Abstract
Objectives: To evaluate the difference in terms of overall complications between surgical and non-surgical management of lower limb fractures in patients with chronic spinal cord injury (SCI).
Design: A 13-year retrospective study including patients with chronic spinal cord lesion admitted for sublesional lower limb fractures.
Setting: University hospital SCI reference departments (Rehabilitation department and orthopedic department).
Participants: Forty patients with SCI were included, 24 men and 16 women. Fifty-six distinct fracture occurrences were responsible for a total of 59 lower limb fractures. We compared the number of overall complications between surgical and non-surgical management of fractures.
Results: Non-surgical management was realized for 19 fractures and surgery for 40. Characteristics of operated and non-operated patients at the time of each fracture occurrence did not differ concerning age (P = 0.430), sex (P = 0.890), lesion levels (P = 0.410) and AIS classification (P = 0.790). Data analysis highlighted 20 complications directly due to the fracture site for 16 distinct fractures. Seven medical complications were found in 5 distinct fracture events. Only 10 (25.0%) of 40 surgical managements had at least one medical or post-surgical complication, whereas 12 (63.2%) of 19 non-operative managements had at least one complication. Therefore, the overall rate of complications was significantly higher after non-surgical treatment (P = 0.044).
Conclusion: Lower extremity fractures due to osteoporosis in patients with SCI are responsible for local and general complications. When possible, surgery may be the best management to propose because of fewer overall complications.
Keywords: Spinal cord injury, Osteoporosis, Fractures, Lower limb, Surgery, Non-operative management
Introduction
Sub-lesional bone loss in patients with spinal cord injury (SCI) is an extremely complex, multifactorial phenomenon. Besides the loss of bone mineral density due to initial immobilization,1,2 many other causes are described, such as biochemical, neurologic or endocrine phenomena,3–5 which are specific to SCI. This inevitable loss of bone mineral density is responsible for frequent lower limb fractures, with an annual incidence of about 2–7.4%.6–8 Between one-third and one-half of patients with SCI will experience at least one sublesional fracture as a secondary condition.4,9 Fractures are a frequent cause of hospitalization10,11 because of orthopedic and medical secondary complications,12 which are sources of important additional costs concerning medical management,13 with increased morbidity and mortality.14 The optimal management of these fractures is essential in order to limit their complications. Yet, the choice between surgery and conservative management, except for technical specificities, is clearly not consensual and differs from a medical team to another. Nevertheless, nonsurgical management appears to be more frequent in the present literature.15 Until now, no study has evaluated overall complications after surgical or nonsurgical management of lower-limb fractures in patients with chronic SCI. Indeed, previous studies focused only on complications directly linked to the fracture sites16 or on overall complications but in only one type of fractures.17 Therefore, it seems important to consider overall complications as they are representative of the complexity of management of paitents with SCI.
The purpose of our study was to evaluate if there was a difference in terms of overall complications between surgical or non-operative management in people with chronic SCI with lower limb fractures.
Methods
We conducted this retrospective study both in the rehabilitation department for patients with SCI and the orthopedic department of Nantes University Hospital, France, either in their respective consultation units or in their hospitalization ones. The rehabilitation department has a prospective follow-up of patients with SCI (about 400 patients with SCI a year), with at least one specialized consultation for each patient every year.
The cohort was identified using data extracted from the French Medical Information System (Programme de Médicalisation des Systèmes d'Information - PMSI) including all the patients with SCI associated with a diagnosis of fracture in the hospital. Diagnoses are coded using the International Classification of Diseases, 10th revision (ICD-10). Then the principal investigator analyzed all patients’ forms to exclude wrong diagnosis. We included all SCI patients over 18, with at least 2-year-old lesions, admitted in hospitalization or in consultation with a sub-lesional lower limb fracture occurred between January, 1st 2000 and December, 31st 2013. The period of 2 years was chosen because we aimed to investigate only patients at the chronic stage. According to previous studies, from that length of time bone metabolism reaches a new state of balance and regarding bony lesions, the chronic phase begins.18 The exclusion criteria were: long-term intake of a treatment inducing osteoporosis such as corticosteroids (from a period of 3 months19), pathology responsible for osteopenia (diagnosis of osteoporosis before SCI, genetic disease, endocrinopathies) and sub-lesional fractures (which did not correspond to the purpose of the study).
