Abstract
Introduction:
Blood transfusion practices affect both patient’s outcomes and utilization of institutional resources. Evidence shows that liberal blood transfusion has a detrimental effect on patient’s outcome. A restrictive approach of blood transfusion is recommended by current clinical guidelines.
Aim:
The aim of this study was to evaluate the attitudes, knowledge, and practices of general surgery (GS) staff and residents regarding peri-operative blood transfusion and anemia management.
Material and Methods:
A self-administered, web-based questionnaire was developed, and its link was sent to the emails of all general surgeons at King Abdul-Aziz University Hospital (KAUH), Jeddah city, Saudi Arabia. The questionnaire included four parts: 1) background of surgeons; 2) preoperative assessment and management of anemia; 3) post-operative blood transfusion and alternatives; and 4) enablers and barriers.
Results:
56 surgeons responded to the questionnaire. We found variations in blood transfusion practices, notably the hemoglobin threshold. For stable non-cardiac cases, 7 g/dL was considered the threshold by 50% of respondents. For stable patients with past cardiac disease, a higher threshold was chosen by most (9 g/dL by 43% and 10 gm/dL by 21%). Most respondents believed that transfusion had no effect on the risk of survival (73%) and on the risk of cancer recurrence (55%) after oncologic surgical resection. Recognized facilitators were the availability of scientific evidence (84%), medicolegal concerns (57%), preference (52%), and institutional protocols (50%).
Conclusion:
Although current clinical guidelines recommend a restrictive transfusion practice, most respondents tended to over-order blood for elective procedures and were not aware of the potential complications of liberal blood transfusion. To implement the restrictive transfusion policies, health institutions should improve the awareness of surgeons and incorporate a strong supporting evidence in formulating local institutional guidelines.
Keywords: blood transfusion, survey, surgeon, Saudi Arabia
1. INTRODUCTION
Approximately 20% of transfused blood is received by patients undergoing surgery. Blood transfusions is given in order to maintain hemodynamic stability and to provide adequate oxygen delivery; resulting in a reduced risk of cardiac events, bleeding, and anemia in the post-operative period (1, 2). Despite these anticipated benefits, an increasing number of studies have suggested that blood transfusions are associated with increased risks of infectious complications, cancer recurrence after oncologic resection, and mortality through transfusion-related immunomodulation. The increased risk of postoperative bacterial infection is dose-related with relative risk of 3.6 for greater than 3 units transfused (3, 4).
Research work (5, 6) have pointed out that the preoperative request of blood units, especially in elective surgery, is often based on the worst case assumptions, demanding large quantities of blood or overestimating the anticipated blood loss, of which little is ultimately used (7). This practice causes exhaustion of technician time, effort, and biochemical reagents, as well as adding to the financial burden of the patients (6).
Published blood transfusion guidelines recommend more restrictive transfusion indicators (with a hemoglobin threshold between 7 and 8 g/dL for most patients); in order to prevent overuse of blood units and to minimize unnecessary or non-indicated transfusions of blood components to surgical patients (8, 9). This restrictive transfusion strategy has lowered the risk of complications in certain surgical patients, including orthopedic and trauma patients, compared to a liberal blood transfusion strategy (10-12).
Up to the best of the authors’ knowledge, blood transfusion practices in Saudi hospitals have not been thoroughly investigated before.
2. AIM
Therefore, the aim of this study was to evaluate the attitude, knowledge, and practice of general surgery staff and residents regarding perioperative blood transfusion and management of anemia.
3. MATERIAL AND METHODS
This study was approved by the Institutional Review Board of King Abdul-Aziz University Hospital (KAUH). We conducted a web-based self-administered cross-sectional survey of general surgery consultants, specialists, and residents who are involved in the care of elective surgery patients. Our sample included all consultants, specialists, and residents in General Surgery Department at KAUH, Jeddah, Saudi Arabia.
The questionnaire was developed by authors after adopting and modifying a validated and standardized questionnaire (6). The questionnaire included 4 parts. The first part focused on the level of education and the level of experience, whereas the second part evaluated the pre-operative assessment and management of anemia. The third part assessed the post-operative RBC transfusion and alternative methods of RBC transfusion based on a scenario of a 55-year-old male who underwent a total gastrectomy, was not bleeding, and was hemodynamically stable. We modified the scenario by changing different key elements potentially associated with the need for the RBC transfusion (no symptoms of anemia, symptoms of anemia, intraoperative blood loss, suspected post-operative blood loss, and cardiac comorbidity), for a total of five modifications of the baseline scenario. The fourth part was to know the enablers and barriers for the use of a restrictive transfusion strategy.
The questionnaire was filled online by the participants themselves via secure web link that was sent by emails. A reminding email was sent two days later to increase the response rate. In compliance with the American Association of Public Opinion Research, surveys were considered completed when more than 80 % of questions were answered (13). The data was kept confidential and was available for the authors only. We used Statistical Package for the Social Sciences (SPSS), version 22 for data entry and analysis.
