Abstract
Objectives
To investigate longitudinal associations between gross motor development, motor milestone achievement and weight-for-length z scores in a sample of infants. In a secondary aim, we explored potential bidirectional relationships, as higher weight-for-length z scores may impede motor development, and poor motor development may lead to obesity.
Design
The design was an observational birth cohort.
Setting
We used data from the Nurture study, a birth cohort of predominately black women and their infants residing in the Southeastern USA.
Participants
666 women enrolled their infants in Nurture. We excluded infants with missing data on exposure, outcome or main covariates, leaving a total analytic sample of 425 infants.
Primary outcome
The outcome was weight-for-length z score, measured when infants were 3, 6, 9 12 months.
Results
Among infants, 64.7% were black, 18.8% were white and 16.9% were other/multiple race. Mean (SD) breastfeeding duration was 17.6 (19.7) weeks. Just over one-third (38.5%) had an annual household income of < $20 000. After adjusting for potential confounders, higher motor development score was associated with lower weight-for-length z score (−0.004; 95% CI −0.001 to –0.007; p=0.01), mainly driven by associations among boys (−0.007; 95% CI −0.014 to –0.001; p=0.03) and not girls (0.001; 95% CI −0.005 to 0.008; p=0.62). Earlier crawling was the only milestone associated with a lower weight-for-length z score at 12 months (−0.328; 95% CI −0.585 to 0.072; p=0.012). However, this association appeared to be driven by male infants only (−0.461; 95% CI −0.825 to −0.096; p=0.01). Weight-for-length z score was unrelated to subsequent motor development score and was thus not bidirectional in our sample.
Conclusions
Higher motor development score and earlier crawling were associated with lower subsequent weight-for-length z score. However, this was primary true for male infants only. These findings contribute to the growing body of evidence suggesting that delayed motor development may be associated with later obesity.
Keywords: developmental milestones, gross motor, infant, motor milestones, obesity
Strengths and limitations of this study.
This study includes multiple prospective measures of motor development and weight-for-length z scores, which allowed for careful assessment of the temporality of the relationship between the two.
Previous studies have not included sufficient representation of participants from racial minority groups. This cohort consists of predominately black women and infants.
We were not able to follow infants in the Nurture sample beyond 12 months of age.
Nurture participants were not representative of the larger population in the Southeastern USA.
We experienced attrition from birth to the 12-month follow-up; approximately 29% of mothers and their infants withdrew or were lost to follow-up.
Background
Early childhood is a critical period for preventing obesity and its related complications.1–3 Identifying early predictors of excessive weight gain can help inform effective interventions to prevent later obesity.4 As a result, recent calls to action highlight the importance of promoting gross motor activity and decreasing sedentary time for very young children.5–9 While there is evidence of an association between gross motor activity and obesity in early childhood,10–18 findings from previous studies have not been consistent—perhaps due to bidirectional relationships among these variables.
Some studies have shown that excess adiposity may impede movement and compromise motor development.16–18 In one study, obesity and excess subcutaneous fat were associated with delayed motor development, but motor development was unrelated to subsequent weight status.18 Another study found that heavier infants sat up without support earlier, but weight status was largely unrelated to other motor milestones.19
Other studies suggest that physical activity and gross motor skills may provide opportunities to expend energy and may help prevent obesity.20 21 Earlier attainment of gross motor milestones, such as crawling and walking, may provide opportunities for infants to move regularly, increasing movement and thus energy expenditure.15 Given the conflicting findings and the potential complexity of the relationship, we investigated longitudinal associations between gross motor development and weight for length, and explored potential bidirectional relationships, in a sample of racially diverse infants.
Methods
Study design and population
We used data from the Nurture study, a birth cohort of predominately black women and their infants residing in the Southeastern USA.22 The overall goal of Nurture is to identify factors related to feeding, physical activity, sleep and stress that contribute to excessive weight gain in infancy, focusing on the role of various caregivers. Between 2013 and 2015, we enrolled women in the study in later pregnancy and confirmed participations shortly after birth. Women provided written, informed consent for themselves and their infants to participate in the study. The Institutional Review Board of Duke University Medical Center approved this study and its protocol.
Trained data collectors conducted home visits when infants were 3, 6, 9 and 12 months of age. In addition, women received automated interactive voice response (IVR) telephone calls in months 1, 2, 4, 5, 7, 8, 10 and 11 to assess a limited set of behaviours, including infant motor milestone achievement. Of the 666 women who enrolled their infants in Nurture after birth, 535 (80.3%) completed the 3 month home visit, 497 (74.6%) completed the 6 month visit, 457 (68.6%) completed the 9 month visit and 468 (70.3%) completed the 12 month visit. For the present study, we excluded infants with missing data on weight-for-length z scores at 12 months (n=35) leaving 433 infants. We further excluded those with missing information on covariates included in all models a priori and those with missing motor development scores or values outside the WHO windows for motor milestone of achievement (n=8), leaving a total analysis sample of 425 infants.
