Abstract
Purpose
Endotype in chronic rhinosinusitis (CRS) has been established in the last decade. However, the exact immunologic profile of CRS still has controversy because it has a considerable immunologic heterogeneity. Therefore, we investigated various inflammatory mediators according to different nasal tissues in chronic rhinosinusitis and compared them within the same subject.
Methods
We collected uncinate process mucosa (UP) and nasal polyp (NP) tissues from controls, CRS without NP (CRSsNP) and CRS with NP (CRSwNP). Expression levels of 28 inflammatory mediators including T helper (Th) 1, Th2, Th17, proinflammatory cytokines and remodeling markers were determined by multiplex immunoassay and were analyzed using paired tests as well as principal component analysis (PCA) to investigate endotype in each subtype of CRS.
Results
Signature inflammatory mediators are interleukin (IL)-5, C-C motif chemokine ligand (CCL)-24, monocyte chemoattractant protein (MCP)-4, and vascular cell adhesion molecule (VCAM)-1 in eosinophilic NP, whereas IL-17A, IL-1β, and matrix metallopeptidase (MMP)-9 were detected as signature inflammatory markers in non-eosinophilic NP. Despite differences in inflammatory cytokine profile between eosinophilic and non-eosinophilic NP, the common upregulation of IL-5, CCL-11, IL-23, IL-2Rα, VCAM-1, MMP-3 and MMP-9 were shown in NP compared to UP within the same subject. In the PCA, we observed that Th2 immune response was helpful in discriminating between nasal tissues in subtypes of CRS and that there was a partial overlap between non-eosinophilic NP and eosinophilic NP in terms of Th2 mediators.
Conclusions
Commonly upregulated mediators in NP were Th2-associated, compared with UP regardless of CRS subtypes, whereas signature markers were distinct in each NP subtype. These findings imply that Th2 inflammatory responses may play a role in the development of NP regardless of CRSwNP subtypes.
Keywords: Cytokines, rhinitis, sinusitis, nasal polyp
INTRODUCTION
Chronic rhinosinusitis (CRS) is a common chronic inflammatory disease of the nasal and paranasal mucosa.1 It usually causes substantial impaired quality of life, reduced workplace productivity, and is related to substantial direct and indirect economic cost.2,3 CRS is a highly heterogeneous disease and currently defined as subgroups of patients based on nasal endoscopic findings, either accompanied by nasal polyps (CRSwNP) or without nasal polyps (CRSsNP).1 However, clinical phenotype dose not adequately reflect the pathophysiologic diversity within patients with CRS.4,5,6 Evidence from several studies suggested that CRSsNP is characterized by a predominant T helper (Th) 1 inflammatory response, whereas CRSwNP is driven by a Th2 inflammation and increased eosinophilic infiltration.4,5,6 In addition, within the same clinical phenotype, several studies have revealed the presence of different immunologic endotypes.7,8,9,10,11,12,13,14 These studies showed that patients with CRSwNP in Asians displayed a mixed T-cell profile with a non-eosinophilic inflammation pattern.10,11,12,13,14
Recent studies have shown regional differences in CRS endotypes. One study has demonstrated that Th1/Th2/Th17 cytokine profile is diverse in terms of the immunologic endotypes among CRS subjects in Europe, China, Japan and Australia.15 Another study also revealed that second-generation Asian patients with CRSwNP living in the United States had a lower percentage of eosinophilic NPs compared to other ethnic groups, probably as a consequence of their genetic influence.16 Moreover, one cluster analysis study with phenotype-free approach has identified that CRS patients have 10 distinct inflammatory endotypes which are correlated with phenotype and that these endotypes comprise 4 clusters with low interleukin (IL)-5 and 6 clusters with moderate to high IL-5.8 To date, some epithelial derived cytokines also have an important role in the development of CRS according to its endotype.17,18,19 Furthermore, one recent study deomnstrated seven CRS clusters with distinct endotypes and treatment outcomes.9 These studies indicate that CRS shows remarkable heterogeneity at the molecular level and various treatment response.
However, the question is still unanswered whether CRS represents a serial clinical spectrum disease (evolution from CRSsNP to CRSwNP) or manifest as 2 different diseases that develop separately. To address this issue, a cohort study should be designed; however, it is difficult to conduct a cohort study due to ethical problems. Although the present study was designed as a cross-sectional study, we used the paired comparison of nasal tissues from uncinate process mucosa (UP) and NP within the same CRSwNP patient to partially overcome the limitation of cross-sectional study. Therefore, in this study, we investigate the differences in immunologic profile among CRS subtypes and intend to seek the signature immunologic markers for the development of NP.
MATERIALS AND METHODS
Patients and tissue samples
Sinonasal and polyp tissues were obtained from patients with bilateral CRS during routine functional endoscopic sinus surgery. All subjects provided written informed consent for study participation, and the study was approved by the internal review board of Seoul National University Hospital, Boramae Medical Center. The diagnosis of CRS was based on personal history, physical examination, nasal endoscopy and computed tomography findings of the sinuses according to the 2012 European position paper on rhinosinusitis and nasal polyps (EPOS) guidelines.1 Exclusion criteria were as follows: 1) younger than 18 years of age; 2) prior treatment with antibiotics, systemic or topical corticosteroids, or other immune-modulating drugs for 4 weeks before surgery; and 3) unilateral rhinosinusitis, antrochoanal polyp, allergic fungal sinusitis, cystic fibrosis, or immotile ciliary disease. Control tissues were obtained during other rhinologic surgeries, such as skull base, lacrimal duct or orbital decompression surgery, from patients without any sinonasal diseases. UP tissue was obtained from control subjects and those with CRSsNP or CRSwNP. NP tissue was also obtained from CRSwNP patients. All samples were homogenized with a mechanical homogenizer at 1,000 rpm for 5 minutes on ice. After homogenization, the suspensions were centrifuged at 3,000 rpm for 10 minutes at 4ºC, and the supernatants were separated and stored at −80ºC for further analysis of cytokines and other inflammatory mediators. The atopic status of study subjects was evaluated using the ImmunoCAP® assay (Phadia, Uppsala, Sweden) to detect immunoglobulin E (IgE) antibodies against 6 mixtures of common aeroallergens (house dust mites, molds, trees, weeds and grass pollen, and animal dander). Subjects were considered atopic if the allergen-specific IgE level was greater than 0.35 kU/L to any 1 or more of the allergens. A diagnosis of asthma was based on the medical history and lung function analysis, including methacholine challenge test by an allergist. In this study, CRSwNP were classified as eosinophilic CRSwNP (E-CRSwNP) if eosinophils comprised more than 10% of the inflammatory cell population and as non-eosinophilic CRSwNPs (NE-CRSwNP) if eosinophils comprised less than 10% of the inflammatory cells.11,20 Additional information and details of the subjects' characteristics are listed in Table 1.
