Abstract
As healthcare systems continue to expand their use of electronic health records (EHRs), barriers to robust and successful engagement with such systems by stakeholders remain tenacious. To this effect, this research presents the results of a survey tool utilizing both original and modified constructs from the Consolidated Framework for Implementation Research to assess key points of engagement barriers and potential points of intervention for stakeholders of EHRs in a large-scale healthcare organization (500-bed level II regional trauma center). Based on the extensive assessment, the paper presents recommendations for the utility of engagement process modeling and discusses how intervention opportunities can be used to mitigate engagement barriers.
Keywords: electronic health records, consolidated framework for implementation, intervention, adoption
Background and Introduction
The integration of technology into healthcare systems presents a complex narrative. While technology use in healthcare settings (clinical and nonclinical) has been touted as an asset for healthcare providers, healthcare consumers, and other relevant business stakeholders,1, 2, 3 resistance to technology implementation and the subsequent failure of health information systems are well documented.4, 5 A more realistic perspective on the implementation of technology would be one that views implementation as an iterative process that must continually take into account the variability of complexity6 and context in healthcare settings. However, the substantial resources involved in implementing a technology-based system into a healthcare setting (financial, human, time, and risk management) necessitates early implementation success and full engagement on the part of all stakeholders to maximize the benefits of using the system. The use of electronic health records (EHRs) is an illustrative case, as the benefits of use may greatly depend on the engaged interactions of patients, healthcare providers, and other healthcare system professionals.7, 8, 9 The term engagement may be most often used to reflect interest in and access to a technology. However, for purposes of this study, the term is applied to a broader context encompassing the range of practices and processes of stakeholders from adoption to integration of EHRs.
As part of a continuation of work on leveraging the cloud for EHR access,10 the researchers developed a process for engagement modeling. A key component of this modeling approach was the construction of a survey tool based on constructs of the Consolidated Framework for Implementation Research (CFIR) to investigate barriers to full engagement of the technologies involved in EHR access and implementation. The CFIR is one of several emergent models from the field of implementation science.11, 12, 13 Despite psychometric measurement challenges,14 the CFIR has shown great promise as a highly adaptable model for investigating the implementation of technology in healthcare settings.15, 16, 17, 18 The CFIR presents a set of holistic and well-defined implementation construct categories stemming in large part from its parent theory, Roger's Diffusion of Innovations theory,19 and subsequent work conducted by Damshroeder et al.20 and others.21 In summary, the CFIR explores how characteristics of the intervention, the inner and outer settings of where an intervention will be deployed, the characteristics of the individuals who will interact with the intervention, and the functional processes involved with implementing the intervention are all key assessment domains.22, 23 Information gleaned from the variables within each of the main construct categories24 can be leveraged to benefit all stakeholders and potentially minimize barriers to successful EHR engagement.
Tool Design and Methodology
Barriers to the implementation of healthcare technology in clinical settings include a wide and diverse continuum ranging from human-related factors (e.g., resistance by healthcare providers) to technical factors (e.g., failed system design).25, 26, 27 While external policies like those of the Meaningful Use program can spur adoption and initial implementation, long-term implementation requires committed engagement by all relevant stakeholders (healthcare providers, information technology [IT] staff, and, to some extent, patient end users). Developing a stakeholder engagement model process may be advantageous for organizations to maintain successful implementation by highlighting priority areas where stakeholders have either concordance or discordance on barriers and benefits of the technology.
This research identifies the CFIR as a beneficial framework for engagement modeling because of the comprehensive and holistic nature of the constructs, as detailed in Table 1. These constructs allow for domain flexibility and a thorough investigation of perceptions of benefits and barriers. Although the CFR includes numerous constructs, it includes only five primary areas to investigate. The categories are defined here in context of the current research.
Intervention characteristics: the attributes and qualities of the intervention (in this case the EHR system)
Outer setting: the external forces shaping adoption and implementation of the EHR system
Inner setting: the internal organizational forces shaping adoption and implementation of the EHR system
Characteristics of the individual: attributes of the stakeholders and end users of the EHR system
Process mandates: the contextual specificities of the implementation process of the EHR
Table 1.
