Abstract
OBJECTIVE
There are variable reports of risk of concordance for progression to islet autoantibodies and type 1 diabetes in identical twins after one twin is diagnosed. We examined development of positive autoantibodies and type 1 diabetes and the effects of genetic factors and common environment on autoantibody positivity in identical twins, nonidentical twins, and full siblings.
RESEARCH DESIGN AND METHODS
Subjects from the TrialNet Pathway to Prevention Study (N = 48,026) were screened from 2004 to 2015 for islet autoantibodies (GAD antibody [GADA], insulinoma-associated antigen 2 [IA-2A], and autoantibodies against insulin [IAA]). Of these subjects, 17,226 (157 identical twins, 283 nonidentical twins, and 16,786 full siblings) were followed for autoantibody positivity or type 1 diabetes for a median of 2.1 years.
RESULTS
At screening, identical twins were more likely to have positive GADA, IA-2A, and IAA than nonidentical twins or full siblings (all P < 0.0001). Younger age, male sex, and genetic factors were significant factors for expression of IA-2A, IAA, one or more positive autoantibodies, and two or more positive autoantibodies (all P ≤ 0.03). Initially autoantibody-positive identical twins had a 69% risk of diabetes by 3 years compared with 1.5% for initially autoantibody-negative identical twins. In nonidentical twins, type 1 diabetes risk by 3 years was 72% for initially multiple autoantibody–positive, 13% for single autoantibody–positive, and 0% for initially autoantibody-negative nonidentical twins. Full siblings had a 3-year type 1 diabetes risk of 47% for multiple autoantibody–positive, 12% for single autoantibody–positive, and 0.5% for initially autoantibody-negative subjects.
CONCLUSIONS
Risk of type 1 diabetes at 3 years is high for initially multiple and single autoantibody–positive identical twins and multiple autoantibody–positive nonidentical twins. Genetic predisposition, age, and male sex are significant risk factors for development of positive autoantibodies in twins.
Introduction
Type 1 diabetes is preceded by the presence of preclinical, persistent islet autoantibodies (1). Autoantibodies against insulin (IAA) (2), GAD (GADA), insulinoma-associated antigen 2 (IA-2A) (3), and/or zinc transporter 8 (ZnT8A) (4) are typically present prior to development of symptomatic hyperglycemia and progression to clinical disease. These autoantibodies may develop many years before onset of type 1 diabetes, and increasing autoantibody number and titers have been associated with increased risk of progression to disease (5–7).
Identical twins have an increased risk of progression of islet autoimmunity and type 1 diabetes after one twin is diagnosed, although reported rates have been highly variable (30–70%) (8–11). This risk is increased if the proband twin develops diabetes at a young age (12). Concordance rates for type 1 diabetes in monozygotic twins with long-term follow-up is >50% (13). Risk for development of islet autoimmunity and type 1 diabetes for nonidentical twins is thought to be similar to nontwin siblings (risk of 6–10% for diabetes) (14). Full siblings who inherit both high-risk HLA (HLA DQA1*05:01 DR3/4*0302) haplotypes identical to their proband sibling with type 1 diabetes have a much higher risk for development of diabetes than those who share only one or zero haplotypes (55% vs. 5% by 12 years of age, respectively; P = 0.03) (15). Despite sharing both HLA haplotypes with their proband, siblings without the HLA DQA1*05:01 DR3/4*0302 genotype had only a 25% risk for type 1 diabetes by 12 years of age (15).
The TrialNet Pathway to Prevention Study (previously the TrialNet Natural History Study; 16) has been screening relatives of patients with type 1 diabetes since 2004 and follows these subjects with serial autoantibody testing for the development of islet autoantibodies and type 1 diabetes. The study offers longitudinal monitoring for autoantibody-positive subjects through HbA1c testing and oral glucose tolerance tests (OGTTs).
The purpose of this study was to evaluate the prevalence of islet autoantibodies and analyze a logistic regression model to test the effects of genetic factors and common twin environment on the presence or absence of islet autoantibodies in identical twins, nonidentical twins, and full siblings screened in the TrialNet Pathway to Prevention Study. In addition, this study analyzed the presence of islet autoantibodies (GADA, IA-2A, and IAA) and risk of type 1 diabetes over time in identical twins, nonidentical twins, and full siblings followed in the TrialNet Pathway to Prevention Study.
Research Design and Methods
Study Population
Siblings without diabetes of patients with type 1 diabetes were recruited to the TrialNet Pathway to Prevention Study (ClinicalTrials.gov identifier: NCT00097292), as previously described (16). TrialNet subjects (N = 50,700) were screened in the Pathway to Prevention Study between 2004 and 2015. Race/ethnicity and zygosity of participants were self-reported. All study participants gave informed consent, and the ethics committee responsible for each clinical site approved the study. Participants who were single autoantibody positive at the screening visit were required to have a confirmatory positive result. Individuals with single confirmed autoantibody positive or multiple islet autoantibodies were offered baseline assessment of OGTTs and monitored every 6–12 months with autoantibody testing, HbA1c, and OGTTs at 6- or 12-month intervals depending on estimated risk (16). In the TrialNet Pathway to Prevention Study, siblings who are initially autoantibody negative are annually retested for islet autoantibodies until 18 years of age, whereas autoantibody-positive subjects are monitored every 6–12 months. The exceptions are identical twins who remain eligible for annual autoantibody rescreening until 45 years of age (new Pathway to Prevention protocol as of November 2017). Type 1 diabetes was diagnosed according to the TrialNet definitions of development of diabetes, which include the American Diabetes Association criteria (17) as well as the following criteria if subjects are not unequivocally symptomatic: two diabetic OGTTs, not on the same day; diabetic OGTT plus fasting plasma glucose ≥126 mg/dL, not on the same day; diabetic OGTT plus HbA1c ≥6.5% (these may be on the same day); and fasting plasma glucose ≥126 mg/dL plus HbA1c ≥6.5% (these may be on the same day).
A total of 48,051 sibling subjects were initially screened (288 identical twins, 630 nonidentical twins, and 47,133 full siblings). Of these, 48,026 had an initial screening visit with GADA, IA2A, and IAA results (287 identical twins, 630 nonidentical twins, and 47,109 full siblings). A total of 17,226 participants (157 identical twins, 283 nonidentical twins and 16,786 full siblings) were followed for a median of 2.1 years (25th percentile 1.1 year and 75th percentile 4.0 years), with follow-up defined as at least ≥12 months follow-up after initial screening visit. These subjects were analyzed in the longitudinal analysis (Supplementary Fig. 1).
Zygosity was self-reported, which is less accurate than questionnaire or DNA-based determination of zygosity (18). However, to measure the uncertainty of self-reported twin zygosity, we have previously determined zygosity for 88 affected and unaffected cotwins. This was based on sex differences and DNA testing using a panel of tetranucleotide polymorphisms with >99% accuracy for zygosity diagnosis. These unpublished results indicated 2.5% of identical twins are misclassified nonidentical, and 14.6% of nonidentical twins are misclassified identical. Thus, on average, unaffected identical twins share 99% of genetic material with their affected cotwin, and unaffected nonidentical twins share 57% of genetic material with their affected cotwin (P. Fain, L.P., A.K.S., unpublished observations). We therefore designed our logistic regression model outlined below, taking this information into account.
IAA
All participants were screened for GADA, IA-2A, and IAA. If any of these were positive, autoantibodies to ZnT8 and islet cell antibodies were also tested. As ZnT8 and islet cell antibody measurements were not consistently performed in this cohort, these were not included in this analysis. GADA, IA-2A, and IAA were measured by radioimmunoassay in the TrialNet Core Laboratory at the Barbara Davis Center for Diabetes, Aurora, CO, as previously described (2,3). In the 2015 Islet Autoantibody Standardization Program Workshop, sensitivities and specificities were 52% and 100%, respectively, for IAA, 82% and 99%, respectively, for GADA, and 72% and 100%, respectively, for IA-2A.
Statistical Analysis
Statistical analyses were performed using Prism (GraphPad Software, Inc., La Jolla, CA) and SAS version 9.4 (SAS Institute, Cary, NC). Follow-up time was defined as the time from initial visit to development of autoantibodies/type 1 diabetes or most recent visit.
