Abstract
Objective
To determine whether diagnoses of traumatic brain injury (TBI), posttraumatic stress disorder (PTSD), and depression, alone or in combination, increase dementia risk among older female veterans.
Methods
This cohort study included data from 109,140 female veterans ≥55 years of age receiving care from Veterans Health Administration medical centers in the United States between October 2004 and September 2015 with at least 1 follow-up visit. TBI, PTSD, depression, and medical conditions at study baseline and incident dementia were determined according to ICD-9-CM codes. Fine-Gray proportional hazards models were used to determine the association between military-related risk factors and dementia diagnosis, accounting for the competing risk of death.
Results
During follow-up (mean 4.0 years, SD 2.3), 4% of female veterans (n = 4,125) developed dementia. After adjustment for demographics and medical conditions, women with TBI, PTSD, and depression had a significant increase in risk of developing dementia compared to women without these diagnoses (TBI-adjusted subdistribution hazard ratio [adjusted sHR] 1.49, 95% confidence interval [CI] 1.01–2.20; PTSD adjusted sHR 1.78, 95% CI 1.34–2.36; and depression-adjusted sHR 1.67, 95% CI 1.55–1.80), while women with >1 diagnosis had the highest risk for dementia (adjusted sHR 2.15, 95% CI 1.84–2.51).
Conclusions
We found that women with military-related risk factors had an ≈50% to 80% increase in developing dementia relative to women without these diagnoses, while female veterans with multiple risk factors had a >2-fold risk of developing dementia. These findings highlight the need for increased screening of TBI, PTSD, and depression in older women, especially female veterans.
Veterans are a population who may be at greater risk for developing dementia due to their high prevalence of traumatic brain injury (TBI), posttraumatic stress disorder (PTSD), and depression.1–4 While these risk factors are not unique to military service, compared to nonveterans, veterans are 2 to 5 times more likely to have TBI, PTSD, or depression.5–7 It is estimated that among veterans previously deployed for Operations Enduring Freedom and Iraqi Freedom, almost 1 in 3 have one of these military-related risk factors.8 Furthermore, the risk of dementia may be further elevated because these conditions often co-occur, particularly with greater frequency, in veterans.9
Notably, studies examining military-related and other risk factors for dementia in veterans have been conducted almost exclusively among men. This is a considerable disparity in the field, especially because more women are joining the military10 and female veterans may be at greater risk for certain psychiatric conditions compared to male veterans.11,12 In addition, the thresholds for certain risk factors may vary by sex, and studies suggest that biological differences between men and women, possibly as a result of hormonal interactions or sex-divergent signaling pathways, could modify the effect of these factors on dementia risk.13–15 We sought to address this critical gap by conducting a study of military-related risk factors for dementia in a large cohort of older female veterans. We hypothesized that military-related risk factors would increase the risk of dementia among female veterans.
Methods
Study population
We identified all female Veterans Health Administration (VHA) patients 55 to 110 years of age who were evaluated (inpatient or outpatient visit) between October 1, 2004, and September 30, 2015. Exposure to military-related risk factors was assessed over a 4-year baseline period (starting from the first encounter date). Data were sourced from 2 nationwide VHA system databases: the inpatient and outpatient visits database (National Patient Care Databases [NPCD]) and the Vital Status File database. Women had to have at least 1 visit during the baseline period and at least 1 follow-up visit (n = 112,831), and we excluded those with prevalent dementia (n = 3,691) during the 4-year baseline period. The final sample size was 109,140.
Standard protocol approvals, registrations, and patient consents
All study procedures were approved by institutional review boards at the University of California, San Francisco; San Francisco Veterans Affairs Medical Center; and US Army Medical Research and Materiel Command, Office of Research Protections, Human Research Protection Office. Informed consent was waived because the data were deidentified administrative data.