Table 1. Demographic and clinical characteristics of patients.
| Parameters | Control (n = 9) | CRSsNP (n = 20) | NE-CRSwNP (n = 11) | E-CRSwNP (n = 16) | NE-CRSwNP (n = 15) | E-CRSwNP (n = 21) |
|---|---|---|---|---|---|---|
| Tissue used | UP | UP | UP | UP | NP | NP |
| Male/female | 14/8 | 12/8 | 11/0 | 14/2 | 13/2 | 17/4 |
| Age (yr) | 63 ± 13.75 | 52 ± 15.2 | 50 ± 28.5 | 44 ± 34.25 | 47 ± 24.5 | 50 ± 8 |
| Atopy (%) | 1 (11) | 5 (25) | 3 (27) | 9 (56) | 3 (20) | 11 (52) |
| Asthma (%) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Smoker (%) | 1 (11) | 7 (35) | 7 (63) | 7 (44) | 7 (46) | 9 (43) |
| Duration (mon) | N/A | 7.5 ± 10.25 | 120 ± 204 | 90 ± 111 | 60 ± 120 | 90 ± 148 |
| CT scores | N/A | 7 ± 2.75 | 15 ± 4.5 | 14.5 ± 5 | 18 ± 6.5 | 14 ± 8 |
UP, uncinate process tissue; NP, nasal polyps; CRSsNP, chronic rhinosinusitis without nasal polyps; E, eosinophilic; NE, non-eosinophilic; CRSwNP, chronic rhinosinusitis with nasal polyps; CT, computed tomography.
Measurement of inflammatory mediators
The protein concentrations for tissue extracts were determined using the Pierce 660 nm Protein Assay Kit (Thermo Scientific Inc., New York, NY, USA). All the protein levels in the tissue homogenate were normalized to the concentration of total protein (mg/mL). Samples were thawed at room temperature and vortexed to ensure well-mixed samples. In the present study, multiplex cytokine analysis kits (IL-1α, IL-1β, IL-2Rα, IL-4, IL-5, IL-6, IL-10, IL-13, IL-17A, IL-22, IL-23, interferon [IFN]-γ, tumor necrosis factor [TNF]-α, C-C motif chemokine ligand [CCL]-11, CCL-24, RANTES, CXCL-1, CXCL-2, CXCL-8, myeloperoxidase [MPO], monocyte chemoattractant protein [MCP]-4, vascular cell adhesion molecule [VCAM]-1, intercellular adhesion molecule [ICAM]-1, matrix metallopeptidase [MMP]-1, MMP-2, MMP-3, MMP-9, tissue inhibitor of metalloproteinase [TIMP]-1 were obtained from R&D systems (Cat. No. LMSAHM), and data were collected using Luminex 100 (Luminex, Austin, TX, USA). Data analysis was performed using the MasterPlex QT version 2.0 (MiraiBio, Alameda, CA, USA). Sensitivity of each cytokine is as follows: IL-1α (0.9 pg/mL), IL-1β (0.8 pg/mL), IL-2Rα (1.3 pg/mL), IL-4 (9.3 pg/mL), IL-5 (0.5 pg/mL), IL-6 (1.7 pg/mL), IL-10 (1.6 pg/mL), IL-13 (32.4 pg/mL), IL-17A (1.8 pg/mL), IL-22 (11.7 pg/mL), IL-23 (11.4 pg/mL), IL-33 (1.8 pg/mL), IFN-γ (0.4 pg/mL), TNF-α (1.2 pg/mL), CCL-11 (14.6 pg/mL), CCL-24 (1.34 pg/mL), RANTES (1.8 pg/mL), CXCL-1 (5.3 pg/mL), CXCL-2 (7.86 pg/mL), CXCL-8 (1.82 pg/mL), MPO (20.4 pg/mL), MCP-4 (0.42 pg/mL), VCAM-1 (238 pg/mL), ICAM-1 (87.9 pg/mL), MMP-1 (2.7 pg/mL), MMP-2 (108 pg/mL), MMP-3 (5.3 pg/mL), MMP-9 (13.6 pg/mL) and TIMP-1 (3.42 pg/mL). All assays were run in duplicate according to the manufacturers' protocol.
Statistical analysis
Statistical analyses were performed using IBM SPSS 21 (SPSS, Inc., Chicago, IL, USA) and GraphPad Prism software 6.0 (GraphPad Software Inc, La Jolla, CA, USA). Descriptive statistics were performed, and values are described as a median ± interquartile range. For comparisons among multiple groups, the Kruskal-Wallis test was first used to establish the significant difference and then, if the significance was found, the Mann-Whitney U test was secondarily performed between 2 groups and Bonferroni correction was used to adjust the significance level for each comparison. Specific differences between 2 groups were determined by the Mann-Whitney test. Correlations were assessed by Spearman rank. The significance level was set at α value of 0.05. A multivariate analysis of multiplex or enzyme-linked immunosorbent assay (ELISA) protein data was performed using principal component analysis (PCA) on correlation matrices of protein levels of all measured mediators of inflammation.
RESULTS
Signature inflammatory markers in subtypes of chronic rhinosinusitis
To characterize the profile of cytokines and inflammatory mediators according to the CRS phenotype, we performed ELISA and multiplex bead-based immunoassay for key inflammatory mediators in UP tissues from controls, CRSsNP and CRSwNP, and in NP tissues from CRSwNP (Tables 2 and 3).
