Abstract
Giant abdominal cyst can lead to various non-specific symptoms such as abdominal bloating, nausea/vomiting, constipation due to its mass effect. In rarer circumstances, it can lead to bowel obstruction, hydronephrosis and even abdominal compartment syndrome. Hereby, we present a case of giant abdominal cyst in a young woman where its origin was a diagnostic dilemma despite exhausting all imaging techniques. A laparotomy was performed and the giant cyst was found to be originating from the left ovary. The final histopathology confirmed it as an ovarian benign serous cystadenoma. The patient made a fully recovery without any complications.
Keywords: surgery, obstetrics and gynaecology, general surgery
Background
Giant abdominal cyst has become increasingly rare in the past few decades due to improved imaging techniques that lead to early detection. Often, the patients are asymptomatic initially until its size is large enough to cause mass effect on surrounding organs. The cyst can originate from a few locations and its origin may pose a challenge to be identified preoperatively. Herein, we present the management of a case of giant abdominal cyst with uncertain origin pre-operatively despite various investigations. The diagnostic dilemmas and management strategies of abdominal cyst are also reviewed and discussed here.
Case presentation
A 21-year-old nulliparous woman first presented to her general practitioner with 6-month history of increasing abdominal distention causing her difficulty in tying her shoelaces. She denied any change in bowel habit, weight loss or loss of appetite. Her menstrual cycle was normal with no per vaginal bleeding or discharge. She has no medical and surgical history. There was no family history of malignancy. Her general practitioner organised an abdominal and pelvic ultrasound scan (USS) which showed a cystic mass measuring 24×23×14 cm occupying most of her abdomen. CT of abdomen/pelvis was organised to further characterise the lesion (figure 1). The CT scan demonstrated the possibility of arising from the left ovary.
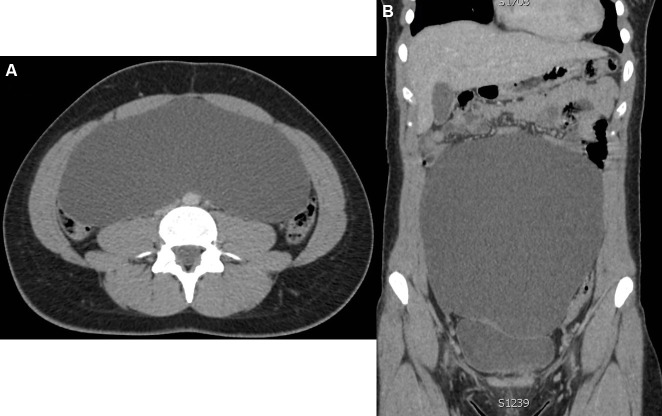
Figure 1.
(A) and (B) CT abdomen/pelvis showing the thin-walled cystic mass arising from the pelvis occupying most of the abdominal cavity.
She was seen by the gynaecologist who organised an MRI of the pelvis. Interestingly, the MRI pelvis did not depict the cyst to be arising from the ovaries (figure 2A). She was then referred to the general surgical clinic for further assessment. On clinical examination, her abdomen was distended but soft. The upper border of the cystic lesion was palpable at the epigastric region and non-tender.
Figure 2.
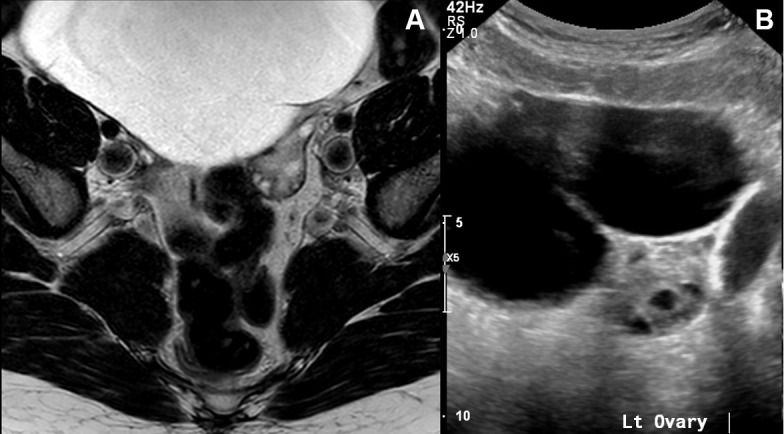
(A) MRI pelvis demonstrating the cystic mass as independent structures from both ovaries. (B) Ultrasound pelvis showing the cystic lesion to be separated from the left multifollicular ovary.
Investigations
Tumour markers including carcinoembryonic antigen, CA-19.9, CA-125 and chromogranin were all negative. A repeat pelvic USS was also inconclusive (figure 2B).
Treatment
The various imaging scans were discussed with the radiologist and the origin of the cyst could not be determined. Although the cyst appeared uncomplicated on imaging, we were in favour of a laparotomy than laparoscopy given the potential of rupturing the cyst and causing spillage of malignant cells intraperitoneally.