Military-related risk factors for dementia: TBI, depression, and PTSD
TBI, depression, and PTSD diagnoses were determined with ICD-9-CM codes at all inpatient and outpatient visits during baseline. TBI was defined by a comprehensive list of ICD-9-CM codes used by the Defense and Veterans Brain Injury Center and the Armed Forces Health Surveillance Branch for TBI surveillance (2012 criteria).16 Diagnosis codes 296.2, 296.3, and 311 were used for depression, and code 309.81 was used for PTSD.
Dementia
Prevalent dementia during baseline and incident dementia over follow-up were identified with the comprehensive list of ICD-9-CM codes provided by the VA Dementia Steering Committee (2016 version).17
Other measures
Demographic information and medical and psychiatric comorbid conditions were obtained from the NPCD. Demographic data, including age and race/ethnicity (categorized as non-Hispanic white, non-Hispanic black, Hispanic, or other/unknown), were based on self-report from the first encounter visit. In addition, we used ZIP code and 2016 American Community Survey data to classify veterans as living in broad educational and income strata. Education was defined as a 2-level variable categorized according to whether veterans were living in a ZIP code tabulation area where ≤25% vs >25% of the adult population had completed a college education (bachelor's degree or higher). Income was defined as a 3-level variable categorized by tertile of median ZIP code tabulation area income for adults.
Comorbid conditions were assessed during the 4-year baseline with standard ICD-9-CM codes from the NPCD. Comorbid conditions potentially associated with dementia included diabetes mellitus, hypertension, myocardial infarction, TIA/stroke, alcohol abuse, and tobacco use.
Analyses
Baseline characteristics of female veterans were grouped on the basis of the following: no military-related risk factors, TBI only, PTSD only, depression only, and >1 military-related risk factor. We compared these groups using analysis of variance for continuous variables and χ2 analysis for categorical variables.
Fine-Gray proportional hazards models were used to examine time to dementia diagnosis, accounting for the competing risk of death, with censoring at the date of the last medical encounter and age as the time scale.18 Models that included all military-related risk factors—TBI only, PTSD only, depression only, and >1 military-related risk factor—were unadjusted and then adjusted for confounding factors selected a priori in steps for demographics (age, race, education, and income) and demographics and comorbid conditions and reported as subdistribution hazard ratios (sHRs) with 95% confidence intervals (CIs). We also performed several sensitivity analyses: 1) requiring 2 diagnoses for each risk factor; 2) imposing a 2-year lag between military-related risk factor exposure and dementia diagnosis; and 3) adjusting for the number of health care follow-up visits (defined as the number of inpatient or outpatient visits per person per year). Proportional hazards model assumptions were checked for all final models. Values of p were 2 sided with statistical significance defined as p < 0.05. All analyses were performed with SAS version 9.4.
Data availability
The study data are derived from VHA electronic health records and contain protected health information; therefore, the data cannot be placed it in a public repository. Please contact the authors for additional details regarding the process of accessing this data.
Results
Of the 109,140 female veterans without dementia at baseline, the average age was 68.5 (SD 9.4) years, and the average follow-up time was 4.0 (SD 2.3) years. Most women (74%) were non-Hispanic white; 12% were non-Hispanic black; and the remaining were Hispanic (1%), Asian (1%), or other/unknown (12%).