Table 2. The profile of inflammatory mediators in the subtype of chronic rhinosinusitis.
| Parameters (pg/mg) | Control (n = 9) | CRSsNP (n = 20) | NE-CRSwNP (n = 15) | E-CRSwNP (n = 21) |
|---|---|---|---|---|
| Tissue used | UP | UP | NP | NP |
| IL-4 | 12.26 (10.09–14.07) | 21.47 (16.07–23.82) | 19.43 (17.22–22.6)* | 23.96 (19.91–27.6)* |
| IL-5 | 1.91 (1.86–2.04) | 3.60 (2.85–6.95)* | 3.186 (2.734–6.198)* | 12.3 (3.441–34.14)*,†,‡ |
| IL-13 | 29.99 (0–59.60) | 55.6 (40.46–101.4)* | 62.1 (49.83–91.5)* | 67.61 (58.01–99.69)* |
| IL-17A | 0.354 (0.264–0.662) | 1.077 (0.5862–3.094)* | 2.427 (1.124–4.18)*,†,‡ | 0.8769 (0.5223–2.584) |
| IL-2 | 18.26 (14.49–29.42) | 28.19 (19.89–62.66) | 49.87 (34.37–56.84) | 41.46 (33.81–118.5) |
| IL-23 | 1.1 (0.00–3.21) | 4.146 (2.631–12.18)* | 47.02 (25.92–60.52)*,† | 39.91 (18.8–58.81)*,† |
| IFN-γ | 3 (0–7.286) | 6.592 (4.271–12.03) | 4.751 (3.852–6.03)* | 3.982 (2.479–4.918) |
| TNF-α | 1.18 (0.72–1.90) | 1.286 (0.9666–3.298) | 1.6 (1.079–2.628) | 1.583 (1.117–2.593) |
| IL-10 | 0.34 (0.31–0.37) | 0.4392 (0.3368–0.8086) | 0.425 (0.3039–0.6192) | 0.3455 (0.2597–0.4748) |
| CCL-11 | 7.8 (1.716–13.04) | 22.47 (17.24–55.23) | 47.34 (29.15–105.8)*,† | 69.21 (33.81–111.85)*,† |
| CCL-24 | 53.13 (36.72–81.53) | 171.5 (130.8–272) | 282.2 (111.3–416.4)* | 1,046 (233.7–1,516)*,†,‡ |
| MCP-4 | 4.33 (2.94–7.69) | 12.35 (4.856–58.11) | 21.08 (12.43–35.97)* | 139.6 (33.36–376.6)*,†,‡ |
| RANTES | 402.2 (340.6–585.8) | 1,498.0 (610.5–2,446.0) | 1,016 (603.5–1,636)* | 691.6 (454.4–1,177) |
| CXCL-1 | 293.7 (166–382.1) | 732.9 (343.6–1,507) | 1,649 (665.9–2,733)* | 1,159 (602.8–3,641) |
| CXCL-2 | 14.97 (11.08–29.39) | 31.01 (26.54–82.43)* | 36.39 (24.8–54.03)* | 33.19 (9.623–44.34) |
| CXCL-8 | 26.89 (19.14–46.71) | 254.7 (76.76–373.4) | 267.7 (120.7–14.8)* | 138.6 (33.11–628.4) |
| MPO | 23,020 (11,160–29,880) | 42,423 (24,148–57,415) | 29,320 (20,270–34,780) | 14,020 (9,842–33,020) |
| IL-1α | 0.094 (0–0.151) | 0.2424 (0–0.591) | 0.981 (0.4724–1.595)*,† | 1.569 (0.6156–2.394)*,† |
| IL-1β | 0.128 (0–1.656) | 0.969 (0.2801–2.399) | 3.903 (2.825–10.27)*,†,‡ | 1.097 (0–2.75) |
| IL-2Rα | 19.07 (10.94–26.36) | 19.54 (14.92–41.39) | 60.84 (52.58–81.79)*,† | 85.43 (63.29–92.5)*,† |
| IL-6 | 1.343 (0.2786–3.217) | 2.793 (0.8654–5.854) | 10.1 (2.982–22.6)*,† | 13.29 (5.348–36.57)*,† |
| ICAM-1 | 44,431 (19,158–84,951) | 107,961 (56,298–192,848)* | 91,530 (62,390–137,100)* | 88,780 (47,640–127,300)* |
| VCAM-1 | 6,326 (5,652–7,446) | 7,045 (5,159–9,613) | 7,622 (6,234–10,510) | 11,910 (8,750–16,850)*,†,‡ |
Values in bold mean higher expression compared with controls.
UP, uncinate process tissue; NP, nasal polyps; CRSsNP, chronic rhinosinusitis without nasal polyps; E, eosinophilic; NE, non-eosinophilic; CRSwNP, chronic rhinosinusitis with nasal polyps; IL, interleukin; IFN, interferon; TNF, tumor necrosis factor; CCL, C-C motif chemokine ligand; MCP, monocyte chemoattractant protein; MPO, myeloperoxidase; ICAM, intercellular adhesion molecule; VCAM, vascular cell adhesion molecule.
*The comparison between control vs. CRSsNP or NE-CRSwNP or E-CRSwNP; †the comparison between CRSsNP vs. NE-CRSwNP or E-CRSwNP; ‡the comparison between NE-CRSwNP vs. E-CRSwNP.
Table 3. The profile of remodeling mediators in the subtype of chronic rhinosinusitis.
| Parameters (pg/mg) | Control (n = 9) | CRSsNP (n = 20) | NE-CRSwNP (n = 15) | E-CRSwNP (n = 21) |
|---|---|---|---|---|
| Tissue used | UP | UP | NP | NP |
| MMP-1 | 49.15 (29.51–84.14) | 99.13 (43.49–105.5) | 178.8.8 (105.2–244.4)*,† | 320.7 (203.6–454.4)*,† |
| MMP-2 | 10,710 (7,338–15,860) | 9,852 (6,192–18,340) | 13,940 (12,150–15,570) | 11,490 (8,440–14,290) |
| MMP-3 | 371.4 (240.2–574.8) | 306.8 (249.3–428.5) | 620 (478.3–945.2) | 853.1 (609.6–1,200)* |
| MMP-9 | 543 (171.6–720.6) | 650.8 (498.8–898.0)* | 13,330 (4,818–28,210)*,†,‡ | 1,699 (966.3–7,847)* |
| TIMP-1 | 11,473 (10,645–11,915) | 12,186 (7,733–15,251) | 6,929 (5,854–8,338)* | 11,280 (8,387–13,240) |
| M1T1 | 0.00291 (0.001948–0.00291) | 0.003917 (0.0029–0.01063) | 0.02681 (0.01152–0.03034)*,† | 0.0272 (0.01989–0.04809)*,† |
| M2T1 | 1.381 (1.254–1.450) | 1.486 (1.115–1.901) | 1.98 (1.752–2.186)*,†,‡ | 1.054 (0.8–1.678) |
| M3T1 | 0.03827 (0.02044–0.06068) | 0.02518 (0.01525–0.06858) | 0.08902 (0.07041–0.1343)* | 0.07475 (0.05746–0.1508)* |
| M9T1 | 0.04875 (0.01708–0.06818) | 0.04312 (0.0112–0.1496) | 1.741 (0.7074–3.566)*,†,‡ | 0.1567 (0.07116–1.034)* |
Values in bold mean higher expression compared with controls.
