Abstract
Context:
The influence of food and beverage labeling (food labeling) on consumer behaviors, industry responses, and health outcomes is not well established.
Evidence acquisition:
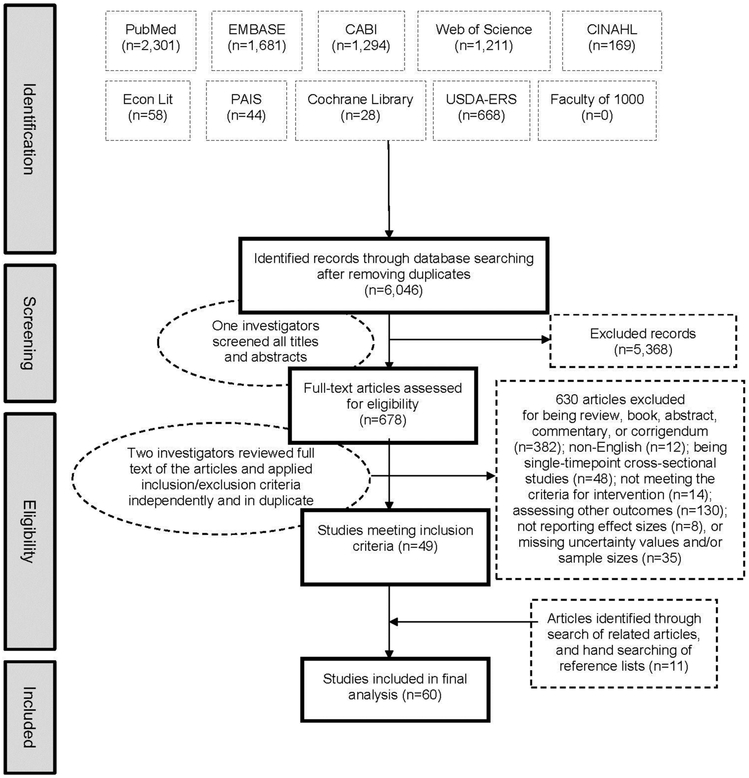
PRISMA guidelines were followed. Ten databases were searched in 2014 for studies published after 1990 evaluating food labeling and consumer purchases/orders, intakes, metabolic risk factors, and industry responses. Data extractions were performed independently and in duplicate. Studies were pooled using inverse-variance random effects meta-analysis. Heterogeneity was explored with I2, stratified analyses, and meta-regression; and publication bias was assessed with funnel plots, Begg’s tests, and Egger’s tests. Analyses were completed in 2017.
Evidence synthesis:
From 6,232 articles, a total of 60 studies were identified including 2 million observations across 111 intervention arms in 11 countries. Food labeling decreased consumer intakes of energy by 6.6% (95% CI= −8.8%, −4.4%, n=31), total fat by 10.6% (95% CI= −17.7%, −3.5%, n=13), and other unhealthy dietary options by 13.0% (95% CI= −25.7%, −0.2%, n=16), while increasing vegetable consumption by 13.5% (95% CI=2.4%, 24.6%, n=5). Evaluating industry responses, labeling decreased product contents of sodium by 8.9% (95% CI= −17.3%, −0.6%, n=4) and artificial trans fat by 64.3% (95% CI= −91.1%, −37.5%, n=3). No significant heterogeneity was identified by label placement or type, duration, labeled product, region, population, voluntary or legislative approaches, combined intervention components, study design, or quality. Evidence for publication bias was not identified.
Conclusions:
From reviewing 60 intervention studies, food labeling reduces consumer dietary intake of selected nutrients and influences industry practices to reduce product contents of sodium and artificial trans fat.
CONTEXT
Poor diet, as a risk factor of obesity and noncommunicable disease, is a leading cause of poor health in the U.S. and globally.1,2 Effective strategies are needed to improve both consumer choices and industry formulations. Food and beverage labeling (food labeling) is increasingly being implemented. Examples include the Nutrition Facts panel,3 menu calorie labels,4–6 “traffic light” labels,7,8 logos such as “Green Keyhole,”9 “Choice,”10 and “Heart-Check,”11 and nutrition or health-related claims.
Although food labeling is widely used and undergoing expansion, early research mostly focused on its influence on consumer attention or awareness, without documenting its effects on actual purchases or intakes.12–21 Currently a growing number of studies have investigated the effects of food labeling on consumer behaviors.22 Yet, the results of the individual studies have been inconsistent, and effectiveness of food labeling remains unclear.23,24 Several reviews provided important insights into labeling,25−28 yet few quantitative meta-analyses have been performed to pool findings across studies, typically focusing on a subset of the evidence, a specific type of label, or a specific dietary target.29–31 From prior scoping reviews,22,23 key gaps were identified in literature including quantitative evidence synthesis of diverse labeling approaches that allows the assessment of overall effects and a comparison of effects of different labeling types.
In addition to effects on consumers, food labeling policies are of interest for effects on industry responses.32,33 For example, experience in the U.S. suggested that mandatory addition of trans fat content to the Nutrition Facts label led to food reformulation.34 Conventional wisdom holds that food labeling could influence industry responses and reformulations, yet such responses have not been systematically reviewed.
This study aims to characterize using a systematic review and meta-analysis the quantitative effects of labeling across multiple approaches, to provide effects estimates, uncertainties, and heterogeneities including stratified analyses, and to assess responses of both consumers and industry. This investigation was performed as part of the Food-PRICE (Policy Review and Intervention Cost-Effectiveness) Project (www.food-price.org).
EVIDENCE ACQUISITION
The authors followed the PRISMA guidelines during all stages of design, implementation, and reporting.35 The study objective, search strategy, and selection criteria were specified in the study protocol (Appendix). This study was not registered in the International Prospective Register of Systematic reviews (PROSPERO) database.
Primary Intervention and Outcomes
Food labeling was evaluated as the primary intervention, characterized as (1) package labeling: all types of standardized provision of nutrition content or healthfulness information on packages, such as nutrient content, nutrition and health-related claims, icons, symbols and logos implemented by government, industry groups or associations, or other non-governmental organizations (i.e., excluding marketing labels developed by individual manufacturers or sellers of the product itself); and (2) menu or other point-of-purchase labeling: standardized provision of nutrition content or healthfulness information at the point-of-purchase including restaurant menus, supermarket or grocery stores, cafeterias, food retail/self-service establishments, and vending machines. Both voluntary and mandatory approaches were included. This study did not include labels only providing ingredient information (e.g., percentage juice), preparation directions, allergen or safety warnings, non-nutritional information (e.g., alcohol content), or ad hoc labeling defined and implemented by individual manufacturers, which were more consistent with nonstandardized marketing. For large-sized printing materials placed adjacent to food/beverage products, careful case-by-case differentiation was made: those denoting the nutrition or healthfulness information of a specific product were included, whereas general dietary health-promoting educational posters and non-nutritional sales-promoting commercial advertisements were excluded.
The outcomes of interests were (1) consumer behaviors, including dietary consumption of labeled foods/beverages and sales/purchases data as proxy measures for consumption; (2) industry responses (i.e., changes in formulations or availabilities of products); and (3) diet-related health measures, including adiposity (e.g., weight, BMI), metabolic risk factors (e.g., blood pressure, serum lipids), and clinical endpoints (e.g., coronary heart disease, diabetes mellitus). This meta-analysis included laboratory studies if foods were ordered and consumed; the meta-analysis excluded cognitive outcomes, such as knowledge, attitudes, or awareness, as well as intended dietary intakes/purchases. Studies had to provide outcome results data that were detailed enough for effective size calculation as specified in the Appendix. Examples of excluding reasons: not reporting sample size of the interested group or arm,36,37 not reporting mean value or its uncertainty of the interested group or arm,38 or both.39–44
Search Strategy
Ten online English databases were systematically searched through February 28, 2014: PubMed, Embase, CABI, Web of Science, CINAHL, EconLit, PAIS, Cochrane Library, U.S. Department of Agriculture Economic Research Service (USDA-ERS), and Faculty of 1000. Search queries included categories on setting (e.g., school, supermarket, restaurant), intervention (e.g., nutrition logo, Nutrition Facts, traffic light), and outcome (e.g., calories, adiposity, coronary heart disease, reformulation). Search terms, dates, and results are provided in the Appendix. Online searches were complemented by hand-searching of reference lists as well as the first 20 “related articles” in PubMed for each included article through May 22, 2015. For all relevant review articles identified through database searches, their reference lists were manually searched. Gray literature was not searched. One investigator screened titles and abstracts. For any potentially relevant articles, full texts were assessed for eligibility by two investigators independently and in duplicate. Discrepancies were resolved by consensus.
Study Selection
This study searched for all intervention studies including natural experiments that assessed the relationship between food labeling and the outcomes and provided an estimate and a measure of uncertainty or sufficient data to calculate these. Articles were excluded if single time point cross-sectional studies, commentaries, reviews, duplicate publications from the same study that did not provide new data, or publications prior to January 1, 1990. Nonrandomized intervention studies having either a pre-/post- or external comparison were included, as each study design has differing strengths and limitations. This included natural experiments with the outcomes assessed over time by cross-sectional sampling.45 This meta-analysis sought to include, as much as possible, investigations that aimed to assess the independent effect of labeling without other major legislative or regulatory interventions, as independently adjudicated by two investigators. Multicomponent interventions were evaluated as a potential source of heterogeneity.
Data Extraction
Two investigators extracted data independently and in duplicate using a standardized electronic format, including: (1) general information (i.e., first author, publication year, study region, design, funding source, site, population setting, consumers demographics), (2) intervention characteristics (i.e., legislation, labeled product, label placement, label type, dietary target, other intervention measures if multicomponent, intervention duration, intervention coverage), and (3) outcome data (i.e., outcome definition, inclusion of compensatory dietary intake outside labeling intervention timeframe, ascertainment method, unit, variable type, sample size, central tendency, uncertainty, and adjusted covariates). Multiple scoring systems are available to assess study quality and risk of bias, without any single accepted standard. This investigation elected to use a previously published scoring system that allows grading across different study designs.46–48 Two investigators independently assessed study quality based on five criteria: study design, assessment of exposure, assessment of outcome, control for confounding, and evidence of selection bias (Appendix Table 1). For each criterion, each study received a score of 0 or 1 (1 being better). A total quality score was calculated by summing individual scores, with 3–5 considered high quality. Discrepancies in data extraction and quality assessment between investigators were resolved by consensus.