Logistic regression was used to test the association of autoantibody outcomes, G (average fraction of genes shared identical by descent with affected proband), and E (environmental factors unique to twins [i.e., shared uterine environment]) in models adjusted for age and sex. Given our findings on misclassification of self-reported twin zygosity, the term for the average proportion of genes shared for each type of sibling (G) was defined as 50% for nontwins, 57% for nonidentical twins, and 99% for identical twins. The model’s second variable, E, was assigned a value of 1 for both identical twins and nonidentical twins and a value of 0 for siblings. Due to the nature of the TrialNet Pathway to Prevention Study, which follows first-degree relatives of patients with type 1 diabetes for development of autoantibodies and diabetes, we are unable to study the probands/twins with type 1 diabetes for whom we only have onset of diabetes.
Survival analysis was performed for development of IAA and/or type 1 diabetes using the log-rank test. Participants were classified as autoantibody negative, single autoantibody positive, or multiple autoantibody positive based on initial screening. Single antibody–positive subjects had to have confirmed results to be classified as single antibody positive. Participants were also classified as autoantibody negative, single autoantibody positive, or multiple autoantibody positive at follow-up by combining the autoantibody results at all follow-up visits. A participant who had any follow-up visit with multiple autoantibody–positive results was classified as multiple autoantibody positive. A participant who had any follow-up visit with a single positive autoantibody but no follow-up visit with multiple positive autoantibodies was classified as single autoantibody positive. For time-to-event analyses, subjects who have the event at time 0 (screening) were excluded, as we do not know when they had the event because TrialNet is not a birth cohort.
Presence of autoantibodies and development of type 1 diabetes by sibling status (full siblings, identical twins, and nonidentical twins) were also analyzed by Cox proportional hazard models, adjusted for age.
Results
A total of 48,051 sibling subjects were initially screened (288 identical twins, 630 nonidentical twins, and 47,133 full siblings). Of these, 48,026 had an initial screening visit with GADA, IA-2A, and IAA results (287 identical twins, 630 nonidentical twins, and 47,109 full siblings). Characteristics of the study population at screening are shown in Supplementary Table 1. Identical twins were more likely to be female, 158 out of 287 (55.0%), compared with nonidentical twins, 296 out of 630 (47.1%), and full siblings, 24,525 out of 47,109 (52.4%) (P = 0.019). The median age at screening was 11 years old in identical and full siblings and 10 years old in nonidentical twins (P = 0.002). There was a slight difference in self-reported race/ethnicity with 84% of identical twins, 81% of nonidentical twins, and 79% of full siblings identifying as non-Hispanic white (P = 0.043). For those for whom HLA genotyping was available, the presence of the high-risk HLA haplotypes DR4*0302 or DQA1*05:01(DR3) was not significantly different between groups. The high-risk HLA genotype DQA1*05:01 DR3/4*0302 was present in 4% of identical twins, 1% of nonidentical twins, and <1% of full siblings (<0.001). The protective HLA haplotype DR2*0602 was not significantly different between groups (Supplementary Table 1).
Prevalence of autoantibodies at initial screening visit by sibling status (N = 48,026) is shown in Table 1. Overall, identical twins were more likely to have positive GADA, IA-2A, and/or IAA than either nonidentical twins or full siblings (all P ≤ 0.0001). The highest proportion of participants with at least one positive autoantibody were identical twins, whereas full siblings had the lowest proportion and nonidentical twins were intermediate. A similar pattern was seen in the proportion of participants with two or more autoantibodies. Interestingly, nonidentical twins were more likely to have at least one positive autoantibody and be positive for IAA and the combination of IA-2A and IAA but not GADA when compared with full siblings. At the initial screening visit, GADA was present in 20.2% of identical twins (58 out of 287), 5.6% of nonidentical twins (35 out of 630), and 4.7% of full siblings (2,205 out of 47,109) (P < 0.0001). Additionally, IA-2A was present primarily in identical twins (9.4%; 27 out of 287) and less so in nonidentical twins (3.3%; 21 out of 630) and full siblings (2.2%; 1,042 out of 47,109) (P = 0.0001). Nearly 12% of identical twins (34 out of 287) were positive for IAA at initial screen, whereas 4.6% of nonidentical twins (29 out of 630) and 2.5% of full siblings (1,152 out of 47,109) were initially IAA positive (P < 0.0001). Odds ratios (ORs) with 95% CIs comparing autoantibody outcomes by sibling status are summarized in Table 1.
Table 1.
Prevalence and autoantibody outcomes at screening by sibling status (N = 48,026)
| IT (%) | NT (%) | FS (%) | IT vs. NT OR (95% CI) | P value (IT vs. NT) | NT vs. FS OR (95% CI) | P value (NT vs. FS) | |
|---|---|---|---|---|---|---|---|
| GADA | 20.2 | 5.6 | 4.7 | 4.31 (2.76–6.73) | <0.0001 | 0.84 (0.59–1.18) | 0.302 |
| IA-2A | 9.4 | 3.3 | 2.2 | 3.01 (1.67–5.42) | 0.0001 | 1.52 (0.98–2.36) | 0.06 |
| IAA | 11.9 | 4.6 | 2.5 | 2.78 (1.66–4.67) | <0.0001 | 1.92 (1.32–2.81) | 0.0005 |
| ≥1 positive Ab | 23.3 | 8.3 | 6.2 | 3.39 (2.28–5.02) | <0.0001 | 1.36 (1.02–1.80) | 0.0365 |
| ≥2 positive Ab | 12.9 | 4.0 | 2.4 | 3.58 (2.11–6.08) | <0.0001 | 1.72 (1.15–2.58) | 0.0079 |
| Both IA-2A and IAA positive | 5.9 | 2.1 | 0.9 | 2.99 (1.43–6.24) | 0.0023 | 2.23 (1.28–3.89) | 0.0038 |
Ab, islet autoantibody; FS, full siblings; IT, identical twins; NT, nonidentical twins.
Logistic regression was used to assess the influence of genes (G) and shared uterine environment (E) on autoantibody outcomes in models adjusted for age and sex: G was defined as the average fraction of genes shared identical by descent with the affected proband, and E was defined as the environmental factors unique to twins (i.e., shared uterine environment) (Table 2). Younger age, male sex, and genetic factors were significantly associated with one or more positive autoantibody, two or more positive autoantibodies, IA-2A, and IAA (separately or combined), whereas only genetic factors were significant for GADA. An influence of common twin environment (E) was not seen.
Table 2.
Effects of genetic and environmental factors on autoantibody outcomes (N = 47,729)
| Covariate | OR (95% CI) | P value |
|---|---|---|
| GADA as outcome | ||
| Age | 1.00 (0.995–1.005) | 0.9664 |
| Genetic factors (G) | 33.89 (11.54–99.48) | <0.0001 |
| Environmental factors (E) | 0.922 (0.614–1.385) | 0.697 |
| Sex (female) | 0.97 (0.89–1.05) | 0.453 |
| IA-2A as outcome | ||
| Age | 0.97 (0.96–0.98) | <0.0001 |
| Genetic factors (G) | 16.82 (4.10–69.72) | 0.0001 |
| Environmental factors (E) | 1.19 (0.71–2.00) | 0.521 |
| Sex (female) | 0.79 (0.70–0.89) | 0.0001 |
| IAA as outcome | ||
| Age | 0.95 (0.94–0.96) | <0.0001 |
| Genetic factors (G) | 15.28 (4.37–53.49) | <0.0001 |
| Environmental factors (E) | 1.48 (0.95–2.32) | 0.085 |
| Sex (female) | 0.75 (0.67–0.84) | <0.0001 |
| ≥1 positive autoantibody as outcome | ||
| Age | 1.00 (0.99–1.00) | 0.033 |
| Genetic factors (G) | 19.78 (7.64–51.21) | <0.0001 |
| Environmental factors (E) | 1.07 (0.77–1.51) | 0.681 |
| Sex (female) | 0.89 (0.83–0.96) | 0.002 |
| ≥2 positive autoantibodies as outcome | ||
| Age | 0.96 (0.95–0.97) | <0.0001 |
| Genetic factors (G) | 26.68 (7.43–95.84) | <0.0001 |
| Environmental factors (E) | 1.28 (0.80–2.07) | 0.307 |
| Sex (female) | 0.82 (0.73–0.92) | 0.0008 |
| Both IA-2A and IAA positive as outcome | ||
| Age | 0.92 (0.91–0.94) | <0.0001 |
| Genetic factors (G) | 19.61 (3.29–116.87) | 0.0011 |
| Environmental factors (E) | 1.67 (0.86–3.23) | 0.1286 |
| Sex (female) | 0.67 (0.57–0.83) | <0.0001 |
Logistic regression models testing the association of autoantibody outcomes, G (average fraction of genes shared identical by descent with affected proband), and E (environmental factors unique to twins [i.e., shared uterine environment]) adjusted for age and sex.
