| KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD) | |
| 3 | Tables and supplementary material |
| 6 | KDIGO Executive Committee |
| 7 | Reference keys |
| 8 | CKD nomenclature |
| 9 | Conversion factors |
| 10 | Abbreviations and acronyms |
| 11 | Notice |
| 12 | Foreword |
| 13 | Work Group membership |
| 14 | Abstract |
| 15 | Summary of KDIGO CKD-MBD recommendations |
| 19 | Summary and comparison of 2017 updated and 2009 KDIGO CKD-MBD recommendations |
| 22 | Chapter 3.2: Diagnosis of CKD-MBD: bone |
| 25 | Chapter 4.1: Treatment of CKD-MBD targeted at lowering high serum phosphate and maintaining serum calcium |
| 33 | Chapter 4.2: Treatment of abnormal PTH levels in CKD-MBD |
| 38 | Chapter 4.3: Treatment of bone with bisphosphonates, other osteoporosis medications, and growth hormone |
| 39 | Chapter 5: Evaluation and treatment of kidney transplant bone disease |
| 41 | Methodological approach to the 2017 KDIGO CKD-MBD guideline update |
| 49 | Biographic and disclosure information |
| 55 | Acknowledgments |
| 56 | References |
Tables
| 24 | Table 1. Utility of KDOQI and KDIGO PTH thresholds for diagnostic decision making |
| 42 | Table 2. Research questions |
| 45 | Table 3. Question-specific eligibility criteria |
| 46 | Table 4. GRADE system for grading quality of evidence for an outcome |
| 47 | Table 5. Final grade for overall quality of evidence |
| 47 | Table 6. Balance of benefits and harms |
| 47 | Table 7. Implications of the strength of a recommendation |
| 47 | Table 8. Determinants of strength of recommendation |
Supplementary Material
| Appendix A. PubMed search strategy |
| Appendix B. Summary of search and review process |
| Table S1. Summary table of randomized controlled trials examining the treatment of CKD-MBD with bisphosphonates in CKD G3a–G5: study characteristics |
| Table S2. Summary table of randomized controlled trials examining the treatment of CKD-MBD with bisphosphonates in CKD G3a–G5: study population characteristics |
| Table S3. Summary table of randomized controlled trials examining the treatment of CKD-MBD with bisphosphonates in CKD G3a–G5: results |
| Table S4. Summary table of randomized controlled trials examining the treatment of CKD-MBD with bisphosphonates in CKD G3a–G5: quality |
| Table S5. Evidence matrix of randomized controlled trials examining the treatment of CKD-MBD with bisphosphonates in CKD G3a–G5 |
| Table S6. Evidence profile of randomized controlled trials examining the treatment of CKD-MBD with bisphosphonates in CKD G3a–G5 |
| Table S7. Summary table of studies evaluating the ability of bone mineral density results to predict fracture or renal osteodystrophy among patients with CKD G3a–G5: study characteristics |
| Table S8. Summary table of studies evaluating the ability of bone mineral density results to predict fracture or renal osteodystrophy among patients with CKD G3a–G5: study population characteristics |
| Table S9. Summary table of studies evaluating the ability of bone mineral density results to predict fracture or renal osteodystrophy among patients with CKD G3a–G5: results |
| Table S10. Summary table of studies evaluating the ability of bone mineral density results to predict fracture or renal osteodystrophy among patients with CKD G3a–G5: quality |
| Table S11. Evidence matrix of studies evaluating the ability of bone mineral density results to predict fracture or renal osteodystrophy among patients with CKD G3a–G5 |
| Table S12. Evidence profile of studies evaluating the ability of bone mineral density results to predict fracture or renal osteodystrophy among patients with CKD G3a–G5 |
| Table S13. Summary table of randomized controlled trials examining the treatment of CKD-MBD with varying dialysate calcium concentration levels in CKD G5D: study characteristics |
| Table S14. Summary table of randomized controlled trials examining the treatment of CKD-MBD with varying dialysate calcium concentration levels in CKD G5D: study population characteristics |
| Table S15. Summary table of randomized controlled trials examining the treatment of CKD-MBD with varying dialysate calcium concentration levels in CKD G5D: results |
| Table S16. Summary table of randomized controlled trials examining the treatment of CKD-MBD with varying dialysate calcium concentration levels in CKD G5D: quality |
| Table S17. Evidence matrix of randomized controlled trials examining the treatment of CKD-MBD with varying dialysate calcium concentration levels in CKD G5D |
| Table S18. Evidence profile of randomized controlled trials examining the treatment of CKD-MBD with varying dialysate calcium concentration levels in CKD G5D |
| Table S19. Summary table of randomized controlled trials examining the treatment of CKD-MBD with calcium-containing phosphate binders versus calcium-free phosphate binders: study characteristics |
| Table S20. Summary table of randomized controlled trials examining the treatment of CKD-MBD with calcium-containing phosphate binders versus calcium-free phosphate binders: study population characteristics |
| Table S21. Summary table of randomized controlled trials examining the treatment of CKD-MBD with calcium-containing phosphate binders versus calcium-free phosphate binders: results |
| Table S22. Summary table of randomized controlled trials examining the treatment of CKD-MBD with calcium-containing phosphate binders versus calcium-free phosphate binders: quality |
| Table S23. Evidence matrix of randomized controlled trials examining the treatment of CKD-MBD with calcium-containing phosphate binders versus calcium-free phosphate binders |
| Table S24. Evidence profile of randomized controlled trials examining the treatment of CKD-MBD with calcium-containing phosphate binders versus calcium-free phosphate binders |
| Table S25. Summary table of randomized controlled trials examining the treatment of CKD-MBD with dietary phosphate: study characteristics |
| Table S26. Summary table of randomized controlled trials examining the treatment of CKD-MBD with dietary phosphate: study population characteristics |
| Table S27. Summary table of randomized controlled trials examining the treatment of CKD-MBD with dietary phosphate: results |
| Table S28. Summary table of randomized controlled trials examining the treatment of CKD-MBD with dietary phosphate: quality |
| Table S29. Evidence matrix of randomized controlled trials examining the treatment of CKD-MBD with dietary phosphate |
| Table S30. Evidence profile of randomized controlled trials examining the treatment of CKD-MBD with dietary phosphate |
| Table S31. Summary table of randomized controlled trials examining the treatment of PTH in CKD-MBD: study characteristics |
| Table S32. Summary table of randomized controlled trials examining the treatment of PTH in CKD-MBD: study population characteristics |
| Table S33. Summary table of randomized controlled trials examining the treatment of PTH in CKD-MBD: results |
| Table S34. Summary table of randomized controlled trials examining the treatment of PTH in CKD-MBD: quality |
| Table S35. Evidence matrix of randomized controlled trials examining the treatment of PTH in CKD-MBD |
| Table S36. Evidence profile of randomized controlled trials examining the treatment of PTH in CKD-MBD |
| Table S37. Summary table of randomized controlled trials examining the treatment of high levels of PTH with calcitriol or activated vitamin D analogs in CKD G3a–G5 not on dialysis: study characteristics |
| Table S38. Summary table of randomized controlled trials examining the treatment of high levels of PTH with calcitriol or activated vitamin D analogs in CKD G3a–G5 not on dialysis: study population characteristics |
| Table S39. Summary table of randomized controlled trials examining the treatment of high levels of PTH with calcitriol or activated vitamin D analogs in CKD G3a–G5 not on dialysis: results |
| Table S40. Summary table of randomized controlled trials examining the treatment of high levels of PTH with calcitriol or activated vitamin D analogs in CKD G3a–G5 not on dialysis: quality |
| Table S41. Evidence matrix of randomized controlled trials examining the treatment of high levels of PTH with calcitriol or activated vitamin D analogs in CKD G3a–G5 not on dialysis |
| Table S42. Evidence profile of randomized controlled trials examining the treatment of high levels of PTH with calcitriol or activated vitamin D analogs in CKD G3a–G5 not on dialysis |
| Table S43. Summary table of randomized controlled trials examining the treatment of high levels of PTH in CKD G5D: study characteristics |
| Table S44. Summary table of randomized controlled trials examining the treatment of high levels of PTH in CKD G5D: study population characteristics |
| Table S45. Summary table of randomized controlled trials examining the treatment of high levels of PTH in CKD G5D: results |
| Table S46. Summary table of randomized controlled trials examining the treatment of high levels of PTH in CKD G5D: quality |
| Table S47. Evidence matrix of randomized controlled trials examining the treatment of high levels of PTH in CKD G5D |
| Table S48. Evidence profile of randomized controlled trials examining the treatment of high levels of PTH in CKD G5D |
| Table S49. Summary table of studies evaluating different concentrations of serum phosphate or calcium among patients with CKD G3a–G5 or G5D: study characteristics |
| Table S50. Summary table of studies evaluating different concentrations of serum phosphate or calcium among patients with CKD G3a–G5 or G5D: study population characteristics |
| Table S51. Summary table of studies evaluating different concentrations of serum phosphate among patients with CKD G3a–G5 or G5D: results |
| Table S52. Summary table of studies evaluating different concentrations of serum calcium among patients with CKD G3a–G5 or G5D: results |
| Table S53. Summary table of studies evaluating different concentrations of serum phosphate or calcium among patients with CKD G3a–G5 or G5D: quality |
| Table S54. Evidence matrix of studies evaluating different concentrations of serum phosphate or calcium among patients with CKD G3a–G5 or G5D |
| Table S55. Evidence profile of studies evaluating different concentrations of serum phosphate or calcium among patients with CKD G3a–G5 or G5D |
Supplementary material is linked to the online version of the paper at www.kisupplements.org.
KDIGO Executive Committee
| Garabed Eknoyan, MD Norbert Lameire, MD, PhD Founding KDIGO Co-chairs | |
| Bertram L. Kasiske, MD Immediate Past Co-chair | |
| David C. Wheeler, MD, FRCP KDIGO Co-chair |
Wolfgang C. Winkelmayer, MD, MPH, ScD KDIGO Co-chair |
| Ali K. Abu-Alfa, MD Olivier Devuyst, MD, PhD Jürgen Floege, MD John S. Gill, MD, MS Kunitoshi Iseki, MD Andrew S. Levey, MD Zhi-Hong Liu, MD |
Ziad A. Massy, MD, PhD Roberto Pecoits-Filho, MD, PhD Brian J.G. Pereira, MBBS, MD, MBA Paul E. Stevens, MB, FRCP Marcello A. Tonelli, MD, SM, FRCPC Angela Yee-Moon Wang, MD, PhD, FRCP Angela C. Webster, MBBS, MM (Clin Ep), PhD |
|
KDIGO Staff John Davis, Chief Executive Officer Danielle Green, Managing Director Michael Cheung, Chief Scientific Officer Tanya Green, Communications Director Melissa McMahan, Programs Director | |
Reference keys
Nomenclature and Description for Rating Guideline Recommendations
Within each recommendation, the strength of recommendation is indicated as Level 1, Level 2, or not graded, and the quality of the supporting evidence is shown as A, B, C, or D.
| Grade∗ | Implications |
||
|---|---|---|---|
| Patients | Clinicians | Policy | |
|
Level 1 “We recommend” |
Most people in your situation would want the recommended course of action, and only a small proportion would not. | Most patients should receive the recommended course of action. | The recommendation can be evaluated as a candidate for developing a policy or a performance measure. |
|
Level 2 “We suggest” |
The majority of people in your situation would want the recommended course of action, but many would not. | Different choices will be appropriate for different patients. Each patient needs help to arrive at a management decision consistent with her or his values and preferences. | The recommendation is likely to require substantial debate and involvement of stakeholders before policy can be determined. |
The additional category “not graded” is used, typically, to provide guidance based on common sense or when the topic does not allow adequate application of evidence. The most common examples include recommendations regarding monitoring intervals, counseling, and referral to other clinical specialists. The ungraded recommendations are generally written as simple declarative statements, but are not meant to be interpreted as being stronger recommendations than Level 1 or 2 recommendations.
| Grade | Quality of evidence | Meaning |
|---|---|---|
| A | High | We are confident that the true effect lies close to that of the estimate of the effect. |
| B | Moderate | The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. |
| C | Low | The true effect may be substantially different from the estimate of the effect. |
| D | Very low | The estimate of effect is very uncertain, and often will be far from the truth. |
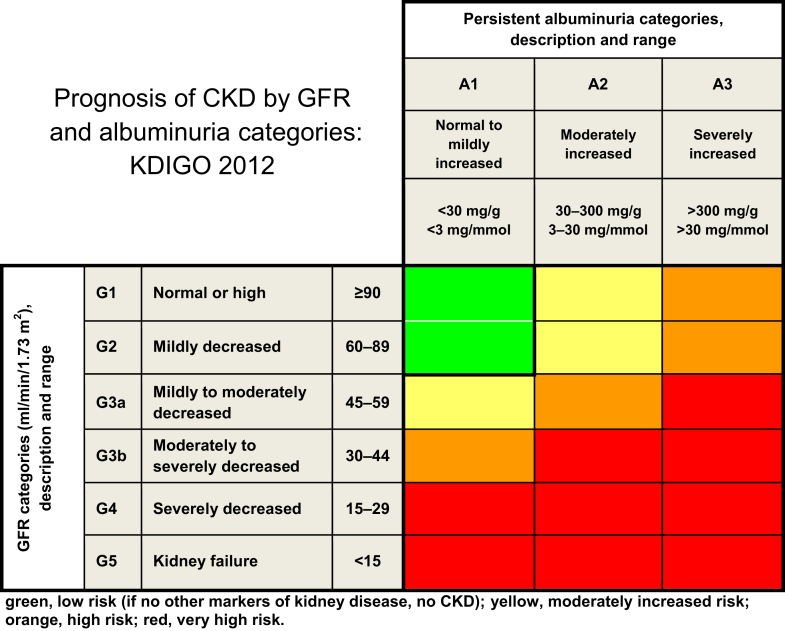
Current Chronic Kidney Disease (CKD) Nomenclature Used by KDIGO
CKD is defined as abnormalities of kidney structure or function, present for > 3 months, with implications for health. CKD is classified based on cause, GFR category (G1–G5), and albuminuria category (A1–A3), abbreviated as CGA.
Prognosis of CKD by GFR and albuminuria category
Conversion Factors of Conventional Units to SI Units
| Conventional unit | Conversion factor | SI unit | |
|---|---|---|---|
| Calcium, total | mg/dl | 0.2495 | mmol/l |
| Calcium, ionized | mg/dl | 0.25 | mmol/l |
| Creatinine | mg/dl | 88.4 | μmol/l |
| Parathyroid hormone | pg/ml | 0.106 | pmol/l |
| Phosphate (inorganic) | mg/dl | 0.3229 | mmol/l |
Note: conventional unit × conversion factor = SI unit.
Abbreviations and acronyms
| 1,25(OH)2D | 1,25-dihydroxyvitamin D |
| 25(OH)D | 25-hydroxyvitamin D |
| AUC | area under the curve |
| bALP | bone-specific alkaline phosphatase |
| BMD | bone mineral density |
| CAC | coronary artery calcification |
| CI | confidence interval |
| CT | computed tomography |
| CV | coefficient of variation |
| DXA | dual-energy X-ray absorptiometry |
| eGFR | estimated glomerular filtration rate |
| ERT | evidence review team |
| FGF | fibroblast growth factor |
| FRAX | fracture risk assessment tool |
| GFR | glomerular filtration rate |
| GI | gastrointestinal |
| GRADE | Grading of Recommendations Assessment, Development, and Evaluation |
| HD | hemodialysis |
| HPT | hyperparathyroidism |
| HR | hazard ratio |
| iPTH | intact parathyroid hormone |
| ISCD | International Society of Clinical Densitometry |
| ITT | intention-to-treat |
| IU | international unit |
| KDIGO | Kidney Disease: Improving Global Outcomes |
| KDOQI | Kidney Disease Outcomes Quality Initiative |
| LVH | left ventricular hypertrophy |
| LVMI | left ventricular mass index |
| MRI | magnetic resonance imaging |
| OR | odds ratio |
| P1NP | amino-terminal propeptide of type 1 procollagen |
| PTH | parathyroid hormone |
| RCT | randomized controlled trial |
| ROC | receiver operating characteristic |
| SD | standard deviation |
| SHPT | secondary hyperparathyroidism |
| VDR | vitamin D receptor |
Notice
Section I: Use of the Clinical Practice Guideline
This Clinical Practice Guideline Update is based upon systematic literature searches last conducted in September 2015 supplemented with additional evidence through February 2017. It is designed to assist decision making. It is not intended to define a standard of care, and should not be interpreted as prescribing an exclusive course of management. Variations in practice will inevitably and appropriately occur when clinicians consider the needs of individual patients, available resources, and limitations unique to an institution or type of practice. Health care professionals using these recommendations should decide how to apply them to their own clinical practice.
Section II: Disclosure
Kidney Disease: Improving Global Outcomes (KDIGO) makes every effort to avoid any actual or reasonably perceived conflicts of interest that may arise from an outside relationship or a personal, professional, or business interest of a member of the Work Group. All members of the Work Group are required to complete, sign, and submit a disclosure and attestation form showing all such relationships that might be perceived as or are actual conflicts of interest. This document is updated annually, and information is adjusted accordingly. All reported information is published in its entirety at the end of this document in the Work Group members’ Biographic and Disclosure section, and is kept on file at KDIGO.
Copyright © 2017, KDIGO. Published by Elsevier on behalf of the International Society of Nephrology. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
Single copies may be made for personal use as allowed by national copyright laws. Special rates are available for educational institutions that wish to make photocopies for nonprofit educational use. No part of this publication may be reproduced, amended, or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, or any information storage and retrieval system, without explicit permission in writing from KDIGO. Details on how to seek permission for reproduction or translation, and further information about KDIGO’s permissions policies can be obtained by contacting Danielle Green, Managing Director, at danielle.green@kdigo.org.
To the fullest extent of the law, neither KDIGO, Kidney International Supplements, nor the authors, contributors, or editors, assume any liability for any injury and/or damage to persons or property as a matter of products liability, negligence or otherwise, or from any use or operation of any methods, products, instructions, or ideas contained in the material herein.
Foreword
With the growing awareness that chronic kidney disease is an international health problem, Kidney Disease: Improving Global Outcomes (KDIGO) was established in 2003 with its stated mission to “improve the care and outcomes of kidney disease patients worldwide through promoting coordination, collaboration, and integration of initiatives to develop and implement clinical practice guidelines.”
When the KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD) was originally published in 2009, the Work Group acknowledged the lack of high-quality evidence on which to base recommendations. The Guideline included specific research recommendations to encourage investigators to help fill the gaps and bolster the evidence base.
Multiple randomized controlled trials and prospective cohort studies have been published since the 2009 Guideline, and therefore KDIGO recognizes the need to reexamine the currency of all of its guidelines on a periodic basis. Accordingly, KDIGO convened a Controversies Conference in 2013, titled “CKD-MBD: Back to the Future,” whose objective was to determine whether sufficient new data had emerged to support a reassessment of the 2009 CKD-MBD Clinical Practice Guideline and, if so, to determine the scope of the potential revisions.
Although most of the recommendations were still considered to be current, the conference identified a total of 12 recommendations for reevaluation based on new data. In addition, the conference prepared a table of additional topic questions to be considered by the guideline update Work Group. The conference noted that, in spite of the completion of several key clinical trials since the 2009 publication of the CKD-MBD guideline, large gaps of knowledge still remained, as demonstrated by the relatively small number of recommendation statements identified for reevaluation. Interested readers should refer to the conference publication for further details regarding its processes and deliberations.1
Therefore, KDIGO commissioned an update to the CKD-MBD guideline and formed a Work Group, led by Drs. Markus Ketteler and Mary Leonard. The Work Group convened in June 2015 to review and appraise the evidence accumulated since the 2009 Guideline. The topics addressed for revision are listed in Table 2 and included issues prompted by EVOLVE post hoc analyses, which were published after the 2013 Controversies Conference. Though 8 years have passed since the 2009 CKD-MBD guideline, evidence in many areas is still lacking, which has resulted in many of the “opinion-based” recommendation statements from the original guideline document remaining unchanged.
Table 2.
Research questions
| Section | 2009 rec. no. | Research question | Key outcomes | Additional outcomes |
|---|---|---|---|---|
| Bone quality | 3.2.1 | In patients with CKD G3a–G5D, what is the effect on bone quality of bisphosphonates, teriparatide, denosumab, and raloxifene? |
|
|
| 4.3.4 | In patients with CKD G4–G5D, what is the effect on bone quality of bisphosphonates, teriparatide, denosumab, and raloxifene? |
|
||
| 3.2.2 | (a) In patients with CKD G3a–G5D, how well do BMD results predict fractures? (b) In patients with CKD G3a–G5D, how well do BMD results predict renal osteodystrophy? |
|
||
| 5.5 | In patients with CKD G1–G3b and transplant recipients, how well do BMD results predict fractures? |
|
||
| 5.7 | In patients with CKD G4–G5 and transplant recipients, how well do BMD results predict fractures? |
|
||
| Calcium and phosphate | 4.1.1 | In patients with G3a–G5 or G5D, what is the evidence for benefit or harm in maintaining serum phosphate in the normal range compared with other targets of serum phosphate in terms of biochemical outcomes, other surrogate outcomes, and patient-centered outcomes? |
|
|
| 4.1.3 | In patients with CKD G5D, what is the evidence for benefit or harm in using a dialysate calcium concentration between 1.25 and 1.50 mmol/l (2.5 and 3.0 mEq/l) compared with other concentrations of dialysate calcium in terms of biochemical outcomes, other surrogate outcomes, and patient-centered outcomes? |
|
|
|
| 4.1.2 | In patients with CKD G3a–G5D, what is the evidence for benefit or harm in maintaining serum calcium in the normal range compared with other targets of serum calcium in terms of biochemical outcomes, other surrogate outcomes, and patient-centered outcomes? |
|
|
|
| 4.1.4 | In patients with CKD G3a–G5 or G5D with hyperphosphatemia, what is the evidence for benefit or harm in using calcium-containing phosphate-binding agents to treat hyperphosphatemia compared with calcium-free phosphate-binding agents in terms of biochemical outcomes, other surrogate outcomes, and patient-centered outcomes? |
|
|
|
| 4.1.7 | In patients with CKD G3a–G5D with hyperphosphatemia, what is the evidence for benefit or harm in limiting dietary phosphate intake compared with a standard diet in terms of biochemical outcomes, other surrogate outcomes, and patient-centered outcomes? |
|
|
|
| Vitamin D and PTH | 4.2.1 | In patients with CKD G3a–G5 not on dialysis with levels of intact PTH above the upper normal limit of the assay, what is the evidence for benefit or harm in reducing dietary phosphate intake or treating with phosphate-binding agents, calcium supplements, or native vitamin D in terms of biochemical outcomes, other surrogate outcomes, and patient-centered outcomes? |
|
|
| 4.2.2 | In patients with CKD G3a–G5 not on dialysis, in whom serum PTH is progressively rising and remains persistently above the upper limit of normal for the assay despite correction of modifiable factors, what is the evidence for benefit or harm in treating with calcitriol or vitamin D analogs compared with placebo or active control in terms of biochemical outcomes, other surrogate outcomes, and patient-centered outcomes? |
|
|
|
| 4.2.4 | In patients with CKD G5D, what is the evidence for benefit or harm in treating with calcitriol, vitamin D analogs, calcimimetics or combination thereof compared with placebo or active control in terms of biochemical outcomes, other surrogate outcomes, and patient-centered outcomes? |
|
|
|
BMD, bone mineral density; CKD, chronic kidney disease; CUA, calcific uremic arteriolopathy; GFR, glomerular filtration rate; FGF23, fibroblast growth factor 23; LVH, left ventricular hypertrophy; PTH, parathyroid hormone; rec. no., recommendation number; TMV, bone turnover mineralization volume.
In keeping with the standard KDIGO policy of maintaining transparency during the guideline development process and attesting to its rigor, we conducted an open public review of the draft CKD-MBD guideline update, and all feedback received was reviewed and considered by the Work Group before finalizing this guideline document for publication. The comments and suggestions greatly assisted us in shaping a final document that we felt would be as valuable as possible to the entire nephrology community.
We wish to thank the Work Group co-chairs, Drs. Markus Ketteler and Mary Leonard, along with all of the Work Group members, who volunteered countless hours of their time to develop this guideline. We also thank Dr. Karen Robinson and her Evidence Review Team at Johns Hopkins University, the KDIGO staff, and many others for their support that made this project possible.
David C. Wheeler, MD, FRCP
Wolfgang C. Winkelmayer, MD, MPH, ScD
KDIGO Co-chairs
Work Group membership
| Work Group Co-chairs | |
| Markus Ketteler, MD, FERA Klinikum Coburg Coburg, Germany |
Mary B. Leonard, MD, MSCE Stanford University School of Medicine Stanford, CA, USA |
| Work Group | |
| Geoffrey A. Block, MD Denver Nephrology Denver, CO, USA Pieter Evenepoel, MD, PhD, FERA University Hospitals Leuven Leuven, Belgium Masafumi Fukagawa, MD, PhD, FASN Tokai University School of Medicine Isehara, Japan Charles A. Herzog, MD, FACC, FAHA Hennepin County Medical Center Minneapolis, MN, USA Linda McCann, RD, CSR Eagle, ID, USA Sharon M. Moe, MD Indiana University School of Medicine Roudebush Veterans Affairs Medical Center Indianapolis, IN, USA |
Rukshana Shroff, MD, FRCPCH, PhD Great Ormond Street Hospital for Children NHS Foundation Trust, London, UK Marcello A. Tonelli, MD, SM, FRCPC University of Calgary Calgary, Canada Nigel D. Toussaint MBBS, FRACP, PhD The Royal Melbourne Hospital University of Melbourne Melbourne, Australia Marc G. Vervloet, MD, PhD, FERA VU University Medical Center Amsterdam Amsterdam, The Netherlands |
|
Evidence Review Team Johns Hopkins University Baltimore, MD, USA Karen A. Robinson, PhD, Associate Professor of Medicine and Project Director Casey M. Rebholz, PhD, MPH, MS, Co-investigator Lisa M. Wilson, ScM, Project Manager Ermias Jirru, MD, MPH, Research Assistant Marisa Chi Liu, MD, MPH, Research Assistant Jessica Gayleard, BS, Research Assistant Allen Zhang, BS, Research Assistant | |
Abstract
The Kidney Disease: Improving Global Outcomes (KDIGO) 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of chronic kidney disease–mineral and bone disorder (CKD-MBD) represents a selective update of the prior guideline published in 2009. This update, along with the 2009 publication, is intended to assist the practitioner caring for adults and children with CKD, those on chronic dialysis therapy, or individuals with a kidney transplant. Specifically, the topic areas for which updated recommendations are issued include diagnosis of bone abnormalities in CKD-MBD; treatment of CKD-MBD by targeting phosphate lowering and calcium maintenance, treatment of abnormalities in parathyroid hormone in CKD-MBD; treatment of bone abnormalities by antiresorptives and other osteoporosis therapies; and evaluation and treatment of kidney transplant bone disease. Development of this guideline update followed an explicit process of evidence review and appraisal. Treatment approaches and guideline recommendations are based on systematic reviews of relevant trials, and appraisal of the quality of the evidence and the strength of recommendations followed the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) approach. Limitations of the evidence are discussed, with areas of future research also presented.