We conducted two distinct sets of analyses. First, we examined associations between motor development measured using the Bayley Scales of Infant and Toddler Development: Third Edition23 and weight-for-length z score. We hypothesised that poor motor development would be associated with higher weight-for-length z scores longitudinally throughout infancy. Second, we examined associations of gross motor milestone achievement (rolling over, sitting up, crawling and walking) and weight-for-length z score. We hypothesised that delayed achievement of motor milestones would be associated with higher weight for length z score at 12 months.
Exposure: motor development and motor milestones
We used two measures to define motor development. First, we used the Bayley Scales of Infant and Toddler Development: Third Edition to measure motor development of infants at each home visit at 3, 6, 9 and 12 months. This is an individually administrated test that has been designed to assess children development in five different functional areas: fine motor, gross motor, cognition, language, social emotion and adaptive. For this study, we used the motor composite score—the sum of the fine and gross motor scores. The fine motor score is composed of 66 items, which assess fine perceptual-motor integration, motor planning and speed, visual tracking, reaching, object grasping, object manipulation, functional hand skills and responses to tactile information. The gross motor score is composed of 72 items, which asses the movement of limbs and torso, static positions, dynamic movement balance and motor planning. The descriptive classification of Bayley Scales of Infant and Toddler Development includes seven ordinal categories: extremely low score (composite score of 69 and below), borderline (composite score of 70–79), low average (composite score of 80–89), average (composite score of 90–109), high average (composite score of 110–119), superior (composite score of 120–129) and very superior (composite score of 130 and above). To allow our results to be comparable with previous studies,16 18 we used the sum of the fine and gross motor scores for the first analysis. However, we also examined the scaled gross motor development score only, as we were most interested in motor development as a marker of physical activity.
Second, mothers reported whether their infants had achieved each of four gross motor milestones monthly during the IVR call: rolling over without assistance, sitting up without assistance, crawling using all four limbs and walking without assistance. Consistent with our previous study24 and based on the WHO windows for motor milestone achievement,15 we categorised age of achievement into three groups. We collapsed groups that contained fewer than 25 infants. Infants who were not able to achieve a particular milestone by the end of the study period were included in the oldest possible age category.
Outcome: weight-for-length z score
Trained data collectors measured infant weight and length at each home visit—recumbent length to the nearest 1/8th inch and weight to the nearest 0.1 pound in triplicate. We then used the average of the three measures. We calculated age- and sex-specific weight-for-length z scores using WHO reference standards.25
Other measures
We collected demographic information from mothers via interviews and questionnaires at recruitment, at birth, during IVR calls and during each home visit. Infant variables of interest included age, gender, birth weight for gestational age z score and race (black, white, other). We abstracted information on infant birth weight in grams and length in centimetres from the medical record. We calculated birth weight for gestational age z score using international reference data put forth by Intergrowth-21st Newborn Birth Weight Standards and Z Scores.26 Maternal variables of interest included age, education (≤high school graduate, some college, college graduate or graduate degree), household income (<$20,000, ≥$20,000), and prepregnancy body mass index (BMI). We also documented breastfeeding status during each IVR call and calculated the total number of months of any breast feeding for each infant.
Statistical analysis
We calculated means and SD for continuous demographic variables and percentages for categorical variables. We explored mean trajectories of both motor development score and weight-for-length z score at 3, 6, 9 and 12 months for male and female infants, separately. In the first analysis, we examined the association between motor development score and weight-for-length z score at a subsequent visit using lagged repeated-measures linear regression. A first-order autoregressive covariance structure to account for association between the repeated measures among infants. We included all covariates discussed above in the model. We also ran the same model to examine the association between gross motor development score only and subsequent weight-for-length z score. Additionally, as some studies have suggested a bidirectional association between motor development and weight status, we investigated the effect of weight-for-length z score at an earlier visit on motor development score at a given current visit. For example, when predicting weight-for-length z score at the 6 month visit, we used motor development score at the 3 month visit. We took this approach to ensure that the exposure preceded the outcome.