Constructs for the Proposed Engagement Modeling
| • Intervention source is identified as the perception of the key stakeholders about whether the selected intervention is externally or internally developed. |
| • Adaptability is defined as the ease of access and use of the healthcare solution for various participants. Adaptability is specific to the participant group. |
| • Trialability is defined as the feasibility of evaluating the healthcare solution on a pilot scenario within the healthcare organization to provide insights and recommendations for a successful overall implementation. |
| • Complexity of a given healthcare solution is defined as the perceived difficulty of implementation. The complexity varies according to the participant group and ranges from healthcare compliance to stability and usability of the solution. |
| • Cost of the healthcare intervention includes the associated costs of implementation, deployment. and maintenance. |
| • Quality of design refers to the assembly and presentation of the healthcare intervention. |
| • Client requirements identifies the level of intervention needed to address barriers and facilitate accuracy and prioritization within the healthcare organization. |
| • Self-efficacy refers to the belief in the individual's capabilities to execute the courses of action for the effective implementation and practice of the healthcare goals. |
| • Regulatory policies and incentives identify external strategies to spread healthcare interventions, including policy regulations from federal, state, and local agents. This construct also includes incentives from both external and internal organizational-level entities. |
| • Engagement practice of any given healthcare organization identifies the policies and procedures for combining social marketing, education, role modeling, and training activities to promote effective healthcare adoption. |
| • External change agents are identified as those that are affiliated with outside entities and who formally influence or facilitate the design and implementation of the healthcare intervention. |
| • Location is identified as the target of the planned adoption, either urban, semi-urban, or rural. |
| • Barriers and needs are identified as the extent to which patient needs and the barriers to and facilitators of meeting those needs are accurately and adequately identified by the target organization. |
| • Organizational culture refers to the norms and values of the organization. |
| • Structural characteristics are identified as the social age and maturity of the organization. |
| • Security changes are identified as the identified organization's security modifications as determined by internal or external agents for the organization. |
| • Readiness of implementation is identified as the immediate indicators of the organization's commitment to its decision to implement the identified intervention. |
| • Resource availability is identified as the dedicated resources for the implementation of ongoing operations for the organization. |
| • Implementation climate is identified as the organizational absorptive capacity for change and the shared receptiveness of the individuals involved for the implementation of the identified intervention. |
| • Goals and feedback is identified as the degree to which organizational goals are clearly communicated and feedback from stakeholders is adequately addressed in a timely manner. |
| • Relative priority is the stakeholders' shared perception of the importance of the implementation within the organization. |
| • Resources for intervention are identified as the level of resources budgeted for identification and implementation of the specific intervention. |
| • Champions are stakeholders identified by the organization to support, manage, and facilitate implementation of the intervention. |
| • Leadership engagement identifies the commitment of organizational management for the implementation of the intervention. |
| • Reflecting and evaluating is identified as the qualitative and quantitative feedback mechanism in place to assess the progress and quality of the intervention implementation. |
| • Accountability is identified as the perception of the key stakeholders as to the protocol execution and audit process of the identified organization. |
| • Evidence strength and quality is identified as the key stakeholders' perceptions of the quality and validity of the evidence supporting the desired outcomes of the identified intervention. |
| • Relative advantage is the organizational stakeholders' perception of the advantage of implementing the intervention in comparison to alternative solutions. |
| • Interoperability is identified as the key stakeholders' perception of the synchronized mechanism for information sharing and dissemination of the identified intervention. |
| • Organizational compliance identifies the overall organizational security, privacy, and compliance posture for effective application of the intervention. |
Using these five categories, one can develop a broad perspective on the “why or why not” of stakeholder engagement and can drill down and focus on specific constructs under each category.