4. RESULTS
In the present study, 56 out of 75 surgeons responded to the questionnaire. Table 1 summarizes the characteristics of the respondents. The highest frequency of respondents were residents (28.6% in years 1 to 3 and 16.1% in year 4 or above); while specialists accounted for about one fifth and consultants for about one third. More than half the respondents (58.9%) were general surgeons with no sub-specialty training. About one third practiced surgery for one to five years after their board certification. Most respondents were used to take care of more than six patients undergoing elective surgery every month. Only 28.6% of respondents were aware that their institution has a blood conservation program; while the majority were either not aware (42.9%) or denied this (28.6%). More than half the respondents (58.9%) stated that anesthetics and pre-admission clinics hold the responsibility of assessing and managing pre-operative anemia; while surgeons were held responsible by about one third.
Table 1. Characteristics of participants and their institutions with regard of blood transfusion.
| n | % | ||
|---|---|---|---|
| Your current position is: | Resident (R1–R3) | 16 | 28.6% |
| Resident (R4 or above) | 9 | 16.1% | |
| Specialist | 12 | 21.4% | |
| Consultant | 19 | 33.9% | |
| Do you have a sub-specialty? | No. | 33 | 58.9% |
| Yes. | 23 | 41.1% | |
| How many years have you been practicing following your board certification? | Not applicable | 21 | 37.5% |
| 1–5 | 19 | 33.9% | |
| 6–10 | 9 | 16.1% | |
| > 10 | 7 | 12.5% | |
| On an average active month, how many patients undergoing an elective surgery did you take care of? | 1–5 | 8 | 14.3% |
| 6–10 | 23 | 41.1% | |
| > 10 | 25 | 44.6% | |
| Does your institution have a preoperative blood conservation program? | I don't know. | 24 | 42.9% |
| No. | 16 | 28.6% | |
| Yes. | 16 | 28.6% | |
| At your institution, who is responsible of assessing and managing pre-operative anemia? | Anesthesia + surgeons | 1 | 1.8% |
| Anesthetics/Pre-admission clinics. | 33 | 58.9% | |
| Hematology. | 3 | 5.4% | |
| Surgeons. | 19 | 33.9% | |
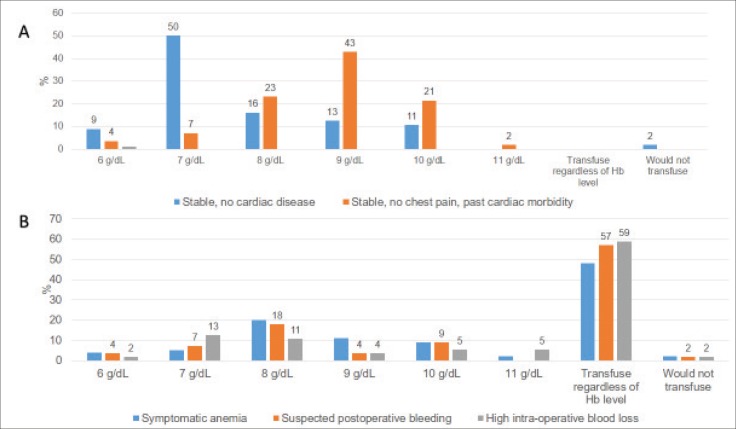
Table 2 and Figures 1 and 2 demonstrate the respondents’ pre-operative assessment of anemic cases. Situations for which respondents stated that they are likely/very likely to conduct anemia workup included: patients with documented or suspected bleeding (91%), gastric resection (66%), hepato-bilio-pancreatic resection (64%), colorectal resection (59%), and extended surgery (59%). Most respondents were unlikely/very unlikely to conduct anemia work up in patients with hemoglobin below 13 g/dL (76.8%), laparoscopic approach (71.4%), abdominal wall reconstruction (67.9%), and breast surgery (64.3%). As regards the likelihood of ordering investigations in a patient who will undergo total gastrectomy with hemoglobin level of 10.5 g/dL, all respondents stated that blood group and screening will be ordered, 86% would order cross match of RBCs units, and 46% would order oral iron supplementation.
Table 2. Likelihood (as indicated by the participants) of conducting/ordering some investigations in pre-operative assessment.
