Abstract
A 7-year-old girl presented with watering and redness in the left eye for 2 months. Her parents reported poor vision in both eyes for 4 years. Visual acuity was finger counting at 1 m and finger counting close to face in the right and left eyes, respectively. Slit lamp examination of the right eye revealed corectopia, aphakia in the pupillary area, temporally subluxated clear crystalline lens, persistent pupillary membrane, irido-hyaloidal adhesion and poorly dilating pupil. Left eye revealed central corneal oedema with descemet scarring, anteriorly dislocated clear crystalline lens with lenticulo-corneal touch. Ultrasound examination of the left eye was normal. Hence a diagnosis of ectopia lentis et pupillae with left eye spontaneous anterior dislocation of the lens along with corneal decompensation was made. The child underwent microscope integrated intraoperative optical coherence tomography guided intralenticular lens aspiration with optical iridectomy in the left eye. Postoperative visual rehabilitation was done with aphakic glasses.
Keywords: ophthalmology, Iris, anterior chamber, congenital disorders
Background
Spontaneous anterior dislocation of the lens into the anterior chamber is an ocular emergency that needs to be managed urgently. Delay in management can predispose the patient to the risk of corneal decompensation and glaucoma.1 Spontaneous anterior dislocation of the lens is associated with various ocular and systemic conditions. However, trauma essentially needs to be ruled out in every case before looking into these causes. Ocular conditions associated with anterior dislocation of the lens include microspherophakia, hypermature cataract, pseudoexfoliation syndrome and retinitis pigmentosa.2 In cases where these factors are absent, systemic conditions like Marfan syndrome, homocystinuria and Weill-Marchesani syndrome needs to be ruled out.1
Ectopia lentis et pupillae (ELP) cases have poor vision since birth. Hence, spontaneous anterior dislocation of the lens in the background of ELP can result in delayed presentation due to the inability to appreciate the diminution of vision. Thus, such cases may present when complications like corneal decompensation or secondary glaucoma develop. To the best of our knowledge, this is the first case of ELP presenting with spontaneous anterior dislocation of lens. Besides, this is the first report of such cases with the novel technique of microscope integrated intraoperative optical coherence tomography (MIOCT) guided intralenticular lens aspiration (ILLA).
Case presentation
A 7-year-old girl presented with watering and redness in the left eye for 2 months. Her parents reported that the child had poor vision in both eyes for 4 years. However, no medical advice was taken for the same. There was no family history of similar symptoms. The child was born out of non-consanguineous marriage. The visual acuity at presentation was finger counting at 1 m and finger counting close to face in the right and left eye, respectively. The intraocular pressure was 16 and 20 mm Hg in the right and left eye, respectively. On slit lamp examination, the right eye showed corectopia with an inferonasally displaced pupil, aphakia in the pupillary area with only the nasal edge of lens visible, persistent pupillary membrane, irido-hyaloidal adhesion and poorly dilating pupil (figure 1A,B). The left eye had central corneal oedema with descemet scarring, clear crystalline lens dislocated in anterior chamber with lenticulo-corneal touch (figure 2A,B). Pupil details were hazily seen and appeared to be inferonasally displaced. On torch light examination of the right eye in left lateral decubitus position, the lens was noted to be mobile and was observed to completely cover the pupillary area. Fundus examination of the right eye revealed normal findings.
Figure 1.
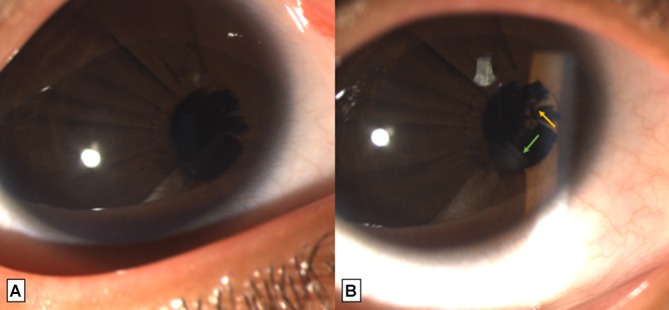
Slit lamp image of right eye (A) in diffuse illumination showing inferonasally displaced pupil (corectopia), aphakia and persistent pupillary membrane (B) in focal slit illumination showing the nasal edge of lens (green arrow) and irido-hyaloidal adhesion (yellow arrow).
Figure 2.
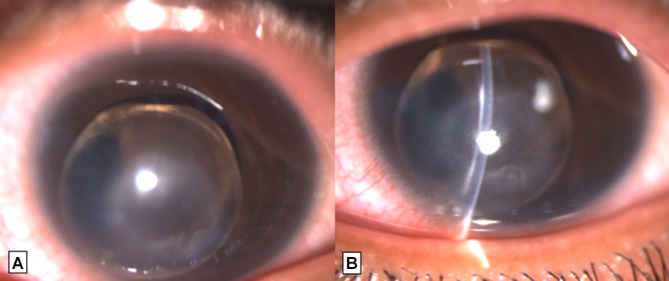
Slit lamp image of left eye (A) in diffuse illumination showing a clear crystalline lens in anterior chamber (B) in focal slit illumination showing corneal oedema, descemet scar and lenticulo-corneal touch.
