Abstract
BACKGROUND:
Administering oxygen therapy (OT) has an essential role in preventing/managing hypoxemia in both acute and chronic conditions. It should be adjusted to achieve the normal oxygen saturation of 94%–98% in most cases. This study aims to evaluate knowledge, attitude and practice (KAP) of nurses, paramedics, emergency medical technicians (EMTs) and Emergency Medical Services (EMS) physicians working at emergency departments (ED) in Riyadh, Saudi Arabia.
METHODS:
In this cross-sectional study, a structured questionnaire was used to assess KAP related to OT of nurses, paramedics, EMTs and EMS physicians currently working at an ED of a tertiary care hospital. Knowledge and attitude were assessed using a Likert scale from 1–5, whereas practice was assessed as a yes/no categorical variable.
RESULTS:
A total of 444 emergency health-care workers (EHCWs) participated, of which 225 (50.7%) were male, with the majority (77%) in the age group of 20–35 years. Over half of the sample were nurses (266; 59.9%). The mean score for knowledge about OT was 5.51±1.45, attitude was 26.31±3.17 and for practices 4.55±1.76. The main factors which were associated with poor KAP were workload and lack of local guidelines. The distribution of overall practice score was significantly better among paramedics – nurses group and EMT – nurses group.
CONCLUSION:
This study demonstrates that there is a gap in EHCWs’ KAP, particularly regarding when to provide OT to a patient. This gap can affect patients’ safety. Extensive educational and training programs about OT are needed to raise awareness among health-care providers.
Keywords: Emergency medicine, Oxygen therapy, Knowledge, Attitude, Practice
INTRODUCTION
Oxygen therapy (OT) is a medical treatment prescribed mainly for hypoxic patients; OT provides oxygen at higher concentrations than that found in atmosphere (>21%).[1] It is listed as a core item on the World Health Organizations (WHO) model of essential medicines, which is a list of the most effective and safe drugs used in a health care system.[2] OT is considered as a key instrument in resuscitating pre-hospital trauma patients during evaluation and transportation by Emergency Medical Services (EMS).[3,4] It is also believed to be an essential treatment for a wide range of hospitalized patients in the developed world as it plays a vital role in improving saturation and reducing effort of breathing. OT has a pivotal role in saving the lives of many patients with heart and lung diseases if used at an appropriate time and in an appropriate amount according to the recently updated guidelines.[2,5]
The British Thoracic Society (BTS) guideline for emergency oxygen use in adult patients emphasized the achievement of normal or near-normal oxygen saturation level for the majority of patients in an emergency department (ED) or intensive care unit.[6] The optimal amount and method of oxygen delivery varies depending on a patient’s underlying medical condition and whether the condition is acute or chronic. The selection of the best oxygen delivery device and flow rate of oxygen depends on many factors some of which are the patient’s age, the therapeutic goals and patient tolerance. Even though OT is one of the most widely used resuscitation methods, it may harm or cause a patient’s status to deteriorate if used inappropriately. Pulmonary oxygen toxicity and oxygen-induced hypercapnia are considered as two of the major side effects of OT.[7,8] A favorable effect that improves survival rates has been reported at OT saturations between 94% and 98% for acutely ill patients; however, lower saturation, 88%–92% should be considered for patients with suspected risk of hypercapnic respiratory failure.[8] A study done in Bethesda on trauma patients admitted to an ED, reported that the mortality rate in patients who received pre-hospital OT was higher than those who did not receive OT.[9]