Intraoperatively, a midline laparotomy was performed (figure 3A). The cystic lesion was easily exteriorised and was found to be originating from the left ovary (figure 3A–C). The cyst was removed at its base with LigaSure Impact (Medtronic, USA).
Figure 3.

(A) Midline laparotomy showing the giant cystic mass. (B) The giant cystic mass originated from the left ovary (arrow). (C) This intraoperative picture depicts the cystic mass transluminate. (D) The excised ovarian cystic mass.
Outcome and follow-up
She made an uneventful recovery and was discharged home on day 3. Histopathology confirmed the cyst as benign serous cystadenoma, measuring up to 21 cm in length and weighing approximately 4 kg.
Discussion
Giant abdominal cystic masses are rare occurrence and require resection due to its associated symptoms and complications associated with mass effect.1 Apart from the non-specific abdominal distention/bloating, pain, nausea and vomiting and altered bowel habit, patients can present with rare complications such as bowel obstruction, hydronephrosis, torsion and abdominal compartment syndrome.1–5 Occasionally, rupture of the cyst can occur which can lead to haemorrhage and shock as an immediate sequelae. The ruptured contents can lead to the development of dense adhesions as a result of granulomatous reaction.
The origin of these giant cystic masses can be confusing and difficult to determine. Differential diagnoses include pelvic endometriosis, intra-abdominal cysts from varying origins (omentum, kidney, liver, pancreas, cystic lymphagiomas, choledochal cyst), accentuated obesity and ovarian cysts.1 2 For ovarian cysts, they are generally seen in women of the weight-bearing age (20–35 years).
Various radiological imaging modalities including USS, CT and MRI have been reported to be useful in identifying the origin and further characterisation of the lesion for preoperative planning.1 Nonetheless, the results were conflicting in our case. Aspiration of the abdominal cystic lesion preoperatively or intraoperatively should be avoided as it can lead to complications such as bleeding, infections and spillage of malignant cells.2 Of the cases of giant ovarian cysts, malignancy constitutes 10% of them.2 Tumour markers are usually non-specific and do not change management strategies.4
The recommendation for giant cysts is for resection/excision of the cyst due to their compressive symptoms and risk of malignancy. Exploratory laparotomy is the preferred management strategy with excision of the cystic mass.2 The patient will need to be counselled preoperatively regarding potential organ involvement and resection.5 Recently, there has been a few cases in the literature reporting the safety and efficacy of laparoscopic-assisted excision of these giant cystic masses.6 7 In these cases, the giant cystic masses were all decompressed with a minilaparotomy prior to excision of the cystic wall laparoscopically. Other options for decompression include USS-guided drainage and laparoscopic-guided aspiration. There is still no consensus of the size limit of the cyst to be safely managed laparoscopically. In our case, we opted not to decompress the cystic lesion as we did not know its exact origin.
Learning points.
Giant abdominal cyst is an infrequent occurrence with wide differential diagnoses. Imaging modality may not identify its origin.
Exploratory laparotomy for complete excision of the cystic mass is favoured.
In women, pelvic-abdominal cysts often originate from the ovary. Therefore, these women should first be evaluated by a gynaecologist.
Footnotes
Contributors: ZQN designed the study, collected and analysed the data, drafted the article and approved the final version of the article to be published. SP and RW analysed the data, revised the article and approved the final version of the article to be published. RW codesigned the study, analysed the data, critically reviewed the article, supervised the study and approved the final version of the article to be published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Bolukbas FF, Bolukbas C, Furuncuoglu Y, et al. Large abdominal cystic masses: Report of seven cases. J Pak Med Assoc 2016;66:226–8. [PubMed] [Google Scholar]
- 2. Yeika EV, Efie DT, Tolefac PN, et al. Giant ovarian cyst masquerading as a massive ascites: a case report. BMC Res Notes 2017;10:749 10.1186/s13104-017-3093-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Magalhães-Costa P, Matos L, Chagas C. A giant intra-abdominal cyst. BMJ Case Rep 2015;2015:bcr2014208020 10.1136/bcr-2014-208020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim HY, Cho MK, Bae EH, et al. Hydronephrosis caused by a giant ovarian cyst. Int Braz J Urol 2016;42:848–9. 10.1590/S1677-5538.IBJU.2015.0354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim TJ, Yeh YT, Zobair K. Impending abdominal compartment syndrome from a giant ovarian cyst torsion. ANZ J Surg 2017. 10.1111/ans.14147 [DOI] [PubMed] [Google Scholar]
- 6. Macciò A, Madeddu C, Kotsonis P, et al. Successful laparoscopic management of a giant ovarian cyst. J Obstet Gynaecol 2014;34:651–2. 10.3109/01443615.2014.902432 [DOI] [PubMed] [Google Scholar]
- 7. Uyanikoglu H, Dusak A. A huge ovarian dermoid cyst: Successful laparoscopic total excision. J Clin Diagn Res 2017;11:QD03–QD5. 10.7860/JCDR/2017/29262.10436 [DOI] [PMC free article] [PubMed] [Google Scholar]