In the second analysis, we used separate linear regressions to investigate the association between age at achievement of each of the four milestones and weight-for-length z score at 12 months. We included the same covariates of interest in the models. To explore differences by gender, we ran the same models separately among girls and boys. We present results in terms of parameter estimates, 95% CI, and two-sided p values. We conducted all analyses using SAS V.9.4 at a significance level of <0.05.
Patient and public involvement
Research participants were not involved in the development, recruitment or conduct of the study. We will disseminate results of the study through scientific publications and mailings to research participants.
Results
Among infants, 50.6% were girls and 49.4% were boys (table 1). The mean (SD) birth weight for gestational age z score was −0.3 (1.0). In terms of race, 64.7% of infants were black, 18.8% were white and 16.9% were of ‘other’ race. The mean (SD) breastfeeding duration was 17.6 (19.7) weeks. Among mothers, 44.1% had some college, college graduate or graduate degree, and 55.9% were married or living with partner. Just over one-third (38.5%) had an annual household income of less than $20 000. Mothers had a mean (SD) prepregnancy BMI of 30.6 (9.4) and age of 28.13 (5.1) years. At 12 months, 66.5% of infants were normal weight and over one-third were considered at risk of overweight, overweight or obese.
Table 1.
Characteristics of mothers and infants participating in the Nurture study (n=433)
| Infant characteristics | Mean (SD) |
| Birth weight for gestational age z score | −0.3 (1.0) |
| Age at 12 month home visit, days | 373.9 (23.6) |
| Weight-for-length z score at 12 months | 0.6 (1.0) |
| Any breast feeding, weeks | 17.6 (19.7) |
| Motor development composite score at 12 months | 97.9 (10.7) |
| Per cent (number) | |
| Gender, female | 50.6 (219) |
| Race | |
| Black | 64.7 (280) |
| White | 18.5 (80) |
| Other race/more than one race | 16.9 (73) |
| Ethnicity, Latino/a | 9.0 (37) |
| Weight-for-length z score at 12 months by WHO category | |
| Severely wasted (severely underweight) | _ |
| Wasted (underweight) | 0.5 (2) |
| Normal | 66.5 (288) |
| Possible risk of overweight | 24.7 (107) |
| Overweight | 6.7 (29) |
| Obese | 1.6 (7) |
| Age of rolling over | |
| 4 months and younger | 72.1 (312) |
| Older than 4 months | 27.9 (121) |
| Age of sitting up | |
| 5 months and younger | 44.3 (192) |
| 5–6 months | 33.0 (143) |
| Older than 6 months | 22.6 (98) |
| Age of crawling | |
| 6 months and younger | 19.9 (86) |
| 7–8 months | 40.4 (175) |
| Older than 8 months | 39.7 (172) |
| Age of walking | |
| 11 months and younger | 34.7 (150) |
| 12 months | 28.9 (125) |
| Older than 12 | 36.3 (157) |
| Maternal characteristics | Mean (SD) |
| Age, years | 28.1 (5.8) |
| Prepregnancy body mass index, kg/m2 | 30.6 (9.3) |
| Per cent (frequency) | |
| Race | |
| Black | 67.4 (292) |
| White | 22.2 (96) |
| Other race/more than one race | 10.4 (45) |
| Ethnicity, Latina | 5.6 (24) |
| Education | |
| ≤High school graduate | 44.1 (191) |
| Some college, college graduate or graduate degree | 55.9 (242) |
| Marital status | |
| Married or living with partner | 59.1 (253) |
| Never married, divorced, separated, other | 40.9 (175) |
| Household Characteristics | Per cent (frequency) |
| Annual household income | |
| < $20 000 | 38.3 (166) |
| ≥ $20 000 | 61.7 (267) |
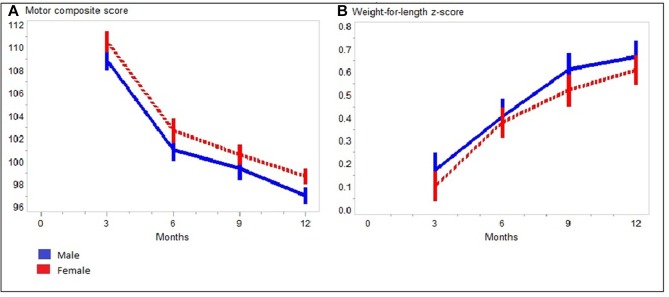
Figure 1 illustrates the mean (SD) of motor development scores and weight-for-length z scores over time among males and females, separately. As figure 1A shows, motor development scores decreased slightly over infancy, with a mean of 109.7 (11.9) at birth and 97.9 (10.7) at 12 months. figure 1B shows an increasing trend for weight-for-length z scores, indicating that infants got relatively heavier throughout the assessment period. In this sample, the mean weight-for-length z score was 0.1 (1.0) at birth and increased to 0.6 (1.0) at 12 months. There was no evidence of outlying observations when we examined the scaled residuals from the final model.27
Figure 1.