Long-term OT is the provision of oxygen supplement over a minimum of 15 hours per day including overnight period. The benefit of long-term OT has been controversial and much disputed within the field of chronic obstructive pulmonary disease.[5,10] According to Kim et al,[11] OT in patients with mild or moderate hypoxemia may improve their neurocognitive function and quality of life but it might not reduce the mortality rate. More literature has emerged that offers contradictory findings on the use of OT in patients with acute exacerbation of chronic obstructive pulmonary disease. Some trials have shown a significant improvement in survival rate among patients with severely hypoxic chronic obstructive pulmonary disease while some trials showed the opposite among less severely hypoxic patients: partial pressure of oxygen in arterial blood (PaO2) <69 mmHg.[12-15] Furthermore, a study done in New Zealand reported that the number of patients receiving high concentration OT decreased significantly following the implementation of an educational program about pre-hospital oxygen delivery by paramedics to all patients with acute exacerbation of chronic obstructive pulmonary disease between 2005 and 2010.[16]
To the best of our knowledge, no study has been conducted in Saudi Arabia to identify the depth of knowledge, attitude and practice (KAP) among nurses, paramedics, emergency medical technicians (EMTs) and EMS physicians on OT at an ED department. A study was conducted in 2015, in Addis Ababa, Ethiopia, showed a clear gap in nurses’ KAP and mentioned some possible contributing factors. These factors included: lack of OT guidelines, inadequate training, heavy workload on ED and inadequate oxygen delivery devices.[17] Therefore, this study aims to assess and identify factors associated with poor KAP on OT specifically in King Abdulaziz Medical City (KAMC), King Saud Medical City (KSMC), King Khalid University Hospital (KKUH) and Saudi Red Crescent (SRC). Education programs on best practice on OT through conferences, courses, workshops, lectures and research are needed to raise awareness and to develop a clear policy that follows guidelines.
METHODS
A cross-sectional study was conducted from October 2017 to January 2018 at four main tertiary care hospitals in Riyadh, Saudi Arabia. The study included 444 nurses, paramedics, EMTs and EMS physicians who worked at KAMC, KSMC, KKUH and SRC between 2017 and 2018. Interns were excluded from this study.
With a 5% margin of error, 95% confidence level, prevalence of 50%, a sample size of 280 was calculated and an extra 36% was taken for non-responses. A total of 444 health care providers working in an ED were selected through purposive sampling. A questionnaire in English was adopted from a previous study done by Weldetsadik.[17] As Weldetsadik’s study was done with nurses, a few questions relating to paramedics, EMTs and EMS physicians were added to the original items.[17] Reliability and content validity was done before final data collection through pilot testing. The questionnaire included demographic information such as gender, age, category of profession and total duration of work. There were an additional four sections: OT knowledge, OT attitude, OT practice and OT-associated factors. The questions were asked using a Likert scale in which “strongly agree” scored five and “strongly disagree” scored one. The questionnaire was self-administered by the participants and collected one hour after distribution on the same day.
The Statistical Package for the Social Sciences V.23 (SPSS) was used for data management and analysis. Descriptive statistics were used to assess the baseline demographics; they were carried out by calculating the frequencies and percentages comparing those who had a fall and those who had not. Prevalence was calculated with a 95%CI. Univariate and bivariate analyses of logistic regression were conducted to investigate risk factors related to falls. The model was run using all predictors at one time to obtain the OR by adjusting for other predictors. The 95%CI, OR and adjusted OR (aOR) were reported. All tests were considered significant if the P value was less than 0.05. After data collection, the questionnaires were entered in an Excel file and checked for correctness. Data were managed and analyzed using SPSS. The mean scores were calculated for the KAP and categorized further into categorical variables: knowledge was reported as having knowledge or no knowledge; attitude was presented as positive and negative attitude; and practices were categorized as good and bad practices. All the categories were done based on a Likert scale of 1 to 5. An ANOVA test was applied and Bonferroni post hoc analysis was done to identify the group which was better than the rest in the case of positive association. For all the tests applied P<0.05 was considered significant.