Statistical Analysis
The primary outcomes were pooled across labeling interventions. Stratified results were also evaluated based on study design, label types, and placements. The primary outcomes were differences in consumer dietary behaviors and diet-related health outcomes, as well as industry responses in product formulations/availabilities. Continuous outcomes were standardized as percentage differences from either baseline or control groups, based on the study design (Appendix). For categorical outcomes (e.g., percentage of people selecting a specific food item), effect sizes were calculated as the absolute difference of percentages. For outcomes with at least three study estimates reported, study-specific effect sizes were pooled using inverse-variance weighted random effect meta-analysis (metan command in Stata). Uncommon outcomes (two or fewer estimates reported) were pooled together as other healthy options or other unhealthy options based on whether they were recommended to be consumed or avoided by the label (detailed lists of items found in the footnotes for Tables 2, 3, and Appendix Table 12). Heterogeneity was assessed by the I2 statistic. Potential sources of heterogeneity were assessed using meta-regression (metareg command in Stata), including region, design, site, consumers demographics, legislation, label placement and type, labeled product, dietary target, single or multicomponent intervention, duration, intervention coverage, compensatory dietary intake, and quality score. To maximize statistical power and minimize the number of comparisons, meta-regression was only performed for outcomes with ten or more estimates. Publication bias was assessed by visual inspection of funnel plots and Egger’s and Begg’s tests. Analyses were conducted using Stata, version 13.0 with two-tailed α value of 0.05.
Table 2.
Meta-Analyses of Effects of Food Labeling Interventions on Consumer Dietary Behaviors (Continuous Outcomes)a
| Dietary factor | Number of study estimates (individual studies) |
Number of consumers or purchases |
Percent difference with labeling (95% CI)b |
|---|---|---|---|
| Calories | 31 (23) | 43,707 | −6.6 (−8.8. −4.4) |
| Total fat | 13 (12) | 4,409 | −10.6 (−17.7.−3.5) |
| Total carbohydrate | 8 (7) | 1,928 | 2.2 (−5.1, 9.5) |
| Total protein | 6 (5) | 1,110 | 0.6 (−2.8, 4.0) |
| Saturated fat | 5 (5) | 2,227 | −8.4 (−23.7, 6.8) |
| Sodium | 5 (5) | 2,016 | −15.3 (−31.3, 0.7) |
| Vegetables | 5 (5) | 1,497 | 13.5 (2.4.24.6) |
| Fruits | 3 (3) | 1,103 | 10.9 (−16.0, 37.7) |
| Whole grains | 3 (2) | 760 | 14.4 (−11.8, 40.6) |
| Other healthy optionsc | 30 (11) | 2,685 | −0.5 (−2.8, 1.7) |
| Other unhealthy optionsd | 16 (7) | 5,548 | −13.0 (−25.7.−0.2) |
Food labeling (i.e., standardized provision of nutrition or health information) included product package, menu, or other point-of-purchase labeling. Dietary behaviors were evaluated by direct observation (e.g., weighed plate waste) or self-report from single sessions, 24-hour diet recalls, food diaries, or food frequency questionnaires; or as consumer purchases, food outlet sales, or choices/orders as a proxy for consumers’ self-reported dietary intakes. When the same study evaluated both sales/purchase data and consumer intake data, the authors utilized sales/purchase data given its objectivity. Pooled findings prioritizing consumer intake data for these studies were not appreciably different (Appendix Table 12). Appendix Figures 1–18 show individual forest plots and more details on each meta-analysis. Results stratified by consumer intake vs purchases/sales are also available but not shown.
Based on the units reported in the study (e.g., most commonly kcal for calories, gram or percent energy for dietary fats, servings or g/d for foods, etc).
Items recommended by labels to consume, such as salads, soups, low-fat dairy, lean meat, low-fat desserts, fish and seafood, water, diet soda, and foods higher in dietary fiber, vitamin C, and calcium.
Items recommended by labels to avoid, such as sugar-sweetened beverages, alcoholic beverages, non-alcoholic caloric beverages, French fries, potatoes, white bread, and foods higher in saturated fat, trans fat, added sugars or sodium.
Table 3.
Meta-Analyses of Effects of Food Labeling Interventions on Consumer Dietary Behaviors (Categorical Outcomes)a
| Dietary factor | Number of study estimates (individual studies) |
Number of consumers or purchases |
Percent change with labeling (95% CI)b |
|---|---|---|---|
| Green options (traffic light system) | 3 (3) | 1,970,452 | 1,9 (1.8, 2.0) |
| Amber options (traffic light system) | 3 (3) | 1,970,452 | 0.4 (0.3, 0.5) |
| Red options (traffic light system) | 3 (3) | 1,970,452 | −2.3 (−2.4. −2.2) |
| Other healthy optionsc | 16 (11) | 42,126 | 6.1 (2.6, 9.5) |
| Other unhealthy optionsd | 22 (10) | 33,990 | −0.9 (−4.6, 2.8) |
Food labeling (i.e., standardized provision of nutrition or health information) includes product package, menu, or other point-of-purchase labeling. Dietary behaviors in these studies were evaluated as consumer purchases, food outlet sales, or choices/orders. Appendix Figure 19 shows individual forest plots and more details on each meta-analysis.
The absolute difference in percentages of consumers or purchases making a certain selection.
Items recommended by labels to consume, such as green salad, “healthy items” not otherwise specified, low-fat items, low-sodium items, moderately nutrient-dense snacks, and high nutrient-dense snacks.
Items recommended by labels to avoid, such as sugar-sweetened beverages, large portion size sugar-sweetened beverages, caloric beverages, desserts, French fries, added cheese to hamburgers/sandwiches, full-fat meals or foods, high calorie meals, high saturated fat meals, high sodium meals, low vegetable content meals, and low nutrient-dense snacks.
EVIDENCE SYNTHESIS
Study Characteristics
From 5,378 identified abstracts, 668 USDA-ERS websites, and 186 full-text articles identified from hand searching of reference lists and related articles in PubMed, 60 studies from 59 articles met inclusion criteria, comprising 2,078,043 unique observations (consumers, receipts, purchases) across 111 intervention arms (Figure 1). These included 16 randomized49–64 and 44 nonrandomized45,65–106 intervention studies conducted in 11 countries across four continents (Table 1, Appendix Tables 3–11). The majority included both sexes, and most evaluated adults. Populations of a range of SES were evaluated. A total of 60.0% of studies had high quality scores of ≥3.
Figure 1.
Screening and selection process for intervention studies evaluating food labeling effects on consumer diet behaviors and industry practices.
Table 1.