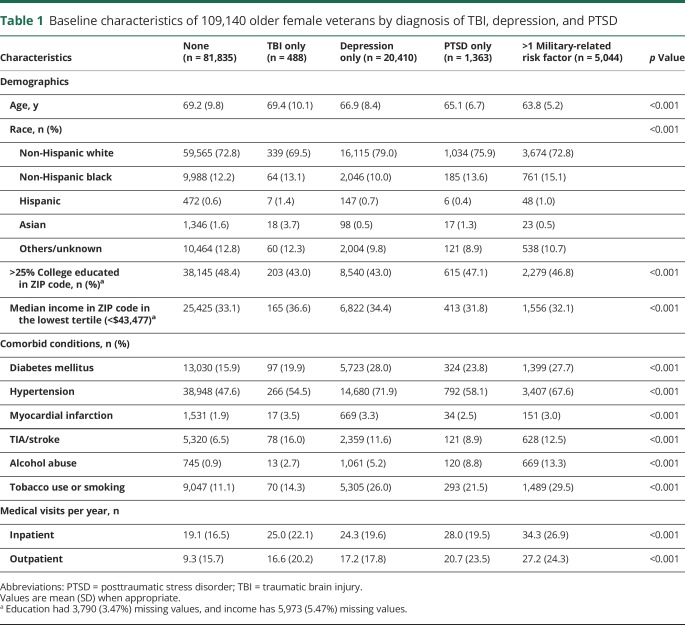
Baseline characteristics of the veterans (separated into nonoverlapping groups determined by depression, PTSD, and TBI diagnoses) are shown in table 1. Women with diagnoses of depression or PTSD were younger than women with no diagnoses or those with TBI. Race, education, and income also differed significantly between the groups, such that relative to women without diagnoses, women with depression were more likely to be white, women with TBI and depression were located in areas with less education, and women with TBI lived in less wealthy ZIP codes. Women with TBI, depression, or PTSD were also more likely to have medical comorbid conditions than women with no diagnoses (p < 0.05 for all).
Table 1.
Baseline characteristics of 109,140 older female veterans by diagnosis of TBI, depression, and PTSD
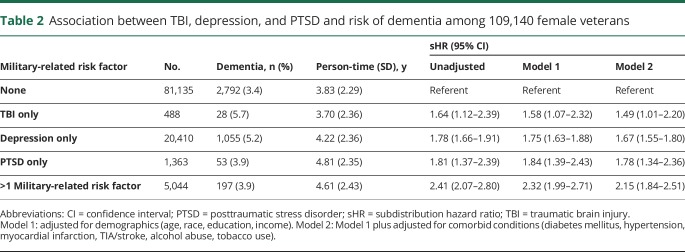
Overall, 4,125 women (4%) developed dementia during follow-up. Compared to women with no military-related risk factors (3.4%), those with diagnoses of TBI, depression, or PTSD had higher rates of incident dementia (with incident rates ranging from 3.9% for PTSD to 5.7% for TBI, p <0.001). Table 2 shows the unadjusted and adjusted risks for the association between TBI, depression, and PTSD and dementia. TBI, depression, and PTSD alone increased the risk of dementia in models fully adjusted for demographics and comorbid conditions (TBI-adjusted sHR 1.49, 95% CI 1.01–2.20; depression-adjusted sHR 1.67, 95% CI 1.55–1.80; PTSD-adjusted sHR 1.78, 95% CI 1.34–2.36). Women with >1 military-related risk factor had the highest risk of dementia (adjusted sHR 2.15, 95% CI 1.84–2.51). Cumulative incidence of dementia adjusted for demographics and comorbid conditions in the 5 groups is shown in the figure.
Table 2.
Association between TBI, depression, and PTSD and risk of dementia among 109,140 female veterans
Figure. Cumulative incidence of dementia among older female veterans.
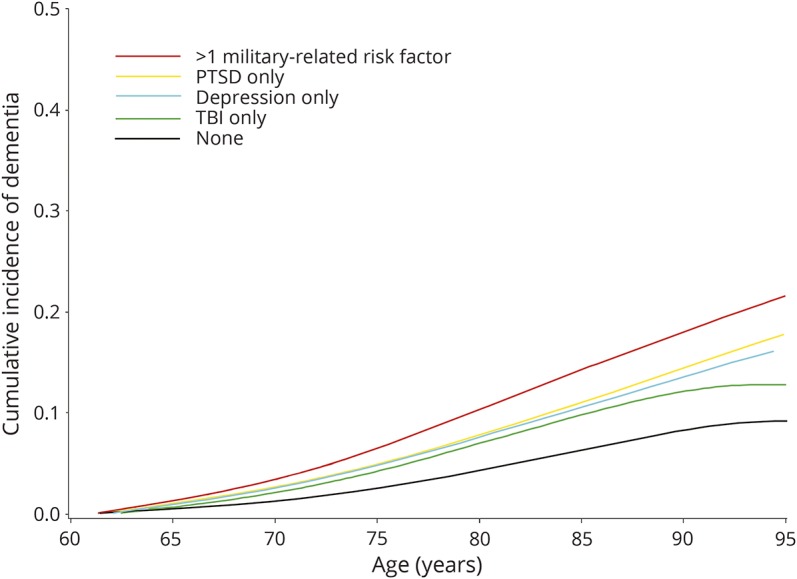
PTSD = posttraumatic stress disorder; TBI = traumatic brain injury.