RESULTS
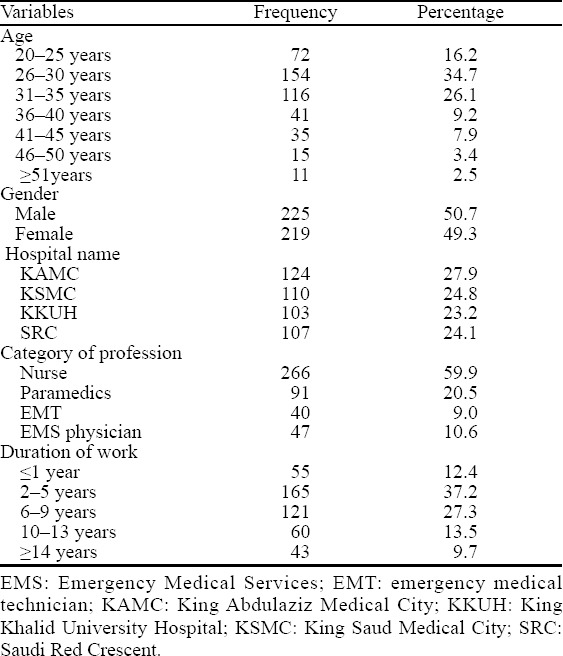
A total of 444 emergency health care workers (EHCWs) participated in this study (Table 1). Of the EHCWs, 342 (77%) were between the age of 20 and 35 years. The proportion of male to female was almost equal with slightly more males: 225 (50.7%). Over half of the sample were nurses, 266 (59.9%), 91 (20.5%) were paramedics, 47 (10.6%) were EMS physicians and 40 (9%) were EMTs. The sample was almost equally divided among all the four hospitals. The majority of participants had 2–9 years, 286 (64.5%), of work experience.
Table 1.
Demographic characteristics of participants (n=444)
Knowledge
There were ten questions concerning knowledge in KAP questionnaire (Tables 2, 3). The mean knowledge score was 5.51±1.45. Among the total participants, only 55 (12.4%) were aware that OT should be administered for both treating and preventing hypoxia while 310 (69.8%) were fully aware of OT contraindication. When asked about the normal oxygen saturation at rest for adults <70 years old, 323 (72.7%) of them answered correctly. Most of the respondents (374, 84.2%) were aware that OT might be harmful to their patients if used inappropriately; however, only 52 (11.7%) knew that patients with ST-elevation myocardial infarction and oxygen ≥90% on room air do not require OT.
Table 2.
Participants’ knowledge, attitude and practice toward oxygen therapy represented by number and percentage (n=444)
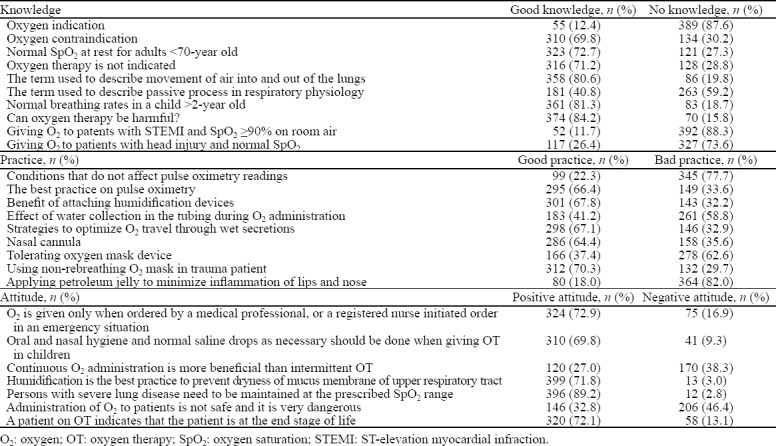
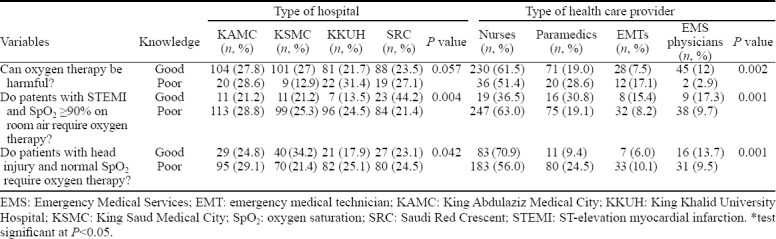
Table 3.