Summary of 60 Interventional Trials Evaluating the Effectiveness of Food and Menu Labeling on Consumer and Industry Behaviora
| Study characteristics | RCTs (n=16) |
Interventions with external controls (n=23) |
Interventions with pre/post comparisons (n=21) |
All studies (n=60) |
|---|---|---|---|---|
| Region | ||||
| U.S./Canada | 12 (75.0) | 17 (73.9) | 14 (66.7) | 44 (73.3) |
| Europe/Australia | 4 (25.0) | 5 (21.7) | 5 (23.8) | 14 (23.3) |
| Asia | 0 (0.0) | 1 (4.3) | 1 (4.8) | 2 (3.3) |
| Siteb,c | ||||
| Cafeterias | 3 (18.8) | 6 (26.1) | 5 (23.8) | 14 (23.3) |
| Restaurants | 1 (6.3) | 8 (34.8) | 8 (38.1) | 17 (28.3) |
| Supermarkets/Shops/Vending | 2 (12.5) | 6 (26.1) | 7 (33.3) | 15 (25.0) |
| Labs | 10 (62.5) | 3 (13.0) | 0 (0.0) | 13 (21.7) |
| Multiple food establishments | 0 (0.0) | 0 (0.0) | 1 (4.76) | 1 (1.7) |
| Not reported | 0 (0.0) | 0 (0.0) | 3 (14.3) | 3 (5.0) |
| Population setting | ||||
| University/School | 7 (43.8) | 3 (13.0) | 5 (23.8) | 15 (25.0) |
| Hospital/Worksite | 2 (12.5) | 5 (21.7) | 5 (23.8) | 12 (20.0) |
| Community/Recreationald | 7 (43.8) | 15 (65.2) | 11 (52.4) | 33 (55.0) |
| Mean age, yearse | 29.7 (21.8, 44.2) | 30.1 (19.7, 50.1) | 21 (21.0, 21.0) | 29.5 (19.7, 50.1) |
| Sex, % mene | 40.2 (0.0, 62.0) | 42.3 (0.0, 100.0) | 41.8 (0.0, 70.0) | 41.2 (0.0, 100.0) |
| Racef | ||||
| Mostly white | 7 (43.8) | 2 (8.7) | 2 (9.5) | 11 (18.3) |
| Black or mostly black | 0 (0.0) | 4 (17.4) | 2 (9.5) | 6 (10.0) |
| Mostly Asian or Hispanic | 0 (0.0) | 2 (8.7) | 0 (0.0) | 2 (3.3) |
| Mixed | 1 (6.3) | 0 (0.0) | 1 (4.8) | 2 (3.3) |
| Not reported or not applicable | 8 (50.0) | 15 (65.2) | 16 (76.2) | 39 (65.0) |
| SESf | ||||
| High or mostly high | 6 (37.5) | 0 (0.0) | 0 (0.0) | 6 (10.0) |
| Mixed | 8 (50.0) | 5 (21.7) | 4 (19.0) | 17 (28.3) |
| Low or mostly low | 1 (6.3) | 7 (30.4) | 4 (19.0) | 12 (20.0) |
| Other or not reported | 1 (6.3) | 11 (47.8) | 13 (61.9) | 25 (41.7) |
| Label placementc | ||||
| Menu | 5 (31.3) | 11 (47.8) | 7 (33.3) | 23 (38.3) |
| Package | 4 (25.0) | 2 (8.7) | 7 (33.3) | 13 (21.7) |
| Other point-of-purchase | 3 (18.8) | 8 (34.8) | 7 (33.3) | 18 (30.0) |
| Not reported | 4 (25.0) | 4 (17.4) | 3 (14.3) | 11 (18.3) |
| Labeled informationc | ||||
| Content quantity | 10 (62.5) | 14 (60.9) | 14 (66.7) | 38 (63.3) |
| Content claim or health claim | 9 (56.3) | 4 (17.4) | 3 (14.3) | 16 (26.7) |
| Logo | 4 (25.0) | 7 (30.4) | 2 (9.5) | 13 (21.7) |
| Grading system | 2 (12.5) | 3 (13.0) | 4 (19.0) | 9 (15.0) |
| Physical activity equivalent | 1 (6.3) | 0 (0.0) | 2 (9.5) | 3 (5.0) |
| Labeled product | ||||
| Meals | 7 (43.8) | 15 (65.2) | 10 (47.6) | 32 (53.3) |
| Single foods/beverages | 6 (37.5) | 3 (13.0) | 3 (14.3) | 12 (20.0) |
| Multiple | 3 (18.8) | 5 (21.7) | 8 (38.1) | 16 (26.7) |
| Dietary targetc | ||||
| Calories | 9 (56.3) | 17 (73.9) | 12 (57.1) | 38 (63.3) |
| Nutrients | 11 (68.8) | 15 (65.2) | 14 (66.7) | 40 (66.7) |
| Food or beverage items | 2 (12.5) | 4 (17.4) | 2 (9.5) | 8 (13.3) |
| Not reported | 0 (0.0) | 0 (0.0) | 2 (9.5) | 2 (3.3) |
| Intervention duration, weeksg | 3.4 (0.1, 26.0) | 53.2 (0.1, 364.0) | 93.6 (1.0, 468.0) | 69.8 (0.1, 468.0) |
| Label mandated by law | 0 (0.0) | 6 (26.1) | 8 (38.1) | 14 (23.3) |
| Nationwide implementation | 0 (0.0) | 1 (4.3) | 5 (23.8) | 6 (10.0) |
| Additional intervention componentsc | ||||
| None (single component) | 12 (75.0) | 16 (69.6) | 18 (85.7) | 46 (76.7) |
| Education | 2 (12.5) | 1 (4.3) | 0 (0.0) | 3 (5.0) |
| Mass media campaign | 1 (6.3) | 4 (17.4) | 1 (4.8) | 6 (10.0) |
| Economic incentives | 2 (12.5) | 2 (8.7) | 0 (0.0) | 4 (6.7) |
| Direct regulation | 1 (6.3) | 4 (17.4) | 3 (14.3) | 8 (13.3) |
| Outcomes evaluatedc | ||||
| Calories | 7 (43.8) | 12 (52.2) | 7 (33.3) | 26 (43.3) |
| Nutrients | 7 (43.8) | 6 (26.1) | 6 (28.6) | 19 (31.7) |
| Food or beverage items | 9 (56.3) | 11 (47.8) | 13 (61.9) | 33 (55.0) |
| Cardiovascular risk factors | 2 (12.5) | 3 (13.0) | 0 (0.0) | 5 (8.3) |
| Other | 0 (0.0) | 1 (4.3) | 2 (9.5) | 3 (5.0) |
| Outcome typec | ||||
| Sales | 2 (12.5) | 5 (21.7) | 4 (19.0) | 11 (18.3) |
| Purchases (or ordersh) | 9 (56.3) | 7 (30.4) | 8 (38.1) | 24 (40.0) |
| Consumption | 11 (68.8) | 10 (43.5) | 3 (14.3) | 24 (40.0) |
| Availability | 0 (0.0) | 1 (4.3) | 2 (9.5) | 3 (5.0) |
| Reformulation content | 0 (0.0) | 2 (8.7) | 4 (19.0) | 6 (10.0) |
| Adiposity | 1 (6.3) | 1 (4.3) | 0 (0.0) | 2 (3.3) |
| Cardiovascular biomarker | 1 (6.3) | 1 (4.3) | 2 (9.5) | 4 (6.7) |
| Fundingc | ||||
| Academic | 7 (43.8) | 7 (30.4) | 2 (9.5) | 16 (26.7) |
| Government | 3 (18.8) | 14 (60.9) | 4 (19) | 21 (35.0) |
| Other non-profit | 2 (12.5) | 4 (17.4) | 9 (42.9) | 15 (25.0) |
| Industry | 1 (6.3) | 1 (4.3) | 0 (0.0) | 2 (3.3) |
| Not reported | 4 (25.0) | 7 (30.4) | 9 (42.9) | 20 (33.3) |
| Quality score, range 0-5i | 4.5 (3.0, 5.0) | 2.2 (0.0, 4.0) | 2.4 (0.0, 4.0) | 2.9 (0.0, 5.0) |
Values are number of studies (percent) for categorical variables and mean (range) for continuous variables. Values may not sum to 100% due to rounding. Details on each of the 60 individual studies are provided in Appendix Tables 3–11.
Study site: Cafeterias=canteen, dining hall, mess hall, kitchen; restaurants=fast food restaurants, carry-out restaurants, full-service restaurants, food outlets; labs or laboratories=classrooms, church rooms or other places serving other purposes rather than real food establishments.
Because multiple responses possible for each study, proportions may sum to greater than 100%.
Setting: Recreation facility=cinema, gym, swimming pool.
Missing values: RCTs: 5 did not report mean age, 3 did not report % males; interventional trials with external controls: 10 did not report mean age, 7 did not report % males; interventional trials with per/post comparisons: 20 did not report mean age, 8 did not report % males.
Population characteristics of the studied sample: not applicable (N/A) to reformulation or availability outcomes. Primary race is defined as ≥50% of the population; SES defined as primarily high: >50% of post-grad education, or high income; primarily low:>50% of blue collar, low income or did not finish college. Otherwise for articles directly reporting the SES status, this study cited the authors’ SES category.
Intervention duration: time from the implementation of food labeling to the time of outcome assessment in weeks. Studies conducted in single sessions were assigned value 0.1. One interventional trial with external control did not report duration.
Orders were evaluated largely in laboratory settings, where meals were selected but not paid for. This study only included interventional studies in laboratory settings which evaluated the actual provision or serving of foods/beverages ordered, not theoretical orders.
Calculated based on 5 criteria (Appendix Table 1), each coded as either 0 or 1 and with values summed. The total score could range from 0 to 5, with 3-5 considered as higher quality.
Most studies evaluated intakes of specific products or meals as outcomes, rather than long-term (habitual) intakes. About half were performed in general community,45,52,53,55–58,61,71–81,84,85,90–93,97,98,101,103–106 and half in universities/schools49,54,59,60,62–64,70,83,88,89,99,100,102 or hospitals/other worksites50,51,65–69,86,87,94–96 (Table 1). Overall across these population settings, sites of interventions were relatively evenly divided between cafeterias,49–51,65–70,86–90 restaurants,45,52,71–77,90–97 supermarkets/shops/vending machines,53,54,78–82,96–103 and laboratories (mostly in RCTs).55–63,83,84 Label placements included packages (21.7%),55,58,60,63,66,80,87,97,98,103–106 menus (38.3%), 45,49,52,56,57,61,66–68,71–77,87,90–92,94,95,101 and other point-of-purchase (on shelf, vending machines, posters; 30.0%).53,54,62,66,69,70,78,79,81,82,84,87,88,96,99–102 The various label approaches were categorized into five types: content quantity, nutrition or health-related claims, logos, grading systems, and physical activity equivalents (Appendix Table 2). Most labels targeted total energy or specific nutrients.
Across all studies, the average intervention duration was 69.8 weeks (range, 3 days to 9 years), except for laboratory studies, which were typically conducted over one to three sessions. In 14 studies, food labeling was combined with other components such as education, mass media campaigns, economic incentives, or direct regulation (restrictions, bans, requirements of the contents or availabilities of certain nutrients or food/beverage items).50,53,54,59,68,69,71,78,79,81,85,86,96,102 Most studies were funded by nonprofit sources including government, academic institutions, or other organizations; two studies received financial support from both government and industry sources.60,65
Consumer Behaviors
In pooled analyses (Table 2), food labeling reduced intakes of energy by 6.6% (95% CI= −8.8%, −4.4%. n=31 estimates; Appendix Figures 1 and 2), total fat by 10.6% (95% CI= −17.7%, −3.5%, n=13; Appendix Figures 3 and 4), and other unhealthy options by 13.0% (95% CI= −25.7%, −0.2%, n=16). Food labeling increased vegetable consumption by 13.5% (95% CI=2.4%, 24.6%, n=5; Appendix Figures 13 and 14). A borderline, nonstatistically significant reduction was seen for sodium (−15.3%, 95% CI= −31.3%, 0.7%, n=5; Appendix Figures 11 and 12). Labeling did not significantly alter intakes of other dietary targets including total carbohydrate (Appendix Figures 5 and 6), protein (Appendix Figures 7 and 8), saturated fat (Appendix Figures 9 and 10), fruits (Appendix Figure 15 and 16), whole grains (Appendix Figures 17 and 18), or other healthy options.
Several studies reported both objective sales/purchase data and self-reported intake data for total energy (n=5),49,56,57,61,70 total fat (n=3),49,57,70 total carbohydrate (n=2),49,57 total protein (n=2),49,57 and saturated fat (n=1).57 Pooled results prioritizing either sales/purchase or intake data from these studies did not materially alter the results (Table 2 versus Appendix Table 12).
