Abstract
Introduction:
Osteoarthritis (OA) is the most common joint disease in the world. At the end stage of the disease, usually when patients cannot handle the pain anymore, the knee replacement surgery is the most common and effective treatment to reduce pain and improve functionality. The effect of preoperative exercise (prehabilitation) for patients undergoing total knee arthroplasty (TKA) is still controversial.
Aim:
To investigate the effect of prehabilitation on postoperative outcome and compare the results of the intervention with the control group.
Material and Methods:
This prospective study included 20 patients with a diagnosis of gonarthrosis, aged 48-70, who were randomly allocated to either the intervention group or control. Ten patients (intervention group) underwent a 6-week home-based exercise program before the TKA surgery. All patients were assessed by Knee Score (KS), Function Score (FS), and Body Mass Index (BMI) according to the following schedule: 6 weeks before surgery (for intervention group it meant before the prehabilitation program), just prior to surgery (for intervention group it meant after the prehabilitation program), after the surgery, at 3rd month, 6th month, and 12th month postoperatively. They were all operated by the same surgeon, for the primary total knee replacement (Zimmer NexGen Complete Knee Solution) at the Clinic for Orthopaedics and Traumatology, Clinical Centre University of Sarajevo, from October 2016 to June 2017.
Results:
There is statistically significant difference for Knee and Function Score between the intervention and control group in testing time: just before surgery–meaning that KS and FS increased after the prehabilitation program. Knee Score was significantly different between the two observed groups postoperatively, 3 months postoperatively and 6 months postoperatively, while the Function Score was not significantly different in that period. Prehabilitation program provides better preoperative KS and FS, and better KS up to 6 months postoperatively. However, 12 months postoperatively there was no significant difference between the intervention and control group for the Knee and Function Score.
Conclusion:
Prehabilitation brings significant difference regarding the Knee Score in favor of the intervention group preoperatively and up to 6 months postoperatively.
Keywords: Osteoarthritis, treatment, arthroplasty
1. INTRODUCTION
Osteoarthritis (OA) is the most common joint disease in the world (1). It brings individual and societal consequences in terms of musculoskeletal pain, disability and socioeconomic costs (2, 3). This degenerative disease substantially affects weight-bearing joints, so in case of knee OA patients suffer from pain and function impairments that prevent them to participate in activities of daily living (4) and participate in work (5).
At the end stage of the disease, usually when patients cannot handle the pain anymore, the knee replacement surgery is the most common and effective treatment to reduce pain and improve functionality. Total knee replacement, also called total knee arthroplasty (TKA), is a surgical procedure whereby the diseased knee joint is replaced with artificial material.
Resurfacing a knee relieves the patient’s pain, stiffness and range of motion. However, high prevalence of persistent mild and infrequent pain after TKA has been reported, and 15% suffers from severe pain at 3-4 years after the surgical procedure (6). Moreover, during the first years after TKA, patients have worse knee function than age-matched subjects (7, 8). Quadriceps strength decreased by 60% and activation decreased 17% after TKA (9).
Together with the age-related loss of muscle mass and the epidemic of obesity, the risk of disability increases, and therefore the surgical procedures are also likely to increase worldwide (10). Existing evidence regarding the significance of body mass index (BMI) and preoperative exercise (prehabilitation) for patients undergoing total knee arthroplasty are still controversial. However, it was found that the preoperative quadriceps strength is strong predictor of functional performance one year (11) and two years after the TKA (12).
A recent systematic review and meta-analysis suggests that prehabilitation programs provide small-to-moderate improvements that vary by joint (hip or knee) (13). In patients undergoing knee replacement, preoperative exercise showed better postoperative function, quadriceps strength and shorter length of stay, while not significantly less pain, what was present in the total hip replacement.
Large part of the literature still fails in showing clear benefits after these programs (14-18).
Analyzing the studies regarding the prehabilitation period prior to surgical procedure of total knee replacement, we conclude that the preoperative training period typically lasts between 4 to 8 weeks, in some studies also 2 weeks (13). During this period of time, Folland et al. proved that muscle strength increases due to neural adaptations rather than hypertrophy (19).
