Abstract
Background
Ever since the first appendectomy has been performed, surgery has been the standard of care for acute appendicitis, with antibiotic therapy being reserved for special situations. Recent studies have shown the feasibility of antibiotic therapy for uncomplicated appendicitis.
Methods
This clinical therapeutic review is based both on author expertise and a selective literature survey in PubMed based on the term ‘appendicitis’, combined with the terms ‘acute’, ‘complicated’, ‘conservative’, ‘non-operative’, ‘therapy’, ‘surgery’, and ‘strategy’. According to these search results as well as to the treatment guidelines from the American College of Surgeons, Society for Surgery of the Alimentary Tract, Society of American Gastrointestinal and Endoscopic Surgeons, European Association of Endoscopic Surgery, and World Society of Emergency Surgery, we present an interdisciplinary treatment concept.
Results
Approximately 90% of patients treated with antibiotics are able to avoid surgery during the initial admission. The other 10% that fail to respond to antibiotics require a rescue appendectomy. Recurrence rates of non-operated patients within 1 year are as high as 20–30%.
Conclusion
In uncomplicated appendicitis without risk factors for failure of non-operative management, a shared decision based on the patient's preferences should be made. In cases with risk factors, appendectomy is still the treatment recommended. If the diagnosis is uncertain or clinical symptoms are rather mild, antibiotic therapy should be started. In complicated appendicitis, management depends on the clinical state, with either immediate surgery or primarily antibiotic therapy and combined with drainage of abscess, being followed by interval appendectomy in some cases.
Keywords: Abdominal infections, Acute appendicitis, Antibiotic therapy, Complicated appendicitis, Laparoscopic surgery
Introduction
Although being one of the most common abdominal emergencies with a lifetime risk of about 8%, the pathogenesis of appendicitis is still not fully understood. It is thought to be multifactorial, with mechanical, infectious and genetic circumstances leading to inflammation of the appendix [1].
Appendicitis can present as simple or uncomplicated, with inflammation of the appendix with or without phlegmonous imbibition of its surroundings, or as complicated appendicitis, with inflammation having led to gangrene or perforation, with or without building of an abscess. Perforation is found in 13–20% of patients who present with acute appendicitis [2]. Although it has been assumed for a long time that uncomplicated appendicitis will eventually lead to a complicated form, recent data have led to speculations that different biologic forms of appendicitis might exist. Although the overall rates of appendicitis are decreasing, the rate of patients presenting with perforated appendicitis and with only a short period of time since onset of symptoms did not [3].
For over a century, open appendectomy was the only standard treatment for appendicitis. Recently published European trials have suggested that it is feasible to treat uncomplicated appendicitis non-operatively with antibiotics alone [4, 5, 6, 7, 8, 9]. With regard to these data, we want to analyze the evidence for non-operative management (NOM) of acute appendicitis and to eventually suggest a clinical pathway for the management of this disease.
Diagnosis of Appendicitis
We recommend a diagnostic algorithm using ultrasound as the primary imaging strategy after history taking, clinical examination, and blood tests. If ultrasound is not diagnostic, we recommend performing a computed tomography (CT) scan or, if available, magnetic resonance imaging (MRI). In pregnant women, MRI should be performed instead of a CT scan. This strategy has shown to reduce the use of a CT scan in up to 50% of cases while achieving a diagnosis in 90% of patients with acute abdominal pain [10].
Treatment of Appendicitis
Since the first appendectomy was performed by McBurney in 1864, surgical removal of the appendix has been considered the standard of care for acute appendicitis. Initially performed via laparotomy, laparoscopic appendectomy has now become the new standard of care in the Western world. In recent years, increasing evidence has emerged, showing that NOM is a genuine alternative treatment option at least in some clinical scenarios. Although many cornerstones have yet to be defined, appendicitis is more and more becoming a disease with many different facets/aspects that require different therapeutic strategies.
Principles of Surgery
Appendectomy can be performed as open surgery or laparoscopically. Both procedures are routine operations with very low operational risks, and morbidity and mortality are mainly determined by the severity of appendiceal disease itself. Although small, differences between both methods exist, with laparoscopic appendectomy emerging as the preferred method in Western countries.