In studies evaluating traffic light systems that included three tiers (Table 3), labeling increased the selections of healthier green (+1.9%, 95% CI=1.8%, 2.0%) and mid-level (+0.4%, 95% 0=0.3%, 0.5%) options, and reduced selection of less healthy red options (−2.3%, 95% CI= −2.4%, −2.2%; Appendix Figure 19). Evaluated in two tiers, food labeling significantly altered the percentage of healthier options selected (+6.1%, 95% 0=2.6%, 9.5%, n=16 estimates), but not unhealthy options (−0.9%, 95% CI= −4.6%, 2.8%, n=22).
Adiposity, Metabolic Risk Factors, and Clinical Endpoints
Very few studies evaluated adiposity (n=2)50,85 or metabolic risk factors (n=4).50,85,103,104 Because of heterogeneity across the outcomes in these studies, quantitative meta-analysis could not be performed. No identified studies evaluated disease endpoints.
Industry Responses
Reformulation outcomes were evaluated by six studies (Appendix Table 13, Appendix Figures 20–24). Food labeling significantly reduced the contents of trans fat (−64.3%, 95% CI= −91.1%, −37.5%, n=3) and sodium (−8.9%, 95% CI= −17.3%, −0.6%, n=4). Significant effects were not identified on product contents of total energy, saturated fat, dietary fiber, or other healthy (protein and unsaturated fat) or unhealthy (total fat, sugar, and dietary cholesterol) dietary components. Few studies evaluated changes in product availability (n=3),74,89,96 with heterogeneity in these studies precluding pooling.
Exploration of Heterogeneity
Statistical heterogeneity was seen in many of the pooled analyses. In univariate meta-regression, the authors explored whether the effectiveness of labeling varied depending on underlying population and labeling characteristics (Appendix Table 14). Given multiple comparisons, the focus was on potential interactions with pinteraction<0.01. Findings were similar when stratified by interventional designs (randomized, nonrandomized), label placements (menu, package, other point-of-purchase), or label types (Appendix Tables 15, 16). Interventions of longer duration observed larger effects of labeling on consumer intake of total fat (pinteraction<0.01), but not on total energy intake. No significant heterogeneity was identified by world region, study design, population, age, sex, race, SES, type of intervention site, labeled products, voluntary or mandatory labeling, presence of other intervention components, inclusion of compensatory intake, or study quality score (pinteraction>0.01 each).
Publication Bias
Visual inspection of funnel plots suggested potential publication bias for lower intake of total energy and total fat, but not for other outcomes (Appendix Figures 25–27). Neither Begg’s test nor Eggers test identified significant evidence for publication bias (p>0.05 each).
DISCUSSION
In this systematic review and meta-analysis of 60 studies including 111 intervention arms and more than 2 million observations across 11 countries, food labeling reduced consumer consumption of total energy and total fat, while increasing consumption of vegetables. Food labeling did not significantly alter consumer intakes of other dietary targets including sodium, total carbohydrate, protein, saturated fat, fruits, or whole grains. This meta-analysis also found that food labeling altered industry formulations for sodium and trans fat, but did not significantly affect product formulations for total energy, saturated fat, dietary fiber, or other healthy/unhealthy dietary components. To the authors’ knowledge, this is the first systematic assessment of the quantitative effects of diverse types of food labeling strategies on both consumers’ dietary intakes and health outcomes, and industry responses.
In the past two decades, various types of food labeling have been developed, with the initial efforts mostly focusing on packaged foods. In the U.S., the 1990 Nutrition Labeling and Education Act mandated the placement of the Nutrition Facts panel on packaged foods and the use of the Food and Drug Administration-authorized nutrient-content and health claims.107 Later that decade, the Dietary Supplement Health and Education Act and Food and Drug Administration Modernization Act established requirements and procedures for other claims, including structure/function, general well-being and nutrient deficiency claims, as well as claims based on “authoritative statements” from scientific bodies.107,108 In 1989, Sweden created The Keyhole logo, which later became a common Nordic label by expanding to Denmark and Norway in 2009 and Iceland in 2013.109–111 However, many manufacturers of eligible products choose not to add this voluntary label, and the Swedish National Food Agency is planning an investigation into the causes of the low uptake.112 The Netherlands Choice logo was launched in 2006 on products containing higher fiber and lower sodium, added sugar, saturated fat, trans fat, and total energy110,113,114 and has been implemented in Belgium, Poland, the Czech Republic, Argentina, and Nigeria.115 With mounting criticism especially that consumers found the Choice logo confusing,116 the Dutch government in 2016 ordered it to be replaced with a cellphone app.117 In 2006, the United Kingdom Food Standards Agency recommended a voluntary front-of-pack traffic-light labeling system to highlight contents of total fat, saturated fat, sugar, and sodium in selected food categories.7,118 In 2015, Chile launched a comprehensive black warning logo program, informing consumers of foods higher in sugar, saturated fat, salt, or energy.119 Other new front-of-pack labels include the Heart Symbol in Finland120; the Health Star Ratings121 and the Pick the Tick logo122,123 in Australia and New Zealand; and Nuval,124 Guiding Stars,125 Smart Choices,126 and Heart-Check127 in the U.S. More recently, the labeling in restaurants and cafeterias has been increasingly considered,5,128 especially after the 2010 Patient Protection and Affordable Care Act required restaurant chains with 20 or more locations to list calorie counts of standard menu items.4
Although the aim of these extensive labeling efforts is to help consumers make informed and healthier choices, and potentially influence manufacturer and restaurant offerings, evidence on these effects had been relatively sparse. Previous systematic reviews and meta-analyses primarily concentrated on a specific type of labels or a specific dietary target, with inconsistent results. Several meta-analyses on effectiveness of menu labeling on total energy intake reported inconsistent findings.29,30,129,130 In one analysis, health-related claims were found to increase consumption and purchases of the labeled products.31 A pooled analysis of nine trials found that labeling systems increased selection of healthier products, but did not alter energy intake.131 In a meta-analysis of 14 studies, menu labeling did not significantly alter intakes of carbohydrate, total fat, saturated fat, sodium, or energy consumed among U.S. adults.132 Most recently, an analysis of 28 studies concluded that evidence was inconclusive for effectiveness of various types of labeling.133 The present investigation builds upon and extends the prior evidence by including more studies, more comprehensive types of labeling, and both consumer and industry responses. This allowed new confirmation of significant effects of labeling on consumer intakes and orders of total energy, total fat, and vegetables, and industry formulations of sodium and trans fat.
This meta-analysis identified no significant effects of labeling on several other consumer and industry targets. Because many of these analyses included fewer studies and the nonsignificant results were often in expected directions, these findings demonstrate a need for additional investigation of these and other specific dietary targets. It is also possible that those dietary outcomes are not the primary targets of the labels, for example most of the labels investigated targeted energy calories and it is questionable if such labels would shift whole grain intake. Alternatively, for certain choices labeling alone may be ineffective. Many barriers exist to consumers responses to labeling, such as limited awareness,12 attention,134 understanding,135 attitude,136 acceptance,137 usage,138 or other challenges such as price, taste, and culture.32,139,140 Other complementary approaches may be crucial, such as choice architecture, economic incentives, novel technologies, mass media campaigns, quality standards, neighborhood environment, and organizational innovations in schools, worksites, and communities.22,23,47,48,141 This meta-analysis also calls for future investigations about the effectiveness of food labeling for improving health outcomes and disease risk factors, because there has been evidence that selecting label-recommended products is associated with lower cardiometabolic syndrome risk.142
It has been proposed that an ideal label should use a simple, interpretative, and standardized symbol, with consistent format and location.32 Other proposals have favored rating systems, such as the traffic light or Health Star Ratings.33, 137, 143 This study did not identify consistent differential effects according to label type, placement, intervention duration, or mandatory versus voluntary labeling. This suggests that varieties of labeling may be less quantitatively relevant than the general presence or absence of information to consumers. Other potential sources of heterogeneity were also not significant, although the numbers of studies may limit the statistical power of such assessments.
Food labeling is a dynamic and evolving policy issue, with industry regularly reformulating or eliminating products to meet mandatory or voluntary guidelines. Among the seven dietary factors evaluated, significant industry responses to labeling were seen only for sodium and trans fat. Of note, industrial additives constitute the predominant dietary sources of these two components,144–146 which can be added to or removed from otherwise similar foods or meals. This suggests that industry responses to labeling may be greatest for additives, compared with intrinsic components of foods, such as macronutrients or energy. With recent efforts in many countries on labeling of added sugars, it will be important to evaluate whether such labeling influences the industry use of this additive. These findings highlight the relative paucity of data in this area.
This meta-analysis did not identify a consistent gradient in responses by SES, age, or sex. This is contrasted to prior reports based on smaller samples, suggesting that these factors may modify the labeling efficacy.22,32 Yet, although this meta-analysis represents the most comprehensive assessment of these questions to date, only 35 studies (58%) reported socioeconomic information which were defined based on various factors (education, income, etc.). Clearly, the determinants of potentially varying effects of labeling require further studies, and conventional wisdom on modifying effects of population demographics should not be considered a tautology.
This meta-analysis has several strengths. The searches were conducted in multiple databases and citation lists and related articles were manually reviewed, reducing the likelihood of missing multiple or large studies. Inclusion decisions and data extractions were performed independently and in duplicate, reducing potential for errors and bias. A wide range of labels and outcomes were evaluated, increasing its generalizability and making heterogeneity assessment possible. Hypothetical outcomes like purchase intention were excluded, resulting in findings more reflective of real-world behaviors. By including both purchase/sales and consumption results as well as analyzing them separately and altogether, this meta-analysis demonstrated consistent findings across these methods while also increasing the numbers of included studies. Several potential sources of heterogeneity were explored with greater statistical power than previously possible. Finally, responses of both consumers and industry were evaluated, providing complementary information on relevance of labeling efforts.