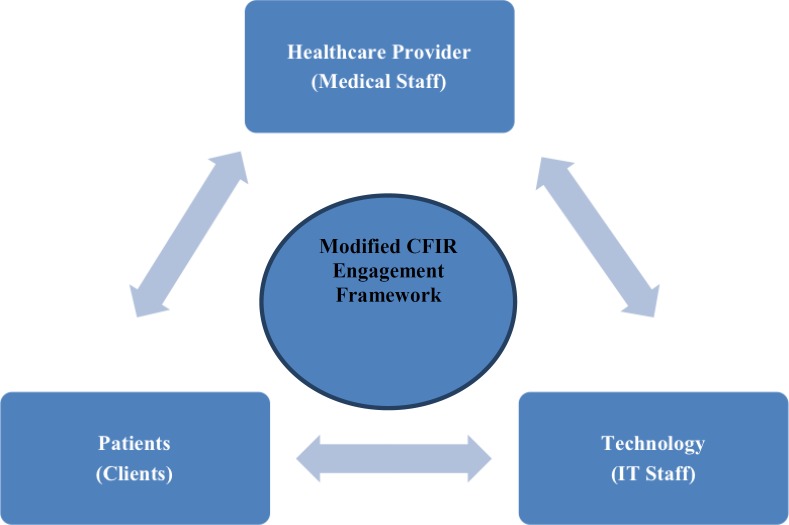
Maximizing the opportunity for successful implementation requires identifying and recommending pivotal attributes to improve engagement outcomes for any given healthcare organization. The current research leverages the CFIR to this effect. The proposed research identified three primary groups of participants for the study: the medical/healthcare staff of a large sized federally recognized healthcare organization, the IT staff at the healthcare organization, and the core in-hospital patients at the organization. The key to a successful healthcare engagement is the focused and directed participation of the stakeholders of the healthcare technology. The three phases, as discussed below, identify the operational process used to design an effective engagement tool across the stakeholder groups.
The first phase of the study (construct identification) included a set of targeted interview sessions conducted to gather qualitative data about the most relevant CFIR constructs for the evaluation study. The interviews were conducted anonymously with the key stakeholders of the healthcare intervention and implementation process. Note that a new iteration of the construct identification process can be conducted if the application domain and/or the patient service environments are modified. Furthermore, our study indicates and recommends that to ensure effective adoption and implementation, the organization should conduct periodic assessments of the construct identification to provide a seamless integration of the developing technology landscape.28 Figure 1 details the overall interaction diagram, which leverages the CFIR framework for the design of the proposed EHR engagement model.
Figure 1.
Proposed Electronic Health Record Engagement Model Abbreviations: CFIR, Consolidated Framework for Implementation Research; IT, information technology.
The construct identification phase lays out the qualitative interviewing process and aids in the instrumentation of the tool to help guide the choice of the constructs. The steps followed in this phase include stakeholder vetting and unique stakeholder identification (this process is done in an anonymous fashion, preserving only the type/experience level of the stakeholder); stakeholder engagement process establishment and verification; and, finally, the controlled study of the process with the target group/community.
After the targeted interview sessions, the researchers used a concept mapping approach (proprietary tool) to identify the CFIR variables29 (i.e., variables under each of the main construct categories previously identified) that are most relevant to the pilot healthcare organization. These variables were then integrated with the authors' previous work on EHRs to augment (add to or modify) the construct categories to yield an integrated construct domain tailored to the specific healthcare IT environment.
The next phase of the tool design process is the data collection and analysis phase. This phase is important to review the appropriate feedback on the identified constructs and assimilate stakeholder input to provide accurate metrics and priorities for the appropriate interventions. The steps followed in this phase include data collection, priority selection, and data analysis (via interview sessions to determine metrics for tool development). The constructs are iteratively modified on the basis of stakeholder feedback to ensure that they are mapped to the appropriate implementation domain.
The next phase of this process is the tool implementation phase, which is based on the feedback from the previous phases. The implementation phase included a targeted functional review of the tool and an iterative evaluation and analysis prior to dissemination. The tool was designed and implemented with a modified set of CFIR constructs identified for the domain-specific study. It also included an augmentation of additional constructs necessary for the specific domain of assessment, such as accountability, interoperability, and organizational compliance. The detailed definitions and mapping of the constructs for the engagement modeling are stated in Table 1.
