Abstract
There has been considerable effort within individual countries to improve the care of patients with kidney disease. There has been no concerted attempt to summarize these efforts, and therefore little is known about structuring health systems to facilitate acute kidney injury and chronic kidney disease (CKD) care and integration with national and international noncommunicable disease strategies. As part of the “Closing the Gaps Initiative,” the International Society of Nephrology will conduct for the first time a survey of the current state of global kidney care covering both acute kidney injury and CKD and present the results in a Global Kidney Health Atlas. Data will be collected via an online questionnaire and targeted at national nephrology societies, policymakers, and consumer organizations. Individual country information will be provided by at least 3 stakeholders. The Global Kidney Health Atlas will provide concise, relevant, and synthesized information on the delivery of care across different health systems to facilitate understanding of performance variations over time and between countries. First, it will provide an overview of existing CKD care policy and context in the health care system. Second, it will provide an overview of how CKD care is organized in individual countries and a description of relevant CKD epidemiology between countries and regions, focusing on elements that are most germane to service delivery and policy development. Finally, synthesis, comparison, and analysis of individual country/regional data will be provided as a platform for recommendations to policymakers, practitioners, and researchers.
Keywords: acute kidney injury, AKI, atlas, chronic kidney disease, CKD, countries, global, health systems, survey, universal health coverage
Chronic kidney disease (CKD) and acute kidney injury (AKI) are both recognized as global public health problems because of associations with adverse health outcomes, high health care costs, and poor quality of life.1, 2, 3, 4 Moreover, CKD is not only common, harmful, and treatable but is also linked to other major noncommunicable chronic diseases (NCDs) such as diabetes, hypertension, and cardiovascular diseases.5, 6 As a result of increasing attention to the costs and consequences of CKD and AKI, there has been considerable effort within individual countries to improve the care of this vulnerable population.7, 8, 9, 10, 11, 12 Anecdotal evidence suggests that there is substantial inter- and intracountry as well as regional variability in the approaches taken and the progress made.13 Because there has been no concerted effort to summarize work and progress to date, little is known about the best way to structure health systems to facilitate CKD and AKI prevention and control or how to integrate these objectives into emerging national and international NCDs management strategies.1, 14, 15
This proposal describes a state-of-the-art knowledge synthesis that will close this knowledge gap and facilitate more coordinated efforts for CKD and AKI prevention and control across the globe.1, 15 It describes the development of a systematic data repository, the Global Kidney Health Atlas (GKHA), under the auspices of the International Society of Nephrology (ISN). The GKHA will summarize the structure, format, and outcomes associated with national, regional, and global efforts to improve kidney care in all world regions. This is more germane with the current momentum to push countries toward universal health care (UHC).16, 17 It is unclear what this would mean for kidney care and the readiness of countries and regions on the specifics of care organization to accomplish UHC for the many patients with kidney diseases. This project will determine the global status of kidney care structures and organization toward achieving UHC and devise policy implications for including CKD in the global NCD agenda. The objectives of the GKHA are as follows:
-
1.
To provide a high-level overview of the current state of kidney care and how it is organized and structured around the world as well as the burden and consequences of CKD and AKI.
-
2.
To conduct a comparative analysis and data synthesis of the collated information across countries and ISN regions to identify key strengths and weaknesses of various systems and explore opportunities for regional networking and collaborations for optimal kidney care around the world.
-
3.
To provide a platform for championing the cause of CKD as a leading NCD and assist in advocacy with major stakeholders (World Health Organization, United Nations, Organization for Economic Cooperation and Development, European Union) to increase the profile of CKD as a public health issue.
-
4.
To provide the foundation for a global CKD and AKI care surveillance network.
Methods
Scope and mandate
We reviewed the mandate provided by the ISN and existing frameworks/initiatives of a similar nature to develop a blueprint/plan of work for the GKHA. The documents reviewed included AKI “0 by 25,” World Heart Federation “25 by 25,” International Diabetes Federation Global Diabetes Atlas, the WHO Global Atlas on Cardiovascular Disease Prevention and Control as well as several United Nations Policy Documents on strategies and policy for NCDs.18, 19, 20, 21, 22, 23, 24, 25, 26 The work will be carried out across all countries (193 states recognized by the United Nations with a specific focus on 130 countries with ISN-affiliated societies) through the 10 ISN Regional Boards, to be led by a steering committee and work group within the stipulated timeline (Appendix 1):
-
1.
Africa
-
2.
Eastern and Central Europe
-
3.
Latin America and the Caribbean
-
4.
Middle East
-
5.
North America and the Caribbean
-
6.
North and East Asia
-
7.
Oceania and South East Asia
-
8.
National Independent States and Russia
-
9.
South Asia
-
10.