Limitations
Limitations should be considered. The interventions and settings were extremely heterogeneous, and although the authors carefully documented and explored potential sources of variation, there are likely remaining differences modifying effectiveness. All studies were interventional, yet many were not randomized; conversely, many of the nonrandomized interventions were natural experiments, increasing generalizability.147 Nearly one quarter of the interventions combined other components, although no evidence was found that these studies had larger effect sizes. Some studies could not be included because of the absence of reported uncertainty or sample size. Searches were performed through 2015, and several newer studies have been published. Given the number of studies already included in the meta-analysis, it is unclear whether the addition of a few new studies would greatly alter many of the conclusions, which can be tested in future updates to this work. In addition, although some recent studies not included here assessed front-of-pack grading systems, such as Health Star Ratings in Australia/New Zealand and NutriScore in France, findings of these studies have been inconsistent148–150 and often evaluated knowledge or attitudes rather than actual purchasing or consumption.151
CONCLUSIONS
From the results of 60 intervention studies, food labeling effectively reduces consumer intakes of total energy and total fat while increasing intake of vegetables. Food labeling also influences industry responses related to product contents of sodium and artificial trans fat. More studies are needed to assess the effects of labeling on other dietary targets, disease risk factors, and clinical endpoints.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank all the collaborators and advisory groups in the Food-PRICE (Policy Review and Intervention Cost-Effectiveness) project.
This research was supported by the National Heart, Lung, and Blood Institute, NIH (R01 HL115189, PI Mozaffarian; R01 HL130735, PI Micha). Dr. Imamura was supported by MRC Epidemiology Unit core funding (MC_UU_12015/5). The funding sources have no role in the design, execution, analyses, data interpretation or the decision to submit results of this study. No financial disclosures were reported by other authors of this paper.
Footnotes
The dataset was curated from published sources, cited herein. Full statistical code available from the first author at sysgserene@gmail.com.
Dr. Mozaffarian reports funding from NIH and the Bill and Melinda Gates Foundation; personal fees from GOED, DSM, Nutrition Impact, Pollock Communications, Bunge, Indigo Agriculture, Amarin, Acasti Pharma, and America’s Test Kitchen; scientific advisory board, Omada Health, Elysium Health, and DayTwo; and chapter royalties from UpToDate; all outside the submitted work. Dr. Micha reports funding from the Bill and Melinda Gates Foundation, Unilever, personal fees from World Bank; all outside the submitted work. Dr. Smith completed the majority of the work related to this manuscript while a research fellow at the Harvard T.H. Chan School of Public Health. All the other authors declare no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Benziger CP, Roth GA, Moran AE. The Global Burden of Disease Study and the preventable burden of NCD. Glob Heart. 2016;11(4):393–397. 10.1016/j.gheart.2016.10.024. [DOI] [PubMed] [Google Scholar]
- 2.Micha R, Penalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912–924. 10.1001/jama.2017.Q947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.FDA. Changes to the Nutrition Facts Label. www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm385663.htm. Published 2018. Accessed June 18, 2018.
- 4.Food labeling; nutrition labeling of standard menu items in restaurants and similar retail food establishments. Final rule. Fed Regist. 2014;79(230):71155–71259. [PubMed] [Google Scholar]
- 5.Johnson DB, Payne EC, McNeese MA, Allen D. Menu-labeling policy in King County, Washington. Am J Prev Med. 2012;43(3 suppl 2):S130–S135. 10.1016/j.amepre.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 6.Fox M New menu labeling requirements: academy advocacy expands opportunities. J Acad Nutr Diet. 2015;115(5):707–708. 10.1016/j.jand.2015.03.005. [DOI] [PubMed] [Google Scholar]
- 7.BMRB Social Research. Comprehension and use of UK nutrition signpost labelling schemes: scientific rationale and design. http://webarchive.nationalarchives.gov.Uk/20120403230459/http://www.food.gov.uk/multimedia/pdfs/quantrationale.pdf. Published 2008. Accessed September 30, 2018.
- 8.Food Standards Agency. Guide to creating a front of pack (FoP) nutrition label for pre-packed products sold through retail outlets. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/566251/FoP_Nutrition_labelling_UK_guidance.pdf. Published 2016. Accessed September 30, 2018.
- 9.Livsmedelsverket. The Keyhole, www.livsmedelsverket.se/en/food-and-content/labelling/nyckelhalet/. Published 2015. Accessed June 18, 2018.
- 10.Dotsch-Klerk M, Jansen L. The Choices programme: a simple, front-of-pack stamp making healthy choices easy. Asia Pac J Clin Nutr. 2008;17(suppl 1):383–386. [PubMed] [Google Scholar]
- 11.American Heart Association. Heart-Check Food Certification Program Nutrition Requirements. www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Heart-CheckMarkCertification/Heart-Check-Food-Certification-Program-Nutrition-Requirements_UCM_300914_Article.jsp. Published 2018. Accessed June 18, 2018.
- 12.Dumanovsky T, Huang CY, Bassett MT, Silver LD. Consumer awareness of fast-food calorie information in New York City after implementation of a menu labeling regulation. Am J Public Health. 2010;100(12):2520–2525. 10.2105/AJPH.2010.191908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Herpen E, van Trijp HCM. Front-of-pack nutrition labels. Their effect on attention and choices when consumers have varying goals and time constraints. Appetite. 2011;57(1):148–160. 10.1016/i.appet.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 14.Miller LM, Cassady DL. Making healthy food choices using nutrition facts panels. The roles of knowledge, motivation, dietary modifications goals, and age. Appetite. 2012;59(1): 129–139. 10.1016/i.appet.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonsmann SS, Celemin LF, Grunert KG. Food labelling to advance better education for life. Eur J Clin Nutr. 2010;64(suppl 3):S14–S19. 10.1038/ejcn.2010.204. [DOI] [PubMed] [Google Scholar]
- 16.Koenigstorfer J, Wasowicz-Kirylo G, Stysko-Kunkowska M, Groeppel-Klein A. Behavioural effects of directive cues on front-of-package nutrition information: the combination matters! Public Health Nutr. 2014;17(9):2115–2121. 10.1017/S136898001300219X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Institute of Medicine. Examination of Front-of-Package Nutrition Rating Systems and Symbols: Phase 1 Report. Washington, DC: The National Academies Press; 2010. [PubMed] [Google Scholar]
- 18.Westcombe A, Wardle J. Influence of relative fat content information on responses to three foods. Appetite. 1997;28(1):49–62. 10.1006/appe.1996.0066. [DOI] [PubMed] [Google Scholar]
- 19.Grimes CA, Riddell LJ, Nowson CA. Consumer knowledge and attitudes to salt intake and labelled salt information. Appetite. 2009;53(2): 189–194. 10.1016/i.appet.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 20.Grunert KG, Fernandez-Celemin L, Wills JM, Bonsmann SSG, Nureeva L. Use and understanding of nutrition information on food labels in six European countries. J Public Health. 2010;18(3):261–277. 10.1007/s10389-009-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lewis JE, Arheart KL, LeBlanc WG, et al. Food label use and awareness of nutritional information and recommendations among persons with chronic disease. Am J Clin Nutr. 2009;90(5):1351–1357. 10.3945/ajcn.2009.27684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mozaffarian D, Afshin A, Benowitz NL, et al. Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation. 2012;126(12): 1514–1563. 10.1161/CIR.0b013e318260a20b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Afshin A, Penalvo J, Del Gobbo L, et al. CVD prevention through policy: a review of mass media, food/menu labeling, taxation/subsidies, built environment, school procurement, worksite wellness, and marketing standards to improve diet. Curr Cardiol Rep. 2015; 17(11): 98 10.1007/s11886-015-0658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seymour JD, Yaroch AL, Serdula M, Blanck HM, Khan LK. Impact of nutrition environmental interventions on point-of-purchase behavior in adults: a review. Prev Med. 2004;39(suppl 2):S108–S136. 10.1016/j.ypmed.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 25.Downs SM, Thow AM, Leeder SR. The effectiveness of policies for reducing dietary trans fat: a systematic review of the evidence. Bull World Health Organ. 2013;91(4):262–269. 10.2471/BLT.12.111468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campos S, Doxey J, Hammond D. Nutrition labels on pre-packaged foods: a systematic review. Public Health Nutr. 2011;14(8):1496–1506. 10.1017/S1368980010003290. [DOI] [PubMed] [Google Scholar]
- 27.Swartz JJ, Braxton D, Viera AJ. Calorie menu labeling on quick-service restaurant menus: an updated systematic review of the literature. Int J Behav Nutr Phys Act. 2011;8:135 10.1186/1479-5868-8-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kanter R, Vanderlee L, Vandevijvere S. Front-of-package nutrition labelling policy: global progress and future directions. Public Health Nutr. 2018;21(8): 1399–1408. 10.1017/S1368980018000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sinclair SE, Cooper M, Mansfield ED. The influence of menu labeling on calories selected or consumed: a systematic review and meta-analysis. J Acad Nutr Diet. 2014;114(9): 1375–1388. 10.1016/j.jand.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 30.Long MW, Tobias DK, Cradock AL, Batchelder H, Gortmaker SL. Systematic review and meta-analysis of the impact of restaurant menu calorie labeling. Am J Public Health. 2015;105(5):e11–e24. 10.2105/AJPH.2015.302570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kaur A, Scarborough P, Rayner M. A systematic review, and meta-analyses, of the impact of health-related claims on dietary choices. Int J Behav Nutr Phys Act. 2017;14:93 10.1186/s12966-017-0548-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lichtenstein AH. 2013 FAO/WHO workshop presentation: IOM Report on Front-of-Package Nutrition Rating Systems and Symbols. www.who.int/nutrition/events/2013_FAQ_WHO_workshop_frontofpack_nutritionlabelling_presentation_Lichtenstein.pdf. Published 2013. Accessed February 26, 2017.