In technical terms, the laparoscopic approach is thought to be superior in terms of a lower rate of wound infections, less pain on postoperative day 1, and a shorter duration of hospital stay [11]. Maybe more importantly, it offers the possibility of inspecting the whole intra-abdominal cavity, therefore detecting other causes mimicking appendicitis as well as leading to fewer short- and long-term adhesive bowel obstructions [12, 13]. Open surgery, meanwhile, is associated with a lower rate of intra-abdominal abscesses, a slightly shorter operative time, and lower costs, although this might change with more widespread use and further developments of laparoscopy.
Timing of appendectomy has been debated controversially. At the time when every appendicitis was thought to progress to perforation and gangrene, surgery was to be performed as soon as possible. Laparoscopic appendectomy for advanced uncomplicated appendicitis should be performed during the first 24 h after diagnosis. Today, there is evidence that in uncomplicated appendicitis, a delay of 12–24 h prior to surgery does not increase the rate of perforation if a course of antibiotics is immediately started, as demonstrated in a meta-analysis of 11 non-randomized studies [14]. Waiting for more than 48 h, though, leads to a higher rate of surgical site infections and other complications.
In patients with complicated appendicitis, the timing of the operation depends on the clinical status of the patient, the nature of the perforation, and, in some cases, the therapeutic strategy preferred [15, 16]. In severely sick patients with signs of free perforation or generalized peritonitis, emergency appendectomy should be performed. Septic, hemodynamically instable patients may need preoperative resuscitation and stabilization. In stable patients with non-free perforation and in patients with an appendiceal abscess or a phlegmon of the right lower quadrant, initial therapy usually is non-operative, and appendectomy is only performed if conservative therapy fails. Especially in patients with a long duration of symptoms and/or extensive abscess formation, immediate surgery has shown to be associated with higher rates of postoperative abscesses or enterocutaneous fistulae, as well as higher ileocecal resection rates [17, 18]. For a selected group of patients with complicated appendicitis, though, immediate appendectomy is an alternative treatment option, especially if the abscess cannot be drained successfully [18, 19]. If recommended, interval appendectomy can be carried out electively after resolving of the inflammation, although its use is discussed controversially [20, 21].
For the authors, it is noteworthy that every single operation is accompanied by at least a single dose of antibiotics given preoperatively to reduce wound infection. If complex appendiceal disease is found intraoperatively, antibiotic therapy is continued for at least 3–5 days [22].
Non-Operative Management
Several European trials have demonstrated in the last 20 years that in adults, conservative management of acute appendicitis is feasible. Treating appendicitis with antibiotics alone is not a new concept. Since the inauguration of antibiotic therapy, it has been shown to be feasible in trials as early as in the 1950s [23], or simply just out of need, e.g. in a maritime or military setting [24]. Gurin et al. [25] published a series of 252 passengers with suspected appendicitis on ships in the sea who did not have the option of immediate surgery and thus where treated with antibiotics, which was successful in 84% of the patients. Also, in some forms of complicated appendicitis, antibiotic therapy is well established as initial treatment, often in combination with drainage of large abscesses [15, 19].
Principals of Non-Operative Management
Most treatment protocols include an initial course of intravenous antibiotics for 1–3 days, followed by oral antibiotics for 7 days [4, 5, 6, 7, 8, 9]. Usually, either a combination of a cephalosporin and tinidazole or a broad-spectrum penicillin combined with a betalactam inhibitor is being administered. In one trial, ertapenem has been used, leading to deserved criticism for inadequately using reserve antibiotics [9]. As experience with non-operative treatment will increase, the length of antibiotic therapy will likely shorten, with the now rigid schedule adapting to a more patient-oriented course with cessation of therapy 1–2 days after significant clinical improvement, as in other abdominal infections.