| Clinical situation | Likelihood | n | % |
|---|---|---|---|
| Conducting an anemia work-up in different clinical situations | |||
| Anemia (Hb <13g/dL): | Unlikely/Very Unlikely to conduct | 43 | 76.8% |
| Likely/Very likely to conduct | 13 | 23.2% | |
| Documented or suspected bleeding disorder: | Unlikely/Very Unlikely to conduct | 5 | 8.9% |
| Likely/Very likely to conduct | 51 | 91.1% | |
| Colo-rectal resection: | Unlikely/Very Unlikely to conduct | 23 | 41.1% |
| Likely/Very likely to conduct | 33 | 58.9% | |
| Gastric resection: | Unlikely/Very Unlikely to conduct | 19 | 33.9% |
| Likely/Very likely to conduct | 37 | 66.1% | |
| Hepato-bilio-pancreatic resection: | Unlikely/Very Unlikely to conduct | 20 | 35.7% |
| Likely/Very likely to conduct | 36 | 64.3% | |
| Abdominal wall reconstruction: | Unlikely/Very Unlikely to conduct | 38 | 67.9% |
| Likely/Very likely to conduct | 18 | 32.1% | |
| Endocrine Surgery: | Unlikely/Very Unlikely to conduct | 28 | 50.0% |
| Likely/Very likely to conduct | 28 | 50.0% | |
| Breast Surgery: | Unlikely/Very Unlikely to conduct | 36 | 64.3% |
| Likely/Very likely to conduct | 20 | 35.7% | |
| Extent of surgery–Major Vs. Minor: | Unlikely/Very Unlikely to conduct | 23 | 41.1% |
| Likely/Very likely to conduct | 33 | 58.9% | |
| Laparoscopic approaches: | Unlikely/Very Unlikely to conduct | 40 | 71.4% |
| Likely/Very likely to conduct | 16 | 28.6% | |
| Patient had surgery before not less than 3 weeks ago: | Unlikely/Very Unlikely to conduct | 33 | 58.9% |
| Likely/Very likely to conduct | 23 | 41.1% | |
| Ordering some investigations in a pre-operative period of 4 weeks for a 55-year-old man, with no significant co-morbidity who will undergo total gastrectomy with Hb level of 10.5 g/dL | |||
| Referral to hematology clinics: | Unlikely/Very Unlikely to order | 47 | 83.9% |
| Likely/Very likely to order | 9 | 16.1% | |
| Group and screen | Unlikely/Very Unlikely to order | 0 | 0.0% |
| Likely/Very likely to order | 56 | 100.0% | |
| Cross-match RBCs units | Unlikely/Very Unlikely to order | 8 | 14.3% |
| Likely/Very likely to order | 48 | 85.7% | |
| RBCs transfusion before surgery | Unlikely/Very Unlikely to order | 52 | 92.9% |
| Likely/Very likely to order | 4 | 7.1% | |
| Oral iron supplementation | Unlikely/Very Unlikely to order | 30 | 53.6% |
| Likely/Very likely to order | 26 | 46.4% | |
Figure 1. Likelihood (as indicated by the participants) of conducting an anemia work-up in different clinical situations.
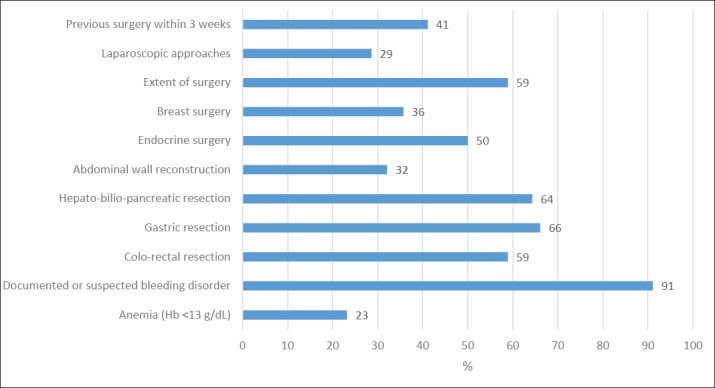
Figure 2. Likelihood (as indicated by the participants) of ordering some investigations in a pre-operative period of 4 weeks for a 55-year-old man, with no significant co-morbidity who will undergo total gastrectomy with Hb level of 10.5 g/dL.
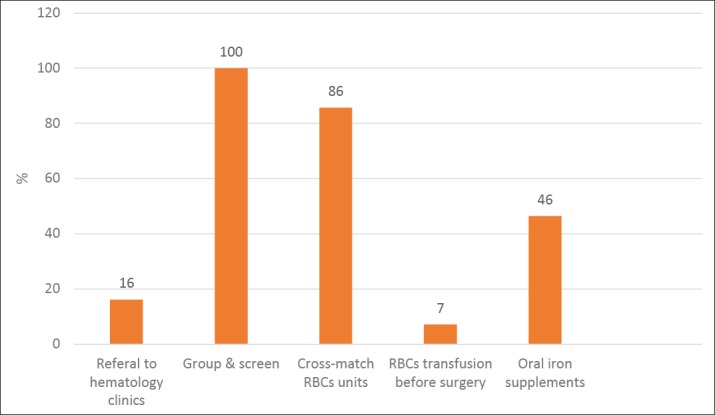
Table 3 and Figures 3 and 4 show the respondents practices in post-operative period. In a response to a case scenario of a patient who underwent elective surgery, and had active intraoperative bleeding that was stopped, with postoperatively Hb level = 6.4 g/dL and was hemodynamically stable, 89% of surgeons stated that they would often/always order two units of RBCs, while 70% would write the infusion rate. The rate of using RBC alternatives was generally low. The most frequently used alternatives to RBCs transfusion were pre-operative oral iron (30%), pre-operative autologous blood transfusion (16%), cell saver device for benign or malignant cases (9% each), and tranexamic acid (4% only).
