Abstract
Introduction
Hypoxemia and hyperoxia may occur after surgery with potential related complications. The FreeO2 PostOp trial is a prospective, multicentre, randomised controlled trial that evaluates the clinical impact of automated O2 administration versus conventional O2 therapy after major abdominal or thoracic surgeries. The study is powered to demonstrate benefits of automated oxygen titration and weaning in term of oxygenation, which is an important surrogate for complications after such interventions.
Methods and analysis
After extubation, patients are randomly assigned to the Standard (manual O2 administration) or FreeO2 group (automated closed-loop O2 administration). Stratification is performed for the study centre and a medical history of chronic obstructive pulmonary disease (COPD). Primary outcome is the percentage of time spent in the target zone of oxygen saturation, during a 3-day time frame. In both groups, patients will benefit from continuous oximetry recordings. The target zone of oxygen saturation is SpO2=88%–92% for patients with COPD and 92%–96% for patients without COPD. Secondary outcomes are the nursing workload assessed by the number of manual O2 flow adjustments, the time spent with severe desaturation (SpO2 <85%) and hyperoxia area (SpO2 >98%), the time spent in a hyperoxia area (SpO2 >98%), the VO2, the duration of oxygen administration during hospitalisation, the frequency of use of mechanical ventilation (invasive or non-invasive), the duration of the postrecovery room stay, the hospitalisation length of stay and the survival rate.
Ethics and dissemination
The FreeO2 PostOp study is conducted in accordance with the declaration of Helsinki and was registered on 11 September 2015 (http://www.clinicaltrials.gov). First patient inclusion was performed on 14 January 2016. The results of the study will be presented at academic conferences and submitted to peer-reviewed journals.
Trial registration number
Keywords: oxygen therapy, postoperative complications, thoracic surgery, abdominal surgery, hypoxemia, hyperoxia
Strengths and limitations.
The FreeO2 PostOp trial is the first and largest clinical evaluation of automated oxygen titration over standard of care in patients undergoing major surgeries.
As automated oxygen titration is not the standard of care for postoperative patients, the study was designed as a superiority study.
The use of continuous and non-averaged SpO2 values monitoring in all groups of patients enables precise oxygenation evaluation during the entire study period.
One limitation of the study is that investigators are aware of the inclusion group, while blinding is difficult in studies with respiratory support.
Second limitation could be that the oxygenation status assessment would have been more precise using arterial blood gases.
Introduction
Background and rationale
Current standards for prescribing oxygen recommend providing adequate flows to correct hypoxemia and avoid hyperoxia.1 2 While deleterious effects of hypoxemia are well known, the potential harmful effects of hyperoxia are underappreciated. Yet, hyperoxia may increase mortality in patients with severe chronic obstructive pulmonary disease (COPD)3–5 and may cause cardiac and neurological adverse toxicities in certain situations.6–8 Precise control of O2 flows is difficult to achieve in clinical practice and is time-consuming.9
The FreeO2 system (Oxynov, Quebec, Canada) is an innovative device, developed in collaboration between our researchers from Brest-France, Quebec-Canada University Hospitals and Oxynov Inc., an R&D spin-off from Laval University-Quebec. FreeO2 is a closed-loop device that automates oxygen administration to spontaneously breathing patients in response to pulse oximetry (SpO2) continuous measurements.10 Automated O2 administration allows to maintain constant SpO2 within a predetermined range using variable O2 flows, as opposed to manual O2 administration where the flow is kept constant, with variable SpO2 values. In preterm infants receiving mechanical ventilation, automated O2 control results in more time spent within the intended SpO2 target.11–13 In a healthy adult model with induced hypoxemia, such a system was more efficient to maintain SpO2 within the oxygenation target, while ensuring a significant reduction of hypoxemia and hyperoxia periods, as compared with constant O2 flows.14 Its efficacy has also been validated in hospitalised patients with COPD15 or during the early emergency care of patients with acute respiratory distress.10
Following major abdominal or thoracic surgery, the risk of hypoxemia may be high while considering patients’ clinical status (obstructive sleep apnoea (OSA), restrictive pathologies related to obesity, frequent comorbidities), the type of surgery and anaesthesia.16–21 Hypoxemia may occur either during the immediate postoperative period (they are mainly related to surgery or anaesthesia) or may be delayed up to 3 days without clear trigger or underlying pathologies. The potential interest of the FreeO2 system, using artificial intelligence closed-loop adjustments and predictive analytics, will thus be (1) to perform frequent and rapid O2 adjustments in response to oxygenation condition variations (up to each second), or to any physiological condition changes (movement, speech, eating, toilet); (2) to enable remote monitoring and data recording in isolated clinical settings (ie, non-ICU surgical ward), in order to detect clinical deterioration at a very early stage through integration and fusion of informations; (3) to avoid maintenance of unnecessary high O2 flow that may be potentially deleterious (hypercapnia worsening, coronary and/or cerebral artery vasoconstriction, etc).
Objectives
The aim of the study is to assess the use feasibility of the FreeO2 system so as to deliver oxygen automatically in the postanaesthesia care unit in a patient population admitted for major abdominal and thoracic surgery. Our hypothesis is that the FreeO2 system will provide a better control of the oxygen saturation and reduce postoperative hypoxemia.