Usually the first days of treatment take place in an inpatient setting, with close monitoring of the patient's condition and the option of performing rescue appendectomy in case of clinical deterioration. If the clinical condition improves, patients are usually discharged and the antibiotic course is completed at home. If treatment has been successful, a colonoscopy and an ultrasound or a CT scan within 6 months are usually recommended to rule out underlying malignant disease, at least in patients with a reasonable risk thereof (usually in patients older than 40 years) [1, 26, 27].
Timing of antibiotic therapy is important since beginning treatment as early as possible has shown to increase success rates significantly [25, 28].
If antibiotic treatment is not successful during the initial admission, rescue appendectomy must be performed. In recurrent disease, either a second course of antibiotics or appendectomy can be applied. Under both conditions, complications and risks of appendectomy are not elevated [9, 29].
Results
Approximately 90% of patients treated with antibiotics are able to avoid surgery during the initial admission. The other 10% that fail to respond to antibiotics require a rescue appendectomy. Recurrence rates of non-operated patients within 1 year are as high as 20–30% [4, 5, 6, 7, 8, 9].
Different risk factors for failure of NOM have been found. In the study by Vons et al. [8], risk factors for failure were fever at initial presentation, high presenting serum C-reactive protein levels, and an intraluminal fecalith. The combination of elevated levels of C-reactive protein and a fecalith predicted failure of antibiotic therapy in a study with 224 patients initially receiving antibiotic therapy [29]. In another trial, the presence of an appendicolith increased the failure rate of antibiotic therapy from 24% without an appendicolith to 50% [30]. One study tried to determine a model of prediction, with a combination of a serum C-reactive protein of less than 60 mg/l, a white blood count lower than 12, and age younger than 60 years presenting a very good chance of successful NOM [31]. In a retrospective cohort analysis of 81 consecutive patients who underwent NOM of uncomplicated appendicitis, duration of symptoms prior to admission >25 h, a maximum temperature of <37.3 °C within 6 h of admission, a modified Alvarado score <4, and an appendiceal diameter <13 mm were independent predictors of successful NOM [32]. Furthermore, in one trial, women with diabetes showed a significantly higher failure rate of NOM [33].
Should Uncomplicated Appendicitis Be Treated Non-Operatively?
As demonstrated above, NOM of acute uncomplicated appendicitis is feasible and a safe alternative to surgery. Consequently, the question is whether it is better than surgery and whether it should become the standard of care or remain an alternative form of therapy for selected cases.
There is no doubt that appendectomy is the most efficient way of treating appendicitis, with success rates of >95% as well as low overall morbidity and mortality [28]. However, it is a way more invasive treatment than a course of antibiotics. When comparing antibiotic therapy with surgery, we should be aware that we are comparing two treatment strategies of different nature and not two different surgical techniques. Therefore, we should take a broader look and not focus on success rates alone.
To undergo surgery, although considered low-risk, is no small feat and represents a burden for many patients. Many patients would consider ‘surgery’ a complication by itself [34]. Therefore, many patients would surely prefer a non-operative approach. For example, when debating NOM of acute appendicitis in children, one study found that most parents prefer NOM for their children [35].
For patients with a history of prior surgical or anesthesiology complications, antibiotic therapy bears potentially great advantages, although those patients have been excluded from all of the trials.
Performing surgery also requires enormous personnel and technical resources. Since incidence of appendicitis is high, even a moderate reduction of the surgery rate might lead to significantly less operations required.
In addition, NOM would thoroughly reduce the rate of negative appendectomies, meaning the avoidance of unnecessary removal of uninflamed appendices. As a consequence of a pure operative strategy, there is a constant number of patients who intraoperatively present with a normal appendix. Those negative appendectomy rates depend on the diagnostic strategy and vary from 6 to 20%, with the best results coming from programs where a CT scan is routinely performed [36]. A small number of patients with a normal appendix is not operated in vain, as surgery, especially when performed laparoscopically, may reveal other underlying diseases in some of these cases.
Why Do Not Remove All of Them?