Keywords: bone abnormalities; bone mineral density; calcium; chronic kidney disease; CKD-MBD; dialysis; guideline; hyperparathyroidism; hyperphosphatemia; KDIGO; kidney transplantation; mineral and bone disorder; parathyroid hormone; phosphate; phosphorus; systematic review
CITATION
In citing this document, the following format should be used: Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease–Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl. 2017;7:1–59.
Summary of KDIGO CKD-MBD recommendations∗
Updated recommendations are denoted in boxes
Chapter 3.1: Diagnosis of CKD-MBD: biochemical abnormalities
3.1.1: We recommend monitoring serum levels of calcium, phosphate, PTH, and alkaline phosphatase activity beginning in CKD G3a (1C). In children, we suggest such monitoring beginning in CKD G2 (2D).
3.1.2: In patients with CKD G3a–G5D, it is reasonable to base the frequency of monitoring serum calcium, phosphate, and PTH on the presence and magnitude of abnormalities, and the rate of progression of CKD (Not Graded).
- Reasonable monitoring intervals would be:
-
•In CKD G3a–G3b: for serum calcium and phosphate, every 6–12 months; and for PTH, based on baseline level and CKD progression.
-
•In CKD G4: for serum calcium and phosphate, every 3–6 months; and for PTH, every 6–12 months.
-
•In CKD G5, including G5D: for serum calcium and phosphate, every 1–3 months; and for PTH, every 3–6 months.
-
•In CKD G4–G5D: for alkaline phosphatase activity, every 12 months, or more frequently in the presence of elevated PTH (see Chapter 3.2).
-
•
In CKD patients receiving treatments for CKD-MBD, or in whom biochemical abnormalities are identified, it is reasonable to increase the frequency of measurements to monitor for trends and treatment efficacy and side effects (Not Graded).
3.1.3: In patients with CKD G3a–G5D, we suggest that 25(OH)D (calcidiol) levels might be measured, and repeated testing determined by baseline values and therapeutic interventions (2C). We suggest that vitamin D deficiency and insufficiency be corrected using treatment strategies recommended for the general population (2C).
3.1.4: In patients with CKD G3a–G5D, we recommend that therapeutic decisions be based on trends rather than on a single laboratory value, taking into account all available CKD-MBD assessments (1C).
3.1.5: In patients with CKD G3a–G5D, we suggest that individual values of serum calcium and phosphate, evaluated together, be used to guide clinical practice rather than the mathematical construct of calcium-phosphate product (Ca × P) (2D).
3.1.6: In reports of laboratory tests for patients with CKD G3a–G5D, we recommend that clinical laboratories inform clinicians of the actual assay method in use and report any change in methods, sample source (plasma or serum), or handling specifications to facilitate the appropriate interpretation of biochemistry data (1B).
Chapter 3.2: Diagnosis of CKD-MBD: bone
3.2.1: In patients with CKD G3a–G5D with evidence of CKD-MBD and/or risk factors for osteoporosis, we suggest BMD testing to assess fracture risk if results will impact treatment decisions (2B).
3.2.2: In patients with CKD G3a–G5D, it is reasonable to perform a bone biopsy if knowledge of the type of renal osteodystrophy will impact treatment decisions (Not Graded).
3.2.3: In patients with CKD G3a–G5D, we suggest that measurements of serum PTH or bone-specific alkaline phosphatase can be used to evaluate bone disease because markedly high or low values predict underlying bone turnover (2B).
3.2.4: In patients with CKD G3a–G5D, we suggest not to routinely measure bone-derived turnover markers of collagen synthesis (such as procollagen type I C-terminal propeptide) and breakdown (such as type I collagen cross-linked telopeptide, cross-laps, pyridinoline, or deoxypyridinoline) (2C).
3.2.5: We recommend that infants with CKD G2–G5D have their length measured at least quarterly, while children with CKD G2–G5D should be assessed for linear growth at least annually (1B).
Chapter 3.3: Diagnosis of CKD-MBD: vascular calcification
3.3.1: In patients with CKD G3a–G5D, we suggest that a lateral abdominal radiograph can be used to detect the presence or absence of vascular calcification, and an echocardiogram can be used to detect the presence or absence of valvular calcification, as reasonable alternatives to computed tomography-based imaging (2C).
3.3.2: We suggest that patients with CKD G3a–G5D with known vascular or valvular calcification be considered at highest cardiovascular risk (2A). It is reasonable to use this information to guide the management of CKD-MBD (Not Graded).
Chapter 4.1: Treatment of CKD-MBD targeted at lowering high serum phosphate and maintaining serum calcium
4.1.1: In patients with CKD G3a–G5D, treatments of CKD-MBD should be based on serial assessments of phosphate, calcium, and PTH levels, considered together (Not Graded).
4.1.2: In patients with CKD G3a–G5D, we suggest lowering elevated phosphate levels toward the normal range (2C).
4.1.3: In adult patients with CKD G3a–G5D, we suggest avoiding hypercalcemia (2C). In children with CKD G3a–G5D, we suggest maintaining serum calcium in the age-appropriate normal range (2C).
4.1.4: In patients with CKD G5D, we suggest using a dialysate calcium concentration between 1.25 and 1.50 mmol/l (2.5 and 3.0 mEq/l) (2C).
4.1.5: In patients with CKD G3a-G5D, decisions about phosphate-lowering treatment should be based on progressively or persistently elevated serum phosphate (Not Graded).
4.1.6: In adult patients with CKD G3a–G5D receiving phosphate-lowering treatment, we suggest restricting the dose of calcium-based phosphate binders (2B). In children with CKD G3a–G5D, it is reasonable to base the choice of phosphate-lowering treatment on serum calcium levels (Not Graded).
4.1.7: In patients with CKD G3a-G5D, we recommend avoiding the long-term use of aluminum-containing phosphate binders and, in patients with CKD G5D, avoiding dialysate aluminum contamination to prevent aluminum intoxication (1C).
4.1.8: In patients with CKD G3a–G5D, we suggest limiting dietary phosphate intake in the treatment of hyperphosphatemia alone or in combination with other treatments (2D). It is reasonable to consider phosphate source (e.g., animal, vegetable, additives) in making dietary recommendations (Not Graded).
4.1.9: In patients with CKD G5D, we suggest increasing dialytic phosphate removal in the treatment of persistent hyperphosphatemia (2C).
Chapter 4.2: Treatment of abnormal PTH levels in CKD-MBD
4.2.1: In patients with CKD G3a–G5 not on dialysis, the optimal PTH level is not known. However, we suggest that patients with levels of intact PTH progressively rising or persistently above the upper normal limit for the assay be evaluated for modifiable factors, including hyperphosphatemia, hypocalcemia, high phosphate intake, and vitamin D deficiency (2C).
4.2.2: In adult patients with CKD G3a–G5 not on dialysis, we suggest that calcitriol and vitamin D analogs not be routinely used (2C). It is reasonable to reserve the use of calcitriol and vitamin D analogs for patients with CKD G4–G5 with severe and progressive hyperparathyroidism (Not Graded).
In children, calcitriol and vitamin D analogs may be considered to maintain serum calcium levels in the age-appropriate normal range (Not Graded).
4.2.3: In patients with CKD G5D, we suggest maintaining iPTH levels in the range of approximately 2 to 9 times the upper normal limit for the assay (2C).
We suggest that marked changes in PTH levels in either direction within this range prompt an initiation or change in therapy to avoid progression to levels outside of this range (2C).
4.2.4: In patients with CKD G5D requiring PTH-lowering therapy, we suggest calcimimetics, calcitriol, or vitamin D analogs, or a combination of calcimimetics with calcitriol or vitamin D analogs (2B).
4.2.5: In patients with CKD G3a–G5D with severe hyperparathyroidism (HPT) who fail to respond to medical or pharmacological therapy, we suggest parathyroidectomy (2B).
Chapter 4.3: Treatment of bone with bisphosphonates, other osteoporosis medications, and growth hormone
4.3.1: In patients with CKD G1–G2 with osteoporosis and/or high risk of fracture, as identified by World Health Organization criteria, we recommend management as for the general population (1A).
4.3.2: In patients with CKD G3a–G3b with PTH in the normal range and osteoporosis and/or high risk of fracture, as identified by World Health Organization criteria, we suggest treatment as for the general population (2B).
4.3.3: In patients with CKD G3a–G5D with biochemical abnormalities of CKD-MBD and low BMD and/or fragility fractures, we suggest that treatment choices take into account the magnitude and reversibility of the biochemical abnormalities and the progression of CKD, with consideration of a bone biopsy (2D).
4.3.4: In children and adolescents with CKD G2–G5D and related height deficits, we recommend treatment with recombinant human growth hormone when additional growth is desired, after first addressing malnutrition and biochemical abnormalities of CKD-MBD (1A).
Chapter 5: Evaluation and treatment of kidney transplant bone disease
5.1: In patients in the immediate post–kidney transplant period, we recommend measuring serum calcium and phosphate at least weekly, until stable (1B).
5.2: In patients after the immediate post–kidney transplant period, it is reasonable to base the frequency of monitoring serum calcium, phosphate, and PTH on the presence and magnitude of abnormalities, and the rate of progression of CKD (Not Graded).
- Reasonable monitoring intervals would be:
-
•In CKD G1T–G3bT, for serum calcium and phosphate, every 6–12 months; and for PTH, once, with subsequent intervals depending on baseline level and CKD progression.
-
•In CKD G4T, for serum calcium and phosphate, every 3–6 months; and for PTH, every 6–12 months.
-
•In CKD G5T, for serum calcium and phosphate, every 1–3 months; and for PTH, every 3–6 months.
-
•In CKD G3aT–G5T, measurement of alkaline phosphatases annually, or more frequently in the presence of elevated PTH (see Chapter 3.2).
-
•
In CKD patients receiving treatments for CKD-MBD, or in whom biochemical abnormalities are identified, it is reasonable to increase the frequency of measurements to monitor for efficacy and side effects (Not Graded).
It is reasonable to manage these abnormalities as for patients with CKD G3a–G5 (see Chapters 4.1 and 4.2) (Not Graded).
5.3: In patients with CKD G1T–G5T, we suggest that 25(OH)D (calcidiol) levels might be measured, and repeated testing determined by baseline values and interventions (2C).
5.4: In patients with CKD G1T–G5T, we suggest that vitamin D deficiency and insufficiency be corrected using treatment strategies recommended for the general population (2C).
5.5: In patients with CKD G1T–G5T with risk factors for osteoporosis, we suggest that BMD testing be used to assess fracture risk if results will alter therapy (2C).
- 5.6: In patients in the first 12 months after kidney transplant with an estimated glomerular filtration rate greater than approximately 30 ml/min/1.73 m2 and low BMD, we suggest that treatment with vitamin D, calcitriol/alfacalcidol, and/or antiresorptive agents be considered (2D).
-
•We suggest that treatment choices be influenced by the presence of CKD-MBD, as indicated by abnormal levels of calcium, phosphate, PTH, alkaline phosphatases, and 25(OH)D (2C).
-
•It is reasonable to consider a bone biopsy to guide treatment (Not Graded).
-
•
There are insufficient data to guide treatment after the first 12 months.
5.7: In patients with CKD G4T–G5T with known low BMD, we suggest management as for patients with CKD G4–G5 not on dialysis, as detailed in Chapters 4.1 and 4.2 (2C).
The 2017 updated recommendations resulted in renumbering of several adjacent guideline statements. Specifically, 2009 Recommendation 4.1.6 now becomes 2017 Recommendation 4.1.7; 2009 Recommendation 4.1.8 now becomes 2017 Recommendation 4.1.9; 2009 Recommendation 4.3.5 now becomes 2017 Recommendation 4.3.4; and 2009 Recommendation 5.8 now becomes 2017 Recommendation 5.7.
Summary and comparison of 2017 updated and 2009 KDIGO CKD-MBD recommendations
| 2017 revised KDIGO CKD-MBD recommendations | 2009 KDIGO CKD-MBD recommendations | Brief rationale for updating |
|---|---|---|
| 3.2.1. In patients with CKD G3a–G5D with evidence of CKD-MBD and/or risk factors for osteoporosis, we suggest BMD testing to assess fracture risk if results will impact treatment decisions (2B). | 3.2.2. In patients with CKD G3a–G5D with evidence of CKD-MBD, we suggest that BMD testing not be performed routinely, because BMD does not predict fracture risk as it does in the general population, and BMD does not predict the type of renal osteodystrophy (2B). | Multiple new prospective studies have documented that lower DXA BMD predicts incident fractures in patients with CKD G3a–G5D. The order of these first 2 recommendations was changed because a DXA BMD result might impact the decision to perform a bone biopsy. |
| 3.2.2. In patients with CKD G3a–G5D, it is reasonable to perform a bone biopsy if knowledge of the type of renal osteodystrophy will impact treatment decisions (Not Graded). | 3.2.1. In patients with CKD G3a–G5D, it is reasonable to perform a bone biopsy in various settings including, but not limited to: unexplained fractures, persistent bone pain, unexplained hypercalcemia, unexplained hypophosphatemia, possible aluminum toxicity, and prior to therapy with bisphosphonates in patients with CKD-MBD (Not Graded). | The primary motivation for this revision was the growing experience with osteoporosis medications in patients with CKD, low BMD, and a high risk of fracture. The inability to perform a bone biopsy may not justify withholding antiresorptive therapy from patients at high risk of fracture. |
| 4.1.1. In patients with CKD G3a–G5D, treatments of CKD-MBD should be based on serial assessments of phosphate, calcium, and PTH levels, considered together (Not Graded). | This new recommendation was provided in order to emphasize the complexity and interaction of CKD-MBD laboratory parameters. | |
| 4.1.2. In patients with CKD G3a–G5D, we suggest lowering elevated phosphate levels toward the normal range (2C). | 4.1.1. In patients with CKD G3a–G5, we suggest maintaining serum phosphate in the normal range (2C). In patients with CKD G5D, we suggest lowering elevated phosphate levels toward the normal range (2C). | There is an absence of data supporting that efforts to maintain phosphate in the normal range are of benefit to CKD G3a–G4 patients, including some safety concerns. Treatment should aim at overt hyperphosphatemia. |
| 4.1.3. In adult patients with CKD G3a–G5D, we suggest avoiding hypercalcemia (2C). In children with CKD G3a–G5D, we suggest maintaining serum calcium in the age-appropriate normal range (2C). |
4.1.2. In patients with CKD G3a–G5D, we suggest maintaining serum calcium in the normal range (2D). | Mild and asymptomatic hypocalcemia (e.g., in the context of calcimimetic treatment) can be tolerated in order to avoid inappropriate calcium loading in adults. |
| 4.1.4. In patients with CKD G5D, we suggest using a dialysate calcium concentration between 1.25 and 1.50 mmol/l (2.5 and 3.0 mEq/l) (2C). | 4.1.3. In patients with CKD G5D, we suggest using a dialysate calcium concentration between 1.25 and 1.50 mmol/l (2.5 and 3.0 mEq/l) (2D). | Additional studies of better quality are available; however, these do not allow for discrimination of benefits and harms between calcium dialysate concentrations of 1.25 and 1.50 mmol/l (2.5 and 3.0 mEq/l). Hence, the wording is unchanged, but the evidence grade is upgraded from 2D to 2C. |
| 4.1.5. In patients with CKD G3a–G5D, decisions about phosphate-lowering treatment should be based on progressively or persistently elevated serum phosphate (Not Graded). | 4.1.4. In patients with CKD G3a–G5 (2D) and G5D (2B), we suggest using phosphate-binding agents in the treatment of hyperphosphatemia. It is reasonable that the choice of phosphate binder takes into account CKD stage, presence of other components of CKD-MBD, concomitant therapies, and side effect profile (Not Graded). | Emphasizes the perception that early “preventive” phosphate-lowering treatment is currently not supported by data (see Recommendation 4.1.2). The broader term “phosphate-lowering” treatment is used instead of phosphate binding agents since all possible approaches (i.e., binders, diet, dialysis) can be effective. |
| 4.1.6. In adult patients with CKD G3a–G5D receiving phosphate-lowering treatment, we suggest restricting the dose of calcium-based phosphate binder (2B). In children with CKD G3a–G5D, it is reasonable to base the choice of phosphate-lowering treatment on serum calcium levels (Not Graded). | 4.1.5. In patients with CKD G3a–G5D and hyperphosphatemia, we recommend restricting the dose of calcium-based phosphate binders and/or the dose of calcitriol or vitamin D analog in the presence of persistent or recurrent hypercalcemia (1B). | New evidence from 3 RCTs supports a more general recommendation to restrict calcium-based phosphate binders in hyperphosphatemic patients across all severities of CKD. |
| In patients with CKD G3a–G5D and hyperphosphatemia, we suggest restricting the dose of calcium-based phosphate binders in the presence of arterial calcification (2C) and/or adynamic bone disease (2C) and/or if serum PTH levels are persistently low (2C). | ||
| 4.1.8. In patients with CKD G3a–G5D, we suggest limiting dietary phosphate intake in the treatment of hyperphosphatemia alone or in combination with other treatments (2D). It is reasonable to consider phosphate source (e.g., animal, vegetable, additives) in making dietary recommendations (Not Graded). | 4.1.7. In patients with CKD G3a–G5D, we suggest limiting dietary phosphate intake in the treatment of hyperphosphatemia alone or in combination with other treatments (2D). | New data on phosphate sources were deemed to be included as an additional qualifier to the previous recommendation. |
| 4.2.1. In patients with CKD G3a–G5 not on dialysis, the optimal PTH level is not known. However, we suggest that patients with levels of intact PTH progressively rising or persistently above the upper normal limit for the assay be evaluated for modifiable factors, including hyperphosphatemia, hypocalcemia, high phosphate intake, and vitamin D deficiency (2C). | 4.2.1. In patients with CKD G3a–G5 not on dialysis, the optimal PTH level is not known. However, we suggest that patients with levels of intact PTH above the upper normal limit of the assay are first evaluated for hyperphosphatemia, hypocalcemia, and vitamin D deficiency (2C). It is reasonable to correct these abnormalities with any or all of the following: reducing dietary phosphate intake and administering phosphate binders, calcium supplements, and/or native vitamin D (Not Graded). |
The Work Group felt that modest increases in PTH may represent an appropriate adaptive response to declining kidney function and has revised this statement to include “persistently” above the upper normal PTH level as well as “progressively rising” PTH levels, rather than “above the upper normal limit.” That is, treatment should not be based on a single elevated value. |
| 4.2.2. In adult patients with CKD G3a–G5 not on dialysis, we suggest that calcitriol and vitamin D analogs not be routinely used. (2C) It is reasonable to reserve the use of calcitriol and vitamin D analogs for patients with CKD G4–G5 with severe and progressive hyperparathyroidism (Not Graded). | 4.2.2. In patients with CKD G3a–G5 not on dialysis, in whom serum PTH is progressively rising and remains persistently above the upper limit of normal for the assay despite correction of modifiable factors, we suggest treatment with calcitriol or vitamin D analogs (2C). | Recent RCTs of vitamin D analogs failed to demonstrate improvements in clinically relevant outcomes but demonstrated increased risk of hypercalcemia. |
| In children, calcitriol and vitamin D analogs may be considered to maintain serum calcium levels in the age-appropriate normal range (Not Graded). | ||
| 4.2.4. In patients with CKD G5D requiring PTH-lowering therapy, we suggest calcimimetics, calcitriol, or vitamin D analogs, or a combination of calcimimetics with calcitriol or vitamin D analogs (2B). | 4.2.4. In patients with CKD G5D and elevated or rising PTH, we suggest calcitriol, or vitamin D analogs, or calcimimetics, or a combination of calcimimetics and calcitriol or vitamin D analogs be used to lower PTH (2B).
|
This recommendation originally had not been suggested for updating by the KDIGO Controversies Conference in 2013. However, due to a subsequent series of secondary and post hoc publications of the EVOLVE trial, the Work Group decided to reevaluate Recommendation 4.2.4 as well. Although EVOLVE did not meet its primary endpoint, the majority of the Work Group members were reluctant to exclude potential benefits of calcimimetics for G5D patients based on subsequent prespecified analyses. The Work Group, however, decided not to prioritize any PTH-lowering treatment at this time because calcimimetics, calcitriol, or vitamin D analogs are all acceptable first-line options in G5D patients. |
| 4.3.3. In patients with CKD G3a–G5D with biochemical abnormalities of CKD-MBD and low BMD and/or fragility fractures, we suggest that treatment choices take into account the magnitude and reversibility of the biochemical abnormalities and the progression of CKD, with consideration of a bone biopsy (2D). | 4.3.3. In patients with CKD G3a–G3b with biochemical abnormalities of CKD-MBD and low BMD and/or fragility fractures, we suggest that treatment choices take into account the magnitude and reversibility of the biochemical abnormalities and the progression of CKD, with consideration of a bone biopsy (2D). | Recommendation 3.2.2 now addresses the indications for a bone biopsy prior to antiresorptive and other osteoporosis therapies. Therefore, 2009 Recommendation 4.3.4 has been removed and 2017 Recommendation 4.3.3 is broadened from CKD G3a–G3b to CKD G3a–G5D. |
| 4.3.4. In patients with CKD G4–G5D having biochemical abnormalities of CKD-MBD, and low BMD and/or fragility fractures, we suggest additional investigation with bone biopsy prior to therapy with antiresorptive agents (2C). | ||
| 5.5. In patients with G1T–G5T with risk factors for osteoporosis, we suggest that BMD testing be used to assess fracture risk if results will alter therapy (2C). | 5.5. In patients with an estimated glomerular filtration rate greater than approximately 30 ml/min/1.73 m2, we suggest measuring BMD in the first 3 months after kidney transplant if they receive corticosteroids, or have risk factors for osteoporosis as in the general population (2D). | 2009 Recommendations 5.5 and 5.7 were combined to yield 2017 Recommendation 5.5. |
| 5.7. In patients with CKD G4T–G5T, we suggest that BMD testing not be performed routinely, because BMD does not predict fracture risk as it does in the general population and BMD does not predict the type of kidney transplant bone disease (2B). | ||
5.6. In patients in the first 12 months after kidney transplant with an estimated glomerular filtration rate greater than approximately 30 ml/min/1.73 m2 and low BMD, we suggest that treatment with vitamin D, calcitriol/alfacalcidol, and/or antiresorptive agents be considered (2D).
|
5.6. In patients in the first 12 months after kidney transplant with an estimated glomerular filtration rate greater than approximately 30 ml/min/1.73 m2 and low BMD, we suggest that treatment with vitamin D, calcitriol/alfacalcidol, or bisphosphonates be considered (2D).
|
The second bullet is revised, consistent with the new bone biopsy recommendation (i.e., 2017 Recommendation 3.2.2). |
25(OH)D, 25-hydroxyvitamin D; BMD, bone mineral density; CKD, chronic kidney disease; CKD-MBD, chronic kidney disease–mineral bone disorder; DXA, dual-energy x-ray absorptiometry; PTH, parathyroid hormone; RCT, randomized controlled trial. Changes to above summarized recommendations resulted in renumbering of several adjacent guideline statements. Specifically, 2009 Recommendation 4.1.6 now becomes 2017 Recommendation 4.1.7; 2009 Recommendation 4.1.8 now becomes 2017 Recommendation 4.1.9; 2009 Recommendation 4.3.5 now becomes 2017 Recommendation 4.3.4; and 2009 Recommendation 5.8 now becomes 2017 Recommendation 5.7.
Chapter 3.2: Diagnosis of CKD-MBD: bone
3.2.1: In patients with CKD G3a–G5D with evidence of CKD-MBD and/or risk factors for osteoporosis, we suggest BMD testing to assess fracture risk if results will impact treatment decisions (2B).
Rationale
It is well established that patients with CKD G3a–G5D have increased fracture rates compared with the general population,2, 3, 4 and moreover, incident hip fractures are associated with substantial morbidity and mortality.5, 6, 7, 8, 9 At the time of the 2009 KDIGO CKD-MBD guideline, publications addressing the ability of dual-energy X-ray absorptiometry (DXA) measures of bone mineral density (BMD) to estimate fracture risk in CKD were limited to cross-sectional studies comparing BMD in CKD patients with and without a prevalent fracture. The results were variable across studies and across skeletal sites. In light of the lack of evidence that DXA BMD predicted fractures in CKD patients as it does in the general population, and the inability of DXA to indicate the histological type of bone disease, the 2009 Guideline recommended that BMD testing not be performed routinely in patients with CKD G3a to G5D with CKD-MBD. Furthermore, the lack of clinical trials in patients with low BMD and CKD also limited the enthusiasm for measuring BMD in the first place.
The current evidence-based review identified 4 prospective cohort studies of DXA BMD and incident fractures in adults with CKD G3a to G5D (Supplementary Tables S7–S12). These studies demonstrated that DXA BMD predicted fractures across the spectrum from CKD G3a to G5D (Supplementary Tables S7–S12).10, 11, 12, 13 In the earliest study, DXA BMD was measured annually in 485 hemodialysis (HD) patients (mean age: 60 years) in a single center in Japan.10 In adjusted Cox proportional analyses, lower baseline femoral neck and total hip BMD predicted a greater risk of fracture; for example, the hazard ratio (HR) was 0.65 (95% confidence interval [CI]: 0.47–0.90) for each standard deviation (SD) higher femoral neck BMD. In receiver operating characteristic (ROC) analyses stratified according to parathyroid hormone (PTH) below or above the median value of 204 pg/ml (21.6 pmol/l), the area under the curve (AUC) for femoral neck BMD was 0.717 in the lower stratum and 0.512 in the higher stratum. Of note, higher serum bone-specific alkaline phosphate levels also predicted incident fractures.
In the second study, Yenchek et al. assessed whether DXA total hip and femoral neck BMD were associated with incident nonspine fragility fractures in participants with estimated glomerular filtration rate (eGFR) < 60 ml/min/1.73 m2 and without CKD in the Health, Aging and Body Composition Study, a prospective study of community-living individuals, 70 to 79 years of age at enrollment.13 A total of 587 (21%) of the 2754 participants had CKD, and among those, 83% and 13% had CKD G3a and G3b, respectively. In adjusted analyses, the fracture HR for each SD lower femoral neck BMD was 2.14 (95% CI: 1.80–2.55) in participants without CKD, and 2.69 (95% CI: 1.96–3.69) in those with CKD. Similar results were observed for total hip BMD. When limited to hip fractures, the adjusted femoral neck BMD HRs were 5.82 (95% CI: 3.27–10.35) among those with CKD and 3.08 (95% CI: 2.29–4.14) among those without CKD. Interaction terms demonstrated that the association of BMD with fracture did not differ in those with versus without CKD. However, the association of femoral neck BMD with fracture was significantly less pronounced (test for interaction, P = 0.04) among those with PTH > 65 pg/ml (6.9 pmol/l; HR: 1.56, 95% CI: 0.90–2.70) compared with those with a PTH ≤ 65 pg/ml (6.9 pmol/l; HR: 2.41, 95% CI: 2.04–2.85) in all participants combined. This is noteworthy in light of the similar pattern observed in dialysis patients, as described above.10
West et al. reported the results of a prospective cohort study of 131 predialysis participants, mean age 62 years, followed up over a 2-year interval.12 At baseline, the proportions with CKD G3a to G3b, G4, and G5 were 34%, 40%, and 26%, respectively. DXA BMD was measured in the total hip, lumbar spine, and ultradistal and one-third radius at baseline and 2 years. Low BMD at all sites, and a greater annualized percentage decrease in BMD predicted fracture. For example, in multivariate models, each SD lower total hip BMD was associated with an odds ratio (OR) of fracture of 1.75 (95% CI: 1.30–2.20). The ROC AUC ranged from 0.62 in the spine to 0.74 in the ultradistal radius in adjusted models.