UP, uncinate process tissue; NP, nasal polyps; CRSsNP, chronic rhinosinusitis without nasal polyps; E, eosinophilic; NE, non-eosinophilic; CRSwNP, chronic rhinosinusitis with nasal polyps; MMP, matrix metalloproteinase; TIMP, tissue inhibitors of metalloproteinase; M1T1, ratio of MMP1 to TIMP1; M2T1, ratio of MMP2 to TIMP1; M3T1, ratio of MMP3 to TIMP1; M9T1, ratio of MMP1 to TIMP1.
*The comparison between control vs. CRSsNP or NE-CRSwNP or E-CRSwNP; †the comparison between CRSsNP vs. NE-CRSwNP or E-CRSwNP; ‡the comparison between NE-CRSwNP vs. E-CRSwNP.
NP tissues from NE-CRSwNP showed higher expression levels of Th2-associated mediators (IL-4, IL-5, IL-13, CCL-11, CCL-24, MCP-4, and RANTES), Th17-associated mediators (IL-17A, IL-23, CXCL-1, CXCL-2 and CXCL-8), IFN-γ as a Th1 cytokine, pro-inflammatory cytokines (IL-1α, IL-1β, IL-2Rα and IL-6), and adhesion molecule (ICAM-1) than UP tissues from controls. These results are consistent with those of previous reports demonstrating a mixed inflammation pattern of NE-CRSwNP.11,12,13 In the analysis of remodeling markers, the increased expression of MMP-1 and MMP-9 was observed in NP tissues from NE-CRSwNP, whereas TIMP-1 was down-regulated. Among them, the signature inflammatory markers which were at the highest level among all the groups in NE-CRSwNP were IL-17A, IL-1β, and MMP-9. Interestingly, MMP-9 has been reported to be associated with neutrophilic inflammation.21,22
Meanwhile, we found that the levels of Th2-associated mediators (IL-4, IL-5, IL-13, CCL-11, CCL-2,4 and MCP-4), pro-inflammatory cytokines (IL-1α, IL-1β, IL-2Rα, and IL-6), adhesion molecule (VCAM-1 and ICAM-1) and IL-23 were increased in NP tissues from E-CRSwNP, compared with UP tissues from controls. These results were in accordance with those of previous reports demonstrating Th2-deviated inflammation in E-CRSwNP.4,5,6 In the analysis of remodeling markers, the increased expression of MMP-1, MMP-3, and MMP-9 was observed in NP tissues from E-CRSwNP. Among them, the signature inflammatory markers of E-CRSwNP are IL-5, CCL-11, MCP-4, and VCAM-1.
On the analysis of UP tissues from CRSsNP, Th2 cytokines (IL-5 and IL-13) and Th17-associated mediators (IL-17A, IL-22, IL-23, CXCL-2, and ICAM-1) and MMP-9 were significantly up-regulated, compared with controls. These results mean that CRSsNP is characterized by mixed inflammation and their immunologic characteristics are similar to those of NE-CRSwNP. However, there are no signature inflammatory markers in CRSsNP, compared with UP or NP tissues of other subtypes of CRS (Supplementary Tables S1 and S2).
The difference in inflammatory cytokine profiles between uncinate process mucosa and NP tissues within the same subject according to the endotype of chronic rhinosinusitis with NP
To evaluate the difference in cytokines, inflammatory mediators, and remodeling markers related to the evolution of NPs, we compared levels of expression between UP and NP tissues within the same patients (Tables 4 and 5). Although NP tissues from NE-CRSwNP and E-CRSwNP showed different signature inflammatory profiles in Tables 2 and 3, both groups showed common changes in several immunologic profiles on the comparison between UP and NP tissues. We found that up-regulation of Th2-associated mediators (IL-5 and CCL-11), IL-23, IL-2Rα, VCAM-1, and remodeling markers such as MMP-3, MMP-9 were observed in both NP tissues from NE-CRSwNP and E-CRSwNP groups. However, the expression of CCL-24, MCP-4, IL-1α, and IL-6 was only increased in NP tissues from patients with E-CRSwNP, but IFN-γ expression as a Th1 cytokine was decreased in those.
Table 4. Paired comparison of inflammatory mediators between UP and NP tissues within each endotype of CRSwNP.