Although NOM of acute appendicitis seems desirable in many aspects, it certainly bears some disadvantages. Criticism of NOM mainly centers on the risk of recurrent disease, which has been estimated to be as high as 38%, although recurrence rates were between 20 and 30% in most trials. However, follow-up periods in these studies mostly covered only 1 year. Long-term follow-up from non-randomized trials and observational studies, lasting up to 7 years, does not demonstrate higher rates of recurrence [37]. The recently published NOTA study demonstrated a success rate of 83% for NOM after a 2-year follow-up [38]. The mean time for recurrence was after approximately 4 months, therefore suggesting that longer follow up-periods do not necessarily lead to significantly higher rates of recurrent disease. However, while there are patients who prefer to avoid any kind of surgery, there are certainly a lot of patients who want to avoid any risk of recurrence and who want their appendix removed as a definite solution (e.g. young people that are often travelling around the world, either for work or as tourists).
Other aspects of NOM which are criticized include the lack of definitive histology, thereby missing a possibly underlying appendiceal tumor, and, if the operation would have been performed laparoscopically, potentially missing a chance to diagnose other intra-abdominal morbidities if the appendix is not inflamed. Appendiceal tumor, e.g., is rare though, with overall rates of less than 1% [25, 26]. It should mainly be considered in patients aged >40 years.
A real drawback of data on NOM is the lack of evidence in some of the patients that might benefit the most from an avoidance of operation: older patients, those with medical comorbidities, and immunocompromised patients, as all of them have been excluded from trials. Further concerns arise because in those patients, diagnosis is often difficult since presentation is often atypical; therefore, clinical evaluation of antibiotic therapy might be even more difficult. As a result, we can only speculate if the aforementioned factors outweigh the risk reduction stemming from an avoidance of operation.
Another possible disadvantage of a generally conservative approach could be a significant rise in the use of antibiotics, as some patients might need a few courses of antibiotic treatment during the course of their lives. Depending on the antibiotic regimen used, this might increase resistance towards antibiotics and lead to an even heavier burden of Clostridium difficile infections. Although this risk does not seem to outweigh the risks of an operation, it may still be of significance to the general burden of disease.
Treatment Scenarios
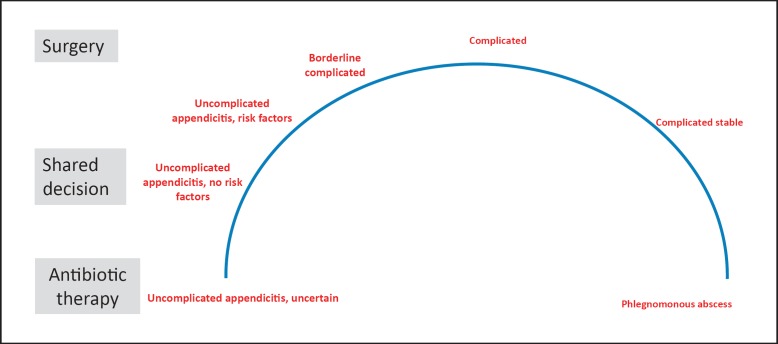
In light of the aforementioned growing evidence on successful non-operative treatment of acute appendicitis, we suggest a clinical pathway with respect to different clinical scenarios, leading to an arc of antibiotic and surgical therapy (fig. 1).
Fig. 1.
Acute appendicitis - the arc of therapy.
Mild Appendicitis Suspected, Low Probability
• Diagnosis not certain, but acute appendicitis likely - antibiotic trial.
These patients often present with atypical clinical symptoms, with equivocal results of imaging and not or only slightly elevated laboratory values. Appendicitis seems to be the most likely diagnosis, but findings are not very convincing. In these patients, an antibiotic trial or, in very mild cases, clinical observation alone should be performed. Laparoscopy can be considered as a diagnostic tool and alternative, especially in young women. If symptoms resolve under antibiotic therapy, an interval appendectomy with regard to the risk of recurrence should be openly discussed.
Uncomplicated Appendicitis Suspected, High Probability
• Clinical presentation, imaging, and laboratory findings typical, no risk factors for failure - shared decision.
In this scenario, typical clinical symptoms, findings in imaging, and elevated inflammation markers point to an acute appendicitis without signs of complications. If no risk factors for failure of NOM are present (see above), a shared decision should be made, with discussion of possible advantages and disadvantages of respective treatment regimens and acknowledgment of personal preferences.