We performed a sensitivity analysis that required women to have at least 2 diagnoses for military-related risk factors of interest. The results of this analysis were similar in magnitude and significance to our main findings. We also conducted an additional sensitivity analysis imposing a 2-year lag between military-related risk factors diagnosis and dementia diagnosis, and the estimated effect sizes and significance were nearly identical to our primary models. Because of the concern that diagnoses (PTSD, depression, TBI) would lead to increased follow-up visits, which in turn could lead to earlier detection of dementia, we conducted a final sensitivity analysis in which we adjusted for the number of follow-up visits per person per year for each group. The number of visits varied significantly between the groups; women with TBI, depression, or PTSD had more than twice the number of medical visits per year than the women with no diagnoses. Results were similar to the original findings but attenuated, particularly for women with TBI and those with >1 military risk factor (TBI-adjusted sHR 1.16, 95% CI 0.77–1.77, depression-adjusted sHR 1.52, 95% CI 1.41–1.64, PTSD-adjusted sHR 1.56, 95% CI 1.18–2.07, >1 risk factor–adjusted sHR 1.57, 95% CI 1.33–1.86).
Discussion
Our study of >100,000 older women investigated the relationship between military-related risk factors and dementia risk in female veterans. We found that women with TBI, depression, or PTSD had an ≈50% to 80% increase in risk of developing dementia relative to women without these diagnoses, while women with multiple conditions (e.g., TBI with depression or PTSD) had a >2-fold increase in dementia risk even after adjustment for demographics, common medical comorbid conditions, alcohol abuse, and tobacco use.
In our study, having a TBI increased dementia risk in female veterans by 50%. A few prior studies reported nonsignificant relationships between TBI and dementia,19–21 possibly as a result of variations in the definition of TBI or other methodologic differences.22 The association observed in our study is consistent with recent research in veteran and civilian populations indicating that TBI increases the risk of developing dementia.3,23,24 In addition, these findings parallel estimates from our prior study of male veterans in which TBI was similarly associated with a 60% increase in the risk of dementia.3 It has been hypothesized that the link between TBI and dementia risk may be due to axonal damage,25 an injury that reduces cognitive reserve, thereby increasing vulnerability to dementia neuropathology or accelerating production of dementia-related proteins such as β-amyloid and tau.26,27 In addition, other neuropathologic changes have been linked to both TBI and dementia, including white matter degeneration and neuroinflammation.28,29 Evidence from humans and animal models suggests that the inflammatory cascade triggered after a TBI may be distinct for men and women30 and that estrogen and progesterone could have neuroprotective effects after brain injury.15,31 While the extent to which TBI outcomes differ between men and women is unclear,32,33 these results demonstrate that women are also vulnerable to the long-term neurologic effects of TBI. Female veterans are an especially critical population because they may acquire a TBI from injuries, falls, or intimate partner violence, similar to women in the general population, but also through their military service and increasing involvement in combat.34
Our findings indicate that PTSD and depression independently increase dementia risk in older female veterans. There is a robust body of evidence to support depression as a risk factor for developing dementia with studies in both community-based populations of women35,36 and (mostly male) veterans,2 but there is very little information pertaining to risk among female veterans, who reportedly have higher rates of depression compared to male veterans.12,37,38 In our cohort, risk of dementia increased by almost 70% for female veterans with depression. While the observed association was slightly lower than the risk reported in a comparable study of older male veterans (hazard ratio 2.18, 95% CI 2.08–2.28),2 it supports a risk relationship between depression and dementia in older women.