The main investigator collected the study parameters and carried out a direct analysis of all the medical patients’ data: patients’ characteristics (age, sex, time since SCI, neurological level of injury, ASIA Impairment Scale (AIS)20), fracture-characteristics (fractured bone, localization, mode of occurrence, management) and the occurrence of local or general complications.
Ethics
During the course of this research, we followed applicable institutional and governmental regulations concerning ethics and declared the data report form to the French data protection authority (Commission Nationale Informatique et Liberté), as required by French law. Since we collected data retrospectively and did not modify patients’ management, according to French law, this study did not need to be approved by a research ethics committee. We conducted it in accordance with the law on data protection and we rendered patients’ data report forms entirely anonymous prior to analysis.
Data analysis
Quantitative variables are given in mean values and standard-error (SD), qualitative variables are given in numbers and percentages. We used the χ2 test (or Fisher's exact test) to determine if patient's characteristics were comparable between both groups (surgical and non-operative treatment). To do so, we chose to consider patients’ characteristics for each fracture occurrence. We chose a level of significance α = 0.05. We also used the χ2 test to compare the number of complications after fractures between operated and non-operated patients. We performed statistical analyses with SPSS software (version 23.0, IBM Corp., Armonk, NY, USA).
Results
Participant characteristics
A total of 40 patients with SCI fulfilled the inclusion criteria, 24 men and 16 women. Thirty-four patients had a traumatic SCI and 6 had SCI from other origins (2 ischemic spinal cord lesions, 1 compression due to a tuberculosis abscess, 1 arachnoid cyst, 1 after scoliosis surgery and 1 after a decompression diving accident). Patients’ characteristics at the first fracture occurrence are presented in Table 1.
Table 1. General characteristics of the studied population at the time of the first fracture event and according to the type of fracture management.
| Total population | Operative group | Non-operative group | |
|---|---|---|---|
| n (%) or mean (SD) | |||
| Patients included | 40 (100.0%) | 27 (67.5%) | 13 (32.5%) |
| Sex | |||
| Male | 24 (60.0%) | 16 (40.0%) | 8 (20.0%) |
| Female | 16 (40.0%) | 11 (27.5%) | 5 (12.5%) |
| Age (years) | 48.4 (13.5) | 46.2 (14.4) | 53.3 (10.9) |
| AIS | |||
| A | 30 (75%) | 21 (52.5%) | 9 (22.5%) |
| B | 4 (10%) | 2 (5.0%) | 2 (5.0%) |
| C | 3 (7.5%) | 2 (5.0%) | 1 (2.5%) |
| D | 3 (7.5%) | 2 (5.0%) | 1 (2.5%) |
| Time since SCI (years) | 14.8 (10.8) | 11.9 (8.4) | 21.2 (12.5) |
| Level of injury | |||
| Paraplegia | 31 (77.5%) | 21 (52.5%) | 10 (25.0%) |
| Tetraplegia | 9 (22.5%) | 6 (15.0%) | 3 (7.5%) |
| Origin of the SCI | |||
| Traumatic | 34 (85%) | 24 (60.0%) | 10 (25.0%) |
| Other | 6 (15%) | 3 (7.5%) | 3 (7.5%) |
Fractures
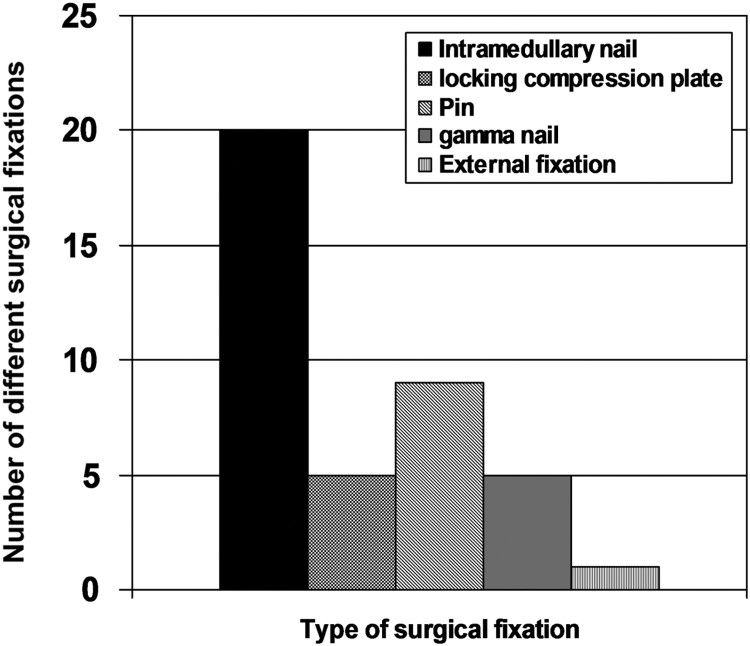
Fifty-six distinct occurrences were responsible for a total of 59 lower limb fractures. One patient had 2 fractures (right distal femur and right diaphyseal tibia) and another one had 3 fractures (right and left distal femurs, right proximal tibia) subsequent to a unique traumatism. During the 13-year period of the study, 27 patients had only one fracture, 10 had 2 successive fractures and 3 patients had 3 successive ones. The most frequent localizations were the distal femur (28.8%), distal tibia (22.0%), proximal tibia (16.9%) and proximal femur (15.3%). The other localizations were diaphyseal femur (8.5%), diaphyseal tibia (6.8%) and foot (1.7%). Many fractures were secondary to wheelchair falls (41.1%) or transfers (14.3%). The other fracture mechanisms were usually minor traumatisms. We found no cause in 16.1%. Non-operative management was proposed for 19 fractures (32.0%) and surgery for 40 (68.0%). Non-operative managements were plaster casts (37%) or braces (63%) and surgical treatments were most of the time open reduction with internal fixation such as intramedullary nails (50%). Details concerning the type of operative managements are given in Fig. 1.
Figure 1.
Number and type of surgical fracture management (n = 40).
Characteristics of operated and non-operated patients at the time of each fracture occurrence did not differ concerning age (P = 0.430), sex (P = 0.890), lesion levels (P = 0.410) and AIS classification (P = 0.790).
Complications
For 34 fracture occurrences, there were neither medical nor surgical complications. Five patients were followed in our rehabilitation center after an initial management in a peripheral surgical center. At the time of their evaluation in our center, no surgery was proposed because the delay to perform a surgical treatment appeared to be already exceeded considering the period between the traumatism and the evaluation. Data analysis highlighted 20 complications directly due to the fracture site (such as non-union, delayed union, mal-alignment, local infection, skin lesion, re-fracture, joint stiffness or osteosynthesis displacement) for 16 distinct fractures. We found seven medical complications in 5 distinct fractures events: 2 sacral pressure sores, 2 pyelonephritis, 1 venous thrombosis, 1 complex regional pain syndrome and 1 episode of severe constipation.
Finally, 14 of the 27 complications (52%) occurred after conservative treatments whereas the other 13 occurred after surgery. So, out of 40 surgical managements, only 10 (25.0%) had at least one medical or post-surgical complication, whereas out of 19 non-operative managements, 12 (63.2%) had at least one complication. Details of fracture complications are given in Table 2.
Table 2. Number and type of post-fracture complications according to the type of fracture management.
| Complications | Operative group (number of fractures = 40) | Non-operative group (number of fractures = 19) |
|---|---|---|
| Delayed-union | 2 | 2 |
| Non-union | 2 | 2 |
| Mal-alignment | 0 | 2 |
| Local infection | 1 | 0 |
| Skin lesion | 0 | 3 |
| Re-fracture | 1 | 0 |
| Osteosynthesis displacement | 2 | 0 |
| joint stiffness | 2 | 1 |
| Sacral pressure sore | 2 | 0 |
| Venous thrombosis | 0 | 1 |
| Complex regional pain syndrome | 0 | 1 |
| Severe constipation | 0 | 1 |
| Pyelonephritis | 1 | 1 |
| Total complications | 13 | 14 |
| At least one complication per fracture occurrence | 10 | 12 |
It is interesting to note that from 8 ankle fractures, 2 were operated and no complication was noticed, whereas 6 were not operated and they were all complicated: 1 patient had non-union and a skin lesion; 1 had a skin lesion and a mal alignment; 2 had non-union; 2 had mal-alignment and only one had no complication.
In the surgery group, 13 complications occurred after 10 fracture occurrences; one patient had 3 post-operative complications and another one 2 medical complications. In the non-operative treatment group, 14 complications occurred after 12 fracture occurrences, one patient had a mal-union of the fracture site and a pressure sore, the other one had a venous thrombosis and a complex regional pain syndrome. Thereby, overall rate of complications (medical and orthopedic) was significantly more frequent after non-operative treatment than after operative one (P = 0.044).