Trial design
The FreeO2 PostOp study is an investigator-initiated, prospective, multicentre, randomised, controlled open trial on medical devices comparing two strategies of oxygen therapy following major surgeries with either standard treatment or automated closed-loop oxygenation. Patients are randomly assigned to the Standard (manual O2 administration) or FreeO2 group (automated closed-loop O2 administration).
Methods: patients, interventions and outcomes
Study setting
The FreeO2 PostOp study is taking place in five different university hospitals in France and Canada (Brest, Clermont-Ferrand, Montpellier, Poitiers, Quebec). The entire study will be performed in accordance with the International Conference on Harmonisation and Good Clinical Practice guidelines.22
Eligibility criteria
Inclusion criteria
To be included, adult patients (≥18 years) may be screened for scheduled abdominal or thoracic surgery during the anaesthesia consultation and be considered as requiring general anaesthesia with an expected duration of 2 hours or more in the participating centres.
Patients with intermediate to high risk for postoperative pulmonary complications following abdominal surgery with general anaesthesia are eligible for participation. To identify such patients, the ARISCAT risk score will be used.23 An ARISCAT risk score ≥26 is associated with an intermediate to high risk for postoperative pulmonary complications.
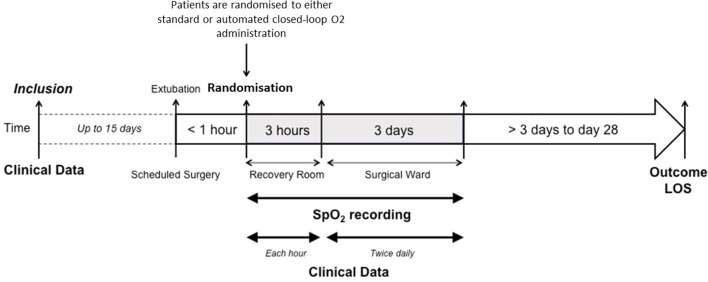
Informed consent is to be signed before the surgery (figure 1).
Figure 1.
Participant timeline of the FreeO2 PostOp study. Inclusion is performed during the anaesthesia consultation, prior to a scheduled major surgery (≥2 hours’ duration; ARISCAT score ≥26). Eligibility criteria are verified and the patient needs to sign the informed consent. Randomisation is performed no later than 1 hour following extubation in the recovery room. Clinical data will be recorded each hour during the first 3 hours of care and twice daily for up to 3 days. Continuous SpO2 recording will be performed in each randomisation groups for up to 3 days. Outcome parameters will be assessed at day 28. LOS, length of stay (days); SpO2, pulse oximetry (%).
Exclusion criteria
Patients fulfilling one or more of the following criteria will not be included: life-threatening condition requiring an unplanned emergent surgery, lack of informed consent prior to randomisation, non-adult patients (age <18 years), patients with a Body Mass Index ≥35 kg/m2, patients with OSA, pregnant or lactating women, perturbed or non-cooperative patients, to provide a relatively homogeneous study population and avoid potential confounding factors in the interpretation.
Randomisation criteria
Patients will be randomised if they fulfil all the following criteria: availability of the FreeO2 prototype; absence of criteria of severity justifying the immediate use of ventilatory support (loss of consciousness with a Glasgow Coma Score ≤12), serious ventricular rhythm disorders, haemodynamic instability (systolic blood pressure <80 mm Hg or recourse to vasopressors), cardiac or respiratory arrest, pH <7.35 and PaCO2 >55 mm Hg (if measured), and necessity of an O2 flow less than 15 L/min to maintain a SpO2 higher than 92%; no emergent surgery required for an adverse event; pulse oximetry signal is available.
Study intervention
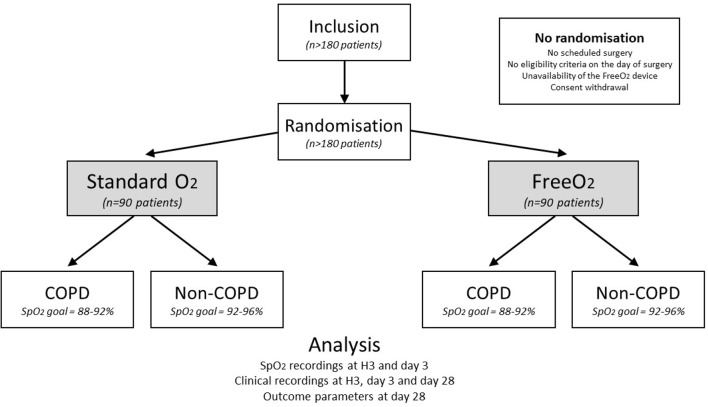
Patients eligible for randomisation will be randomly assigned to the Standard or FreeO2 group (figure 2). The maximal study duration is 3 days. The study was stopped before 3 days if patient was discharged earlier from hospital or in case of discomfort while keeping nasal prongs and sensors.
Figure 2.