| Parameters (pg/mg) | NE-CRSwNP (UP) | NE-CRSwNP (NP) | E-CRSwNP (UP) | E-CRSwNP (NP) |
|---|---|---|---|---|
| IL-4 | 14.04 (13–23) | 18.17 (16.22–19.95) | 20.12 (16.62–21.47) | 24.28 (21.35–28.14) |
| IL-5 | 2.293 (1.408–2.708) | 3.319 (2.846–6.027)* | 2.879 (2.19–3.257) | 12.07 (2.759–25.43)‡ |
| IL-13 | 84 (39.31–138.4) | 63.52 (41.89–90.3) | 61.27 (32.33–91.62) | 64.01 (56.02–97.15) |
| IL-17A | 2.599 (1.142–5.508) | 2.587 (1.622–4.81) | 0.7004 (0.5851–1.585) | 0.8769 (0.5656–3.302) |
| IL-22 | 52.11 (18.59–59.28) | 50.82 (36.26–61.42) | 53.24 (41.97–68.89) | 41.46 (26.07–49.87) |
| IL-23 | 5.255 (2.14–9.004) | 52.53 (31.25–60.46)† | 4.063 (2.757–8.881) | 51.43 (23.9–64.21)‡ |
| IFN-γ | 4.648 (3.251–6.484) | 4.74 (3.381–5.53) | 5 (3.897–5.757) | 4.081 (2.899–4.994)† |
| TNF-α | 2.255 (1.575–2.512) | 1.499 (1.004–2.158) | 2.008 (1.1714–2.672) | 1.592 (1.09–2.573) |
| IL-10 | 0.3731 (0.2366–0.5108) | 0.4265 (0.3394–0.5171) | 0.3834 (0.3238–0.4084) | 0.3426 (0.277–0.5025) |
| CCL-11 | 16.27 (5.453–28.97) | 47.69 (39.34–103.8)† | 14.56 (4.033–33.35) | 75.26 (30.86–110)‡ |
| CCL-24 | 200.6 (56.02–357.3) | 277.3 (133.6–398.4) | 184.1 (87.81–756.4) | 1,046 (216.5–1,844)† |
| CXCL-1 | 1,221 (662.3–2,130) | 1,652 (789.4–2,675) | 742.9 (446.4–1,258) | 1,946 (822–3,988)† |
| MCP-4 | 15.66 (8.747–34.57) | 17.73 (13.4–33.96) | 24.55 (13.62–110.5) | 139.6 (25.07–379.3)‡ |
| RANTES | 1,511 (1,160–2,803) | 1,085 (907.2–1,625)* | 1,239 (967–3,031) | 692.6 (540–1,337)† |
| CXCL-2 | 40.93 (23.91–63.76) | 29.25 (25.38–42.5) | 46.37 (27.56–64.93) | 34.77 (20.09–44.68) |
| CXCL-8 | 171.9 (52.49–457.3) | 249.5 (137.2–348.6) | 67.42 (34.17–183) | 152.9 (29.46–662.1) |
| MPO | 41,680 (24,010–52,540) | 30,020 (17,200–36,290) | 28,410 (18,210–43,070) | 14,690 (9,709–40,600) |
| IL-1α | 0.5609 (0.2557–1.548) | 0.5974 (0.2205–1.504) | 0.48 (0–0.9427) | 1.62 (0.5916–3.155)† |
| IL-1β | 3.641 (1.416–7.886) | 2.939 (0.8613–6.436) | 1.054 (0.1264–2.01) | 1.33 (0–3.115) |
| IL-2Rα | 41.61 (29.59–55.64) | 58.26 (53.26–71.32)* | 35.64 (32–42.62) | 84.43 (63.15–89.83)‡ |
| IL-6 | 4.239 (1.689–12.58) | 10.92 (5.554–15.82) | 2.338 (0.5062–9.244) | 13.29 (5.711–41.43)‡ |
| ICAM-1 | 139,100 (57,360–165,200) | 111,200 (72,000–148,000) | 89,140 (76,300–116,700) | 97,050 (47,880–146,400) |
| VCAM-1 | 5,720 (3,881–7,288) | 7,175 (6,149–15,360)* | 6,357 (4,683–7,549) | 12,030 (8,436–17,590)‡ |
Values in bold means significant differences compared with those of uncinate mucosa.
UP, uncinate process tissue; NP, nasal polyps; E, eosinophilic; NE, non-eosinophilic; CRSwNP, chronic rhinosinusitis with nasal polyps IL, interleukin; IFN, interferon; TNF, tumor necrosis factor; CCL, C-C motif chemokine ligand; MCP, monocyte chemoattractant protein; MPO, myeloperoxidase; ICAM, intercellular adhesion molecule; VCAM, vascular cell adhesion molecule.
*,†,‡The paired comparison of cytokine profiles between UP and NP: (*P < 0.05, †P < 0.01, and ‡P < 0.001; n = 9 in NE-CRSwNP and n = 14 in E-CRSwNP.
Table 5. Paired comparison of remodeling mediators between UP and NP tissues within each endotype of CRSwNP.
| Parameters (pg/mg) | NE-NP (UP) | NE-CRSwNP (NP) | E-CRSwNP (UP) | E-CRSwNP (NP) |
|---|---|---|---|---|
| MMP-1 | 15.66 (8.747–34.57) | 175.5 (82.13–251.8) | 133.1 (110.3–152.8) | 315.1 (186.3–462.6)‡ |
| MMP-2 | 13,250 (9,540–15,300) | 13,360 (12,380–15,800) | 13,550 (10,840–15,830) | 12,300 (9,641–14,480) |
| MMP-3 | 432.8 (248.4–504.7) | 606.5 (522.3–860.4)* | 395 (363.3–562) | 852.1 (670.5–1,179)‡ |
| MMP-9 | 1,639 (985.8–5,451) | 8,857 (5,209–25,420)‡ | 761.3 (432.6–2,715) | 1,500 (1,166–9,699)* |
| TIMP-1 | 10,790 (6,341–11,630) | 6,868 (5,891–8,632) | 11,530 (10,960–12,160) | 9,872 (8,047–12,930) |
| M1T1 | 0.0132 (0.008751–0.01483) | 0.02511 (0.009179–0.03808) | 0.01183 (0.009449–0.01386) | 0.02692 (0.01977–0.04809)‡ |
| M2T1 | 1.308 (1.137–2.049) | 2.125 (1.632–2.237) | 1.2 (0.9085–1.367) | 1.115 (0.8052–1.766) |
| M3T1 | 0.04305 (0.03549–0.06414) | 0.08649 (0.06457–0.1419)† | 0.03433 (0.03048–0.04356) | 0.07475 (0.05614–0.158)‡ |
| M9T1 | 0.2287 (0.1061–0.5736) | 1.29 (0.6508–4.026)† | 0.0638 (0.03824–0.2365) | 0.1572 (0.0813–1.244)* |
Values in bold means significant differences compared with those of uncinate mucosa.
UP, uncinate process tissue; NP, nasal polyps; E, eosinophilic; NE, non-eosinophilic; CRSwNP, chronic rhinosinusitis with nasal polyps; MMP, matrix metalloproteinase; TIMP, tissue inhibitors of metalloproteinase; M1T1, ratio of MMP1 to TIMP1; M2T1, ratio of MMP2 to TIMP1; M3T1, ratio of MMP3 to TIMP1; M9T1, ratio of MMP1 to TIMP1.