Moreover, if evaluating fracture management depending on bone localizations (femur or tibia), femoral fractures are significantly more operated on than tibial ones (P < 0.001) (Table 3).
Table 3. Total number of fractures per anatomical sites and according to the fracture management.
| Fracture sites | Total population | Operative group | Non-operative group |
|---|---|---|---|
| Distal femur: | 17 | 15 | 2 |
| - Supra-condylar | 11 | 1 | |
| - Metaphyseal | 3 | 1 | |
| - Condylar | 1 | 0 | |
| - | |||
| Distal tibia: | 13 | 4 | 9 |
| - Ankle | 8 | 2 | 6 |
| Proximal tibia: | 10 | 4 | 6 |
| - Metaphyseal | 1 | 3 | |
| - Plateau | 1 | 3 | |
| - Complex articular | 2 | 0 | |
| Proximal femur: | 9 | 8 | 1 |
| - Cervical | 3 | 0 | |
| - Intertrochanteric | 2 | 0 | |
| - Subtrochanteric | 3 | 0 | |
| Diaphyseal femur | 5 | 5 | 0 |
| Diaphyseal tibia | 4 | 3 | 1 |
| Foot (metatarsal fracture) | 1 | 1 | 0 |
When grouping fractures per bones, that is to say femur or tibia localizations (the unique foot fracture was excluded), the exact Fisher's test indicates that femoral fractures are more likely operated (P<0.001).
Discussion
The physiopathology of bone demineralization in people with SCI remains a subject of study.4 Initial immobilization is known to be responsible for an early loss of bone density associated with hypercalcemia and hypercalciuria.1 It has been suggested that sclerotin could play a central role in early bone loss with a reduction of bone formation due to direct action on osteocytes and an indirect activation of bone resorption.4 Experimentally, mice with SCI have an increase of their osteoclastic potential in the sub-lesional bone marrow.21 Other specific ways are studied and seem to be involved in SCI bone loss, such as neural factors with a modification of the density of certain types of nerve fibers especially substance P nerve fibers.22 Hormonal modifications could also appear as potential explanations because leptine is known to be implicated in bone remodelling and an elevation of the leptine rate has previously been described in patients with SCI compared to able-bodied controls.23
Our study is the first one to compare overall complications after surgical or non surgical management of lower-limb fractures in patients with chronic SCI. Indeed, Frotzler et al.16 studied fracture complications after surgery or non-surgical management in a recent study, but they investigated complications at the site of the fracture rather than overall complications. Bishop et al.17 were interested in overall adverse events after operative and non-operative treatments in patients with SCI and studied only femoral fractures but did not study other fracture sites. The assessment of all types of complications is representative of the complexity of cases in patients with SCI, as lower limb fractures are responsible for local but also general complications,12 such as venous thrombosis, infections or pressure sores. These complications are responsible for an aggravation of disabilities, especially pressure injuries.24 In terms of time, in our study the first fracture occurred 14.8±10.8 years after the initial SCI, which was of traumatic origin for 85% of our subjects. ASIA impairment scale classification was A (AIS A) for 75.0% of the patients.
Lower limb fractures in patients with SCI are usually due to low energy mechanism11 such as wheelchair falls25 or transfers. We found such causes in at least 75% of our patients. Fractures are mainly situated on lower limbs, especially close to the knee,26,27 28.8% for distal femurs and 16.9% for proximal tibias in our study. Concerning fracture management, there is currently no consensus regarding operative or non-operative procedures,15,16,28–31 although non-operative treatment seems to be often the chosen solution.11,15 The main aim of fracture management in patients with SCI is definitely to have correct bone healing, but also to prevent general complications, reduce immobilization time and preserve patients’ independence.32 Surgery allows quick stabilization of fractures and early lower limb mobilization, thus accelerating the return to usual daily life activities.33 Nevertheless, surgery may be responsible for infection, hemorrhage and skin non-healing. Non-operative treatment does not often have those risks but can be responsible for more frequent mal-alignments or non-union.