Mean trajectories of motor development score (A) and weight-for-length z score (B) throughout infancy.
After adjusting for potential confounders, higher motor development score was associated with lower weight-for-length z score (−0.004; 95% CI −0.001 to –0.007; p=0.01) (table 2). For every ten-unit increase in motor development score (measured at a previous visit), weight-for-length z score decreased by 0.04 on average. In the stratified analysis, higher motor development score was associated with lower weight-for-length z score (at the subsequent assessment) among males (−0.007; 95% CI −0.01 to –0.001; p=0.03) but not females (0.001; 95% CI −0.005 to 0.008; p=0.62). Similarly, when we examined gross motor score only, higher motor development score was associated with lower weight-for-length z score (−0.02; 95% CI −0.03 to –0.004; p=0.01). This association appeared driven by male infants only (−0.03; 95% CI −0.06 to –0.003; p=0.03).
Table 2.
Adjusted* longitudinal regression estimates and 95% CI in analyses examining motor development score and subsequent weight-for-length z score from 3 to 12 months
| Infant weight-for-length z score | |||
| Estimate | 95% CI | P value | |
| Motor development score | |||
| All infants (n=425) | −0.004 | −0.007 to −0.001 | 0.03 |
| Male infants only (n=213) | −0.007 | −0.01 to −0.001 | 0.03 |
| Female infants only (n=211) | 0.001 | −0.005 to 0.008 | 0.62 |
| Gross motor development score | |||
| All infants (n=425) | −0.02 | −0.031 to −0.004 | 0.01 |
| Male infants only (n=213) | −0.03 | −0.06 to −0.003 | 0.03 |
| Female infants only (n=211) | 0.005 | −0.02 to 0.034 | 0.74 |
*Adjusted for maternal prepregnancy body mass index, age and education; household income; infant race, gender, birth weight for gestational age z score, breast feeding and motor development score at previous visit.
Earlier achievement of rolling over, sitting up and walking were not associated with weight-for-length z score at 12 months (table 3). However, earlier crawling was associated with lower weight-for-length z score at 12 months: infants who crawled at 6 months or younger had an average z score 0.33 lower than those who crawled at 9 months or older (−0.33; 95% CI −0.59 to 0.07; p=0.01). In stratified analyses, we observed this association in male infants only (−0.46; 95% CI −0.83 to –0.10; p=0.01). Finally, weight-for-length z score was unrelated to subsequent motor development score (0.07; 95% CI −0.81 to 0.96; p=0.87), and thus the association appears to be primarily from motor development to weight status rather than vice versa.
Table 3.
Adjusted* longitudinal regression estimates and 95% CI in analyses examining motor milestone achievement and subsequent weight-for-length z score from 3 to 12 months
| Age of motor milestone achievement | Estimate | 95% CI | P value |
| All infants (n=425) | |||
| Rolling over (ref=older than 4 months) | |||
| 4 months or younger | −0.19 | −0.40 to 0.008 | 0.06 |
| Sitting up (ref=older than 6 months) | |||
| 5 months or younger | 0.19 | −0.06 to 0.43 | 0.13 |
| 5–6 months | 0.22 | −0.03 to 0.48 | 0.09 |
| Crawling (ref=9 months and older) | |||
| 6 months or younger | −0.34 | −0.59 to −0.09 | 0.008 |
| 7–8 months | 0.01 | −0.20 to 0.21 | 0.94 |
| Walking (ref=older than 12 months) | |||
| 11 months and younger | −0.17 | −0.39 to 0.06 | 0.14 |
| 12 months | 0.13 | −0.10 to 0.37 | 0.27 |
| Male infants only (n=208) | |||
| Rolling over (ref=older than 4 months) | |||
| 4 months or younger | −0.29 | −0.60 to 0.02 | 0.06 |
| Sitting up (ref=older than 6 months) | |||
| 5 months or younger | 0.18 | −0.17 to 0.54 | 0.31 |
| 5–6 months | 0.27 | −0.10 to 0.64 | 0.15 |
| Crawling (ref=9 months and older) | |||
| 6 months or younger | −0.46 | −0.83 to −0.10 | 0.01 |
| 7–8 months | −0.06 | −0.37 to 0.25 | 0.91 |
| Walking (ref=older than 12 months) | |||
| 11 months and younger | −0.09 | −0.44 to 0.26 | 0.63 |
| 12 months | 0.08 | −0.28 to 0.44 | 0.66 |
| Female infants only (n=217) | |||
| Rolling over (ref=older than 4 months) | |||
| 4 months or younger | −0.12 | −0.40 to 0.16 | 0.39 |
| Sitting up (ref=older than 6 months) | |||
| 5 months or younger | 0.18 | −0.16 to 0.52 | 0.30 |
| 5–6 months | 0.16 | −0.20 to 0.53 | 0.37 |
| Crawling (ref=9 months and older) | |||
| 6 months or younger | −0.27 | −0.63 to 0.08 | 0.13 |
| 7–8 months | 0.05 | −0.24 to 0.33 | 0.75 |
| Walking (ref=older than 12 months) | |||
| 11 months and younger | −0.25 | −0.56 to 0.05 | 0.10 |
| 12 months | 0.20 | −0.14 to 0.54 | 0.24 |
*Adjusted for maternal prepregnancy body mass index, age and education; household income; infant race, gender, birth weight for gestational age z score and breast feeding.