If surgery is the preferred treatment, a delay of 12–24 h prior to surgery does not increase the rate of perforation if a course of antibiotics is started immediately, as demonstrated in a meta-analysis of 11 non-randomized studies [14]. Waiting for more than 48 h, though, leads to a higher rate of surgical site infections and other complications.
Advanced Uncomplicated Appendicitis or Proven Complicated Appendicitis
• Strong clinical symptoms (local peritonism), highly elevated inflammation markers, or proven complicated appendicitis - surgery as soon as possible.
If patients present with strong clinical symptoms (e.g. local peritonism in right lower quadrant), highly elevated inflammation markers, and/or signs of complication in imaging studies, surgery should be performed as soon as possible. In this group, patients are more likely to have a complicated form of appendicitis even if imaging does not show it. In severely sick patients with signs of free perforation or generalized peritonitis, emergency appendectomy should be performed. Septic, hemodynamically instable patients may need preoperative resuscitation and stabilization.
Complicated Appendicitis with a Phlegmon/Larger Abscess
• Evidence of an appendiceal abscess or phlegmon on imaging studies - antibiotics and drainage in most cases, alternatively surgery.
In patients with complicated appendicitis with abscess formation, the timing of the operation depends on the clinical status of the patient, the nature of the perforation, and, in some cases, the therapeutic strategy preferred. In stable patients with non-free perforation and in patients with an appendiceal abscess or a phlegmon of the right lower quadrant, initial therapy usually is non-operative, and appendectomy only is performed if conservative therapy fails. Especially in patients with a long duration of symptoms and/or extensive abscess formation, immediate surgery was shown to be associated with higher rates of postoperative abscesses or enterocutaneous fistulae as well as higher ileocecal resection rates [18]. For a selected group of patients with complicated appendicitis, though, immediate appendectomy is an alternative treatment option, especially if the abscess cannot be drained successfully. If recommended, interval appendectomy can be carried out electively after resolving of the inflammation.
Future Aspects
The success of conservative therapy will eventually depend on the experience gained in further trials as well as in everyday practice, especially regarding recurrence rates and nature of recurrence episodes over the years.
We do not know yet if recurrence primarily happens within the first year or if failure rates will steadily rise over the years. The available data hint at a rather early recurrence, with a mean time to appendectomy of 4.2–7 months in trials. Also, when comparing long-term data, a progression in recurrence is not noticeable, whereas the studies are very heterogeneous.
Overall, if a recurrence rate of 20–30% is considered to be acceptable and clinical practice is therefore changed, it could potentially lead to a reduction of surgery in 70–80% of cases in a selected group of patients with uncomplicated appendicitis. Otherwise, if upcoming experience with NOM shows a higher recurrence rate of almost 50% or even more, NOM would remain more of a short-term therapeutic option and a valid definitive option in selected cases (e.g. in elderly with a high operation risk or in cancer patients with advanced disease).
So far, recent data has not changed the treatment of uncomplicated appendicitis in everyday clinical practice. In 2016, a study investigated the treatment strategy applied in more than 4,000 patients with acute uncomplicated appendicitis, demonstrating a dominance of surgical management with a rate of 96%. Interestingly, almost 45% of operations were open appendectomy [39]. This reflects the ongoing notion that operative management of uncomplicated appendicitis is still considered to be superior by surgeons. Furthermore, medicolegal aspects may also play a major role in a rather slow change of clinical practice.
Outlook
We can envision appendicitis to be understood as a widely more complex disease than it has been perceived in the past. Maybe the term ‘uncomplicated appendicitis’ alone subsumes at least three different variants of disease: i) never, ii) slowly, or iii) rapidly progressing to perforation. Considering this and the emerging evidence that appendicitis can be safely treated non-operatively, in our point of view there is no doubt that treatment of appendicitis will become more complex. Whether surgery will remain the main overall treatment modality or will be widely replaced by antibiotic therapy remains open and seems to be dependent on the results of upcoming trials as well as the experience gained in everyday clinical practice. However, there is no doubt that, just as in diverticular disease, there will always be a significant number of patients who will require surgery, either immediately or in intervals. To identify which patients will need surgery with high probability/anyway is one of the major tasks in this scenario, with our current risk factors for failure of NOM needing to be re-evaluated by further trials and daily practice.