Survival analyses were performed for the development of antibodies or type 1 diabetes in those subjects who were followed in the monitoring phase of TrialNet Pathway to Prevention Study. A total of 17,226 subjects (157 identical twins, 283 nonidentical twins, and 16,786 full siblings) were followed over time with a median follow-up of 2.1 years (25th percentile 1.1 year and 75th percentile 4.0 years). Characteristics of these participants are shown in Supplementary Table 2.
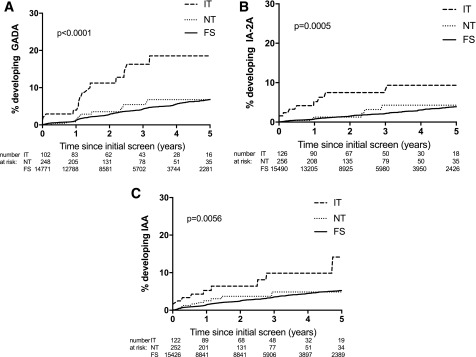
At 3 years of follow-up, the risk for development of GADA was 16% for identical twins, 5% for nonidentical twins, and 4% for full siblings (P < 0.0001) (Fig. 1A). The risk for development of IA-2A by 3 years of follow-up was 7% for identical twins, 4% for nonidentical twins, and 2% for full siblings (P = 0.0005) (Fig. 1B). At 3 years of follow-up, the risk of development of IAA was 10% for identical twins, 5% for nonidentical twins, and 4% for full siblings (P = 0.006) (Fig. 1C). For time-to-event analyses, it is important to note that subjects who had the event at time 0 (screening) were excluded, as we do not know when they had the event because TrialNet is not a birth cohort.
Figure 1.
Development of autoantibodies by sibling status: development of GADA (A), development of IA-2A (B), and development of IAA (C). FS, full siblings; IT, identical twins; NT, nonidentical twins.
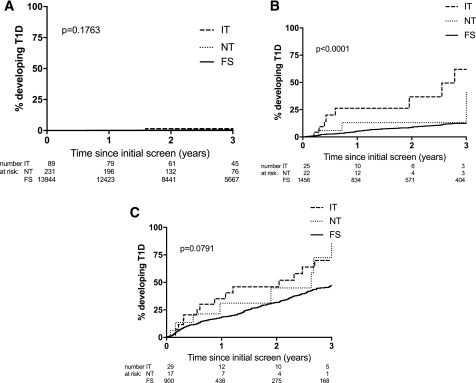
Survival analyses for development of type 1 diabetes by antibody positivity at screening are shown in Fig. 2. In initially autoantibody-negative subjects, 1.5% of identical twins, 0% of nonidentical twins, and 0.5% of full siblings progressed to diabetes at 3 years of follow-up (P = 0.18) (Fig. 2A). For initially single autoantibody–positive subjects, at 3 years of follow-up, 69% of identical twins, 13% of nonidentical twins, and 12% of full siblings developed type 1 diabetes (P < 0.0001) (Fig. 2B). Subjects who were positive for multiple autoantibodies at screening had a higher risk of developing type 1 diabetes at 3 years of follow-up with 69% of identical twins, 72% of nonidentical twins, and 47% of full siblings developing type 1 diabetes (P = 0.079) (Fig. 2C). Onset of type 1 diabetes in the proband twin was more closely correlated in identical twins (r = 0.89; P < 0.0001) (Supplementary Fig. 2A) versus nonidentical twins (r = 0.62; P = 0.01) (Supplementary Fig. 2B). For initially single antibody–positive twins, a total of nine identical twins progressed to diabetes, with three of them progressing through the intermediate stage of multiple antibody positive. A total of four nonidentical twins who initially were positive for one autoantibody developed type 1 diabetes, with two of them progressing through the intermediate stage of multiple antibodies. Because TrialNet is not a birth cohort and the median age at screening visit was 11 years overall, this study would not capture subjects who had initial seroconversion at a young age and then progressed through the intermediate stage of multiple antibody positivity before developing diabetes.
Figure 2.
Development of type 1 diabetes (T1D) by initial autoantibody status: autoantibody negative (A), single autoantibody positive (B), and multiple autoantibody positive (C). FS, full siblings; IT, identical twins; NT, nonidentical twins.
Development of autoantibodies and type 1 diabetes by sibling status was also analyzed by Cox proportional hazard models, adjusted for age (Supplementary Table 3). Younger age was a significant factor, with identical twins still having significantly higher hazard ratios (HRs) compared with full siblings for all autoantibody outcomes (GADA, IA-2A, and IAA). Nonidentical twins did not have a significantly higher HR compared with full siblings for all autoantibody outcomes (IAA, GADA, or IA-2A). For the type 1 diabetes outcome, age was a significant factor for identical twins and full siblings, but not in nonidentical twins (Supplementary Table 4).
Conclusions
This study of >48,000 siblings of patients with type 1 diabetes shows that at initial screening, identical twins were more likely to have at least one positive autoantibody and be positive for GADA, IA-2A, and IAA than either nonidentical twins or full siblings. Interestingly, nonidentical twins were more likely to have at least one positive autoantibody and be positive for IAA but not GADA when compared with full siblings. In addition, risk for development of type 1 diabetes at 3 years of follow-up was high for both single and multiple autoantibody–positive identical twins (62–69%) and multiple autoantibody–positive nonidentical twins (72%) compared with 47% for initially multiple autoantibody–positive full siblings and 12–13% for initially single autoantibody–positive nonidentical twins and full siblings. To our knowledge, this is the largest prediagnosis study to evaluate the effects of genetic factors and common twin environment on the presence or absence of islet autoantibodies.
In this study, younger age, male sex, and genetic factors were significantly associated with expression of IA-2A, IAA, more than one autoantibody, and more than two autoantibodies, whereas only genetic factors were significant for GADA. An influence of common twin environment (E) was not seen. In those subjects monitored in the TrialNet Pathway to Prevention Study (N = 17,226), risk of development of autoantibodies at 3 years follow-up was higher in identical twins than nonidentical twins or siblings, with the highest increase seen in development of GADA. As the median age of this cohort is 11 years old at initial visit, it is not surprising that the highest risk for development of autoantibodies is seen for GADA. Besides younger age and genetic factors, our study also revealed an effect of male sex on expression of islet autoimmunity, consistent with other studies that report a similar increased risk for males (19–21).
Previous studies have shown that identical twin siblings of patients with type 1 diabetes have a higher concordance rate for development of type 1 diabetes compared with nonidentical twins, although reported rates for identical twins have been highly variable (30–70%) (13,14,21–24). Studies from various countries (Australia, Denmark, Finland, Great Britain, and U.S.) have reported concordance rates for nonidentical twins ∼5–15% (8,13,22,23). Concordance rates have been higher when the proband was diagnosed at a younger age (8), which may explain the variability in these reported rates. In this study, autoantibody-negative nonidentical and identical twins had a low risk of type 1 diabetes by 3 years of follow-up. In contrast, once twins developed autoantibodies, risk for type 1 diabetes was high for multiple autoantibody nonidentical twins and both single and multiple autoantibody identical twins.
In addition, nonidentical twins at screening were more likely to have at least one positive autoantibody and be positive for IAA and the combination of IA-2A and IAA when compared with full siblings. These findings may suggest that early postnatal factors such as exposure to illnesses and timing of these factors may be important in the development of type 1 diabetes. Both identical and nonidentical twins share a common in utero environment (E, which was not significant in this study) as well as experience environmental exposures at the same time and age (early shared postnatal environment), whereas full siblings are not necessarily exposed to environmental factors at the same time/age. Other studies have found an influence of environmental factors in addition to genetic risk in twin type 1 diabetes studies (25,26). This early shared postnatal environment could not be evaluated in this study, as the proband sibling with diabetes is not followed in the TrialNet Pathway to Prevention Study. The Environmental Determinants of Diabetes in the Young (TEDDY birth cohort) study has demonstrated differences in autoimmunity initiation according to genetic factors and environmental exposures (19,20).