Consort diagram of the FreeO2 PostOp study. Randomisation will be performed after verification of the eligibility criteria and it will be stratified according to the presence of a medical history of chronic obstructive pulmonary disease (COPD). For patients without COPD, the target will be a SpO2 range=92%–96%; for patients with COPD, the target will be a SpO2range=88%–92%. Patients will be assigned either to standard continuous O2 administration (Standard: manual adjustment) or automated closed-loop O2 administration (FreeO2: automated adjustment, up to each second); in both groups, continuous SpO2 recordings will be performed during up to 3 days according to the FreeO2 system. SpO2, pulse oximetry (%).
Automated O2 administration is performed using the FreeO2 system (Oxynov) that is set to maintain SpO2 between 92% and 96% for patients without COPD or between 88% and 92% for patients with COPD. FreeO2 is equipped with a SpO2 monitor and an electronically controlled valve that automatically adjusts O2 flows from 0 to 20 L/min on a per-second basis, with a 0.1 L/min precision, according to a closed-loop algorithm in order to reach the predetermined SpO2 target.14 Conventional O2 is administered using manual flowmeters, according to standard procedures. All participating units were encouraged to use the same standardised SpO2 target as in the automated O2 administration group, as recommended in international guidelines.1 2 In both arms, oxygen can be administered either using nasal prongs for low flow (O2<6 L/min) or standard face mask in all cases (O2=0–20 L/min).
Continuous oximetry recordings are performed in each group during the 3 days of the study, using the FreeO2 monitoring system connected to Nonin 6000 CA flexible adult single-use digital sensors. Position of the sensors is to be controlled at least every 12 hours. In the FreeO2 group, the FreeO2 will be used both for oxygen administration and for recording. In the Standard group, the FreeO2 will be used in the recording only and the oxygen administration will be set manually.
Standard procedures
Considering the variety of pathological cases for patients attending the recovery room, medical treatment, including the other respiratory support, is determined by the attending physicians based on clinical needs assessment. All other aspects of patient care after inclusion in the study, including fluid administration, prophylactic antibiotics and postoperative pain management, are made at clinicians’ discretion based on the expertise of the staff at each centre and routine clinical practice.
Primary outcome measure
The primary outcome measure will be the percentage of time spent in the target zone of oxygen saturation, during a 3-day time frame. In both groups (Standard and FreeO2), patients will be connected to the FreeO2 system to enable continuous oximetry recordings of one SpO2 value per second, either in the recording mode for patients assigned to the Standard group or in the automated closed-loop mode for patients assigned to the FreeO2 group.
The target zone of oxygen saturation is SpO2=88%–92% for patients with COPD and 92%–96% for patients without COPD.
Secondary outcome measures
Several secondary outcome measures will be evaluated during a 3-day time frame: nursing workload assessed by the number of manual O2 flow adjustments and airway management procedures (twice daily assessment); time spent with severe desaturation (SpO2 <85%); time spent with hyperoxia (SpO2 >98%); VO2 measured at the end of administration. All data related to oxygenation will be recorded in both groups using the FreeO2 device, enabling us to qualify desaturation using the Oxygen Desaturation Index at different levels (ODI2% and ODI4%).
Otheroutcome measures will be assessed during a maximal 28-day time frame: duration of oxygen administration during hospitalisation, number of complications related to the administration of oxygen; frequency of use of ventilation (invasive or non-invasive); duration of hospitalisation; survival rate.
Participant timeline
Figure 1 shows the participant timeline of the FreeO2 PostOp study.
Sample size
Based on previous studies and data from the literature,10 20 we estimated an 85% time within oxygenation range with the automated closed-loop oxygen administration system (FreeO2) during the 3 days following surgery and a SD equal or more than 30%. A total number of 180 patients will be needed to demonstrate a 15% decrease in absolute difference between the Standard and FreeO2 groups (90 patients in each group). The α risk is 5% and the β risk is 10% with a bilateral formulation. The expected duration of patient enrolment will be 3 years.
Methods: assignment of intervention
Allocation and sequence generation
A computer-generated randomisation is performed in the postrecovery room within a 1-hour delay after endotracheal extubation. It is performed using random blocks in a 1:1 ratio, with the use of a centralised web-based management system (Clinfile). Stratification is performed either according to the study centre and a medical history of COPD. After randomisation, treatment is to be initiated within less than 1 hour.
Blinding
Although the individual study assignments of the patients will not be masked, the coordinating centre and all the investigators will remain unaware of the study group outcomes until the data will be locked.
Methods: data collection, management and analysis
Data collection and management
At the time of enrolment, physiological characteristics, coexisting medical conditions, surgery and anaesthetics characteristics, and oxygen flow rates are recorded. In both groups, pulse oximetry, respiratory and heart rate are continuously monitored using a dedicated software enabling data extraction from the FreeO2 device. Each hour during the first 3 hours following randomisation and daily during the following 3 days, all standard clinical parameters are collected. Evolution and clinical outcomes are monitored at day 28.
Data are collected and recorded on an electronic case-report form (e-CRF) by a trained investigator or research assistant at each centre. A blank copy of the e-CRF can be printed from the e-CRF; this enables the investigator or research assistant to fill it out with the data of the included patients, which will be captured. Once data collection has been completed, the investigator or research assistant shall sign and date the copy. This document will constitute an integral part of the patient’s medical records; as such, it shall be retained permanently. Data recorded in the e-CRF that originate in source documents must be consistent with each other; if they are not, the differences have got to be justified and documented.