Moreover, a study showed that the conventional exercises made low levels of neuromuscular activation (<35%) (20). In the study, only a few of many different conventional exercises were observed, and that might be one of the limitations. The highest level of neuromuscular activation (67%-79%) was observed during the open kinetic chain resistance exercises (isolated knee extension and hamstring muscle curl). This study concluded that heavy resistance exercises should be included in the rehabilitation programs, in order to activate sufficient levels of neuromuscular activation which leads to stimulation of the muscle growth and strength. This is important especially when the goal is to improve muscle strength during a few weeks only. A major goal for orthopedic surgeons and rehabilitation specialists is to regain muscle strength (21).
Total knee arthroplasty corrects instability and deformity of the knee joint (22). Despite constant attempts to improve the prosthesis design (23, 24), surgical procedures and postoperative rehabilitation (25), TKA rarely allows full range of motion (ROM) with flexion of more than 120°. It is obvious that with a postoperative ROM between 100° and 120°, most activities of daily living can easily be performed (26).
Although some patients have expectations to perform flexion 140°-150°, what is essential for various religious, cultural (27) and athletic activities, and daily activities such as taking a bath and gardening (28).
However, stiffness after total knee arthroplasty, defined as flexion less than 90° 1 year postoperatively, has been reported to be 3.7% (29).
In 2012, Matassi et al. stated that preoperative ROM is the most decisive regarding the final flexion after TKA (30). It seems logical that greater preoperative ROM helps to maximize flexion after TKA, although it is not clearly proven which exercises are most effective.
Additionally, pain due to OA leads to restricting knee movements. Patients are therefore vulnerable to gain weight. Most of candidates undergoing the knee replacement are overweight (31). Obesity is associated with increased risks of short- and long- term complications, and thus higher costs due to surgical procedures, both primary and revision cases. Moreover, decreased functional results are associated with obesity. Consequently, orthopedic surgeons advise their patients to lose weight and prepare physically prior to surgical procedure. Losing weight and/or better preoperative health status (greater physical function and strength) are strong predictor of good postoperative outcome following TKA.
There are different scores by which knee could be assessed. In this study, we used the Knee Society Clinical Rating System that was established in 1989 (32), even though the new Knee Society Scoring System was published in 2011. The knee scoring system we used in our study is subdivided into a knee score that rates only the knee joint itself and a functional score that rates the patient’s ability to walk and climb stairs.
The Knee Society Clinical Rating System from 1989 was simple, but objective scoring system to rate the patient’s knee and functional abilities (32). The new Knee Society Scoring System is more complex, and in order to be used, a license is needed. It is validated and responsive method for assessing objective and subjective outcomes after total and partial knee arthroplasty, without ambiguities of the prior scoring system. Patients have different expectations, demands, and functional requirements than those of prior generations who underwent knee arthroplasty.
2. AIM
Aim of article was to investigate the effect of prehabilitation on postoperative outcome and compare the results of the intervention with the control group.
3. MATERIAL AND METHODS
This prospective study included 20 patients with a diagnosis of gonarthrosis, aged 48-70, who were randomly allocated to either the intervention group or control. Ten patients (intervention group) underwent a 6-week home-based exercise program before the TKA surgery. All patients were assessed by Knee Score (KS), Function Score (FS), and Body Mass Index (BMI) according to the following schedule: 6 weeks before surgery (for intervention group it meant before the prehabilitation program), just prior to surgery (for intervention group it meant after the prehabilitation program), after the surgery, at 3rd month, 6th month, and 12th month postoperatively. They were all operated by the same surgeon, for the primary total knee replacement (Zimmer NexGen Complete Knee Solution) at the Clinic for Orthopaedics and Traumatology, Clinical Centre University of Sarajevo, from October 2016 to June 2017.
Prehabilitation program consisted of 6 week home-based exercises: quadriceps strengthening, flexibility and resistance training. The exercises were shown to the patients, and they needed to make them 3 times per day for 6 weeks. Patients with systemic inflammatory disease, diabetes mellitus and concomitant lower extremity deformities were excluded from the study, as so the patients who could not tolerate protocol of preoperative and postoperative treatment. Patients were obliged to get the approval status by the internal medicine specialist, where should be written that the patient has no contraindications for the surgical procedure.