The final phase is the dissemination of the designed tool over the three vital stakeholder domains, namely medical staff, IT staff, and patients. The survey was disseminated over a 500-bed Level II certified regional trauma center at stage 6 of the HIMSS Analytics Electronic Medical Record Adoption Model, managing more than 500,000 patient admissions per year. The healthcare organization houses a large data center that caters to three medium-scale auxiliary hospitals and 20 participating specialized clinical practice centers. The tool included an intuitive tiered numerical mapping for the survey. The participants were advised by the tool to identify, with a score of 0 (no relevance), 1 (positive relevance), or −1 (negative relevance), each construct's influence on EHR healthcare technology adoption and their role's mandate to achieve the goal. The data collection was conducted over six months through an online secure anonymous survey tool, with only limited role identification required from the participants.
Evaluation
The survey instrument was successful in retrieving more than 60 responses from the participants. Participation was mainly targeted toward the medical staff who provide clinical services, to assess their views on the factors necessary for effective EHR adoption.
Table 2 details the summative score for each construct based on their response. For example, for the construct “complexity,” 20 of the 35 medical staff participants responded that the construct is a relevant factor for addressing and improving effective adoption. Similarly, for the construct “engagement,” none of the 15 patient participants responded that the construct has no relevance to their role to enforce and/or promote adoption. For participants in the IT staff role, constructs such as “adaptability,” “trialability,” “complexity,” “client needs/requirements,” and “regulatory policies and incentives” hold the highest relevance for effective implementation of technology interventions.
Table 2.
Summative Construct Response Distribution
| Construct | Organizational Medical Staff (50 Responses) | Organizational Information Technology Staff (14 Responses) | Patients (20 Responses) |
|---|---|---|---|
| Intervention source | 37 | 8 | 0 |
| Adaptability | 40 | 12 | 8 |
| Trialability | 31 | 12 | 7 |
| Complexity | 32 | 10 | 10 |
| Cost | 30 | 5 | 9 |
| Quality of design | 30 | 6 | 0 |
| Client requirements | 31 | 10 | 7 |
| Self-efficacy | 15 | 5 | 7 |
| Regulatory policies and incentives | 20 | 10 | 5 |
| Engagement | 20 | 2 | 2 |
| External change agents | 25 | 7 | 4 |
| Location | 25 | 10 | 8 |
| Barriers and needs | 32 | 10 | 10 |
| Organizational culture | 20 | 5 | 0 |
| Structural characteristics | 22 | 4 | 0 |
| Security changes | 30 | 10 | 0 |
| Readiness of implementation | 22 | 10 | 0 |
| Resource availability | 36 | 8 | 3 |
| Implementation climate | 35 | 5 | 0 |
| Goals and feedback | 20 | 5 | 0 |
| Relative priority | 15 | 10 | 3 |
| Resources for intervention | 33 | 7 | 0 |
| Champions | 20 | 5 | 0 |
| Leadership engagement | 30 | 7 | 0 |
| Reflecting and evaluating | 31 | 6 | 0 |
| Accountability | 35 | 5 | 3 |
| Evidence strength and quality | 20 | 8 | 0 |
| Relative advantage | 15 | 5 | 0 |
| Interoperability | 40 | 7 | 15 |
| Organizational compliance | 30 | 7 | 4 |
Note that the negative relevance identified by some participants in a given group has the potential to reduce the summative rank and score of the construct for that particular category. The survey tool enabled the researchers to analyze the data collected and identify interventions for each stakeholder group. Table 3 details the engagement barriers with priority rankings for each such group. The priority levels designed for each group are proportional to the participation ratio.
Table 3.