- 33.NICE (National Institute For Health And Care Excellence). NICE Guidance: Cardiovascular disease prevention, www.nice.org.uk/guidance/PH25/chapter/1-Recommendations. Published 2010. Accessed February 26, 2017.
- 34.Mozaffarian D, Jacobson MF, Greenstein JS. Food reformulations to reduce trans fatty acids. N Engl J Med. 2010;362(21): 2037–2039. 10.1056/NEJMc1001841. [DOI] [PubMed] [Google Scholar]
- 35.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wisdom J, Downs JS, Loewenstein G. Promoting healthy choices: information versus convenience. Am Econ J Appl Econ. 2010;2(2): 164–178. 10.1257/app.2.2.164. [DOI] [Google Scholar]
- 37.Ellison B, Lusk JL, Davis D. Looking at the label and beyond: the effects of calorie labels, health consciousness, and demographics on caloric intake in restaurants. Int J Behav Nutr Phys Act. 2013;10:21 10.1186/1479-5868-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tandon PS, Zhou C, Chan NL, et al. The impact of menu labeling on fast-food purchases for children and parents. Am J Prev Med. 2011;41(4):434–438. 10.1016/j.amepre.2011.06.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: a first look at the effects on low-income people in New York City. Health Aff (Millwood). 2009;28(6):w1110–w1121. 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 40.Elbel B, Mijanovich T, Dixon LB, et al. Calorie labeling, fast food purchasing and restaurant visits. Obesity (Silver Spring). 2013;21(11):2172–2179. 10.1002/oby.20550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bollinger B, Leslie P, Sorensen A. Calorie posting in chain restaurants. Am Econ J Econ Policy. 2011. ;3(1):91–128. 10.1257/po1.3.1.91. [DOI] [Google Scholar]
- 42.Holmes AS, Serrano EL, Machin JE, Duetsch T, Davis GC. Effect of different children’s menu labeling designs on family purchases. Appetite. 2013;62:198–202. 10.1016/j.appet.2012.05.029. [DOI] [PubMed] [Google Scholar]
- 43.Pulos E, Leng K. Evaluation of a voluntary menu-labeling program in full-service restaurants. Am J Public Health. 2010;100(6): 1035–1039. 10.2105/AJPH.2009.174839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Finkelstein EA, Strombotne KL, Chan NL, Krieger J. Mandatory menu labeling in one fast-food chain in King County, Washington. Am J Prev Med. 2011;40(2):122–127. 10.1016/j.amepre.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 45.Auchincloss AH, Mallya GG, Leonberg BL, Ricchezza A, Glanz K, Schwarz DF. Customer responses to mandatory menu labeling at full-service restaurants. Am J Prev Med. 2013;45(6):710–719. 10.1016/j.amepre.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 46.Afshin A, Micha R, Khatibzadeh S, Mozaffarian D. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2014;100(l):278–288. 10.3945/ajcn.113.076901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Afshin A, Penalvo JL, Del Gobbo L, et al. The prospective impact of food pricing on improving dietary consumption: a systematic review and meta-analysis. PLoS One. 2017; 12(3):e0172277 10.1371/journal.pone.0172277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Micha R, Karageorgou D, Bakogianni I, et al. Effectiveness of school food environment policies on children’s dietary behaviors: a systematic review and meta-analysis. PLoSOne. 2018;13(3):e0194555 10.1371/journal.pone.0194555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.James A, Adams-Huet B, Shah M. Menu labels displaying the kilocalorie content or the exercise equivalent: effects on energy ordered and consumed in young adults. Am J Health Promot. 2015;29(5):294–302. 10.4278/ajhp.130522-QUAN-267. [DOI] [PubMed] [Google Scholar]
- 50.Lowe MR, Tappe KA, Butryn ML, et al. An intervention study targeting energy and nutrient intake in worksite cafeterias. Eat Behav. 2010; 11(3): 144–151. 10.1016/j.eatbeh.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Steenhuis I, Van Assema P, Van Breukelen G, Glanz K, Kok G, De Vries H. The impact of educational and environmental interventions in Dutch worksite cafeterias. Health Promot Int. 2004;19(3):335–343. 10.1093/heapro/dah307. [DOI] [PubMed] [Google Scholar]
- 52.Stubenitsky K, Aaron J, Catt S, Mela D. The influence of recipe modification and nutritional information on restaurant food acceptance and macronutrient intakes. Public Health Nutr. 2000;3(2):201–209. 10.1017/S1368980000000239. [DOI] [PubMed] [Google Scholar]
- 53.Steenhuis I, Van Assema P, Van Breukelen G, Glanz K. The effectiveness of nutrition education and labeling in Dutch supermarkets. Am J Health Promot. 2004;18(3):221–224. 10.4278/0890-1171-18.3.221. [DOI] [PubMed] [Google Scholar]
- 54.Bergen D, Yeh MC. Effects of energy-content labels and motivational posters on sales of sugar-sweetened beverages: stimulating sales of diet drinks among adults study. J Am Diet Assoc. 2006; 106(11): 1866–1869. 10.1016/j.jada.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 55.Roberto CA, Shivaram M, Martinez O, Boles C, Harris JL, Brownell KD. The Smart Choices front-of-package nutrition label. Influence on perceptions and intake of cereal. Appetite. 2012;58(2):651–657. 10.1016/j.appet.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 56.Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. Am J Public Health. 2010;100(2):312–318. 10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harnack LJ, French SA, Oakes JM, Story MT, Jeffery RW, Rydell SA. Effects of calorie labeling and value size pricing on fast food meal choices: results from an experimental trial. Int J Behav Nutr Phys Act. 2008;5:63 10.1186/1479-5868-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goodman S, Hammond D, Hanning R, Sheeshka J. The impact of adding front-of-package sodium content labels to grocery products: an experimental study. Public Health Nutr. 2013;16(3):383–391. 10.1017/S1368980012003485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Temple JL, Johnson KM, Archer K, LaCarte A, Yi C, Epstein LH. Influence of simplified nutrition labeling and taxation on laboratory energy intake in adults. Appetite. 2011;56(3):184–192. 10.1016/j.appet.2011.04.018. [DOI] [PubMed] [Google Scholar]
- 60.Miller DL, Castellanos VH, Shide DJ, Peters JC, Rolls BJ. Effect of fat-free potato chips with and without nutrition labels on fat and energy intakes. Am J Clin Nutr. 1998;68(2):282–290. 10.1093/ajcn/68.2.282. [DOI] [PubMed] [Google Scholar]
- 61.Hammond D, Goodman S, Hanning R, Daniel S. A randomized trial of calorie labeling on menus. Prev Med. 2013;57(6):860–866. 10.1016/j.ypmed.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 62.Gravel K, Doucet E, Herman CP, Pomerleau S, Bourlaud AS, Provencher V. “Healthy,” “diet,” or “hedonic”. How nutrition claims affect food-related perceptions and intake? Appetite. 2012;59(3):877–884. 10.1016/j.appet.2012.08.028. [DOI] [PubMed] [Google Scholar]
- 63.Steenhuis IHM, Kroeze W, Vyth EL, Valk S, Verbauwen R, Seidell JC. The effects of using a nutrition logo on consumption and product evaluation of a sweet pastry. Appetite. 2010;55(3):707–709. 10.1016/j.appet.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 64.Bushman BJ. Effects of warning and information labels on consumption of full-fat, reduced-fat, and no-fat products. J Appl Psychol. 1998;83(1):97–101. 10.1037/0021-9010.83.1.97. [DOI] [PubMed] [Google Scholar]
- 65.Lassen AD, Beck AM, Leedo E, et al. Effectiveness of offering keyhole labelled meals in improving the nutritional quality of lunch meals eaten in worksite canteens. Ann Nutr Metab. 2013;63(suppl I):954. [DOI] [PubMed] [Google Scholar]
- 66.Thorndike AN, Sonnenberg L, Riis J, Barraclough S, Levy DE. A 2-phase labeling and choice architecture intervention to improve healthy food and beverage choices. Am J Public Health. 2012;102(3):527–533. 10.2105/AJPH.2011.300391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Levin S Pilot study of a cafeteria program relying primarily on symbols to promote healthy choices. J Nutr Educ. 1996;28:282–285. 10.1016/S0022-3182196170102-4. [DOI] [Google Scholar]
- 68.Vanderlee L, Hammond D. Does nutrition information on menus impact food choice? Comparisons across two hospital cafeterias. Public Health Nutr. 2014;17(6):1393–1402. 10.1017/S136898001300164X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Uglem S, Stea TH, Kjollesdal MKR, Frolich W, Wandel M. A nutrition intervention with a main focus on vegetables and bread consumption among young men in the Norwegian National Guard. Food Nutr Res. 2013;57 10.3402/fnr.v57i0.21036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Aaron JI, Evans RE, Mela DJ. Paradoxical effect of a nutrition labelling scheme in a student cafeteria. Nutr Res. 1995; 15(9): 1251–1261. 10.1016/0271-5317195102001-C. [DOI] [Google Scholar]
- 71.Lee-Kwan SH, Bleich SN, Kim H, Colantuoni E, Gittelsohn J. Environmental intervention in carryout restaurants increases sales of healthy menu items in a low-income urban setting. Am J Health Promot. 2015;29(6):357–364. 10.4278/ajhp.130805-QUAN-408. [DOI] [PubMed] [Google Scholar]