Western Europe
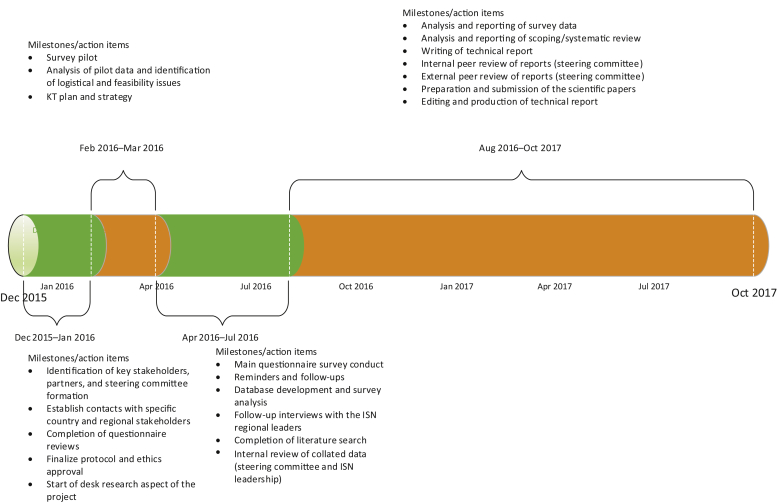
Appendix 1.
Project timeline. ISN, International Society of Nephrology.
Identification and use of regional and country-specific project leaders
We will utilize our international contacts, collaborators, and ISN leadership and regional boards to facilitate identification and engagement of project leaders at regional and country levels, which will include individual country nephrology association leadership and opinion leaders across regions and countries.
Roles for regional project leadership
-
a.
To organize and follow up on responses for all countries within the region
-
b.
To serve as a link between the steering committee, ISN, and regional stakeholders
-
c.
To serve as a resource for additional data sources and contacts for surveys
-
d.
To identify or serve as an opinion leader on the project for the region
-
e.
To identify or serve as a resource person to vet and review regional data
Roles for individual country project leadership
-
a.
To organize and follow up on responses within the country
-
b.
To serve as a link between the steering committee, ISN, and country stakeholders
-
c.
To serve as a resource for additional data sources and contacts for surveys
-
d.
To identify or serve as a national opinion leader
-
e.
To identify or serve as a resource person to vet and review national data
Ethical approval
The project is approved by the University of Alberta Research Ethics Committee (Protocol number: PRO00063121).
Project Conduct/Approach
The project will involve 2 major elements: (A), desk research and (B), a survey including a mix of quantitative and qualitative methods.
A. Desk research
The desk research includes a review of published scientific literature, government reports, and other relevant data sources on the various aspects of CKD epidemiology and health systems characteristics using the WHO UHC domains (service delivery, health work force, information systems, medicines and medical products, financing, and leadership) (Table 1, Table 2, Table 3). Although the published literature is important to consider, much of the available evidence is expected to be in the gray literature, including websites and reports with limited circulation. We will engage the various country and regional project leaders to identify these sources and will conduct a detailed gray literature search designed by an expert research librarian. The specific research elements in this section are (i) scoping literature review of national health systems characteristics based on the UHC domains focusing on important elements relevant to CKD care organization and delivery and (ii) systematic review of relevant CKD epidemiology data (burden and outcomes) across countries and regions.
Table 1.
A summary of the project approach: methodology and data sources
| Objective | Methods/approach | Coverage/elements | Primary data sources | Secondary data sources |
|---|---|---|---|---|
| To obtain a snapshot of individual country and regional health systems characteristics and specific elements relevant to CKD care | Scoping review Survey |
WHO UHC domainsa | Survey data Interviews |
WHO Global Observatory UN, World Bank, and OECD reports on NCDs Published data/reports |
| To obtain data on relevant CKD epidemiology (risk factors, burden, and outcomes) across countries and regions | Systematic reviews Scoping review Survey |
Estimates of CKD prevalence Estimates for RRT Mortality and disability attributable to CKD CKD risk factors |
Survey data Interviews |
Systematic reviews and consortia publications GBD reports World Health Report World Health Indicators Reports Global NCD Repository IDF Diabetes Atlas WHF World Cardiovascular Disease Atlas Published reports Renal registries |
CKD, chronic kidney disease; GBD, global burden of disease; IDF, International Diabetes Federation; NCDs, noncommunicable diseases; OECD, Organization for Economic Cooperation and Development; RRT, renal replacement therapy; UHC, Universal Health Coverage; UN, United Nations; WHF, World Heart Federation
WHO UHC domains (service delivery, health work force, information systems, medicines and medical products, financing, and leadership).
Table 2.