Distribution of knowledge across the hospital type and health care provider (n=444)
Practice
Practice was assessed with nine questions and the mean practice score was 4.55±1.76 (Table 2). All participants who got ≥4 points were considered to have positive practice toward OT. The majority (77.7%) stated that pulse oximetry monitoring is not affected by all the following: patient motion, carbon monoxide poisoning, jaundice/anemia, false nails and nail varnish and only 22.3% gave responses that represented good practice. More than two thirds of the participants (67.8%) reported good practice by attaching a humidification device to reduce the risk of side effects associated with dry gas administration and to promote patient comfort. Only 18% of participants agreed that applying a petroleum jelly on a patient’s lips and nose is not appropriate during OT. When respondents were asked about a favorable device to deliver high percentage of oxygen saturation (60%–90%) for a short-term trauma patient, 312 (70.3%) responded with the correct practice.
Attitude
Attitude was assessed with seven questions, three of them were reversed score (Table 3). The mean attitude score was 26.31±3.17 (males 25.23±3.16 and females 27.42±2.77). The total attitude score based on demographics showed a significantly higher score among the age group of 46–50 years. In addition, females had significantly higher attitude score than males (P=0.04). The assessment by hospital showed that SRC had a lower mean attitude score than the other hospitals with a significant difference based on Bonferroni post hoc analysis with P<0.000. Also, KKUH had a lower attitude score than KSMC (P=0.037). Health care workers who had ≤1 year of experience showed a significantly lower attitude score than all others with P<0.000.
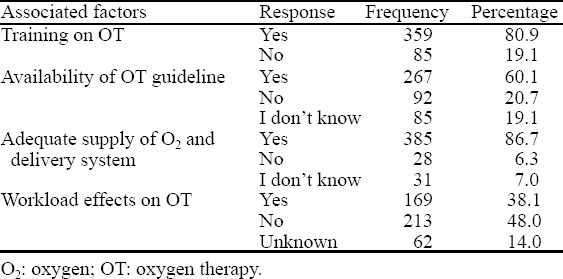
Among all 444 participants, 80.9% (359) were trained on how to provide OT to patients and 267 (60.1%) were aware of the existence of OT guideline in their ED. Interestingly, 85 (19.1%) did not know whether any guidelines were even available. Almost 169 (38.1%) reported excessive workload affecting the quality of patient care (Table 4).
Table 4.
Associated factors of poor knowledge, attitude and practice toward oxygen therapy
DISCUSSION
This study focused on the KAP of health care providers working in an ED setting in tertiary care hospitals about the OT given to patients. Results showed that majority of EHCW have a moderate to high knowledge about OT contraindication and poor knowledge about OT indications. This poor knowledge in using OT in those critical situations could deteriorate patients’ condition and outcome. Therefore, EHCWs need further education about the risk of administering OT to patients with ST-elevation myocardial infarction and trauma. The distribution of knowledge score was significantly better among EMT – paramedics group, EMT – nurses group and EMT – EMS physicians group than all other participants, with a significant P value of 0.035, 0.003 and 0.004, respectively thus, the EMT group had better knowledge than all other participants. A study in Texas reported that after two years of experience, the average loss of didactic knowledge for EMTs and paramedics was 11% greater in paramedics than in EMTs.[18] This might be attributed to the frequency of applying OT.[18] Another possible explanation for this finding is that the workload of EMTs is less than the workload of other groups, which gives them more time to read. Further research is needed to explore the reasons for these results.