Table 3. Post-operative RBCs transfusion and use of RBCs alternatives.
| Never | Rarely | Often | Always | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Management of a 55-year-old male who underwent elective surgery and had active intraoperative bleeding that was stopped. Postoperatively Hb level = 6.4 g/dL and was hemodynamically stable | ||||||||
| I order 1 unit if RBCs transfusion: | 2 | 3.6% | 18 | 32.1% | 25 | 44.6% | 11 | 19.6% |
| I order 2 units if RBCs transfusion | 1 | 1.8% | 5 | 8.9% | 16 | 28.6% | 34 | 60.7% |
| I write the infusion rate for the RBC transfusion: | 7 | 12.5% | 10 | 17.9% | 24 | 42.9% | 15 | 26.8% |
| Use of alternative strategies to RBCs transfusion A 55-year-old male, undergoing elective total gastrectomy with a Hb level of 10.5 g\dL | ||||||||
| Cell-saver device for benign case | 38 | 67.9% | 13 | 23.2% | 4 | 7.1% | 1 | 1.8% |
| Cell-saver for malignant case | 42 | 75.0% | 9 | 16.1% | 4 | 7.1% | 1 | 1.8% |
| Tranexamic acid | 31 | 55.4% | 23 | 41.1% | 2 | 3.6% | 0 | 0.0% |
| Pre-operative oral iron for anemic patients | 18 | 32.1% | 21 | 37.5% | 11 | 19.6% | 6 | 10.7% |
| Pre-operative autologous blood transfusions | 33 | 58.9% | 14 | 25.0% | 8 | 14.3% | 1 | 1.8% |
Figure 3. Management of a 55-year-old male who underwent elective surgery, and had active intraoperative bleeding that was stopped. Postoperatively Hb level = 6.4 g/dL and was hemodynamically stable.
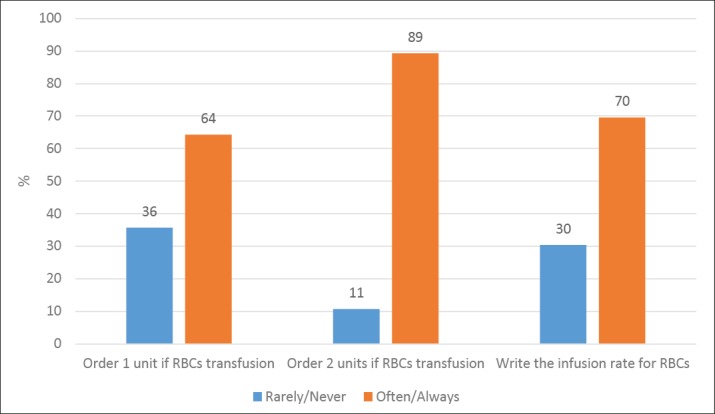
Figure 5 (A and B) illustrate the hemoglobin thresholds (as reported by the participants) for red blood cell transfusion for five clinical scenarios. For stable non-cardiac cases, 7 g/dL was considered the threshold by 50% of respondents. For stable patients with past cardiac disease, a higher threshold was chosen by most doctors (9 g/dL by 43% and 10 gm/dL by 21%). Transfusion regardless of the hemoglobin level was indicated in symptomatic anemia by 45%; in suspected postoperative bleeding by 57%; and in high intraoperative bleeding by 59%.
Figure 5. Hemoglobin thresholds (as reported by the participants) for red blood cell transfusion for five clinical scenarios.
Table 4 and Figure 6 summarize the participants’ opinions about how RBCs transfusions increase or decrease the risk of patients’ outcomes. Half the respondents stated that it will increase post-operative morbidity. As regards post-operative mortality, the respondents’ views were more split as 39% stated that it will decrease the risk while the remainder were divided equally to increased risk or no effect. Most respondents believed that transfusion had no effect on the risk of survival (73%) and on the risk of cancer recurrence (55%) after oncologic surgical resection.
Table 4. The participants’ opinions about how RBCs transfusions increase or decrease the risk of patients’ outcomes.
| n | % | ||
|---|---|---|---|
| Post-operative morbidity | Decrease/Strongly decrease | 21 | 37.5% |
| Increase/Strongly increase | 28 | 50.0% | |
| Neither increase nor decrease | 7 | 12.5% | |
| Post-operative mortality | Decrease/Strongly decrease | 22 | 39.3% |
| Increase/Strongly increase | 17 | 30.4% | |
| Neither increase nor decrease | 17 | 30.4% | |
| Cancer recurrence after oncologic surgical resection | Decrease/Strongly decrease | 0 | 0.0% |
| Increase/Strongly increase | 25 | 44.6% | |
| Neither increase nor decrease | 31 | 55.4% | |
| Survival after oncologic surgical resection | Decrease/Strongly decrease | 5 | 8.9% |
| Increase/Strongly increase | 10 | 17.9% | |
| Neither increase nor decrease | 41 | 73.2% | |
Figure 6. The participants’ opinions about how RBCs transfusions increase or decrease the risk of patients’ outcomes.