General health system characteristics, WHO UHC domains,a and relevant data sources
| Building blocks | Indicators/metrics | Data sources | Essential elements |
|---|---|---|---|
| Country profile | Total population (millions) Annual population growth rate (%) Literacy rate among adults 15 years of age and older (%) Gross national income per capita (PPP int. $) Population living on <$1 (PPP int. $) per day (%) Cellular phone subscribers (per 100 population) |
Literature reviews | |
| Health service delivery | Description of health care system: public/private health insurance funded by national taxation/income contributions covering all/a proportion of the population. Recording of ratio of public/private MDs, renal care centers and/or HD centers | Literature reviews Surveys Interviews |
Comprehensiveness Accessibility Coverage Quality Coordination Efficiency Accountability |
| Health work force | Density of physicians (per 10,000 population) Density of nursing and midwifery personnel (per 10,000 population) Density of pharmaceutical personnel (per 10,000 population) |
Literature reviews Surveys Interviews WHO Global Observatory |
Reach and distribution Accessibility |
| Health information systems | Literature reviews Surveys Interviews |
Reach Scope |
|
| Essential medicines and technologies | Hospitals (per 100,000 population) Computed tomography units (per million population) Median availability of selected generic medicines in public and private sectors (%) Median consumer price ratio of selected generic medicines in public and private sectors |
Literature reviews Surveys Interviews WHO Global Observatory |
|
| Health financing | Total expenditure on health as a percentage of GDP General government expenditure on health as a percentage of total expenditure on health Private expenditure on health as a percentage of total expenditure on health General government expenditure on health as a percentage of total government expenditure Out-of-pocket expenditure as a percentage of private expenditure on health Private prepaid plans as a percentage of private expenditure on health |
Literature reviews WHO Global Observatory Database |
|
| Leadership and governance (national policies and frameworks) | National chronic/noncommunicable disease policy, overarching disease policy targeting long-term conditions including CVD, diabetes, cancer, CKD, etc. (where it exists). | Literature reviews Surveys Interviews WHO Global Observatory WHO NCD strategy |
CKD, chronic kidney disease; CVD, cardiovascular disease; GDP, gross domestic product; HD, hemodialysis; PPP, purchasing power parity; UHC, universal health coverage, NCD, noncommunicable disease; OECD, Organization for Economic Cooperation and Development.
WHO UHC domains (service delivery, health work force, information systems, medicines and medical products, financing, and leadership).
Table 3.
Kidney care–specific elements based on WHO UHC domainsa and relevant data sources
| Building blocks | Indicators/metrics | Data sources | Essential elements |
|---|---|---|---|
| Health service delivery | Number of health facilities for general CKD care RRT services (e.g., number of health facilities offering HD services per country) Public and private Nondialysis CKD care structure RRT care structure |
Literature reviews Surveys Interviews |
Accessibility of dialysis and kidney transplant units to all within the countries Access to medications Reimbursement of treatment and care Kidney transplant wait list Access to psychosocial counseling and support Existence of patient organizations in each country to facilitate advocacy |
| Health work force | No. of nephrologists (per million population) No. of general physicians (per million population) No. of community health workers (per million population) No. of nurses (per million population) Regional distribution Nephrology trainees/graduates per year Availability of MDT |
Literature reviews Surveys Interviews WHO Global Observatory |
Professionals (GPs, nephrologists, diabetologists, endocrinologists, cardiologists, other related disciplines): total and as a ratio to whole population/ or dialysis population Financial resources, remuneration and incentives (including those for GPs/specialists to identify and manage CKD patients) Presence of other credentialed health care providers (e.g., nephrology nurses, dietitians) |
| Health information systems | CKD (nondialysis) registry RRT registry |
Literature reviews Surveys Interviews |
Reach Scope |
| Essential medicines and technologies | ACEIs/ARBs Statins Aspirin Other BP medications Anemia meds (Epo/iron) CKD-MBD (calcium binders, renagel, cinacalcet) Specific (GN and transplant) Dialysis availability, access, and coverage Transplant availability, access, and coverage |
Literature reviews Surveys Interviews WHO Global Observatory (for some essential medicines) |
|
| Health financing | Total expenditure on health for CKD Public + private contributions Out-of-pocket payments for essential medicines Out-of-pocket payments for nondialysis CKD care Out-of-pocket payments for dialysis Out-of-pocket payments for transplant |
Literature reviews Surveys Interviews WHO Global Observatory |
|
| Leadership and governance (national policies and frameworks) |
Guidelines/frameworks on CKD care Advocacy efforts and initiatives Early detection and prevention programs eGFR reporting |
Literature reviews Surveys Interviews WHO Global Observatory WHO NCD Strategy |
ACEIs/ARBs, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers; BP, blood pressure; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; Epo, erythropoietin; GN, glomerulonephritis; GPs, general practitioners; HD, hemodialysis; MDT, multidisciplinary team; MBD; mineral bone disorder; NCD, noncommunicable disease; RRT, renal replacement therapy; UHC, universal health care.
WHO UHC domains (service delivery, health work force, information systems, medicines and medical products, financing, and leadership).
Scoping review of health systems’ characteristics based on UHC domains and elements specific to CKD
The steps in data collation are as follows:
-
i.
The review will first cover CKD risk factors (biological, behavioral, sociodemographic) available from relevant sources including the WHO Observatory, Organization for Economic Cooperation and Development, World Bank, and related international and regional organizations.
-
ii.
We will utilize data from recent Global Burden of Disease (GBD) study work, and the WHO Global Health Repository to highlight estimates for mortality and disability for CKD.27, 28, 29
-
iii.
We will search published and unpublished documents from international organizations/bodies (e.g., Organization for Economic Cooperation and Development, WHO, UN, Commonwealth Fund, World Bank, European Union and its affiliates) and reports published by national governments (and occasionally regional governments within countries) on the organization and delivery of CKD care.