Knee replacement surgery was performed via anterior mid line skin incision and medial parapatellar incision with fixed bearing cemented retaining knee prosthesis sacrificing cruciate ligaments–primary case. Until the day of discharge, according to the standard clinic protocol, all patients performed isometric and isotonic quadriceps exercises, exercises for the range of motion and walking up and down stairs. The day after surgery all patients were mobilized with full weight bearing via two crutches. All patients were allowed to walk without crutches 6 weeks after the operation.
Detailed information on surgical interventions was provided to all patients. An informed consent regarding all procedures was signed by all patients. They were advised not to gain weight prior and after the surgical procedure, take care about the diet, although these processes could not be fully controlled.
4. RESULTS
The study included 20 subjects, equally divided into two groups: with prehabilitation program (n=10; 3 males, 7 females) and without prehabilitation program (n=10; 3 males and 7 females). Patients were similar age–male subjects (6; 30%) had a median age of 59.0 ± 9.47 years while female subjects (14; 70%) had a median age of 59.7 ± 6.28 years.
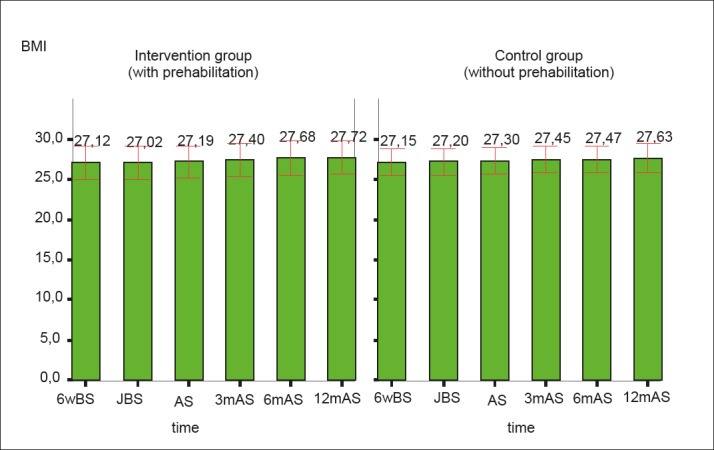
Both groups (with prehabilitation program and without prehabilitation program) showed statistically significant increase in knee and functional score over time (p<0.05), while there were no statistically significant changes in BMI (p> 0.05) over time (Figures 1, 2, 3).
Figure 1. The trend of the Knee Score increase over time (6 weeks before surgery up to 12 months after surgery) is presented in both groups. In both groups, there was a statistically significant increase in knee score (p<0.05) over the displayed period of time. 6wBS–6 weeks before surgery, JBS–just before surgery, AS–after surgery, 3mAS–3 months after surgery, 6mAS – 6 months after surgery, 12mAS–12 months after surgery.
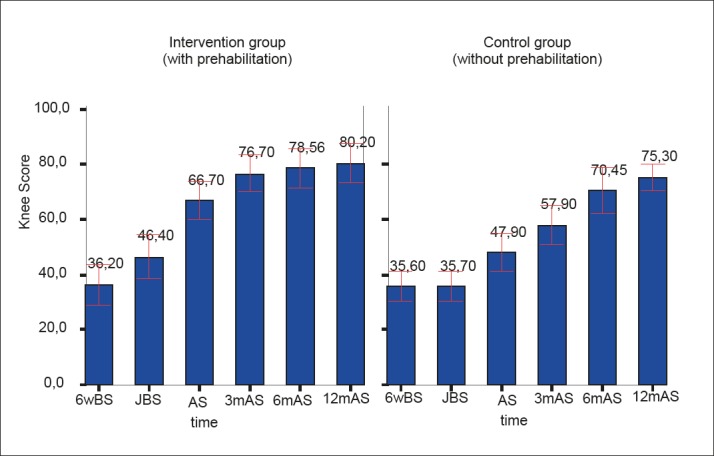
Figure 2. The trend of the Functional Score increase over time (6 weeks before surgery up to 12 months after surgery) is presented in both groups. In both groups, there was a statistically significant increase in Functional Score (p<0.05) over the displayed period of time. 6wBS–6 weeks before surg ery, JBS–just before surgery, AS–after surgery, 3mAS–3 months after surgery, 6mAS – 6 months after surgery, 12mAS–12 months after surgery.