Statistical methods
All the analyses will be performed by the study statistician.
A predefined statistical analysis plan will be followed. The analysis will be performed on an intention-to-treat basis after validation by a blind review committee of the inclusion and exclusion criteria for each patient. All the analyses will be conducted by the biostatistics department of the Centre d’Investigation Clinique from Brest University Hospital (CIC INSERM 1412) using SAS V.9.3 statistical software (SAS Institute, Cary, North Carolina, USA). A two-tailed p value equal or less than 0.05 will be considered as statistically significant.
Descriptive analysis of patient groups at baseline
The continuous variables will be analysed using standard parameters (median, IQRs and extreme values, or mean and SD), while indicating the number of missing data. The category variables will be presented in the form of absolute frequency and percentage, in each treatment group.
The criteria of subject selection will be verified based on the data recorded in the electronic case reports. Falsely included subjects such as those lost to follow-up will be described. Deviations from the protocol will be described and analysed on a case-by-case basis.
Analysis pertaining to the main criteria of evaluation
The percentages of time within the considered SpO2 range will be compared between the two groups by means of a variance analysis, according to stratification.
Analysis pertaining to the secondary criteria of evaluation
Secondary criteria of evaluation will be compared between the two treatment groups by means of Student’s t-test (or the Mann-Whitney U test, if necessary) for continuous quantitative variables and by means of the χ2 test (or Fisher’s exact test) for qualitative variables.
Methods: monitoring
Data monitoring
Before starting patient enrolment, all physicians and other healthcare workers in the ICU attend formal training sessions on the study protocol and data collection.
An investigator at each centre is responsible for daily patient screening, enrolling patients in the study, ensuring adherence to the protocol and completing the e-CRF. Research assistants regularly monitor all the centres on site to check adherence to the protocol and the accuracy of the data recorded.
Harms
The investigator is allowed to temporarily or permanently discontinue the participation of a patient in the study for any reason that would optimally serve the interests of the subject, particularly in case of serious adverse events suspected to be associated with the type of oxygenation method that is used.
Auditing
The trial is overseen by a steering committee and an independent safety monitoring board composed of three independent experts (Jean-Pierre Frat, Christophe Guitton, Alain Mercat). All centres are monitored by the promoter to check adherence to the protocol and accuracy of recorded data. An investigator at each centre is responsible for enrolling patients and ensuring adherence to the protocol. Research assistants at each centre are responsible for patients’ follow-up and for completing the e-CRF.
Ethics and dissemination
The French national agency for drug and biomedical devices security (ANSM) approved the use of the FreeO2 device within this study on 5 August 2014. The main modification of the protocol was made after obtaining CE marking for the device (protocol version no. 3); other amendments were related to investigators’ changes and an extension of the study length (final version: no. 5). The study sponsor notified all amendments to investigators.
Consent or assent
The patient is included after having provided a written informed consent to the investigator according to the decision of the central ethics committee. If the patient is not able to understand the information given, he/she can be included if the same procedure is completed with a next of kin. After the patient’s recovery, he/she will be asked if he/she agrees to continue the trial.
Patient and public involvement
Patients and the public were not involved in the design or conduct of the study. There is no plan to disseminate the results to study participants.
Confidentiality
Data will be handled according to French law. All original records will be archived at trial sites for 15 years. The clean database file will be anonymised and kept for 15 years.
Dissemination policy
The protocol is reported according to the SPIRIT guidelines.24 Findings will be submitted to peer-reviewed journals and presented at local, national and international meetings and conferences according to CONSORT guidelines,25 to publicise and explain the research to clinicians, commissioners and service users.
Authorship eligibility guidelines will take into account participation to the protocol design and writing, final analysis of the results, patients’ recruitment and final manuscript revision.
Discussion
In postoperative patients, pulmonary function is markedly altered both by general anaesthesia, mechanical ventilation and surgery. Postoperative respiratory complications following surgery are the second most frequent complications after surgery19 and considered as a major cause of morbidity and mortality.17 26 27 The FreeO2 PostOp trial is the first clinical evaluation of automated oxygen titration in patients undergoing major abdominal or thoracic surgeries. The objectives of the study are to compare the oxygenation parameters (time in the oxygenation target, time with hypoxemia and with hyperoxia) with usual oxygen therapy and automated oxygen titration and weaning.
Risk and consequences of hypoxemia
There is a good level of evidence and good acceptation by the medical community that hypoxemia is harmful,28 especially in adult patients with myocardial ischaemia29 and neurotrauma.30 Data also suggest that even short periods of hypoxemia may promote significant negative haemodynamic effects.31 In an animal model, right ventricular dilation was observed with only 2 hours of daily hypoxemia.32
During the postoperative period, the occurrence of marked oxygen desaturation related to periodic apnoea and hypoventilation for several hours has been recognised for a long time,33 34 with potentially severe consequences such as myocardial ischaemia.35 The incidence of hypoxemia is high in the recovery room (10%–50%),20 and up to 50% of postoperative patients will demonstrate episodic hypoxemia in the absence of O2 therapy.36 37 It has also been shown that desaturation episodes are more frequent on the first night after surgery, but may also worsen 3–5 days postoperatively, especially in patients with OSA.38–40
Pathophysiology of these O2 desaturations is complex but may be due either to the patient’s condition itself (advanced age, COPD, diabetes, obesity, etc), respiratory mechanics modifications (reduction of functional residual capacity, atelectasis, thoracoabdominal compliance decrease), but also to the use of pharmaceutical agents that are given during surgery (anaesthetics and neuromuscular blocking drugs) or those that are given to relief postoperative pain (opioids and sedatives).34
Our hypothesis is that desaturations will be reduced with the automated oxygen titration (FreeO2 group), as the oxygen flow is titrated every second and that desaturations will immediately lead to increasing of oxygen flowrate. In previous studies comparing manual and automated oxygen administration, it was demonstrated that time with hypoxemia was reduced with FreeO2.10 15 However, no data are available during the postoperative care.