Risk for development of type 1 diabetes is increased if the proband twin is diagnosed at a young age (8). Previous reports have shown a low rate of concordance in twins diagnosed after 25 years of age (12). However, if identical twin pairs are followed over time, autoantibody positivity and type 1 diabetes frequently develop in twins who are initially discordant for diabetes (13). In Cox proportional hazard models adjusted for age, younger age was a significant factor, with identical twins still having significantly higher HRs compared with full siblings for all autoantibody outcomes. For development of type 1 diabetes, age was a significant factor for identical twins and full siblings but not in nonidentical twins. However, it is important to note that the HR was the same for nonidentical twins as for full siblings (HR 0.97), but the number of nonidentical twins who developed type 1 diabetes over a median follow-up of 2 years was relatively small (N = 17), which likely explains why age did not reach statistical significance in this group.
Limitations of this study include self-reported zygosity, older age at initial screening (overall median 11 years), and small numbers of subjects in some of the groups (in particular in the longitudinal analysis). Additionally, there is limited information for the proband sibling with diabetes other than onset of type 1 diabetes. As this is not a birth cohort, initial seroconversion of these subjects is not known for younger subjects. Furthermore, this study cannot evaluate overall rates of progression to type 1 diabetes as autoantibody-negative subjects have not been followed in the TrialNet Pathway to Prevention Study after the age of 18 years. It is possible that the higher risk of development of diabetes in nonidentical twins is influenced by self-reported zygosity, and inaccurate self-report of zygosity may have influenced (decreased) the risk of diabetes development in identical twins. In regard to the uncertainty of self-reported twin zygosity, we have previously determined zygosity for 88 affected and unaffected cotwins based on sex differences and DNA testing, with unpublished results indicating 2.5% of identical twins are misclassified nonidentical and 14.6% of nonidentical twins are misclassified identical; we have therefore included these variables in the logistic regression models to try to adjust for the misclassification in self-reported zygosity. Additionally, this model only accounts for shared intrauterine environment, and identical twins may have a greater early postnatal shared environment than nonidentical twins or full siblings. Another limitation is the relatively short period of follow-up in this study and the fact that siblings who are initially antibody negative are annually retested in TrialNet only until 18 years of age. This could underestimate the concordance rate for islet autoimmunity over time. Additional follow-up of this cohort over time will be beneficial to determine if the risk of development of type 1 diabetes of multiple autoantibody–positive nonidentical twins remains similar to identical twins.
This study shows that risk for development of type 1 diabetes at 3 years of follow-up is high for both initially multiple and single autoantibody–positive identical twins and multiple autoantibody–positive nonidentical twins. Although genetic predisposition is an important risk factor in development of autoantibodies in twins of patients with type 1 diabetes, age and male sex also seem to play a role in the development of islet autoimmunity and type 1 diabetes.
Supplementary Material
Article Information
Acknowledgments. The authors thank the subjects and families.
Funding. T.M.T. is supported by the National Institute of Diabetes and Digestive and Kidney Diseases T32 training fellowship (5T32-DK-063687-14). A.K.S. is supported by American Diabetes Association grant 1-14-CD-17. The Type 1 Diabetes TrialNet Pathway to Prevention Study Group is a clinical trials network funded by the National Institutes of Health through the National Institute of Diabetes and Digestive and Kidney Diseases, the National Institute of Allergy and Infectious Diseases, and the Eunice Kennedy Shriver National Institute of Child Health and Human Development through cooperative agreements U01-DK-061010, U01-DK-061034, U01-DK-061042, U01-DK-061058, U01-DK-085465, U01-DK-085453, U01-DK-085461, U01-DK-085463, U01-DK-085466, U01-DK-085499, U01-DK-085504, U01-DK-085505, U01-DK-085509, U01-DK-103180, U01-DK-103153, U01-DK-085476, and U01-DK-103266 and by JDRF International.
The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or JDRF.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. T.M.T. researched data and wrote the manuscript. A.F., L.P., and L.Y. researched data and reviewed and edited the manuscript. P.A.G. contributed to discussion and reviewed and edited the manuscript. A.K.S. designed the study, contributed to discussion, and reviewed and edited the manuscript. T.M.T. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented in abstract form at the 77th Scientific Sessions of the American Diabetes Association, San Diego, CA, 9–13 June 2017, and the 43rd Annual Conference of the International Society for Pediatric and Adolescent Diabetes, Innsbruck, Austria, 18–21 October 2017.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc18-0288/-/DC1.
A complete list of the Type 1 Diabetes TrialNet Study Group can be found in the Supplementary Data online.
Contributor Information