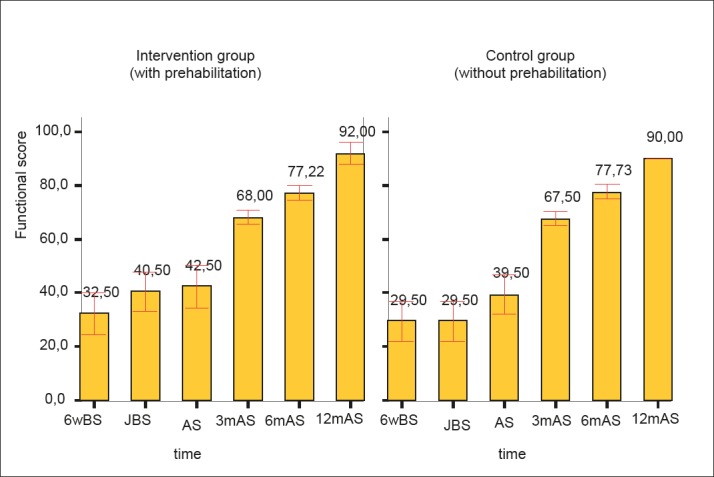
Figure 3. The trend of BMI score increase over time (6 weeks prior to surgery up to 12 months after surgery) is presented in both groups. In both groups, there were no statistically significant changes in BMI (p> 0.05) over time. 6wBS–6 weeks before surgery, JBS–just before surgery, AS–after surgery, 3mAS–3 months after surgery, 6mAS – 6 months after surgery, 12mAS–12 months after surgery.
Both groups had a similar KS 6 weeks before surgery (36.20±7.52 vs. 35.60±5.48; p=0.841). In the next 4 measurements, the intervention group had a statistically higher knee score compared to the control group (p<0.05). In the intervention group, KS just before the surgery was 46.40±8.00, postoperatively KS was 66.70±6.83, three months postoperatively KS was 76.70±6.83 and six months postoperative KS was 79.10±6.97, while in the control group KS just before surgery was 35.70±5.58, postoperatively KS was 47.90±6.89, 3 months postoperatively KS was 57.90±7.05 and 6 months postoperatively KS was 69.10±7.34. However, 12 months postoperatively, KS was similar between groups (80.20±7.07 vs. 75.30±4.88; p=0.09).
Both groups had a similar FS in all measurements, except just before surgery, where group the intervention group had a significantly higher FS compared to the control group (40.50±7.25 vs. 29.50±7.25; p=0.003). In the first measurement (6 weeks before surgery) FS was 32.50±7.91 in the intervention group vs. 29.50±7.25 in control group, p=0.338. Postoperatively FS was 42.50±7.91 in intervention group and 39.50±7.25 in control group, p=0.388. 3 months postoperatively FS was 68.00±2.58 in first group vs. 67.50±2.64 in second group, p=0.673. 6 months postoperatively FS was equal in both groups (p=1.00), FS was 77.50±2.64. 12 months postoperatively FS was 92.00±4.22 in the intervention group vs. 90.00±0.00 in control group, p=0.151.
5. DISCUSSION
Different studies used different scoring systems in order to evaluate the effect of preoperative exercises on postoperative outcome (13). Outcome could be measured by WOMAC (Western Ontario and McMaster Universities Osteoarthritis Index), Knee Society Clinical Rating System, LOS (Length of Stay), VAS (Visual Analog Scale for pain), etc. A systematic review and meta-analysis published in 2017 suggest that prehabilitation programs provide small-to-moderate improvements that differ by joint (13). In patients undergoing Total Hip Arthroplasty, significant improvements were observed for pain, function, and length of stay. On the other hand, in patients undergoing Total Knee Arthroplasty, significant improvements were observed for function, quadriceps strength, and length of stay.
In 2012, Matassi et al. proved that preoperative exercise program is beneficial on short-term postoperative recovery after TKA, and it helps patients to reach 90° of knee flexion earlier (30). They demonstrated that after 6 weeks of training, there was a significant improvement (p<0,0001) of passive and active flexion, extension and knee score for the intervention group. No difference for the function score was detected. Furthermore, there was no evidence for an effect of exercise on the knee score or function score, measured by the same rating system as we did–Knee Society Clinical Rating System.
