Case presentation
A 50-year-old woman with a recent diagnosis of poorly differentiated nonteratomatous cervicouterine cancer presented to our hospital for breath-holding episodes resulting in perioral cyanosis. Her medical history was significant for chickenpox at age 8 and shingles at age 15. Before her admission and 10 days after her cancer diagnosis, she was admitted to an outside hospital for confusion and intermittent catatonia. Workup at the outside hospital was unremarkable, and she was diagnosed with adjustment disorder. At home, she continued to decompensate and ultimately became incomprehensible, anorexic, and bedbound, prompting admission to our hospital.
On presentation, the patient was encephalopathic and dysautonomic. She was unresponsive to pain and exhibited diffuse hyperreflexia, episodes of generalized body tremors, and trismus to the point of transecting her tongue. Because of breath-holding spells with oxygen desaturations and the need to acquire a brain MRI, she was intubated. Her continuous EEG and brain MRI were unremarkable. Acyclovir was empirically started for 2 days but discontinued after CSF studies revealed lymphocytic pleocytosis (17 white blood cells/μL with 86% lymphocytes) with negative herpes simplex virus (HSV) PCR (figure). A 5-day course of intravenous methylprednisolone (IVMP) and intravenous immunoglobulin (IVIG) for presumed anti-N-methyl-D-aspartate receptor encephalitis (NMDAR) encephalitis was administered. CSF testing for varicella zoster virus (VZV) by PCR returned positive, prompting a 21-day course of IV acyclovir. The NMDAR antibody CSF titer later also returned positive (1:50; Dalmau Laboratory, University of Pennsylvania, Philadelphia, PA). A diagnosis of anti-NMDAR encephalitis with concomitant VZV detection was made. A week into antiviral treatment, the patient's vital signs normalized and agitation decreased. By discharge, the patient was alert, oriented, and following simple commands but not yet at neurologic baseline.
Figure. Time course of the patient's diagnostics and treatment.
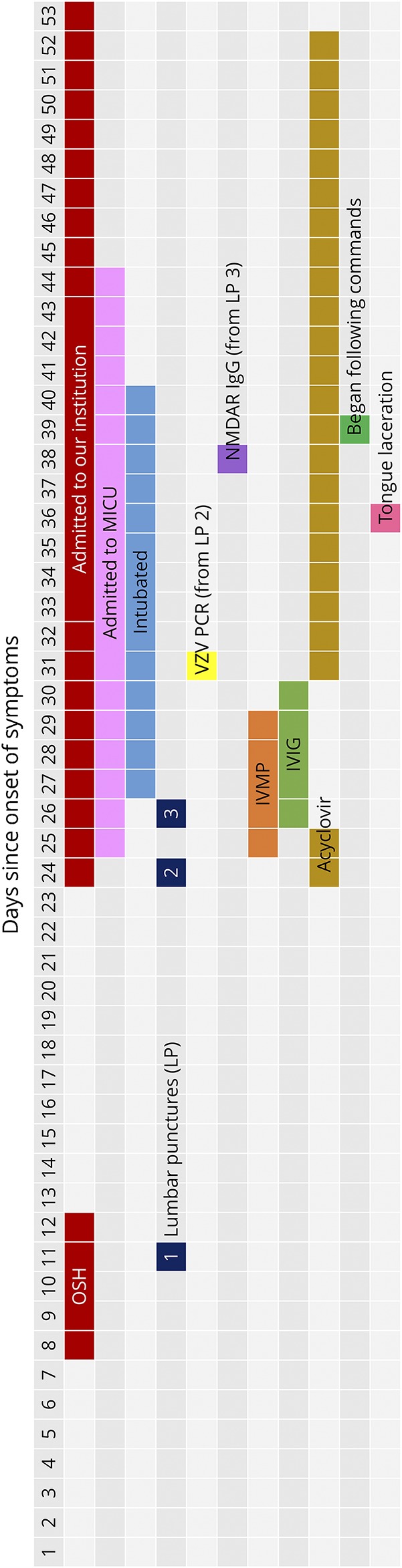
The patient initially presented to an outside hospital for altered behavior and was discharged home with a psychiatric diagnosis. When she continued to deteriorate, she presented to our hospital with breath-holding spells, encephalopathy, and dysautonomia. The patient completed a 5-day course of IVMP and IVIG for presumed anti-NMDAR encephalitis. She was initially started on broad-spectrum antibiotics and acyclovir, which were discontinued after a negative HSV PCR. Once her CSF returned positive for VZV, she was started on a 21-day course of acyclovir. HSV = herpes simplex virus; IVIG = intravenous immunoglobulin; IVMP = intravenous methylprednisolone; LP = lumbar puncture; VZV = varicella zoster virus.
Discussion
This case report demonstrates a rare presentation of anti-NMDAR encephalitis with concomitant VZV detection in the setting of a nonteratomatous gynecologic tumor.1,2 In a seminal case series published in 2008, about 60% of patients with anti-NMDAR encephalitis had a tumor, most often an ovarian teratoma.3 Anti-NMDAR encephalitis has also been linked with tumors of endocervical and endometrial origin.4 These tumors express NMDA receptor 1 (NR1), as well as synaptophysin, neuron-specific enolase, CD56, and chromogranin. Resection of tumors that express NRs can shorten recovery time.5 Our patient's tumor expressed synaptophysin, but NR1 testing was not performed. Thus, it is unknown whether her cervicouterine tumor demonstrates a true association with NMDAR immunoreactivity.