One of the main future goals will be to improve diagnosis of appendicitis, especially the diagnostic capability to differentiate between the various forms of appendicitis. Efforts should be made to try to reduce radiation exposure by improving and spreading ultrasound competence, thus firmly establishing ultrasound as the first-line imaging modality in acute abdominal disease. Alternatively, or additionally, by improving technical (and pecuniary) aspects of MRI, this modality will establish itself as a more widely available and faster technology, thereby allowing for quicker evaluation in acute abdominal disease.
Furthermore, better understanding of appendiceal disease may come from research of the appendiceal microbiome and a better knowledge of the pathophysiology. Maybe the composition of the appendiceal microbiome will help to understand the various forms of appendicitis, or a specific organ-derived biomarker will arise, helping to identify either acute appendicitis itself or to distinguish between the subforms.
Finally, as first preliminary data on endoscopic treatment of acute appendicitis is published, maybe conservative treatment will be further improved by combining antibiotic treatment with endoscopic drainage of the appendiceal lumen by a stent [40, 41].
Disclosure Statement
The authors state that there is no conflict of interest
References
- 1.Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 2.Andersson RE, Hugander A, Thulin AJ. Diagnostic accuracy and perforation rate in appendicitis: association with age and sex of the patient and with appendicectomy rate. Eur J Surg. 1992;158:37–41. [PubMed] [Google Scholar]
- 3.Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245:886–892. doi: 10.1097/01.sla.0000256391.05233.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eriksson S, Granström L. Randomized controlled trial of appendicectomy versus antibiotic therapy for acute appendicitis. Br J Surg. 1995;82:166–169. doi: 10.1002/bjs.1800820207. [DOI] [PubMed] [Google Scholar]
- 5.Styrud J, Eriksson S, Nilsson I, et al. Appendectomy versus antibiotic treatment in acute appendicitis A prospective multicenter randomized controlled trial. World J Surg. 2006;30:1033–1037. doi: 10.1007/s00268-005-0304-6. [DOI] [PubMed] [Google Scholar]
- 6.Hansson J, Körner U, Khorram-Manesh A, et al. Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 2009;96:473–481. doi: 10.1002/bjs.6482. [DOI] [PubMed] [Google Scholar]
- 7.Turhan AN, Kapan S, Kütükçü E, et al. Comparison of operative and non operative management of acute appendicitis. Ulus Travma Acil Cerrahi Derg. 2009;15:459–462. [PubMed] [Google Scholar]
- 8.Vons C, Barry C, Maitre S, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377:1573–1579. doi: 10.1016/S0140-6736(11)60410-8. [DOI] [PubMed] [Google Scholar]
- 9.Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313:2340–2348. doi: 10.1001/jama.2015.6154. [DOI] [PubMed] [Google Scholar]
- 10.van Randen A, Laméris W, van Es HW, van Heesewijk HP, van Ramshorst B, Ten Hove W, Bouma WH, van Leeuwen MS, van Keulen EM, Bossuyt PM, Stoker J, Boermeester MA. OPTIMA Study Group: A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol. 2011;21:1535–1545. doi: 10.1007/s00330-011-2087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jaschinski T, Mosch C, Eikermann M, Neugebauer EA. Laparoscopic versus open appendectomy in patients with suspected appendicitis: a systematic review of meta-analyses of randomised controlled trials. BMC Gastroenterol. 2015;15:48. doi: 10.1186/s12876-015-0277-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moberg AC, Ahlberg G, Leijonmarck CE, et al. Diagnostic laparoscopy in 1043 patients with suspected acute appendicitis. Eur J Surg. 1998;164:833–840. doi: 10.1080/110241598750005246. [DOI] [PubMed] [Google Scholar]