- 72.Brissette I, Lowenfels A, Noble C, Spicer D. Predictors of total calories purchased at fast-food restaurants: restaurant characteristics, calorie awareness, and use of calorie information. J Nutr Educ Behav. 2013;45(5):404–411. 10.1016/j.jneb.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 73.Namba A, Auchincloss A, Leonberg BL, Wootan MG. Exploratory analysis of fast-food chain restaurant menus before and after implementation of local calorie-labeling policies, 2005–2011. Prev Chronic Dis. 2013;10(6):E101 10.5888/pcd10.120224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Saelens BE, Chan NL, Krieger J, et al. Nutrition-labeling regulation impacts on restaurant environments. Am J Prev Med. 2012;43(5):505–511. 10.1016/j.amepre.2012.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Elbel B, Gyamfi J, Kersh R. Child and adolescent fast-food choice and the influence of calorie labeling: a natural experiment. Int J Obes (Lond). 2011;35(4):493–500. 10.1038/ijo.2011.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vadiveloo MK, Dixon LB, Elbel B. Consumer purchasing patterns in response to calorie labeling legislation in New York City. Int J Behav Nutr Phys Act. 2011. ;8:51 10.1186/1479-5868-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bassett MT, Dumanovsky T, Huang C, et al. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am J Public Health. 2008;98(8): 1457–1459. 10.2105/AJPH.2008.135020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gittelsohn J, Song HJ, Suratkar S, et al. An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Educ Behav. 2010;37(3):390–402. 10.1177/1090198109343886. [DOI] [PubMed] [Google Scholar]
- 79.Patterson BH, Kessler LG, Wax Y et al. Evaluation of a supermarket intervention: the NCI-Giant food eat for health study. Eval Rev. 1992;16(5):464–490. 10.1177/0193841X9201600502. [DOI] [Google Scholar]
- 80.Louie JC, Dunford EK, Walker KZ, Gill TP. Nutritional quality of Australian breakfast cereals. Are they improving? Appetite. 2012;59(2):464–470. 10.1016/j.appet.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 81.Ogawa Y, Tanabe N, Honda A, et al. Point-of-purchase health information encourages customers to purchase vegetables: objective analysis by using a point-of-sales system. Environ Health Prev Med. 2011;16(4):239–246. 10.1007/s12199-010-0192-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Vermeer WM, Steenhuis IH, Leeuwis FH, Bos AE, de Boer M, Seidell JC. View the label before you view the movie: a field experiment into the impact of portion size and Guideline Daily Amounts labelling on soft drinks in cinemas. BMC Public Health. 2011;11:438 10.1186/1471-2458-11-438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kral TV, Roe LS, Rolls BJ. Does nutrition information about the energy density of meals affect food intake in normal-weight women? Appetite. 2002;39(2): 137–145. 10.1006/appe.2002.0498. [DOI] [PubMed] [Google Scholar]
- 84.Shide DJ, Rolls BJ. Information about the fat content of preloads influences energy intake in healthy women. J Am Diet Assoc. 1995;95(9):993–998. 10.1016/S0002-8223(95)00273-1. [DOI] [PubMed] [Google Scholar]
- 85.Brannstrom I, Weinehall L, Persson LA, Wester PO, Wall S. Changing social patterns of risk factors for cardiovascular disease in a Swedish community intervention programme. Int J Epidemiol. 1993. ;22(6): 1026–1037. 10.1093/ije/22.6.1026. [DOI] [PubMed] [Google Scholar]
- 86.Sato JN, Wagle A, McProud L, Lee L. Food label effects on customer purchases in a hospital cafeteria in Northern California. Journal of Foodservice Business Research. 2013; 16(2): 155–168. 10.1080/15378020.2013.782235. [DOI] [Google Scholar]
- 87.Sonnenberg L, Gelsomin E, Levy DE, Riis J, Barraclough S, Thorndike AN. A traffic light food labeling intervention increases consumer awareness of health and healthy choices at the point-of-purchase. Prev Med. 2013;57(4):253–257. 10.1016/j.ypmed.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Freedman MR. Point-of-selection nutrition information influences choice of portion size in an all-you-can-eat university dining hall. Journal of Foodservice Business Research. 2011; 14(1):86–98. 10.1080/15378020.2011.548228. [DOI] [Google Scholar]
- 89.Hoefkens C, Lachat C, Kolsteren P, Van Camp J, Verbeke W. Posting point-of-purchase nutrition information in university canteens does not influence meal choice and nutrient intake. Am J Clin Nutr. 2011. ;94(2):562–570. 10.3945/ajcn.111.013417. [DOI] [PubMed] [Google Scholar]
- 90.Krieger JW, Chan NL, Saelens BE, Ta ML, Solet D, Fleming DW. Menu labeling regulations and calories purchased at chain restaurants. Am J Prev Med. 2013;44(6):595–604. 10.1016/j.amepre.2013.01.031. [DOI] [PubMed] [Google Scholar]
- 91.Wu HW, Sturm R. Changes in the energy and sodium content of main entrees in U.S. chain restaurants from 2010 to 2011. J Acad Nutr Diet. 2014; 114(2):209–219. 10.1016/j.jand.2013.07.035. [DOI] [PubMed] [Google Scholar]
- 92.Dumanovsky T, Huang CY, Nonas CA, Matte TD, Bassett MT, Silver LD. Changes in energy content of lunchtime purchases from fast food restaurants after introduction of calorie labelling: cross sectional customer surveys. BMJ. 2011;343:d4464 10.1136/bmj.d4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Horgen KB, Brownell KD. Comparison of price change and health message interventions in promoting healthy food choices. Health Psychol. 2002;21(5):505–512. 10.1037/0278-6133.21.5.505. [DOI] [PubMed] [Google Scholar]
- 94.Fotouhinia-Yepes M Menu calorie labelling in a fine dining restaurant: will it make a difference? Journal of Quality Assurance in Hospitality & Tourism. 2013;14(3):281–293. 10.1080/1528008X.2013.802550. [DOI] [Google Scholar]
- 95.Thunstrom L, Nordstrom J. Does easily accessible nutritional labelling increase consumption of healthy meals away from home? A field experiment measuring the impact of a point-of-purchase healthy symbol on lunch sales. Acta Agricultura Scandinavica. Section C, Food Economics. 2011;8(4):200–207. [Google Scholar]
- 96.Bell C, Pond N, Davies L, Francis JL, Campbell E, Wiggers J. Healthier choices in an Australian health service: a pre-post audit of an intervention to improve the nutritional value of foods and drinks in vending machines and food outlets. BMC Health Serv Res. 2013;13:492 10.1186/1472-6963-13-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lee JH, Adhikari P, Kim SA, Yoon T, Kim IH, Lee KT. Trans fatty acids content and fatty acid profiles in the selected food products from Korea between 2005 and 2008. J Food Sci. 2010;75(7):C647–C652. 10.1111/j.1750-3841.2010.01737.x. [DOI] [PubMed] [Google Scholar]
- 98.Ricciuto L, Lin K, Tarasuk V. A comparison of the fat composition and prices of margarines between 2002 and 2006, when new Canadian labelling regulations came into effect. Public Health Nutr. 2009;12(8): 1270–1275. 10.1017/S1368980008003868. [DOI] [PubMed] [Google Scholar]
- 99.Bleich SN, Barry CL, Gary-Webb TL, Herring BJ. Reducing sugar-sweetened beverage consumption by providing caloric information: how black adolescents alter their purchases and whether the effects persist. Am J Public Health. 2014;104(12):2417–2424. 10.2105/AJPH.2014.302150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bleich SN, Herring BJ, Flagg DD, Gary-Webb TL. Reduction in purchases of sugar-sweetened beverages among low-income black adolescents after exposure to caloric information. Am J Public Health. 2012;102(2):329–335. 10.2105/AJPH.2011.300350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Olstad DL, Vermeer J, McCargar LJ, Prowse RJ, Raine KD. Using traffic light labels to improve food selection in recreation and sport facility eating environments. Appetite. 2015;91:329–335. 10.1016/j.appet.2015.04.057. [DOI] [PubMed] [Google Scholar]
- 102.Hoerr SM, Louden VA. Can nutrition information increase sales of healthful vended snacks? J Sch Health. 1993;63(9):386–390. 10.1111/j.1746-1561.1993.tb06167.x. [DOI] [PubMed] [Google Scholar]
- 103.Friesen R, Innis SM. Trans fatty acids in human milk in Canada declined with the introduction of trans fat food labeling. J Nutr. 2006;136(10):2558–2561. 10.1093/jn/136.10.2558. [DOI] [PubMed] [Google Scholar]
- 104.Vesper HW, Kuiper HC, Mirel LB, Johnson CL, Pirkle JL. Levels of plasma transfatty acids in non-Hispanic white adults in the United States in 2000 and 2009. JAMA. 2012;307(6):562–563. 10.1001/jama.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ippolito PM, Mathios AD. Health claims in food marketing: evidence on knowledge and behavior in the cereal market. Journal of Public Policy & Marketing. 1991; 10(1): 15–32. [Google Scholar]
- 106.Vyth EL, Steenhuis IH, Roodenburg AJ, Brug J, Seidell JC. Front-of-pack nutrition label stimulates healthier product development: a quantitative analysis. Int J Behav Nutr Phys Act. 2010;7:65 10.1186/1479-5868-7-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.U.S. Food and Drug Administration. Label Claims for Conventional Foods and Dietary Supplements. www.fda.gov/Food/LabelingNutrition/ucm111447.htm. Published 2018. Accessed September 30, 2018.
- 108.U.S. Food and Drug Administration. Guidance for Industry: Food Labeling Guide. www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm2006828.htm. Published 1994; Revised 2013. Accessed September 30, 2018.
- 109.Neuman N, Persson Osowski C, Mattsson Sydner Y, Fjellstrom C. Swedish students’ interpretations of food symbols and their perceptions of healthy eating. An exploratory study. Appetite. 2014;82:29–35. 10.1016/j.appet.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 110.Wang Q, Oostindjer M, Amdam GV, Egelandsdal B. Snacks with nutrition labels: tastiness perception, healthiness perception, and willingness to pay by Norwegian adolescents. J Nutr Educ Behav. 2016;48(2):104–111.e1. 10.1016/j.jneb.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 111.Larsson I, Lissner L, Wilhelmsen L. The ‘Green Keyhole’ revisited: nutritional knowledge may influence food selection. Eur J Clin Nutr. 1999;53(10):776–780. 10.1038/sj.ejcn.1600839. [DOI] [PubMed] [Google Scholar]
- 112.Michail N Sweden to investigate low uptake of Keyhole logo. www.foodnavigator.com/Article/2018/04/09/Sweden-to-investigate-low-uptake-of-Keyhole-logo. Published April 9, 2018. Accessed July 21, 2018.