Recently, Bethel et al.15 found no difference in mortality between operative and non-operative management of fractures in people with SCI but they did not compare the occurrence of complications between these different treatments. Bishop et al.17 reported no increase of mortality and overall adverse events in patients with femoral fractures treated operatively. In our study, 68.0% of the overall fractures were treated surgically. One complication at least was present in 25.0% of the cases treated surgically, whereas after non-operative treatment 63.2% of complications were reported, which was significantly higher. These results may appear surprising compared to those of Frotzler et al.,16 who found no differences between surgery and non-operative management, and a lower overall complication rate than in the present study (13.1% in operated patients vs. 15.4% in non-operated ones). Actually, the explanation is that Frotzler et al.16 considered only bone healings in their study, and did not pay attention to overall complications. Bone healing is an important point to consider in the evaluation of lower limb fracture management but medical secondary complications such as urinary infections, venous thrombosis or pressure sores, are also primordial consequences to look at because of functional and lethal risks. In fact, other studies have results concordant with ours, implying that surgery causes fewer complications than non operative treatment. Martinez et al.29 studied mostly surgical treatments (65.4%) and it is interesting to note that 60.0% of the complications occurred after non-operative managements, which is close to the results of the present study. In comparison, Morse et al.34 described that 53% of the fracture managements became complicated while non-surgical management had been preferred in 91% of the cases. It is also interesting to note that in their study, 25% of the complications were pressure sores, either due to bed rest or brace contact.32 These data highlight the need for considering overall complications and not only fracture healing, in order to compare post-operative or non-operative complications.
Study limitations
The relatively small number of patients constitutes a limitation in our work. Nevertheless, our patient population corresponds to the clinical activity of a SCI reference department over a 13-year period. Besides, as mentioned above, this population presents the characteristics that are known to be associated with lower-limb fractures in chronic SCI. We therefore assume the relevance of the present results. Another limitation could be linked to a selection bias due to the decision making between surgery and conservative treatment, as non-surgical management results from technical difficulties. In our study, femoral fractures are clearly more operated on than tibial ones. We always discuss fracture management in multidisciplinary meetings including orthopedic surgeons and physical medicine and rehabilitation specialists for all the patients of our regional SCI cohort. Thus, an evaluation of benefit-risk between the different types of management and the possibilities of a surgical approach is made. The results of the present study, indicating that operative treatment is associated with a reduced-risk of overall complications, should be taken into account for the evaluation of this risk-benefit ratio in the future. We think that a small part of the patients could be concerned by such technical limitations, but the literature analysis clearly shows that medical practice habits are the main factor in decision making.15,16,26,29 Our study confirms this point, that all the patients who were initially not managed in our University Hospital Centre had not been operated, because of different habits.
Conclusion
Lower extremity fractures are common specific complications in patients with SCI due to the loss of bone mineral density. These fractures are responsible, directly or indirectly, for local and general secondary complications. According to the present study, surgical management of lower-limb fractures in patients with chronic SCI is associated with a reduced risk of overall complications. These results argue that surgery should be systematically considered in these patients. Furthermore, the present study highlights the need for a prospective, randomized controlled trial comparing the surgical vs. non-operative management of sub-lesional fractures in chronic patients with SCI.