Rates of PTSD are also high among female veterans,38,39 and in our study, risk of dementia increased by almost 80% for female veterans with PTSD. This is consistent with other investigations in male veterans that report an increase in risk of 80% to 100%.1,40 Mechanisms linking PTSD and depression to dementia are less well defined but may include inflammation, high levels of cortisol or other stress markers, and increased vascular disease.41–43 These results highlight the possibility that early and more targeted treatment of PTSD and depression might reduce the risk of developing dementia.
Depression, PTSD, and TBI often co-occur44–46; however, few studies consider the effects of these risk factors together. In our cohort, almost 80% of women with PTSD also had depression or TBI, and almost half of women with TBI also had a psychiatric diagnosis. For those female veterans with a combination of military-related risk factors, dementia risk was found to increase >2-fold. Although the mechanisms remain unclear, having co-occurring conditions may increase an individual's vulnerability to dementia through increased neural damage1,4,41 or decreased cognitive reserve,47 consequences that are common across brain injuries, PTSD, and depression. While the proportion of women in our cohort reporting combat exposure was small, ≈2%, these numbers are expected to increase with the changing roles of women in the military, which could result in greater numbers of female veterans with TBI, PTSD, and depression. Additional longitudinal research is needed to understand the interplay between these risk factors and to determine the potential benefits of targeted prevention for high-risk veterans with multiple military-related risk factors.
Notably, although TBI, PTSD, and depression were associated with incident dementia in our study, these effects were attenuated after accounting for the number of medical follow-up visits. Women with TBI, depression, or PTSD had 2 to 3 times as many visits as women without any diagnosis. This closer follow-up may allow the opportunity to receive a dementia diagnosis earlier because providers have more opportunities to note changes in a veteran's cognition or functioning. Alternatively, individuals with dementia and cognitive decline have an increased risk for hospitalization48,49 and are more likely to present with challenges concerning treatment and diagnosis,50 which can also increase the number of follow-up visits required.
This study has a number of important strengths, including its longitudinal design to determine the effects of military-related risk factors on dementia risk in a large sample of older female veterans. We adjusted for critical medical and demographic variables (although we only had ZIP code–level estimates of education and income) to test the robustness of our findings, and we accounted for possible detection bias by adjusting our models for the number of follow-up visits per year. In the interpretation of these results, it is also necessary to consider the limitations of this study, particularly the use of ICD-9-CM codes to establish diagnoses. Administrative diagnostic codes are less sensitive than structured diagnostic interviews, and it is likely that female veterans with less severe symptoms of depression, PTSD, mild TBI, and dementia did not receive diagnoses. Misdiagnosis and miscoding of military-related risk factors and dementia are also probable. While we conducted a sensitivity analysis requiring 2 diagnoses for our exposures of interest, we were not able to conduct validation studies for these diagnostic codes. However, we expect that such misclassification would most likely lead to a bias toward the null. In addition, despite the results of our sensitivity analysis imposing a 2-year lag, we cannot completely eliminate the possibility that these associations reflect prodromal relationships or reverse causality. Finally, we had limited ability to examine dementia subtypes, so we cannot determine whether the military-related risk factors increase dementia risk differentially.
In a very large cohort of older female veterans, military-related risk factors increased dementia risk by 50% to 80% when occurring independently and 2-fold when occurring together. These results emphasize the need for more comprehensive studies of dementia risk among women, particularly female veterans, and highlight the potential role of military-related risk factor screening and treatment to reduce dementia risk.