In 2017, Calatayud et al. described that high-intensity strength training during preoperative period reduces pain and improves lower limb muscle strength, ROM and functional task performance before surgery, resulting in a reduced length of stay and a faster physical and functional recovery after TKA (1).
In 2015, Skoffer et al. stated that supervised preoperative PRT (progressive resistance training) is an efficacious and safe intervention for improving postoperative functional performance and muscle strength, but improvements in patient-reported outcomes were not detected (33). Patients who are about to get the TKA are less active and their BMI is usually higher. It is obvious that inactivity leads to decrease in range of motion and those patients have more difficult post-surgery time and rehabilitation. In our study, it was shown that the prehabilitation plays an important role for the better post-operative outcome after primary total knee arthroplasty.
There were similar values of KS, FS and BMI between the intervention and control group, 6 weeks before surgery, meaning that the groups were pretty similar regarding these variables. However, the intervention group made an increase in Knee Score prior to surgery and that is crucial, because the rehabilitation is easier when muscles are stronger and more activated. Surgery is a stress to the organism, and if we get not ready for the procedure, the post-operative outcome does not go the way we want. Although at the later stage, more exactly 12 months postoperatively, the differences between the two groups decreased.
Future clinical trials should have a standardized regimen of seeking the outcomes (meaning which outcome are we looking for and at which time points). After that, the treatment methods (exercises and educational program) should be evaluated in order to improve post-operative patient’s expectations, and clinical signs (13).
6. CONCLUSION
Our study proves statistically significant difference for Knee and Function Score between the intervention and control group in testing time: just before surgery–meaning that KS and FS increased after the prehabilitation program (6 weeks home-based exercise program).
Knee Score was significantly different between the two observed groups postoperatively, 3 months postoperatively and 6 months postoperatively, while the Function Score was not significantly different in that period. Preoperative home exercises provide better preoperative KS and FS, and better Knee Score up to 6 months postoperatively. However, 12 months postoperatively there was no significant difference between the intervention and control group for the Knee and Function Score.
To sum up, prehabilitation brings significant difference regarding the Knee Score in favor of the intervention group preoperatively and 6 months postoperatively.
Table 1. Mean values (mean±SD) for Knee Score, Functional Score and BMI in intervention and control group.
| Intervention group n=10 |
Control group n=10 |
test | ||
|---|---|---|---|---|
| Testing time | Variable | Mean±SD | Mean±SD | t-test |
| 6 weeks before surgery | Knee Score | 36.20±7,52 | 35.60±5,48 | 0.841 |
| Function Score | 32.50±7,91 | 29.0±7,25 | 0.338 | |
| Body Mass Index | 27.12±2,11 | 27.15±1,67 | 0.972 | |
| Just before surgery | Knee Score | 46.40±8,00 | 35.70±5,58 | 0.003 |
| Function Score | 40.50±7,25 | 29.50±7,25 | 0.003 | |
| Body Mass Index | 27.02±2,07 | 27.20±1,70 | 0.834 | |
| After surgery | Knee Score | 66.70±6,83 | 47.90±6,89 | 0.0001 |
| Function Score | 42.50±7,91 | 39.50±7,25 | 0.388 | |
| Body Mass Index | 27.19±2,04 | 27.30±1,71 | 0.898 | |
| 3 months after surgery | Knee Score | 76.70±6,83 | 57.90±7,05 | 0.0001 |
| Function Score | 68.00±2,58 | 67.50±2,64 | 0.673 | |
| Body Mass Index | 27,40±2,08 | 27,45±1,66 | 0,953 | |
| 6 months after surgery | Knee Score | 79.10±6,97 | 69.10±7,34 | 0.006 |
| Function Score | 77.50±2,64 | 77.50±2,64 | 1.00 | |
| Body Mass Index | 27.50±2,11 | 27.63±1,72 | 0.881 | |
| 12 months after surgery | Knee Score | 80.20±7,07 | 75.30±4,88 | 0.09 |
| Function Score | 92.00±4,22 | 90.00±0,00 | 0.151 | |
| Body Mass Index | 27.72±2,11 | 27.63±1,83 | 0.920 |
Author’s Contribution:
Dz.J. and Dj.O. gave substantial contribution to the conception or design of the work and in the acquisition, analysis and interpretation of data for the work. Dz.J., Dj.O., A.T.T. and F.Dz. had role in drafting the work and revising it critically for important intellectual content. Each author gave final approval of the version to be published and they agreed to be accountable for all aspects of the work in ensuring the questions related to the accuracy or integrity of any part of the work.