Most recently, Naylor, et al.11 assessed the ability of the Fracture Risk Assessment Tool (FRAX) to predict a major osteoporotic fracture in 2107 adults ≥ 40 years of age in the Canadian Multicenter Osteoporosis Study, including 320 with an eGFR ≤ 60 ml/min/1.73 m2. Of these, 72% and 24% had CKD G3a and G3b, respectively. FRAX with BMD, FRAX without BMD, and the femoral neck T-score all predicted fractures (AUC: 0.65 to 0.71); the AUC was highest for femoral neck T-score with inclusion of fall history. Importantly, the AUCs did not differ between those with and without CKD.
There is growing evidence that DXA BMD predicts fractures in healthy children and adolescents, and those with chronic disease.14, 15 However, no studies have examined the associations among DXA BMD and fractures in children and adolescents with CKD. In light of the lack of evidence that the ability of DXA BMD to predict fracture in children with CKD is different than in adults, no specific recommendations are provided for children. However, it should be noted that children and adolescents with CKD frequently exhibit substantial growth failure. Given that DXA measures of areal BMD (g/cm2) underestimate volumetric BMD (g/cm3) in children with short stature,16 DXA results should be adjusted for bone size, consistent with the 2013 International Society of Clinical Densitometry (ISCD) Pediatric Official Positions.17 Prediction equations to adjust DXA results for height Z-score are now available,16 and the impact on DXA BMD Z-scores in children with CKD is substantial.18 Finally, a single-center study in 171 children with CKD G2 to G5D reported that lower cortical volumetric BMD in the tibia, as measured by peripheral quantitative computed tomography (CT), predicted fractures over a 1-year interval (Supplementary Tables S7–S12).19 The HR per unit lower cortical BMD Z-score was 1.75 (95% CI: 1.15–2.67; P < 0.01).
The evidence-based review also evaluated clinical trials of the effects of osteoporosis medications on BMD in CKD G3a to G5D (Supplementary Tables S1–S6). Prior analyses of large randomized clinical trials (RCTs) evaluating medications for the treatment of postmenopausal osteoporosis (risedronate, alendronate, teriparatide, and raloxifene) were described in the 2009 Guideline. These trials specifically excluded patients with an elevated serum creatinine, hyperparathyroidism, or abnormal alkaline phosphate levels (i.e., CKD-MBD).20, 21, 22, 23 However, post hoc analyses found that these drugs had similar efficacy on improving BMD and reducing fracture incidence in individuals with moderately reduced eGFR, compared with those with mildly decreased or normal eGFR. Three new trials were identified. The denosumab study was also a post hoc analysis of an RCT in women with postmenopausal osteoporosis and normal PTH levels.24 The analysis demonstrated efficacy of denosumab in decreasing fracture risk and increasing BMD in 2817 women with CKD G3a to G3b and 73 with CKD G4. Here, the risk of hypocalcemia associated with denosumab in advanced CKD requires mentioning. The remaining 2 new trials on alendronate25 and raloxifene26 were small studies (<60 participants) that did not exclude patients with evidence of CKD-MBD. These studies did not show consistent beneficial effects on DXA BMD. Generally, a major limitation is the lack of data on fracture prevention by such therapeutic interventions in advanced CKD (especially in CKD G5–G5D).
In summary, the aforementioned 4 prospective studies evaluating BMD testing in adults with CKD represent a substantial advance since the original guideline from 2009. Despite the fact that they were conducted across a spectrum of CKD severity, the finding that hip BMD predicted fractures was consistent across studies, and 2 studies demonstrated associations comparable to those seen in the absence of CKD.11, 13 Based on these insights, if a low or declining BMD will lead to additional interventions to reduce falls or use osteoporosis medications, then BMD assessment is reasonable.
Research recommendations
-
•
RCTs are needed to determine whether interventions based on DXA BMD are associated with lower fracture rates, and whether the effects vary based on clinical variables such as the baseline PTH level, underlying cause of kidney disease, and CKD GFR category.
-
•
Prospective studies are needed to determine whether alternative imaging techniques, such as quantitative CT, improve fracture prediction in CKD.
-
•
Prospective studies are needed in children and adolescents to determine whether DXA predicts fractures in children and to determine whether the ISCD recommendations to measure whole-body and spine BMD in children are the appropriate sites in the context of CKD.17 Hip and radius BMD pediatric reference data are now available and predict incident fractures in healthy children and adolescents.27, 28
3.2.2: In patients with CKD G3a–G5D, it is reasonable to perform a bone biopsy if knowledge of the type of renal osteodystrophy will impact treatment decisions (Not Graded).
Rationale
Renal osteodystrophy is defined as abnormal bone histology and is 1 component of the bone abnormalities of CKD-MBD.29 Bone biopsy is the gold standard for the diagnosis and classification for renal osteodystrophy. As detailed in the 2009 KDIGO CKD-MBD Guideline,30 DXA BMD does not distinguish among types of renal osteodystrophy, and the diagnostic utility of biochemical markers is limited by poor sensitivity and specificity. Differences in PTH assays (e.g., intact vs. whole PTH) and reference ranges have contributed to differences across studies. Unfortunately, cross-sectional studies have provided conflicting information on the use of biomarkers to predict underlying bone histology. This is not surprising given the short half-lives of most of the circulating biomarkers, and the long (3–6 months) bone remodeling (turnover) cycle.
KDIGO recently led an international consortium to conduct a cross-sectional retrospective diagnostic study of biomarkers (all run in a single laboratory) and bone biopsies in 492 dialysis patients.31 The objective was to determine the predictive value of PTH (determined by both intact PTH [iPTH] and whole PTH assays), bone-specific alkaline phosphatase (bALP), and amino-terminal propeptide of type 1 procollagen (P1NP) as markers of bone turnover. Although iPTH, whole PTH, and bALP levels were associated with bone turnover, no biomarker singly or in combination was sufficiently robust to diagnose low, normal, and high bone turnover in an individual patient. The conclusion was in support of the 2009 KDIGO Guideline to use trends in PTH rather than absolute “target” values when making decisions as to whether to start or stop treatments to lower PTH. Table 1 provides the sensitivity, specificity, and positive and negative predictive value of PTH in helping clinicians determine therapies, demonstrating the challenges clinicians face. Thus, the Work Group encourages the continued use of trends in PTH to guide therapy, and when trends in PTH are inconsistent, a bone biopsy should be considered.
Table 1.
Utility of KDOQI and KDIGO PTH thresholds for diagnostic decision making
| KDOQI∗ |
KDIGO+ |
|||||||
|---|---|---|---|---|---|---|---|---|
| Sens | Spec | PPV | NPV | Sens | Spec | PPV | NPV | |
| Differentiating low-turnover from non–low-turnover bone disease, or “When do I stop therapy?” | 69% | 61% | 72% | 58% | 66% | 65% | 73% | 57% |
| Differentiating high-turnover from non–high-turnover bone disease, or “When do I start therapy?” | 58% | 78% | 35% | 90% | 37% | 86% | 35% | 87% |
iPTH, intact parathyroid hormone; KDIGO, Kidney Disease: Improving Global Outcomes; KDOQI, Kidney Disease Outcomes Quality Initiative; NPV, negative predictive value; PPV, positive predictive value; PTH, parathyroid hormone; Sens, sensitivity; Spec, specificity.
Using serum iPTH < 150 pg/ml (16 pmol/l) for lower and > 300 pg/ml (32 pmol/l) for upper threshold.
Using serum iPTH < 130 pg/ml (14 pmol/l) for lower and > 585 pg/ml (62 pmol/l) for upper threshold (2X and 9X of upper limit of normal for assay).
Reproduced with permission from Sprague SM, Bellorin-Font E, Jorgetti V, et al. Diagnostic accuracy of bone turnover markers and bone histology in patients with CKD treated by dialysis. Am J Kidney Dis. 2016;67:559–566.
A bone biopsy should also be considered in patients with unexplained fractures, refractory hypercalcemia, suspicion of osteomalacia, an atypical response to standard therapies for elevated PTH, or progressive decreases in BMD despite standard therapy. The goal of a bone biopsy would be to: (i) rule out atypical or unexpected bone pathology; (ii) determine whether the patient has high- or low-turnover disease, which may alter the dose of medications to treat renal osteodystrophy (e.g., initiate or discontinue calcimimetics, calcitriol, or vitamin D analogs); or (iii) identify a mineralization defect that would alter treatment (e.g., stop intake of aluminum, or aggressively treat hypophosphatemia or vitamin D deficiency).
The 2009 Guideline recommended a bone biopsy prior to antiresorptive therapy in patients with CKD G4 to G5D and evidence of biochemical abnormalities of CKD-MBD, low BMD, and/or fragility fractures. The rationale was that low BMD may be due to CKD-MBD (e.g., high PTH) and that lowering PTH is a safer and more appropriate therapy than an antiresorptive. In addition, there was concern that bisphosphonates would induce low-turnover bone disease. This was based on a single cross-sectional study in 13 patients with CKD G2 to G4 that were referred for bone biopsy after a variable duration of bisphosphonate therapy.32 To date, studies in patients with CKD have not definitively demonstrated that bisphosphonates cause adynamic bone disease. Furthermore, the concerns in patients with CKD are only theoretical, as it is well established that antiresorptive medications suppress bone formation rates, even in the absence of kidney disease. For example, in an RCT of zoledronic acid for the treatment of postmenopausal osteoporosis, bALP levels were 59% lower in the zoledronic acid group compared with the placebo group at 12 months.33
Despite these limitations, in weighing the risk-benefit ratio of bisphosphonate treatment, the 2009 KDIGO Guideline suggested a biopsy prior to therapy. Since 2009, an additional antiresorptive treatment (denosumab) has proven to be effective in CKD G3a to G3b and G4, as discussed in Recommendation 3.2.1. The growing experience with osteoporosis medications in patients with CKD increases the comfort of treating patients with low BMD and a high risk of fracture with antiresorptive therapy, although definitive trials are lacking. Furthermore, additional data clearly support that the incidence of fracture is markedly increased in patients with CKD, and thus the inability to perform a bone biopsy may not justify withholding antiresorptive therapy to patients at high risk of fracture. Thus, the Work Group voted to remove the requirement of bone biopsy prior to the use of antiresorptive therapy for osteoporosis because the use of these drugs must be individualized in patients with CKD. However, it is still prudent that these drugs be used with caution and that the underlying renal osteodystrophy be addressed first. With regard to efficacy, one may speculate that antiresorptive therapies confer less benefit in the absence of activated osteoclasts, as is the case in adynamic bone disease. Moreover, additional side effects such as acute kidney injury may also merit consideration in CKD G3a to G5.
In summary, bone biopsy is the gold standard for the assessment of renal osteodystrophy and should be considered in patients in whom the etiology of clinical symptoms and biochemical abnormalities is in question, and the results may lead to changes in therapy. With this statement, the Work Group is well aware that experience concerning performance and evaluation of bone biopsies is limited in many centers.34 With this in mind, in addition to the growing evidence that antiresorptive therapies are effective in patients with CKD G3a to G3b and G4, and the lack of robust evidence that these medications induce adynamic bone disease, the guideline no longer suggests that a bone biopsy be performed prior to initiation of these medications.
Research recommendation
-
•
Prospective studies of circulating biomarkers are needed to determine whether they can predict changes in bone histology.
Chapter 4.1: Treatment of CKD-MBD targeted at lowering high serum phosphate and maintaining serum calcium
4.1.1: In patients with CKD G3a–G5D, treatments of CKD-MBD should be based on serial assessments of phosphate, calcium, and PTH levels, considered together (Not Graded).
Rationale
The previous Recommendation 4.1.1 from the 2009 KDIGO CKD-MBD guideline gave treatment directions concerning serum phosphate levels in different GFR categories of CKD. The accumulated evidence on this issue to date is now depicted in Supplementary Tables S49–S51, S53–S55. Results of this evidence review can be summarized as follows: most studies showed increasing risk of all-cause mortality with increasing levels of serum phosphate in a consistent and direct fashion, with moderate risk of bias and low quality of evidence, thus not essentially different from the study results before 2009. For GFR decline and cardiovascular event rate, results were considered less conclusive.
Serum phosphate, calcium, and PTH concentrations are all routinely measured in CKD patients, and clinical decisions are often made based on these values. However, the results of these tests are influenced by food intake, adherence to and the timing of drug intake and dietary modifications, differences in assay methods and their intra-assay coefficient of variation (CV), and also by the interval from the last dialysis session in CKD G5D patients. Furthermore, it has recently been suggested that these markers undergo significant diurnal changes even in CKD patients.35, 36 Accordingly, the decision should be based not on a single result, but rather on the trends of serial results, which stands very much in accordance to 2009 Recommendation 3.1.4. In addition, recent post hoc analyses of large dialysis cohorts suggest that the prognostic implications of individual biochemical components of CKD-MBD largely depend on their context with regard to constellations of the full array of MBD biomarkers.37 This analysis identified a wide range of CKD-MBD phenotypes, based on phosphate, calcium, and PTH measurements categorized into mutually exclusive categories of low, medium, and high levels using previous Kidney Disease Outcomes Quality Initiative (KDOQI)/KDIGO guideline targets, further illustrating important potential interactions between components of CKD-MBD in terms of risk prediction for death or cardiovascular events. This analysis, however, did not provide guidance for treatment, because it is unknown whether switching from “risk classes” parallels changes in incidence of complications or mortality over time. Of note, biomarkers such as bALP and 25(OH)vitamin D were also still considered valuable, but as no new evidence has been published on their account, recommendations remained unchanged from the previous guideline (2009 Recommendations 3.1.3, 3.2.3).
Finally, therapeutic maneuvers aimed at improving 1 parameter often have unintentional effects on other parameters, as exemplified by the recent EVOLVE trial.38 The guideline Work Group considered it reasonable to take the context of therapeutic interventions into account when assessing values of phosphate, calcium, and PTH, and felt that it was important to emphasize the interdependency of these biochemical parameters for clinical therapeutic decision making.
Based on these assumptions, it was also decided to split previous 2009 Recommendation 4.1.1 into 2 new Recommendations, 4.1.1 (diagnostic recommendation based on accumulated observational evidence) and 4.1.2 (therapeutic recommendation based mostly on RCTs).
Research recommendations
-
•
Prospective cohort studies or RCTs are needed to evaluate whether changes in CKD-MBD risk marker patterns over time associate with changes in risk (e.g., multiple interventions).
-
•
Prospective cohort studies or RCTs are needed to examine whether biochemical abnormalities of CKD-MBD must be weighed differently when induced by pharmacotherapy compared with baseline values (e.g., past experience with hemoglobin as risk predictor vs. active treatment to targets by erythropoiesis-stimulating agents).
-
•
Investigations contributing to the understanding of the usefulness of fibroblast growth factor 23 (FGF23) as a complementary marker for treatment indications (e.g., phosphate-lowering therapies to halt CKD progression) and direct treatment target (e.g., regression of left ventricular hypertrophy [LVH]) should be undertaken.
4.1.2: In patients with CKD G3a–G5D, we suggest lowering elevated phosphate levels toward the normal range (2C).
Rationale
As outlined above, since publication of the 2009 KDIGO CKD-MBD Guideline, additional high-quality evidence now links higher concentrations of phosphate with mortality among patients with CKD G3a to G5 or after transplantation39, 40, 41, 42, 43, 44, 45, 46, 47, 48 (Supplementary Tables S49–S51, S53–S55), although some studies did not confirm this association.49, 50 However, trial data demonstrating that treatments that lower serum phosphate will improve patient-centered outcomes are still lacking, and therefore the strength of this recommendation remains weak (2C). The rationale of interventions, therefore, is still only based on epidemiological evidence as described above and biological plausibility pointing to possible phosphorus toxicity as recently summarized.51 Three recent historical cohort analyses from DOPPS, ArMORR, and COSMOS were not eligible for this evidence-based review; however, it is noteworthy that these analyses suggested that those dialysis patients who had been prescribed phosphate-binder therapy showed improved survival.52, 53, 54 It is important to note that phosphate-binder prescription was associated with better nutritional status. Indeed, correction for markers of nutritional status in the DOPPS study did mitigate the strength of the association, yet a statistically significant benefit persisted. In addition, propensity scoring attempting to correct for selection bias and subgroup analysis applied by Isakova et al.53 in the ArMORR cohort suggested robustness of the beneficial findings for those treated with phosphate binders. However, residual confounding still cannot be completely ruled out, and due to the nature of the observational data, these studies did not affect the current recommendation.
Methods to prevent the development of hyperphosphatemia essentially include dietary modification, the use of phosphate-lowering therapy, and intensified dialysis schedules for those with CKD G5D. In the 2009 KDIGO Guideline it was suggested to maintain serum phosphate in the normal range in the predialysis setting and lower serum phosphate toward the normal range in patients on dialysis. Interestingly, in the prospective observational COSMOS study cohort of HD patients (Supplementary Tables S49–S51, S53–S55), the best patient survival was observed with serum phosphate close to 4.4 mg/dl (1.42 mmol/l).55
The previous recommendation suggested that clinicians “maintain serum phosphate in the normal range” for patients with CKD G3a to G3b and G4. The Work Group reevaluated the evidence underlying this assumption. The majority of studies (Supplementary Table S49) found phosphate to be consistently associated with excess mortality at levels above and below the limits of normal, but not in the normal range.40, 41, 42, 43, 47, 48, 56, 57 This finding is in line with the previously found U-shaped relation of phosphate with mortality risk in dialysis patients.58 However, a recent trial comparing placebo with active phosphate-binder therapy in predialysis patients (CKD G3b–G4) with a mean baseline phosphate concentration of 4.2 mg/dl (1.36 mmol/l), found a minimal decline in serum phosphate, no effect on FGF23, and increases in coronary calcification scores for the active treatment group59—calling into question the efficacy and safety of phosphate binding in this population, with normal phosphate concentration prior to initiation of binder treatment (Supplementary Tables S19–24). In this analysis, all phosphate binders were analyzed collectively, and the study was underpowered to detect differences between phosphate binders. Although the data suggested that the observed increase in coronary artery calcification (CAC) was mainly driven by the group treated with calcium-containing phosphate binders, those treated with calcium-free binders had no advantage over placebo in terms of progression of CAC. In addition, a well-executed mineral balance study in predialysis patients using calcium-containing phosphate binders demonstrated the absence of any effect on phosphate balance (while showing in the short term a positive calcium balance).60
The second principal option to control phosphate in predialysis patients is dietary restriction, as will be addressed in Recommendation 4.1.8. However, in both the NHANES and MDRD cohorts that examined the general population and advanced CKD, respectively, dietary intake or intervention to reduce dietary phosphate intake as assessed by either urinary excretion or dietary recall had only minimal effects on serum phosphate.61, 62 It is unknown whether this minimal decline in serum phosphate concentrations or the more robust lower phosphate intake translates into beneficial clinical outcome. A subsequent analysis of the MDRD study found no impact of low phosphate intake as compared with higher intake on cardiovascular disease or all-cause mortality.63 It needs to be noted that in this study baseline phosphate levels were normal on average, so results are possibly not applicable to CKD patients with progressively or persistently elevated serum phosphate (see rationale for Recommendation 4.1.5).
Taken together, the key insights from these data were: (i) the association between serum phosphate and clinical outcome is not monotonic; (ii) there is a lack of demonstrated efficacy of phosphate binders for lowering serum phosphate in patients with CKD G3a to G4; (iii) the safety of phosphate binders in this population is unproven; and (iv) there is an absence of data showing that dietary phosphate restriction improves clinical outcomes. Consequently, the Work Group has abandoned the previous suggestion to maintain phosphate in the normal range, instead suggesting that treatment be focused on patients with hyperphosphatemia. The Work Group recognizes that preventing, rather than treating, hyperphosphatemia may be of value in patients with CKD G3a to G5D, but acknowledges that current data are inadequate to support the safety or efficacy of such an approach and encourages research in this specific area.
Only 2 RCTs have examined phosphate-lowering therapy in children with CKD or on dialysis;64, 65 due to the low number of patients and short follow-up, both studies did not meet literature inclusion criteria set a priori together with the evidence review team (ERT). The first RCT examined biochemical endpoints only and showed equivalent phosphate control with calcium acetate and sevelamer hydrochloride in an 8-week cross-over trial.65 In the second, 29 children were randomized to different combinations of phosphate binders and vitamin D analogs; bone biopsies suggested that the sevelamer group had reduced bone formation versus baseline at 8-month follow-up, but numbers were too small for comparison versus the calcium carbonate–treated group.64 Several studies in children on dialysis have shown an association between high phosphate levels and increased vessel thickness,66, 67, 68 vessel stiffness68, 69 and CAC.67, 68, 70, 71 In young adults on dialysis, the CAC score was shown to double within 20 months, and progression was associated with higher serum phosphate levels.71
Research recommendations
-
•
RCTs for controlling hyperphosphatemia in patients with CKD G3a to G5D, with appropriate follow-up and power, should be conducted to assess various phosphate-lowering therapy strategies for reducing the incidence of patient-level endpoints (e.g., CKD progression) in children and adults.
-
•
RCTs of low and high dietary phosphate intake in patients in CKD G3a to G5 should be conducted to test the hypothesis that high dietary phosphate intake increases cardiovascular risk either directly or indirectly through induction of FGF23.
-
•
If the feasibility of a placebo-controlled trial is threatened due to perceived lack of equipoise (i.e., “unethical” to not lower elevated serum phosphate levels, despite the lack of high-quality data), a prospective trial comparing 2 different phosphate targets in patients with CKD G3a to G5D is encouraged.
-
•
RCTs should be conducted in normophosphatemic CKD patients in order to test the hypothesis that active compensatory mechanisms to counterbalance increased phosphate intake (such as increases in FGF23 and PTH) are associated with poorer clinical outcome, despite comparable serum phosphate concentration. Interventions could include dietary phosphate restriction, phosphate-binder therapy, novel compounds to limit phosphate uptake, or a combination thereof.
4.1.3: In adult patients with CKD G3a–G5D, we suggest avoiding hypercalcemia (2C). In children with CKD G3a–G5D, we suggest maintaining serum calcium in the age-appropriate normal range (2C).
Rationale
As is the case for phosphate, novel epidemiological evidence linking higher calcium concentrations to increased mortality in adults with CKD has accumulated since the 2009 KDIGO CKD-MBD guideline (Supplementary Tables S49–S50, S52–S55).42, 43, 44, 47, 50, 60, 72, 73, 74 Moreover, and in addition to previous observations,48 novel studies link higher concentrations of serum calcium to nonfatal cardiovascular events.75, 76 This consistency justifies the change of this recommendation from 2D to 2C, although the overall evidence base remains limited due to the lack of prospective controlled trial data.
Hypocalcemia is a classical feature of untreated CKD, in part secondary to diminished gastrointestinal (GI) uptake of calcium due to vitamin D deficiency.77 Hypocalcemia contributes to the pathogenesis of secondary hyperparathyroidism (SHPT) and renal osteodystrophy. Therefore, the previous recommendation suggested maintaining serum calcium in the normal range, including the correction of hypocalcemia. A more recent retrospective observational analysis of a large dialysis cohort confirmed the association between hypocalcemia and mortality risk.50 Two other recent observations, however, raised doubt within the KDIGO guideline Work Group about the generalizability of the suggestion to correct hypocalcemia. The first is the potential harm for some adults associated with a positive calcium balance (while serum calcium levels do not necessarily reflect calcium balance).78, 79 The second observation is that the prevalence of hypocalcemia may have increased after the introduction of calcimimetics (cinacalcet) in patients on dialysis.38, 80, 81 The clinical implications of this increased incidence of low calcium due to the therapeutic institution of a calcimimetic is uncertain, but may be less harmful. With regard to the intention-to-treat (ITT) population of the EVOLVE trial, no negative signals were associated with the persistently low serum calcium levels in the cinacalcet arm of the trial. Retaining the 2009 KDIGO Guideline on this issue would support the concept that patients developing hypocalcemia during calcimimetic treatment require aggressive calcium treatment. Given the unproven benefits of this treatment and the potential for harm, the Work Group emphasizes an individualized approach to the treatment of hypocalcemia rather than recommending the correction of hypocalcemia for all patients. However, significant or symptomatic hypocalcemia should still be addressed. Symptomatic or severe hypocalcemia may benefit from correction to prevent adverse consequences such as bone disease, hyperparathyroidism, and QTc interval prolongation.
Childhood and adolescence are critical periods for bone mass accrual: in healthy children the calcium content of the skeleton increases from ∼25 g at birth to ∼1000 g in adults, and ∼25% of total skeletal mass is laid down during the 2-year interval of peak height velocity.82 The mean calcium accretion rate in healthy pubertal boys and girls peaks at 359 and 284 mg/d, respectively.83 The updated evidence review identified a prospective cohort study in 170 children and adolescents with CKD G2 to G5D (Supplementary Table S49–S50, S52–S55) that showed that lower serum calcium levels were independently associated with lower cortical volumetric BMD Z-scores.19 Over 1 year of follow-up in 89 children, a change in the cortical BMD Z-score positively correlated with baseline calcium (P = 0.008) and increase in calcium (P = 0.002) levels, particularly in growing children. During the 1-year follow-up, 6.5% of children sustained a fracture. Notably, a lower cortical BMD Z-score predicted future fractures: the HR for fracture was 1.75 (95% CI: 1.15–2.67; P = 0.009) per SD decrease in baseline BMD.19
Thus, the Work Group recognizes the higher calcium requirements of the growing skeleton and suggests that serum calcium levels are maintained in the age-appropriate normal range in children and adolescents.
Research recommendations
-
•
Calcium balance study in dialysis patients should be pursued at baseline versus after start of calcimimetic treatment (with and without calcium supplementation, adaptations in dialysate calcium concentrations, and/or concomitant active vitamin D analog treatment).
-
•
RCTs in children and adolescents with CKD should be conducted to determine whether calcium-based phosphate binders, as compared with calcium-free phosphate binders, promote bone accrual (as measured by bone density and structure, and fractures), and to determine the impact of phosphate binders on arterial calcification in the context of the high calcium requirement of growing bones.
4.1.4: In patients with CKD G5D, we suggest using a dialysate calcium concentration between 1.25 and 1.50 mmol/l (2.5 and 3.0 mEq/l) (2C).