Automated weaning of oxygen
Oxygen supplementation has initially been promoted to decrease postoperative hypoxemia, even if it is also known that it will not have any effect on the overall number of central or obstructive apnoea, neither atelectasis.33 Not all patients will benefit from systematic O2 administration,41 but probably only specific patients with a high-risk profile, especially those following long duration and major thoracic or abdominal surgery.42–44 Moreover, standard continuous O2 therapy tends to reduce but not abolish the occurrence of desaturation,36 given the fact that only point checks are made to adjust O2 flow to actual patients’ needs.
It has also been demonstrated that the duration of O2 therapy was an independent risk factor for developing postoperative respiratory complications. Patients who require O2 for ≥75% of recovery room time (or greater than 90 min) appear to be at greater risk of developing respiratory complications.45 This fact may suggest that some patients are not adequately screened for risk factors such as OSA by standard preanaesthesia testing, and that a device dedicated to continuous monitoring of O2 administration (either alarms on duration and flow variations) may help to detect such high-risk patients. The increased resource use in patients with longer oxygen therapy requirement in the recovery room likely reflects the increase in occurrence of pulmonary respiratory complications requiring invasive and non-invasive ventilatory support, especially on the day of surgery.
In L’her et al’s study, it was shown that the partial or complete oxygen weaning was significantly increased with automated oxygen titration in comparison with standard oxygen administration, in patients managed in the emergency department during 3 hours.10
In the specific setting of postoperative patients, the reduction of the weaning time may improve the efficiency of the turnover of the patients in the recovery room.
Risk and consequences of hyperoxemia
Few studies have promoted the use of hyperoxia during and after colorectal surgery to reduce wound infection,46 but this is not recommended in routine, given controversial data.47–49 In a post hoc analysis of the PROXI trial, the authors even pointed out the potential risks of acute coronary syndromes associated with perioperative hyperoxia.50 The pathophysiological risks associated with hyperoxia are described for a long time, especially in patients with COPD.4 The first recommendation to adjust oxygen flow rates in order to reduce the risks of hyperoxia was published in the early 1960s,51 and several more recent guidelines have reiterated similar recommendations.1 2 The recent demonstration in a large randomised controlled trial (RCT) of an increased mortality for ICU patients assigned to a standard O2 therapy practice, as compared with a more conservative one (absolute risk reduction 0.086 (95% CI 0.017 to 0.150); p=0.01), has revived the debate about potential harm of excessive oxygen therapy in an unselected patients’ population.52 Adverse effects of hyperoxia could be mediated through a higher oxidative stress, but also increased coronary6 7 and cerebral artery resistances,8 all being associated with a potential clinical impact.53 54 Such potential adverse events related to hyperoxia clearly mandates attention in avoiding unnecessary O2 administration. It was demonstrated in two randomised trials from our team10 15 that time with hyperoxia could be reduced with automated oxygen titration, and the hypothesis of the present study is that this problem will also be reduced after thoracic or abdominal surgeries.
Clinical data with automated oxygen titration
Several systems have been developed to titrate oxygen flow rate in neonates and in adult patients.10 14 In a previous RCT on adult patients admitted to the ED for acute hypoxemic respiratory failure, the use of automated O2 administration was found superior to manual O2 administration to improve the time spent within oxygenation targets, with a between-group difference of 29%,10 as already observed in other studies on O2 automated administration.55 56 In L’Her et al’s study, patients experienced less time with hypoxemia and hyperoxia in the FreeO2 group.10 When receiving automated oxygen, partial or complete oxygen weaning was more frequent during initial care, as compared with standard manual O2 administration.
As automated closed-loop O2 administration is not the standard of care for postoperative patients, we did not design this study as a non-inferiority study but rather as a superiority study. One limitation of the study is that investigators are aware of the inclusion group, and blinding is difficult in studies with respiratory support. However, given the characteristics of the two strategies under evaluation, a double-blind trial was not possible. Second, the assessment of the oxygenation status could be considered as more precise by analysing blood gas sample rather than SpO2. However, this would not enable continuous oxygenation monitoring up to 3 days. Moreover, only continuous of non-averaged SpO2 values do enable precise and rapid adjustments of the O2 flow, in response to exact patients’ needs.
Noteworthy, all patients in both groups will be continuously monitored using the same oximeter, which may represent a strength of this study; therefore, the FreeO2 PostOp will also represent the largest prospective study comparing two oxygenation strategies over such a period in the postoperative setting.