Discussion
Among this sample of racially diverse infants, we found that higher motor development score was associated with lower subsequent weight-for-length z score. We also found that earlier crawling was associated with lower weight-for-length z score at 12 months. However, earlier achievement of the other three gross motor milestones was not associated weight-for-length z score at 12 months. Multiple studies found that delayed or poor motor development was associated with excessive weight among infants and young children,15 although a few found no association.18 28 There are some differences in these studies in the timing and the method of assessing both motor development and obesity. For example, a study of 25 148 children in Denmark showed that later achievement of motor milestones (sitting up and walking) was not associated with overweight at age 7 years, and later achievement of motor milestones was not a substantial risk factor for later increasing BMI.29 Infant motor milestone achievement was reported retrospectively by mothers in this study. Nevertheless, their results support our finding that sitting up and walking were not associated with later weight. However, another study reported significant associations of age of achievement of rolling over, sitting up and walking but not crawling with adiposity at age 3 years. Motor milestone achievement was also reported retrospectively by mothers. Also relevant to our study, Slining et al.18 found that overweight infants were more likely to have concurrent delayed motor development among a sample of low-income African-American infants. However, in contrast to our findings, motor development was unrelated to subsequent anthropometry. We used Bayley Scales of Infant and Toddler Development: Third Edition23 (the composite motor score) to measure motor development of infant while Slining et al used the second edition of the same scale. This might explain some of the differences in the findings. To test the sensitivity of our findings to the measure of exposure, we performed the analysis using the gross motor development score only and found similar results.
We also observed clear differences by gender. Higher motor development score was associated with lower weight-for-length z score among males but not females in our sample of infants. Additionally, among males only, earlier crawling was associated with lower weight-for-length z score at 12 months. Previous studies examining this research question did not present differences by gender.18 29 However, in studies of older children, and consistent with our findings, researchers observed differences in motor development among boys only.12 14 30 In these prior studies, obesity in boys was associated with poorer gross motor performance. As a possible explanation, the researchers suggest that society may put greater pressure on boys to participate in physical activity from a young age—boys who opt out of these activities may not have the same opportunity to fully develop their motor skills.12 30 The researchers hypothesise that gender-specific associations between obesity and motor development impairment may be evident in even younger children, and suggest further research. A recent systematic review in children ages 4–6 years notes a positive relation between physical activity and motor milestone achievement, which could help explain the association.31 Parental support of physical activity may also play a role in motor development differences between boys and girls. In a longitudinal study among 12-year-old children,32 girls reported less parental support of physical activity when compared with boys. Findings from the same study suggested that higher levels of parental support were translated to higher levels of physical activity in boys but not girls. These differences may be evident even earlier in childhood, although evidence is lacking.
Another explanation could be physiological differences in body composition between males and females in infancy. There is some evidence that very young male and female infants show differences in body fat and fat-free mass percentages, with girls having more fat mass at 1 month of age.33 However, these differences by gender were no longer evident by 6 months.33 Other studies have essentially found no differences in infant percent body fat by gender.34 We consistently observed associations between motor development and weight-for-length z score in male infants only and agree that this finding warrants further exploration.
Breast feeding may also influence the relationship between obesity and motor development in infancy. Some evidence suggests improved motor development in breastfed infants and toddlers,35 but findings have not been consistent across multiple studies.36 In our study, 28.51% of infants were breast fed at 6 months of age, which is lower than the national prevalence of 57.6%.37 Further research is needed to investigate the exact role of breast feeding on the relationship between early obesity and motor development. In our study, we controlled for breast feeding in the final model.