-
iv.
Additional literature will be identified based on guidance from key stakeholders (opinion leaders and national nephrology society/ISN leaders). We will consult national nephrology societies and ISN regional boards to elucidate alternative data sources relevant to their own countries and regions.
-
v.
Data will be stratified and extracted by country/region into standard data extraction files, with each data source identified as regional, national, and subnational (e.g., within-country regions, provinces, states, counties) considering potential bias and uncertainties in data sources that were not representative of their regional or national populations.
-
vi.
We will utilize various sources and a comprehensive search strategy developed in conjunction with an expert librarian.
A systematic review of relevant CKD epidemiology data (burden and outcomes) across countries and regions
For this aspect of the project, we will leverage the methodology applied by the International Diabetes Federation to generate the Diabetes Atlas.22 Briefly, the population-based data on CKD burden will be obtained from a systematic literature search of original publications and existing reviews on the CKD burden across the world.30, 31, 32 We will search PubMed, Google Scholar, CINAHL, Embase, Cochrane Database of Systematic Reviews, and WHO Global InfoBase to identify all original publications reporting the prevalence of CKD in the adult general population. Because the Kidney Disease Outcomes Quality Initiative published a guideline on CKD definitions in 2002, we will explore articles published from January 1, 2003 to December 31, 2016. We will consider literature published in English and other languages that examined CKD and/or albuminuria in a community setting. If multiple studies are identified that used the same population or data source, the first original publication and/or the most recent (as appropriate) will be selected for review. Studies will be included if they were peer-reviewed and meet the following criteria:
-
1.
Report a measure of population-based prevalence for CKD and/or albuminuria in the general population.
-
2.
Enrolled adults aged 18 years of age and older.
-
3.
Recruited subjects from a community-based population sample.
-
4.
Present detailed methodology and results.
Regional and country nephrology society leaders will also be asked to identify additional data sources on gray literature from surveys and/or prevention programs not yet in the public domain. The literature search will be performed by 2 investigators, and any study that is judged relevant based on its title will be retrieved in abstract form and, if relevant, in full-text form. Any doubt about eligibility will be resolved by discussion within the team.
Study quality and risk of bias assessment
Each study will be assessed for risk of bias and quality based on standard methods and by application of a scoring system using a well-validated framework.21, 33 This would allow for a comparison of different study parameters (Table 4) using a system of weights to derive a composite score for quality. The composite score will be used to select studies based on a predetermined cutoff derived from a distribution curve of the score cluster. As in the International Diabetes Federation methodology framework, studies that scored above an upper threshold (0.5) will be selected and those that scored below a lower threshold (0.3) excluded.21 Studies scoring between 0.3 and 0.5 will be considered for selection if no studies scoring >0.5 are available from the same country. In countries where >1 study is available, the prevalence of CKD will be calculated using a weighted average considering the underlying study scores for that country and/or using a study with the highest quality parameters. If there is no high-quality study for a given country, results from a “data region” will be used as a proxy.21 A data region represents countries in the same geographic area (ISN region) and/or economic status (on the basis of the World Bank classification) as well as the same predominant ethnic group.21, 34
Table 4.
Study characteristics using Analytic Hierarchy Process Framework
| Item | Variable definition |
|---|---|
| Year of publication | Based on year of NKF-KDOQI CKD definition and classification
|
| CKD defining criteria (KDIGO convention or ICD codes) | ICD codes diagnosis NKF/KDQI convention KDIGO convention (2012 onward) |
| Setting/sampling frame | Single community Admin data/hospital-based records Regional/provincial National Across continent/world region Special populations (e.g., natives, SES, racial) |
| Sample size (N) | |
| Sex distribution | |
| Age distribution | |
| Risk factor/etiology profiling Prevalence distribution by subgroups:
|
|
| Study design | Cross-sectional Cohort Registry/surveillance system (e.g., UK QoF) Secondary modeled data (systematic reviews and meta-analysis, CKD consortia reports) |
| Data source | Published literature Published government reports National/regional/community-based surveys or screening programs Data provided by national/regional leaders |
| Study era | Year of assessment of CKD prevalence |
CKD, chronic kidney disease; ICD, International Classification of Diseases; NKF, National Kidney Foundation; KDIGO, Kidney Disease Improving Global Outcomes; KDOQI, Kidney Disease Outcomes Quality Initiative; QoF, quality and outcomes framework; SES, socioeconomic status.
Data extraction and analysis
Demographic information by age, sex, diabetes, hypertension, obesity status, and race/ethnicity (if applicable) will be extracted. The representativeness of the study population will be tested by comparing their age and sex profiles with the distribution of each country’s population as reported in the WHO Standard Population Metrics. The prevalence of CKD stages 1 to 5 with 95% confidence interval will be presented as unadjusted rates and weighted averages for population rates using the individual country population data. For each country/region, age-sex standardized prevalence will be calculated and compared with expected standardized prevalence estimates using the WHO Standard Population framework.