Engagement Barriers by Stakeholder Role and Priority Level
| Stakeholder Role | Barrier Construct | Priority Level |
|---|---|---|
| Medical staff (administrators, internal) | Adaptability, interoperability, intervention source, resource availability, implementation climate, accountability, resources for intervention, complexity, barriers and needs, trialability, client requirements, reflecting and evaluating | High (40–31) |
| Cost, quality of design, security changes, leadership engagement, organizational compliance, external change agents, location, structural characteristics, readiness of implementation | Medium (30–21) | |
| Regulatory policies and incentives, engagement, organizational culture, goals and feedback, champions, evidence strength and quality, self-efficacy, relative priority (security and privacy), relative advantage | Low (20–15) | |
| Information technology staff (management, internal) | Adaptability, trialability, complexity, client requirements, regulatory policies and incentives, location, barriers and needs, security changes, readiness of implementation, relative priority (security and privacy), resource availability, intervention source, evidence strength and quality | High (12–8) |
| External change agents, resources for intervention, leadership engagement, interoperability, organizational compliance, quality of design, reflecting and evaluating, cost, self-efficacy, organizational culture, implementation climate, goals and feedback, champions, accountability, relative advantage | Medium (7–5) | |
| Engagement, structural characteristics | Low (4–2) | |
| Patients (clients, external) | Interoperability, complexity, barriers and needs, cost, adaptability, location | High (15–8) |
| Trialability, client requirements, self-efficacy, regulatory policies and incentives, external change agents, organizational compliance, resource availability, relative priority (security and privacy), accountability | Medium (7–3) | |
| Engagement, quality of design, organizational culture, structural characteristics, security changes, readiness of implementation, implementation climate, goals and feedback, resources for intervention, champions, leadership engagement, reflecting and evaluating, intervention source, evidence strength and quality, relative advantage | Low (2–0) |
The survey tool and the analyzed results enabled the development of the five-step engagement process identified in Figure 2. Each step identifies the barriers to engagement and prompts output to design the appropriate engagement implementation. An iterative feedback loop is integrated to ensure periodic assessment of the outcomes and provide feedback for use in the tool design and analysis phase. The proposed engagement process is portable and can be applied in both inpatient and outpatient healthcare settings.
Figure 2.
Proposed Electronic Health Record Engagement Process
Discussion and Recommendations
On the basis of the areas identified as the highest priorities, the researchers developed the EHR engagement barrier model (see Figure 1). The model stratifies participant groups, highlights the areas of highest priority to support robust engagement with the EHR system, and notes preliminary recommendations to begin the process of addressing the barriers within the organization. While all the identified barriers hold importance, the focus on the shared highest-priority areas may yield the most benefit in time- and resource-limited environments; therefore, the researchers chose to leverage those specific constructs for the model.
Recommendations for Shared Engagement Barriers across All Stakeholder Groups (Adaptability, Complexity, and Barriers and Needs)
Perceptions of adaptability, complexity, and barriers and needs were noted as significant engagement barriers across stakeholder groups. Both adaptability and complexity correspond to the “intervention characteristic” domain of the CFIR. In this context, the intervention would be the EHR technology innovation purchased and/or built and utilized. Possible interventions include ensuring that all stakeholders have early input on vendor-based or in-house EHR projects via demos prior to adoption. End users (patients and medical staff) sometimes are not included in these decisions until later stages, if at all. Perceptions of complexity can be mitigated via training opportunities, particularly peer-to-peer trainings. The modified “barriers and needs” construct aligns with the CFIR “outer setting” domain. The outer setting domain frames the importance of external variables in the implementation of new processes and products. While barriers and needs may be considered end-user issues, the survey results highlight how important these issues are perceived to be from the perspective of the IT staff as well. In effort to better understand and communicate the landscape of barriers and needs, an iterative rather than a static process of needs assessment and usability testing may be a preferred approach. Additionally, greater understanding of the technology products that end users interact with regularly outside of the organization may give IT staff valuable information regarding barriers, preferred interfaces, and features to support fuller engagement.