*,†,‡The paired comparison of cytokine profiles between UP and NP: *P < 0.05, †P < 0.01, and ‡P < 0.001; n = 9 in NE-CRSwNP and n = 14 in E-CRSwNP).
Principal component analysis
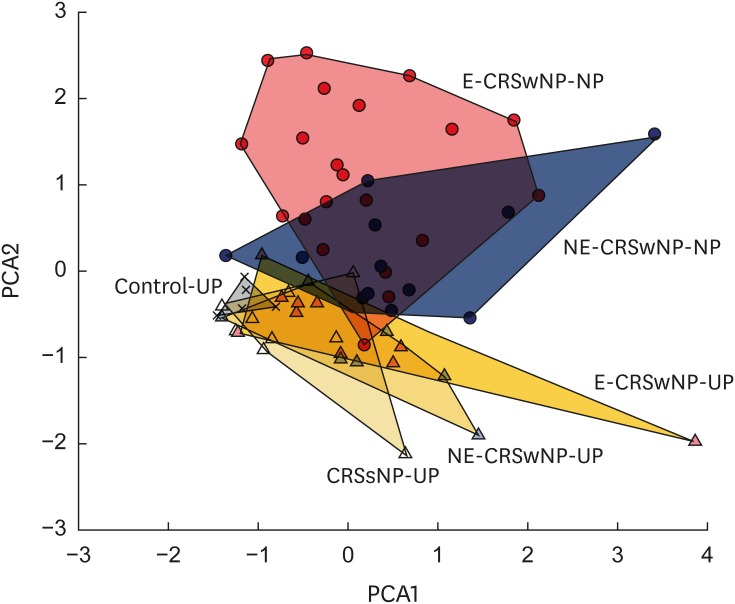
To investigate whether the overall profile of multiple mediators could discriminate CRS subtypes and sinonasal tissue types, we performed the PCA using the interpretation of multivariate immunoplex data (Fig. 1). The PCA retained 4 components and it presented in Supplementary Table S3. The first component (PC1) accounted for 23.1% of the variance in the dataset and its greater discriminators were IL-1β, IFN-γ, IL-6, MMP-9, and IL-1α (in order). The second component (PC2) accounted for 14.8% of the variance in the dataset and its greater discriminators included MMP3, CCL-24, VCAM-1, MMP-1, and IL-5 (in order). Thus, PC1 represented a predominant Th1 or proinflammatory profile, whereas PC2 indicated a relative Th2 profile. In this analysis, we observed that both PC1 and PC2 were helpful in discriminating between controls and subtypes of CRS. Additionally, the Th2 profile on PC2 could help distinctly discriminate the different tissues of CRS (UP vs. NP) but were not helpful in clearly defining for subtypes of NP (NE-CRSwNP-NP vs. E-CRSwNP-NP).
Fig. 1. PCA consists of first and second PCA components of inflammatory mediator levels according to the different sinonasal tissues. UP, uncinate process tissue; NP, nasal polyps; CRSsNP, chronic rhinosinusitis without nasal polyps; E, eosinophilic; NE, non-eosinophilic; CRSwNP, chronic rhinosinusitis with nasal polyps.
DISCUSSION
In the present study, we compared the profiles of 28 different immunologic markers (T cell-associated cytokine and chemokine, pro-inflammatory mediators, adhesion molecule and remodeling markers) according to the clinical phenotypes (CRSsNP and CRSwNP) and histologic subtypes (eosinophilic and non-eosinophilic) of CRSwNP. It has been known that CRSsNP showed a predominant Th1-skewed response, whereas CRSwNP were classified into 2 subtypes (E-CRSwNP: Th2-dominant response with eosinophil infiltration; NE-CRSwNP: mixed T cell subsets with neutrophilic infiltration).10,12,13 In accordance with the findings of previous studies, this study revealed that E-CRSwNP showed higher levels of Th2 cytokines than controls, whereas NE-CRSwNP significantly related to Th1/Th2/Th17 cytokines compared to controls. Unlike previous studies, we detected the signature inflammatory markers which have a significantly increased expression compared with all the other groups. The signature inflammatory markers are IL-17A, IL-1β (markers for Th17) and MMP-9 (a marker for neutrophil) in patients with NE-CRSwNP, whereas IL-5, CCL-11, MCP-4 (markers for Th2), and VCAM-1 are the signature inflammatory markers in patients with E-CRSwNP. Our results also showed the positive relationship between MMP-9 and neutrophil-associated cytokines, including IL-1α (r = 0.7257, P = 0.0021), IL-1β (r = 0.6706, P = 0.0058), IL-6 (r = 0.7500, P = 0.0012), CXCL-1 (r = 0.8853, P < 0.0001), CXCL-2 (r = 0.8000, P = 0.0003) and CXCL-8 (r = 0.6882, P = 0.0042) (data not shown). Furthermore, we could not detect the significant difference of IFN-γ expression between control, CRSsNP and CRSwNP (Table 2 and Supplementary Table S1). Several prior studies have demonstrated the increased levels of IFN-γ expression on CRSsNP.4,15,23,24,25 However, some recent studies supported our findings and it also similarly described the IFN-γ expression, which was not significantly elevated in CRSsNP.26,27,28
To date, CRSwNP accounts for approximately 20%–30% of all CRS and has been associated with a more severe clinical disease.29 The concept of this disease has been developed based on its endotypes, because CRS shows highly heterogeneity which causes different therapeutic responses.30 However, human studies are very difficult to prove the mechanism for evolution of NP. This is because CRS patients must be monitored for several years and immunologic changes must be verified by continuous testing until NP develops. Thus, to investigate the exact pathophysiology of nasal polypogenesis, the study design should be followed prospectively, not cross-sectionally. Thus, the present study has an essential limitation related to study design. To overcome this limitation, in this study, we obtained UP tissues where NP occurs commonly, as internal controls, then, compared the changes between UP and NP within the same patient. These comparisons might give us the clue to what the key protein is while nasal mucosa changes to NP, because the most common sites of origin for nasal polyposis are where the UP mucosa, the middle concha, and the ethmoid bulla are in contact with each other.31,32 Based on this paired analysis, we observed that Th2 mediators may play a role in development of NP, regardless of CRSwNP subtypes. Additionally, PCA showed there was a partial overlap between NE-CRSwNP and E-CRSwNP in terms of PC2, discriminators for Th2 mediators, which support the hypothesis that Th2 might be involved in the development of NE-CRSwNP.