Good attitude and practice pattern regarding OT was low in more than half of participants in this study. According to the clinical guidelines for the administration of oxygen in adults (Nottingham University Hospitals NHS Trust), OT should be used with caution in patients with ischemic heart disease and stroke.[19] In the current study, knowledge wise, more than 15% of participants incorrectly stated that oxygen can never be harmful, which is in line with the attitude of 32.8% of the participants who believed that using OT is very safe for any condition. In comparison with the current study, the previous study done in in Addis Ababa, Ethiopia, showed lower knowledge and attitude mean score than this study.[17]
Regarding practice of OT, the main concern was about optimizing a patient’s benefit by using the appropriate oxygen devices and the best practices on pulse oximetry specifically. The distribution of overall practice score was significantly better among paramedics – nurses group and EMT – nurses group with a significant P value of 0.000 and 0.004, respectively. There was no significant different in practice scores between different hospitals. Out of the total number of participants, 11% thought that OT is not indicated in patients with carbon monoxide poisoning, which is a bad mistake, and most of these participants were nurses. Also, half of the respondents did not agree that carbon monoxide poisoning could affect oxygen saturation reading on pulse oximetry. This demonstrates a clear practice gap on OT and effort should be applied in educational and awareness programs to close this gap. This result was in line with another multi-center study done in Serbia in 2016, which emphasized that nurses have low scores in understanding how pulse oximetry works and the conditions that affect reliability and accuracy of the readings.[20]
The possible associated leading factors for these findings were identified; they include but are not limited to: shortage of training programs, unavailability of national OT guideline, excessive workload, and insufficient supply of oxygen and delivery devices. Further investigation is required to identify the causes of poor knowledge in OT. The lack of availability of a national OT guideline leaves a space for EHCWs, especially nurses, paramedics, EMTs and EMS physicians, to manage the treatment based on their own cumulative experience. Even though cumulative experience may help, it does not always ensure that patients’ treatment is of good quality. Developing a locally updated OT guideline and recommendations would eventually support practitioners’ work.
This study had certain limitations, and thus the results might not represent KAP of the whole population. The study used nonrandom sampling, which is a limitation, but the data were collected from four different hospitals and the results segregated accordingly to cater for this limitation to some extent. Also, the self-reporting nature of the data collection is a limitation in that some participants might have under-reported or over-reported their views. Another limitation is the mode of data collection at the work setting itself. Many people are busy during their usual work hours and may have read the questionnaire with incomplete concentration; this could have led to some under-reporting or over-reporting of the results. Despite these limitations, the strength of the study is the inclusion of four main tertiary care hospitals and it can be considered representative of other hospitals settings as well.
CONCLUSION
In conclusion, this study demonstrates that there is a clear gap of KAP among all groups of participants related to OT use. The possible associated factors for this gap included shortage of training programs, unavailability of national OT guideline and excessive workload. Education programs on the occupational use of OT through conferences, workshops, research and lectures are needed to raise the awareness of health care workers about OT. Also, the participants need to be made aware of the recent updated guidelines for OT.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Institutional Review Board King Abdullah International Medical Research Center as well as Nursing Research Committee, in Riyadh, Saudi Arabia. All questionnaire forms were accompanied by a cover letter explaining the purpose of the study and clearly stating that anonymity and confidentiality of all participants would be guaranteed. Informed written consent was obtained from participants. Informed consents were written in both Arabic and English language.
Conflicts of Interest: The authors declare that they have no competing interests. All of the authors have approved the final article to be submitted.
Contributors: AFO designed the study, collected the data, and wrote the manuscript. FAM, RNG, FIN, AFD collected the data. NAJ designed the study, supervised the conductance of the survey and reviewed the manuscript. NM performed the statistical analysis and reviewed the manuscript. All authors interpreted the results, participated in the related discussions, and read and approved the final version of the manuscript.