- 113.Schilpzand R Choices International Foundation/Choices Programme. http://ec.europa.eu/health//sites/health/files/nutrition physical_activitv/docs/ev20130_926_co04_en.pdf. Published 2013. Accessed June 18, 2018.
- 114.Vyth EL, Steenhuis IH, Mallant SF, et al. A front-of-pack nutrition logo: a quantitative and qualitative process evaluation in the Netherlands. J Health Commun. 2009; 14(7):631–645. 10.1080/10810730903204247. [DOI] [PubMed] [Google Scholar]
- 115.Choice International Foundation. Choices Programme. www.choicesprogramme.org/. Published 2018. Accessed June 18, 2018.
- 116.Michail N Dutch industry-backed nutrition label ticked off with mounting criticism. www.foodnavigator.com/Article/2016/04/22/Dutch-industry-backed-nutrition-label-ticked-off-with-mounting-criticism. Published April 21, 2016. Accessed July 21, 2018.
- 117.Michail N Dutch ditch healthy eating logo for an app. www.foodnavigator.com/Article/2016/10/25/Dutch-ditch-healthy-eating-logo-for-an-app. Published October 24, 2016. Accessed July 21, 2018.
- 118.Sacks G, Rayner M, Swinburn B. Impact of front-of-pack “traffic-light” nutrition labeling on consumer food purchases in the UK. Health Promot Int. 2009;24(7):344–352. 10.1093/heapro/dap032. [DOI] [PubMed] [Google Scholar]
- 119.Carreno I Chile’s black STOP sign for foods high in fat, salt or sugar. Eur J Risk Regal. 2015;6(4): 622–628. [Google Scholar]
- 120.Kinnunen TI. The Heart symbol: a new food labelling system in Finland. Nutr Bull. 2000;25(4):335–339. 10.1046/j.1467-3010.2000.00079.x. [DOI] [Google Scholar]
- 121.The Health Star Rating. About Health Star Ratings. http://healthstarrating.gov.au/internet/healthstarrating/publishing.nsf/Content/About+the+Health+Star+Rating+System. Published December 6, 2014. Accessed July 21, 2018.
- 122.Stehbens WE. The National Heart Foundation of Australia Pick the Tick Program. Med J Aust. 1992; 157(8): 569. [PubMed] [Google Scholar]
- 123.Young L, Swinburn B. Impact of the Pick the Tick food information programme on the salt content of food in New Zealand. Health Promot Int. 2002; 17(1): 13–19. 10.1093/heapro/17,1.13. [DOI] [PubMed] [Google Scholar]
- 124.Katz DL, Njike VY, Rhee LQ, Reingold A, Ayoob KT. Performance characteristics of NuVal and the Overall Nutritional Quality Index (ONQI). Am J Clin Nutr. 2010;91(4): 1102s–1108s. 10.3945/ajcn.2010.28450E. [DOI] [PubMed] [Google Scholar]
- 125.Sutherland LA, Kaley LA, Fischer L. Guiding stars: the effect of a nutrition navigation program on consumer purchases at the supermarket. Am J Clin Nutr. 2010;91(4):1090s–1094s. 10.3945/ajcn.2010.28450C. [DOI] [PubMed] [Google Scholar]
- 126.Lupton JR, Balentine DA, Black RM, et al. The Smart Choices front-of-package nutrition labeling program: rationale and development of the nutrition criteria. Am J Clin Nutr. 2010;91(4):1078s–1089s. 10.3945/ajcn.2010.28450B. [DOI] [PubMed] [Google Scholar]
- 127.American Heart Association. How the Heart-Check Food Certification Program Works. www.heart.org/en/healthy-living/company-collaboration/heart-check-certification/how-the-heart-check-food-certification-program-works. Published 2016. Accessed March 17, 2017.
- 128.New York City Department of Health and Mental Hygiene. Intention to Repeal and Reenact Sec 81.50 of the New York City Health Code; 2007. [Google Scholar]
- 129.Nikolaou CK, Hankey CR, Lean ME. Calorie-labelling: does it impact on calorie purchase in catering outlets and the views of young adults? Int J Obes (Lond) 2015;39(3):542–545. 10.1038/ijo.2014.162. [DOI] [PubMed] [Google Scholar]
- 130.Littlewood JA, Lourenco S, Iversen CL, Hansen GL. Menu labelling is effective in reducing energy ordered and consumed: a systematic review and meta-analysis of recent studies. Public Health Nutr. 2016;19(12):2106–2121. 10.1017/S1368980015003468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cecchini M, Warin L. Impact of food labelling systems on food choices and eating behaviours: a systematic review and meta-analysis of randomized studies. Obes Rev. 2016;17(3):201–210. 10.1111/obr.12364. [DOI] [PubMed] [Google Scholar]
- 132.Cantu-Jungles TM, McCormack LA, Slaven JE, Slebodnik M, Eicher-Miller HA. A meta-analysis to determine the impact of restaurant menu labeling on calories and nutrients (ordered or consumed) in U.S. adults. Nutrients. 2017;9(10):1088 10.3390/nu9101088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Crockett RA, King SE, Marteau TM, et al. Nutritional labelling for healthier food or non-alcoholic drink purchasing and consumption. Cochrane Database Syst Rev. 2018;2:CD009315 10.1002/14651858.CD009315.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Graham DJ, Orquin JL, Visschers VHM. Eye tracking and nutrition label use: a review of the literature and recommendations for label enhancement. Food Policy. 2012;37(4):378–382. 10.1016/j.foodpol.2012.03.004. [DOI] [Google Scholar]
- 135.Annunziata A, Vecchio R. Factors affecting use and understanding of nutrition information on food labels: evidences from consumers. Agricultural Economics Review. 2012; 13(2): 103–116. [Google Scholar]
- 136.Wong CL, Arcand J, Mendoza J, et al. Consumer attitudes and understanding of low-sodium claims on food: an analysis of healthy and hypertensive individuals. Am J Clin Nutr. 2013;97(6): 1288–1298. 10.3945/ajcn.112.052910. [DOI] [PubMed] [Google Scholar]
- 137.Kelly B, Hughes C, Chapman K, et al. Consumer testing of the acceptability and effectiveness of front-of-pack food labelling systems for the Australian grocery market. Health Promot Int. 2009;24(2): 120–129. 10.1093/heapro/dap012. [DOI] [PubMed] [Google Scholar]
- 138.Wiles NL, Paterson M, Meaker JL. What factors determine the use of the nutrition information on the food label when female consumers from Pietermaritzburg select and purchase fat spreads? South Afr J Clin Nutr. 2009;22(2):69–73. 10.1080/16070658.2009.11734221. [DOI] [Google Scholar]
- 139.Hoefkens C, Verbeke W. Consumers’ health-related motive orientations and reactions to claims about dietary calcium. Nutrients. 2013;5(l):82–96. 10.3390/nu5010082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Zezelj I, Milosevic J, Stojanovic Z, Ognjanov G. The motivational and informational basis of attitudes toward foods with health claims. Appetite. 2012;59(3):960–967. 10.1016/j.appet.2012.09.008 [DOI] [PubMed] [Google Scholar]
- 141.Afshin A, Babalola D, McLean M, et al. Information technology and lifestyle: a systematic evaluation of internet and mobile interventions for improving diet, physical activity, obesity, tobacco, and alcohol use. J Am Heart Assoc. 2016;5(9):e003058 10.1161/JAHA.115.003058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Lichtenstein AH, Carson JS, Johnson RK, et al. Food-intake patterns assessed by using front-of-pack labeling program criteria associated with better diet quality and lower cardiometabolic risk. Am J Clin Nutr. 2014;99(3):454–462. 10.3945/ajcn.113.071407. [DOI] [PubMed] [Google Scholar]
- 143.Neal B, Crino M, Dunford E, et al. Effects of different types of front-of-pack labelling information on the healthiness of food purchases-a randomised controlled trial. Nutrients. 2017;9(12):1284 10.3390/nu9121284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Harnack LJ, Cogswell ME, Shikany JM, et al. Sources of sodium in U.S. adults from 3 geographic regions. Circulation. 2017;135(19):1775–1783. 10.1161/CIRCULATIONAHA.116.024446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991:10(4):383–393. 10.1080/07315724.1991.10718167. [DOI] [PubMed] [Google Scholar]
- 146.Wanders AJ, Zock PL, Brouwer IA. Trans fat intake and its dietary sources in general populations worldwide: a systematic review. Nutrients. 2017;9(8):840 10.3390/nu9080840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Craig P, Cooper C, Gunnell D, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Community Health. 2012;66(12):1182–1186. 10.1136/jech-2011-200375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mhurchu CN, Eyles H, Choi YH. Effects of a voluntary front-of-pack nutrition labelling system on packaged food reformulation: the Health Star Rating System in New Zealand. Nutrients. 2017;9(8):918 10.3390/nu9080918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Acton RB, Hammond D. The impact of price and nutrition labelling on sugary drink purchases: results from an experimental marketplace study. Appetite. 2018;121:129–137. 10.1016/j.appet.2017.11.089. [DOI] [PubMed] [Google Scholar]
- 150.Mhurchu CN, Volkova E, Jiang Y, et al. Effects of interpretive nutrition labels on consumer food purchases: the Starlight randomized controlled trial. Am J Clin Nutr 2017;105(3):695–704. 10.3945/ajcn.116.144956. [DOI] [PubMed] [Google Scholar]
- 151.Julia C, Peneau S, Buscail C, et al. Perception of different formats of front-of-pack nutrition labels according to sociodemographic, lifestyle and dietary factors in a French population: cross-sectional study among the NutriNet-Sante cohort participants. BMJ Open. 2017;7(6):e016108 10.1136/bmjopen-2017-016108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.