Numerous studies have reported that there was a clear association between smoking history and development of CRS. Generally, cigarette smoke could induce physiologic nasal responses including increased nasal airway resistance, nasal irritation, nasal congestion, and rhinorrhea, whereas tobacco smoke extract has been demonstrated to have adverse effects on sinonasal epithelial mucociliary clearance and innate immune function. However, the exact effect of smoking on immunologic profile in CRS patients is still unclear. In the present study, we also investigated the effect of smoking history on immunologic profile according to the endotypes. We found that the neutrophils-associated mediators such as MPO and MMP-9 were up-regulated in E-CRSwNP with smoking history, whereas E-CRSwNP with no smoking history was typified as Th2 mediators such as IL-5 and MCP-4. Meanwhile, there was no any difference in NE-CRSwNP according to the smoking history (Supplementary Table S3).
This study has some limitations. First, regarding study population, asthmatic patients were not included, and male patients were the majority. It remains unclear whether sex can influence levels of cytokines in CRS mucosal tissues. Thus, this issue does not seem to bias our findings. However, our results might be relevant in a selected phenotype such as non-asthmatics because this study did not include asthmatic subjects. Secondly, the sample size was relatively small. Thirdly, the study was designed as a retrospective and cross-sectionally fashion. Therefore, future studies investigating a large sample and cohort design with a relatively long follow-up can provide additional evidence for the link between CRSsNP and CRSwNP.
In conclusion, this study shows that there are distinct immunologic profiles among subtypes of CRS. Specifically, the signature markers of NP tissues from NE-CRSwNP are IL-17A, IL-1β, and MMP-9 (Th17/neutrophilic related inflammatory markers), whereas IL-5, CCL-11, MCP-4 and VCAM-1 (Th2 related inflammatory markers) are the signature markers in NP tissues from E-CRSwNP. Moreover, the increased Th2 immune response was observed by the paired comparison between NP and UP tissues, regardless of CRSwNP subtypes.
ACKNOWLEDGMENTS
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (NRF-2015R1C1A1A01054573 to Dong-Kyu Kim and NRF-2017R1A2B4003445 to Dae Woo Kim).
Footnotes
Disclosure: There are no financial or other issues that might lead to conflict of interest.
SUPPLEMENTARY MATERIALS
The profile of inflammatory mediators in the subtype of chronic rhinosinusitis
The profile of remodeling mediators in the subtype of chronic rhinosinusitis
Coordinates of principal component analysis for the first 4 orthogonally rotated principal components: inflammatory mediators
References
- 1.Fokkens WJ, Lund VJ, Mullol J, Bachert C, Alobid I, Baroody F, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology. 2012;50:1–12. doi: 10.4193/Rhino12.000. [DOI] [PubMed] [Google Scholar]
- 2.Brandsted R, Sindwani R. Impact of depression on disease-specific symptoms and quality of life in patients with chronic rhinosinusitis. Am J Rhinol. 2007;21:50–54. doi: 10.2500/ajr.2007.21.2987. [DOI] [PubMed] [Google Scholar]
- 3.Kim DH, Han K, Kim SW. Effect of chronic rhinosinusitis with or without nasal polyp on quality of life in South Korea: 5th Korea National Health and Nutrition Examination Survey Korean. Clin Exp Otorhinolaryngol. 2016;9:150–156. doi: 10.21053/ceo.2015.01053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Zele T, Claeys S, Gevaert P, Van Maele G, Holtappels G, Van Cauwenberge P, et al. Differentiation of chronic sinus diseases by measurement of inflammatory mediators. Allergy. 2006;61:1280–1289. doi: 10.1111/j.1398-9995.2006.01225.x. [DOI] [PubMed] [Google Scholar]
- 5.Polzehl D, Moeller P, Riechelmann H, Perner S. Distinct features of chronic rhinosinusitis with and without nasal polyps. Allergy. 2006;61:1275–1279. doi: 10.1111/j.1398-9995.2006.01132.x. [DOI] [PubMed] [Google Scholar]
- 6.Van Bruaene N, Pérez-Novo CA, Basinski TM, Van Zele T, Holtappels G, De Ruyck N, et al. T-cell regulation in chronic paranasal sinus disease. J Allergy Clin Immunol. 2008;121:1435–1441. doi: 10.1016/j.jaci.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 7.Kim DK, Kang SI, Kong IG, Cho YH, Song SK, Hyun SJ, et al. Two-track medical treatment strategy according to the clinical scoring system for chronic rhinosinusitis. Allergy Asthma Immunol Res. 2018;10:490–502. doi: 10.4168/aair.2018.10.5.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tomassen P, Vandeplas G, Van Zele T, Cardell LO, Arebro J, Olze H, et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J Allergy Clin Immunol. 2016;137:1449–1456.e4. doi: 10.1016/j.jaci.2015.12.1324. [DOI] [PubMed] [Google Scholar]
- 9.Liao B, Liu JX, Li ZY, Zhen Z, Cao PP, Yao Y, et al. Multidimensional endotypes of chronic rhinosinusitis and their association with treatment outcomes. Allergy. 2018;73:1459–1469. doi: 10.1111/all.13411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ikeda K, Shiozawa A, Ono N, Kusunoki T, Hirotsu M, Homma H, et al. Subclassification of chronic rhinosinusitis with nasal polyp based on eosinophil and neutrophil. Laryngoscope. 2013;123:E1–E9. doi: 10.1002/lary.24154. [DOI] [PubMed] [Google Scholar]
- 11.Cao PP, Li HB, Wang BF, Wang SB, You XJ, Cui YH, et al. Distinct immunopathologic characteristics of various types of chronic rhinosinusitis in adult Chinese. J Allergy Clin Immunol. 2009;124:478–484. doi: 10.1016/j.jaci.2009.05.017. [DOI] [PubMed] [Google Scholar]
- 12.Shi LL, Xiong P, Zhang L, Cao PP, Liao B, Lu X, et al. Features of airway remodeling in different types of Chinese chronic rhinosinusitis are associated with inflammation patterns. Allergy. 2013;68:101–109. doi: 10.1111/all.12064. [DOI] [PubMed] [Google Scholar]