Rationale
Based on the available evidence, the 2009 Work Group considered that a dialysate calcium concentration of 1.25 mmol/l (2.5 mEq/l) would yield neutral calcium balance, but this statement was subsequently challenged by kinetic modeling studies.84
Two relevant new RCTs are available concerning this topic (Supplementary Tables S13–S18).85, 86 In the study by Spasovski et al.,86 the effects of 2 different dialysate calcium concentrations were examined in patients with adynamic bone disease, and the lower dialysate calcium (1.25 mmol/l [2.5 mEq/l]) was found to improve bone and mineral parameters compared with the higher concentration of 1.75 mmol/l (3.5 mEq/l). Their data confirmed the results of previous papers and also support individualization of dialysate calcium concentrations as recommended previously by the Work Group. The comparator in this study, however, was a high dialysate calcium concentration of 1.75 mmol/l (3.5 mEq/l), leaving open the possibility that lower levels of dialysate calcium (>1.25 mmol/l [2.5 mEq/l] but <1.75 mmol/l [3.5 mEq/l]) would be equally beneficial. Ok et al. randomized 425 HD patients with iPTH levels < 300 pg/ml (32 pmol/l) and baseline dialysate calcium concentrations between 1.5 and 1.75 mmol/l (3.0–3.5 mEq/l) to concentrations of either 1.25 mmol/l (2.5 mEq/l) or 1.75 mmol/l (3.5 mEq/l).85 Lowering dialysate calcium levels slowed the progression of CAC and improved biopsy-proven bone turnover (low bone turnover decreased from 85.0% to 41.8%) in this cohort of patients on HD. In this trial, the comparative effects of a 1.5 mmol/l (3.0 mEq/l) calcium concentration were not addressed.
Retrospective observational data by Brunelli et al.87 suggested safety concerns (i.e., heart failure events, hypotension) associated with the default use of dialysate calcium concentrations < 1.25 mmol/l (2.5 mEq/l). Conversely, at the high end of dialysate calcium concentration (1.75 mmol/l [3.5 mEq/l]), Kim et al.88 found increased risk for all-cause mortality and cardiovascular or infection-related hospitalization in incident HD patients for high dialysate calcium. However, observational studies, in general, may not be sufficient to warrant changes to treatment recommendations.
Patients with mild hypocalcemia might potentially even have a positive calcium mass transfer when dialyzed against a concentration of 1.25 mmol/l (2.5 mEq/l), but no such metabolic balance studies exist. Taken together, the Work Group felt that this recommendation remains valid as written in 2009 and that there is no new evidence justifying a change in the wording. However, additional studies of better quality are now available, and as such the evidence grade has been upgraded from 2D to 2C.
Research recommendation
-
•
Calcium balance studies should be performed with non–calcium-containing versus calcium-containing phosphate binders, and vitamin D sterols versus cinacalcet in different calcium dialysate settings. These studies should include children and adolescents and assess calcium balance in the context of skeletal calcium accrual.
4.1.5: In patients with CKD G3a–G5D, decisions about phosphate-lowering treatment should be based on progressively or persistently elevated serum phosphate (Not Graded).
Rationale
With regard to 2017 Recommendation 4.1.5 (formerly 2009 Recommendation 4.1.4), the previous 2009 KDIGO CKD-MBD guideline commented that available phosphate binders are all effective in the treatment of hyperphosphatemia, and that there is evidence that calcium-free binders may favor halting progression of vascular calcifications compared with calcium-containing binders.30 Concerns about calcium balance and uncertainties about phosphate lowering in CKD patients not on dialysis, coupled with additional hard endpoint RCTs and a systematic review (comparing effects on mortality for calcium-free vs. calcium-containing phosphate binders), resulted in the decision to reevaluate this recommendation.
Based on new pathophysiological insights into phosphate regulation and the roles of FGF23 and (soluble) Klotho in early CKD, clinical studies had been initiated investigating phosphate-lowering therapies in CKD patients in whom hyperphosphatemia had not yet developed. Here, the concept of early phosphate retention, possibly represented by increases in FGF23 serum or plasma concentrations, was the focus of scientific attention. The most notable RCT was performed by Block et al.59 In this study, predialysis patients (CKD G3b–G4) with mean baseline serum phosphate concentrations of 4.2 mg/dl (1.36 mmol/l) were exposed to 3 different phosphate binders (sevelamer, lanthanum, or calcium acetate) versus matching placebos, in order to explore effects on serum phosphate levels, urinary phosphate excretion, serum FGF23 levels, vascular calcification, bone density, etc., with a 9-month follow-up (Supplementary Tables S19–S24). While there was a small decrease in serum phosphate concentrations (for those allocated to active treatment) and a 22% decrease in urinary phosphate excretion (suggesting adherence to therapy), no differences in changes in FGF23 levels were observed versus placebo, as already discussed in Recommendation 4.1.2. In contrast to the authors’ expectations, progression of coronary and aortic calcification was observed with active phosphate-binder treatment, while there was no progression in the placebo arm. Subgroup analysis suggested that this negative effect was accounted for by calcium acetate treatment, but neither calcium-free binders were superior to placebo with regard to this surrogate endpoint.
This study was further supported by another metabolic study in a small group of patients with CKD G3b to G4, in whom the addition of 3 × 500 mg calcium carbonate to meals containing 1 g of calcium and 1.5 g of phosphorus per day did not affect baseline neutral phosphate balance, but caused a significantly positive calcium balance,60 at least in the short term. Due to its low number of patients and short duration, this study did not fulfill the predefined inclusion criteria for full evidence review. Nevertheless, in the Work Group’s opinion, this well-performed metabolic study may present a plausible and relevant safety signal, and thus should be mentioned here.
Both Block et al.59 and Hill et al.60 studied subjects with essentially normal phosphate concentrations at baseline. Thus, there may be 2 key messages from these studies. First, normophosphatemia may not be an indication to start phosphate-lowering treatments. Second, the concept that not all phosphate binders are interchangeable must be noted. Whether disproportional elevations in FGF23 serum concentrations may become a signal in order to start phosphate-lowering therapies in early CKD will need to be investigated in appropriate trial settings.
Considering these insights, especially regarding CKD patients not on dialysis, and as already suggested in the rationale of Recommendation 4.1.2, the Work Group felt that the updated guideline should clarify that phosphate-lowering therapies may only be indicated in the event of “progressive or persistent hyperphosphatemia,” and not to prevent hyperphosphatemia. When thinking about risk-benefit ratios, even calcium-free binders may possess a potential for harm (e.g., due to side effects such as GI distress and binding of essential nutrients). The broader term “phosphate-lowering therapies” instead of phosphate-binding agents was introduced, because all possible approaches (i.e., binders, diet, and dialysis) can be effective and because phosphate transport inhibitors may expand the therapeutic armamentarium in the not-so-distant future.
There have been no additional data since 2008 with regard to “safe” phosphate level thresholds or hard endpoints (i.e., mortality, cardiovascular events, and progression of CKD) from RCTs treating patients toward different phosphate (or FGF23) targets. The previous qualifiers (presence of other components of CKD-MBD, concomitant therapies, side effect profile) were deleted because the Work Group thought that their consideration was self-evident. Diurnal variation of serum phosphate concentrations was discussed as another pathophysiologically relevant aspect of evaluation. While it was felt that these variations in daily phosphate levels do affect the accuracy of evaluations, the notion of variable timing for blood sampling was considered unfeasible in clinical routine practice and therefore not included in the guideline text.
Research recommendations
-
•
Prospective clinical trials studying the value of levels of FGF23 (and possibly soluble Klotho) as indicators for establishing phosphate-lowering therapies should be undertaken; desirable endpoints should include: CKD progression, cardiovascular calcification, cardiovascular events, and mortality.
-
•
See research recommendations following Recommendation 4.1.2.
4.1.6: In adult patients with CKD G3a–G5D receiving phosphate-lowering treatment, we suggest restricting the dose of calcium-based phosphate binders (2B). In children with CKD G3a–G5D, it is reasonable to base the choice of phosphate-lowering treatment on serum calcium levels (Not Graded).
Rationale
The Work Group thought that the new available data and the changes applied to 2009 Recommendation 4.1.4 (now Recommendation 4.1.5) suggested a need to revise the 2009 Recommendation 4.1.5 (now Recommendation 4.1.6). The balance study by Hill et al.60 supported results reported by Spiegel and Brady79 in normophosphatemic adults with CKD G3b to G4, which suggested potential harms of liberal calcium exposure in such cohorts, but due to their study designs were not eligible for full evidence review by the ERT. The RCT by Block et al.59 in a much larger, similar cohort and 2 additional RCTs in hyperphosphatemic CKD patients have added hard endpoint data when prospectively comparing the calcium-free binders, mostly sevelamer, with calcium-containing binders in predialysis or dialysis adult patients, respectively (Supplementary Tables S19–S24)59, 89, 90 These results were also supported by results from recent systematic reviews;91, 92, 93, 94 however, because the evidence review team (ERT) had considered all included studies separately and individually during this update process, these meta-analyses did not have additional bearing on the decision making by the Work Group.
Overall, the Work Group determined that there is new evidence suggesting that excess exposure to calcium through diet, medications, or dialysate may be harmful across all GFR categories of CKD, regardless of whether other candidate markers of risk such as hypercalcemia, arterial calcification, adynamic bone disease, or low PTH levels are also present. Therefore, these previous qualifiers in the 2009 KDIGO recommendation were deleted, acknowledging that they may still be valid in high-risk scenarios.
Di Iorio et al. reported RCTs in both predialysis and dialysis patients showing significant survival benefits over a 3-year interval for patients treated with sevelamer versus calcium-containing binders (Supplementary Tables S19–S24).89, 90 Both studies were analyzed by the ERT and were graded as relevant RCTs with a moderate risk of bias (Supplementary Tables S23 and S24), leading to a 2B recommendation. Overall, the findings from all identified studies seemed to show either a potential for benefit or an absence of harm associated with calcium-free phosphate-binding agents to treat hyperphosphatemia compared with calcium-based agents (Supplementary Tables S20 and S21).
The wording in Recommendation 4.1.6 of “restricting the dose of calcium-based phosphate binders” was retained from previous 2009 Recommendation 4.1.5; however, the qualifier that the recommendation applies to patients with persistent or recurrent hypercalcemia was removed. Given the fact of 2 reasonably large RCTs demonstrating mortality risks associated with calcium-containing binder treatment, it was debated within the Work Group whether the recommendation should be stronger, possibly using “avoid” instead of “restrict.” However, some members of the Work Group felt that available evidence does not conclusively demonstrate that calcium-free agents are superior to calcium-based agents. In addition, none of the studies provided sufficient dose threshold information about calcium exposure, nor did they give information on the safety of moderately dosed calcium-containing binders in combination therapies. Finally, because KDIGO guidelines are intended for a global audience and calcium-free agents are not available or affordable in all jurisdictions, recommending against the use of calcium-based binders would imply that no treatment is preferable to using calcium-based agents. Despite the understandable clinical desire to have numeric targets and limits, the Work Group could not make an explicit recommendation about a maximum dose of calcium-based binders, preferring to leave this to the judgment of individual physicians while acknowledging the potential existence of a safe upper limit of calcium dose. Of note, 2 short-term studies in stable CKD patients not on dialysis found that positive calcium balance may occur with total intakes as low as 800 and 1000 mg/d, respectively.60, 79 Such short-terms results are informative but not conclusive, and decisions must be individualized for each patient.
The recent availability of iron-containing phosphate binders was discussed within the Work Group but did not affect the recommendations given the absence of data on long-term patient-centered outcomes in the published phase 3 trials.95, 96, 97
All of the above studies were limited to adults. Importantly, concerns regarding the adverse effects of excess exposure to calcium through diet, medications, or dialysate may not be generalizable to children. Skeletal growth and development are characterized by rapid calcium accrual,83 as described in Recommendation 4.1.3. Furthermore, recent studies demonstrated that bone accrual continues into the third decade of life in healthy individuals, well beyond cessation of linear growth.98, 99 Of relevance to adolescents with CKD, bone accrual between ages 18 and 24 was especially pronounced among those with late puberty.100 Therefore, studies of calcium- and non–calcium-containing binders and other therapies that impact calcium balance should consider the needs of the developing skeleton. The observation that serum calcium levels were positively associated with increases in BMD in children with CKD, and that this association was significantly more pronounced with greater linear growth velocity,19 illustrates the unique needs of the growing skeleton (see Recommendation 4.1.3). Lastly, a recent prospective cohort study in 537 children with predialysis CKD demonstrated that phosphate-binder treatment (calcium-based in 82%) was associated with decreased risk of incident fractures (HR: 0.37, 95% CI: 0.15–0.91), independent of age, sex, eGFR, and PTH levels.101 Although this study did not meet the criteria for inclusion in the evidence review, it highlights the need for additional studies in children. There is a lack of data suggesting adverse effects of excess exposure to calcium through diet, medications or dialysate in children. The Work Group concluded that there was insufficient evidence to change this recommendation in children, who may be uniquely vulnerable to calcium restriction.
Research recommendations
-
•
Calcium and phosphate balance studies should be conducted using different calcium-based binder doses and combinations with calcium-free binders in hyperphosphatemic patients across all GFR categories of CKD.
-
•
RCTs assessing the effect of iron-based phosphate binders on patient-centered and surrogate outcomes across all GFR categories of CKD should be undertaken; comparators should be placebo, calcium-based binders, or other calcium-free binders.
-
•
RCTs using phosphate transport inhibitors (e.g., nicotinamide,102 tenapanor103) as “add-on” treatments in patients with resistant hyperphosphatemia should be investigated.
-
•
Prospective clinical and balance studies should examine the role of magnesium as a phosphate binder, with regard to patient-centered outcomes, calcification, and cardiovascular event rates.
-
•
RCTs in children and adolescents with CKD should be conducted to determine whether calcium-based phosphate binders, as compared with calcium-free phosphate binders, promote bone accrual (as measured by bone density and structure, and fractures), and to determine the impact of phosphate binders on arterial calcification in the context of the high calcium requirement of growing bones.
4.1.8: In patients with CKD G3a–G5D, we suggest limiting dietary phosphate intake in the treatment of hyperphosphatemia alone or in combination with other treatments (2D). It is reasonable to consider phosphate source (e.g., animal, vegetable, additives) in making dietary recommendations (Not Graded).
Rationale
There was no general controversy toward the 2009 KDIGO CKD-MBD Guideline on dietary phosphate restriction as an important standard of practice to lower elevated phosphate levels, but previous 2009 recommendation 4.1.7 (now 4.1.8) on limiting dietary phosphate intake was considered vague, especially with regard to new evidence on different phosphate and phosphoprotein sources. Within this guideline update, predefined criteria on study duration and cohort size prohibited inclusion of some study reports for full evidence review. Nevertheless, the Work Group felt that some of these reports presented safety signals demanding a brief discussion.
As summarized in Supplementary Tables S25–S30, only 2 studies on this topic in dialysis patients fulfilled the evidence review criteria.104, 105 Both studies investigated the impact of intensified versus routine dietary counseling on serum phosphate levels after a follow-up of 6 months. In both studies, the intensified counseling groups more successfully reached the laboratory targets; however, no hard endpoints were documented. Accordingly, the quality of evidence for outcome was rated as very low. Similarly, a recent Cochrane review concluded that there is low-quality evidence that dietary interventions positively affect CKD-MBD biomarkers.106
The daily phosphate intake for a typical American diet varies with age and gender. A majority of young to middle-aged men take in more than 1600 mg/d, whereas women in the same age groups take in about 1000 mg/d.107 On a global scale, there are quite significant differences in diet compositions to be considered. Estimates of dietary phosphate from food composition tables likely underestimate the phosphate content because they may mostly reflect the “natural” phosphate content of foods that are highest (e.g., dairy products, meats, poultry, fish, and grains). There are actually 3 major sources of phosphates: natural phosphates (as cellular and protein constituents) contained in raw or unprocessed foods, phosphates added to foods during processing, and phosphates in dietary supplements/medications.
Russo et al.108 assessed the effect of dietary phosphate restriction on the progression of CAC. This study was not designed to compare the efficacy of phosphate binders against dietary phosphate restriction. However, they found that dietary phosphate restriction alone did not lead to a decrease in urinary phosphate excretion, nor did it prevent progression of CAC. However, the urine data cast doubt on compliance with the diet, and there was no control group on a normal or high-phosphate diet.
Aggressive dietary phosphate restriction is difficult because it has the potential to compromise adequate intake of other nutrients, especially protein. Zeller et al.109 showed that the restriction of dietary protein and phosphate could be achieved with maintenance of good nutrition status with intense counseling. They demonstrated that dietary protein/phosphate restriction resulted in a significant reduction in urinary phosphate excretion when compared with a control diet.
Dietary supplements and over-the-counter or prescription medications are hidden sources of phosphate. They may contain phosphate salts within their inactive ingredients. The data on the amount of phosphate in oral medications and vitamin/mineral supplements is limited, but they have the potential to contribute significantly to the phosphate load considering the number of medications CKD patients are required to take.110, 111
Another consideration for modification of dietary phosphate and control of serum phosphate is the “bioavailability” of phosphorus in different foods based on the form—organic versus inorganic sources of phosphate. Animal- and plant-based foods contain the organic form of phosphate. Food additives contain inorganic phosphate. About 40% to 60% of animal-based phosphate is absorbed, depending on the GI vitamin D receptor activations. Plant phosphate, mostly associated with phytates, is less absorbable (generally 20%–50%) in the human GI tract. It behooves the dietitian and other interdisciplinary staff to include education about the best food choices as they relate to absorbable phosphate. Additionally, it is important for patients to be guided toward fresh and homemade foods rather than processed foods in order to avoid additives.
Organic phosphate in such plant foods as seeds and legumes is less bioavailable because of limited GI absorption of phytate-based phosphorus. In this context, Moe et al.35 recently demonstrated that a vegetable-based diet showed significantly lower phosphate absorption versus a meat-based diet with similar phosphate content. Inorganic phosphate is more readily absorbed, and its presence in additive-laden processed, preserved, or enhanced foods or soft drinks is likely to be underreported in nutrient databases. Hence, the phosphate burden from food additives is disproportionately high relative to natural sources that are derived from organic (animal and vegetable) food proteins, and these additives are almost completely absorbed in the GI tract. For example, Benini et al. showed that foods that contain phosphate additives have a phosphorus content nearly 70% higher than those that do not contain additives.112 Sherman and Mehta also demonstrated that phosphate contents between unprocessed and processed meat or poultry may differ by more than 60%, and thus the absorbable phosphate may even be 2 to 3 times higher per weight in processed food.113
In contrast, many of the foods that are traditionally labeled as high phosphorus may be more acceptable with the knowledge that the phosphorus is absorbed more slowly and not as efficiently. For example, beans and nuts have always been listed as very high in phosphorus; however, considering their lower absorption rate, they may be acceptable as protein sources, if they are not too high in other nutrients such as potassium.
The amount of phosphorus contributed by food intake is increasing with current and new processing practices that utilize phosphorus-containing ingredients, including popular foods such as restructured meats (formed, pressed, rolled, and shaped for ease of preparation and ingestion), processed and spreadable cheeses, “instant” products (puddings, sauces), frozen breaded products, and soft drinks.114 Phosphate additives are also widely used in fast foods and convenience foods that are fully or partially pre-made or instant.110
Various types of nutrition education have had mixed results for control of serum phosphate. Intense education focusing on phosphate intake has been useful to reduce retention in some studies.105, 115 A simple education tool on how to read food labels and “look for PHOS” (the study acronym) was successful in helping dialysis patients reduce their phosphate intake. A magnifying glass was provided to help patients read labels,116 as well as instructions available to guide “better choices” in fast-food restaurants. Other studies have had less favorable results.117
Taken together, these insights led the Work Group to the decision to not change the principal recommendation, but to add a qualifier statement suggesting that phosphate sources should be better substantiated and patient education should focus on best choices. Finally, it must be emphasized that efforts to restrict dietary phosphate must not compromise adequate protein intake.
Research recommendations
-
•
RCTs comparing low, medium, and high phosphate intake on phosphate metabolism and homeostasis, including responses concerning FGF23, PTH, calcification, and CKD progression, in patients in CKD G3b to G4, should be performed.
-
•
In such study designs, the role of the phosphate quality should be studied: vegetable versus meat versus additive sources.
-
•
Kinetic and balance studies on the uptake of phosphate additives in dialysis patients should be performed.
-
•
Prospective trials identifying the most effective phosphate-lowering approach (benefit-risk-cost ratio) should be performed across all CKD GFR categories—such as how best to combine phosphate binders, phosphate transport inhibitors and diet (plus dialysis treatment in CKD G5D)—with appropriate patient-centered and surrogate endpoints in mind (e.g., calcification, FGF23 levels, and LVH).
Chapter 4.2: Treatment of abnormal PTH levels in CKD-MBD
4.2.1: In patients with CKD G3a–G5 not on dialysis, the optimal PTH level is not known. However, we suggest that patients with levels of intact PTH progressively rising or persistently above the upper normal limit for the assay be evaluated for modifiable factors, including hyperphosphatemia, hypocalcemia, high phosphate intake, and vitamin D deficiency (2C).
Rationale
The pathogenesis of SHPT is complex and driven by several factors, including vitamin D deficiency, hypocalcemia, and hyperphosphatemia. Elevated FGF23 concentrations exacerbate SHPT through further reductions in 1,25(OH)2 vitamin D (calcitriol) levels. Calcitriol deficiency results in decreased intestinal absorption of calcium and may lead to hypocalcemia, a major stimulus for PTH secretion. This leads to parathyroid cell proliferation, contributing to SHPT. The incidence and severity of SHPT increases as kidney function declines and can lead to significant abnormalities in bone mineralization and turnover.
The 2009 KDIGO CKD-MBD Guideline recommended addressing modifiable risk factors for all patients with a PTH level above the upper limit of normal for the assay used.30 Unfortunately, there is still an absence of RCTs that define an optimal PTH level for patients with CKD G3a to G5, or clinical endpoints of hospitalization, fracture, or mortality. The Work Group felt that modest increases in PTH may represent an appropriate adaptive response to declining kidney function, due to its phosphaturic effects and increasing bone resistance to PTH,118 and have revised this statement to include “persistently” above the upper normal PTH level as well as “progressively rising” PTH levels, rather than simply “above the upper normal limit” as in the 2009 KDIGO Guideline. Thus, treatment should not be based on a single elevated value.
Although the optimal PTH is not known, the Work Group felt that rising PTH levels in CKD G3a-G5 warrant examination of modifiable factors, such as vitamin D insufficiency or deficiency, hypocalcemia, and hyperphosphatemia. In the interval since the 2009 KDIGO Guideline, 1 eligible RCT examined the impact of cholecalciferol supplementation (Supplementary Table S31) and 3 examined the impact of phosphate binders on PTH levels in the nondialysis CKD population. Oksa et al.119 reported an RCT of a high (20,000 international units [IU]/wk) versus low (5,000 IU/wk) dose of cholecalciferol supplementation in 87 adults with CKD G2 to G4 (Supplementary Tables S31–S36). Serum 25(OH) vitamin D levels increased significantly in both groups and were significantly greater in the high-dose arm at the completion of the 12-month intervention. PTH levels decreased significantly in both groups; however, the PTH levels did not differ significantly between groups at the completion of the study. In this context, Recommendation 3.1.3 on native vitamin D supplementation remains valid from the previous 2009 guideline publication.
Three recent RCTs in the nondialysis CKD population evaluated phosphate binders and their effects on surrogate endpoints, such as vascular calcification, arterial compliance, left ventricular mass, and BMD, as well as calcium, phosphate, and PTH levels. Two RCTs compared sevelamer with placebo (Supplementary Tables S31–S36), the first in 109 nondiabetic CKD G3a to G3b patients120 and the second in 117 CKD patients with a mean eGFR of 36 ± 17 ml/min/1.73 m2.121 The studies were conducted over 36 weeks and 24 months, respectively, and neither study demonstrated significant differences in PTH levels between sevelamer and placebo groups. Another RCT involving 148 CKD patients (eGFR: 20–45 ml/min/1.73 m2) compared placebo with 3 different phosphate binders (calcium-based, lanthanum, and sevelamer) over a 9-month period and reported that PTH levels remained stable in those on active therapy (combined phosphate-binder groups) but increased by 21% in the placebo group (P = 0.002)59 (Supplementary Table S33).
In the updated recommendation, an additional modifiable risk factor, “high phosphate intake,” was added because of the increasing recognition that excess phosphate intake does not always result in hyperphosphatemia, especially in early CKD, and that high phosphate intake may promote SHPT. While dietary phosphate, whether from food or additives, is modifiable, better methods for assessment of dietary phosphate intake are required.
4.2.2: In adult patients with CKD G3a–G5 not on dialysis, we suggest that calcitriol and vitamin D analogs not be routinely used (2C). It is reasonable to reserve the use of calcitriol and vitamin D analogs for patients with CKD G4–G5 with severe and progressive hyperparathyroidism (Not Graded).
In children, calcitriol and vitamin D analogs may be considered to maintain serum calcium levels in the age-appropriate normal range (Not Graded).
Rationale
Prevention and treatment of SHPT is important because imbalances in mineral metabolism are associated with CKD-MBD and higher PTH levels are associated with increased morbidity and mortality in CKD patients. Calcitriol and other vitamin D analogs have been the mainstay of treatment of SHPT in individuals with CKD for many decades. The 2009 KDIGO CKD-MBD Guideline summarized multiple studies demonstrating that administration of calcitriol or vitamin D analogs (such as paricalcitol, doxercalciferol, and alfacalcidol) resulted in suppression of PTH levels.30 However, there was a notable lack of trials demonstrating improvements in patient-centered outcomes.
Multiple well-conducted RCTs cited in the 2009 guideline reported benefits of calcitriol or vitamin D analogs in treating SHPT in patients with CKD G3a to G5; 2 primarily involved biochemical endpoints,122, 123 and 2 evaluated bone histomorphometry.124, 125 Despite the lack of hard clinical endpoints, these data led to the original recommendation to treat elevated PTH with calcitriol or vitamin D analogs early in CKD to prevent parathyroid hyperplasia and its skeletal consequences (2C). Although benefits were predominantly related to suppression of SHPT, adverse effects of hypercalcemia were noted to be of concern in the 2009 KDIGO CKD-MBD Guideline.30
The effects of vitamin D therapy on biochemical endpoints in CKD have been previously documented, especially with regard to reduced PTH levels. Numerous previous studies have reported significant reductions of PTH levels with calcitriol or vitamin D analogs in CKD G3a to G3b and G4 when compared with placebo123, 125, 126 and recent RCTs have also demonstrated that vitamin D treatment effectively lowers PTH levels in CKD G3a to G5.127, 128
Additional RCTs of calcitriol or vitamin D analog therapy have been published since the 2009 KDIGO CKD-MBD Guideline (Supplementary Tables S37–S42). Two, in particular, demonstrated a significantly increased risk of hypercalcemia in patients treated with paricalcitol, compared with placebo, in the absence of beneficial effects on surrogate cardiac endpoints, as detailed below.127, 128 These results, combined with the opinion that moderate PTH elevations may represent an appropriate adaptive response, led the Work Group to conclude that the risk-benefit ratio of treating moderate PTH elevations was no longer favorable and that the use of calcitriol or vitamin D analogs should be reserved for only severe and progressive SHPT.