Glossary
- CI
confidence interval
- ICD-9-CM
International Classification of Diseases, 9th Revision, Clinical Modification
- NPCD
National Patient Care Databases
- PTSD
posttraumatic stress disorder
- sHR
subdistribution hazard ratio
- TBI
traumatic brain injury
- VHA
Veterans Health Administration
Footnotes
Editorial, page 117
Author contributions
K.Y. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. K.Y. obtained funding and designed and supervised the study. K.Y., C.B.P., S.J.L., F.X., and T.D.H. were responsible for acquisition, analysis, and interpretation of data. All authors contributed to the writing and review of the manuscript.
Study funding
This research was supported by Department of Defense grant W81XWH-16-1-0507 (principal investigator: Yaffe) and National Institute on Aging grant K24 AG031155 (principal investigator: Yaffe).
Disclosure
K. Yaffe serves on the Data Safety Monitoring Board for Takeda Inc and a National Institute on Aging–sponsored study and is member of the Beeson Scientific Advisory Board. S. Lwi, T. Hoang, F. Xia, D. Barnes, S. Maguen, and C. Peltz report no disclosures relevant to the manuscript. Go to Neurology.org/N for full disclosures.
Publication history
Received by Neurology April 12, 2018. Accepted in final form August 31, 2018.
References
- 1.Yaffe K, Vittinghoff E, Lindquist K, et al. Posttraumatic stress disorder and risk of dementia among US veterans. Arch Gen Psychiatry 2010;67:608–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Byers AL, Covinsky KE, Barnes DE, Yaffe K. Dysthymia and depression increase risk of dementia and mortality among older veterans. Am J Geriatr Psychiatry 2012;20:664–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnes DE, Kaup A, Kirby KA, Byers AL, Diaz-Arrastia R, Yaffe K. Traumatic brain injury and risk of dementia in older veterans. Neurology 2014;83:312–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Veitch DP, Friedl KE, Weiner MW. Military risk factors for cognitive decline, dementia and Alzheimer's disease. Curr Alzheimer Res 2013;10:907–930. [DOI] [PubMed] [Google Scholar]
- 5.Richardson LK, Frueh BC, Acierno R. Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry 2010;44:4–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jordan BK, Schlenger WE, Hough R, et al. Lifetime and current prevalence of specific psychiatric disorders among Vietnam veterans and controls. Arch Gen Psychiatry 1991;48:207–215. [DOI] [PubMed] [Google Scholar]
- 7.Eibner C, Krull H, Brown KM, et al. Current and projected characteristics and unique health care needs of the patient population served by the Department of Veterans Affairs. Rand Health Q 2016;5:13. [PMC free article] [PubMed] [Google Scholar]
- 8.Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND Corp; 2008. [Google Scholar]
- 9.Chapman JC, Diaz-Arrastia R. Military traumatic brain injury: a review. Alzheimers Demen 2014;10:S97–S104. [DOI] [PubMed] [Google Scholar]
- 10.US Department of Veterans Affairs (VA) National Center for Veterans Analysis and Statistics. Women Veterans Report: The Past, Present, and Future of Women Veterans. Washington, D.C.:2017. [Google Scholar]
- 11.Haskell SG, Gordon KS, Mattocks K, et al. Gender differences in rates of depression, PTSD, pain, obesity, and military sexual trauma among Connecticut war veterans of Iraq and Afghanistan. J Women's Health 2010;19:267–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramchand R, Rudavsky R, Grant S, Tanielian T, Jaycox L. Prevalence of, risk factors for, and consequences of posttraumatic stress disorder and other mental health problems in military populations deployed to Iraq and Afghanistan. Curr Psychiatry Rep 2015;17:37. [DOI] [PubMed] [Google Scholar]
- 13.Yan Y, Dominguez S, Fisher DW, Dong H. Sex differences in chronic stress responses and Alzheimer's disease. Neurobiol Stress 2018;8:120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nebel RA, Aggarwal NT, Barnes LL, et al. Understanding the impact of sex and gender in Alzheimer's disease: a call to action. Alzheimers Dement 2018;14:1171–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Engler-Chiurazzi EB, Brown CM, Povroznik JM, Simpkins JW. Estrogens as neuroprotectants: estrogenic actions in the context of cognitive aging and brain injury. Prog Neurobiol 2017;157:188–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armed Forces Health Surveillance Branch. Standard surveillance case definitions [online]. Available at: health.mil/Military-Health-Topics/Health-Readiness/Armed-Forces-Health-Surveillance-Branch/Epidemiology-and-Analysis/Surveillance-Case-Definitions. Accessed May 15, 2017.
