical documentation and presentation of a treatment concept. Periodontol 2000. 2008;47:90–112. doi: 10.1111/j.1600-0757.2007.00244.x. [DOI] [PubMed] [Google Scholar]
- 23.Meredith N, Book K, Friberg B, Jemt T, Sennerby L. Resonance frequency measurements of implant stability in vivo. A cross-sectional and longitudinal study of resonance frequency measurements on implants in the edentulous and partially dentate maxilla. Clin Oral Implants Res. 1997;8:226–33. doi: 10.1034/j.1600-0501.1997.080309.x. [DOI] [PubMed] [Google Scholar]
- 24.Friberg B, Sennerby L, Roos J, Lekholm U. Identification of bone quality in conjunction with insertion of titanium implants. A pilot study in jaw autopsy specimens. Clin Oral Implants Res. 1995;6:213–9. doi: 10.1034/j.1600-0501.1995.060403.x. [DOI] [PubMed] [Google Scholar]
- 25.Kim DR, Lim YJ, Kim MJ, Kwon HB, Kim SH. Self-cutting blades and their influence on primary stability of tapered dental implants in a simulated low-density bone model: A laboratory study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:573–80. doi: 10.1016/j.tripleo.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Turkyilmaz I, Sennerby L, McGlumphy EA, Tözüm TF. Biomechanical aspects of primary implant stability: A human cadaver study. Clin Implant Dent Relat Res. 2009;11:113–9. doi: 10.1111/j.1708-8208.2008.00097.x. [DOI] [PubMed] [Google Scholar]
- 27.Huwiler MA, Pjetursson BE, Bosshardt DD, Salvi GE, Lang NP. Resonance frequency analysis in relation to jawbone characteristics and during early healing of implant installation. Clin Oral Implants Res. 2007;18:275–80. doi: 10.1111/j.1600-0501.2007.01336.x. [DOI] [PubMed] [Google Scholar]
- 28.Trisi P, Perfetti G, Baldoni E, Berardi D, Colagiovanni M, Scogna G, et al. Implant micromotion is related to peak insertion torque and bone density. Clin Oral Implants Res. 2009;20:467–71. doi: 10.1111/j.1600-0501.2008.01679.x. [DOI] [PubMed] [Google Scholar]
- 29.Trisi P, De Benedittis S, Perfetti G, Berardi D. Primary stability, insertion torque and bone density of cylindric implant ad modum branemark: Is there a relationship. An in vitro study? Clin Oral Implants Res. 2011;22:567–70. doi: 10.1111/j.1600-0501.2010.02036.x. [DOI] [PubMed] [Google Scholar]
- 30.Szmukler-Moncler S, Piattelli A, Favero GA, Dubruille JH. Considerations preliminary to the application of early and immediate loading protocols in dental implantology. Clin Oral Implants Res. 2000;11:12–25. doi: 10.1034/j.1600-0501.2000.011001012.x. [DOI] [PubMed] [Google Scholar]
- 31.Rabel A, Köhler SG, Schmidt-Westhausen AM. Clinical study on the primary stability of two dental implant systems with resonance frequency analysis. Clin Oral Investig. 2007;11:257–65. doi: 10.1007/s00784-007-0115-2. [DOI] [PubMed] [Google Scholar]
- 32.Zix J, Hug S, Kessler-Liechti G, Mericske-Stern R. Measurement of dental implant stability by resonance frequency analysis and damping capacity assessment: Comparison of both techniques in a clinical trial. Int J Oral Maxillofac Implants. 2008;23:525–30. [PubMed] [Google Scholar]
- 33.Trisi P, Todisco M, Consolo U, Travaglini D. High versus low implant insertion torque: A histologic, histomorphometric, and biomechanical study in the sheep mandible. Int J Oral Maxillofac Implants. 2011;26:837–49. [PubMed] [Google Scholar]
- 34.Cehreli MC, Karasoy D, Akca K, Eckert SE. Meta-analysis of methods used to assess implant stability. Int J Oral Maxillofac Implants. 2009;24:1015–32. [PubMed] [Google Scholar]
- 35.Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010;38:612–20. doi: 10.1016/j.jdent.2010.05.013. [DOI] [PubMed] [Google Scholar]
- 36.Piattelli A, Corigliano M, Scarano A, Quaranta M. Bone reactions to early occlusal loading of two-stage titanium plasma-sprayed implants: A pilot study in monkeys. Int J Periodontics Restorative Dent. 1997;17:162–9. [PubMed] [Google Scholar]
- 37.Chiapasco M. Early and immediate restoration and loading of implants in completely edentulous patients. Int J Oral Maxillofac Implants. 2004;19(Suppl):76–91. [PubMed] [Google Scholar]
- 38.Fazel A, Aalai S, Rismanchian M. Effect of macro-design of immediately loaded implants on micromotion and stress distribution in surrounding bone using finite element analysis. Implant Dent. 2009;18:345–52. doi: 10.1097/ID.0b013e31819cd938. [DOI] [PubMed] [Google Scholar]
- 39.Cochran DL, Morton D, Weber HP. Consensus statements and recommended clinical procedures regarding loading protocols for endosseous dental implants. Int J Oral Maxillofac Implants. 2004;19(Suppl):109–13. [PubMed] [Google Scholar]
- 40.Kim JM, Kim SJ, Han I, Shin SW, Ryu JJ. A comparison of the implant stability among various implant systems: Clinical study. J Adv Prosthodont. 2009;1:31–6. doi: 10.4047/jap.2009.1.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]