The 2 recent RCTs were designed to detect potential benefits of calcitriol or vitamin D analogs on cardiac structure and function, as measured by magnetic resonance imaging (MRI), in adults with CKD (Supplementary Tables S37–S42). The rationale for these studies is that calcitriol and vitamin D analogs act through the vitamin D receptor (VDR) to exert their benefits to inhibit PTH secretion, and the VDR is also present in many tissues and organs including vascular smooth muscle, endothelial cells, and the heart. The key evidence for changes in Recommendation 4.2.2 predominantly came from these trials.
The first study was a double-blind RCT by Thadhani et al. (the PRIMO study), where participants with CKD G3a to G4, mild to moderate LVH, and PTH levels between 50 and 300 pg/ml (5.3–32 pmol/l) were assigned to placebo (n = 112) or paricalcitol (n = 115) to test the primary hypothesis that paricalcitol will reduce left ventricular mass index (LVMI) over a 48-week interval.128 Paricalcitol was administered at a dose of 2 μg/d, with protocol-specified dose reduction to 1 μg/d, if the serum calcium was > 11 mg/dl (2.75 mmol/l). Baseline PTH levels were approximately 1.5 times the upper limit of normal. The ITT analysis revealed that paricalcitol did not reduce LVMI, nor did it modify diastolic function. Of subjects on paricalcitol, the mean serum calcium increased by 0.32 mg/dl (0.08 mmol/l) (95% CI: 0.19–0.45 mg/dl; 0.05–0.11 mmol/l) versus a decrease by 0.25 mg/dl (0.06 mmol/l) (95% CI: −0.37 to −0.12 mg/dl; −0.09 to –0.03 mmol/l) in the placebo group. Hypercalcemia was defined as 2 consecutive measurements of serum calcium > 10.5 mg/dl (> 2.63 mmol/l), and the number of patients requiring dose reductions from 2 μg/d to 1 μg/d and episodes of hypercalcemia were more common in the paricalcitol group (22.6%) compared with the placebo (0.9%) group.
In the second key study, a double-blind RCT by Wang et al. (the OPERA study), subjects with CKD G3a to G5, LVH, and PTH ≥ 55 pg/ml (5.83 pmol/l) were randomly assigned to receive paricalcitol (n = 30) or placebo (n = 30).127 The primary endpoint was change in LVMI over 52 weeks. Baseline PTH levels were approximately twice the upper limit of normal. Change in LVMI did not differ significantly between groups, nor did secondary outcomes such as measures of systolic and diastolic function. The median (interquartile range) changes in serum calcium were 0.08 mmol/l (0.32 mg/dl) (95% CI: 0.02–0.16 mmol/l; 0.08–0.64 mg/dl) and 0.01 mmol/l (0.04 mg/dl) (95% CI: –0.06 to 0.05 mmol/l; –0.24 to 0.2 mg/dl) in the paricalcitol and placebo arms, respectively. Hypercalcemia, defined as any serum calcium > 2.55 mmol/l (> 10.2 mg/dl), occurred in 43.3% and 3.3% of participants in the paricalcitol and placebo arms, respectively. Of note, 70% of those who were hypercalcemic received concomitant calcium-based phosphate binders. Generally the hypercalcemia was mild and could be corrected by stopping the binder without changing the paricalcitol dose.
Recent meta-analyses were largely confirmatory and supported the hypercalcemia risk association with calcitriol and vitamin D analogs.129, 130
The evidence review identified 2 RCTs comparing paricalcitol with calcitriol (Supplementary Tables S37–S42); neither demonstrated differences in the incidence of hypercalcemia.131, 132 Coyne et al.131 compared calcitriol (0.25 μg/d) with paricalcitol (1 μg/d) in 110 patients with CKD G3a to G3b and G4 and PTH > 120 pg/ml (12.7 pmol/l). The change in PTH was comparable in the 2 arms (a decline of 52% vs. 46%) over the 6-month trial, and the incidence of hypercalcemia was very low in both groups (only 3 with paricalcitol and 1 with calcitriol). Further details regarding changes in biochemical parameters are provided in Supplementary Tables S37–S42.
An alternative to calcitriol and its analogs is “nutritional” vitamin D supplementation (cholecalciferol and ergocalciferol), which can also suppress PTH (especially in CKD G3a–G3b) and decrease hypercalcemia because the normal homeostatic loops that suppress the CYP27B remain intact. However, no studies of sufficient duration were identified in this evidence review, and thus this therapy remains unproven.
Several studies have assessed the effect of PTH-lowering comparing nutritional vitamin D supplements and calcitriol or vitamin D analogs.133, 134 However, these studies were not identified in this evidence review because of their short duration.
The use of extended-release calcifediol, a novel vitamin D prohormone, to correct low serum 25(OH) vitamin D levels and lower PTH has also been recently studied. This agent reduces the catabolism of both 25(OH) vitamin D and 1,25(OH)2 vitamin D and increases levels of both. An RCT of 429 patients with CKD G3a to G3b and G4 published after our guideline systematic review reported at least a 10% reduction of intact PTH levels in 72% of participants after 12 months, with no significant impact on calcium, phosphate, or FGF23 levels.135 No patient-level outcomes were reported, and thus this study did not impact the current recommendation.
All of the above studies were conducted in adults. A recent Cochrane review examined vitamin D therapy for bone disease in children with CKD G2 to G5 on dialysis.136 Bone disease, as assessed by changes in PTH levels, was improved by all vitamin D preparations regardless of route or frequency of administration. The prospective cohort study demonstrated that high PTH levels were independently associated with reduced cortical BMD Z-scores at baseline (P = 0.002) and 1-year follow-up (P < 0.001).19 High PTH levels are associated with CAC in children on dialysis.67, 68 The Cochrane review has not shown any significant difference in hypercalcemia risk with vitamin D preparations compared with placebo, but 1 study showed a significantly greater risk of hypercalcemia with i.v. calcitriol administration.136 No difference in growth rates was detected between different vitamin D analogs or use of oral or i.v. vitamin D treatments.136 As noted in Recommendation 4.1.3, the Work Group recommended that serum calcium should be maintained within age-appropriate reference range in children, and given the association of high PTH levels with reduced bone mineralization and increased vascular calcification, children are likely to require calcitriol or other active vitamin D analog therapy.
In summary, the PRIMO and OPERA studies failed to demonstrate improvements in clinically relevant outcomes but demonstrated increased risk of hypercalcemia. Accordingly, the guideline no longer recommends routine use of calcitriol or its analogs in CKD G3a to G5. This was not a uniform consensus among the Work Group. It should be noted that the participants in the PRIMO and OPERA trials only had moderately increased PTH levels, thus therapy with calcitriol and vitamin D analogs may be considered in those with progressive and severe SHPT.
There are still no RCTs demonstrating beneficial effects of calcitriol or vitamin D analogs on patient-level outcomes, such as cardiac events or mortality, and the optimal level of PTH in CKD G3a to G5 is not known. Furthermore, therapy with these agents may have additional harmful effects related to increases in serum phosphate and FGF23 levels. If initiated for severe and progressive SHPT, calcitriol or vitamin D analogs should be started with low doses, independent of the initial PTH concentration, and then titrated based on the PTH response. Hypercalcemia should be avoided.
Research recommendation
-
•
Multicenter RCTs should be conducted in children and adults to determine the benefits or harms of calcitriol or vitamin D analogs in patients with CKD G3a to G5; patient-level outcomes including falls, fractures, sarcopenia, muscle strength, physical function, progression to end-stage kidney disease, cardiovascular events, hospitalizations, and mortality should be assessed. Additional important patient-level outcomes to include are bone pain, pruritus, and health-related quality of life. Studies should also include patients with more severe SHPT and should determine the impact of reducing PTH to different target levels, such as the normal range versus higher levels.
4.2.4: In patients with CKD G5D requiring PTH-lowering therapy, we suggest calcimimetics, calcitriol, or vitamin D analogs, or a combination of calcimimetics with calcitriol or vitamin D analogs (2B).
Rationale
New data published since the 2013 KDIGO Madrid Controversies Conference prompted the Work Group to reappraise the use of PTH-lowering therapies in patients with CKD G5D. As shown in Supplementary Table S43, the ERT identified 2 new trials evaluating treatment with cinacalcet versus placebo and 1 new trial evaluating calcitriol versus a vitamin D analog. One open-label clinical trial was conducted evaluating the effect of cinacalcet on bone histomorphometry.145 There are still no new trials of calcitriol or vitamin D analogs that demonstrated clear benefits in patient-level outcomes.
The Work Group discussed the EVOLVE trial at length. EVOLVE evaluated the effect of cinacalcet versus placebo on patient-level outcomes in 3883 HD patients using a composite endpoint of all-cause mortality, nonfatal myocardial infarction, hospitalization for unstable angina, congestive heart failure, and peripheral vascular events. Secondary endpoints included individual components of the primary endpoint, clinical fracture, stroke, parathyroidectomy, and cardiovascular events and cardiovascular death.38
The results of EVOLVE have proven controversial. The unadjusted primary composite endpoint showed a nonsignificant reduction (HR: 0.93; P = 0.112) with cinacalcet use. However, analyses adjusted for imbalances in baseline characteristics demonstrated a nominally significant reduction in the primary composite endpoint (HR: 0.88; P = 0.008), as did sensitivity analyses accounting for patient nonadherence to randomized study medication (HR: 0.77; 95% CI: 0.70–0.92)137 or when patients were censored at the time of kidney transplant, parathyroidectomy, or the use of commercial cinacalcet (HR: 0.84; P ≤ 0.001).38 Further challenging the interpretation of the nonsignificant reduction in risk seen with the unadjusted primary endpoint was a significant treatment-age interaction (P = 0.03),38 leading to speculation that cinacalcet may be effective predominantly in older dialysis patients. Approximately one-third of the EVOLVE participants were under the age of 55, and prespecified analyses that evaluated subjects above or below age 65 demonstrated a significant reduction in risk associated with use of cinacalcet for both the primary endpoint (HR: 0.74; P ≤ 0.001) and all-cause mortality (HR: 0.73; P ≤ 0.001) for those aged above 65.138
The Work Group also considered additional prespecified and post hoc analyses from EVOLVE. These included a demonstrated significant reduction in the risk of severe unremitting SHPT (defined by the persistence of markedly elevated PTH concentrations [2 consecutive PTH values over 1000 pg/ml (106 pmol/l)] together with hypercalcemia [serum calcium > 10.5 mg/dl (2.63 mmol/l)] or parathyroidectomy). Cinacalcet appeared to consistently reduce the risk of this endpoint regardless of baseline PTH (HR: 0.31, P ≤ 0.001 for those with baseline PTH 300–600 pg/ml [32–64 pmol/l]; HR: 0.49, P ≤ 0.001 for those with baseline PTH 600–900 pg/ml [64–95 pmol/l]; HR: 0.41, P < 0.001 for those with PTH > 900 pg/ml [95 pmol/l]).139 Cinacalcet had no effect on the risk of clinical fractures in unadjusted analyses (HR: 0.93; P = 0.111) and showed a nominally significant reduction in risk of fracture when adjusted for age (HR: 0.88; P = 0.007).140
Thus, EVOLVE did not meet its primary endpoint that cinacalcet reduces the risk of death or clinically important vascular events in CKD G5D patients. However, the results of secondary analyses suggest that cinacalcet may be beneficial in this population or a subset. There was a lack of uniform consensus among the Work Group members in their interpretation of these data with regard to establishing cinacalcet as the recommended first-line therapy for patients with CKD G5D requiring PTH-lowering therapy. While some felt that only the primary analysis should be used to interpret the outcome, others were equally convinced that the secondary analyses strongly suggested a benefit of treatment with cinacalcet on important patient-level outcomes.
Despite these differences in interpretation, there was agreement among Work Group members that the higher cost of cinacalcet was also a relevant consideration given its uncertain clinical benefits. There was also agreement that the documented association between good clinical outcomes and the extent of FGF23 reduction with cinacalcet warrants further study.141
No trials demonstrated the benefits of combination therapy (cinacalcet plus another agent) on clinically relevant outcomes. However, several additional RCTs were identified that studied the effect of combination therapy on putative surrogate outcomes (summarized in Supplementary Tables S43–S48). Two trials evaluated the use of cinacalcet with low-dose active vitamin D versus standard therapy. Urena-Torres et al.142 demonstrated improved PTH-lowering efficacy in subjects treated with cinacalcet or low-dose active vitamin D, while Raggi et al.143 found that cinacalcet with low-dose vitamin D attenuated the progression of coronary artery calcium accumulation when assessed using calcium volume scores (P = 0.009) although not when using the more common Agatston score (P = 0.07). Two open-label trials of cinacalcet were considered important in reaching consensus for Recommendation 4.2.4. The PARADIGM trial compared a cinacalcet-based treatment strategy with an active vitamin D–based strategy in 312 HD patients and demonstrated similar reductions in PTH in both treatment arms.144 The BONAFIDE trial evaluated bone histomorphometry in 77 paired bone biopsy samples in cinacalcet-treated subjects with proven high-turnover bone disease and demonstrated reductions in bone formation rates and substantial increase in the number of subjects with normal bone histology (from 0 at baseline to 20 after 6–12 months of therapy).145 Two subjects developed adynamic bone disease, both of whom had PTH values < 150 pg/ml (16 pmol/l), and 1 patient developed osteomalacia coincident with hypophosphatemia. Despite being a prospective interventional trial, the BONAFIDE trial did not fulfill our literature inclusion criteria, because there was no control group and only longitudinal assessments were available, and thus is not listed in the Supplementary Tables.
It was recognized by the Work Group that newer, i.v. calcimimetic agents have undergone clinical trial investigation and were published after our guideline systematic review. However, while data on safety and efficacy were generated, no patient-level outcomes were reported. Therefore, these trials did not impact the current recommendation.146, 147
In summary, the Work Group was divided as to whether the EVOLVE data are sufficient to recommend cinacalcet as first-line therapy for all patients with SHPT and CKD G5D requiring PTH lowering. One viewpoint is that the primary endpoint of the EVOLVE study was negative. The alternative viewpoint is that secondary analyses found effects on patient-level endpoints, while there are no positive data on mortality or patient-centered endpoints from trials with calcitriol or other vitamin D analogs. Given the lack of uniform consensus among the Work Group and the higher acquisition cost of cinacalcet, it was decided to modify the 2009 recommendation to list all acceptable treatment options in alphabetical order. The individual choice should continue to be guided by considerations about concomitant therapies and the present calcium and phosphate levels. In addition, the choice of dialysate calcium concentrations will impact on serum PTH levels. Finally, it should be pointed out that parathyroidectomy remains a valid treatment option especially in cases when PTH-lowering therapies fail, as advocated in Recommendation 4.2.5 from the 2009 KDIGO CKD-MBD guideline.
To date, studies of cinacalcet in children are limited to case reports,148 case series,149, 150 a single-center experience (with 28 patients with CKD G4–G5),151 and an open-label study of a single dose in 12 children on dialysis.152 In recognition of the unique calcium demands of the growing skeleton, PTH-lowering therapies should be used with caution in children to avoid hypocalcemia. Future studies are needed in children before pediatric-specific recommendations can be issued.
Research recommendations
-
•
The Work Group explicitly endorses the presence of clinical equipoise and the need to conduct placebo-controlled trials with calcimimetics versus standard therapy for the treatment of SHPT in patients with CKD G5D with emphasis on those at greatest risk (e.g., older, with cardiovascular disease).
-
•
Prospective RCTs aiming at patient-centered surrogate outcomes (primary endpoints: mortality, cardiovascular events; secondary endpoints: FGF23, LVH progression, calcification) should be performed with the new parenteral calcimimetic compound (e.g., etelcalcitide).
-
•
Given the disparate effects of calcimimetic and active vitamin D therapies on FGF23 and data suggesting a clinical benefit from FGF23 reduction, RCTs evaluating the specific reduction of FGF23 as a therapeutic endpoint should be undertaken.
Chapter 4.3: Treatment of bone with bisphosphonates, other osteoporosis medications, and growth hormone
4.3.3: In patients with CKD G3a–G5D with biochemical abnormalities of CKD-MBD and low BMD and/or fragility fractures, we suggest that treatment choices take into account the magnitude and reversibility of the biochemical abnormalities and the progression of CKD, with consideration of a bone biopsy (2D).
Rationale
Recommendation 3.2.2 now addresses the indications for a bone biopsy prior to antiresorptive and other osteoporosis therapies. Therefore, the original Recommendation 4.3.4 from the 2009 KDIGO CKD-MBD Guideline has been removed, and Recommendation 4.3.3 has broadened from CKD G3a to G3b to CKD G3a to G5D. Nevertheless, when such treatment choices are considered, their specific side effects must also be taken into account (e.g., antiresorptives will exacerbate low bone turnover, denosumab may induce significant hypocalcemia), and the risk of their administration must be weighed against the accuracy of the diagnosis of the underlying bone phenotype.
Chapter 5: Evaluation and treatment of kidney transplant bone disease
5.5: In patients with CKD G1T–G5T with risk factors for osteoporosis, we suggest that BMD testing be used to assess fracture risk if results will alter therapy (2C).
Rationale
Fracture risk is 4-fold higher in patients with end-stage kidney disease153 compared with the general population and increases further in the early post-transplant period.154 A 2002 study examined the risk of hip fracture in kidney transplant recipients and estimated the fracture rate at 3.3 events per 1000 person-years, a 34% higher risk compared with patients receiving dialysis who were waitlisted for transplantation.3 Bone disease in transplant recipients is complex and heterogeneous.155 Essentially, transplant bone disease is the composite of preexisting damage to the bone acquired during the period of renal insufficiency and damage to the bone starting in the period of transplantation. In contrast to older studies,156 recent cohort studies showed minimal BMD losses in the early post-transplant period, which seem to be restricted to sites rich in cortical bone such as the distal radius.157 A low cumulative steroid exposure along with persistent hyperparathyroidism most likely accounts for this shift.157 The widespread implementation of steroid minimization protocols may explain the favorable trend in fracture risk in kidney transplant recipients observed over the last 2 decades.158, 159, 160
The 2009 KDIGO CKD-MBD Guideline30 recommended BMD testing in the first 3 months following transplantation in patients with an eGFR greater than 30 ml/min/1.73 m2 if they receive corticosteroids or have risk factors for osteoporosis (Recommendation 5.5), but recommended that DXA BMD not be performed in those with CKD G4T to G5T (Recommendation 5.7). As detailed in the new aforementioned Recommendation 3.2.1, there is growing evidence that DXA BMD predicts fractures across the spectrum of CKD severity, including 4 prospective cohort studies in patients with CKD G3a to G5D10, 13 (Supplementary Tables S7–S12). To date, there are no prospective studies addressing the ability of DXA to predict fractures in transplant recipients. However, a retrospective cohort study conducted in 238 kidney transplant recipients with CKD G1T to G5T examined the associations of DXA BMD with fracture events.161 Lumbar spine and total-hip BMD results were expressed as T-scores and categorized as normal (T-score ≥ −1), osteopenic (T-score < −1 and > −2.5), or osteoporotic (T-score ≤ −2.5). A total of 46 incident fractures were recorded in 53 patients. In a multivariate Cox analysis of DXA BMD results in the total hip, osteopenia (HR: 2.7, 95% CI: 1.6–4.6) and osteoporosis (HR: 3.5, 95% CI: 1.8–6.4) were associated with significantly increased risk of fracture compared with normal BMD, independent of age, sex, and diabetes. Multivariate models were not provided for the lumbar spine BMD T-score results; however, unadjusted analyses suggested that spine BMD provided less fracture prediction compared with total-hip BMD. Although this DXA study in kidney transplant recipients was not eligible for the evidence-based review due to its retrospective design, the Work Group concluded that the findings were consistent with the other studies in CKD G3a to G5D described above.
In summary, there is growing evidence that DXA BMD predicts fractures in patients with CKD across the spectrum, with limited data suggesting these findings extend to transplant recipients. The revised guideline statement recommends BMD testing in transplant recipients, as in those with CKD G3a to G5D, if the results will impact treatment decisions.
Research recommendations
-
•
The research recommendations outlined for Recommendation 3.2.1 should be expanded to include studies in kidney transplant recipients.
-
•
Prospective studies in patients with CKD G1T to G5T should be performed to determine the value of BMD and bone biomarkers as predictors of fractures.
- 5.6: In patients in the first 12 months after kidney transplant with an estimated glomerular filtration rate greater than approximately 30 ml/min/1.73 m2 and low BMD, we suggest that treatment with vitamin D, calcitriol/alfacalcidol, and/or antiresorptive agents be considered (2D).
-
•We suggest that treatment choices be influenced by the presence of CKD-MBD, as indicated by abnormal levels of calcium, phosphate, PTH, alkaline phosphatases, and 25(OH)D (2C).
-
•It is reasonable to consider a bone biopsy to guide treatment (Not Graded).
- There are insufficient data to guide treatment after the first 12 months.
-
•
Rationale
The rationale for revised guideline Recommendation 3.2.2 now addresses the indications for a bone biopsy prior to antiresorptive and other osteoporosis therapies. Therefore, the second bullet statement above concerning bone biopsies has been modified.
Cinacalcet is not approved for the treatment of hyperparathyroidism in kidney transplant recipients; however, it is clinically used, especially in patients with significant hypercalcemia. While efficiently correcting hypercalcemia, cinacalcet so far has failed to show a beneficial impact on bone mineralization in the transplant population.162 Denosumab was recently shown to effectively increase BMD in de novo kidney transplant recipients.163 However, baseline BMD on average was not very low in this trial, and there was no progressive BMD loss in the control group. Furthermore, an increased rate of urinary tract infections was observed. In terms of safety and efficacy, an RCT comparing denosumab and bisphosphonates in eligible patients at risk may be a reasonable future study approach. As pointed out in the rationale for Recommendation 5.5, however, the urgency for correcting bone mineralization in transplant recipients may diminish due to the wide application of steroid minimization schemes.159
Methodological approach to the 2017 KDIGO CKD-MBD guideline update
Purpose
In 2009, KDIGO developed a clinical practice guideline on the diagnosis, evaluation, prevention, and treatment of CKD-MBD.30 Because of the limited evidence, many of the recommendations were deliberately vague.
In October of 2013, KDIGO held a Controversies Conference to determine whether there was sufficient new evidence to support updating any of the recommendations. Based on the discussions at the conference, the participants opted for a “selective update” of the guideline.1
The purpose of this chapter is to describe the methods used to conduct the evidence review and to develop and update the guideline recommendations.
Overview of the Process
The process of updating the guideline consisted of the following steps:
-
•
Convening of a Controversies Conference to determine whether sufficient new data exist to support a reassessment of the guideline
-
•
Appointing a Work Group and an ERT
-
•
Refining the research questions
-
•
Developing the search strategy, inclusion/exclusion criteria, and data extraction tables
-
•
Drafting the evidence matrices and evidence profiles
-
•
Revising the recommendations
-
•
Grading the quality of the evidence
-
•
Grading the strength of the recommendation
Controversies Conference
In October 2013, KDIGO held a Controversies Conference entitled, “CKD-MBD: Back to the Future,” in Madrid, Spain.1 The purpose of the conference was to determine whether there was sufficient new evidence to support updating any of the recommendations from the 2009 KDIGO guideline on the diagnosis, evaluation, prevention, and treatment of CKD-MBD. Seventy-four experts in adult, pediatric, and transplant nephrology, endocrinology, cardiology, bone histomorphometry pathology, and epidemiology attended the conference.
Four topic areas were considered: (i) vascular calcification; (ii) bone quality; (iii) calcium and phosphate; and (iv) vitamin D and PTH. Each participant was assigned to 1 of the 4 topics based on their area of expertise. Participants identified new studies in their topic area and answered a set of questions to determine which recommendations required reevaluation.1
The result was a list of recommendations to be addressed in a selected update (i.e., to use specific methods to update only those parts of the guideline in need of update). There was a public review of the scope of work for the guideline.
Appointment of guideline Work Group and evidence review team
The KDIGO co-chairs appointed 2 chairs for the Guideline Work Group, who then assembled the Work Group to be responsible for the development of the guideline. The Work Group comprised domain experts, including individuals with expertise in adult and pediatric nephrology, bone disease, cardiology, and nutrition. The Johns Hopkins University in Baltimore, MD, was contracted as the ERT to provide expertise in guideline development methodology and systematic evidence review. KDIGO support staff provided administrative assistance and facilitated communication.
The ERT consisted of methodologists with expertise in nephrology and internal medicine, and research associates and assistants. The ERT and the Work Group worked closely throughout the project. In January 2015, the ERT and the Work Group Co-Chairs held a 2-day meeting in Baltimore, MD, to discuss the guideline development and systematic review processes and to refine the key questions.
The ERT performed systematic reviews for each of the questions conducting literature searches, abstract and full-text screening, data extraction, risk of bias assessment, and synthesis. The ERT provided suggestions and edits on the wording of recommendations, and on the use of specific grades for the strength of the recommendations and the quality of evidence. The Work Group took on the primary role of writing the recommendations and rationale, and retained final responsibility for the content of the recommendations and the accompanying narrative.
Refinement of the research questions
The first task was to define the overall topics and goals for the guideline. Using the recommendations identified during the Controversies Conference, the ERT drafted research questions and identified the population, interventions, comparison, and outcomes (PICO elements) for each research question.
The ERT recruited a technical expert panel to review the research questions. The technical expert panel included internal and external clinicians and researchers in nephrology and CKD. During a conference call, the technical expert panel provided feedback on the research questions.
The Work Group Co-Chairs and the ERT refined the research questions at the 2-day meeting in Baltimore, MD. During this meeting decisions were also made about outcomes, including those considered most important for decision making that would be graded (key outcomes). The finalized research questions and outcomes are presented in Table 2.
Search strategy
The ERT searched MEDLINE and the Cochrane Central Register of Controlled Trials (CENTRAL) for the date range of December 2006 through September 2015. The December 2006 date provided the recommended 1-year overlap with the end of the previous search.164 The search yield was also supplemented by articles provided by the Work Group members through February 2017.
The search strategy included MeSH and text terms for CKD and the interventions and markers of interest (Supplementary Appendix A) and was limited to the English language. The ERT also reviewed the list of references that were suggested during the Controversies Conference.
All studies that had been included in the prior guideline were rereviewed to ensure that they met the eligibility criteria.
Inclusion and exclusion criteria
With input from the Work Group, the ERT defined the eligibility criteria a priori. The eligibility criteria for all studies were: (i) original data published in English, (ii) followed up at least 10 patients with CKD for at least 6 months, and (iii) addressed 1 of the research questions. The minimum mean duration of follow-up of 6 months was chosen on the basis of clinical reasoning, accounting for the hypothetical mechanisms of action. For treatments of interest, the proposed effects on patient-centered outcomes require long-term exposure and typically would not be evident before several months of follow-up. The question-specific eligibility criteria are provided in Table 3, and the overall search yield for the guideline systematic review is summarized in Supplementary Appendix B.
Table 3.
Question-specific eligibility criteria
| 2009 recommendation no. | Exposure or intervention | Eligibility criteria |
|---|---|---|
| 3.2.1, 4.3.4 | Bisphosphonates, teriparatide, denosumab, or raloxifene |
|
| 3.2.2, 5.5, 5.7 | Predictive value of BMD results |
|
| 4.1.1, 4.1.2 | Serum phosphate or serum calcium levels |
|
| 4.1.3 | Dialysate calcium concentrations |
|
| 4.1.4, 4.1.7, 4.2.1, 4.2.2, 4.2.4 | Dietary phosphate intake, phosphate-binding agents, calcium supplements, native vitamin D, vitamin D analogs, calcitriol, or calcimimetics |
|
BMD, bone mineral density; FGF23, fibroblast growth factor 23; GFR, glomerular filtration rate; LVH, left ventricular hypertrophy; RCT, randomized controlled trial.