Deriving estimates of renal replacement therapy
We will obtain estimates of the population burden of renal replacement therapy (RRT) (dialysis or transplant) through identification of relevant data from regional and national renal registries (United States Renal Data System [USRDS]; European Renal Association [ERA]-EDTA Registry; UK Renal Registry [UKRR]; Canadian Organ Replacement Registry [ORR]; Australian and New Zealand Renal Registry [ANZDATA]; Latin American Dialysis and Transplant Registry; the Hong Kong Renal Registry) and from population-based surveys of countries with no registries as well as from estimates provided by the survey participants and recently published work on global RRT estimates (1990–2010) from GBD.29
Mortality and disability attributable to CKD
We will leverage the GBD reports to extract estimates on the CKD-attributable mortality, Years of Life Lost from Premature Death, Years Lived with Disability, Disability-Adjusted Life-Years due to CKD, and ranking in relation to other NCDs.27, 29 The GBD 2010 reports provide important information based on data from 187 countries for the period 1990 through 2010 on the burden of disease for 1990 and estimates for 2005, 2010, and 2015, with meaningful comparisons of trends.
CKD risk factors
The key estimates of risk data will be the prevalence of diabetes, impaired fasting blood glucose, increased blood pressure, obesity, alcohol per capita consumption, and smoking burden.35 These will be extracted based on information provided in key reports including the WHO World Health Report, World Health Indicators and Global NCD Repository, as well the International Diabetes Federation Diabetes Atlas. Global atlas on cardiovascular disease prevention and control.
Economic burden of CKD
The measurement of the economic consequences of CKD is complicated as this involves several factors that include cost consequences for individuals and families, as well as costs to the health care system.36, 37 The costs of care are based on published reports that cover advanced stages of CKD and RRT, and thus the most expensive cases. We will capture reported costs analyses from developed nations, which are usually rigorous, and will attempt to obtain estimates for all countries and regions using our survey instruments that leverage the standard metrics defined by the USRDS:
-
•
Per-person per-year total costs of CKD care (non-RRT)
-
•
Per-person per-year total costs of CKD care (dialysis)
-
•
Per-person per-year total costs of CKD care (transplant)
B. GKHA Survey
The second component of the project will comprise a survey to be delivered electronically via the SurveyMonkey portal (http://www.surveymonkey.com). These hosted survey tools allow the use of a customized and secure e-mail list to reach an audience, a collector to gather all responses, and an avenue to export those responses to various analytical software programs, such as the SPSS, Stata, and SAS. An additional advantage of this platform is the ability to track and monitor responses, and issue reminders as appropriate. We leveraged the framework that was applied to derive information about national capacities and responses to NCD prevention and control across 193 WHO member states in the design of our own questionnaires.38
The main questionnaire was designed in 2 sections that addressed the core areas of country and regional capacity for kidney care delivery:
-
1.The first section comprised 6 modules assessing country and regional profile for readiness, capacity, and response to CKD and AKI premised on the 6 health system building blocks39:
-
•Health Finance: questions evaluating funding mechanisms for AKI and CKD care (including RRT)
-
•Essential Medications and Technology Access: questions on the availability and access to medicines for CKD and RRT technologies (dialysis and transplantation)
-
•Service Delivery and Safety: questions assessing infrastructures (availability, adequacy, and reach) for AKI and CKD care
-
•Health Workforce: questions on the availability (and number) of nephrologists, capacity for nephrology training, and adequacy of other work force essential for AKI and CKD care delivery
-
•Health Information System and Statistics: questions on availability of registries and/or other surveillance systems for AKI and CKD care (including RRT)
-
•Governance and leadership: strategies and policy frameworks (including care guidelines, position papers, service frameworks, and advocacy initiatives)
-
•
-
2.The second section contained questions that assessed response of the nephrology community:
-
•Capacity for research and development
-
•
The questionnaire was accompanied by a detailed information sheet about the GKHA, detailed instructions for completion, and a glossary defining key terms used in the survey (Supplementary Appendixes S1 and S2).
Study population
The audience will comprise the various stakeholders identified by the country and regional leaders through the ISN including at least 3 key representatives per country sourced from:
-
●
National nephrology society leadership
-
●
Policymakers, including those involved directly with the organization of CKD care (renal policymakers) and those with a more general remit (non-renal)
-
●
Patients
Patient engagement and partnership
We recognize the high priority accorded patient engagement in policy-relevant research and health system improvement across the globe. This is particularly important for a project of this nature and scope. We plan to engage individual patients, patient groups, and organizations across the broad spectrum of CKD (nondialysis-dependent CKD patients, dialysis patients, and kidney transplant patients). This is to ensure that patient views and perspectives are taken into consideration and remain the focus of this project. A separate questionnaire will be used to capture patients’ views and perceptions on the broader objectives of GKHA, with a focus on barriers to accessing high-quality care across the CKD spectrum (from early CKD to RRT) (Supplementary Appendix S3).