Conflicts of interest:
None declared.
Financial support and sponsorship:
None.
REFERENCES
- 1.Calatayud J, Casaña J, Ezzatvar Y, et al. High-intensity preoperative training improves physical and functional recovery in the early post-operative periods after total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25:2864–2872. doi: 10.1007/s00167-016-3985-5. [DOI] [PubMed] [Google Scholar]
- 2.Allen KD, Golightly YM. State of the evidence. Curr Opin Rheumatol. 2015;27:276–283. doi: 10.1097/BOR.0000000000000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Glyn-Jones S, Palmer AJR, Agricola R, et al. Osteoarthritis. The Lancet. 2015;386:376–387. doi: 10.1016/S0140-6736(14)60802-3. [DOI] [PubMed] [Google Scholar]
- 4.Jones CA, Voaklander DC, Johnston DW, et al. Health related quality of life outcomes after total hip and knee arthroplasties in a community based population. J Rheumatol. 2000;27:1745–1752. [PubMed] [Google Scholar]
- 5.Palmer KT. The older worker with osteoarthritis of the knee. Br Med Bull. 2012;102:79–88. doi: 10.1093/bmb/lds011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wylde V, Hewlett S, Learmonth ID, et al. Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566–572. doi: 10.1016/j.pain.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 7.Ritter MA, Thong AE, Davis KE, et al. Long-term deterioration of joint evaluation scores. J Bone Joint Surg Br. 2004;86:438–442. doi: 10.1302/0301-620x.86b3.14243. [DOI] [PubMed] [Google Scholar]
- 8.Silva M, Shepherd EF, Jackson WO, et al. Knee strength after total knee arthro- plasty. J Arthroplasty. 2003;18:605–611. doi: 10.1016/s0883-5403(03)00191-8. [DOI] [PubMed] [Google Scholar]
- 9.Stevens JE, Mizner RL, Snyder-Mackler L. Quadriceps strength and volitional activation before and after total knee arthroplasty for osteoarthritis. J Orthop Res. 2003;21:775–779. doi: 10.1016/S0736-0266(03)00052-4. [DOI] [PubMed] [Google Scholar]
- 10.Volpi E, Nazemi R, Fujita S. Muscle tissue changes with aging. Curr Opin Clin Nutr Metab Care. 2004;7:405–410. doi: 10.1097/01.mco.0000134362.76653.b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mizner RL, Petterson SC, Stevens JE, et al. Preoperative quadriceps strength predicts functional ability one year after total knee arthroplasty. J Rheumatol. 2005;32:1533–1539. [PubMed] [Google Scholar]
- 12.Zeni JA, Snyder-Mackler L. Preoperative predictors of persistent impairments during stair ascent and descent after total knee arthroplasty. J Bone Joint Surg Am. 2010;92:1130–1136. doi: 10.2106/JBJS.I.00299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moyer R, Ikert K, Long K, et al. The Value of Preoperative Exercise and Education for Patients Undergoing Total Hip and Knee Arthroplasty: A Systematic Review and Meta-Analysis. JBJS Rev. 2017;5(12):e2. doi: 10.2106/JBJS.RVW.17.00015. [DOI] [PubMed] [Google Scholar]
- 14.van Leeuwen DM, de Ruiter CJ, Nolte PA, et al. Preoperative strength training for elderly patients awaiting total knee arthroplasty. Rehabil Res Pract. 2014;2014:e462750. doi: 10.1155/2014/462750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McKay C, Prapavessis H, Doherty T. The effect of a pre- habilitation exercise program on quadriceps strength for patients undergoing total knee arthroplasty: a randomized controlled pilot study. PM&R. 2012;4:647–656. doi: 10.1016/j.pmrj.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 16.Rodgers JA, Garvin KL, Walker CW, et al. Preoperative physical therapy in primary total knee arthroplasty. J Arthroplasty. 1998;13:414–421. doi: 10.1016/s0883-5403(98)90007-9. [DOI] [PubMed] [Google Scholar]