Investigations
An ultrasound B scan of the left eye for posterior segment assessment showed normal findings. The axial length was 20.56 mm and 22 mm in the right and left eye, respectively. The keratometry could be captured only in the right eye and was 43.25 D at 5˚ and 45 D at 95˚. A complete systemic evaluation was done by a pediatrician, and no systemic abnormality was noted.
Differential diagnosis
Spontaneous anterior dislocation of the lens in a child can be associated with systemic conditions like Marfan syndrome, Weill-Marchesani syndrome, and homocystinuria. All of these conditions are associated with some systemic abnormalities. However, in our case, the absence of any systemic association and the typical clinical picture of corectopia with ectopia lentis in the other eye helped us arrive at the diagnosis of ELP with left eye spontaneous anterior dislocation of lens.
Treatment
The patient was started on topical hypertonic saline 5% four times a day, hypertonic saline 6% (ointment) three times a day, prednisolone acetate 1% four times a day, timolol maleate 0.5% two times a day, moxifloxacin hydrochloride 0.5% two times a day, carboxy-methyl cellulose six times a day and planned for surgical removal of the lens in the left eye without any delay. The patient underwent MIOCT guided ILLA in the left eye under general anaesthesia. The corneal thickness was noted to be 720 µm on MIOCT with lenticulo-corneal touch. Microvitreoretinal blade assisted two limbal entries were made at 10 and 2 o’clock positions, and the blade was further advanced into the lens to create two stab entries in the lens capsule near its equator. A viscodispersive ophthalmic viscoelastic device was injected to create separation between the corneal endothelium and anterior capsule of the lens. However, the lens capsule was noted to be adherent to the corneal endothelium on iOCT (figure 3). Bimanual irrigation aspiration of the lens matter was performed in the bag. The capsule was peeled with the help of intravitreal forceps to separate it from the corneal endothelium followed by its removal with vitrectomy cutter. Limited anterior vitrectomy and peripheral iridotomy was done. In view of the central corneal scar, optical iridectomy was performed with vitrectomy cutter. The anterior chamber was formed with air and balanced salt solution. The limbal wound was closed with 10–0 monofilament suture. Postoperatively, the patient was continued on same treatment as advised in the preoperative period along with topical homatropine 2% four times a day.
Figure 3.
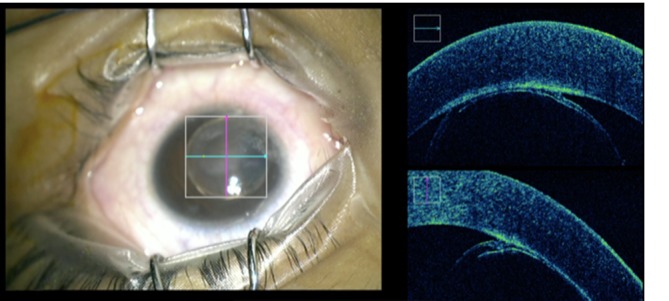
Intraoperative MIOCT image showing lenticulo-corneal touch with hyper-reflective descemet at the site of adhesion. MIOCT, microscope integrated optical coherence tomography.
Outcome and follow-up
Postoperatively, the visual acuity was noted to be finger counting at 1 m. Mild corneal oedema with central disc-shaped descemet scar was present (figure 4A,B). Aphakic glasses were prescribed for both eyes after 2 weeks, and best corrected visual acuity of finger counting at 3 m was noted with aphakic glasses.
Figure 4.
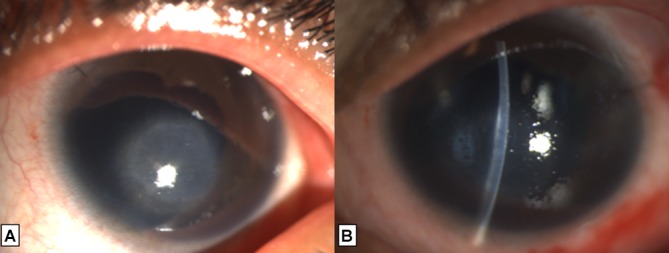
Slit lamp image of left eye on postoperative day 1 (A) in diffuse illumination showing a central disc-shaped corneal scar with nasal iris defect (B) in focal slit illumination showing corneal oedema with descemet scar.