Survey administration
We will administer standardized and pilot-tested survey questionnaires designed to gather primary data required to complete the GKHA, particularly concerning policy and organization of care.40, 41, 42, 43, 44 Respondents will be asked specifically about important within-country heterogeneity in these areas, which will be flagged for further study and addressed in the current survey where possible. Survey respondents will also be asked to identify other potential key respondents, increasing the likelihood that relevant information is widely captured. We will first pilot the project across the membership of the 10 ISN regional boards to identify any logistical and feasibility issues; test the face and construct validity of the survey questionnaire; and finalize the format used to collate and present the data collected from each country and region. In parallel with conducting the pilot, we will gather the information needed to conduct the work across countries and regions, including identifying key stakeholders, data sources, and potential partners. This will ensure that (once the pilot is completed), we can immediately scale up our efforts at data collection in multiple countries and regions using methods that are appropriate to our goals. This will minimize delays that might result from applying unproven methods to multiple countries at once. We will focus our work based on the detailed content and scope of the GKHA provided by the ISN leadership and reviewed by the steering committee.
Data handling, analysis, and reporting
To facilitate data collation, responses to the French and Spanish surveys will be first converted to English by certified translators. Data from all individual questionnaires will subsequently be automatically extracted and cleaned using Microsoft Excel and merged into a single file to create the global database. This will be housed in a secured centralized computer system with automated backups. Any major inconsistencies that remain following the reviews will be systematically addressed by follow-up inquiries with the stakeholders involved with the survey. Further validation will be carried out at country and regional levels by triangulation of the findings with published literature and gray sources of information (government reports and other sources provided by the survey respondents).
The framework developed by the WHO (Assessing National Capacity for the Prevention and Control of NCDs) will be leveraged in the approach to the statistical analysis of the collated data.45 The analysis will be conducted using STATA 13 software (StataCorp, College Station, TX). The unit of analysis is responding country, and results will be stratified by ISN regions and World Bank country classification, 2014. Responses will be summarized based on the key questionnaire domains using a descriptive statistical approach and reported as counts and percentages or medians and interquartile ranges, as appropriate. Nonquantitative data (text response items of the questionnaire) will be thematically analyzed using a standard approach.46 The results will be reported per the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) statement.47
Data quality and consistency
We will liaise with key individuals, ISN regional and country leaders to ensure that identified data are consistent with their understanding and are of high quality. Each regional board will review the yield from the literature and gray literature review to clarify any preexisting ambiguity or inconsistencies. Any major inconsistencies that remain following the reviews will be systematically addressed by brief follow-up inquiries; areas where ambiguity remains will be specifically mentioned in our report.
Conclusions
It is imperative to devise strategies and policies toward an improved understanding of AKI, CKD, and optimal care delivery. This requires the development of baseline data on the current global status of kidney care structures and delivery systems. This represents the first effort by the ISN to develop a GKHA to assess national capacity, readiness, and response for optimal kidney care around the world to be conducted as part of the ISN “Closing the Gaps Initiative.” The survey will provide an overview of the current capacity for kidney care (comprising both AKI and CKD) and an assessment of individual country and regional readiness to enhance this capacity. The findings will be applied to engage relevant stakeholders across countries and regions to advocate for improved access to and quality of kidney care. The data have appreciable policy implications because they provide a baseline platform to hold countries to account by measuring country and region progress over time.
Disclosure
The study was funded by the International Society of Nephrology (ISN). The ISN holds all copyrights on the data obtained through this study. Analysis and interpretation of data, writing of the report, and the decision to submit the manuscripts are the responsibility of the GKHA study team. DWJ declared receiving consulting fees from AstraZeneca; lecture fees from Baxter Healthcare, Fresenius, and Medical Care; and support from Baxter Extramural and CEC grants. DH declared receiving lecture fees from Roche Myanmar and Otsuka. All the other authors declared no competing interests.
Publication of this article was supported by the International Society of Nephrology.
Acknowledgments
We thank Sandrine Damster, Research Project Manager at the International Society of Nephrology (ISN), and Alberta Kidney Disease Network (AKDN) staff (Ghenette Houston, Sue Szigety, and Sophanny Tiv) for their support with the organization and conduct of the survey and project management. We thank the ISN staff (Louise Fox and Luca Segantini) for their support. We thank the Executive Committee of the ISN, the ISN regional leadership as well as the leaders of the ISN Affiliate Societies at regional and country levels for their support toward the success of this initiative, particularly with identification of survey respondents and data acquisition.
Footnotes
Appendix S1. Main survey information sheet.
Appendix S2. Patient survey information sheet.
Appendix S3. Patient survey questionnaire.
Supplementary material is linked to the online version of the paper at http://www.kisupplements.org/.
Appendix
Supplementary Material
Main survey information sheet.
Patient survey information sheet.
Patient survey questionnaire.