- 17.US Department of Veterans Affairs (VA) Veterans Health Administration (VHA) Dementia Steering Committee (DSC). VHA dementia steering committee recommendations for dementia care in the VHA health care system 2016 [online]. Available at: https://www.va.gov/GERIATRICS/docs/VHA_DSC_RECOMMENDATIONS_SEPT_2016_9-12-16.pdf. Accessed May 15, 2017.
- 18.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999;94:496–509. [Google Scholar]
- 19.Dams-O'Connor K, Gibbons LE, Bowen JD, McCurry SM, Larson EB, Crane PK. Risk for late-life re-injury, dementia and death among individuals with traumatic brain injury: a population-based study. J Neurol Neurosurg Psychiatry 2013;84:177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lindsay J, Laurin D, Verreault R, et al. Risk factors for Alzheimer's disease: a prospective analysis from the Canadian Study of Health and Aging. Am J Epidemiol 2002;156:445–453. [DOI] [PubMed] [Google Scholar]
- 21.Mehta K, Ott A, Kalmijn S, et al. Head trauma and risk of dementia and Alzheimer's disease the Rotterdam Study. Neurology 1999;53:1959. [DOI] [PubMed] [Google Scholar]
- 22.Kristman VL, Borg J, Godbolt AK, et al. Methodological issues and research recommendations for prognosis after mild traumatic brain injury: results of the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil 2014;95:S265–S277. [DOI] [PubMed] [Google Scholar]
- 23.Gardner RC, Yaffe K. Traumatic brain injury may increase risk of young onset dementia. Ann Neurol 2014;75:339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nordström A, Nordström P. Traumatic brain injury and the risk of dementia diagnosis: a nationwide cohort study. PLoS Med 2018;15:e1002496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson VE, Stewart W, Smith DH. Axonal pathology in traumatic brain injury. Exp Neurol 2013;246:35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson VE, Stewart W, Smith DH. Widespread tau and amyloid-beta pathology many years after a single traumatic brain injury in humans. Brain Pathol (Zurich, Switzerland) 2012;22:142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uryu K, Chen XH, Martinez D, et al. Multiple proteins implicated in neurodegenerative diseases accumulate in axons after brain trauma in humans. Exp Neurol 2007;208:185–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson VE, Stewart JE, Begbie FD, Trojanowski JQ, Smith DH, Stewart W. Inflammation and white matter degeneration persist for years after a single traumatic brain injury. Brain 2013;136:28–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kraus MF, Susmaras T, Caughlin BP, Walker CJ, Sweeney JA, Little DM. White matter integrity and cognition in chronic traumatic brain injury: a diffusion tensor imaging study. Brain 2007;130:2508–2519. [DOI] [PubMed] [Google Scholar]
- 30.Villapol S, Loane DJ, Burns MP. Sexual dimorphism in the inflammatory response to traumatic brain injury. Glia 2017;65:1423–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brotfain E, Gruenbaum SE, Boyko M, Kutz R, Zlotnik A, Klein M. Neuroprotection by estrogen and progesterone in traumatic brain injury and spinal cord injury. Curr Neuropharmacol 2016;14:641–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mollayeva T, El-Khechen-Richandi G, Colantonio A. Sex & gender considerations in concussion research. Concussion 2018;3:CNC51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cancelliere C, Donovan J, Cassidy JD. Is sex an indicator of prognosis after mild traumatic brain injury: a systematic analysis of the findings of the World Health Organization Collaborating Centre Task Force on Mild Traumatic Brain Injury and the International Collaboration on Mild Traumatic Brain Injury Prognosis. Arch Phys Med Rehabil 2016;97:S5–S18. [DOI] [PubMed] [Google Scholar]