Two reviewers independently screened titles and abstracts and full-text articles for inclusion. Differences regarding inclusion were resolved through consensus adjudication.
Any study not meeting the inclusion criteria could be cited in the narrative but was not considered part of the body of evidence for a particular recommendation.
Data extraction
The ERT modified the online supplementary tables from the prior guideline. One reviewer abstracted data directly into the modified tables, and a second reviewer confirmed the data abstraction. The ERT abstracted data on general study characteristics, participant characteristics, interventions and co-interventions, and outcome measures, including measures of variability.
Two reviewers independently assessed individual study quality using the Cochrane Collaboration’s tool165 for assessing risk of bias for RCTs and using the Quality in Prognosis Studies tool166 for observational studies.
The Work Group critically reviewed draft tables, and tables were revised as appropriate.
Evidence matrices and evidence profiles
The ERT created evidence matrices for each of the key outcomes for each research question. For each key outcome, the matrix lists the individual studies, their sample size, follow-up duration, and the individual study quality. The ERT also drafted evidence profiles to display the total number and overall quality of the studies addressing each key outcome for each research question.
Revising recommendations
In June 2015, the Work Group and the ERT convened a 3-day meeting in Baltimore, MD, to review the summary tables, evidence profiles, and evidence matrices; to decide whether and how the recommendations should be revised; and to determine a grade that described the quality of the overall evidence and a grade for the strength of each recommendation.
Grading
A structured approach—modeled after Grading of Recommendations Assessment, Development, and Evaluation (GRADE)167, 168, 169, 170, 171, 172 and facilitated by the use of evidence profiles and evidence matrices—was used to determine a grade that described the quality of the overall evidence and a grade for the strength of a recommendation. For each topic, the discussion on grading of the quality of evidence was led by the ERT, and the discussion regarding the strength of the recommendations was led by the Work Group Chairs.
Grading the quality of evidence for each outcome
The ‘quality of a body of evidence’ refers to the extent to which our confidence in an estimate of effect is sufficient to support a particular recommendation. Following GRADE, the quality of a body of evidence pertaining to a particular outcome of interest is initially categorized on the basis of study design. For questions of interventions, the initial quality grade is “high” if the body of evidence consists of RCTs, “low” if it consists of observational studies, or “very low” if it consists of studies of other study designs. For questions of interventions, the Work Group graded only RCTs. The grade for the quality of evidence for each intervention–outcome pair was then decreased if there were serious limitations to the methodological quality of the aggregate of studies; if there were important inconsistencies in the results across studies; if there was uncertainty about the directness of evidence including a limited applicability of findings to the population of interest; if the data were imprecise or sparse; or if there was thought to be a high likelihood of bias. The final grade for the quality of evidence for an intervention–outcome pair could be 1 of the following 4 grades: “high,” “moderate,” “low,” or “very low” (Table 4).
Table 4.
GRADE system for grading quality of evidence for an outcome
| Step 1: starting grade for quality of evidence based on study design | Step 2: reduce grade | Step 3: raise grade | Final grade for quality of evidence for an outcomea |
|---|---|---|---|
| High for randomized controlled trials Moderate for quasi-randomized trial Low for observational study Very low for any other evidence |
Study quality –1 level if serious limitations –2 levels in very serious limitations Consistency –1 level if important inconsistency Directness –1 level if some uncertainty –2 levels if major uncertainty Other –1 level if sparse or imprecise data –1 level if high probability of reporting bias |
Strength of association +1 level is strong,b no plausible confounders, consistent and direct evidence +2 levels if very strong,c no major threats to validity and direct evidence Other +1 level if evidence of a dose-response gradient +1 level if all residual confounders would have reduced the observed effect |
High Moderate Low Very low |
GRADE, grading of recommendations assessment, development, and evaluation; RR, relative risk.
The highest possible grade is “high” and the lowest possible grade is “very low.”
Strong evidence of association is defined as “significant RR of > 2 (< 0.5)” based on consistent evidence from two or more observational studies, with no plausible confounders.
Very strong evidence of association is defined as “significant RR of > 5 (< 0.2)” based on direct evidence with no major threats to validity.
Modified with permission from Uhlig K, Macleod A, Craig J, et al. Grading evidence and recommendations for clinical practice guidelines in nephrology. A position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2006;70:2058–2065.171
Grading the overall quality of evidence
The quality of the overall body of evidence was then determined on the basis of the quality grades for all outcomes of interest, taking into account explicit judgments about the relative importance of each outcome. The resulting 4 final categories for the quality of overall evidence were A, B, C, and D (Table 5). This grade for overall evidence is indicated behind the strength of recommendations. The summary of the overall quality of evidence across all outcomes proved to be very complex. Thus, as an interim step, the evidence profiles recorded the quality of evidence for each of 3 outcome categories: patient-centered outcomes, other bone and vascular surrogate outcomes, and laboratory outcomes. The overall quality of evidence was determined by the Work Group and is based on an overall assessment of the evidence. It reflects that, for most interventions and tests, there is no high-quality evidence for net benefit in terms of patient-centered outcomes.
Table 5.
Final grade for overall quality of evidence
| Grade | Quality of evidence | Meaning |
|---|---|---|
| A | High | We are confident that the true effect lies close to that of the estimate of the effect. |
| B | Moderate | The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. |
| C | Low | The true effect may be substantially different from the estimate of the effect. |
| D | Very low | The estimate of effect is very uncertain, and often will be far from the truth. |
Assessment of the net health benefit across all important clinical outcomes
Net health benefit was determined on the basis of the anticipated balance of benefits and harm across all clinically important outcomes. The assessment of net health benefit by the Work Group and ERT is summarized in one of the following statements: (i) There is net benefit from intervention when benefits outweigh harm; (ii) there is no net benefit; (iii) there are trade-offs between benefits and harm when harm does not altogether offset benefits but requires consideration in decision making; or (iv) uncertainty remains regarding net benefit (Table 6).
Table 6.
Balance of benefits and harms
| When there was evidence to determine the balance of medical benefits and harm of an intervention to a patient, conclusions were categorized as follows: | |
|---|---|
| Net benefits | The intervention clearly does more good than harm. |
| Trade-offs | There are important trade-offs between the benefits and harm. |
| Uncertain trade-offs | It is not clear whether the intervention does more good than harm. |
| No net benefits | The intervention clearly does not do more good than harm. |
Grading the recommendations
The “strength of a recommendation” indicates the extent to which one can be confident that adherence to the recommendation will do more good than harm. The strength of a recommendation is graded as Level 1 or Level 2.173 Table 7 shows the nomenclature for grading the strength of a recommendation and the implications of each level for patients, clinicians, and policy makers. Recommendations can be for or against doing something. Table 8 shows that the strength of a recommendation is determined not just by the quality of evidence, but also by other, often complex judgments regarding the size of the net medical benefit, values and preferences, and costs.
Table 7.
Implications of the strength of a recommendation
| Grade | Implications |
||
|---|---|---|---|
| Patients | Clinicians | Policy | |
| Level 1: “We recommend” |
Most people in your situation would want the recommended course of action, and only a small proportion would not. | Most patients should receive the recommended course of action. | The recommendation can be evaluated as a candidate for developing a policy or a performance measure. |
| Level 2: “We suggest” |
The majority of people in your situation would want the recommended course of action, but many would not. | Different choices will be appropriate for different patients. Each patient needs help to arrive at a management decision consistent with her or his values and preferences. | The recommendation is likely to require substantial debate and involvement of stakeholders before policy can be determined. |
Table 8.
Determinants of strength of recommendation
| Factor | Comment |
|---|---|
| Balance between desirable and undesirable effects | The larger the difference between the desirable and undesirable effects, the more likely a strong recommendation is warranted. The narrower the gradient, the more likely a weak recommendation is warranted. |
| Quality of the evidence | The higher the quality of evidence, the more likely a strong recommendation is warranted. |
| Values and preferences | The more variability in values and preferences, or the more uncertainty in values and preferences, the more likely a weak recommendation is warranted. |
| Costs (resource allocation) | The higher the costs of an intervention—that is, the more resources consumed—the less likely a strong recommendation is warranted. |
Ungraded statements
The Work Group felt that having a category that allows it to issue general advice would be useful. For this purpose, the Work Group chose the category of a recommendation that was not graded. Typically, this type of ungraded statement met the following criteria: it provides guidance on the basis of common sense; it provides reminders of the obvious; and it is not sufficiently specific to allow an application of evidence to the issue, and therefore it is not based on a systematic review. Common examples include recommendations regarding the frequency of testing, referral to specialists, and routine medical care. The ERT and Work Group strove to minimize the use of ungraded recommendations.
Limitations of approach
Although the literature searches were intended to be comprehensive, they were not exhaustive. MEDLINE and Cochrane CENTRAL were the only databases searched, and the search was limited to English language publications. Hand searches of journals were not performed, and review articles and textbook chapters were not systematically searched. However, Work Group members did identify additional or new studies for consideration.
Nonrandomized studies were not systematically reviewed for studies of interventions. The ERT and Work Group resources were devoted to review of randomized trials, as these were deemed most likely to provide data to support treatment recommendations with higher-quality evidence.
Evidence for patient-relevant clinical outcomes was low. Usually, low-quality evidence required a substantial use of expert judgment in deriving a recommendation from the evidence reviewed.
Formulation and vetting of recommendations
Recommendations were drafted to be clear and actionable, and the wording also considered the ability of concepts to be translated accurately into other languages. The final wording of recommendations and corresponding grades for the strength of the recommendations and the quality of evidence were voted upon by the Work Group and required a majority to be accepted.
The process of peer review included an external review by the public to ensure widespread input from numerous stakeholders, including patients, experts, and industry and national organizations.
Format for chapters
Each chapter contains one or more specific recommendations. Within each recommendation, the strength of the recommendation is indicated as level 1 or level 2, and the quality of the overall supporting evidence is shown as A, B, C, or D. The recommendations are followed by a section that describes the body of evidence and rationale for the recommendations. In relevant sections, research recommendations suggest future research to resolve current uncertainties.
Biographic and disclosure information

Markus Ketteler, MD, FERA (Work Group co-chair), is professor of medicine and currently serves as Division Chief of Nephrology at the Klinikum Coburg in Coburg, Germany. In 2016, he was additionally appointed as chief medical officer at this institution. He is also chairman of the Medical Board of a large German not-for-profit dialysis provider (KfH Kuratorium für Dialyse und Nierentransplantation e.V.). His research focus is aimed at the understanding of the pathomechanisms involved in extraosseous calcifications, and of phosphate and vitamin D metabolism in CKD. He has authored more than 190 peer-reviewed publications including in The Lancet, Journal of the American Society of Nephrology (JASN), Journal of Clinical Investigation, and Kidney International. Dr. Ketteler has acted as local, national, or European Principal Investigator in several clinical multicenter trials in the CKD-MBD field (e.g., SVCARB, CALMAG, IMPACT-SHPT, PA-CL-05A and -05B, and NOPHOS). He serves on the editorial boards of nephrology journals such as JASN and Nephrology Dialysis Transplantation (theme editor), acted as a KDIGO Work Group member on the CKD-MBD Guideline from 2006 to 2009, and co-leads the German Calciphylaxis Registry. Dr. Ketteler is currently council member and chairman of the administrative office of the European Renal Association–European Dialysis and Transplant Association (ERA-EDTA) (2012–2018). He acted as co-chair of the KDIGO Controversies Conference on CKD-MBD, which took place in Madrid in October 2013. In 2017, he was elected into the board of directors of the Kidney Health Initiative, representing the ERA-EDTA for 3 years.
Consultant: Amgen, Fresenius Medical Care, Pfizer, Sanifit, Sanofi, Vifor Fresenius Medical Care Renal Pharma
Speaker: Amgen, BMS, Medice, Pfizer, Sanofi, Vifor Fresenius Medical Care Renal Pharma

Mary B. Leonard, MD, MSCE (Work Group co-chair), is the Arline and Pete Harman Professor and chair of the Department of Pediatrics at Stanford University School of Medicine. She is also the Adalyn Jay Physician-in-Chief of Lucile Packard Children’s Hospital, and the director of the Stanford Child Health Research Institute. Dr. Leonard received her MD degree from Stanford University and subsequently completed her pediatrics internship, residency, and nephrology fellowship at the Children’s Hospital of Philadelphia. After completing a master’s degree in clinical epidemiology at the University of Pennsylvania in 1997, she joined the faculty in the Departments of Pediatrics and Biostatistics and Epidemiology. She has maintained continuous National Institutes of Health funding for over 20 years, and her multidisciplinary research program is primarily focused on the impact of childhood chronic diseases on growth, skeletal development, nutrition, and physical function, with an emphasis on the detrimental effects of CKD. She co-chaired the ISCD Pediatric Position Development Conferences in 2007 and 2013. Dr. Leonard has served as an Associate Editor for Journal of the American Society of Nephrology and Journal of Bone and Mineral Research. She has published over 150 peer-reviewed manuscripts and is a member of the American Society of Clinical Investigation, American Pediatric Society, and the Society for Pediatric Research.
Dr. Leonard declared no competing interests.

Geoffrey A. Block, MD, is a clinical nephrologist and director of research at Denver Nephrology. He received his MD at the University of Cincinnati and completed his fellowship in nephrology at the University of Michigan, where he was trained under the mentorship of Dr. Friedrich Port at the United States Renal Data System. Dr. Block started a clinical research department at Denver Nephrology in 1998, and his primary research focus has been on clinical outcomes associated with CKD-MBD. He has published observational reports on the risks associated with disorders of mineral metabolism and has designed, conducted, and published numerous RCTs using a variety of interventions related to mineral metabolism and complications of CKD. He has served as a Work Group member on the 2009 KDIGO CKD-MBD guideline, 2 technical expert panels for Centers for Medicare and Medicaid Services related to bone and mineral disorders, and as a member of the steering committee for the EVOLVE trial. He serves as a reviewer for Clinical Journal of the American Society of Nephrology, Journal of the American Society of Nephrology, American Journal of Kidney Diseases, and Kidney International and was associate editor of Nephron-Clinical Practice.
Consultant: Ardelyx, Amgen, AstraZeneca, Celgene, Keryx, Kirin, Ono Pharmaceutical, OPKO
Grant/research support: Keryx*
Speaker: OPKO
Development of educational materials: Amgen, Keryx, OPKO
Stock/stock options: Ardelyx
Other: medical director, DaVita
*Monies paid to institution.

Pieter Evenepoel, MD, PhD, FERA, is head of the dialysis unit, division of nephrology, at the University Hospitals Leuven. Dr. Evenepoel completed his medical training at the Catholic University of Leuven, Belgium, in 1992, where he also received his PhD for research on protein assimilation and fermentation in 1997. In 2000, he joined the University Hospitals Leuven, where he gained his certification as Specialist in Internal Medicine and Nephrology. Dr. Evenepoel has maintained an active research interest in mainly clinical aspects of CKD-MBD, as exemplified by numerous original articles, review papers, and commentaries in this field. He is currently a board member of the European Renal Association–European Dialysis and Transplant Association (ERA-EDTA) working group on CKD-MBD. His research interests span areas including uremic toxins, nutrition, and anticoagulation, and he has authored over 200 publications. He serves presently as associate editor of Nephrology Dialysis Transplantation and editorial board member for Kidney International. He is also an Ordinary Council Member of the ERA-EDTA.
Consultant: Amgen, Vifor Fresenius Medical Care Renal Pharma
Grant/research support: Amgen, TECOmedical
Speaker: Amgen, Vifor Fresenius Medical Care Renal Pharma
Miscellaneous travel and meeting expenses unrelated to above: Amgen, Shire

Masafumi Fukagawa, MD, PhD, FASN, received his MD in 1983 from the University of Tokyo School of Medicine, Tokyo, Japan. Following a subspecialty training and PhD program in Tokyo, he was a research fellow at Vanderbilt University School of Medicine, Nashville, TN, until 1995. From 2000 to 2009, he was associate professor and director of the Division of Nephrology and Kidney Center at Kobe University School of Medicine, Kobe, Japan, and he later moved to Tokai University School of Medicine, Isehara, Japan, as professor of medicine and the director of the Division of Nephrology, Endocrinology, and Metabolism. He was international associate editor of Clinical Journal of the American Society of Nephrology (CJASN) (2005–2010) and currently serves as associate editor for Journal of Bone and Mineral Metabolism. He is an editorial board member for Kidney International, American Journal of Kidney Diseases, CJASN, Nephrology Dialysis Transplantation, and Clinical and Experimental Nephrology. In addition, he served as a Work Group member for the 2009 KDIGO CKD-MBD guideline and also chaired the committee for the new version of the Japanese clinical guideline on CKD-MBD by the Japanese Society for Dialysis Therapy.
Consultant: Kyowa Hakko Kirin, Ono Pharmaceutical, Torii
Grant/research support: Bayer Japan*, Kyowa Hakko Kirin*
Speaker: Bayer Japan, Kyowa Hakko Kirin, Torii
Manuscript preparation: Bayer Japan, Kyowa Hakko Kirin
*Monies paid to institution.
Charles A. Herzog, MD, FACC, FAHA, is professor of medicine at University of Minnesota and a cardiologist at Hennepin County Medical Center (HCMC) for 32 years. He founded the program in interventional cardiology at HCMC and served as cardiac catheterization laboratory director from 1985 to 1991, and cardiac ultrasound laboratory director from 1997 to 2012. He was director of the United States Renal Data System Cardiovascular Special Studies Center from 1999 to 2014. Dr. Herzog participated in the development of the National Kidney Foundation’s K/DOQI Clinical Practice Guidelines for Cardiovascular Disease in Dialysis Patients and KDIGO Clinical Practice Guideline on Acute Kidney Injury. He also co-chaired the 2010 KDIGO Controversies Conference, “Cardiovascular Disease in CKD: What is it and What Can We Do About It?” and is a co-chair of the ongoing KDIGO Kidney, Heart, and Vascular Conference Series. Dr. Herzog was an executive committee member of the EVOLVE trial, and presently he is chairing the renal committee of the ISCHEMIA-CKD trial and is co-principal investigator of the WED-HED (Wearable Cardioverter Defibrillator in Hemodialysis Patients) study. He has over 220 published papers and has served on the editorial boards of the American Heart Journal, Journal of Nephrology, Clinical Journal of the American Society of Nephrology, and liaison editor for Nephrology Dialysis Transplantation. His special interests include cardiac disease and CKD, and echocardiography.
Consultant: AbbVie, Fibrogen, Relypsa, Sanifit, ZS Pharma
Employment: Hennepin County Medical Center, Chronic Disease Research Group
Grants/research support: Amgen*, Zoll*
*Monies paid to institution.

Linda McCann, RD, CSR, has been a nephrology dietitian for over 43 years, focused on quality patient care, professional management, and electronic applications for kidney disease and nutrition. She is currently a nephrology nutrition consultant and speaker. Ms. McCann was a member of the original KDOQI and KDIGO advisory committees as well as the KDOQI and KDIGO (original and update) Work Groups that developed and published clinical practice guidelines and recommendations for bone and mineral abnormalities in CKD. She is the author of the popular National Kidney Foundation (NKF) publication, Pocket Guide to Nutrition Assessment of the Patient with Kidney Disease, currently in its fifth edition. She has authored book chapters and published multiple peer-reviewed papers in the area of nephrology nutrition. She has a long history of mentoring other professionals, driving clinical excellence, and is a dedicated patient advocate. Ms. McCann has also received numerous awards including: Recognized Renal Dietitian (Council on Renal Nutrition), Multiple Outstanding Service Awards (NKF), Award of Distinguished Service (NKF Northern California), Champion of Hope (NKF Northern California), Joel D. Kopple Award (NKF National), San Jose Business Journal 100 Women of Influence 2012, and the American Association of Kidney Patients Medal of Excellence.
Consultant: Amgen, Relypsa, Sanofi
Speaker: Amgen, Relypsa, Sanofi
Development of educational presentations: Amgen, Relypsa, Sanofi

Sharon M. Moe, MD, is the director of the Division of Nephrology and Stuart A. Kleit Professor of Medicine for the Indiana University School of Medicine. She received her medical degree from the University of Illinois–College of Medicine at Chicago in 1989 and completed her residency in Internal Medicine at Loyola University Medical Center in Maywood, IL. Her research and clinical fellowships were completed in nephrology at the University of Chicago in Illinois. Dr. Moe has been a faculty member at Indiana University since 1992 and is currently division director for nephrology in the Department of Medicine at Indiana University School of Medicine and section chief for nephrology at the Roudebush VA Medical Center. She has also served as the associate dean for Research Support in the Indiana University School of Medicine and the vice-chair for research in the Department of Medicine.
Dr. Moe is the principal investigator for several ongoing basic and clinical research studies in the field of CKD-MBD, including studies on vascular calcification, mineral metabolism, and bone metabolism in kidney disease. Her research is funded by the Veterans Affairs Department, the National Institutes of Health, foundations, and pharmaceutical companies. She has authored over 200 scientific manuscripts, teaching manuscripts, and textbook chapters. Dr. Moe served on the National Kidney Foundation's (NKF) KDOQI Bone and Mineral Metabolism Clinical Practice Guideline Work Group in 2003 and was co-chair of the international KDIGO CKD-MBD guideline released in 2009.
Dr. Moe’s key honors include: election to the American Society for Clinical Research in 2005; the NKF Garabed Eknoyan Award for exceptional contributions to key initiatives such as KDOQI in 2009; councilor to the American Heart Association Kidney Council (2002–2004); International Society of Nephrology (2005–2007); councilor for the American Society of Nephrology (2008–2015) and president of the American Society of Nephrology (2013-2014); and election to the Association of American Physicians in 2017.
Consultant: Lilly, Ultragenyx
Grants/research support: NIH, Veterans Administration
Speaker: Sanofi, University of Kansas
Stock/stock options: Lilly

Rukshana Shroff, MD, FRCPCH, PhD, is a consultant in pediatric nephrology at Great Ormond Street Hospital for Children in London, UK, and holds an academic position (reader) in nephrology at University College London. Her research focuses on cardiovascular disease in childhood CKD, including laboratory work, clinical research studies, and clinical trials. She is the principal investigator on a multicenter study comparing long-term outcomes of conventional hemodialysis and hemodiafiltration in children. She currently holds a prestigious senior fellowship from the National Institute for Health Research to continue research into mineral dysregulation in CKD. She has published more than 130 original articles, reviews, and book chapters in the fields of nephrology and dialysis. Dr. Shroff has also served on 2 guideline committees for the National Institute for Health and Care Excellence. She is on the council for the European Society for Pediatric Nephrology. She is presently an associate editor for Pediatric Nephrology and serves on the editorial board of Clinical Journal of the American Society of Nephrology.
Consultant: AstraZeneca
Grant/research support: Fresenius Medical Care*
Speaker: Amgen, Fresenius Medical Care
*Monies paid to institution.

Marcello A. Tonelli, MD, SM, FRCPC, is senior associate dean (clinical research) at the Cumming School of Medicine and associate vice president (health research) at the University of Calgary. He received an MD from the University of Western Ontario, specialist certification in nephrology (FRCPC) at Dalhousie University, an SM in epidemiology from Harvard University, and an MSc in health policy from Imperial College London. He is a nephrologist and professor at the University of Calgary.
Dr. Tonelli is the past president of the Canadian Society of Nephrology, a past councilor of the International Society of Nephrology, and the chair of the International Society of Nephrology Research Committee. He is a fellow of the Canadian Academy of Health Sciences, and a member of the American Society for Clinical Investigation. Dr. Tonelli is the chair of the Canadian Task Force for Preventive Health Care, a national panel of experts that makes recommendations about preventive health services to Canada’s 36,000 family physicians.
Dr. Tonelli was the recipient of the 2013 United States National Kidney Foundation Medal for Distinguished Service and also the 2013 Kidney Foundation of Canada Medal for Research Excellence.
Dr. Tonelli declared no competing interests.

Nigel D. Toussaint, MBBS, FRACP, PhD, is the deputy director of nephrology at Melbourne Health and a clinical associate professor within the Department of Medicine at the University of Melbourne, Australia. Dr. Toussaint completed his nephrology training in Melbourne in 2005 and completed his PhD studies at Monash University in 2009, undertaking clinical research in the area of vascular calcification and cardiovascular risk in patients with CKD. He has also completed a graduate diploma in clinical epidemiology (Monash University, 2007), and a National Health and Medical Research Council National Institute of Clinical Studies Fellowship (2011) in the area of implementation research. He is a member of the Editorial Board for Nephrology and is currently a member of council for the Australian and New Zealand Society of Nephrology.
Dr. Toussaint practices nephrology at The Royal Melbourne Hospital, where he is also the lead physician for clinical research within the Nephrology Department. His current research involves clinical epidemiology and clinical trials, as well as translational research, in the areas of CKD-MBD biomarkers, vascular calcification, and renal osteodystrophy. He has been an awardee of the Royal Australasian College of Physicians Jacquot Research Establishment Award and is a member of the Scientific Committee for the Australasian Kidney Trials Network and the steering committee for the Australia and New Zealand Dialysis and Transplant Registry.
Advisory board: Amgen, Sanofi, Shire
Consultant: Amgen, Sanofi, Shire
Grants/research support: Amgen*, Shire*
Speaker: Amgen, Sanofi, Shire
*Monies paid to institution.
Marc G. Vervloet, MD, PhD, FERA, is a nephrologist, associate professor of nephrology, and director of the nephrology research program and senior consultant at the Intensive Care Medicine and Vascular Medicine, VU University Medical Center, Amsterdam, Netherlands. He is program leader at the Institute of Cardiovascular Research VU (ICaR-VU), secretary of the CKD-MBD working group of the European Renal Association–European Dialysis and Transplant Association, and a member of the scientific committee of the Dutch Kidney Foundation. Dr. Vervloet obtained his medical degree in 1989, and graduated as internist in 1997 and as nephrologist in 1999. His current research interests encompass research on the deranged bone and metabolism in CKD. Dr. Vervloet currently heads the hemodialysis unit at his hospital, where he performs instructional duties to medical students, residents, and nephrology fellows, and guides several PhD students. He has gained numerous research grants, mainly covering topics related to CKD-MBD, in particular on the role of FGF23 and Klotho, and the clinical use of calcimimetic therapy. In addition, his laboratory research comprises several animal models of CKD and vitamin D deficiency, examining mainly cardiovascular endpoints as assessed by imaging and functional testing in vivo.
Advisory board: Amgen, Fresenius Medical Care
Consultant: Amgen, Fresenius Medical Care, Otsuka
Grants/research support: AbbVie*, Fresenius Medical Care*, Sanofi*, Shire*
Speaker: Amgen, Baxter
*Monies paid to institution.