Recommendations for Other High-Priority Engagement Barriers
Other engagement barriers of note may be those mentioned by at least two of the three stakeholder groups. The other high priority barriers noted in the current study were interoperability (patients and medical staff), intervention source (medical staff and IT staff), trialability (medical staff and IT staff), client requirements (medical staff and IT staff), resource availability (medical staff and IT staff), and location (patients and IT staff). The intervention source and trialability constructs correspond to the “intervention characteristic” domain of the CFIR, and the aforementioned recommendations to address intervention characteristics also apply. Resource availability applies to the “inner setting” domain of the CFIR. The inner setting domain encompasses the internal organizational characteristics that affect implementation of an innovation. Of note, the CFIR emphasizes resources beyond the fiscal. To enhance EHR engagement, it may be worthwhile to clarify with stakeholders which categories of resources are most important. Interoperability, client requirements, and location align most closely with the process and outer setting domains, respectively. While the focus of the current research was a fairly large suburban hospital system, the resource challenges faced when the hospital interacts with rural and distant care partners remain a concern. A lack of interoperability of EHR systems further exacerbates perceptions of the location barrier. Ensuring that health technology systems in place meet federal and regional recommendations for interoperability would mitigate this barrier. Meeting these guidelines may require federally based support resources (financial and training).
Conclusion
The researchers formulated a multistakeholder EHR engagement process model by identifying and mapping the CFIR and modifying the relevant constructs for the domain of healthcare technology. The goal was to illustrate an effective process and engagement modeling tool that could be used to quantify EHR engagement barriers. The survey results identified the focus of each participant group and informed the appropriate stakeholders of the need to provide resources to address the high-frequency constructs. The results also aided in the data-driven process of requesting external (federal and/or state) support and funding opportunities, which are needed to provide a sustainable and construct-driven iterative intervention action plan for the healthcare system. The proposed process and tool can be seamlessly replicated in any healthcare organization.
Contributor Information
Subrata Acharya, Department of Computer and Information Sciences at Towson University in Towson, MD..
Niya Werts, Department of Health Sciences at Towson University in Towson, MD..
Notes
- 1.Buntin M. B., Burke M. F., Hoaglin M. C., Blumenthal D. “Benefits of Health Information Technology: A Review of the Recent Literature Shows Predominantly Positive Results.”. Health Affairs. (2010);30(no. 3):464–471. doi: 10.1377/hlthaff.2011.0178. [DOI] [PubMed] [Google Scholar]
- 2.Fiscella K., Geiger H. J. “Health Information Technology and Quality Improvement for Community Health Centers.”. Health Affairs. (2006);25(no. 2):405–412. doi: 10.1377/hlthaff.25.2.405. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan B., Harris-Salamone K. D. “Health IT Success and Failure: Recommendations from Literature and an AMIA Workshop.”. Journal of the American Medical Informatics Association. (2009);16(no. 3):291–299. doi: 10.1197/jamia.M2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ibid.
- 5.Abbott P. A., Foster J., de Fatima Marin H., Dykes P. C. “Complexity and the Science of Implementation in Health IT—Knowledge Gaps and Future Visions.”. International Journal of Medical Informatics. (2014);83(no.7):e12–e22. doi: 10.1016/j.ijmedinf.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Ibid.
- 7.King J., Patel E., Jamoom W., Furukawa M. F. “Clinical Benefits of Electronic Health Record Use: National Findings.”. Health Services Research. (2014);49(no. 1, pt. 2):392–404. doi: 10.1111/1475-6773.12135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Irizarry T., Dabbs A. D., Curran C. R. “Patient Portals and Patient Engagement: A State of the Science Review.”. Journal of Medical Internet Research. (2015);17(no. 6):e148. doi: 10.2196/jmir.4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McGinn C. A., Grenier S., Duplantie J., Shaw N., Sicotte C., Mathieu L., Gagnon M. P. “Comparison of User Groups' Perspectives of Barriers and Facilitators to Implementing Electronic Health Records: A Systematic Review.”. BMC Medicine. (2011);9(no. 1):46. doi: 10.1186/1741-7015-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coats B., Acharya S.“Leveraging the Cloud for Electronic Health Record Access,” Perspectives in Health Information Management, January 2014, http://perspectives.ahima.org/leveraging-the-cloud-for-electronic-health-record-access/#.UyZIGoW2_QM. [PMC free article] [PubMed] [Google Scholar]
- 11.Ross J., Stevenson R., Lau J., Murray E. “Factors That Influence the Implementation of E-health: A Systematic Review of Systematic Reviews (an Update).”. Implementation Science. (2016);11(no. 1):146. doi: 10.1186/s13012-016-0510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudoir S. R., Dugan A. G., Barr C. H. “Measuring Factors Affecting Implementation of Health Innovations: A Systematic Review of Structural, Organizational, Provider, Patient and Innovation Level Measures.”. Implementation Science. (2013);8(no. 1):22. doi: 10.1186/1748-5908-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.“The CFIR Guide.” CFIR Research Team, Center for Clinical Management Research, https://cfirguide.org/ (accessed May 30, 2018).