Disclaimer statements
Conflicts of interest The authors have no conflicts of interest to report.
ORCID
Marc Dautyhttp://orcid.org/0000-0003-4798-293X
References
- 1.Uebelhart D, Demiaux-Domenech B, Roth M, Chantraine A.. Bone metabolism in spinal cord injured individuals and in others who have prolonged immobilisation. A review. Paraplegia 1995;33(11):669–73. [DOI] [PubMed] [Google Scholar]
- 2.Dauty M, Perrouin Verbe B, Maugars Y, Dubois C, Mathe JF.. Supralesional and sublesional bone mineral density in spinal cord-injured patients. Bone 2000;27(2):305–9. doi: 10.1016/S8756-3282(00)00326-4 [DOI] [PubMed] [Google Scholar]
- 3.Ding W-G, Jiang S-D, Zhang Y-H, Jiang L-S, Dai L-Y.. Bone loss and impaired fracture healing in spinal cord injured mice. Osteoporos Int 2011;22(2):507–15. doi: 10.1007/s00198-010-1256-8 [DOI] [PubMed] [Google Scholar]
- 4.Battaglino RA, Lazzari AA, Garshick E, Morse LR.. Spinal cord injury-induced osteoporosis: pathogenesis and emerging therapies. Curr Osteoporos Rep 2012;10(4):278–85. doi: 10.1007/s11914-012-0117-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang L, Liu L, Pan Z, Zeng Y.. Serum leptin, bone mineral density and the healing of long bone fractures in men with spinal cord injury. Bosn J Basic Med Sci 2015;15(4):69–74. doi: 10.17305/bjbms.2015.693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zehnder Y, Lüthi M, Michel D, Knecht H, Perrelet R, Neto I, et al. Long-term changes in bone metabolism, bone mineral density, quantitative ultrasound parameters, and fracture incidence after spinal cord injury: a cross-sectional observational study in 100 paraplegic men. Osteoporos Int 2004;15(3):180–9. doi: 10.1007/s00198-003-1529-6 [DOI] [PubMed] [Google Scholar]
- 7.Garland DE, Adkins RH, Kushwaha V, Stewart C.. Risk factors for osteoporosis at the knee in the spinal cord injury population. J Spinal Cord Med 2004;27:202–6. doi: 10.1080/10790268.2004.11753748 [DOI] [PubMed] [Google Scholar]
- 8.Pelletier CA, Dumont FS, Leblond J, Noreau L, Giangregorio L, Craven BC.. Self-report of one-year fracture incidence and osteoporosis prevalence in a community cohort of Canadians with spinal cord injury. Top Spinal Cord Inj Rehabil 2014;20(4):302–9. doi: 10.1310/sci2004-302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazo MG, Shirazi P, Sam M, Giobbie-Hurder A, Blacconiere MJ, Muppidi M.. Osteoporosis and risk of fracture in men with spinal cord injury. Spinal Cord 2001;39(4):208–14. doi: 10.1038/sj.sc.3101139 [DOI] [PubMed] [Google Scholar]
- 10.Middleton JW, Lim K, Taylor L, Soden R, Rutkowski S.. Patterns of morbidity and rehospitalisation following spinal cord injury. Spinal Cord 2004;42(6):359–67. doi: 10.1038/sj.sc.3101601 [DOI] [PubMed] [Google Scholar]
- 11.Nelson A, Ahmed S, Harrow J, Fitzgerald S, Sanchez-Anguiano A, Gavin-Dreschnack D.. Fall-related fractures in persons with spinal cord impairment: a descriptive analysis. SCI Nurs 2003;20(1):30–7. [PubMed] [Google Scholar]
- 12.Carbone LD, Chin AS, Burns SP, Svircev JN, Hoenig H, Heggeness M, et al. Morbidity following lower extremity fractures in men with spinal cord injury. Osteoporos Int 2013;24(8):2261–7. doi: 10.1007/s00198-013-2295-8 [DOI] [PubMed] [Google Scholar]
- 13.Young A, Webster B, Giunti G, Pransky G, Nesathurai S.. Rehospitalization following compensable work-related tetraplegia. Spinal Cord 2006;44(6):374–82. doi: 10.1038/sj.sc.3101858 [DOI] [PubMed] [Google Scholar]
- 14.Carbone LD, Chin AS, Burns SP, Svircev JN, Hoenig H, Heggeness M, et al. Mortality after lower extremity fractures in men with spinal cord injury. J Bone Miner Res 2014;29(2):432–9. doi: 10.1002/jbmr.2050 [DOI] [PubMed] [Google Scholar]
- 15.Bethel M, Bailey L, Weaver F, Le B, Burns SP, Svircev JN, et al. Surgical compared with nonsurgical management of fractures in male veterans with chronic spinal cord injury. Spinal Cord 2015;53(5):402–7. doi: 10.1038/sc.2015.5 [DOI] [PubMed] [Google Scholar]
- 16.Frotzler A, Cheikh-Sarraf B, Pourtehrani M, Krebs J, Lippuner K.. Long-bone fractures in persons with spinal cord injury. Spinal Cord 2015;53(9):701–4. doi: 10.1038/sc.2015.74 [DOI] [PubMed] [Google Scholar]