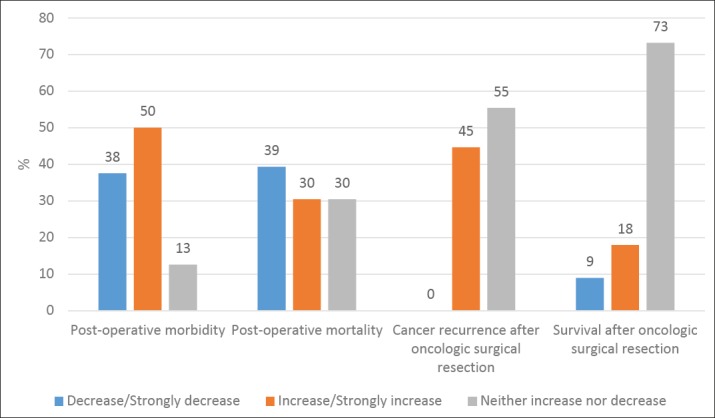
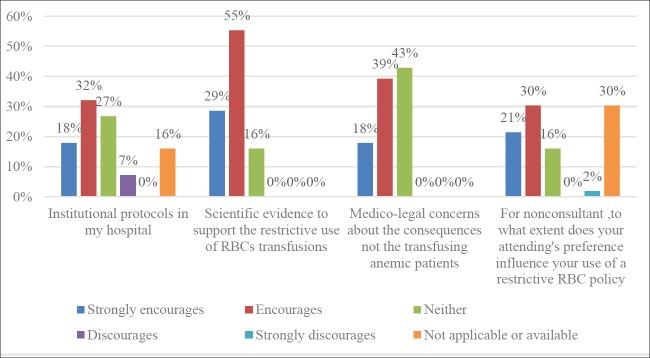
Table 5 and Figure 7 reveal the respondents’ opinion about barriers and facilitators of the use of restrictive RBCs policy. The most indicated facilitators were the availability of scientific evidence that supports the restrictive policy (84%), medicolegal concerns (57%), preference (52%), and institutional protocols (50%).
Table 5. Barriers and facilitators of use of restrictive RBC policy (i.e. RBC transfusion if Hb < or = 7 g/dL or patient is symptomatic, e.g. hypotension, lightheadedness).
| Strongly encourages. | Encourages. | Neither encourages, nor discourages. | Discourages. | Strongly discourages. | Not applicable/ Not available. | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Institutional protocols in my hospital | 10 | 17.9% | 18 | 32.1% | 15 | 26.8% | 4 | 7.1% | 0 | 0.0% | 9 | 16.1% |
| Scientific evidence to support the restrictive use of RBCs transfusions | 16 | 28.6% | 31 | 55.4% | 9 | 16.1% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Medico-legal concerns about the consequences of not transfusing anemic patients | 10 | 17.9% | 22 | 39.3% | 24 | 42.9% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| For non-consultant ,to what extent does your attending's preference influence your use of a restrictive RBC policy (i.e. RBC transfusion if Hb ): | 12 | 21.4% | 17 | 30.4% | 9 | 16.1% | 0 | 0.0% | 1 | 1.8% | 17 | 30.4% |
Figure 2. Facilitators of use of restrictive RBC policy.
5. DISCUSSION
Blood transfusion practices affect both patients’ outcomes and utilization of institutional resources. Evidence shows that liberal blood transfusion has a detrimental effect on patients’ outcome. A restrictive approach of blood transfusion is recommended by current clinical guidelines (8, 9).
We observed variations in the management of anemia and the use of blood transfusion between the respondents. Also, the practices of respondents (as indicated by their responses in case scenarios) contradicted with the recommended restrictive policy of blood transfusion.
Anemia is commonly encountered in surgical patients pre-operatively which is associated with increased risk of post-operative complications (14-16). It has been found that pre-operative anemia management and blood transfusion have beneficial effects during and after the surgery, particularly on wound healing, but blood transfusions also carry increased risks of post-operative morbidity and mortality (17-23). In our study most, respondents (73%) were not aware that transfusion affects survival after oncological surgical resection. 55% of them believed that blood transfusion neither increases nor decreases the risk of recurrences of cancer after oncological resection. With regards of post-operative mortality, even lower percentage believed that transfusion increased the risk, while the majority believed that transfusion decreases the risk of mortality or not affecting it all. Majority of surgeons identified detrimental effect of transfusion was the increased risk of post-operative morbidity- which may have been best recognized due to the fear of transmitted infections. The detrimental effects of blood transfusion could be attributed also to transfusion-related immunomodulation (TRIM), stimulating the immunity, and inducing several clinical syndromes such as potentiation of some autoimmune disorders, multiple organ failure, graft-versus-host disease, and transfusion-related acute lung injury (24). Moreover, the TRIM effect can cause the host immune system to gain tolerance, resulting in increased chance for postoperative and nosocomial infections, cancer recurrence, and improved allograft survival (25). A meta-analysis study on patients with colorectal cancer found that perioperative blood transfusion is associated with an increased risk of tumor recurrence (level III) (14).