- 13.Zhang N, Van Zele T, Perez-Novo C, Van Bruaene N, Holtappels G, DeRuyck N, et al. Different types of T-effector cells orchestrate mucosal inflammation in chronic sinus disease. J Allergy Clin Immunol. 2008;122:961–968. doi: 10.1016/j.jaci.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 14.Kim DK, Jin HR, Eun KM, Mutusamy S, Cho SH, Oh S, et al. Non-eosinophilic nasal polyps shows increased epithelial proliferation and localized disease pattern in the early stage. PLoS One. 2015;10:e0139945. doi: 10.1371/journal.pone.0139945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang X, Zhang N, Bo M, Holtappels G, Zheng M, Lou H, et al. Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: a multicenter study in Europe, Asia, and Oceania. J Allergy Clin Immunol. 2016;138:1344–1353. doi: 10.1016/j.jaci.2016.05.041. [DOI] [PubMed] [Google Scholar]
- 16.Mahdavinia M, Suh LA, Carter RG, Stevens WW, Norton JE, Kato A, et al. Increased noneosinophilic nasal polyps in chronic rhinosinusitis in US second-generation Asians suggest genetic regulation of eosinophilia. J Allergy Clin Immunol. 2015;135:576–579. doi: 10.1016/j.jaci.2014.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shin HW, Kim DK, Park MH, Eun KM, Lee M, So D, et al. IL-25 as a novel therapeutic target in nasal polyps of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2015;135:1476–1485.e7. doi: 10.1016/j.jaci.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Kim DK, Jin HR, Eun KM, Mo JH, Cho SH, Oh S, et al. The role of interleukin-33 in chronic rhinosinusitis. Thorax. 2017;72:635–645. doi: 10.1136/thoraxjnl-2016-208772. [DOI] [PubMed] [Google Scholar]
- 19.Lam M, Hull L, Imrie A, Snidvongs K, Chin D, Pratt E, et al. Interleukin-25 and interleukin-33 as mediators of eosinophilic inflammation in chronic rhinosinusitis. Am J Rhinol Allergy. 2015;29:175–181. doi: 10.2500/ajra.2015.29.4176. [DOI] [PubMed] [Google Scholar]
- 20.Jeong WJ, Lee CH, Cho SH, Rhee CS. Eosinophilic allergic polyp: a clinically oriented concept of nasal polyp. Otolaryngol Head Neck Surg. 2011;144:241–246. doi: 10.1177/0194599810391738. [DOI] [PubMed] [Google Scholar]
- 21.Liu X, Dong H, Wang M, Gao Y, Zhang T, Hu G, et al. IL-1α-induced microvascular endothelial cells promote neutrophil killing by increasing MMP-9 concentration and lysozyme activity. Immunol Res. 2016;64:133–142. doi: 10.1007/s12026-015-8731-4. [DOI] [PubMed] [Google Scholar]
- 22.Owen CA. Roles for proteinases in the pathogenesis of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2008;3:253–268. doi: 10.2147/copd.s2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Bruaene N, Derycke L, Perez-Novo CA, Gevaert P, Holtappels G, De Ruyck N, et al. TGF-beta signaling and collagen deposition in chronic rhinosinusitis. J Allergy Clin Immunol. 2009;124:253–259. doi: 10.1016/j.jaci.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 24.Wang H, Li ZY, Jiang WX, Liao B, Zhai GT, Wang N, et al. The activation and function of IL-36γ in neutrophilic inflammation in chronic rhinosinusitis. J Allergy Clin Immunol. 2018;141:1646–1658. doi: 10.1016/j.jaci.2017.12.972. [DOI] [PubMed] [Google Scholar]
- 25.Shi LL, Song J, Xiong P, Cao PP, Liao B, Ma J, et al. Disease-specific T-helper cell polarizing function of lesional dendritic cells in different types of chronic rhinosinusitis with nasal polyps. Am J Respir Crit Care Med. 2014;190:628–638. doi: 10.1164/rccm.201402-0234OC. [DOI] [PubMed] [Google Scholar]
- 26.Tan BK, Klingler AI, Poposki JA, Stevens WW, Peters AT, Suh LA, et al. Heterogeneous inflammatory patterns in chronic rhinosinusitis without nasal polyps in Chicago, Illinois. J Allergy Clin Immunol. 2017;139:699–703.e7. doi: 10.1016/j.jaci.2016.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stevens WW, Ocampo CJ, Berdnikovs S, Sakashita M, Mahdavinia M, Suh L, et al. Cytokines in chronic rhinosinusitis. role in eosinophilia and aspirin-exacerbated respiratory disease. Am J Respir Crit Care Med. 2015;192:682–694. doi: 10.1164/rccm.201412-2278OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nagarkar DR, Poposki JA, Tan BK, Comeau MR, Peters AT, Hulse KE, et al. Thymic stromal lymphopoietin activity is increased in nasal polyps of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013;132:593–600.e12. doi: 10.1016/j.jaci.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tan BK, Chandra RK, Pollak J, Kato A, Conley DB, Peters AT, et al. Incidence and associated premorbid diagnoses of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013;131:1350–1360. doi: 10.1016/j.jaci.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim DW, Cho SH. Emerging endotypes of chronic rhinosinusitis and its application to precision medicine. Allergy Asthma Immunol Res. 2017;9:299–306. doi: 10.4168/aair.2017.9.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stammberger H. Endoscopic endonasal surgery--concepts in treatment of recurring rhinosinusitis. Part I. Anatomic and pathophysiologic considerations. Otolaryngol Head Neck Surg. 1986;94:143–147. doi: 10.1177/019459988609400202. [DOI] [PubMed] [Google Scholar]
- 32.Stammberger H, Posawetz W. Functional endoscopic sinus surgery. Concept, indications and results of the Messerklinger technique. Eur Arch Otorhinolaryngol. 1990;247:63–76. doi: 10.1007/BF00183169. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The profile of inflammatory mediators in the subtype of chronic rhinosinusitis
The profile of remodeling mediators in the subtype of chronic rhinosinusitis
Coordinates of principal component analysis for the first 4 orthogonally rotated principal components: inflammatory mediators