- 17.Bishop JA, Suarez P, Diponio L, Ota D, Curtin CM.. Surgical versus nonsurgical treatment of femur fractures in people with spinal cord injury: an administrative analysis of risks. Arch Phys Med Rehabil 2013;94(12):2357–64. doi: 10.1016/j.apmr.2013.07.024 [DOI] [PubMed] [Google Scholar]
- 18.Garland DE, Adkins RH, Stewart CA.. Five-year longitudinal bone evaluations in individuals with chronic complete spinal cord injury. J Spinal Cord Med 2008;31(5):543–50. doi: 10.1080/10790268.2008.11753650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Staa TP Van, Leufkens HGM, Cooper C.. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 2002;13(10):777–87. doi: 10.1007/s001980200108 [DOI] [PubMed] [Google Scholar]
- 20.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med 2011;34(6):535–46. doi: 10.1179/204577211X13207446293695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiang S-D, Jiang L-S, Dai L-Y.. Effects of spinal cord injury on osteoblastogenesis, osteoclastogenesis and gene expression profiling in osteoblasts in young rats. Osteoporos Int 2007;18(3):339–49. doi: 10.1007/s00198-006-0229-4 [DOI] [PubMed] [Google Scholar]
- 22.Liu D, Li H, Zhao C-Q, Jiang L-S, Dai L-Y.. Changes of substance P-immunoreactive nerve fiber innervation density in the sublesional bones in young growing rats at an early stage after spinal cord injury. Osteoporos Int 2008;19(4):559–69. doi: 10.1007/s00198-007-0481-2 [DOI] [PubMed] [Google Scholar]
- 23.Hjeltnes N, De Groot P, Birkeland KI, Falch JA, Iversen PO.. Tetraplegic subjects have hyperleptinaemia with marked circadian variation. Clin Endocrinol (Oxf) 2005;62(2):223–7. doi: 10.1111/j.1365-2265.2005.02204.x [DOI] [PubMed] [Google Scholar]
- 24.Lala D, Dumont FS, Leblond J, Houghton PE, Noreau L.. Impact of pressure ulcers on individuals living with a spinal cord injury. Arch Phys Med Rehabil 2014;95(12):2312–9. doi: 10.1016/j.apmr.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 25.Nelson AL, Groer S, Palacios P, Mitchell D, Sabharwal S, Kirby RL, et al. Wheelchair-related falls in veterans with spinal cord injury residing in the community: a prospective cohort study. Arch Phys Med Rehabil 2010;91(8):1166–73. doi: 10.1016/j.apmr.2010.05.008 [DOI] [PubMed] [Google Scholar]
- 26.Freehafer AA.Limb fractures in patients with spinal cord injury. Arch Phys Med Rehabil 1995;76(9):823–7. doi: 10.1016/S0003-9993(95)80546-X [DOI] [PubMed] [Google Scholar]
- 27.Vestergaard P, Krogh K, Rejnmark L, Mosekilde L.. Fracture rates and risk factors for fractures in patients with spinal cord injury. Spinal Cord 1998;36(11):790–6. doi: 10.1038/sj.sc.3100648 [DOI] [PubMed] [Google Scholar]
- 28.Uehara K, Akai M, Kubo T, Yamasaki N, Okuma Y, Tobimatsu Y, et al. Soft-plastic brace for lower limb fractures in patients with spinal cord injury. Spinal Cord 2013;51(4):327–30. doi: 10.1038/sc.2012.145 [DOI] [PubMed] [Google Scholar]
- 29.Martínez ÁA, Cuenca J, Herrera A, Domingo J.. Late lower extremity fractures in patients with paraplegia. Injury 2002;33(7):583–6. doi: 10.1016/S0020-1383(02)00163-8 [DOI] [PubMed] [Google Scholar]
- 30.McMaster WC, Stauffer ES.. The management of long bone fracture in the spinal cord injured patient. Clin Orthop Relat Res 1975;(112):44–52. [PubMed] [Google Scholar]
- 31.Fattal C, Mariano-Goulart D, Thomas E, Rouays-Mabit H, Verollet C, Maimoun L.. Osteoporosis in persons with spinal cord injury: the need for a targeted therapeutic education. Arch Phys Med Rehabil 2011;92(1):59–67. doi: 10.1016/j.apmr.2010.09.019 [DOI] [PubMed] [Google Scholar]
- 32.Freehafer AA, Hazel CM, Becker CL.. Lower extremity fractures in patients with spinal cord injury. Paraplegia 1981;19(6):367–72. [DOI] [PubMed] [Google Scholar]
- 33.Sugi MT, Davidovitch R, Montero N, Nobel T, Egol KA.. Treatment of lower-extremity long-bone fractures in active, nonambulatory, wheelchair-bound patients. Orthopedics 2012;35(9):1376–82. doi: 10.3928/01477447-20120822-25 [DOI] [PubMed] [Google Scholar]
- 34.Morse LR, Battaglino RA, Stolzmann KL, Hallett LD, Waddimba A, Gagnon D, et al Osteoporotic fractures and hospitalization risk in chronic spinal cord injury. Osteoporos Int 2009;20(3):385–92. doi: 10.1007/s00198-008-0671-6 [DOI] [PMC free article] [PubMed] [Google Scholar]