Regardless, motor development in infancy may influence a number of behaviours and outcomes in later childhood. Prior studies suggest that earlier attainment was associated with educational achievement,38 intelligence39 40 and executive function28 in later life. Moreover, motor milestone achievement within normal windows during infancy was associated with better physical performance41 and greater grip strength42 in middle adulthood. Unfortunately, we were not able to follow infants in the Nurture sample beyond 12 months of age. Future studies may consider longer follow-up periods to more fully assess outcomes throughout childhood.
This study has other limitations. First, Nurture participants were not representative of the larger population in the Southeastern USA. We enrolled some women from an obstetric clinic that served a high percentage of low-income white women with high-risk pregnancies, but overall, our sample included a higher percentage of black women. Also, we experienced attrition from birth to the 12 month follow-up; approximately 29% of mothers and their infants withdrew or were lost to follow-up. This retention rate, however, is not unusual. In a similar birth cohort from the same geographic region, attrition at the 12 month follow-up exceeded 50%.43 Moreover, this study reports on findings up to 12 months of follow-up for the Nurture cohort. However, a relatively large percent of children walk after 12 months of age.24 Given the relatively short study period, we were not able to assess children who walked after the end of data collection.
Conclusions
Preventing excessive weight gain in infancy is especially important, and the first year of life represents a critical window for intervention. Although rates of weight gain and obesity did not increase substantially in children ages 6–23 months from 1976 to 2014, there were significant increases among non-Hispanic black children.44 Additionally, a recent study suggests that rapid weight gain in infancy may be more detrimental for black children compared with white children by the time they reach age 5 years.45 Thus, it is a public health priority to better understand factors contributing to excess weight gain in infancy—especially among black children. Our study contributes to the growing body of evidence suggesting that delayed motor development may be associated with higher weight-for-length z scores in the future. Intervention efforts may be warranted to encourage movement and help facilitate gross motor development in young children.46
Supplementary Material
Footnotes
Patient consent for publication: Not required.
Contributors: AS conducted the analysis, drafted components of the manuscript, and approved the final manuscript. BN oversaw the analysis, reviewed and edited the manuscript, and approved the final manuscript. SEB-N designed the study, conceived of the analysis, drafted components of the manuscript, and approved the final manuscript. TØ contributed to the design of the study, reviewed and edited the manuscript, and approved the final manuscript.
Funding: This study was supported by a grant from the National Institutes of Health (R01DK094841). The funders had no role in the design of the study, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The datasets generated and analysed for the current study are not publicly available due to human subject’s restrictions at Duke University Medical Center but may available from the corresponding author on reasonable request with appropriate permissions and agreements in place.
References
- 1. Kim J, Lee I, Lim S. Overweight or obesity in children aged 0 to 6 and the risk of adult metabolic syndrome: A systematic review and meta-analysis. J Clin Nurs 2017;26:3869–80. 10.1111/jocn.13802 [DOI] [PubMed] [Google Scholar]
- 2. Lloyd LJ, Langley-Evans SC, McMullen S. Childhood obesity and adult cardiovascular disease risk: a systematic review. Int J Obes 2010;34:18–28. 10.1038/ijo.2009.61 [DOI] [PubMed] [Google Scholar]
- 3. Perng W, Rifas-Shiman SL, Kramer MS, et al. . Early Weight Gain, Linear Growth, and Mid-Childhood Blood Pressure: A Prospective Study in Project Viva. Hypertension 2016;67:301–8. 10.1161/HYPERTENSIONAHA.115.06635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gillman MW. Early infancy as a critical period for development of obesity and related conditions. Nestle Nutr Workshop Ser Pediatr Program 2010;65:13–20. 10.1159/000281141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Obesity prevention policies. Early childhood obesity prevention policies. http://www.iom.edu/Reports/2011/Early-Childhood-Obesity-Prevention-Policies.aspx