- 14.Clinton-McHarg T., Yoong S. L., Tzelepis F., Regan T., Fielding A., Skelton E., Wolfenden L. “Psychometric Properties of Implementation Measures for Public Health and Community Settings and Mapping of Constructs against the Consolidated Framework for Implementation Research: A Systematic Review.”. Implementation Science. (2013);11(no. 1):148. doi: 10.1186/s13012-016-0512-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ross J., Stevenson R., Lau J., Murray E. “Factors That Influence the Implementation of E-health: A Systematic Review of Systematic Reviews (an Update).”. doi: 10.1186/s13012-016-0510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramsey A., Lord J., Torrey L., Marsch A., Lardiere M. “Paving the Way to Successful Implementation: Identifying Key Barriers to Use of Technology-based Therapeutic Tools for Behavioral Health Care.”. Journal of Behavioral Health Services and Research. (2016);43(no. 1):54–70. doi: 10.1007/s11414-014-9436-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Damschroder L. J., Aron D. C., Keith R. E., Kirsh S. R., Alexander J. A., Lowery J. C. “Fostering Implementation of Health Services Research Findings into Practice: A Consolidated Framework for Advancing Implementation Science.”. Implementation Science. (2009);4(no. 1):50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richardson J. E., Abramson E. L., Pfoh E. R., Kaushal R., HITEC Investigators “Bridging Informatics and Implementation Science: Evaluating a Framework to Assess Electronic Health Record Implementations in Community Settings.”. AMIA Annual Symposium Proceedings. (2012):770. [PMC free article] [PubMed] [Google Scholar]
- 19.Rogers E. Diffusion of Innovations. New York: Simon and Schuster; 2010. [Google Scholar]
- 20.Damschroder L. J., Aron D. C., Keith R. E., Kirsh S. R., Alexander J. A., Lowery J. C. “Fostering Implementation of Health Services Research Findings into Practice: A Consolidated Framework for Advancing Implementation Science.”. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.“The CFIR Guide.”
- 22.Ross J., Stevenson R., Lau J., Murray E. “Factors That Influence the Implementation of E-health: A Systematic Review of Systematic Reviews (an Update).”. doi: 10.1186/s13012-016-0510-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.“The CFIR Guide.”
- 24.“The CFIR Guide.” [Google Scholar]
- 25.Kaplan B., Harris-Salamone K. D. “Health IT Success and Failure: Recommendations from Literature and an AMIA Workshop.”. doi: 10.1197/jamia.M2997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Irizarry T., Dabbs A. D., Curran C. R. “Patient Portals and Patient Engagement: A State of the Science Review.”. doi: 10.2196/jmir.4255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McGinn C. A., Grenier S., Duplantie J., Shaw N., Sicotte C., Mathieu L., Gagnon M. P. “Comparison of User Groups' Perspectives of Barriers and Facilitators to Implementing Electronic Health Records: A Systematic Review.”. doi: 10.1186/1741-7015-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Acharya S., Werts N.“Guiding Healthcare Adoption Implementation via the Consolidated Framework Approach,” The 22nd Colloquium for Information Systems Security Education, June, 2018. [Google Scholar]
- 29.“The CFIR Guide.”