Collaborators: Carla J. Greenbaum, M. Atkinson, D. Baidal, M. Battaglia, D. Becker, P. Bingley, E. Bosi, J. Buckner, M. Clements, P. Colman, L. DiMeglio, S. Gitelman, R. Goland, P. Gottlieb, K. Herold, M. Knip, J. Krischer, A. Lernmark, W. Moore, A. Moran, A. Muir, J. Palmer, M. Peakman, L. Philipson, P. Raskin, M. Redondo, H. Rodriguez, W. Russell, L. Spain, D.A. Schatz, J. Sosenko, J. Wentworth, D. Wherrett, D. Wilson, W. Winter, A. Ziegler, M. Anderson, P. Antinozzi, C. Benoist, J. Blum, K. Bourcier, P. Chase, M. Clare-Salzler, R. Clynes, G. Eisenbarth, C.G. Fathman, G. Grave, B. Hering, R. Insel, F. Kaufman, T. Kay, E. Leschek, J. Mahon, J.B. Marks, K. Nanto-Salonen, G. Nepom, T. Orban, R. Parkman, M. Pescovitz, J. Peyman, A. Pugliese, B. Roep, M. Roncarolo, P. Savage, O. Simell, R. Sherwin, M. Siegelman, J.S. Skyler, A. Steck, J. Thomas, M. Trucco, J. Wagner, Jeffrey P. Krischer, Ellen Leschek, Lisa Rafkin, Katarzyna Bourcier, Catherine Cowie, Mary Foulkes, Richard Insel, Heidi Krause-Steinrauf, John M. Lachin, Saul Malozowski, John Peyman, John Ridge, Peter Savage, Jay S. Skyler, Stephanie J. Zafonte, Lisa Rafkin, Jay M. Sosenko, Norma S. Kenyon, Irene Santiago, Jeffrey P. Krischer, Brian Bundy, Michael Abbondondolo, Timothy Adams, Darlene Amado, Ilma Asif, Matthew Boonstra, Cristina Burroughs, David Cuthbertson, Mary Deemer, Christopher Eberhard, Steve Fiske, Julie Ford, Jennifer Garmeson, Heather Guillette, Susan Geyer, Brian Hays, Courtney Henderson, Martha Henry, Kathleen Heyman, Belinda Hsiao, Christina Karges, Nichole Keaton, Amanda Kinderman, Pat Law, Ashely Leinbach, Shu Liu, Jennifer Lloyd, Jamie Malloy, Kristin Maddox, Julie Martin, Jessica Miller, Eric Milliot, Margaret Moore, Sarah Muller, Thuy Nguyen, Ryan O’Donnell, Amy Roberts, Kelly Sadler, Tina Stavros, Roy Tamura, Keith Wood, Ping Xu, Kenneth Young, Persida Alies, Franz Badias, Aaron Baker, Monica Bassi, Craig Beam, David Boulware, London Bounmananh, Susan Bream, Doug Freeman, Jessica Gough, Jinin Ginem, Moriah Granger, Mary Holloway Michelle Kieffer, Page Lane, Cristin Linton, Lavanya Nallamshetty, Vanessa Oduah, Yazandra Parrimon, Kate Paulus, Jennifer Pilger, Joy Ramiro, AQesha Luvon Ritzie, Archana Sharma, Audrey Shor, Xiaohong Song, Amanda Terry, Jeanne Weinberger, Margaret Wootten, John M. Lachin, Mary Foulkes, Pamela Harding, Heidi Krause-Steinrauf, Susan McDonough, Paula F. McGee, Kimberly Owens Hess, Donna Phoebus, Scott Quinlan, Erica Raiden, Emily Batts, Chris Buddy, Kristin Kirpatrick, Mary Ramey, Ann Shultz, Chris Webb, Melita Romesco, Judith Fradkin, Ellen Leschek, Lisa Spain, Peter Savage, Sean Aas, Emily Blumberg, Gerald Beck, David Brillon, Rose Gubitosi-Klug, Lori Laffel, Robert Vigersky, Dennis Wallace, Jonathan Braun, Ake Lernmark, Bernard Lo, Herman Mitchell, Ali Naji, Jorn Nerup, Trevor Orchard, Michael Steffes, Anastasios Tsiatis, Robert Veatch, Bernard Zinman, Brett Loechelt, Lindsey Baden, Michael Green, Adriana Weinberg, Santica Marcovina, Jerry P. Palmer, Adriana Weinberg, Liping Yu, Sunanda Babu, William Winter, George S. Eisenbarth, Polly Bingley, Raphael Clynes, Linda DiMeglio, George Eisenbarth, Brian Hays, Ellen Leschek, Jennifer Marks, Della Matheson, Lisa Rafkin, Henry Rodriguez, Lisa Spain, Darrell Wilson, Maria Redondo, David Gomez, Andrene McDonald, Sandra Pena, Massimo Pietropaolo, Kathy Shippy, Emily Batts, Tyler Brown, Jane Buckner, Angela Dove, Marissa Hammond, Deborah Hefty, Jani Klein, Kristen Kuhns, McKenzie Letlau, Sandra Lord, Marli McCulloch-Olson, Lisa Miller, Gerald Nepom, Jared Odegard, Mary Ramey, Elaine Sachter, Marissa St. Marie, Kimberly Stickney, Dana VanBuecken, Ben Vellek, Christine Webber, Laurie Allen, Jenna Bollyk, Nicole Hilderman, Hebatullah Ismail, Steve Lamola, Srinath Sanda, Heather Vendettuoli, David Tridgell, Roshanak Monzavi, Meredith Bock, Lynda Fisher, Mary Halvorson, Debra Jeandron, Mimi Kim, Jamie Wood, Mitchell Geffner, Francine Kaufman, Robertson Parkman, Christine Salazar, Robin Goland, Raphael Clynes, Steve Cook, Matthew Freeby, Mary Pat Gallagher, Rachelle Gandica, Ellen Greenberg, Amy Kurland, Sarah Pollak, Amy Wolk, Mary Chan, Linda Koplimae, Elizabeth Levine, Kelly Smith, Jeniece Trast, Linda DiMeglio, Janice Blum, Carmella Evans-Molina, Robin Hufferd, Bonnie Jagielo, Christy Kruse, Vanessa Patrick, Mark Rigby, Maria Spall, Kim Swinney, Jennifer Terrell, Lyla Christner, LeeAnn Ford, Sheryl Lynch, Martha Menendez, Patricia Merrill, Mark Pescovitz, Henry Rodriguez, Cielo Alleyn, David Baidal, Steve Fay, Jason Gaglia, Brittany Resnick, Sarah Szubowicz, Gordon Weir, Ronald Benjamin, Debbie Conboy, Andrea deManbey, Richard Jackson, Heyam Jalahej, Tihmar Orban, Alyne Ricker, Joseph Wolfsdorf, Hui H. Zhang, Darrell Wilson, Tandy Aye, Bonita Baker, Karen Barahona, Bruce Buckingham, Kerry Esrey, Trudy Esrey, Garry Fathman, Radhika Snyder, Beenu Aneja, Maya Chatav, Oralia Espinoza, Eliana Frank, Jenny Liu, Jennifer Perry, Rebecca Pyle, Alison Rigby, Kristin Riley, Adriana Soto, Stephen Gitelman, Saleh Adi, Mark Anderson, Ashley Berhel, Kathy Breen, Kathleen Fraser, Andrea Gerard-Gonzalez, Paula Jossan, Robert Lustig, Sara Moassesfar, Amy Mugg, David Ng, Priya Prahalod, Martha Rangel-Lugo, Srinath Sanda, Joshua Tarkoff, Christine Torok, Rebecca Wesch, Ivy Aslan, Jeanne Buchanan, Jennifer Cordier, Celia Hamilton, Louise Hawkins, Thu Ho, Anjali Jain, Karen Ko, Theresa Lee, Shelly Phelps, Stephen Rosenthal, Taninee Sahakitrungruang, Lorraine Stehl, Lisa Taylor, Marcia Wertz, Jenise Wong, Louis Philipson, Rosemary Briars, Nancy Devine, Elizabeth Littlejohn, Tiffany Grant, Peter Gottlieb, Georgeanna Klingensmith, Andrea Steck, Aimon Alkanani, Kimberly Bautista, Ruth Bedoy, Aaron Blau, Betsy Burke, Laraine Cory, MyLinh Dang, Lisa Fitzgerald-Miller, Alex Fouts, Vicky Gage, Satish Garg, Patricia Gesauldo, Raymond Gutin, Cory Hayes, Michelle Hoffman, Kaitlin Ketchum, Nyla Logsden-Sackett, David Maahs, Laurel Messer, Lisa Meyers, Aaron Michels, Stesha Peacock, Marian Rewers, Perla Rodriguez, Flor Sepulbeda, Rachel Sippl, Andrea Steck, Iman Taki, Bao-Khan Tran, Tuan Tran, R. Paul Wadwa, Philip Zeitler, Jennifer Barker, Sandra Barry, Laurie Birks, Leah Bomsburger, Terra Bookert, Leah Briggs, Patricia Burdick, Rosio Cabrera, Peter Chase, Erin Cobry, Amy Conley, Gabrielle Cook, Joseph Daniels, Dominic DiDomenico, Jennifer Eckert, Angelica Ehler, George Eisenbarth, Pamela Fain, Rosanna Fiallo-Scharer, Nicole Frank, Hannah Goettle, Michelle Haarhues, Sherrie Harris, Lauren Horton, John Hutton, Joy Jeffrrey, Rachael Jenison, Kelly Jones, Whitney Kastelic, Maria Amelia King, Debbie Lehr, Jenna Lungaro, Kendra Mason, Heather Maurer, Luy Nguyen, Allison Proto, Jaime Realsen, Kristina Schmitt, Mara Schwartz, San Skovgaard, Jennifer Smith, Brandon Vanderwel, Mary Voelmle, Rebecca Wagner, Amy Wallace, Philip Walravens, Laurie Weiner, Becky Westerhoff, Emily Westfall, Katina Widmer, Hali Wright, Desmond Schatz, Annie Abraham, Mark Atkinson, Miriam Cintron, Michael Clare-Salzler, Jessica Ferguson, Michael Haller, Jennifer Hosford, Diane Mancini, Hank Rohrs, Janet Silverstein, Jamie Thomas, William Winter, Gloria Cole, Roberta Cook, Ryan Coy, Elena Hicks, Nancy Lewis, Jennifer Marks, Alberto Pugliese, Carlos Blaschke, Della Matheson, Alberto Pugliese, Natalia Sanders-Branca, Luz Arazo Ray Arce, Mario Cisneros, Samir Sabbag, Antoinette Moran, Carrie Gibson, Brian Fife, Bernhard