Discussion
ELP is a congenital anomaly inherited in an autosomal recessive pattern.3 It is classically characterised by the presence of an ectopic pupil (corectopia), lens subluxation in a direction opposite to the pupil, persistent pupillary membrane, poorly dilating pupil and transillumination defects of the iris.4 The other associations are cataract, glaucoma, uveitis, myopia, irido-hyaloidal adhesion, megalocornea and retinal detachment.4
The pathogenesis of this condition is unknown and is hypothesised to be due to neuroectodermal abnormality. Goldberg reported the largest case series of 16 patients with ELP. In this study, the typical findings observed were ectopia lentis (93%), persistent pupillary membrane (87%), iridodonesis (85%), iris transillumination (66%), poor pupillary dilation (60%) and ectopia pupillae (59%).3 None of the cases had an anterior dislocation of lens.
Our patient had an ectopic pupil, ectopia lentis, poorly dilating pupil, irido-hyaloidal adhesion and a persistent pupillary membrane that suggested a diagnosis of ELP. In addition, the patient had an anteriorly dislocated lens in the left eye. Progressive zonular abnormality with an increase in the amount of subluxation has been well reported in the literature.5 This increasing zonular abnormality may explain the anterior dislocation of the lens in extreme condition.
The management of anteriorly dislocated lens reported in the literature includes intracapsular cataract extraction, lensectomy, phacoemulsification in the bag and in the bag bimanual irrigation and aspiration. In our case, ILLA was performed for surgical removal of the lens from the anterior chamber. There are various advantages of this procedure over the previously described techniques.6First, there is a small surgical wound; therefore the risk of postoperative astigmatism is less. The chance of lens matter drop is negligible as the whole procedure is performed inside the capsular bag. Also, the risk of posterior segment complications is less as there is no vitreous traction during this procedure.
Microscope integrated optical coherence tomography (MIOCT) has been reported to be of great help in various anterior segment surgeries.7 In our case, MIOCT showed an adherent anterior lens capsule to the corneal endothelium. As a result, the capsule was first peeled from the endothelium rather than using a vitrectomy cutter from the beginning itself. This is especially useful in the presence of corneal oedema where adherence of the lens capsule to the corneal endothelium can be missed, and the use of cutter may damage the corneal endothelium.
However, we would like to emphasise here that a good quality microscope along with caution on the surgeon’s part can avoid inadvertent corneal endothelial trauma and MIOCT is not an absolute necessity in these cases. But, when available it is an handy tool especially in cases where the visibility is poor.
To conclude, ELP may be associated with spontaneous anterior dislocation of the lens and surgical removal of the anteriorly dislocated lens is the treatment of choice to avoid long-term complications. Intralenticular lens aspiration can be safely performed in these cases, and MIOCT (if available) can aid in the intraoperative assessment of the lenticulo-corneal adhesion to avoid further damage to the corneal endothelium.
Learning points.
Spontaneous anterior dislocation of the lens can occur in cases of ectopia lentis et pupillae.
Intralenticular lens aspiration can be performed for removal of an anteriorly dislocated lens.
Microscope integrated optical coherence tomography can be a useful guide for the surgical management of these cases to avoid further damage to the already compromised descemet endothelium complex.
Footnotes
Contributors: PS has contributed to the concept and design, manuscript preparation and image collection. KRS has contributed in data collection and manuscript editing. PKM has contributed to the idea and manuscript editing. JST has contributed to the manuscript editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Vasavada AR, Praveen MR, Desai C. Management of bilateral anterior dislocation of a lens in a child with Marfan’s syndrome. J Cataract Refract Surg 2003;29:609–13. 10.1016/S0886-3350(02)01529-8 [DOI] [PubMed] [Google Scholar]
- 2. Lezrek O, Boutimzine N, Daoudi C, et al. [Anterior dislocation of a hypermature cataract]. J Fr Ophtalmol 2016;39:332 10.1016/j.jfo.2015.09.013 [DOI] [PubMed] [Google Scholar]
- 3. Goldberg MF. Clinical manifestations of ectopia lentis et pupillae in 16 patients. Ophthalmology 1988;95:1080–7. 10.1016/S0161-6420(88)33043-5 [DOI] [PubMed] [Google Scholar]
- 4. Cruysberg JR, Pinckers A. Ectopia lentis et pupillae syndrome in three generations. Br J Ophthalmol 1995;79:135–8. 10.1136/bjo.79.2.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Colley A, Lloyd IC, Ridgway A, et al. Ectopia lentis et pupillae: the genetic aspects and differential diagnosis. J Med Genet 1991;28:791–4. 10.1136/jmg.28.11.791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sinha R, Sharma N, Vajpayee RB. Intralenticular bimanual irrigation: aspiration for subluxated lens in Marfan’s syndrome. J Cataract Refract Surg 2005;31:1283–6. 10.1016/j.jcrs.2004.11.043 [DOI] [PubMed] [Google Scholar]
- 7. Ehlers JP, Goshe J, Dupps WJ, et al. Determination of feasibility and utility of microscope-integrated optical coherence tomography during ophthalmic surgery: the DISCOVER Study RESCAN Results. JAMA Ophthalmol 2015;133:1124–32. 10.1001/jamaophthalmol.2015.2376 [DOI] [PMC free article] [PubMed] [Google Scholar]