References
- 1.Couser W.G., Remuzzi G., Mendis S., Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011;80:1258–1270. doi: 10.1038/ki.2011.368. [DOI] [PubMed] [Google Scholar]
- 2.James M.T., Hemmelgarn B.R., Tonelli M. Early recognition and prevention of chronic kidney disease. Lancet. 2010;375:1296–1309. doi: 10.1016/S0140-6736(09)62004-3. [DOI] [PubMed] [Google Scholar]
- 3.Meguid El, Nahas A., Bello A.K. Chronic kidney disease: the global challenge. Lancet. 2005;365:331–340. doi: 10.1016/S0140-6736(05)17789-7. [DOI] [PubMed] [Google Scholar]
- 4.Levey A.S., de Jong P.E., Coresh J. The definition, classification, and prognosis of chronic kidney disease: a KDIGO Controversies Conference report. Kidney Int. 2011;80:17–28. doi: 10.1038/ki.2010.483. [DOI] [PubMed] [Google Scholar]
- 5.Levey A.S., Eckardt K.U., Tsukamoto Y. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2005;67:2089–2100. doi: 10.1111/j.1523-1755.2005.00365.x. [DOI] [PubMed] [Google Scholar]
- 6.Levey A.S., Coresh J. Chronic kidney disease. Lancet. 2012;379:165–180. doi: 10.1016/S0140-6736(11)60178-5. [DOI] [PubMed] [Google Scholar]
- 7.Levin A., Steven S., Selina A. Canadian chronic kidney disease clinics: a national survey of structure, function and models of care. Can J Kidney Health Dis. 2014;1:29. doi: 10.1186/s40697-014-0029-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levin A., Stevens P.E. Summary of KDIGO 2012 CKD Guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85:49–61. doi: 10.1038/ki.2013.444. [DOI] [PubMed] [Google Scholar]
- 9.Ahlawat R., Tiwari P., D'Cruz S., Singhal R. Prevalence Of Chronic Kidney Disease In India: A Systematic Review And Meta-Analysis Of Observational Studies. Value Health. 2015;18:A509. [Google Scholar]
- 10.Anothaisintawee T., Rattanasiri S., Ingsathit A., Attia J., Thakkinstian A. Prevalence of chronic kidney disease: a systematic review and meta-analysis. Clin Nephrol. 2009;71:244–254. doi: 10.5414/cnp71244. [DOI] [PubMed] [Google Scholar]
- 11.Coca S.G., Singanamala S., Parikh C.R. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81:442–448. doi: 10.1038/ki.2011.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lopez-Vargas P.A., Tong A., Sureshkumar P. Prevention, detection and management of early chronic kidney disease: a systematic review of clinical practice guidelines. Nephrology (Carlton) 2013;18:592–604. doi: 10.1111/nep.12119. [DOI] [PubMed] [Google Scholar]
- 13.Johnson D.W., Atai E., Chan M. KHA-CARI guideline: Early chronic kidney disease: detection, prevention and management. Nephrology (Carlton) 2013;18:340–350. doi: 10.1111/nep.12052. [DOI] [PubMed] [Google Scholar]
- 14.Rettig R.A., Norris K., Nissenson A.R. Chronic kidney disease in the United States: a public policy imperative. Clin J Am Soc Nephrol. 2008;3:1902–1910. doi: 10.2215/CJN.02330508. [DOI] [PubMed] [Google Scholar]
- 15.Feehally J. Chronic kidney disease: Health burden of kidney disease recognized by UN. Nat Rev Nephrol. 2012;8:12–13. doi: 10.1038/nrneph.2011.191. [DOI] [PubMed] [Google Scholar]
- 16.McCarthy M. Reducing inequality is crucial to implementing universal health coverage, says WHO report. BMJ. 2013;347:f5902. doi: 10.1136/bmj.f5902. [DOI] [PubMed] [Google Scholar]
- 17.Groves T. Development of health systems and universal coverage should be evidence based, says WHO. BMJ. 2012;345:e7530. doi: 10.1136/bmj.e7530. [DOI] [PubMed] [Google Scholar]
- 18.Mehta R.L., Cerda J., Burdmann E.A. International Society of Nephrology's 0by25 initiative for acute kidney injury (zero preventable deaths by 2025): a human rights case for nephrology. Lancet. 2015;385:2616–2643. doi: 10.1016/S0140-6736(15)60126-X. [DOI] [PubMed] [Google Scholar]
- 19.Huffman M.D., Perel P., Beller G.A. World Heart Federation Emerging Leaders Program: An Innovative Capacity Building Program to Facilitate the 25 x 25 Goal. Glob Heart. 2015;10:229–233. doi: 10.1016/j.gheart.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 20.Moran A.E., Roth G.A., Narula J., Mensah G.A. 1990-2010 global cardiovascular disease atlas. Glob Heart. 2014;9:3–16. doi: 10.1016/j.gheart.2014.03.1220. [DOI] [PubMed] [Google Scholar]
- 21.Linnenkamp U., Guariguata L., Beagley J. The IDF Diabetes Atlas methodology for estimating global prevalence of hyperglycaemia in pregnancy. Diabetes Res Clin Pract. 2014;103:186–196. doi: 10.1016/j.diabres.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Guariguata L., Whiting D., Weil C., Unwin N. The International Diabetes Federation diabetes atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res Clin Pract. 2011;94:322–332. doi: 10.1016/j.diabres.2011.10.040. [DOI] [PubMed] [Google Scholar]