Hering, Christine Kwong, Janice Leschyshyn, Brandon Nathan, Beth Pappenfus, Anne Street, Mary Ann Boes, Sarah Peterson Eck, Lois Finney, Theresa Albright Fischer, Andrea Martin, Chenai Jacqueline Muzamhindo, Missy Rhodes, Jennifer Smith, John Wagner, Bryan Wood, Dorothy Becker, Kelli Delallo, Ana Diaz, Barbara Elnyczky, Ingrid Libman, Beata Pasek, Karen Riley, Massimo Trucco, Brian Copemen, Diane Gwynn, Frederico Toledo, Henry Rodriguez, Sureka Bollepalli, Frank Diamond, Emily Eyth, Danielle Henson, Anne Lenz, Dorothy Shulman, Phillip Raskin, Soumya Adhikari, Brian Dickson, Erin Dunnigan, Ildiko Lingvay, Lourdes Pruneda, Maria Ramos-Roman, Philip Raskin, Chanhaeng Rhee, John Richard, Mark Siegelman, Daytheon Sturges, Kathryn Sumpter, Perrin White, Marilyn Alford, Jamie Arthur, M. Larissa Aviles-Santa, Erica Cordova, Renee Davis, Stefani Fernandez, Steve Fordan, Tauri Hardin, Aris Jacobs, Polina Kaloyanova, Ivanna Lukacova-Zib, Sasan Mirfakhraee, Alok Mohan, Hiroshi Noto, Oralenda Smith, Nenita Torres, Diane Wherrett, Diana Balmer, Lesley Eisel, Roze Kovalakovska, Mala Mehan, Farah Sultan, Brenda Ahenkorah, Jose Cevallos, Natasha Razack, Mary Jo Ricci, Angela Rhode, Mithula Srikandarajah, Rachel Steger, William E. Russell, Margo Black, Faith Brendle, Anne Brown, Daniel Moore, Eric Pittel, Alyssa Robertson, April Shannon, James W. Thomas, Kevan Herold, Laurie Feldman, Robert Sherwin, William Tamborlane, Stuart Weinzimer, Jorma Toppari, Tiina Kallio, Maarit Kärkkäinen, Elina Mäntymäki, Tiina Niininen, Birgitta Nurmi, Petro Rajala, Minna Romo, Sointu Suomenrinne, Kirsti Näntö-Salonen, Olli Simell, Tuula Simell, Emanuele Bosi, Manuela Battaglia, Eleonora Bianconi, Riccardo Bonfanti, Pauline Grogan, Andrea Laurenzi, Sabina Martinenghi, Franco Meschi, Matteo Pastore, Luca Falqui, Maria Teresa Muscato, Matteo Viscardi, Polly Bingley, Harriet Castleden, Nicola Farthing, Sam Loud, Claire Matthews, Jennifer McGhee, Ann Morgan, Joanna Pollitt, Rebecca Elliot-Jones, Carole Wheaton, Mikael Knip, Heli Siljander, Heli Suomalainen, Peter Colman, Felicity Healy, Shelley Mesfin, Leanne Redl, John Wentworth, Jinny Willis, Maree Farley, Leonard Harrison, Christine Perry, Fiona Williams, A. Mayo, J. Paxton, V. Thompson, L. Volin, C. Fenton, L. Carr, E. Lemon, M. Swank, M.K. Luidens, M. Salgam, V. Sharma, D. Schade, C. King, R. Carano, J. Heiden, N.D. Means, L. Holman, I. Thomas, D. Madrigal, T. Muth, C.L. Martin, C. Plunkett, C. Ramm, R.J. Auchus, W. Lane, E. Avots, M. Buford, C. Hale, J. Hoyle, B. Lane, A. Muir, S. Shuler, N. Raviele, E. Ivie, M. Jenkins, K. Lindsley, I. Hansen, D.O. Fadoju, E.I. Felner, B. Bode, R. Hosey, J. Sax, C. Jefferies, S. Mannering, R. Prentis, J.X. She, M. Stachura, D. Hopkins, J. Williams, L. Steed, E. Asatapova, S. Nunez, S. Knight, P. Dixon, J. Ching, T. Donner, S. Longnecker, K. Abel, K. Arcara, S. Blackman, L. Clark, D. Cooke, L. Plotnick, P.A. Levin, L. Bromberger, K. Klein, K. Sadurska, C. Allen, D. Michaud, H. Snodgrass, G. Burghen, S. Chatha, C. Clark, J. Silverberg, C. Wittmer, J. Gardner, C. LeBoeuf, P. Bell, O. McGlore, H. Tennet, N. Alba, M. Carroll, L. Baert, H. Beaton, E. Cordell, A. Haynes, C. Reed, K. Lichter, P. McCarthy, S. McCarthy, T. Monchamp, J. Roach, S. Manies, F. Gunville, L. Marosok, T. Nelson, K. Ackerman, J. Rudolph, M. Stewart, K. McCormick, S. May, T. Falls, T. Barrett, K. Dale, L. Makusha, C. McTernana, K. Penny-Thomas, K. Sullivan, P. Narendran, J. Robbie, D. Smith, R. Christensen, B. Koehler, C. Royal, T. Arthur, H. Houser, J. Renaldi, S. Watsen, P. Wu, L. Lyons, B. House, J. Yu, H. Holt, M. Nation, C. Vickers, R. Watling, R. Heptulla, J. Trast, C. Agarwal, D.J. Newell, R. Katikaneni, C. Gardner, A. Del, A. Rio, H. Logan, C. Collier, G. Rishton, A. Whalley, S. Ali, T. Ramtoola, L. Quattrin, A.J. Mastrandea, M. House, C. Ecker, C. Huang, J. Gougeon, D. Ho, D. Pacuad, J. Dunger, C. May, C. O’Brien, B. Acerini, A. Salgin, R. Thankamony, J. Williams, G. Buse, M. Fuller, J. Duclos, H. Tricome, D. Brown, D. Pittard, A. Bowlby, T. Blue, S. Headley, K. Bendre, K. Lewis, C. Sutphin, J. Soloranzo, H. Puskaric, M. Madison, M. Rincon, R. Carlucci, B. Shridharani, E. Rusk, D.M. Tessman, H. Huffman, B. Abrams, M.D. Biederman, V. Jones, W. Leathers, P. Brickman, D. Petrie, J. Zimmerman, L. Howard, R. Miller, D.V. Alemzadeh, R. Mihailescu, N. Melgozza-Walker, C. Abdulla, D. Boucher-Berry, R. Ize-Ludlow, C. Levy, Swenson, N. Brousell, D. Crimmins, T. Edler, C. Weis, D. Schultz, D. Rogers, C. Latham, C. Mawhorter, W. Switzer, P. Spencer, S. Konstantnopoulus, J. Broder, L. Klein, L. Knight, G. Szadek, B. Welnick, R. Thompson, A. Hoffman, J. Revell, K. Cherko, E. Carter, J. Gilson, G. Haines, B. Arthur, W.B. Bowen, P. Zipf, R.A. Graves, D. Lozano, K. Seiple, A. Spicer, J. Chang, J. Fregosi, C. Harbinson, S. Paulson, P. Stalters, D. Wright, A.E. Zlock, J. Freeth, H. Victory, A. Maheshwari, T. Maheshwari, J. Holmstrom, R. Bueno, J. Arguello, L. Ahern, V. Noreika, S. Watson, P. Hourse, C. Breyer, Y. Kissel, M. Nicholson, S. Pfeifer, J. Almazan, M. Bajaj, K. Quinn, J. Funk, E. McCance, R. Moreno, A. Veintimilla, J. Wells, S. Cook, J. Trunnel, S. Henske, K. Desai, F. Frizelis, R. Khan, K. Sjoberg, P.P. Allen, G. Manning, B. Hendry, S. Taylor, W. Jones, M.E. Strader, T. Bencomo, L. Bailey, C. Bedolla, C. Roldan, B. Moudiotis, C. Vaidya, S. Anning, S. Bunce, E. Estcourt, E. Folland, C. Gordon, J. Harrill, J. Ireland, L. Piper, K. Scaife, S. Sutton, M. Wilkins, J. Costelloe, L. Palmer, C. Casas, M. Miller, C. Burgard, J. Erickson, P. Hallanger-Johnson, W. Clark, A. Taylor, S. Lafferty, C. Gillett, M. Nolan, L. Pathak, T. Sondrol, S. Hjelle, J. Hafner, R. Kotrba, A.P. Hendrickson, T. Cemeroglu, M. Symington, Y. Daniel, D.C. Appiagyei-Dankah, M.S. Postellon, L. Racine, K. Kleis, S.E. Barnes, H. Godwin, K. McCullough, G. Shaheen, L. Buck, M.L. Noel, S. Warren, S.M. Weber, I. Parker, B.A. Gillespie, C. Nelson, J. Frost, E.C. Amrhein, A. Moreland, J. Hayes, J. Peggram, M.E. Aisenberg, J. Riordan, E. Zasa, K. Cummings, T. Scott, A. Pinto, K. Mokashi, E. McAssey, P. Helden, L. Hammond, S. Dinning, S. Rahman, C. Ray, S. Dimicri, H. Guppy, C.K. Nielsen, C. Vogel, L. Ariza, Y.T. Morales, R.A. Chang, L. Gabbay, L. Ambrocio, R. Manley, W. Nemery, P. Charlton, L. Smith, B. Kerr, M. Steindel-Kopp, D. Alamaguer, G. Liljenquist, T. Browning, M.B. Coughenour, E. Sulk, M. Tsalikan, J. Tansey, N. Cabbage, S. Dixit, M. Pasha, K. King, H. Adcock, L. Atterberry, K. Fox, N. Englert, J. Mauras, K. Permuy, T. Sikes, B. Berhe, L. Guendling, L. McLennan, C. Paganessi, M.B. Murphy, M. Draznin, S. Kamboj, V. Sheppard, L. Lewis, W. Coates, G. Moore, J. Babar, D. Bedard, J. Brenson-Hughes, M. Cernich, R. Clements, S. Duprau, L. Goodman, L. Hester, A. Huerta-Saenz, T. Karmazin, S. Letjen, D. Raman, W. Morin, E.J. Bestermann, J.L. Morawski, A. White, R. Brockmyer, S. Bays, A