Most of the physicians use the level of hemoglobin alone to determine the need for blood transfusion. In fact, they must consider anemic symptoms additionally. Evading unnecessary usage of blood units can be beneficial in preserving resources and protecting patients against the probability of developing post transfusion unfavorable consequences (26). Clinical practice guidelines recommend restrictive transfusion policies in stable patients, so that blood transfusion should be indicated only in the case of hemoglobin below 7 g/dL in the absence of active bleeding. These strategies have been reported to be safe and effective in randomized controlled trials (27-29); resulting in reduction of peri-operative blood transfusion (12). In the presence of manifestations of impaired oxygen delivery (e.g., dizziness while standing, shortness of breath, and chest pain) or a history of coronary artery disease, a higher threshold of hemoglobin level (8 g/dL) is recommended (30). In our study, half of respondents (50%) reported using the recommended lower hemoglobin thresholds in scenarios involving patients without cardiac disease. However, most respondents did not consider the hemoglobin level at all in the presence of in symptomatic anemia (45%); in suspected postoperative bleeding (57%); and in high intraoperative bleeding (59%) , stating that they would order blood transfusion at any hemoglobin level in such cases. For stable patients with past cardiac disease, a higher threshold was chosen by most doctors (9 g/dL by 43% and 10 gm/dL by 21%), which was in partial agreement to the result reported by Yohanathan et al. (6) who stated that a hemoglobin level of 9 g/dL or higher was reported by a fourth of respondents for asymptomatic patients with cardiac comorbidities, by (70%) for patients with acute cardiac disease, and by half for non-cardiac symptoms of anemia (e.g., dizziness). These results also are in line with those reported by Sim and his colleagues (31).
Guidelines recommend the transfusion of one unit at a time to reduce the associated risks. However, (89%) of respondents reported ordering two units at a time. Over ordering with minimal utilization wastes technical time, reagents and imposes extra expenses on patients. Vibhute et al. (7) studied practices of blood ordering and transfusion in elective surgical patients and reported a rate of non-utilization of (76.9%) of cross-matched blood. This finding was also reported by subsequent studies that reported non- utilization rates of cross matched blood ranging from (43.6%) to (69.7%) (32). Yohanathan et al. found that (28%) of his respondents preferred to order 2 units or more at a time. Other studies also revealed (33-35) that (64 to 78%) of physicians order 2-unit transfusions when a single unit would have sufficed in more than (95%) of cases. Some studies (36, 37) evaluated gastrointestinal procedures and found that more than (40%) of transfusions were unnecessary (as judged by the guidelines). Intra-operative blood transfusion is decreasing with the time because of improved anesthesia and surgical techniques, organ preservation, and the use of intra-operative blood saver (38).
The most indicated facilitators were the availability of scientific evidence that supports the restrictive policy (84%), medicolegal concerns (57%), preference (52%), and institutional protocols (50%). These indicates that doctors perceived the need for improving their awareness through evidence-based guidelines that were adopted by local institutional protocols. Medicolegal concerns to affect the decision of surgeons requires more analysis in future studies.
6. CONCLUSION
Great variations exist between the respondents with regard of blood transfusion practices. Although current clinical guidelines recommend a restrictive transfusion practice, most respondents tended to over-order blood for elective procedures and were not aware of the potential complications of liberal blood transfusion. Blood ordering pattern for elective surgeries should be revised to minimize over-ordering of blood. Health institutions should improve the awareness of surgeons through incorporating supporting evidence, in formulating local institutional guidelines.
Acknowledgments:
Manar Abdullah Makin, Alya Sameer, Alharbi, Shoruq Abdulaziz Alwagdani, Salwa Abdullah Alshiqayhi, Maeen Nezar Almadani and Nisar Haider Zaidi.
Author’s contribution:
all authors were included in all steps of preparation this article. Final proof reading was made by the first author.
Conflict of interest:
There are no conflicts of interest.
Financial support and sponsorship:
None.
REFERENCES
- 1.Wu WC, Schifftner TL, Henderson WG, Eaton CB, Poses RM, Uttley G, et al. Preoperative hematocrit levels and postoperative outcomes in older patients undergoing noncardiac surgery. JAMA. 2007;297(22):2481–2488. doi: 10.1001/jama.297.22.2481. [DOI] [PubMed] [Google Scholar]
- 2.Abdelsattar ZM, Hendren S, Wong SL, Campbell DA, Jr, Henke P. Variation in transfusion practices and the effect on outcomes after noncardiac surgery. Annals of surgery. 2015;262(1):1–6. doi: 10.1097/SLA.0000000000001264. [DOI] [PubMed] [Google Scholar]
- 3.Callum JL, Waters JH, Shaz BH, Sloan SR, Murphy MF. The AABB recommendations for the C hoosing W isely campaign of the A merican B oard of I nternal M edicine. Transfusion. 2014;54(9):2344–2352. doi: 10.1111/trf.12802. [DOI] [PubMed] [Google Scholar]
- 4.Chung M, Steinmetz O, Gordon P. Perioperative blood transfusion and outcome after resection for colorectal carcinoma. British Journal of Surgery. 1993;80(4):427–432. doi: 10.1002/bjs.1800800407. [DOI] [PubMed] [Google Scholar]
- 5.Olawumi H, Bolaji B. Blood utilization in elective surgical procedures in Ilorin. 2006.