In conclusion, the FreeO2 PostOp trial is a pragmatic RCT designed to test the hypothesis that automated closed-loop O2 administration is superior to standard manual O2 administration, during the postoperative care of patients with major abdominal or thoracic surgery. To the best of our knowledge, the FreeO2 PostOp trial is the first to evaluate the usefulness of automated closed-loop O2 administration after extubation in such an indication.
Supplementary Material
Footnotes
Contributors: EL’h and FL designed this study, drafted the manuscript of the protocol and critically revised the manuscript. EL’h, SJ, DV, CJ, BH, EF, TK, VP, P-AB and FL participated in the conduct of the study. MG and EN participated in the protocol methodological assessment and statistical plan. All authors read and approved the final manuscript.
Funding: This trial was funded by the French Ministry of Health obtained in 2014 from a regional hospital clinical research programme (Programme Hospitalier de Recherche Clinique Interrégional HUGO 2014).
Competing interests: EL’h reports lecture fees and travel expenses for lectures given at academic meetings from GE Healthcare, Sedana Medical, Smiths Medical, Air Liquide Medical Systems. EL’h and FL are the inventors of the FreeO2 device and founded Oxynov Inc. to develop the commercial device. The firm Oxynov Inc. provides the automated oxygen therapy equipment to all the participating centres but has no other involvement in the study.
Patient consent: Not required.
Ethics approval: The Institutional Review Board of the University Hospital of Brest, France (CPP Ouest 6-845) approved the trial for all French centres on 2 February2015 (IDRCB RB14-060). The institutional review board from the Québec Heart and Lung Institute (Canada) approved the trial for their own centre. Any protocol modification will be submitted for review and approval by the ethics committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: All investigators will have access to the final data set. Participant-level data sets will be made accessible on a controlled access basis.
References
- 1. O’Driscoll BR, Howard LS, Earis J, et al. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax 2017;72:ii1–ii90. 10.1136/thoraxjnl-2016-209729 [DOI] [PubMed] [Google Scholar]
- 2. Committee GS. Global strategy for the diagnosis, maagement, and prevention of chronic obstructive pulmonary disease. 2016. Date http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016 (last accessed 30 Mar 2018).
- 3. Abdo WF, Heunks LM. Oxygen-induced hypercapnia in COPD: myths and facts. Crit Care 2012;16:323 10.1186/cc11475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Aubier M, Murciano D, Milic-Emili J, et al. Effects of the administration of O2 on ventilation and blood gases in patients with chronic obstructive pulmonary disease during acute respiratory failure. Am Rev Respir Dis 1980;122:747–54. 10.1164/arrd.1980.122.5.747 [DOI] [PubMed] [Google Scholar]
- 5. Austin MA, Wills KE, Blizzard L, et al. Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ 2010;341:c5462 10.1136/bmj.c5462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wijesinghe M, Perrin K, Ranchord A, et al. Routine use of oxygen in the treatment of myocardial infarction: systematic review. Heart 2009;95:198–202. 10.1136/hrt.2008.148742 [DOI] [PubMed] [Google Scholar]
- 7. Farquhar H, Weatherall M, Wijesinghe M, et al. Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am Heart J 2009;158:371–7. 10.1016/j.ahj.2009.05.037 [DOI] [PubMed] [Google Scholar]
- 8. Floyd TF, Clark JM, Gelfand R, et al. Independent cerebral vasoconstrictive effects of hyperoxia and accompanying arterial hypocapnia at 1 ATA. J Appl Physiol 2003;95:2453–61. 10.1152/japplphysiol.00303.2003 [DOI] [PubMed] [Google Scholar]
- 9. Mok W, Wang W, Cooper S, et al. Attitudes towards vital signs monitoring in the detection of clinical deterioration: scale development and survey of ward nurses. Int J Qual Health Care 2015;27:207–13. 10.1093/intqhc/mzv019 [DOI] [PubMed] [Google Scholar]
- 10. L’Her E, Dias P, Gouillou M, et al. Automatic versus manual oxygen administration in the emergency department. Eur Respir J 2017;50:1602552 10.1183/13993003.02552-2016 [DOI] [PubMed] [Google Scholar]
- 11. Claure N, Gerhardt T, Everett R, et al. Closed-loop controlled inspired oxygen concentration for mechanically ventilated very low birth weight infants with frequent episodes of hypoxemia. Pediatrics 2001;107:1120–4. 10.1542/peds.107.5.1120 [DOI] [PubMed] [Google Scholar]
- 12. Claure N, Bancalari E, D’Ugard C, et al. Multicenter crossover study of automated control of inspired oxygen in ventilated preterm infants. Pediatrics 2011;127:e76–e83. 10.1542/peds.2010-0939 [DOI] [PubMed] [Google Scholar]