KDIGO Chairs

David C. Wheeler, MD, FRCP, is professor of kidney medicine at University College London, UK, and honorary consultant nephrologist at the Royal Free London NHS Foundation Trust. He is a clinician scientist with an interest in the complications of CKD, specifically those that increase the burden of cardiovascular disease and/or accelerate progression of kidney failure. He has participated in the design, roll-out, and monitoring of several large-scale clinical trials. He was a member of the steering committee of the Study of Heart and Renal Protection (SHARP) and the EValuation Of Cinacalcet HCl Therapy to Lower CardioVascular Events (EVOLVE). He currently sits on the steering committee of Canaglifozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE), acting as UK principal investigator for this study. He is clinical lead for Division 2 of the North Thames Clinical Research Network and heads a team of eight clinical trial nurses and practitioners at the Centre for Nephrology, Royal Free Hospital in London. He is past president of the UK Renal Association and past chair of the UK Renal Registry. His other responsibilities include serving as associate editor of Nephrology Dialysis Transplantation and member of the editorial board of Journal of the American Society of Nephrology.
Consultant: Akebia, Alberta Innovates Health Solutions, Amgen, AstraZeneca, Bio Nano Consulting, Boehringer Ingelheim, Bristol-Myers Squibb, Fresenius, GSK, Janssen*, Otsuka, UCB Celltech, Vifor
Speaker: Amgen, Fresenius Medical Care, Janssen, Vifor Fresenius Medical Care Renal Pharma, ZS Pharma
*Monies paid to institution.

Wolfgang C. Winkelmayer, MD, MPH, ScD, is the Gordon A. Cain Chair of Nephrology and professor of medicine at Baylor College of Medicine in Houston, TX. Dr. Winkelmayer received his medical degree (1990) from the University of Vienna, Austria, and later earned a Master of Public Health degree in health care management (1999) and a Doctor of Science degree in health policy (2001) from Harvard University. He then spent 8 years on the faculty of Brigham and Women’s Hospital and Harvard Medical School, where he established himself as a prolific investigator and leader in the discipline of comparative-effectiveness research as it pertains to patients with kidney disease. From 2009 to 2014, he was the director of clinical research in the Division of Nephrology at Stanford University School of Medicine, Palo Alto, CA. He assumed his current position as chief of nephrology at Baylor College of Medicine in September 2014. His main areas of research interest include comparative effectiveness and safety research of treatment strategies in anemia as well as of various interventions for cardiovascular disease in patients with kidney disease. His clinical passion lies in providing quality kidney care to the predominantly disadvantaged and un(der)insured population in the public safety net health system of Harris County, TX. Dr. Winkelmayer has authored over 270 peer-reviewed publications, and he has a particular interest in medical publishing. He currently serves as an associate editor for The Journal of the American Medical Association, was a co-editor of the American Journal of Kidney Diseases from 2007 to 2016, and has been appointed to several other editorial boards of leading nephrology and epidemiology journals. He also volunteers his time toward important initiatives of the American Society of Nephrology (e.g., public policy board). He joined KDIGO volunteer leadership as an executive committee member in 2015 and has served as its co-chair since 2016.
Advisory board: Akebia, AMAG Pharmaceuticals, Amgen, AstraZeneca, Bayer, Daichi Sankyo, Medtronic, Relypsa, Vifor Fresensius Medical Care Renal Pharma
Consultant: Akebia, AMAG Pharmaceuticals, Amgen, AstraZeneca, Bayer, Daichi Sankyo, Medtronic, Relypsa, Vifor Fresensius Medical Care Renal Pharma
Evidence review team
Karen A. Robinson, PhD, is associate professor of medicine, epidemiology and health policy & management, and director of the Evidence-Based Practice Center at Johns Hopkins University, serving as the project director. She provided methodological expertise in the conduct of the systematic review and guideline development processes, and oversaw and participated in all aspects of the project, including topic refinement, abstract and full-text screening, data extraction, study assessment, evidence grading, and recommendation formulation.
Dr. Robinson declared no competing interests.
Casey M. Rebholz, PhD, MPH, MS, is assistant professor of epidemiology at Johns Hopkins Bloomberg School of Public Health and Core Faculty at the Welch Center for Prevention, Epidemiology, and Clinical Research. She guided the team through all phases of the project, including refining the questions, conducting literature searches, screening abstracts and full-text articles, abstracting data, drafting and finalizing the evidence tables, and synthesizing the results.
Dr. Rebholz declared no competing interests.
Lisa M. Wilson, ScM, is a research associate at the Johns Hopkins University Bloomberg School of Public Health. As the project coordinator for the evidence review team, Ms. Wilson managed and participated in all phases of the project, including conducting literature searches, screening abstracts and full-text articles, abstracting data, drafting and finalizing the evidence tables, and synthesizing the results.
Ms. Wilson declared no competing interests.
Ermias Jirru, MD, MPH, is currently an internal medicine resident at Mount Sinai St. Luke’s and Mount Sinai West. He completed his MPH at the Johns Hopkins University Bloomberg School of Public Health. For this project, he participated in screening abstracts and full-text articles, and abstracting data.
Dr. Jirru declared no competing interests.
Marisa Chi Liu, MD, MPH, is currently a resident physician at University of California, Irvine, in obstetrics and gynecology. She completed her MPH at Johns Hopkins University Bloomberg School of Public Health and graduated from the University of Vermont College of Medicine. For this project, she participated in screening abstracts and articles, and abstracting data.
Dr. Liu declared no competing interests.
Jessica Gayleard, BS, is a research assistant within the Johns Hopkins University Evidence-Based Practice Center. She participated in all phases of the project, including conducting literature searches, screening abstracts and full-text articles, abstracting data, and drafting and finalizing the evidence tables.
Ms. Gayleard declared no competing interests.
Allen Zhang, BS, is a research data analyst at the Johns Hopkins University Evidence-Based Practice Center. He has a degree in microbiology from the Virginia Polytechnic Institute and University. Mr. Zhang participated in the systematic review development, including search string creation, screening, data cleaning, data management, and writing. In addition, he supplied the necessary statistical analysis, including meta-analyses and meta-regression calculations.
Mr. Zhang declared no competing interests.
Acknowledgments
A special debt of gratitude is owed to the KDIGO co-chairs, David Wheeler and Wolfgang Winkelmayer, for their invaluable guidance throughout the development of this guideline. In particular, we thank Karen Robinson and her ERT members for their substantial contribution to the rigorous assessment of the available evidence. We are also especially grateful to the Work Group members for their expertise throughout the entire process of literature review, data extraction, meeting participation, the critical writing and editing of the statements and rationale, which made the publication of this guideline possible. The generous gift of their time and dedication is greatly appreciated. Finally, and on behalf of the Work Group, we gratefully acknowledge the careful assessment of the draft guideline by external reviewers. The Work Group considered all of the valuable comments made, and where appropriate, suggested changes were incorporated into the final publication. The following individuals provided feedback during the public review of the draft guideline:
Patricia Abreu, Adama Lengani, Kamal Ahmed, Bülent Altun, Luis Felipe Alva, Rui Alves, Pablo Amair, Alessandro Amore, Andrea Angioi, Mustafa Arici, Mariano Arriola, Rommel Bataclan, Ezequiel Bellorin-Font, Deborah Benner, Mohammed Benyahia, Patrick Biggar, Charles Bishop, Boris Bogov, Jordi Bover, Laura Brereton, Philippe Brunet, Rafael Burgos-Calderon, Stephen Carrithers, Sue Cary, Rolando Claure-Del Granado, Adrian Covic, Mario Cozzolino, Andrew Crannage, John Cunningham, Pierre Delanaye, Nida Dinçel, Tilman B. Drüeke, Nordin Eezsafryna Azalin, Grahame J. Elder, Madgy ElSharkawy, Joyce Ezaki-Yamaguchi, Toshiro Fujita, Alvaro Garcia, Carlo Francisco Gochuico, Heong Keong Goh, Hai An Ha Phan, Takayuki Hamano, Ditte Hansen, Li Hao, Eero Honkanen, Alastair Hutchison, Atul Ingale, Joachim H. Ix, Faical Jarraya, Chandra Mauli Jha, Kamyar Kalantar-Zadeh, Arif Khwaja, Csaba P. Kovesdy, Holly Kramer, Craig B. Langman, Kevin V. Lemley, Edgar V. Lerma, Nathan W. Levin, Maria Jesus Lloret, José António Lopes, Franklin W. Maddux, Francesca Mallamaci, Sandro Mazzaferro, Peter A. McCullough, Donald A. Molony, Sameh Morgan, Eugen Mota, Ricardo Mouzo, Lavinia Negrea, Armando Negri, Michal Nowicki, Tom Nusbickel, Basma Osman, Susan M. Ott, Antonino Paglialunga, Saime Paydas, Adriana Peñalba, Gerson Marques Pereira Junior, Eduardo Perez, Ligia Petrica, Friedrich K. Port, Pradeep Kumar Rai, Dwarakanathan Ranganathan, Nicolas Roberto Robles, Cibele Rodrigues, Hector Rodriguez, Guillermo Rosa Diez, Ibrahim Saig, Deepak Sharma, Laura Sola, David M. Spiegel, Kyriaki Stamatelou, Ekamol Tantisattamo, Mihály Tapolyai, Francesca Tentori, Katrin Uhlig, Harun Ur Rashid, Pablo Ureña Torres, Keth Vuthy, Angela Yee-Moon Wang, Talia Weinstein, Jane Wheeler, Janie Xiong, and Xueqing Yu.
Participation in the review does not necessarily constitute endorsement of the content of this report by the above individuals, or the organization or institution they represent.
Markus Ketteler, MD, FERA
Mary B. Leonard, MD, MSCE
Work Group Co-chairs
Footnotes
The 2009 Guideline Chapters 1 and 2 provide the Introduction and Methodological Approach, respectively, and therefore guideline recommendations begin in Chapter 3.1.
Supplementary Material
References
- 1.Ketteler M., Elder G.J., Evenepoel P. Revisiting KDIGO clinical practice guideline on chronic kidney disease-mineral and bone disorder: a commentary from a Kidney Disease: Improving Global Outcomes controversies conference. Kidney Int. 2015;87:502–528. doi: 10.1038/ki.2014.425. [DOI] [PubMed] [Google Scholar]
- 2.Alem A.M., Sherrard D.J., Gillen D.L. Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int. 2000;58:396–399. doi: 10.1046/j.1523-1755.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- 3.Ball A.M., Gillen D.L., Sherrard D. Risk of hip fracture among dialysis and renal transplant recipients. JAMA. 2002;288:3014–3018. doi: 10.1001/jama.288.23.3014. [DOI] [PubMed] [Google Scholar]
- 4.Nickolas T.L., McMahon D.J., Shane E. Relationship between moderate to severe kidney disease and hip fracture in the United States. J Am Soc Nephrol. 2006;17:3223–3232. doi: 10.1681/ASN.2005111194. [DOI] [PubMed] [Google Scholar]
- 5.Beaubrun A.C., Kilpatrick R.D., Freburger J.K. Temporal trends in fracture rates and postdischarge outcomes among hemodialysis patients. J Am Soc Nephrol. 2013;24:1461–1469. doi: 10.1681/ASN.2012090916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin Z.Z., Wang J.J., Chung C.R. Epidemiology and mortality of hip fracture among patients on dialysis: Taiwan National Cohort Study. Bone. 2014;64:235–239. doi: 10.1016/j.bone.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 7.Maravic M., Ostertag A., Torres P.U. Incidence and risk factors for hip fractures in dialysis patients. Osteoporos Int. 2014;25:159–165. doi: 10.1007/s00198-013-2435-1. [DOI] [PubMed] [Google Scholar]
- 8.Mittalhenkle A., Gillen D.L., Stehman-Breen C.O. Increased risk of mortality associated with hip fracture in the dialysis population. Am J Kidney Dis. 2004;44:672–679. [PubMed] [Google Scholar]
- 9.Tentori F., McCullough K., Kilpatrick R.D. High rates of death and hospitalization follow bone fracture among hemodialysis patients. Kidney Int. 2014;85:166–173. doi: 10.1038/ki.2013.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Iimori S., Mori Y., Akita W. Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients–a single-center cohort study. Nephrol Dial Transplant. 2012;27:345–351. doi: 10.1093/ndt/gfr317. [DOI] [PubMed] [Google Scholar]
- 11.Naylor K.L., Garg A.X., Zou G. Comparison of fracture risk prediction among individuals with reduced and normal kidney function. Clin J Am Soc Nephrol. 2015;10:646–653. doi: 10.2215/CJN.06040614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.West S.L., Lok C.E., Langsetmo L. Bone mineral density predicts fractures in chronic kidney disease. J Bone Miner Res. 2015;30:913–919. doi: 10.1002/jbmr.2406. [DOI] [PubMed] [Google Scholar]
- 13.Yenchek R.H., Ix J.H., Shlipak M.G. Bone mineral density and fracture risk in older individuals with CKD. Clin J Am Soc Nephrol. 2012;7:1130–1136. doi: 10.2215/CJN.12871211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bianchi M.L., Leonard M.B., Bechtold S. Bone health in children and adolescents with chronic diseases that may affect the skeleton: the 2013 ISCD Pediatric Official Positions. J Clin Densitom. 2014;17:281–294. doi: 10.1016/j.jocd.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Bishop N., Arundel P., Clark E. Fracture prediction and the definition of osteoporosis in children and adolescents: the ISCD 2013 Pediatric Official Positions. J Clin Densitom. 2014;17:275–280. doi: 10.1016/j.jocd.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Zemel B.S., Leonard M.B., Kelly A. Height adjustment in assessing dual energy x-ray absorptiometry measurements of bone mass and density in children. J Clin Endocrinol Metab. 2010;95:1265–1273. doi: 10.1210/jc.2009-2057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crabtree N.J., Arabi A., Bachrach L.K. Dual-energy X-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD Pediatric Official Positions. J Clin Densitom. 2014;17:225–242. doi: 10.1016/j.jocd.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 18.Griffin L.M., Kalkwarf H.J., Zemel B.S. Assessment of dual-energy X-ray absorptiometry measures of bone health in pediatric chronic kidney disease. Pediatr Nephrol. 2012;27:1139–1148. doi: 10.1007/s00467-012-2116-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Denburg M.R., Tsampalieros A.K., de Boer I.H. Mineral metabolism and cortical volumetric bone mineral density in childhood chronic kidney disease. J Clin Endocrinol Metab. 2013;98:1930–1938. doi: 10.1210/jc.2012-4188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ishani A., Blackwell T., Jamal S.A. The effect of raloxifene treatment in postmenopausal women with CKD. J Am Soc Nephrol. 2008;19:1430–1438. doi: 10.1681/ASN.2007050555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jamal S.A., Bauer D.C., Ensrud K.E. Alendronate treatment in women with normal to severely impaired renal function: an analysis of the fracture intervention trial. J Bone Miner Res. 2007;22:503–508. doi: 10.1359/jbmr.070112. [DOI] [PubMed] [Google Scholar]
- 22.Miller P.D., Roux C., Boonen S. Safety and efficacy of risedronate in patients with age-related reduced renal function as estimated by the Cockcroft and Gault method: a pooled analysis of nine clinical trials. J Bone Miner Res. 2005;20:2105–2115. doi: 10.1359/JBMR.050817. [DOI] [PubMed] [Google Scholar]
- 23.Miller P.D., Schwartz E.N., Chen P. Teriparatide in postmenopausal women with osteoporosis and mild or moderate renal impairment. Osteoporos Int. 2007;18:59–68. doi: 10.1007/s00198-006-0189-8. [DOI] [PubMed] [Google Scholar]
- 24.Jamal S.A., Ljunggren O., Stehman-Breen C. Effects of denosumab on fracture and bone mineral density by level of kidney function. J Bone Miner Res. 2011;26:1829–1835. doi: 10.1002/jbmr.403. [DOI] [PubMed] [Google Scholar]
- 25.Toussaint N.D., Lau K.K., Strauss B.J. Effect of alendronate on vascular calcification in CKD stages 3 and 4: a pilot randomized controlled trial. Am J Kidney Dis. 2010;56:57–68. doi: 10.1053/j.ajkd.2009.12.039. [DOI] [PubMed] [Google Scholar]
- 26.Haghverdi F., Farbodara T., Mortaji S. Effect of raloxifene on parathyroid hormone in osteopenic and osteoporotic postmenopausal women with chronic kidney disease stage 5. Iran J Kidney Dis. 2014;8:461–466. [PubMed] [Google Scholar]
- 27.Wren T.A., Kalkwarf H.J., Zemel B.S. Longitudinal tracking of dual-energy X-ray absorptiometry bone measures over 6 years in children and adolescents: persistence of low bone mass to maturity. J Pediatr. 2014;164:1280–1285. doi: 10.1016/j.jpeds.2013.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zemel B.S., Kalkwarf H.J., Gilsanz V. Revised reference curves for bone mineral content and areal bone mineral density according to age and sex for black and non-black children: results of the bone mineral density in childhood study. J Clin Endocrinol Metab. 2011;96:3160–3169. doi: 10.1210/jc.2011-1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moe S., Drueke T., Cunningham J. Definition, evaluation, and classification of renal osteodystrophy: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2006;69:1945–1953. doi: 10.1038/sj.ki.5000414. [DOI] [PubMed] [Google Scholar]
- 30.Kidney Disease: Improving Global Outcomes (KDIGO) CKD–MBD Work Group KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease–mineral and bone disorder (CKD–MBD) Kidney Int. 2009;76(Suppl 113):S1–S130. doi: 10.1038/ki.2009.188. [DOI] [PubMed] [Google Scholar]
- 31.Sprague S.M., Bellorin-Font E., Jorgetti V. Diagnostic accuracy of bone turnover markers and bone histology in patients with CKD treated by dialysis. Am J Kidney Dis. 2016;67:559–566. doi: 10.1053/j.ajkd.2015.06.023. [DOI] [PubMed] [Google Scholar]
- 32.Amerling R., Harbord N.B., Pullman J. Bisphosphonate use in chronic kidney disease: association with adynamic bone disease in a bone histology series. Blood Purif. 2010;29:293–299. doi: 10.1159/000276666. [DOI] [PubMed] [Google Scholar]
- 33.Black D.M., Delmas P.D., Eastell R. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 34.Evenepoel P, D'Haese P, Bacchetta J, et al. Bone biopsy practice patterns across Europe: the European renal osteodystrophy (EU-ROD) initiative-a position paper [e-pub ahead of print]. Nephrol Dial Transplant. 10.1093/ndt/gfw468. [DOI] [PubMed]
- 35.Moe S.M., Zidehsarai M.P., Chambers M.A. Vegetarian compared with meat dietary protein source and phosphorus homeostasis in chronic kidney disease. Clin J Am Soc Nephrol. 2011;6:257–264. doi: 10.2215/CJN.05040610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Viaene L., Meijers B., Vanrenterghem Y. Daytime rhythm and treatment-related fluctuations of serum phosphorus concentration in dialysis patients. Am J Nephrol. 2012;35:242–248. doi: 10.1159/000336308. [DOI] [PubMed] [Google Scholar]
- 37.Block G.A., Kilpatrick R.D., Lowe K.A. CKD-mineral and bone disorder and risk of death and cardiovascular hospitalization in patients on hemodialysis. Clin J Am Soc Nephrol. 2013;8:2132–2140. doi: 10.2215/CJN.04260413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chertow G.M., Block G.A., Correa-Rotter R. Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med. 2012;367:2482–2494. doi: 10.1056/NEJMoa1205624. [DOI] [PubMed] [Google Scholar]
- 39.Chartsrisak K., Vipattawat K., Assanatham M. Mineral metabolism and outcomes in chronic kidney disease stage 2-4 patients. BMC Nephrol. 2013;14:14. doi: 10.1186/1471-2369-14-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Connolly G.M., Cunningham R., McNamee P.T. Elevated serum phosphate predicts mortality in renal transplant recipients. Transplantation. 2009;87:1040–1044. doi: 10.1097/TP.0b013e31819cd122. [DOI] [PubMed] [Google Scholar]
- 41.Eddington H., Hoefield R., Sinha S. Serum phosphate and mortality in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:2251–2257. doi: 10.2215/CJN.00810110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fouque D., Roth H., Pelletier S. Control of mineral metabolism and bone disease in haemodialysis patients: which optimal targets? Nephrol Dial Transplant. 2013;28:360–367. doi: 10.1093/ndt/gfs404. [DOI] [PubMed] [Google Scholar]
- 43.Fukagawa M., Kido R., Komaba H. Abnormal mineral metabolism and mortality in hemodialysis patients with secondary hyperparathyroidism: evidence from marginal structural models used to adjust for time-dependent confounding. Am J Kidney Dis. 2014;63:979–987. doi: 10.1053/j.ajkd.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 44.Lacson E., Jr., Wang W., Hakim R.M. Associates of mortality and hospitalization in hemodialysis: potentially actionable laboratory variables and vascular access. Am J Kidney Dis. 2009;53:79–90. doi: 10.1053/j.ajkd.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 45.McGovern A.P., de Lusignan S., van Vlymen J. Serum phosphate as a risk factor for cardiovascular events in people with and without chronic kidney disease: a large community based cohort study. PLoS One. 2013;8:e74996. doi: 10.1371/journal.pone.0074996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Moore J., Tomson C.R., Tessa Savage M. Serum phosphate and calcium concentrations are associated with reduced patient survival following kidney transplantation. Clin Transplant. 2011;25:406–416. doi: 10.1111/j.1399-0012.2010.01292.x. [DOI] [PubMed] [Google Scholar]
- 47.Nakai S., Akiba T., Kazama J. Effects of serum calcium, phosphorous, and intact parathyroid hormone levels on survival in chronic hemodialysis patients in Japan. Ther Apher Dial. 2008;12:49–54. doi: 10.1111/j.1744-9987.2007.00540.x. [DOI] [PubMed] [Google Scholar]
- 48.Tentori F., Blayney M.J., Albert J.M. Mortality risk for dialysis patients with different levels of serum calcium, phosphorus, and PTH: the Dialysis Outcomes and Practice Patterns Study (DOPPS) Am J Kidney Dis. 2008;52:519–530. doi: 10.1053/j.ajkd.2008.03.020. [DOI] [PubMed] [Google Scholar]
- 49.Fliser D., Kollerits B., Neyer U. Fibroblast growth factor 23 (FGF23) predicts progression of chronic kidney disease: the Mild to Moderate Kidney Disease (MMKD) study. J Am Soc Nephrol. 2007;18:2600–2608. doi: 10.1681/ASN.2006080936. [DOI] [PubMed] [Google Scholar]
- 50.Floege J., Kim J., Ireland E. Serum iPTH, calcium and phosphate, and the risk of mortality in a European haemodialysis population. Nephrol Dial Transplant. 2011;26:1948–1955. doi: 10.1093/ndt/gfq219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gross P., Six I., Kamel S. Vascular toxicity of phosphate in chronic kidney disease: beyond vascular calcification. Circ J. 2014;78:2339–2346. doi: 10.1253/circj.cj-14-0735. [DOI] [PubMed] [Google Scholar]
- 52.Cannata-Andia J.B., Fernandez-Martin J.L., Locatelli F. Use of phosphate-binding agents is associated with a lower risk of mortality. Kidney Int. 2013;84:998–1008. doi: 10.1038/ki.2013.185. [DOI] [PubMed] [Google Scholar]
- 53.Isakova T., Gutierrez O.M., Chang Y. Phosphorus binders and survival on hemodialysis. J Am Soc Nephrol. 2009;20:388–396. doi: 10.1681/ASN.2008060609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lopes A.A., Tong L., Thumma J. Phosphate binder use and mortality among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study (DOPPS): evaluation of possible confounding by nutritional status. Am J Kidney Dis. 2012;60:90–101. doi: 10.1053/j.ajkd.2011.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fernandez-Martin J.L., Martinez-Camblor P., Dionisi M.P. Improvement of mineral and bone metabolism markers is associated with better survival in haemodialysis patients: the COSMOS study. Nephrol Dial Transplant. 2015;30:1542–1551. doi: 10.1093/ndt/gfv099. [DOI] [PubMed] [Google Scholar]
- 56.Scialla J.J., Astor B.C., Isakova T. Mineral metabolites and CKD progression in African Americans. J Am Soc Nephrol. 2013;24:125–135. doi: 10.1681/ASN.2012070713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Silva A.P., Fragoso A., Pinho A. Phosphorus as an early marker of morbidity and mortality in type 2 chronic kidney disease diabetic patients. J Diabetes Complications. 2013;27:328–332. doi: 10.1016/j.jdiacomp.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 58.Kalantar-Zadeh K., Kuwae N., Regidor D.L. Survival predictability of time-varying indicators of bone disease in maintenance hemodialysis patients. Kidney Int. 2006;70:771–780. doi: 10.1038/sj.ki.5001514. [DOI] [PubMed] [Google Scholar]
- 59.Block G.A., Wheeler D.C., Persky M.S. Effects of phosphate binders in moderate CKD. J Am Soc Nephrol. 2012;23:1407–1415. doi: 10.1681/ASN.2012030223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hill K.M., Martin B.R., Wastney M.E. Oral calcium carbonate affects calcium but not phosphorus balance in stage 3-4 chronic kidney disease. Kidney Int. 2013;83:959–966. doi: 10.1038/ki.2012.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.de Boer I.H., Rue T.C., Kestenbaum B. Serum phosphorus concentrations in the third National Health and Nutrition Examination Survey (NHANES III) Am J Kidney Dis. 2009;53:399–407. doi: 10.1053/j.ajkd.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Newsome B., Ix J.H., Tighiouart H. Effect of protein restriction on serum and urine phosphate in the modification of diet in renal disease (MDRD) study. Am J Kidney Dis. 2013;61:1045–1046. doi: 10.1053/j.ajkd.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 63.Selamet U., Tighiouart H., Sarnak M.J. Relationship of dietary phosphate intake with risk of end-stage renal disease and mortality in chronic kidney disease stages 3-5: The Modification of Diet in Renal Disease Study. Kidney Int. 2016;89:176–184. doi: 10.1038/ki.2015.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Salusky I.B., Goodman W.G., Sahney S. Sevelamer controls parathyroid hormone-induced bone disease as efficiently as calcium carbonate without increasing serum calcium levels during therapy with active vitamin D sterols. J Am Soc Nephrol. 2005;16:2501–2508. doi: 10.1681/ASN.2004100885. [DOI] [PubMed] [Google Scholar]