- 13.Markar SR, Penna M, Harris A. Laparoscopic approach to appendectomy reduces the incidence of short- and long-term post-operative bowel obstruction: systematic review and pooled analysis. J Gastrointest Surg. 2014;18:1683–1692. doi: 10.1007/s11605-014-2572-7. [DOI] [PubMed] [Google Scholar]
- 14.United Kingdom National Surgical Research Collaborative; Bhangu A. Safety of short, in-hospital delays before surgery for acute appendicitis: multicentre cohort study, systematic review, and meta-analysis. Ann Surg. 2014;259:894–903. doi: 10.1097/SLA.0000000000000492. [DOI] [PubMed] [Google Scholar]
- 15.Oliak D, Yamini D, Udani VM, Lewis RJ, Arnell T, Vargas H, Stamos MJ. Initial nonoperative management for periappendiceal abscess. Dis Colon Rectum. 2001;44:936–941. doi: 10.1007/BF02235479. [DOI] [PubMed] [Google Scholar]
- 16.Cheng Y, Xiong X, Lu J, et al. Early versus delayed appendicectomy for appendiceal phlegmon or abscess. Cochrane Database Syst Rev. 2017;6 doi: 10.1002/14651858.CD011670.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mentula P, Sammalkorpi H, Leppäniemi A. Laparoscopic surgery or conservative treatment for appendiceal abscess in adults? A randomized controlled trial. Ann Surg. 2015;262:237–242. doi: 10.1097/SLA.0000000000001200. [DOI] [PubMed] [Google Scholar]
- 18.Gee D, Babineau TJ. The optimal management of adult patients presenting with appendiceal abscess: ‘conservative’ vs immediate operative management. Curr Surg. 2004;61:524–528. doi: 10.1016/j.cursur.2004.07.004. [DOI] [PubMed] [Google Scholar]
- 19.Simillis C, Symeonides P, Shorthouse AJ, Tekkis PP. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon) Surgery. 2010;147:818–829. doi: 10.1016/j.surg.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Darwazeh G, Cunningham SC, Kowdley GC. A systematic review of perforated appendicitis and phlegmon: interval appendectomy or wait-and-see? Am Surg. 2016;82:11–15. [PubMed] [Google Scholar]
- 21.Kaminski A, Liu IL, Applebaum H, et al. Routine interval appendectomy is not justified after initial nonoperative treatment of acute appendicitis. Arch Surg. 2005;140:897–901. doi: 10.1001/archsurg.140.9.897. [DOI] [PubMed] [Google Scholar]
- 22.van Rossem CC van, Schreinemacher MH, Treskes K, van Hogezand RM, van Geloven AA. Duration of antibiotic treatment after appendicectomy for acute complicated appendicitis. Br J Surg. 2014;101:715–719. doi: 10.1002/bjs.9481. [DOI] [PubMed] [Google Scholar]
- 23.Coldrey E. Treatment of acute appendicitis. Br Med J. 1956;2:1458–1461. doi: 10.1136/bmj.2.5007.1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wojciechowicz KH, Hoffkamp HJ, van Hulst RA. Conservative treatment of acute appendicitis: an overview. Int Marit Health. 2010;62:265–272. [PubMed] [Google Scholar]
- 25.Gurin NN, Slobodchuk IuS, Gavrilov IuF. The efficacy of the conservative treatment of patients with acute appendicitis on board ships at sea (Article in Russian) Vestn Khir Im I I Grek. 1992;148:144–150. [PubMed] [Google Scholar]
- 26.Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum. 1998;41:75–80. doi: 10.1007/BF02236899. [DOI] [PubMed] [Google Scholar]
- 27.Ma KW, Chia NH, Yeung HW, Cheung MT. If not appendicitis, then what else can it be? A retrospective review of 1492 appendectomies. Hong Kong Med J. 2010;16:12–17. [PubMed] [Google Scholar]