- 6. Larson N, Ward DS, Neelon SB, et al. . What role can child-care settings play in obesity prevention? A review of the evidence and call for research efforts. J Am Diet Assoc 2011;111:1343–62. 10.1016/j.jada.2011.06.007 [DOI] [PubMed] [Google Scholar]
- 7. Child Care Providers. Let’s Move! Chlid Care. https://letsmove.obamawhitehouse.archives.gov/child-care-providers
- 8. Active start. A statement of physical activity guidelines for children from birth to age. www.shapeamerica.org/standards/guidelines/activestart.cfm
- 9. American Academy of Pediatrics APHA, National Resource Center for Health and Safety in Child Care and Early Education. Caring for our children:national health and safety performance standards; guidelines for early care and education programs. 3rd Edn Elk Grove Village: ednIL: American Academy of Pediatrics, 2011. [Google Scholar]
- 10. Kakebeeke TH, Lanzi S, Zysset AE, et al. . Association between body composition and motor performance in preschool children. Obes Facts 2017;10:420–31. 10.1159/000477406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Graf C, Koch B, Kretschmann-Kandel E, et al. . Correlation between BMI, leisure habits and motor abilities in childhood (CHILT-project). Int J Obes Relat Metab Disord 2004;28:22–6. 10.1038/sj.ijo.0802428 [DOI] [PubMed] [Google Scholar]
- 12. Mond JM, Stich H, Hay PJ, et al. . Associations between obesity and developmental functioning in pre-school children: a population-based study. Int J Obes 2007;31:1068–73. 10.1038/sj.ijo.0803644 [DOI] [PubMed] [Google Scholar]
- 13. Okely AD, Booth ML, Chey T. Relationships between body composition and fundamental movement skills among children and adolescents. Res Q Exerc Sport 2004;75:238–47. 10.1080/02701367.2004.10609157 [DOI] [PubMed] [Google Scholar]
- 14. Cawley J, Spiess CK. Obesity and skill attainment in early childhood. Econ Hum Biol 2008;6:388–97. 10.1016/j.ehb.2008.06.003 [DOI] [PubMed] [Google Scholar]
- 15. Benjamin Neelon SE, Oken E, Taveras EM, et al. . Age of achievement of gross motor milestones in infancy and adiposity at age 3 years. Matern Child Health J 2012;16:1015–20. 10.1007/s10995-011-0828-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Camargos ACR, Mendonça VA, Andrade CA, et al. . Overweight and obese infants present lower cognitive and motor development scores than normal-weight peers. Res Dev Disabil 2016;59:410–6. 10.1016/j.ridd.2016.10.001 [DOI] [PubMed] [Google Scholar]
- 17. Shibli R, Rubin L, Akons H, et al. . Morbidity of overweight (>or=85th percentile) in the first 2 years of life. Pediatrics 2008;122:267–72. 10.1542/peds.2007-2867 [DOI] [PubMed] [Google Scholar]
- 18. Slining M, Adair LS, Goldman BD, et al. . Infant overweight is associated with delayed motor development. J Pediatr 2010;157:20–5. 10.1016/j.jpeds.2009.12.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. WHO Multicentre Growth Reference Study Group. Relationship between physical growth and motor development in the WHO Child Growth Standards. Acta Paediatr Suppl 2006;450:96–101. [DOI] [PubMed] [Google Scholar]
- 20. Wells JC, Ritz P. Physical activity at 9-12 months and fatness at 2 years of age. Am J Hum Biol 2001;13:384–9. 10.1002/ajhb.1062 [DOI] [PubMed] [Google Scholar]
- 21. Li R, O’Connor L, Buckley D, et al. . Relation of activity levels to body fat in infants 6 to 12 months of age. J Pediatr 1995;126:353–7. 10.1016/S0022-3476(95)70447-7 [DOI] [PubMed] [Google Scholar]
- 22. Benjamin Neelon SE, Østbye T, Bennett GG, et al. . Cohort profile for the Nurture Observational Study examining associations of multiple caregivers on infant growth in the Southeastern USA. BMJ Open 2017;7:e013939 10.1136/bmjopen-2016-013939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bayley N. Bayley scales of infant and toddler development: Bayley-III. San Antonio, Texas, USA, 2006. [Google Scholar]
- 24. WHO Multicentre Growth Reference Study Group. WHO motor development study: windows of achievement for six gross motor development milestones. Acta Paediatr Suppl 2006;450:86–95. [DOI] [PubMed] [Google Scholar]
- 25. WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl 2006;450:76–85. [DOI] [PubMed] [Google Scholar]
- 26. Villar J, Altman DG, Purwar M, et al. . The objectives, design and implementation of the INTERGROWTH-21 st Project. BJOG: An International Journal of Obstetrics & Gynaecology 2013;120:9–26. 10.1111/1471-0528.12047 [DOI] [PubMed] [Google Scholar]