Neurotropic viruses, most frequently HSV, have been linked to anti-NMDAR encephalitis.6 One proposed mechanism for this association is that these viruses may lyse neurons, releasing antigens that sensitize IgG antibodies to the NR and triggering autoimmune encephalitis.1,2 Another hypothesis is that CNS inflammation from anti-NMDAR encephalitis may cause shedding of latent viral DNA or a viral reactivation leading to secondary encephalitis.7
To date, VZV has been documented twice in the setting of anti-NMDAR encephalitis.1,2 One patient presented with cranial nerve palsies and improved significantly after treatment with IV acyclovir and immunoadsorption. The other patient had a teratoma and presented with confusion and behavioral changes after a viral-like illness. She was refractory to treatment with teratoma resection, acyclovir, IVIG, and plasma exchange.
Our patient completed the full first-line therapy for both anti-NMDAR and VZV encephalitis. Although her improvement in symptoms correlated temporally with antiviral therapy, the effects of the IVMP and IVIG treatment cannot be discounted because the response to immunotherapy often lags behind its completion. Because she was treated for both disease processes, it is unclear whether VZV triggered our patient's autoimmune condition or was present in the CSF as a result of latent viral shedding. Her presenting symptoms were more consistent with anti-NMDAR encephalitis than VZV encephalitis. Nevertheless, we recommend antiviral treatment in cases of anti-NMDAR encephalitis with concomitant VZV detection because the immunosuppressive regimen for anti-NMDAR encephalitis may worsen an underlying VZV infection.
Previous literature suggests that anti-NMDAR encephalitis should be considered in any person aged 50 years or younger who presents with acute psychotic changes of less than 4 weeks' duration, especially in the setting of a viral prodrome or abnormal movements.5 Current standard of care for patients with suspected anti-NMDAR encephalitis is to treat with acyclovir until HSV PCR testing is complete. Our case is part of a growing body of evidence that suggests providers should continue antiviral treatment until VZV PCR testing has resulted negative as well. Additional research could investigate the optimum treatment course and prognosis when anti-NMDAR encephalitis presents with concomitant viral detection.
Acknowledgment
The authors thank Dr. Jennifer Chu for her invaluable help in interpreting the patient's EEG studies.
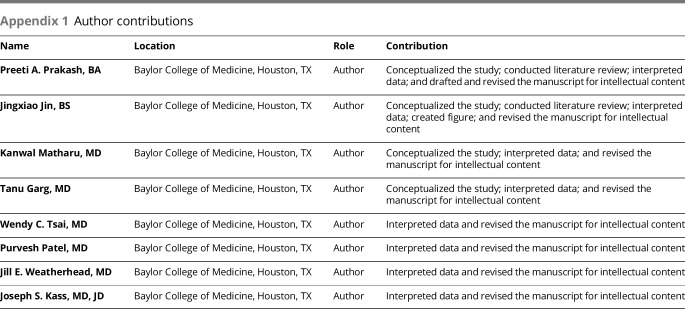
Appendix 1. Author contributions
Study funding
No targeted funding reported.
Disclosure
P.A. Prakash and J. Jin report no disclosures. K. Matharu owns stock in Johnson and Johnson. T. Garg, W.C. Tsai, P. Patel, and J.E. Weatherhead report no disclosures. J.S. Kass received travel funding and/or speaker honoraria from the National Board of Medical Examiners, American Academy of Neurology, BrainPac; is an associate editor for Continuum and Continuum Audio; received publishing royalties from Elsevier; and has been a paid speaker for Pri-Med. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/NN.
References
- 1.Schäbitz WR, Rogalewski A, Hagemeister C, Bien CG. VZV brainstem encephalitis triggers NMDA receptor immunoreaction. Neurology 2014;83:2309–2311. [DOI] [PubMed] [Google Scholar]
- 2.Solís N, Salazar L, Hasbun R. Anti-NMDA Receptor antibody encephalitis with concomitant detection of Varicella zoster virus. J Clin Virol 2016;83:26–28. [DOI] [PubMed] [Google Scholar]
- 3.Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008;7:1091–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hara M, Morita A, Kamei S, et al. Anti-N-methyl-D-aspartate receptor encephalitis associated with carcinosarcoma with neuroendocrine differentiation of the uterus. J Neurol 2011;258:1351–1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalmau J, Lancaster E, Martinez-Hernandez E, Rosenfeld MR, Balice-Gordon R. Clinical experience and laboratory investigations in patients with NMDAR encephalitis. Lancet Neurol 2011;10:63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nosadini M, Mohammad SS, Corazza F, et al. Herpes simplex virus-induced anti-N-methyl-d-aspartate receptor encephalitis: a systematic literature review with analysis of 43 cases. Dev Med Child Neurol 2017;59:796–805. [DOI] [PubMed] [Google Scholar]
- 7.Linnoila J, Binnicker M, Majed M, Klein C, McKeon A. CSF herpes virus and autoantibody profiles in the evaluation of encephalitis. Neurol Neuroimmunol Neuroinflamm 2016;3:245 doi: 10.1212/NXI.0000000000000245. [DOI] [PMC free article] [PubMed] [Google Scholar]