- 13. Hallenberger A, Poets CF, Horn W, et al. Closed-loop automatic oxygen control (CLAC) in preterm infants: a randomized controlled trial. Pediatrics 2014;133:e379–e385. 10.1542/peds.2013-1834 [DOI] [PubMed] [Google Scholar]
- 14. Lellouche F, L’her E, L’Her E. Automated oxygen flow titration to maintain constant oxygenation. Respir Care 2012;57:1254–62. 10.4187/respcare.01343 [DOI] [PubMed] [Google Scholar]
- 15. Lellouche F, Bouchard PA, Roberge M, et al. Automated oxygen titration and weaning with FreeO2 in patients with acute exacerbation of COPD: a pilot randomized trial. Int J Chron Obstruct Pulmon Dis 2016;11:1983–90. 10.2147/COPD.S112820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 2008;372:139–44. 10.1016/S0140-6736(08)60878-8 [DOI] [PubMed] [Google Scholar]
- 17. Khuri SF, Henderson WG, DePalma RG, et al. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg 2005;242:32–48. 10.1097/01.sla.0000179621.33268.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Shander A, Fleisher LA, Barie PS, et al. Clinical and economic burden of postoperative pulmonary complications: patient safety summit on definition, risk-reducing interventions, and preventive strategies. Crit Care Med 2011;39:2163–72. 10.1097/CCM.0b013e31821f0522 [DOI] [PubMed] [Google Scholar]
- 19. Arozullah AM, Daley J, Henderson WG, et al. Multifactorial risk index for predicting postoperative respiratory failure in men after major noncardiac surgery. The National Veterans Administration Surgical Quality Improvement Program. Ann Surg 2000;232:242–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lawrence VA, Dhanda R, Hilsenbeck SG, et al. Risk of pulmonary complications after elective abdominal surgery. Chest 1996;110:744–50. 10.1378/chest.110.3.744 [DOI] [PubMed] [Google Scholar]
- 21. Lindberg P, Gunnarsson L, Tokics L, et al. Atelectasis and lung function in the postoperative period. Acta Anaesthesiol Scand 1992;36:546–53. 10.1111/j.1399-6576.1992.tb03516.x [DOI] [PubMed] [Google Scholar]
- 22. International council for harmonization of technical requirements for pharmaceuticals for human use. Guidelines for good clinical practice—R2. 2016. Date http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R2__Step_4_2016_1109.pdf (last accessed 7 Aug 2018).
- 23. Mazo V, Sabaté S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology 2014;121:219–31. 10.1097/ALN.0000000000000334 [DOI] [PubMed] [Google Scholar]
- 24. Chan AW, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schulz KF, Altman DG, Moher D. CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Karcz M, Papadakos PJ. Respiratory complications in the postanesthesia care unit: a review of pathophysiological mechanisms. Can J Respir Ther 2013;49:21–9. [PMC free article] [PubMed] [Google Scholar]
- 27. Serpa Neto A, Hemmes SN, Barbas CS, et al. Incidence of mortality and morbidity related to postoperative lung injury in patients who have undergone abdominal or thoracic surgery: a systematic review and meta-analysis. Lancet Respir Med 2014;2:1007–15. 10.1016/S2213-2600(14)70228-0 [DOI] [PubMed] [Google Scholar]
- 28. Bateman NT, Leach RM. ABC of oxygen. Acute oxygen therapy. BMJ 1998;317:798–801. 10.1136/bmj.317.7161.798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Galatius-Jensen S, Hansen J, Rasmussen V, et al. Nocturnal hypoxaemia after myocardial infarction: association with nocturnal myocardial ischaemia and arrhythmias. Br Heart J 1994;72:23–30. 10.1136/hrt.72.1.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. DeWitt DS, Prough DS. Blast-induced brain injury and posttraumatic hypotension and hypoxemia. J Neurotrauma 2009;26:877–87. 10.1089/neu.2007.0439 [DOI] [PubMed] [Google Scholar]
- 31. Selinger SR, Kennedy TP, Buescher P, et al. Effects of removing oxygen from patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1987;136:85–91. 10.1164/ajrccm/136.1.85 [DOI] [PubMed] [Google Scholar]
- 32. Nattie EE, Doble EA. Threshold of intermittent hypoxia-induced right ventricular hypertrophy in the rat. Respir Physiol 1984;56:253–9. 10.1016/0034-5687(84)90109-9 [DOI] [PubMed] [Google Scholar]
- 33. Jones JG, Jordan C, Scudder C, et al. Episodic postoperative oxygen desaturation: the value of added oxygen. J R Soc Med 1985;78:1019–22. 10.1177/014107688507801208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Catley DM, Thornton C, Jordan C, et al. Pronounced, episodic oxygen desaturation in the postoperative period: its association with ventilatory pattern and analgesic regimen. Anesthesiology 1985;63:20–8. [DOI] [PubMed] [Google Scholar]
- 35. Gögenur I, Rosenberg-Adamsen S, Lie C, et al. Relationship between nocturnal hypoxaemia, tachycardia and myocardial ischaemia after major abdominal surgery. Br J Anaesth 2004;93:333–8. 10.1093/bja/aeh208 [DOI] [PubMed] [Google Scholar]