- 6.Yohanathan L, Coburn NG, McLeod RS, Kagedan DJ, Pearsall E, Zih FS, et al. Understanding Perioperative Transfusion Practices in Gastrointestinal Surgery–a Practice Survey of General Surgeons. Journal of Gastrointestinal Surgery. 2016;20(6):1106–1122. doi: 10.1007/s11605-016-3111-5. [DOI] [PubMed] [Google Scholar]
- 7.Vibhute M, Kamath S, Shetty A. Blood utilisation in elective general surgery cases: requirements, ordering and transfusion practices. Journal of postgraduate medicine. 2000;46(1):13. [PubMed] [Google Scholar]
- 8.Napolitano LM. Current status of blood component therapy in surgical critical care. Current Opinion in Critical Care. 2004;10(5):311–317. doi: 10.1097/01.ccx.0000140948.98019.8a. [DOI] [PubMed] [Google Scholar]
- 9.Carson JL, Grossman BJ, Kleinman S, Tinmouth AT, Marques MB, Fung MK, et al. Red blood cell transfusion: a clinical practice guideline from the AABB. Annals of internal medicine. 2012;157(1):49–58. doi: 10.7326/0003-4819-157-1-201206190-00429. [DOI] [PubMed] [Google Scholar]
- 10.Carson JL, Hill S, Carless P, Hébert P, Henry D. Transfusion triggers: a systematic review of the literature. Transfusion medicine reviews. 2002;16(3):187–199. doi: 10.1053/tmrv.2002.33461. [DOI] [PubMed] [Google Scholar]
- 11.Robertson CS, Hannay HJ, Yamal J-M, Gopinath S, Goodman JC, Tilley BC, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014;312(1):36–47. doi: 10.1001/jama.2014.6490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Almeida JP, Vincent J-L, Galas FRBG, de Almeida EPM, Fukushima JT, Osawa EA, et al. Transfusion Requirements in Surgical Oncology PatientsA Prospective, Randomized Controlled Trial. The Journal of the American Society of Anesthesiologists. 2015;122(1):29–38. doi: 10.1097/ALN.0000000000000511. [DOI] [PubMed] [Google Scholar]
- 13.The American Association for Public Opinion. Deerfield, Illinois: 2016. American Association for Public Opinion Research Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys; p. 16. [Google Scholar]
- 14.Dunne JR, Gannon CJ, Osborn TM, Taylor MD. Preoperative anemia in colon cancer: assessment of risk factors. The American Surgeon. 2002;68(6):582. [PubMed] [Google Scholar]
- 15.Dunne JR, Malone D, Tracy JK, Gannon C, Napolitano LM. Perioperative anemia: an independent risk factor for infection, mortality, and resource utilization in surgery. Journal of Surgical Research. 2002;102(2):237–244. doi: 10.1006/jsre.2001.6330. [DOI] [PubMed] [Google Scholar]
- 16.Musallam KM, Tamim HM, Richards T, Spahn DR, Rosendaal FR, Habbal A, et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet. 2011;378(9800):1396–1407. doi: 10.1016/S0140-6736(11)61381-0. [DOI] [PubMed] [Google Scholar]
- 17.Hill GE, Frawley WH, Griffith KE, Forestner JE, Minei JP. Allogeneic blood transfusion increases the risk of postoperative bacterial infection: a meta-analysis. Journal of Trauma and Acute Care Surgery. 2003;54(5):908–914. doi: 10.1097/01.TA.0000022460.21283.53. [DOI] [PubMed] [Google Scholar]
- 18.O’Brien S, Yi QL, Fan W, Scalia V, Fearon M, Allain JP. Current incidence and residual risk of HIV, HBV, and HCV at Canadian Blood Services. Vox Sanguinis. 2012;103(1):83–86. doi: 10.1111/j.1423-0410.2012.01584.x. [DOI] [PubMed] [Google Scholar]
- 19.Hallet J, Mahar AL, Tsang ME, Lin Y, Callum J, Coburn NG, et al. The impact of peri-operative blood transfusions on post-pancreatectomy short-term outcomes: an analysis from the A merican C ollege of S urgeons N ational S urgical Q uality I mprovement P rogram. HPB. 2015;17(11):975–982. doi: 10.1111/hpb.12473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Amato A, Pescatori M. Perioperative blood transfusions for the recurrence of colorectal cancer. 2006. [DOI] [PMC free article] [PubMed]
- 21.Ferraris VA, Davenport DL, Saha SP, Bernard A, Austin PC, Zwischenberger JB. Intraoperative transfusion of small amounts of blood heralds worse postoperative outcome in patients having noncardiac thoracic operations. The Annals of thoracic surgery. 2011;91(6):1674–1680. doi: 10.1016/j.athoracsur.2011.01.025. [DOI] [PubMed] [Google Scholar]
- 22.Hallet J, Tsang M, Cheng ES, Habashi R, Kulyk I, Hanna SS, et al. The impact of perioperative red blood cell transfusions on long-term outcomes after hepatectomy for colorectal liver metastases. Annals of surgical oncology. 2015;22(12):4038–4045. doi: 10.1245/s10434-015-4477-4. [DOI] [PubMed] [Google Scholar]
- 23.American Medical Association–Joint Commission. 2013. editor Proceedings from the National Summit on Overuse 2013.