Campbell, N. Stapleton, A. Stone, H. Donoho, H. Everett, M. Hensley, C. Johnson, N. Marshall, P. Skirvin, R. Taylor, L. Williams, C. Ray, D.A. Wolverton, C. Nickels, P.W. Dothard, M. Speiser, L. Pellizzari, K. Bokor, S. Izuora, P. Abdelnour, S. Cummings, M. Paynor, M. Leahy, S. Riedl, R. Shockley, T. Saad, S. Briones, C. Casella, K. Herz, J. Walsh, F. Greening, S. Hay, N. Hunt, L. Sikotra, D.G. Simons, R. Karounos, L. Oremus, L. Dye, D. Myers, W. Ballard, R. Miers, K.M. Sparks, K. Thraikill, J. Edwards, S. Fowlkes, A. Kemp, L. Morales, L. Holland, P. Johnson, A. Paul, K. Ghatak, H. Phelen, T. Leyland, D. Henderson, E. Brenner, I. Oppenheimer, C. Mamkin, C. Moniz, M. Clarson, A. Lovell, V. Peters, D. Ruelas, D. Borut, M. Burt, S. Jordan, P. Castilla, M. Flores, L. Ruiz, J. Hanson, R.J. Green-Blair, K.A. Sheridan, G. Wintergerst, A. Pierce, M. Omoruyi, S. Foster, A. Kingery, I. Lunsford, T. Cervantes, P. Parker, J. Price, I. Urben, H. Doughty, V. Haydock, P. Parker, S. Bergman, C. Duncum, A. Rodda, R. Perelman, C. Calendo, E. Barrera, Y. Arce-Nunez, M. Martinez, I. De la Portilla, L. Cardenas, M. Garrido, R. Villar, E. Lorini, G. Calandra, K. D’Annuzio, N. Perri, C. Minuto, R. Rebora, O. Callegari, J. Ali, B. Kramer, S. Auble, P. Cabrera, R. Donohoue, M. Fiallo-Scharer, P. Hessner, A. Wolfgram, N. Kansra, R. Bettin, A. McCuller, S. Miller, J. Accacha, E. Corrigan, R.L. Fiore, T.A. Levine, C. Mahoney, V. Polychronakos, H. Gagne, M. Starkman, D. Fox, F. Chin, L.A. Melchionne, I. Silverman, L. Marshall, J. Cerracchio, A. Cruz, J. Viswanathan, S. Wilson, S. Chalew, S. Valley, A. Layburn, P. Lala, M. Clesi, G. Genet, A. Uwaifo, T. Charron, W. Allerton, L. Cefalu, R. Melendez-Ramirez, C. Richards, E. Alleyn, M. Gustafson, J. Lizanna, S. Wahlen, M. Aleiwe, H. Hansen, C.J. Wahlen, A. Levy, R. Bonaccorso, Y. Rapaport, D. Tomer, M. Chia, L. Goldis, M. Iazzetti, C. Klein, L. Levister, E. Waldman, M.O. Wallach, Z. Regelmann, M. Antal, C. Aranda, A. Reynholds, P. Vinik, M. Barlow, M.L. Bourcier, J. Nevoret, S. Couper, N. Beresford, H. Thalagne, J. Roper, J. Gibbons, S. Hill, C. Balleaut, J. Brennan, L. Ellis-Gage, T. Fear, L. Gray, C. Jones, L. McNerney, N. Pointer, K. Price, D. Few, N. Tomlinson, D. Leech, C. Wake, M. Owens, J. Burns, A. Wotherspoon, K. Murray, G. Short, S. Curry, J. Kelsey, J. Lawson, S. Porter, E. Stevens, S. Thomson, L. Winship, E. Wynn, J. Wiltshire, P. Krebs, H. Cresswell, C. Faherty, L. Ross, J. Denvir, T. Drew, P. Randell, S.A. Mansell, S. Bell, Y. Butler, H. Hooton, A. Navarra, G. Roper, L. Babington, H. Crate, A. Cripps, C. Ledlie, R. Moulds, B. Norton, O. Petrova, C. Silkstone, K. Smith, M. Ghai, V. Murray, M. Viswanathan, O. Henegan, J.A. Kawadry, L. Olson, T. Patterson, B. Ahmad, D. Flores, S. Domek, K. Domek, M. Copeland, J. George, T. Less, M. Davis, A. Short, P. Dwarakanathan, B. O’Donnell, L. Boerner, M. Larson, M. Phillips, K. Rendell, C. Larson, K. Smith, L. Zebrowski, M. Kuechenmeister, M. Thevarayapillai, H. Daniels, N. Speer, R. Forghani, C. Quintana, A. Reh, P. Bhangoo, L. Desrosiers, T. Ireland, C. Misla, S. Torres, J. Wells, M. Villar, D. Yu, D. Berry, J. Cook, A. Soder, M. Powell, M. Ng, Z. Morrison, M. Haslam, B. Lawson, J. Bradley, C. Courtney, C. Richardson, E. Watson, D. Keely, M. DeCurtis, Z. Vaccarcello-Cruz, K. Torres, H. Sandberg, B. Hsiang, D. Joy, A. McCormick, H. Powell, J. Jones, S. Bell, S. Hargadon, M. Hudson, S. Kummer, E. Sauder, K. Sutton, R. Gensel, V. Aguirre-Castaneda, Benavides, D. Lopez, S. Hemp, J. Allen, E. Stear, T. Davis, A. Jones, J.A. Roberts, N. Dart, L.E. Paramalingam, N. Levitt Katz, K.M. Chaudhary, S.M. Murphy, B. Willi, C. Schwartzman, D. Kapadia, D. Larson, G. McClellan, L.A. Shaibai, G. Kelley, C. Villa, R. Kelley, M. Diamond, T. Kabbani, F. Dajani, M. Hoekstra, J. Magorno, V. Holst, N. Chauhan, P. Wilson, M. Bononi, A. Sperl, M. Millward, L. Eaton, J. Dean, H. Olshan, C. Renna, Milliard, L. Brodksy, J.B. Bacon, L.S. Quintos, S. Topor, B. Bialo, A.G. Bancroft, W. Soto, H. Lagarde, T. Lockemer, M.A. Vanderploeg, M. Ibrahim, V. Huie, R. Sanchez, R. Edelen, J. Marchiando, T. Palmer, M. Repas, P. Wasson, J. Auker, T. Culbertson, D. Kieffer, T. Voorhees, L. Borgwardt, K. DeRaad, E. Eckert, H. Isaacson, A. Kuhn, M. Carroll, G. Schubert, S. Francis, T. Hagan, M. Le, E. Penn, C. Wickham, K. Leyva, J. Rivera, I. Padilla, N. Rodriguez, J. Jospe, B. Czyzyk, U. Johnson, N. Nadgir, G. Marlen, C. Prakasam, N. Rieger, E.C. Glaser, B. Heiser, C. Harris, H. Foster, K. Slater, D.L. Wheeler, M. Donaldson, D.E. Murray, R. Hale, D.R. Tragus, J. Word, L. Lynch, W. Pankratz, R. Rogers, S. Newfield, M. Holland, M. Hashiguchi, A. Gottschalk, R. Philis-Tsimikas, S. Rosal, S.M. Franklin, N. Guardado, M. Bohannon, T. Garcia, J. Aguinaldo, V. Phan, D. Barraza, J. Cohen, U. Pinsker, J. Khan, L Wiley, P. Jovanovic, M. Misra, D. Wright, K. Cohen, M. Huang, S. Skiles, C. Maxcy, K. Pihoker, J. Cochrane, S. Fosse, M. Kearns, N. Klingsheim, L. Wright, H. Viles, S. Smith, M. Heller, A. Cunningham, L. Daniels, J. Zeiden, R. Field, K.J. Walker, L. Griffin, C. Bartholow, J. Erickson, B. Howard, C. Krabbenhoft, A. Sandman, J. Vanveldhuizen, A. Wurlger, K. Zimmerman, L. Hanisch, A. Davis-Keppen, J. Cotterill, M. Kirby, A. Harris, C. Schmidt, C. Kishiyama, J. Flores, W. Milton, C. Martin, A. Whysham, T. Yerka, J.M. Freels, J. Hassing, R. Webster, P. Green, J. Carter, D. Galloway, S. Hoelzer, S. Roberts, P. Said, H.F. Sullivan, E. Allen, E. Reiter, C. Feinberg, L.A. Johnson, D. Newhook, N.H. Hagerty, L. White, J. Levandoski, M. Kyllo, C. Johnson, P. Benoit, F. Iyer, H. Diamond, S. Hosono, L. Jackman, P. Barette, I. Jones, S. Sills, J. Bzdick, R. Bulger, I. Weinstock, R. Douek, G. Andrews, G. Modgill, L. Gyorffy, N. Robin, S. Vaidya, K. Crouch, C. O’Brien, N. Thompson, J. Thorne, J. Blumer, L. Kalic, J. Klepek, B. Paulett, J. Rosolowski, M. Horner, J.L. Watkins, K. Casey, C. Carpenter, J. Burns, C. Horton, D. Pritchard, A.G. Soetaert, C. Wynne, O.Y. Chin, C. Molina, R. Patel, M. Senguttuvan, O. Wheeler, C. Furet, D.H. Steuhm, S. Jelley, L. Goudeau, D. Chalmers, C. Greer, D.L. Panagiotopoulos, D. Metzger, M. Nguyen, M.P. Horowitz, E. Christiansen, C. Glades, M. Morimoto, R. Macarewich, K. Norman, C. Patin, A. Vargas, A. Barbanica, P. Yu, W. Vaidyanathan, R. Osborne, S. Mehra, S. Kaster, J. Neace, G. Horner, C. Reeves, L. Cordrey, T. Marrs, S. Miller, D. Dowshen, S. Doyle, D. Walker, H. Catte, M. Dean, B. Drury-Brown, M.M.C. Hackman, S. Lee, K. Malkani, K. Cullen, P. Johnson, M. Hampton, C. McCarrell, E. Curtis, Paul, and Y. Zambrano