- 36. Canet J, Ricos M, Vidal F. Early postoperative arterial oxygen desaturation. Determining factors and response to oxygen therapy. Anesth Analg 1989;69:207–12. [PubMed] [Google Scholar]
- 37. Ramachandran SK, Nafiu OO, Ghaferi A, et al. Independent predictors and outcomes of unanticipated early postoperative tracheal intubation after nonemergent, noncardiac surgery. Anesthesiology 2011;115:44–53. 10.1097/ALN.0b013e31821cf6de [DOI] [PubMed] [Google Scholar]
- 38. Gögenur I, Wildschiøtz G, Rosenberg J. Circadian distribution of sleep phases after major abdominal surgery. Br J Anaesth 2008;100:45–9. 10.1093/bja/aem340 [DOI] [PubMed] [Google Scholar]
- 39. Chung F, Liao P, Elsaid H, et al. Factors associated with postoperative exacerbation of sleep-disordered breathing. Anesthesiology 2014;120:299–311. 10.1097/ALN.0000000000000041 [DOI] [PubMed] [Google Scholar]
- 40. Rosenberg J, Wildschiødtz G, Pedersen MH, et al. Late postoperative nocturnal episodic hypoxaemia and associated sleep pattern. Br J Anaesth 1994;72:145–50. 10.1093/bja/72.2.145 [DOI] [PubMed] [Google Scholar]
- 41. Gift AG, Stanik J, Karpenick J, et al. Oxygen saturation in postoperative patients at low risk for hypoxemia: is oxygen therapy needed? Anesth Analg 1995;80:368–72. [DOI] [PubMed] [Google Scholar]
- 42. Pedersen T, Viby-Mogensen J, Ringsted C. Anaesthetic practice and postoperative pulmonary complications. Acta Anaesthesiol Scand 1992;36:812–8. 10.1111/j.1399-6576.1992.tb03570.x [DOI] [PubMed] [Google Scholar]
- 43. Mathew JP, Rosenbaum SH, O’Connor T, et al. Emergency tracheal intubation in the postanesthesia care unit: physician error or patient disease? Anesth Analg 1990;71:691???697–7. 10.1213/00000539-199012000-00020 [DOI] [PubMed] [Google Scholar]
- 44. Smetana GW, Lawrence VA, Cornell JE, et al. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med 2006;144:581–95. 10.7326/0003-4819-144-8-200604180-00009 [DOI] [PubMed] [Google Scholar]
- 45. Ramachandran SK, Thompson A, Pandit JJ, et al. Retrospective observational evaluation of postoperative oxygen saturation levels and associated postoperative respiratory complications and hospital resource utilization. PLoS One 2017;12:e0175408 10.1371/journal.pone.0175408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Greif R, Akça O, Horn EP, et al. Supplemental perioperative oxygen to reduce the incidence of surgical-wound infection. N Engl J Med 2000;342:161–7. 10.1056/NEJM200001203420303 [DOI] [PubMed] [Google Scholar]
- 47. Meyhoff CS, Wetterslev J, Jorgensen LN, et al. Effect of high perioperative oxygen fraction on surgical site infection and pulmonary complications after abdominal surgery: the PROXI randomized clinical trial. JAMA 2009;302:1543–50. 10.1001/jama.2009.1452 [DOI] [PubMed] [Google Scholar]
- 48. Togioka B, Galvagno S, Sumida S, et al. The role of perioperative high inspired oxygen therapy in reducing surgical site infection: a meta-analysis. Anesth Analg 2012;114:334–42. 10.1213/ANE.0b013e31823fada8 [DOI] [PubMed] [Google Scholar]
- 49. Wetterslev J, Meyhoff CS, Jørgensen LN, et al. The effects of high perioperative inspiratory oxygen fraction for adult surgical patients. Cochrane Database Syst Rev 2015;6:CD008884 10.1002/14651858.CD008884.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Fonnes S, Gögenur I, Søndergaard ES, et al. Perioperative hyperoxia—Long-term impact on cardiovascular complications after abdominal surgery, a post hoc analysis of the PROXI trial. Int J Cardiol 2016;215:238–43. 10.1016/j.ijcard.2016.04.104 [DOI] [PubMed] [Google Scholar]
- 51. Campbell EJ. The J. Burns Amberson Lecture. The management of acute respiratory failure in chronic bronchitis and emphysema. Am Rev Respir Dis 1967;96:626–39. 10.1164/arrd.1967.96.4.626 [DOI] [PubMed] [Google Scholar]
- 52. Girardis M, Busani S, Damiani E, et al. Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit: the oxygen-ICU randomized clinical trial. JAMA 2016;316:1583–9. 10.1001/jama.2016.11993 [DOI] [PubMed] [Google Scholar]
- 53. Stub D, Smith K, Bernard S, et al. Air versus oxygen in ST-segment-elevation myocardial infarction. Circulation 2015;131:2143–50. 10.1161/CIRCULATIONAHA.114.014494 [DOI] [PubMed] [Google Scholar]
- 54. Damiani E, Adrario E, Girardis M, et al. Arterial hyperoxia and mortality in critically ill patients: a systematic review and meta-analysis. Crit Care 2014;18:711 10.1186/s13054-014-0711-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cirio S, Nava S. Pilot study of a new device to titrate oxygen flow in hypoxic patients on long-term oxygen therapy. Respir Care 2011;56:429–34. 10.4187/respcare.00983 [DOI] [PubMed] [Google Scholar]
- 56. Rice KL, Schmidt MF, Buan JS, et al. AccuO2 oximetry-driven oxygen-conserving device versus fixed-dose oxygen devices in stable COPD patients. Respir Care 2011;56:1901–5. 10.4187/respcare.01059 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.