- 23.Thomas B., Wulf S., Bikbov B. Maintenance Dialysis throughout the World in Years 1990 and 2010. J Am Soc Nephrol. 2015;26:2621–2633. doi: 10.1681/ASN.2014101017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Lancet Diabetes Endocrinology Monitoring progress in NCDs: key to accountability. Lancet Diabetes Endocrinol. 2015;3:159. doi: 10.1016/S2213-8587(15)00005-4. [DOI] [PubMed] [Google Scholar]
- 25.Bello A.K., Levin A., Manns B.J. Effective CKD care in European countries: challenges and opportunities for health policy. Am J Kidney Dis. 2015;65:15–25. doi: 10.1053/j.ajkd.2014.07.033. [DOI] [PubMed] [Google Scholar]
- 26.Pearce N., Ebrahim S., McKee M. The road to 25x25: how can the five-target strategy reach its goal? Lancet Glob Health. 2014;2:e126–e128. doi: 10.1016/S2214-109X(14)70015-4. [DOI] [PubMed] [Google Scholar]
- 27.GBD Risk Collaborators. Forouzanfar M.H., Alexander L., Anderson H.R. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murray C.J., Barber R.M., Foreman K.J. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990-2013: quantifying the epidemiological transition. Lancet. 2015;386:2145–2191. doi: 10.1016/S0140-6736(15)61340-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Noubiap J.J., Naidoo J., Kengne A.P. Diabetic nephropathy in Africa: a systematic review. World J Diabetes. 2015;6:759–773. doi: 10.4239/wjd.v6.i5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stanifer J.W., Jing B., Tolan S. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2014;2:e174–e181. doi: 10.1016/S2214-109X(14)70002-6. [DOI] [PubMed] [Google Scholar]
- 32.Liyanage T., Ninomiya T., Jha V. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 33.Whiting D.R., Guariguata L., Weil C., Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 34.Kearney P.M., Whelton M., Reynolds K. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 35.Bruck K., Stel V.S., Fraser S. Translational research in nephrology: chronic kidney disease prevention and public health. Clin Kidney J. 2015;8:647–655. doi: 10.1093/ckj/sfv082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Honeycutt A.A., Segel J.E., Zhuo X. Medical costs of CKD in the Medicare population. J Am Soc Nephrol. 2013;24:1478–1483. doi: 10.1681/ASN.2012040392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trivedi H. Cost implications of caring for chronic kidney disease: are interventions cost-effective? Adv Chronic Kidney Dis. 2010;17:265–270. doi: 10.1053/j.ackd.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 38.Wagenaar B.H., Sherr K., Fernandes Q., Wagenaar A.C. Using routine health information systems for well-designed health evaluations in low- and middle-income countries. Health Policy Plan. 2016;31:129–135. doi: 10.1093/heapol/czv029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Countdown Working Group on Health Policy and Health Systems. Cavagnero E., Daelmans B., Gupta N. Assessment of the health system and policy environment as a critical complement to tracking intervention coverage for maternal, newborn, and child health. Lancet. 2008;371:1284–1293. doi: 10.1016/S0140-6736(08)60563-2. [DOI] [PubMed] [Google Scholar]
- 40.Newman L. Telephone survey methods: implications of the increasing mobile-only population for public health research. Aust N Z J Public Health. 2011;35:491–492. doi: 10.1111/j.1753-6405.2011.00763.x. [DOI] [PubMed] [Google Scholar]
- 41.Calder J. Survey research methods. Med Educ. 1998;32:638–652. doi: 10.1046/j.1365-2923.1998.00227.x. [DOI] [PubMed] [Google Scholar]
- 42.Eaden J., Mayberry M.K., Mayberry J.F. Questionnaires: the use and abuse of social survey methods in medical research. Postgrad Med J. 1999;75:397–400. doi: 10.1136/pgmj.75.885.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Etchegaray J.M., Fischer W.G. Understanding evidence-based research methods: reliability and validity considerations in survey research. HERD. 2010;4:131–135. doi: 10.1177/193758671000400109. [DOI] [PubMed] [Google Scholar]
- 44.Molitor F., Kravitz R.L., To Y.Y., Fink A. Methods in survey research: evidence for the reliability of group administration vs personal interviews. Am J Public Health. 2001;91:826–827. doi: 10.2105/ajph.91.5.826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leowski J., Krishnan A. Capacity to control noncommunicable diseases in the countries of South-East Asia. Health Policy. 2009;92:43–48. doi: 10.1016/j.healthpol.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 46.Chapman A.L., Hadfield M., Chapman C.J. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb. 2015;45:201–205. doi: 10.4997/JRCPE.2015.305. [DOI] [PubMed] [Google Scholar]
- 47.Stevens G.A., Alkema L., Black R.E. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet. 2016;388:e19–e23. doi: 10.1016/S0140-6736(16)30388-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Main survey information sheet.
Patient survey information sheet.
Patient survey questionnaire.