REFERENCES
- 1.Chakrabarti B, Calverley PM. Management of acute ventilatory failure. Postgraduate Medical Journal. 2006;82(969):438–45. doi: 10.1136/pgmj.2005.043208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization (WHO) Essential medicines and health products: WHO Model Lists of Essential Medicines. Geneva: WHO; 2016. pp. 33–47. [Google Scholar]
- 3.McMullan J, Rodriquez D, Hart KW, Lindsell CJ, Vonderschmidt K, et al. Prevalence of Pre-hospital Hypoxemia and Oxygen Use in Trauma Patients. Journal of Surgery Pakistan. 2013;178(10):1121–5. doi: 10.7205/MILMED-D-13-00126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adib-Hajbaghery M, Maghaminejad F, Paravar M. The quality of pre-hospital oxygen therapy in patients with multiple trauma: a cross-sectional study. Iran Red Crescent Med J. 2014;16(3):e14274. doi: 10.5812/ircmj.14274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hardinge M, Annandale J, Bourne S, Cooper B, Evans A, Freeman D, et al. British Thoracic Society Home Oxygen Guideline Development Group; British Thoracic Society Standards of Care Committee. British Thoracic Society guidelines for home oxygen use in adults. Thorax. 2015;70(1):1–43. [Google Scholar]
- 6.Beasley R, Chien J, Douglas J, Eastlake L, Farah C, King G, et al. Thoracic Society of Australia and New Zealand oxygen guidelines for acute oxygen use in adults:'Swimming between the flags'. Respirology. 2015;20(8):1182–91. doi: 10.1111/resp.12620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Newnam KM. Oxygen saturation limits and evidence supporting the targets. Adv Neonatal Care. 2014;14(6):403–9. doi: 10.1097/ANC.0000000000000150. [DOI] [PubMed] [Google Scholar]
- 8.Kane BI, Decalmer SA, O'Driscoll BR. Emergency oxygen therapy: from guideline to implementation. Breathe. 2013;9:246–53. [Google Scholar]
- 9.Stockinger ZT, Mcswain NE. Prehospital supplemental oxygen in trauma patients: its efficacy and implications for military medical care. Mil Med. 2004;169(8):609–12. doi: 10.7205/milmed.169.8.609. [DOI] [PubMed] [Google Scholar]
- 10.Ekström M. Clinical usefulness of long-term oxygen therapy in adults. N Engl J Med. 2016;375(17):1683–4. doi: 10.1056/NEJMe1611742. [DOI] [PubMed] [Google Scholar]
- 11.Kim V, Benditt JO, Wise RA, Sharafkhaneh A. Oxygen therapy in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5(4):513–8. doi: 10.1513/pats.200708-124ET. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nocturnal Oxygen Therapy Trial Group. Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung disease: a clinical trial. Ann Intern Med. 1980;93(3):391–8. doi: 10.7326/0003-4819-93-3-391. [DOI] [PubMed] [Google Scholar]
- 13.The Medical Research Council Working Party. Long term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysema. Lancet. 1981;1(8222):681–6. [PubMed] [Google Scholar]
- 14.Chaouat A, Weitzenblum E, Kessler R, Charpentier C, Ehrhart M, Schott R, et al. A randomized trial of nocturnal oxygen therapy in chronic obstructive pulmonary disease patients. Eur Respir J. 1999;14(5):1002–8. doi: 10.1183/09031936.99.14510029. [DOI] [PubMed] [Google Scholar]
- 15.Górecka D, Gorzelak K, Sliwiński P, Tobiasz M, Zieliński J. Effect of long-term oxygen therapy on survival in patients with chronic obstructive pulmonary disease with moderate hypoxaemia. Thorax. 1997;52(8):674–9. doi: 10.1136/thx.52.8.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pilcher J, Cameron L, Braithwaite I, Bowles D, Swain A, Bailey M, et al. Comparative audit of oxygen use in the prehospital setting in acute COPD exacerbation over 5 years. Emerg Med J. 2015;32(3):234–8. doi: 10.1136/emermed-2013-203094. [DOI] [PubMed] [Google Scholar]
- 17.Weldetsadik AS. Assessment of nurse's knowledge, attitude and practice about oxygen therapy at emergency departments of one federal and three regional hospitals in Addis Ababa, Ethiopia. 2015. http://etd.aau.edu.et/handle/123456789/1888?show=full .
- 18.Latman NS, Wooley K. Knowledge and skill retention of emergency care attendants, EMT-As, and EMT-Ps. Ann Emerg Med. 1980;9(4):183–9. doi: 10.1016/s0196-0644(80)80003-5. [DOI] [PubMed] [Google Scholar]
- 19.Douglas E. Guidelines for Administration of Oxygen in Adults and Paediatrics Excluding Inpatients on the Neonatal Unit. Nottingham University Hospitals NHS Trust. 2017. https://www.nuh.nhs.uk/download.cfm?doc=docm93jijm4n1229 .
- 20.Milutinović D, Repić G, Aranđelović B. Clinical nurses'knowledge level on pulse oximetry: A descriptive multi-center study. Intensive Crit Care Nurs. 2016;37:19–26. doi: 10.1016/j.iccn.2016.05.006. [DOI] [PubMed] [Google Scholar]