- 65.Pieper A.K., Haffner D., Hoppe B. A randomized crossover trial comparing sevelamer with calcium acetate in children with CKD. Am J Kidney Dis. 2006;47:625–635. doi: 10.1053/j.ajkd.2005.12.039. [DOI] [PubMed] [Google Scholar]
- 66.Litwin M., Wuhl E., Jourdan C. Evolution of large-vessel arteriopathy in paediatric patients with chronic kidney disease. Nephrol Dial Transplant. 2008;23:2552–2557. doi: 10.1093/ndt/gfn083. [DOI] [PubMed] [Google Scholar]
- 67.Oh J., Wunsch R., Turzer M. Advanced coronary and carotid arteriopathy in young adults with childhood-onset chronic renal failure. Circulation. 2002;106:100–105. doi: 10.1161/01.cir.0000020222.63035.c0. [DOI] [PubMed] [Google Scholar]
- 68.Shroff R.C., Donald A.E., Hiorns M.P. Mineral metabolism and vascular damage in children on dialysis. J Am Soc Nephrol. 2007;18:2996–3003. doi: 10.1681/ASN.2006121397. [DOI] [PubMed] [Google Scholar]
- 69.Mitsnefes M.M., Kimball T.R., Kartal J. Cardiac and vascular adaptation in pediatric patients with chronic kidney disease: role of calcium-phosphorus metabolism. J Am Soc Nephrol. 2005;16:2796–2803. doi: 10.1681/ASN.2005030291. [DOI] [PubMed] [Google Scholar]
- 70.Civilibal M., Caliskan S., Adaletli I. Coronary artery calcifications in children with end-stage renal disease. Pediatr Nephrol. 2006;21:1426–1433. doi: 10.1007/s00467-006-0159-6. [DOI] [PubMed] [Google Scholar]
- 71.Goodman W.G., Goldin J., Kuizon B.D. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000;342:1478–1483. doi: 10.1056/NEJM200005183422003. [DOI] [PubMed] [Google Scholar]
- 72.Coen G., Pierantozzi A., Spizzichino D. Risk factors of one year increment of coronary calcifications and survival in hemodialysis patients. BMC Nephrol. 2010;11:10. doi: 10.1186/1471-2369-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fein P.A., Asadi S., Singh P. Relationship between alkaline phosphatase and all-cause mortality in peritoneal dialysis patients. Adv Perit Dial. 2013;29:61–63. [PubMed] [Google Scholar]
- 74.Markaki A., Kyriazis J., Stylianou K. The role of serum magnesium and calcium on the association between adiponectin levels and all-cause mortality in end-stage renal disease patients. PLoS One. 2012;7:e52350. doi: 10.1371/journal.pone.0052350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gallieni M., Caputo F., Filippini A. Prevalence and progression of cardiovascular calcifications in peritoneal dialysis patients: A prospective study. Bone. 2012;51:332–337. doi: 10.1016/j.bone.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 76.Nakano C., Hamano T., Fujii N. Combined use of vitamin D status and FGF23 for risk stratification of renal outcome. Clin J Am Soc Nephrol. 2012;7:810–819. doi: 10.2215/CJN.08680811. [DOI] [PubMed] [Google Scholar]
- 77.Rutherford W.E., Blondin J., Hruska K. Effect of 25-hydroxycholecalciferol on calcium absorption in chronic renal disease. Kidney Int. 1975;8:320–324. doi: 10.1038/ki.1975.119. [DOI] [PubMed] [Google Scholar]
- 78.Raggi P., Bommer J., Chertow G.M. Valvular calcification in hemodialysis patients randomized to calcium-based phosphorus binders or sevelamer. J Heart Valve Dis. 2004;13:134–141. [PubMed] [Google Scholar]
- 79.Spiegel D.M., Brady K. Calcium balance in normal individuals and in patients with chronic kidney disease on low- and high-calcium diets. Kidney Int. 2012;81:1116–1122. doi: 10.1038/ki.2011.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chonchol M., Locatelli F., Abboud H.E. A randomized, double-blind, placebo-controlled study to assess the efficacy and safety of cinacalcet HCl in participants with CKD not receiving dialysis. Am J Kidney Dis. 2009;53:197–207. doi: 10.1053/j.ajkd.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 81.St Peter W.L., Li Q., Liu J. Cinacalcet use patterns and effect on laboratory values and other medications in a large dialysis organization, 2004 through 2006. Clin J Am Soc Nephrol. 2009;4:354–360. doi: 10.2215/CJN.05241008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Baxter-Jones A.D., Faulkner R.A., Forwood M.R. Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res. 2011;26:1729–1739. doi: 10.1002/jbmr.412. [DOI] [PubMed] [Google Scholar]
- 83.Bailey D.A., Martin A.D., McKay H.A. Calcium accretion in girls and boys during puberty: a longitudinal analysis. J Bone Miner Res. 2000;15:2245–2250. doi: 10.1359/jbmr.2000.15.11.2245. [DOI] [PubMed] [Google Scholar]
- 84.Gotch F.A., Kotanko P., Thijssen S. The KDIGO guideline for dialysate calcium will result in an increased incidence of calcium accumulation in hemodialysis patients. Kidney Int. 2010;78:343–350. doi: 10.1038/ki.2010.157. [DOI] [PubMed] [Google Scholar]
- 85.Ok E., Asci G., Bayraktaroglu S. Reduction of dialysate calcium level reduces progression of coronary artery calcification and improves low bone turnover in patients on hemodialysis. J Am Soc Nephrol. 2016;27:2475–2486. doi: 10.1681/ASN.2015030268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Spasovski G., Gelev S., Masin-Spasovska J. Improvement of bone and mineral parameters related to adynamic bone disease by diminishing dialysate calcium. Bone. 2007;41:698–703. doi: 10.1016/j.bone.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 87.Brunelli S.M., Sibbel S., Do T.P. Facility dialysate calcium practices and clinical outcomes among patients receiving hemodialysis: a retrospective observational study. Am J Kidney Dis. 2015;66:655–665. doi: 10.1053/j.ajkd.2015.03.038. [DOI] [PubMed] [Google Scholar]
- 88.Kim H.W., Kim S.H., Kim Y.O. Impact of dialysate calcium concentration on clinical outcomes in incident hemodialysis patients. Medicine (Baltimore) 2015;94:e1694. doi: 10.1097/MD.0000000000001694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Di Iorio B., Bellasi A., Russo D. Mortality in kidney disease patients treated with phosphate binders: a randomized study. Clin J Am Soc Nephrol. 2012;7:487–493. doi: 10.2215/CJN.03820411. [DOI] [PubMed] [Google Scholar]
- 90.Di Iorio B., Molony D., Bell C. Sevelamer versus calcium carbonate in incident hemodialysis patients: results of an open-label 24-month randomized clinical trial. Am J Kidney Dis. 2013;62:771–778. doi: 10.1053/j.ajkd.2013.03.023. [DOI] [PubMed] [Google Scholar]
- 91.Jamal S.A., Vandermeer B., Raggi P. Effect of calcium-based versus non-calcium-based phosphate binders on mortality in patients with chronic kidney disease: an updated systematic review and meta-analysis. Lancet. 2013;382:1268–1277. doi: 10.1016/S0140-6736(13)60897-1. [DOI] [PubMed] [Google Scholar]
- 92.Palmer S.C., Gardner S., Tonelli M. Phosphate-binding agents in adults With CKD: a network meta-analysis of randomized trials. Am J Kidney Dis. 2016;68:691–702. doi: 10.1053/j.ajkd.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 93.Patel L., Bernard L.M., Elder G.J. Sevelamer versus calcium-based binders for treatment of hyperphosphatemia in CKD: a meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol. 2016;11:232–244. doi: 10.2215/CJN.06800615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sekercioglu N., Thabane L., Diaz Martinez J.P. Comparative effectiveness of phosphate binders in patients with chronic kidney disease: a systematic review and network meta-analysis. PLoS One. 2016;11:e0156891. doi: 10.1371/journal.pone.0156891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Floege J., Covic A.C., Ketteler M. A phase III study of the efficacy and safety of a novel iron-based phosphate binder in dialysis patients. Kidney Int. 2014;86:638–647. doi: 10.1038/ki.2014.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Van Buren P.N., Lewis J.B., Dwyer J.P. The phosphate binder ferric citrate and mineral metabolism and inflammatory markers in maintenance dialysis patients: results from prespecified analyses of a randomized clinical trial. Am J Kidney Dis. 2015;66:479–488. doi: 10.1053/j.ajkd.2015.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lewis J.B., Sika M., Koury M.J. Ferric citrate controls phosphorus and delivers iron in patients on dialysis. J Am Soc Nephrol. 2015;26:493–503. doi: 10.1681/ASN.2014020212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ohlsson C., Darelid A., Nilsson M. Cortical consolidation due to increased mineralization and endosteal contraction in young adult men: a five-year longitudinal study. J Clin Endocrinol Metab. 2011;96:2262–2269. doi: 10.1210/jc.2010-2751. [DOI] [PubMed] [Google Scholar]
- 99.Berger C., Goltzman D., Langsetmo L. Peak bone mass from longitudinal data: implications for the prevalence, pathophysiology, and diagnosis of osteoporosis. J Bone Miner Res. 2010;25:1948–1957. doi: 10.1002/jbmr.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Darelid A., Ohlsson C., Nilsson M. Catch up in bone acquisition in young adult men with late normal puberty. J Bone Miner Res. 2012;27:2198–2207. doi: 10.1002/jbmr.1675. [DOI] [PubMed] [Google Scholar]
- 101.Denburg M.R., Kumar J., Jemielita T. Fracture burden and risk factors in childhood CKD: results from the CKiD cohort study. J Am Soc Nephrol. 2016;27:543–550. doi: 10.1681/ASN.2015020152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.El Borolossy R., El Wakeel L.M., El Hakim I. Efficacy and safety of nicotinamide in the management of hyperphosphatemia in pediatric patients on regular hemodialysis. Pediatr Nephrol. 2016;31:289–296. doi: 10.1007/s00467-015-3208-1. [DOI] [PubMed] [Google Scholar]
- 103.Block G.A., Rosenbaum D.P., Leonsson-Zachrisson M. Effect of tenapanor on serum phosphate in patients receiving hemodialysis. J Am Soc Nephrol. 2017;28:1933–1942. doi: 10.1681/ASN.2016080855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Karavetian M., de Vries N., Elzein H. Effect of behavioral stage-based nutrition education on management of osteodystrophy among hemodialysis patients. Lebanon. Patient Educ Couns. 2015;98:1116–1122. doi: 10.1016/j.pec.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 105.Lou L.M., Caverni A., Gimeno J.A. Dietary intervention focused on phosphate intake in hemodialysis patients with hyperphosphoremia. Clin Nephrol. 2012;77:476–483. [PubMed] [Google Scholar]
- 106.Liu Z., Su G., Guo X. Dietary interventions for mineral and bone disorder in people with chronic kidney disease. Cochrane Database Syst Rev. 2015:CD010350. doi: 10.1002/14651858.CD010350.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Calvo M.S., Park Y.K. Changing phosphorus content of the U.S. diet: potential for adverse effects on bone. J Nutr. 1996;126:1168S–1180S. doi: 10.1093/jn/126.suppl_4.1168S. [DOI] [PubMed] [Google Scholar]
- 108.Russo D., Miranda I., Ruocco C. The progression of coronary artery calcification in predialysis patients on calcium carbonate or sevelamer. Kidney Int. 2007;72:1255–1261. doi: 10.1038/sj.ki.5002518. [DOI] [PubMed] [Google Scholar]
- 109.Zeller K., Whittaker E., Sullivan L. Effect of restricting dietary protein on the progression of renal failure in patients with insulin-dependent diabetes mellitus. N Engl J Med. 1991;324:78–84. doi: 10.1056/NEJM199101103240202. [DOI] [PubMed] [Google Scholar]
- 110.Anderson J.J.B., Sell M.L., Garner S., Calvo M.S. Phosphorus. In: Bowman B.A., Russell R.M., editors. Present Knowledge of Nutrition. ILSI Press; Washington, DC: 2001. [Google Scholar]
- 111.Sherman R.A., Ravella S., Kapoian T. The phosphate content of prescription medication: a new consideration. Ther Innov Regul Sci. 2015;49:886–889. doi: 10.1177/2168479015592194. [DOI] [PubMed] [Google Scholar]
- 112.Benini O., D'Alessandro C., Gianfaldoni D. Extra-phosphate load from food additives in commonly eaten foods: a real and insidious danger for renal patients. J Ren Nutr. 2011;21:303–308. doi: 10.1053/j.jrn.2010.06.021. [DOI] [PubMed] [Google Scholar]
- 113.Sherman R.A., Mehta O. Phosphorus and potassium content of enhanced meat and poultry products: implications for patients who receive dialysis. Clin J Am Soc Nephrol. 2009;4:1370–1373. doi: 10.2215/CJN.02830409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Calvo M.S. Dietary considerations to prevent loss of bone and renal function. Nutrition. 2000;16:564–566. doi: 10.1016/s0899-9007(00)00313-0. [DOI] [PubMed] [Google Scholar]
- 115.Caldeira D., Amaral T., David C. Educational strategies to reduce serum phosphorus in hyperphosphatemic patients with chronic kidney disease: systematic review with meta-analysis. J Ren Nutr. 2011;21:285–294. doi: 10.1053/j.jrn.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 116.Sullivan C., Sayre S.S., Leon J.B. Effect of food additives on hyperphosphatemia among patients with end-stage renal disease: a randomized controlled trial. JAMA. 2009;301:629–635. doi: 10.1001/jama.2009.96. [DOI] [PubMed] [Google Scholar]
- 117.Durose C.L., Holdsworth M., Watson V. Knowledge of dietary restrictions and the medical consequences of noncompliance by patients on hemodialysis are not predictive of dietary compliance. J Am Diet Assoc. 2004;104:35–41. doi: 10.1016/j.jada.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 118.Evenepoel P., Bover J., Urena Torres P. Parathyroid hormone metabolism and signaling in health and chronic kidney disease. Kidney Int. 2016;90:1184–1190. doi: 10.1016/j.kint.2016.06.041. [DOI] [PubMed] [Google Scholar]
- 119.Oksa A., Spustova V., Krivosikova Z. Effects of long-term cholecalciferol supplementation on mineral metabolism and calciotropic hormones in chronic kidney disease. Kidney Blood Press Res. 2008;31:322–329. doi: 10.1159/000157177. [DOI] [PubMed] [Google Scholar]
- 120.Chue C.D., Townend J.N., Moody W.E. Cardiovascular effects of sevelamer in stage 3 CKD. J Am Soc Nephrol. 2013;24:842–852. doi: 10.1681/ASN.2012070719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lemos M.M., Watanabe R., Carvalho A.B. Effect of rosuvastatin and sevelamer on the progression of coronary artery calcification in chronic kidney disease: a pilot study. Clin Nephrol. 2013;80:1–8. doi: 10.5414/CN107630. [DOI] [PubMed] [Google Scholar]
- 122.Coyne D., Acharya M., Qiu P. Paricalcitol capsule for the treatment of secondary hyperparathyroidism in stages 3 and 4 CKD. Am J Kidney Dis. 2006;47:263–276. doi: 10.1053/j.ajkd.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 123.Coburn J.W., Maung H.M., Elangovan L. Doxercalciferol safely suppresses PTH levels in patients with secondary hyperparathyroidism associated with chronic kidney disease stages 3 and 4. Am J Kidney Dis. 2004;43:877–890. doi: 10.1053/j.ajkd.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 124.Nordal K.P., Dahl E. Low dose calcitriol versus placebo in patients with predialysis chronic renal failure. J Clin Endocrinol Metab. 1988;67:929–936. doi: 10.1210/jcem-67-5-929. [DOI] [PubMed] [Google Scholar]
- 125.Hamdy N.A., Kanis J.A., Beneton M.N. Effect of alfacalcidol on natural course of renal bone disease in mild to moderate renal failure. BMJ. 1995;310:358–363. doi: 10.1136/bmj.310.6976.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Fishbane S., Chittineni H., Packman M. Oral paricalcitol in the treatment of patients with CKD and proteinuria: a randomized trial. Am J Kidney Dis. 2009;54:647–652. doi: 10.1053/j.ajkd.2009.04.036. [DOI] [PubMed] [Google Scholar]
- 127.Wang A.Y., Fang F., Chan J. Effect of paricalcitol on left ventricular mass and function in CKD–the OPERA trial. J Am Soc Nephrol. 2014;25:175–186. doi: 10.1681/ASN.2013010103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Thadhani R., Appelbaum E., Pritchett Y. Vitamin D therapy and cardiac structure and function in patients with chronic kidney disease: the PRIMO randomized controlled trial. JAMA. 2012;307:674–684. doi: 10.1001/jama.2012.120. [DOI] [PubMed] [Google Scholar]
- 129.Li X.H., Feng L., Yang Z.H. The effect of active vitamin d on cardiovascular outcomes in predialysis chronic kidney diseases: a systematic review and meta-analysis. Nephrology (Carlton) 2015;20:706–714. doi: 10.1111/nep.12505. [DOI] [PubMed] [Google Scholar]
- 130.Xu L., Wan X., Huang Z. Impact of vitamin D on chronic kidney diseases in non-dialysis patients: a meta-analysis of randomized controlled trials. PLoS One. 2013;8:e61387. doi: 10.1371/journal.pone.0061387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Coyne D.W., Goldberg S., Faber M. A randomized multicenter trial of paricalcitol versus calcitriol for secondary hyperparathyroidism in stages 3-4 CKD. Clin J Am Soc Nephrol. 2014;9:1620–1626. doi: 10.2215/CJN.10661013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Riccio E., Sabbatini M., Bruzzese D. Effect of paricalcitol vs calcitriol on hemoglobin levels in chronic kidney disease patients: a randomized trial. PLoS One. 2015;10:e0118174. doi: 10.1371/journal.pone.0118174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Kovesdy C.P., Lu J.L., Malakauskas S.M. Paricalcitol versus ergocalciferol for secondary hyperparathyroidism in CKD stages 3 and 4: a randomized controlled trial. Am J Kidney Dis. 2012;59:58–66. doi: 10.1053/j.ajkd.2011.06.027. [DOI] [PubMed] [Google Scholar]
- 134.Moe S.M., Saifullah A., LaClair R.E. A randomized trial of cholecalciferol versus doxercalciferol for lowering parathyroid hormone in chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:299–306. doi: 10.2215/CJN.07131009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sprague S.M., Crawford P.W., Melnick J.Z. Use of extended-release calcifediol to treat secondary hyperparathyroidism in stages 3 and 4 chronic kidney disease. Am J Nephrol. 2016;44:316–325. doi: 10.1159/000450766. [DOI] [PubMed] [Google Scholar]
- 136.Hahn D., Hodson E.M., Craig J.C. Interventions for metabolic bone disease in children with chronic kidney disease. Cochrane Database Syst Rev. 2015:CD008327. doi: 10.1002/14651858.CD008327.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kubo Y., Sterling L.R., Parfrey P.S. Assessing the treatment effect in a randomized controlled trial with extensive non-adherence: the EVOLVE trial. Pharm Stat. 2015;14:242–251. doi: 10.1002/pst.1680. [DOI] [PubMed] [Google Scholar]
- 138.Parfey P.S., Drüeke T.B., Block G.A. The effects of cinacalcet in older and younger patients on hemodialysis: the Evaluation of Cinacalcet HCI Therapy to Lower Cardiovascular Events (EVOLVE) trial. Clin J Am Soc Nephrol. 2015;10:791–799. doi: 10.2215/CJN.07730814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Parfrey P.S., Chertow G.M., Block G.A. The clinical course of treated hyperparathyroidism among patients receiving hemodialysis and the effect of cinacalcet: the EVOLVE trial. J Clin Endocrinol Metab. 2013;98:4834–4844. doi: 10.1210/jc.2013-2975. [DOI] [PubMed] [Google Scholar]
- 140.Moe S.M., Abdalla S., Chertow G.M. Effects of cinacalcet on fracture events in patients receiving hemodialysis: the EVOLVE trial. J Am Soc Nephrol. 2015;26:1466–1475. doi: 10.1681/ASN.2014040414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Moe S.M., Chertow G.M., Parfrey P.S. Cinacalcet, fibroblast growth factor-23, and cardiovascular disease in hemodialysis: the evaluation of cinacalcet HCl therapy to lower cardiovascular events (EVOLVE) trial. Circulation. 2015;132:27–39. doi: 10.1161/CIRCULATIONAHA.114.013876. [DOI] [PubMed] [Google Scholar]
- 142.Urena-Torres P., Bridges I., Christiano C. Efficacy of cinacalcet with low-dose vitamin D in incident haemodialysis subjects with secondary hyperparathyroidism. Nephrol Dial Transplant. 2013;28:1241–1254. doi: 10.1093/ndt/gfs568. [DOI] [PubMed] [Google Scholar]
- 143.Raggi P., Chertow G.M., Torres P.U. The ADVANCE study: a randomized study to evaluate the effects of cinacalcet plus low-dose vitamin D on vascular calcification in patients on hemodialysis. Nephrol Dial Transplant. 2011;26:1327–1339. doi: 10.1093/ndt/gfq725. [DOI] [PubMed] [Google Scholar]
- 144.Wetmore J.B., Gurevich K., Sprague S. A randomized trial of cinacalcet versus vitamin D analogs as monotherapy in secondary hyperparathyroidism (PARADIGM) J Clin Am Soc Nephrol. 2015;10:1031–1040. doi: 10.2215/CJN.07050714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Behets G.J., Spasovski G., Sterling L.R. Bone histomorphometry before and after long-term treatment with cinacalcet in dialysis patients with secondary hyperparathyroidism. Kidney Int. 2015;87:846–856. doi: 10.1038/ki.2014.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Block G.A., Bushinsky D.A., Cheng S. Effect of etelcalcetide vs cinacalcet on serum parathyroid hormone in patients receiving hemodialysis with secondary hyperparathyroidism: a randomized clinical trial. JAMA. 2017;317:156–164. doi: 10.1001/jama.2016.19468. [DOI] [PubMed] [Google Scholar]
- 147.Block G.A., Bushinsky D.A., Cunningham J. Effect of etelcalcetide vs placebo on serum parathyroid hormone in patients receiving hemodialysis with secondary hyperparathyroidism: two randomized clinical trials. JAMA. 2017;317:146–155. doi: 10.1001/jama.2016.19456. [DOI] [PubMed] [Google Scholar]
- 148.Nichols K.R., Knoderer C.A., Johnston B. Cinacalcet administration by gastrostomy tube in a child receiving peritoneal dialysis. J Pediatr Pharmacol Ther. 2014;19:202–205. doi: 10.5863/1551-6776-19.3.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Dotis J., Printza N., Ghogha C. Short- and middle-term continuous use of cinacalcet in children on peritoneal dialysis. J Pediatr Endocrinol Metab. 2013;26:39–43. doi: 10.1515/jpem-2012-0214. [DOI] [PubMed] [Google Scholar]
- 150.Platt C., Inward C., McGraw M. Middle-term use of Cinacalcet in paediatric dialysis patients. Pediatr Nephrol. 2010;25:143–148. doi: 10.1007/s00467-009-1294-7. [DOI] [PubMed] [Google Scholar]
- 151.Alharthi A.A., Kamal N.M., Abukhatwah M.W. Cinacalcet in pediatric and adolescent chronic kidney disease: a single-center experience. Medicine (Baltimore) 2015;94:e401. doi: 10.1097/MD.0000000000000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Padhi D., Langman C.B., Fathallah-Shaykh S. An open-label study to evaluate a single-dose of cinacalcet in pediatric dialysis subjects. Pediatr Nephrol. 2012;27:1953–1959. doi: 10.1007/s00467-012-2186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Jadoul M., Albert J.M., Akiba T. Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2006;70:1358–1366. doi: 10.1038/sj.ki.5001754. [DOI] [PubMed] [Google Scholar]
- 154.Vautour L.M., Melton L.J., 3rd, Clarke B.L. Long-term fracture risk following renal transplantation: a population-based study. Osteoporos Int. 2004;15:160–167. doi: 10.1007/s00198-003-1532-y. [DOI] [PubMed] [Google Scholar]
- 155.Evenepoel P. Recovery versus persistence of disordered mineral metabolism in kidney transplant recipients. Semin Nephrol. 2013;33:191–203. doi: 10.1016/j.semnephrol.2012.12.019. [DOI] [PubMed] [Google Scholar]
- 156.Heaf J.G. Bone disease after renal transplantation. Transplantation. 2003;75:315–325. doi: 10.1097/01.TP.0000043926.74349.6D. [DOI] [PubMed] [Google Scholar]
- 157.Iyer S.P., Nikkel L.E., Nishiyama K.K. Kidney transplantation with early corticosteroid withdrawal: paradoxical effects at the central and peripheral skeleton. J Am Soc Nephrol. 2014;25:1331–1341. doi: 10.1681/ASN.2013080851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Naylor K.L., Jamal S.A., Zou G. Fracture incidence in adult kidney transplant recipients. Transplantation. 2016;100:167–175. doi: 10.1097/TP.0000000000000808. [DOI] [PubMed] [Google Scholar]
- 159.Nikkel L.E., Mohan S., Zhang A. Reduced fracture risk with early corticosteroid withdrawal after kidney transplant. Am J Transplant. 2012;12:649–659. doi: 10.1111/j.1600-6143.2011.03872.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sukumaran Nair S., Lenihan C.R., Montez-Rath M.E. Temporal trends in the incidence, treatment and outcomes of hip fracture after first kidney transplantation in the United States. Am J Transplant. 2014;14:943–951. doi: 10.1111/ajt.12652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Akaberi S., Simonsen O., Lindergard B. Can DXA predict fractures in renal transplant patients? Am J Transplant. 2008;8:2647–2651. doi: 10.1111/j.1600-6143.2008.02423.x. [DOI] [PubMed] [Google Scholar]
- 162.Evenepoel P., Cooper K., Holdaas H. A randomized study evaluating cinacalcet to treat hypercalcemia in renal transplant recipients with persistent hyperparathyroidism. Am J Transplant. 2014;14:2545–2555. doi: 10.1111/ajt.12911. [DOI] [PubMed] [Google Scholar]
- 163.Bonani M., Frey D., Brockmann J. Effect of twice-yearly denosumab on prevention of bone mineral density loss in de novo kidney transplant recipients: a randomized controlled trial. Am J Transplant. 2016;16:1882–1891. doi: 10.1111/ajt.13692. [DOI] [PubMed] [Google Scholar]
- 164.Tsertsvadze A., Maglione M., Chou R. Updating comparative effectiveness reviews: current efforts in AHRQ's Effective Health Care Program. J Clin Epidemiol. 2011;64:1208–1215. doi: 10.1016/j.jclinepi.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 165.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions, version 5.1.0. The Cochrane Collaboration; 2011.
- 166.Hayden J.A., van der Windt D.A., Cartwright J.L. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158:280–286. doi: 10.7326/0003-4819-158-4-201302190-00009. [DOI] [PubMed] [Google Scholar]
- 167.Guyatt G.H., Thorlund K., Oxman A.D. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles-continuous outcomes. J Clin Epidemiol. 2013;66:173–183. doi: 10.1016/j.jclinepi.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 168.Guyatt G., Oxman A.D., Akl E.A. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 169.Guyatt G.H., Oxman A.D., Santesso N. GRADE guidelines: 12. Preparing summary of findings tables-binary outcomes. J Clin Epidemiol. 2013;66:158–172. doi: 10.1016/j.jclinepi.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 170.Guyatt G., Oxman A.D., Sultan S. GRADE guidelines: 11. Making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol. 2013;66:151–157. doi: 10.1016/j.jclinepi.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 171.Uhlig K., Macleod A., Craig J. Grading evidence and recommendations for clinical practice guidelines in nephrology. A position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2006;70:2058–2065. doi: 10.1038/sj.ki.5001875. [DOI] [PubMed] [Google Scholar]
- 172.Atkins D., Best D., Briss P.A. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Guyatt G.H., Oxman A.D., Kunz R. Going from evidence to recommendations. BMJ. 2008;336:1049–1051. doi: 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.