- 34.Amoroso T, Iverson KM. Acknowledging the risk for traumatic brain injury in women veterans. J Nerv Ment Dis 2017;205:318–323. [DOI] [PubMed] [Google Scholar]
- 35.Zeki Al Hazzouri A, Vittinghoff E, Byers A, et al. Long-term cumulative depressive symptom burden and risk of cognitive decline and dementia among very old women. J Gerontol A Biol Sci Med Sci 2014;69:595–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goveas JS, Espeland MA, Woods NF, Wassertheil-Smoller S, Kotchen JM. Depressive symptoms and incidence of mild cognitive impairment and probable dementia in elderly women: the Women's Health Initiative Memory Study. J Am Geriatr Soc 2011;59:57–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ramsey C, Dziura J, Justice AC, et al. Incidence of mental health diagnoses in veterans of Operations Iraqi Freedom, Enduring Freedom, and New Dawn, 2001–2014. Am J Public Health 2016;107:329–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Curry JF, Aubuchon-Endsley N, Brancu M, et al. Lifetime major depression and comorbid disorders among current-era women veterans. J Affect Disord 2014;152–154:434–440. [DOI] [PubMed] [Google Scholar]
- 39.Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran status. Am J Prev Med 2018;54:e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Qureshi SU, Kimbrell T, Pyne JM, et al. Greater prevalence and incidence of dementia in older veterans with posttraumatic stress disorder. J Am Geriatr Soc 2010;58:1627–1633. [DOI] [PubMed] [Google Scholar]
- 41.Byers AL, Yaffe K. Depression and dementias among military veterans. Alzheimers Demen 2014;10:S166–S173. [DOI] [PubMed] [Google Scholar]
- 42.Greenberg MS, Tanev K, Marin MF, Pitman RK. Stress, PTSD, and dementia. Alzheimers Demen 2014;10:S155–S165. [DOI] [PubMed] [Google Scholar]
- 43.Miller MW, Lin AP, Wolf EJ, Miller DR. Oxidative stress, inflammation, and neuroprogression in chronic PTSD. Harv Rev Psychiatry 2017;26:57–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ciurli P, Formisano R, Bivona U, Cantagallo A, Angelelli P. Neuropsychiatric disorders in persons with severe traumatic brain injury: prevalence, phenomenology, and relationship with demographic, clinical, and functional features. J Head Trauma Rehabil 2011;26:116–126. [DOI] [PubMed] [Google Scholar]
- 45.Bhalerao SU, Geurtjens C, Thomas GR, Kitamura CR, Zhou C, Marlborough M. Understanding the neuropsychiatric consequences associated with significant traumatic brain injury. Brain Inj 2013;27:767–774. [DOI] [PubMed] [Google Scholar]
- 46.Iverson KM, Hendricks AM, Kimerling R, et al. Psychiatric diagnoses and neurobehavioral symptom severity among OEF/OIF VA patients with deployment-related traumatic brain injury: a gender comparison. Women Health Issues 2011;21:S210–S217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Butters MA, Young JB, Lopez O, et al. Pathways linking late-life depression to persistent cognitive impairment and dementia. Dialogues Clin Neurosci 2008;10:345–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. JAMA 2012;307:165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ehlenbach WJ, Hough CL, Crane PK, et al. Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA 2010;303:763–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harris DP, Chodosh J, Vassar SD, Vickrey BG, Shapiro MF. Primary care providers' views of challenges and rewards of dementia care relative to other conditions. J Am Geriatr Soc 2009;57:2209–2216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The study data are derived from VHA electronic health records and contain protected health information; therefore, the data cannot be placed it in a public repository. Please contact the authors for additional details regarding the process of accessing this data.