- 17.Rooks DS, Huang J, Bierbaum BE, et al. Effect of pre- operative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum. 2006;55:700–708. doi: 10.1002/art.22223. [DOI] [PubMed] [Google Scholar]
- 18.Swank AM, Kachelman JB, Bibeau W, et al. Prehabilitation before total knee arthroplasty increases strength and function in older adults with severe osteoarthritis. J Strength Cond Res. 2011;25:318–325. doi: 10.1519/JSC.0b013e318202e431. [DOI] [PubMed] [Google Scholar]
- 19.Folland JP, Williams AG. The adaptations to strength training: morphological and neurological contributions to increased strength. Sports Med. 2007;37:145–168. doi: 10.2165/00007256-200737020-00004. [DOI] [PubMed] [Google Scholar]
- 20.Andersen LL, Magnusson SP, Nielsen M, et al. Neuromuscular activation in conventional therapeutic exercises and heavy resistance exercises: implications for rehabilitation. Phys Ther. 2006;86:683–697. [PubMed] [Google Scholar]
- 21.Saleh KJ, Lee LW, Gandhi R, et al. Quadriceps strength in relation to total knee arthroplasty outcomes. Instr Course Lect. 2010;59:119–130. [PubMed] [Google Scholar]
- 22.Insall J, Scott WN, Ranawat CS. The total condylar knee prosthesis: a report of two hundred and twenty cases. J Bone Jt Surg Am. 1979;61-A:173–180. [PubMed] [Google Scholar]
- 23.Akagi M, Nakamura T, Matsusue Y, et al. The bisurface total knee replacement: a unique design for flexion: four-to-nine year follow-up study. J Bone Jt Surg Am. 2000;82-A:1626–1633. doi: 10.2106/00004623-200011000-00017. [DOI] [PubMed] [Google Scholar]
- 24.Ranawat CS. Design may be counterproductive for opti- mizing flexion after TKR. Clin Orthop Relat Res. 2003;416:174–176. doi: 10.1097/01.blo.0000093028.56370.46. [DOI] [PubMed] [Google Scholar]
- 25.Esler CAN, Lock K, Harper WM, et al. Manipulation of total knee replacements. J Bone Jt Surg Br. 1999;81-B:27–29. doi: 10.1302/0301-620x.81b1.8848. [DOI] [PubMed] [Google Scholar]
- 26.Laubenthal KN, Smidt GL, Kettelkamp DB. A quantitative analysis of knee motion during activities of daily living. Phys Ther. 1972;52:34–42. doi: 10.1093/ptj/52.1.34. [DOI] [PubMed] [Google Scholar]
- 27.Mulholland SJ, Wyss UP. Activities of daily living in non- western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24:191–198. doi: 10.1097/00004356-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Rowe PJ, Myles CM, Walker C, et al. Knee joint kinematics in gait and other functional activities measured using flexible electrogoniometry: how much knee motion is sufficient for normal daily life? Gait Posture. 2000;12:143–155. doi: 10.1016/s0966-6362(00)00060-6. [DOI] [PubMed] [Google Scholar]
- 29.Gandhi R, de Beer J, Leone J, et al. Predictive risk factors for stiff knees in total knee arthroplasty. J Arthroplasty. 2006;21(1):46–52. doi: 10.1016/j.arth.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 30.Matassi F, Duerinckx J, Vandenneucker H, et al. Range of motion after total knee arthroplasty: the effect of a preoperative home exercise program. Knee Surg Sports Traumatol Arthrosc. 2012;22(3):703–709. doi: 10.1007/s00167-012-2349-z. [DOI] [PubMed] [Google Scholar]
- 31.Polat G, Ceylan HH, Sayar S, et al. Effect of body mass index on functional outcomes following arthroplasty procedures. World J Orthop. 2015;6(11):991–995. doi: 10.5312/wjo.v6.i11.991. 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Insall JN, Dorr LD, Scott RD, et al. Rationale of the Knee Society Clinical Rating System. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 33.Skoffer B, Maribo T, Mechlenburg I, et al. Efficacy of preoperative progressive resistance training on postoperative outcomes in patients undergoing total knee arthroplasty. Arthritis Care Res (Hoboken) 2016;68(9):1239–1251. doi: 10.1002/acr.22825. [DOI] [PubMed] [Google Scholar]