- 27. Fitzmaurice GM, Laird NM. Ware JH: applied longitudinal analysis: John Wiley and Sons, 2012. [Google Scholar]
- 28. Murray GK, Veijola J, Moilanen K, et al. . Infant motor development is associated with adult cognitive categorisation in a longitudinal birth cohort study. J Child Psychol Psychiatry 2006;47:25–9. 10.1111/j.1469-7610.2005.01450.x [DOI] [PubMed] [Google Scholar]
- 29. Schmidt Morgen C, Andersen AM, Due P, et al. . Timing of motor milestones achievement and development of overweight in childhood: a study within the danish national birth cohort. Pediatr Obes 2014;9:239–48. 10.1111/j.2047-6310.2013.00177.x [DOI] [PubMed] [Google Scholar]
- 30. Cairney J, Hay JA, Faught BE, et al. . Developmental coordination disorder and overweight and obesity in children aged 9-14 y. Int J Obes 2005;29:369–72. 10.1038/sj.ijo.0802893 [DOI] [PubMed] [Google Scholar]
- 31. Zeng N, Ayyub M, Sun H, et al. . Effects of physical activity on motor skills and cognitive development in early childhood: a systematic review. Biomed Res Int 2017;2017:1–13. 10.1155/2017/2760716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Telford RM, Telford RD, Olive LS, et al. . Why are girls less physically active than boys? findings from the LOOK longitudinal study. PLoS One 2016;11:e0150041 10.1371/journal.pone.0150041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fields DA, Krishnan S, Wisniewski AB. Sex differences in body composition early in life. Gend Med 2009;6:369–75. 10.1016/j.genm.2009.07.003 [DOI] [PubMed] [Google Scholar]
- 34. Eriksson B, Löf M, Forsum E. Body composition in full-term healthy infants measured with air displacement plethysmography at 1 and 12 weeks of age. Acta Paediatr 2010;99:563–8. 10.1111/j.1651-2227.2009.01665.x [DOI] [PubMed] [Google Scholar]
- 35. Dewey KG, Cohen RJ, Brown KH, et al. . Effects of exclusive breastfeeding for four versus six months on maternal nutritional status and infant motor development: results of two randomized trials in Honduras. J Nutr 2001;131:262–7. 10.1093/jn/131.2.262 [DOI] [PubMed] [Google Scholar]
- 36. Michels KA, Ghassabian A, Mumford SL, et al. . Breastfeeding and motor development in term and preterm infants in a longitudinal US cohort. Am J Clin Nutr 2017;106:1456–62. 10.3945/ajcn.116.144279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. CDC. Centers of disease control and prevention website. 2018. https://www.cdc.gov/breastfeeding/data/facts.html
- 38. Taanila A, Murray GK, Jokelainen J, et al. . Infant developmental milestones: a 31-year follow-up. Dev Med Child Neurol 2005;47:581–6. 10.1111/j.1469-8749.2005.tb01207.x [DOI] [PubMed] [Google Scholar]
- 39. Murray GK, Jones PB, Kuh D, et al. . Infant developmental milestones and subsequent cognitive function. Ann Neurol 2007;62:128–36. 10.1002/ana.21120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Flensborg-Madsen T, Mortensen EL. Infant developmental milestones and adult intelligence: A 34-year follow-up. Early Hum Dev 2015;91:393–400. 10.1016/j.earlhumdev.2015.04.006 [DOI] [PubMed] [Google Scholar]
- 41. Kuh D, Hardy R, Butterworth S, et al. . Developmental origins of midlife physical performance: evidence from a british birth cohort. Am J Epidemiol 2006;164:110–21. 10.1093/aje/kwj193 [DOI] [PubMed] [Google Scholar]
- 42. Kuh D, Hardy R, Butterworth S, et al. . Developmental origins of midlife grip strength: findings from a birth cohort study. J Gerontol A Biol Sci Med Sci 2006;61:702–6. 10.1093/gerona/61.7.702 [DOI] [PubMed] [Google Scholar]
- 43. Fuemmeler BF, Lee CT, Soubry A, et al. . DNA methylation of regulatory regions of imprinted genes at birth and its relation to infant temperament. Genet Epigenet 2016;8:GEG.S40538–67. 10.4137/GEG.S40538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Akinbami LJ, Kit BK, Carroll MD, et al. . Trends in anthropometric measures among us children 6 to 23 months, 1976-2014. Pediatrics 2017;139:e20163374 10.1542/peds.2016-3374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hawkins SS, Rifas-Shiman SL, Gillman MW, et al. . Racial differences in crossing major growth percentiles in infancy. Arch Dis Child 2018;103:795–7. 10.1136/archdischild-2016-311238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Han A, Fu A, Cobley S, et al. . Effectiveness of exercise intervention on improving fundamental movement skills and motor coordination in overweight/obese children and adolescents: a systematic review. J Sci Med Sport 2018;21:89–102. 10.1016/j.jsams.2017.07.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.