References
- 1.Bonifacio E. Predicting type 1 diabetes using biomarkers. Diabetes Care 2015;38:989–996 [DOI] [PubMed] [Google Scholar]
- 2.Yu L, Rewers M, Gianani R, et al. Antiislet autoantibodies usually develop sequentially rather than simultaneously. J Clin Endocrinol Metab 1996;81:4264–4267 [DOI] [PubMed] [Google Scholar]
- 3.Bonifacio E, Yu L, Williams AK, et al. Harmonization of glutamic acid decarboxylase and islet antigen-2 autoantibody assays for National Institute of Diabetes and Digestive and Kidney Diseases consortia. J Clin Endocrinol Metab 2010;95:3360–3367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wenzlau JM, Juhl K, Yu L, et al. The cation efflux transporter ZnT8 (Slc30A8) is a major autoantigen in human type 1 diabetes. Proc Natl Acad Sci U S A 2007;104:17040–17045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ziegler AG, Rewers M, Simell O, et al. Seroconversion to multiple islet autoantibodies and risk of progression to diabetes in children. JAMA 2013;309:2473–2479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bingley PJ, Boulware DC, Krischer JP; Type 1 Diabetes TrialNet Study Group . The implications of autoantibodies to a single islet antigen in relatives with normal glucose tolerance: development of other autoantibodies and progression to type 1 diabetes. Diabetologia 2016;59:542–549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bosi E, Boulware DC, Becker DJ, et al. Impact of age and antibody type on progression from single to multiple autoantibodies in type 1 diabetes relatives. J Clin Endocrinol Metab 2017;102:2881–2886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hyttinen V, Kaprio J, Kinnunen L, Koskenvuo M, Tuomilehto J. Genetic liability of type 1 diabetes and the onset age among 22,650 young Finnish twin pairs: a nationwide follow-up study. Diabetes 2003;52:1052–1055 [DOI] [PubMed] [Google Scholar]
- 9.Metcalfe KA, Hitman GA, Rowe RE, et al. Concordance for type 1 diabetes in identical twins is affected by insulin genotype. Diabetes Care 2001;24:838–842 [DOI] [PubMed] [Google Scholar]
- 10.Fava D, Gardner S, Pyke D, Leslie RD. Evidence that the age at diagnosis of IDDM is genetically determined. Diabetes Care 1998;21:925–929 [DOI] [PubMed] [Google Scholar]
- 11.Verge CF, Gianani R, Yu L, et al. Late progression to diabetes and evidence for chronic β-cell autoimmunity in identical twins of patients with type I diabetes. Diabetes 1995;44:1176–1179 [DOI] [PubMed] [Google Scholar]
- 12.Redondo MJ, Yu L, Hawa M, et al. Heterogeneity of type I diabetes: analysis of monozygotic twins in Great Britain and the United States. Diabetologia 2001;44:354–362 [DOI] [PubMed] [Google Scholar]
- 13.Redondo MJ, Jeffrey J, Fain PR, Eisenbarth GS, Orban T. Concordance for islet autoimmunity among monozygotic twins. N Engl J Med 2008;359:2849–2850 [DOI] [PubMed] [Google Scholar]
- 14.Redondo MJ, Rewers M, Yu L, et al. Genetic determination of islet cell autoimmunity in monozygotic twin, dizygotic twin, and non-twin siblings of patients with type 1 diabetes: prospective twin study. BMJ 1999;318:698–702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aly TA, Ide A, Jahromi MM, et al. Extreme genetic risk for type 1A diabetes. Proc Natl Acad Sci U S A 2006;103:14074–14079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahon JL, Sosenko JM, Rafkin-Mervis L, et al.; TrialNet Natural History Committee; Type 1 Diabetes TrialNet Study Group . The TrialNet Natural History Study of the Development of Type 1 Diabetes: objectives, design, and initial results. Pediatr Diabetes 2009;10:97–104 [DOI] [PubMed] [Google Scholar]
- 17.American Diabetes Association Classification and diagnosis of diabetes. Sec. 2. In Standards of Medical Care in Diabetes—2017. Diabetes Care 2017;40(Suppl. 1):S11–S2427979889 [Google Scholar]
- 18.Cohen DJ, Dibble E, Grawe JM, Pollin W. Reliably separating identical from fraternal twins. Arch Gen Psychiatry 1975;32:1371–1375 [DOI] [PubMed] [Google Scholar]
- 19.Krischer JP, Lynch KF, Lernmark A, et al. Genetic and environmental interactions modify the risk of diabetes-related autoimmunity by 6 years of age: the TEDDY study. Diabetes Care 2017;40:1194–1202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Krischer JP, Lynch KF, Schatz DA, et al. The 6 year incidence of diabetes-associated autoantibodies in genetically at-risk children: the TEDDY study. Diabetologia 2015;58:980–987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar D, Gemayel NS, Deapen D, et al. North-American twins with IDDM. Genetic, etiological, and clinical significance of disease concordance according to age, zygosity, and the interval after diagnosis in first twin. Diabetes 1993;42:1351–1363 [DOI] [PubMed] [Google Scholar]
- 22.Kyvik KO, Green A, Beck-Nielsen H. Concordance rates of insulin dependent diabetes mellitus: a population based study of young Danish twins. BMJ 1995;311:913–917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Condon J, Shaw JE, Luciano M, Kyvik KO, Martin NG, Duffy DL. A study of diabetes mellitus within a large sample of Australian twins. Twin Res Hum Genet 2008;11:28–40 [DOI] [PubMed] [Google Scholar]
- 24.Bogdanos DP, Smyk DS, Rigopoulou EI, et al. Twin studies in autoimmune disease: genetics, gender and environment. J Autoimmun 2012;38:J156–J169 [DOI] [PubMed] [Google Scholar]
- 25.Beyan H, Riese H, Hawa MI, et al. Glycotoxin and autoantibodies are additive environmentally determined predictors of type 1 diabetes: a twin and population study. Diabetes 2012;61:1192–1198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nisticò L, Iafusco D, Galderisi A, et al.; Study Group on Diabetes of the Italian Society of Pediatric Endocrinology and Diabetology . Emerging effects of early environmental factors over genetic background for type 1 diabetes susceptibility: evidence from a Nationwide Italian Twin Study. J Clin Endocrinol Metab 2012;97:E1483–E1491 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.