- 24.Raghavan M, Marik PE. Anemia, allogenic blood transfusion, and immunomodulation in the critically ill. Chest. 2005;127(1):295–307. doi: 10.1378/chest.127.1.295. [DOI] [PubMed] [Google Scholar]
- 25.Bernard AC, Davenport DL, Chang PK, Vaughan TB, Zwischenberger JB. Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical-site infection, pneumonia, and sepsis in general surgery patients. Journal of the American College of Surgeons. 2009;208(5):931–937e2. doi: 10.1016/j.jamcollsurg.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 26.Hutton B, Fergusson D, Tinmouth A, McIntyre L, Kmetic A, Hébert PC. Transfusion rates vary significantly amongst Canadian medical centres. Canadian journal of anaesthesia. 2005;52(6):581–590. doi: 10.1007/BF03015766. [DOI] [PubMed] [Google Scholar]
- 27.Cooper HA, Rao SV, Greenberg MD, Rumsey MP, McKenzie M, Alcorn KW, et al. Conservative versus liberal red cell transfusion in acute myocardial infarction (the CRIT Randomized Pilot Study) The American journal of cardiology. 2011;108(8):1108–1111. doi: 10.1016/j.amjcard.2011.06.014. [DOI] [PubMed] [Google Scholar]
- 28.Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. New England Journal of Medicine. 2011;365(26):2453–2462. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Carson JL, Carless PA, Hebert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. The Cochrane database of systematic reviews. 2012;4(1) doi: 10.1002/14651858.CD002042.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Retter A, Wyncoll D, Pearse R, Carson D, McKechnie S, Stanworth S, et al. Guidelines on the management of anaemia and red cell transfusion in adult critically ill patients. British journal of haematology. 2013;160(4):445–464. doi: 10.1111/bjh.12143. [DOI] [PubMed] [Google Scholar]
- 31.Sim V, Kao LS, Jacobson J, Frangos S, Brundage S, Wilson CT, et al. Can old dogs learn new “transfusion requirements in critical care”: a survey of packed red blood cell transfusion practices among members of The American Association for the Surgery of Trauma. The American Journal of Surgery. 2015;210(1):45–51. doi: 10.1016/j.amjsurg.2014.08.024. [DOI] [PubMed] [Google Scholar]
- 32.Belayneh T, Messele G, Abdissa Z, Tegene B. Blood requisition and utilization practice in surgical patients at university of gondar hospital, northwest ethiopia. Journal of blood transfusion. 2013;2013 doi: 10.1155/2013/758910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hebert PC, Wells G, Martin C, Tweeddale M, Marshall J, Blajchman M, et al. A Canadian survey of transfusion practices in critically ill patients. Critical care medicine. 1998;26(3):482–487. doi: 10.1097/00003246-199803000-00019. [DOI] [PubMed] [Google Scholar]
- 34.Hébert PC, Wells G, Martin C, Tweeddale M, Marshall J, Blajchman M, et al. Variation in red cell transfusion practice in the intensive care unit: a multicentre cohort study. Critical Care. 1999;3(2):57. doi: 10.1186/cc310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ma M, Eckert K, Ralley F, Chin-Yee I. A retrospective study evaluating single-unit red blood cell transfusions in reducing allogeneic blood exposure. Transfusion Medicine. 2005;15(4):307–312. doi: 10.1111/j.0958-7578.2005.00592.x. [DOI] [PubMed] [Google Scholar]
- 36.Ejaz A, Spolverato G, Kim Y, Frank SM, Pawlik TM. Identifying variations in blood use based on hemoglobin transfusion trigger and target among hepatopancreaticobiliary surgeons. Journal of the American College of Surgeons. 2014;219(2):217–228. doi: 10.1016/j.jamcollsurg.2014.02.033. [DOI] [PubMed] [Google Scholar]
- 37.Ross A, Mohammed S, VanBuren G, Silberfein EJ, Artinyan A, Hodges SE, et al. An assessment of the necessity of transfusion during pancreatoduodenectomy. Surgery. 2013;154(3):504–511. doi: 10.1016/j.surg.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 38.Bismuth H, Castaing D, Garden OJ. Major hepatic resection under total vascular exclusion. Annals of Surgery. 1989;210(1):13. doi: 10.1097/00000658-198907000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]