- 28.Podda M, Cillara N, Di Saverio S, et al. ACOI (Italian Society of Hospital Surgeons) Study Group on Acute Appendicitis: Antibiotics-first strategy for uncomplicated acute appendicitis in adults is associated with increased rates of peritonitis at surgery. A systematic review with meta-analysis of randomized controlled trials comparing appendectomy and non-operative management with antibiotics. Surgeon. 2017;15:303–314. doi: 10.1016/j.surge.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Shindoh J, Niwa H, Kawai K, Ohata K, Ishihara Y, Takabayashi N, Kobayashi R, Hiramatsu T. Predictive factors for negative outcomes in initial non-operative management of suspected appendicitis. J Gastrointest Surg. 2010 Feb;14:309–314. doi: 10.1007/s11605-009-1094-1. [DOI] [PubMed] [Google Scholar]
- 30.Lee SL, Spence L, Mock K, Wu JX, Yan H, DeUgarte DA. Expanding the inclusion criteria for nonoperative management of uncomplicated appendicitis: outcomes and cost. J Pediatr Surg. 2018;53:42–47. doi: 10.1016/j.jpedsurg.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 31.Hansson J, Khorram-Manesh A, Alwindawe A, Lundholm K. A model to select patients who may benefit from antibiotic therapy as the first line treatment of acute appendicitis at high probability. J Gastrointest Surg. 2014;18:961–967. doi: 10.1007/s11605-013-2413-0. [DOI] [PubMed] [Google Scholar]
- 32.Loftus TJ, Brakenridge SC, Croft CA, Stephen Smith R, Efron PA, Moore FA, Mohr AM, Jordan JR. Successful nonoperative management of uncomplicated appendicitis: predictors and outcomes. J Surg Res. 2018;222:212–218. doi: 10.1016/j.jss.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsai MC, Lin HC, Lee CZ. Diabetes increases the risk of an appendectomy in patients with antibiotic treatment of noncomplicated appendicitis. Am J Surg. 2017;214:24–28. doi: 10.1016/j.amjsurg.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 34.Talan DA, Moran GJ, Saltzman DJ. Nonoperative management of appendicitis: avoiding hospitalization and surgery. J Am Coll Surg. 2017;224:994. doi: 10.1016/j.jamcollsurg.2017.01.001. [DOI] [PubMed] [Google Scholar]
- 35.Steiner Z, Buklan G, Gutermacher M, Litmanovitz I, Landa T, Arnon S. Conservative antibiotic treatment for acute uncomplicated appendicitis is feasible. Pediatr Surg Int. 2018;34:283–288. doi: 10.1007/s00383-018-4226-4. [DOI] [PubMed] [Google Scholar]
- 36.SCOAP Collaborative; Cuschieri J, Florence M, Flum DR, et al. Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg. 2008;248:557–563. doi: 10.1097/SLA.0b013e318187aeca. [DOI] [PubMed] [Google Scholar]
- 37.Lundholm K, Hansson-Assarsson J, Engström C, Iresjö BM. Long-term results following antibiotic treatment of acute appendicitis in adults. World J Surg. 2017;41:2245–2250. doi: 10.1007/s00268-017-3987-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Di Saverio S, Sibilio A, Giorgini E, et al. The NOTA Study (Non Operative Treatment for Acute Appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann Surg. 2014;260:109–117. doi: 10.1097/SLA.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 39.Sartelli M, Baiocchi GL, Di Saverio S, et al. Prospective Observational Study on acute Appendicitis Worldwide (POSAW) World J Emerg Surg. 2018;13:19. doi: 10.1186/s13017-018-0179-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu BR, Ma X, Feng J, Yang Z, Qu B, Feng ZT, Ma SR, Yin JB, Sun R, Guo LL, Liu WG. Endoscopic retrograde appendicitis therapy (ERAT): a multicenter retrospective study in China. Surg Endosc. 2015;29:905–909. doi: 10.1007/s00464-014-3750-0. [DOI] [PubMed] [Google Scholar]
- 41.Ye LP, Mao XL, Yang H, He BL, Zhu LH, Zhang Y. Endoscopic retrograde appendicitis techniques for the treatment of patients with acute appendicitis. Z Gastroenterol. 2018;56:899–904. doi: 10.1055/a-0581-9119. [DOI] [PubMed] [Google Scholar]